Supplemental Digital Content is available in the text.
Abstract
Introduction:
There has been a recent interest in injecting large body and face areas with local anesthetic in a minimally painful manner. The method includes adherence to minimal pain injection details as well feedback from the patient who counts the number of times he feels pain during the injection process. This article describes the successes and limitations of this technique as applied to primary cleft lip/nasal repair in grown patients.
Methods:
Thirty-two primary cleft lip patients were injected with local anesthesia by 3 surgeons and then underwent surgical correction of their deformity. At the beginning of the injection of the local anesthetic, patients were instructed to clearly inform the injector each and every time they felt pain during the entire injection process.
Results:
The average patient felt pain only 1.6 times during the injection process. This included the first sting of the first 27-gauge needle poke. The only pain that 51% of the patients felt was that first poke of the first needle; 24% of the patients only felt pain twice during the whole injection process. The worst pain score occurred in a patient who felt pain 6 times during the injection process. Ninety-one percent of the patients felt no pain at all after the injection of the local anesthetic and did not require a top-up.
Conclusion:
It is possible to successfully and reliably inject local anesthesia in a minimally painful manner for cleft lip and nasal repair in the fully grown cleft patient.
Cleft lip/nasal repair is ideally performed during infancy, but in many countries, this is not always possible. When these children become fully grown, many are being repaired under local anesthesia. The pain of traditional local anesthetic injection for the repair of cleft lip/nasal deformity can be significant because of the great sensitivity of this region of the face and the large area that needs to be infiltrated. There has been a recent interest in injecting large body and face areas with local anesthetic in a minimally painful manner with tumescent local anesthesia. The technique has been used in hand surgery1 and can be reliably taught to medical students and residents.2
This article describes this minimal pain tumescent local anesthetic injection technique as applied to wide awake primary cleft lip/nasal repair in grown patients.
MATERIALS AND METHODS
In August 2013, at an Operation Smile mission in Lilongwe, Malawi, 32 adult patients were scheduled for repair of cleft lip/nasal deformity under local anesthesia. To minimize the pain of local anesthetic injection for these patients, the 3 surgeons who injected the patients used the recently described minimal pain injection technique in which the patient may only feel the first sting of the first needle entry site, even when large areas are injected.3 This article is an observational descriptive analysis of what we found when we counted how many times patients felt pain during the minimal pain tumescent local anesthetic injection process.
The inclusion criteria for this technique were age older than 12 with unilateral complete or incomplete deformity. The patients had to have the ability to understand and tolerate the procedure under local anesthesia. If they were not able to communicate, a competent interpreter had to be present. Parents consented to the surgery for patients who were not of Malawi age of consent. Exclusion criteria included wide complete cleft lip with an obvious need for extensive periosteal undermining.
The following demographic information and outcome data were collected: age, sex, ability to speak English, technique of repair, volume of local anesthetic administered, time taken to administer the local anesthesia, number of times the patient felt pain during local anesthetic injection, and the need for intraoperative additional local anesthesia.
Method of Local Anesthetic Injection and Pain Scoring
The patients were injected as they lay on a stretcher outside the operating room. The timing of the injections was such that a minimum of 30 minutes would elapse between the end of the injection and the beginning of surgery to allow the lidocaine and epinephrine time to work effectively. (See Video 1, Supplemental Digital Content 1, which shows how to inject minimally painful local anesthesia for the primary cleft lip and nasal repair in fully grown patients. This video is available in the “Related Videos” section of the full-text article on PRSGO.com or available at http://links.lww.com/PRSGO/A35.)
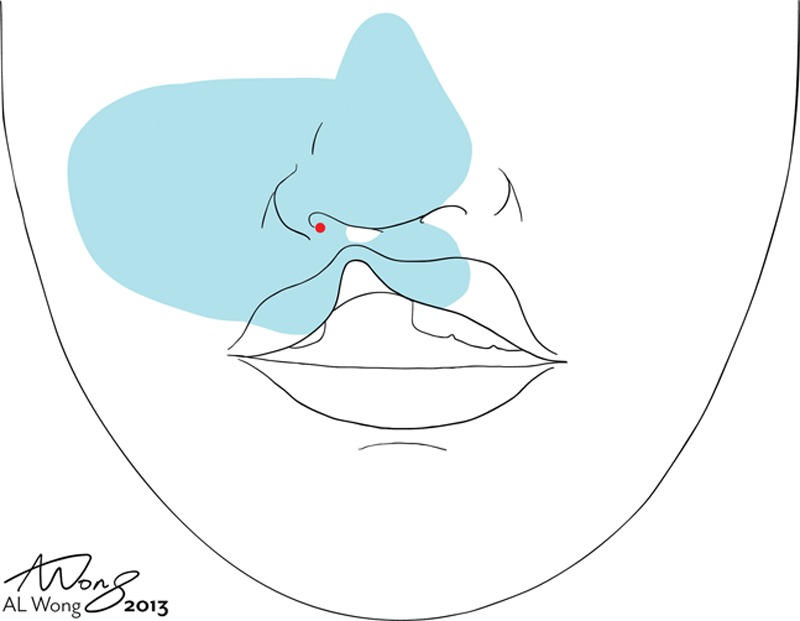
Fig. 1.
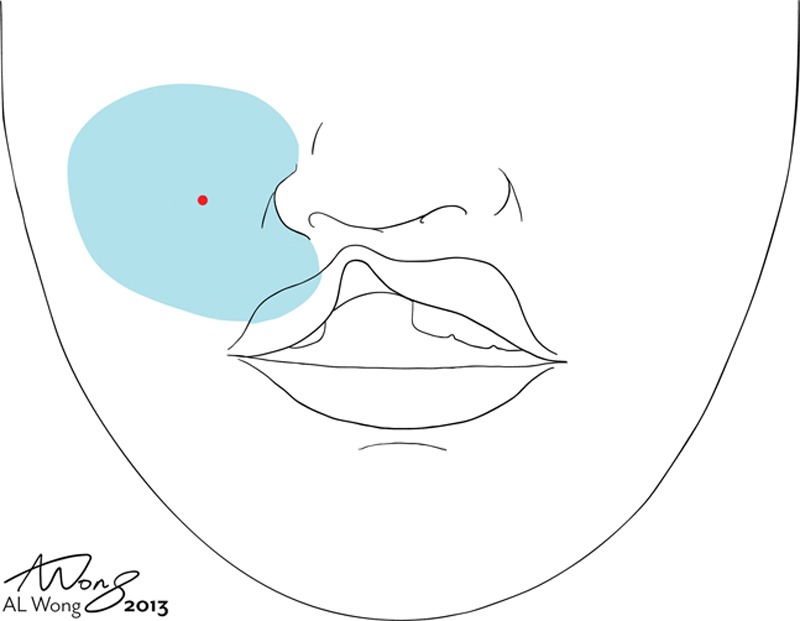
First injection: We started injecting under the dermis in the cleft side cheek midway between the infraorbital nerve and the base of the ala. After the needle site was numb, we very slowly injected an additional 2–5 ml without moving the needle at all to anesthetize all involved branches of the infraorbital nerve.
Video 1.

See Video 1, Supplemental Digital Content 1, which shows how to inject minimally painful local anesthesia for the primary cleft lip and nasal repair in fully grown patients. This video is available in the “Related Videos” section of the full-text article on PRSGO.com or available at http://links.lww.com/PRSGO/A35.
A mixture of 1% lidocaine with 1:100,000 epinephrine was injected with 0.5-inch 27-gauge needles, as this was all that was available to us in a small bore needle. Each 10 ml of local anesthetic was buffered with 1 ml of 8.4% bicarbonate.4 We always kept the total dosage of lidocaine with epinephrine below 7 mg/kg, which has been shown to be very safe.5
For the first injection, the syringe was stabilized with 2 hands, and the thumb was ready on the plunger before the needle penetrated the skin to minimize painful needle wobbling movement until the needle site was numb. The patient was warned to hold still to prevent accidental withdrawal which would require a second stick. The needle was inserted as perpendicularly as possible. As soon as the needle tip was just below the dermis, a visible amount of local anesthesia (0.2–0.5 ml) was injected until it could be seen as a 0.3–0.5 mm wheal encircling the needle. The injection was then paused and the needle immobilized. The patient was addressed and asked to tell us when the pain of the needle sting was completely gone. After a minimum of 15 seconds after the pain was gone, the patient was asked to tell the injector each and every time he or she felt any additional pain events during the injection process.
If the patient only felt pain of the first needle poke, the injector scored a hole-in-one, as in the game of golf. If the patient felt patient twice during the injection process, the score was an eagle. Three pain events scored a birdie, 4 scored a bogie, 5 a double bogie, and so on. Each time the patient felt a pain event, the injector would wait until the pain was completely gone before proceeding.
We started injecting under the dermis in the cleft side cheek midway between the infraorbital nerve and the base of the ala. After the needle site was numb, we very slowly injected an additional 2–5 ml without moving the needle at all to anesthetize all involved branches of the infraorbital nerve. We avoided needle laceration of the nerve itself by never inserting the needle into the infraorbital foramen (Fig. 1).
We then angled the needle parallel to and just under the skin. We injected very slowly antegradely as we gradually advanced the needle medially to numb up the lateral nasal sidewall. We were careful to always have at least 1 cm of palpable or visible local anesthesia ahead of the sharp needle tip. We tried very hard to never let the tip hit unanesthetized nerves to preserve a good pain score.
We then pulled the needle back and redirected it toward the lip, again injecting slowly ahead of the needle tip, always palpating with our noninjecting fingertips and looking at the skin to be sure the local was expanding the subcutaneous tissue well ahead of the potentially painful needle tip.
We then reinserted the needle at the lateral nasal sidewall base to numb up the lateral nasal dorsum and lateral tip (Fig. 2). Every time the needle was withdrawn and reinserted into the skin, we were careful to insert the needle least 1 cm inside the edge of skin that was clearly white with epinephrine or swollen with palpable local anesthetic fluid tumesced under the skin.
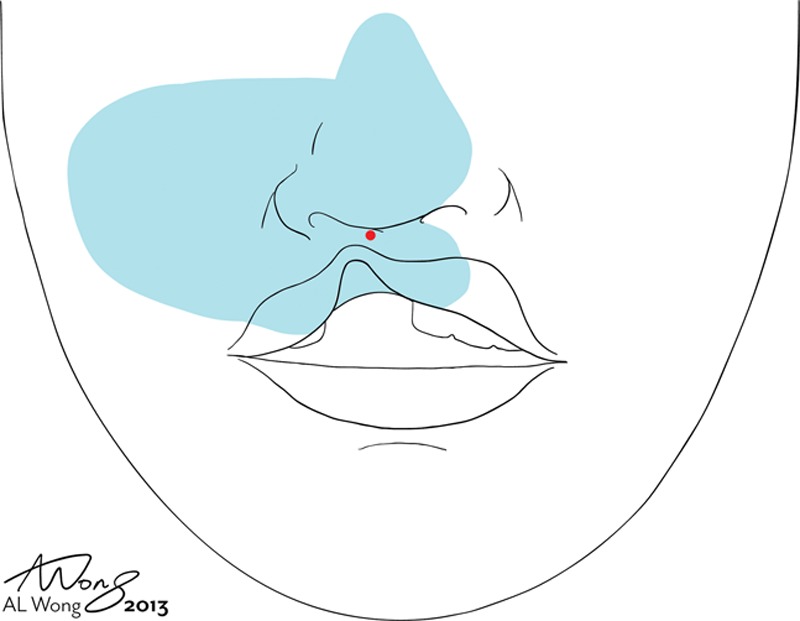
Fig. 2.
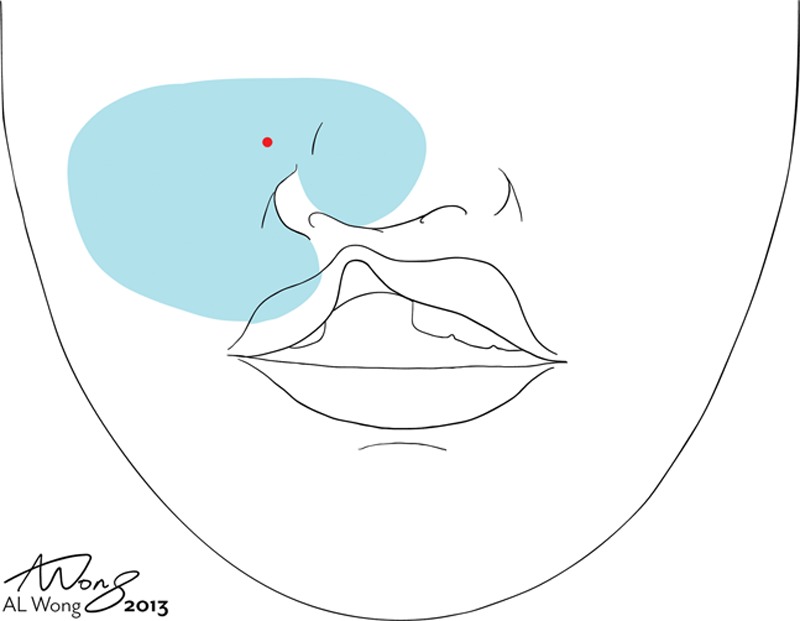
Lateral nasal injection: We then angled the needle parallel to and just under the skin. We injected very slowly antegradely as we gradually advanced the needle medially to numb up the lateral nasal sidewall and lateral nasal tip. We were careful to always have at least 1 cm of palpable or visible local anesthesia ahead of the sharp needle tip.
We alternated between lip and nose needle reinsertions to give time for the local anesthesia to numb up reinsertion sites (Figs. 3–5). Simonart’s band of the cleft was crossed very slowly as we were getting into a new unanesthetized nerve distribution across the cleft. After the needle tip had crossed the band, we injected 2–4 ml local anesthesia very slowly on the noncleft side without moving the needle. We felt and saw the base of the columella tumescence before coming down the columella from above. The nasal floor was anesthetized on both sides of the cleft with the needle slowly approaching and finally touching the bone to allow periosteal dissection inside the nose wherever an elevator was to be used (Figs. 6, 7).
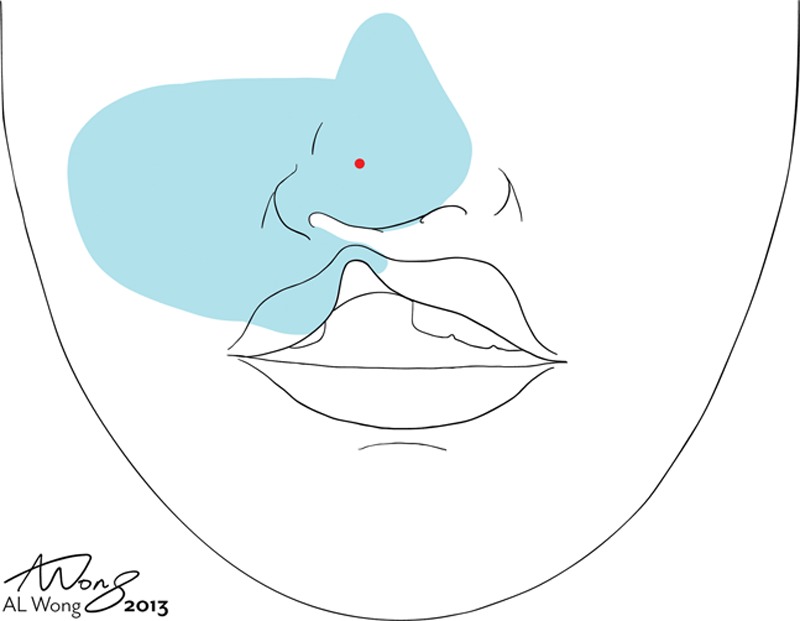
Fig. 3.
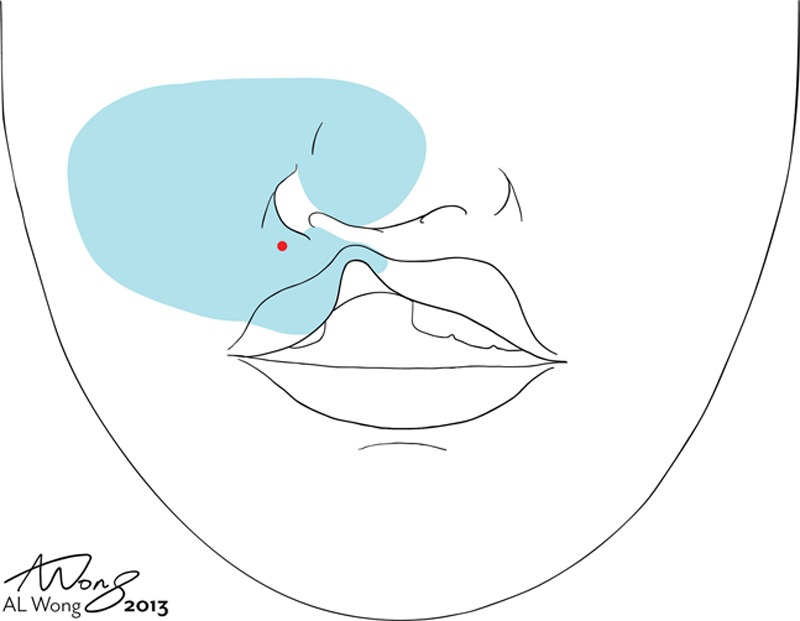
Lateral lip injection: We reinserted the needle in numb skin of the lateral lip, injecting slowly ahead of the needle tip, always palpating with our noninjecting fingertips and looking at the skin to be sure the local was expanding the subcutaneous tissue well ahead of the potentially painful needle tip.
Fig. 5.
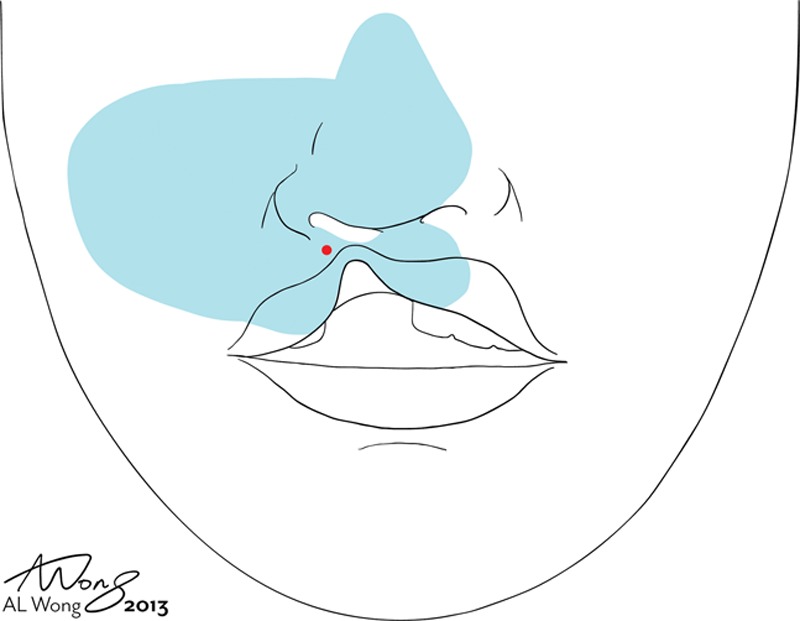
Simonart’s band of the cleft was crossed very slowly as we were getting into a new unanesthetized nerve distribution across the cleft. After the needle tip had crossed the band, we injected 2–4 ml very slowly on the noncleft side without moving the needle.
Fig. 6.
The lateral nasal floor was anesthetized with the needle slowly approaching and finally touching the bone to allow periosteal dissection inside the nose wherever an elevator was to be used, and 3–4 ml was liberally injected to get the whole lateral floor and sidewall below the turbinates.
Fig. 7.
The medial nasal floor and septal mucosa were infiltrated as required, as was the lateral nasal floor. All areas to be dissected were liberally tumesced.
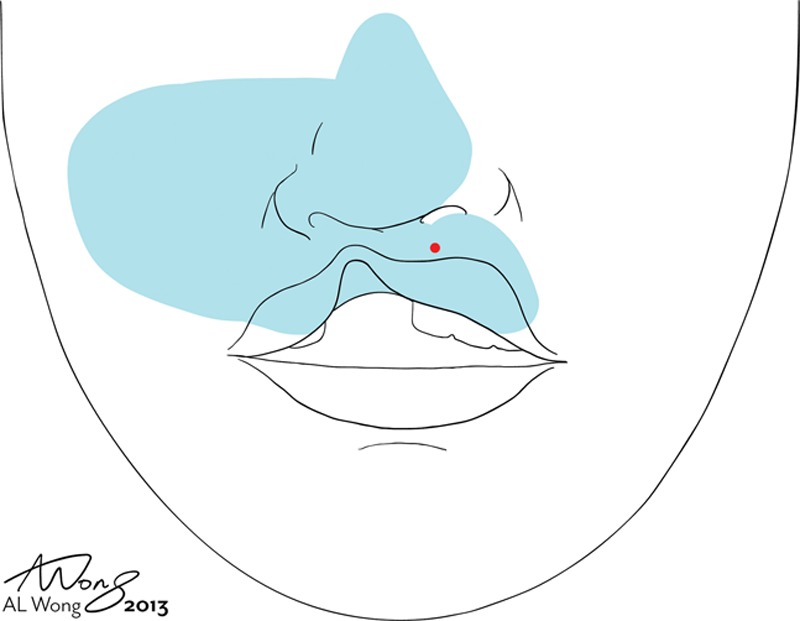
Fig. 4.
Nasal tip: We reinserted the needle in the numb lateral nasal tip. When the correct plane between the fat and the perichondrium was infiltrated, the whole nasal tip blanched with 2–3 ml of tumescent local anesthesia.
We reinserted the needle in the numb skin of the noncleft medial lip to finish tumescing the medial lip as we had done for the lateral lip (Fig. 8). The adherent alar skin and columella were anesthetized last, so the tissues surrounding them had time to get numb. The needle traversed the alar cartilage to tumesce the mucosa beneath the ala and the upper lateral cartilage. At the end, all areas to be dissected had at least 1 cm of local beyond their borders, so no further injections (top-ups) would be required intraoperatively.
Fig. 8.
Medial lip: We reinserted the needle in the numb skin of the noncleft medial lip to finish tumescing the medial lip, as we had done for the lateral lip.
After injection of the nasal soft tissues and nasal periosteum, if periosteal dissection of the nasal floor was to be extensive, we also numbed the oral side of the hard palate from inside the mouth.
RESULTS
Thirty-two primary cleft lip patients were injected with local anesthesia and then underwent surgery. There were 14 male and 18 female patients. There were 15 left incomplete cleft lip repairs, 13 right unilateral incomplete lip repairs, 3 left complete cleft lip repairs, and a single midline cleft repair. The mean age was 22 years (range, 14–49 years). The overall, mean total volume of local anesthetic administered was 27 ml (range, 15–40 ml). The mean time to administer local anesthetic was 21 minutes (range, 10–45 minutes) (Fig. 9).
Fig. 9.
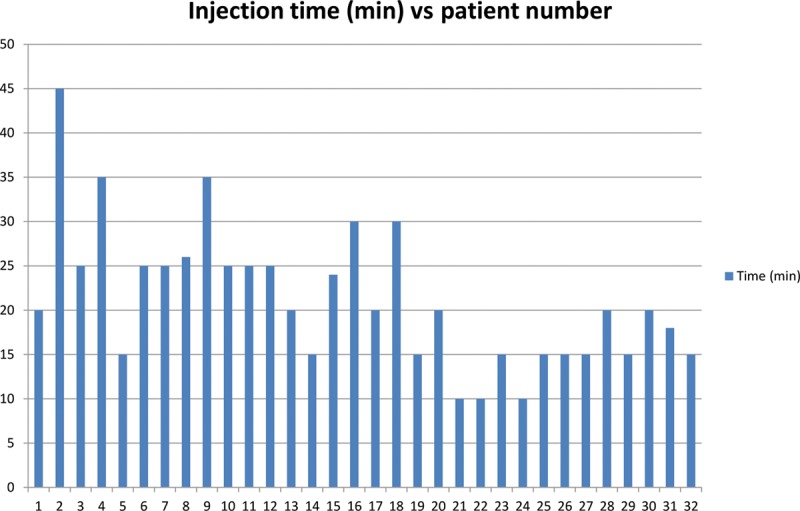
Injection time vs patient number. It can be seen that the injection times were higher early in the week at the front end of the learning curve of injection technique. The first 10 patients had the longest injection times. The last 10 patients had the shortest injection times.
Eighteen patients (51%) felt pain only once during the injection process (hole-in-one). Seven patients (24%) felt pain twice (eagle). Five patients (17%) felt pain 3 times (birdie). One patient felt pain 4 times (bogie). One felt pain 6 times (triple bogie) (Fig. 10).
Fig. 10.
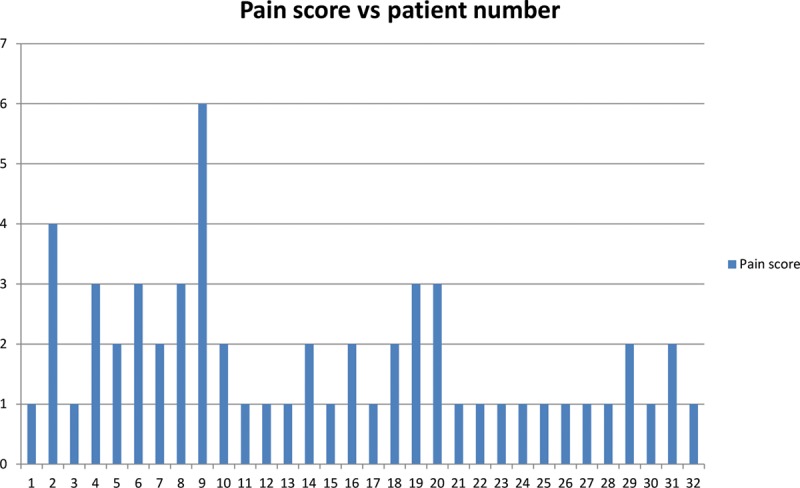
Pain score vs patient number. It can be seen that the pain numbers were higher (patients felt pain a greater number of times) early in the week at the front end of the learning curve of injection technique. It can be seen that the pain scores were higher early in the week at the front end of the learning curve of injection technique. The first 10 patients had the highest pain scores (felt pain more times). The last 11 patients (21–32) all scored an eagle (pain score = 2) or a hole-in-one (pain score = 1).
The only intraoperative additional local anesthetic injection that was required were the 3 left unilateral complete cleft lip patients who required top-up for dissection of their nasal floor. Ninety-one percent of the patients (29 of 32) felt no surgical pain at all after the injection of the local anesthetic.
DISCUSSION
This article describes how we injected local anesthetic in a minimally painful manner in 32 consecutive adult cleft lip repairs. The average patient felt pain only 1.6 times during the injection process in this series. Fifty-one percent of the patients only felt the first poke of the first needle with the injector scoring a hole-in-one. The injectors scored an eagle in 24% of the patients feeling pain only twice during the whole injection process of the time. In other words, 75% of the patients only felt the sting of a 27-gauge needle either only once or twice during the whole injection process. Ninety-one percent of the patients felt no pain at all after the injection of the local anesthetic and did not require a top-up.
This was a remarkably low pain number for the following reasons: (1) Although the process of minimal pain injection had been worked out for operations such as carpal tunnel and facial cosmetic/reconstructive procedures,1,3,6,7 this was our first attempt at using the hole-in-one approach for cleft lip and nasal repair in this very large and sensitive area of the face. (2) The local anesthesia was performed by 3 different surgeons, 2 of whom had never used the hole-in-one approach before. (3) We only had short (1/2 inch) 27-gauge needles available to us in Malawi. This meant that we had to reinsert the needle more often than we would have if we had been able to use the usual longer 1¼ inch 30-gauge needles we would have preferred for this process. Each time a needle is reinserted, a possible pain event may occur if the surgeon does not put the needle in a clearly numbed area. Longer needles would have likely improved our pain scores.
As the 3 injecting surgeons gained experience over the 5 days of surgery, the pain scores improved, as did the speed of injection. The usual cause of a high pain score was injecting or advancing the needle too rapidly or reinserting the needles in an area still not numb. The only intraoperative additional local anesthetic injection that was required were the 3 LUCCL patients who required top-up for dissection of their nasal floor. As this became apparent as the surgical week progressed, we began to inject the oral side of the hard palate from inside the mouth in patients who required periosteal undermining.
The principles of minimal pain local anesthesia have been published with drawings and videos.3 To summarize, in order to minimize the pain of local anesthetic injection, consider (1) buffering 1% lidocaine and 1:100,000 epinephrine with 8.4% bicarbonate at a 10:1 concentration; (2) warming the local anesthetic; (3) distracting the patient (music and soft conversation) or the area of injection (gentle pinch and pressure); (4) using smaller 27- or 30-gauge needles; (5) stabilizing the syringe to avoid needle wobble until the needle puncture site is numb; (6) injecting 0.5 ml perpendicularly subdermally and pausing until the patient says the needle pain is gone; (7) injecting an additional 2 ml before moving the needle and then moving antegrade very slowly with 1 cm of local always palpable or visible ahead of the needle (blow slow before you go…); (8) reinserting needles within 1 cm of blanched or tumesced areas; (9) tumescing more local anesthesia than you need is better than not using enough (top-ups are bad and tumescence is good); and (10) most importantly, learning from each patient you inject by asking them to score you by telling you each time they feel pain after the first needle poke. (See Video 1, Supplemental Digital Content 1, which shows how to inject minimally painful local anesthesia for the primary cleft lip and nasal repair in fully grown patients. This video is available in the “Related Videos” section of the full-text article on PRSGO.com or available at http://links.lww.com/PRSGO/A35.)
The surgical flow with these 32 cases was very efficient. The average turnover time was approximately 10 minutes between the local anesthetic cleft lip/nasal repair procedures. The patients were injected as they lay on a stretcher outside the operating room waiting for their surgery. The timing of the injections was such that a minimum of 30 minutes would elapse between the end of the injections and the beginning of surgery to allow the lidocaine and epinephrine time to work effectively. There is recent level I evidence that it takes a mean of 26 minutes after injection of epinephrine before the maximal vasoconstriction effect occurs, not the frequently quoted 7 minutes.8
There are few studies in the literature describing the use of pure local anesthesia for cleft lip surgery.9–11 Eberlin et al9 reported primary cleft lip repair and primary rhinoplasty on 22 adolescents/adults under pure local anesthesia in 2003. After ethyl chloride spray, they all received infraorbital12 and external nasal nerve blockade13 and 5–10 ml of subcutaneous infiltration for the epinephrine effect. Ahmad10 also described cleft lip repair under local anesthesia in 39 adults in 2008. He used lidocaine 1% with epinephrine 1:200,000 as infiltration. In 2006, Eipe et al14 reported their experience with 20 patients who had cleft lip repair under infraorbital nerve block. Hodges and Hodges15 reviewed 336 cleft lip repairs in Uganda in 2000. Those who became anxious were given a small dose of ketamine. Naushad16 reported on 13 adult males with cleft lip had procedures under local anesthesia in 1999. None of the previous authors asked the patients to count the number of times they felt pain during the injection process as we did in this study.
We feel that the golf analogy (patient feels pain once = hole-in-one, pain twice = eagle, pain 3 times = birdie, etc) is very important for 2 reasons. First, most surgeons are inherently competitive and want to improve their score in most endeavors in which they are actually scored. We have observed that medical students and residents want to improve their injection pain scores,2 and the patients become the beneficiaries of this gamesmanship. Second, this approach sets up a situation whereby surgeons get immediate feedback and evaluation by the patient on the quality of their injection technique. Each patient becomes an opportunity for the injector to get better and better at minimal pain local anesthetic injection instead of being a lost opportunity.
In this study, the cleft lip repairs were performed by 5 different surgeons on the 5 different operating days. The surgeons who had not previously used tumescence for their cleft repairs were concerned that the tissue distortion may make the lip repair more difficult. By the end of their day of local cases, they were all pleased that this was not an issue for 4 main reasons. First, much of the local anesthesia fluid diffuses out of the wound when dissection is performed. Second, much of the rest of the local is absorbed by the end of the case when the skin is closed. Third, the local is injected symmetrically so the tissues are symmetrically swollen. Fourth, targets such as the lip vermillion cutaneous junction are easier to hit as they are expanded. By the end of the case, the visibility of symmetrical closure was felt to be very acceptable by all 5 surgeons.
Limitations
This technique is not applicable to patients who are too young to understand or comply with local anesthetic injection. It is also not possible without the presence of a good, calm interpreter if the surgeon does not speak the language of the patient. The injecting surgeon needs to be patient and willing to invest an average of 20 minutes. The surgeon also needs to become comfortable with the repair of the cleft lip/nasal deformity in the presence of tissue tumescence.
CONCLUSIONS
In summary, this article and its film describe how to successfully inject local anesthesia in a minimally painful manner for cleft lip and nasal repair in the fully grown cleft patient. The technique was taught to young surgeon injectors who were able to consistently get low pain scores in 32 grown cleft lip/nasal repair patients.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Lalonde DH. “Hole-in-one” local anesthesia for wide-awake carpal tunnel surgery. Plast Reconstr Surg. 2010;126:1642–1644. doi: 10.1097/PRS.0b013e3181f1c0ef. [DOI] [PubMed] [Google Scholar]
- 2.Farhangkhoee H, Lalonde J, Lalonde DH. Teaching medical students and residents how to inject local anesthesia almost painlessly. Can J Plast Surg. 2012;20:169–172. doi: 10.1177/229255031202000315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strazar AR, Leynes PG, Lalonde DH. Minimizing the pain of local anesthesia injection. Plast Reconstr Surg. 2013;132:675–684. doi: 10.1097/PRS.0b013e31829ad1e2. [DOI] [PubMed] [Google Scholar]
- 4.Frank SG, Lalonde DH. How acidic is the lidocaine we are injecting, and how much bicarbonate should we add? Can J Plast Surg. 2012;20:71–73. doi: 10.1177/229255031202000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burk RW, 3rd, Guzman-Stein G, Vasconez LO. Lidocaine and epinephrine levels in tumescent technique liposuction. Plast Reconstr Surg. 1996;97:1379–1384. doi: 10.1097/00006534-199606000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Mustoe TA, Buck DW, 2nd, Lalonde DH. The safe management of anesthesia, sedation and pain in plastic surgery. Plast Reconstr Surg. 2010;126:165e–176e. doi: 10.1097/PRS.0b013e3181ebe5e9. [DOI] [PubMed] [Google Scholar]
- 7.Lalonde DH, Wong A. Dosage of local anesthesia in wide awake hand surgery. J Hand Surg Am. 2013;38:2025–2028. doi: 10.1016/j.jhsa.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 8.McKee DE, Lalonde DH, Thoma A, et al. Optimal time delay between epinephrine injection and incision to minimize bleeding. Plast Reconstr Surg. 2013;131:811–814. doi: 10.1097/PRS.0b013e3182818ced. [DOI] [PubMed] [Google Scholar]
- 9.Eberlin KR, Vyas RM, Abi-Haidar Y, et al. Adult cleft lip repair under local anesthesia: an effective technique in resource-poor settings. Cleft Palate Craniofac J. 2013;50:59–63. doi: 10.1597/11-256. [DOI] [PubMed] [Google Scholar]
- 10.Ahmad M. Cleft lip repair under local anesthesia in adults. J Surg Pakistan (Int) 2008;13:170–172. [Google Scholar]
- 11.Salloum ML, Eberlin KR, Sethna N, et al. Combined use of infraorbital and external nasal nerve blocks for effective perioperative pain control during and after cleft lip repair. Cleft Palate Craniofac J. 2009;46:629–635. doi: 10.1597/08-142.1. [DOI] [PubMed] [Google Scholar]
- 12.Rajamani A, Kamat V, Rajavel VP, et al. A comparison of bilateral infraorbital nerve block with intravenous fentanyl for analgesia following cleft lip repair in children. Paediatr Anaesth. 2007;17:133–139. doi: 10.1111/j.1460-9592.2006.02032.x. [DOI] [PubMed] [Google Scholar]
- 13.Han SK, Shin YW, Kim WK. Anatomy of the external nasal nerve. Plast Reconstr Surg. 2004;114:1055–1059. doi: 10.1097/01.prs.0000135335.60575.d9. [DOI] [PubMed] [Google Scholar]
- 14.Eipe N, Choudhrie A, Pillai AD, et al. Regional anesthesia for cleft lip repair: a preliminary study. Cleft Palate Craniofac J. 2006;43:138–141. doi: 10.1597/05-025.1. [DOI] [PubMed] [Google Scholar]
- 15.Hodges AM, Hodges SC. A rural cleft project in Uganda. Br J Plast Surg. 2000;53:7–11. doi: 10.1054/bjps.1999.3238. [DOI] [PubMed] [Google Scholar]
- 16.Naushad MAB. Day care surgery for cleft lip in adults. J Surg Pakistan. 1999;4:23–24. [Google Scholar]


