Abstract
The University of Zimbabwe College of Health Sciences (UZCHS) is Zimbabwe's premier health professions training institution. However, several concerns were raised during the past decade over the quality of health education at UZCHS. The number of faculty and students declined markedly until 2010, when there was a medical student intake of 147 while the faculty comprised only 122 (39%) of a possible 314 positions. The economic and political crises that the country experienced from 1999 to 2009 compounded the difficulties faced by the institution by limiting the availability of resources. The Medical Education Partnership Initiative (MEPI) funding opportunity has given UZCHS the stimulus to embark on reforms to improve the quality of health education it offers. UZCHS, in partnership with the University of Colorado School of Medicine (UCSOM), the University of Colorado Denver Evaluation Center (UCDEC), and Stanford University designed the Novel Education Clinical Trainees and Researchers (NECTAR) program to implement a series of health education innovations to meet this challenge. Between 2010 and 2013, innovations that have positively affected the quality of health professions education at UZCHS include the launch of comprehensive faculty development programs and mentored clinical and research programs for postgraduate students. A competency-based curriculum reform process has been initiated; a health professions department has been established; and the Research Support Center has been strengthened, providing critical resources to institutionalize health education and research implementation at the college. A core group of faculty trained in medical education has been assembled, helping to ensure the sustainability of these NECTAR activities.
The medical school at the University of Zimbabwe was established as an affiliate to the University of Birmingham, United Kingdom, in 1963 as a bachelor of medicine and bachelor of surgery (MB ChB) program. The school initially produced approximately 20 doctors annually for a population of 4.1 million.1 Student admissions gradually increased, reaching a height of 212 in 2007 when the institution became the University of Zimbabwe College of Health Sciences (UZCHS), training a variety of health professionals (doctors, pharmacists, dentists, nurses, rehabilitation practitioners, and laboratory scientists) to serve the country's 13 million people.
As a result of the nation's 1999-2009 economic and political crises, the medical student intake in 2010 dropped to 147 (70%). The student failure rate increased from 15% in the 1990s to 45% for first-time MB ChB exam-takers in 2010. That year, of the 314 faculty positions available at UZCHS, only 122 (39%) were filled. Resources and academic support deteriorated dramatically, prompting many students to seek postgraduate training abroad. In 2009, only 3 out of 16 (19%) of the available internal medicine positions for the postgraduate master's in medicine (MMed) program were filled. The limited number of faculty further resulted in the neglect of curriculum reform and inconsistent faculty development. Limited financial and infrastructure support resulted in poor library resources, inadequate teaching aids, poor Internet access, and limited information and communication technology (ICT) resources for both students and faculty.
MEPI and NECTAR
The Novel Education Clinical Trainees and Researchers program (NECTAR) was crafted in 2010 by a partnership of UZCHS, University of Colorado Denver Evaluation Center (UCDEC), University of Colorado School of Medicine (UCSOM), and Stanford University in response to the Medical Education Partnership Initiative (MEPI) funding opportunity.2, 3 In addition to the programmatic NECTAR award, UZCHS was awarded two linked awards in 2010 to pursue cardiovascular and mental health research objectives.
A key requirement of the MEPI award was the development of partnerships and consortia as well as collaboration with in-country ministries of health and education. Building on the longstanding collaboration between the Ministry of Higher and Tertiary Education, Science, and Technology Development and the Ministry of Health and Child Care to train health professionals, NECTAR developed a seven-member consortium to help achieve its objectives (Figure 1). NECTAR's goals are to increase the number and improve the proficiency of UZCHS medical graduates; improve the retention of graduates to serve as faculty and practitioners in both urban and rural settings; and strengthen research capacity.
Figure 1.
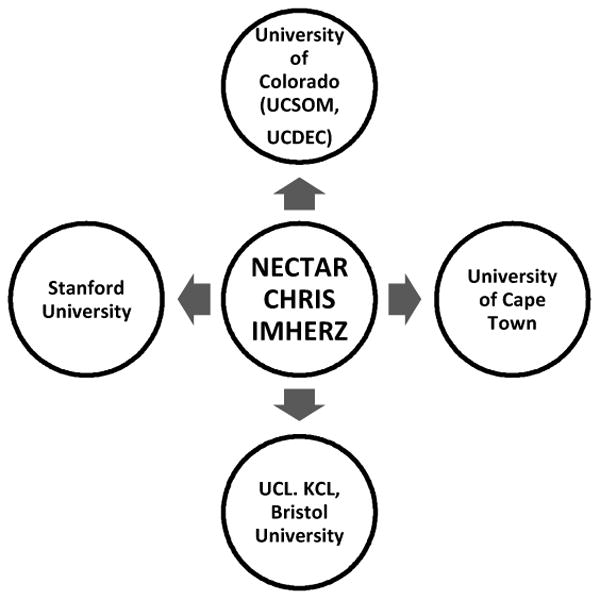
NECTAR (Novel Education Clinical Trainees and Researchers); CHRIS (Cerebrovascular Heart failure, Rheumatic heart disease Interventions Strategy); IMHERZ (Improving Mental Health Education and Research Capacity in Zimbabwe); UCSOM (University of Colorado, School of Medicine), UCDEC (University of Colorado Denver, Evaluation Center), Stanford University (Stanford University), UCL (University College London); KCL-IOP (Kings College, London-Institute of Psychiatry).
NECTAR launched a multi-pronged approach that included:
Faculty development to ensure a critical mass of trained medical educators;
Training MMeds in education and research skills;
Development of a comprehensive competency-based curriculum;
Improvements in infrastructure to support these initiatives.
This paper highlights the recent transformative innovations and reforms that UZCHS has undertaken to improve the quality of health professions education at the College since receiving MEPI funding in 2010.
Program Description
Faculty development
Like medical schools elsewhere, UZCHS lecturers were recruited on the basis of their subject matter knowledge. Teaching, university service, and publications were attributes used for promotion with little regard to the individual's training in or ability to teach.4 Extensive faculty development was needed for successful implementation of the initiatives proposed. Faculty agreed that curriculum change was their responsibility. A critical mass of faculty was deemed necessary to train as change agents. Two programs were developed: a core program for all faculty and an intensive program for faculty who were identified as potential leaders of the curriculum reform process.
During NECTAR's first three years (2010 to 2012), eight two- to three-day faculty development workshops were offered to all faculty members (Table 1). Topics were identified by the faculty development committee with a combined UZCHS, UCSOM, and UCDEC team. The first workshop was attended by 69/122 (56%), and by the eighth workshop, 139/188 (74%) of the faculty had attended at least one workshop. In exit questionnaires following each workshop, nearly all respondents indicated that the sessions were “helpful” and “relevant” and that they planned to implement what they had learned. In the 2013 survey of UZCHS faculty, all 50 of the respondents “agreed” or “strongly agreed” that they will incorporate faculty development learning into their practice.
Table 1. Faculty Development and Mentored Clinical Scholars Program Workshop Topics.
| Date | Faculty Development Topics | Mentored Clinical Scholars Topics |
|---|---|---|
| July 2011 | Principles of curriculum development, teaching methods, learner assessment | None |
| November 2011 | Student assessment: multiple choice question (MCQ) development, direct observation, feedback, and global assessment | None |
| March 2012 | Adult learning principles, teaching/learner contact, assessing clinical skills, teaching procedures | Learning styles, professional ethics, team management, assessment, and feedback |
| August 2012 | Clinical reasoning, effective feedback, clinical teaching, teaching procedures | Stress management and life skills, self-directed learning, formal presentations |
| December 2012 | Writing goals and objectives, large group instruction, presentation skills, professional and ethical behavior | Standardization and principles of teaching procedures, end-of-life care, death and dying, evidence-based medical decision-making |
| March 2013 | Team-based learning (TBL): writing objectives, MCQs, and TBL modules | Physician/surgeon self-care, understanding and communicating prognosis, understanding caregiver needs, grief and bereavement |
| July 2013 | MCQ development; competency-based curriculum reform | Evidence-based practice, library search skills, critical appraisal, Myers-Briggs and personality types |
| October 2013 | Using simulation and standardized patients for teaching and assessment | Professional standards and medico-legal system in Zimbabwe, informed consent, patient safety, errors in medical-surgical care |
At the early planning stage of NECTAR, it was felt that a core group of specially trained education leaders was necessary to lead NECTAR educational initiatives and ensure their sustainability beyond MEPI funding. Four faculty members were trained through the Sub-Saharan Africa FAIMER (Foundation for Advancement of International Medical Education and Research) Regional Institute fellowship program, SAFRI, South Africa.5 However, annual program evaluation data suggested that more-rapid training of larger cohorts of faculty in curriculum development and educational leadership was needed. Moreover, UZCHS leaders believed this training should occur locally rather than online or abroad because of faculty shortages and limited funding.
Thus, in 2012, the Health Education Advanced Leadership for Zimbabwe (HEALZ) program was developed by UCSOM, UCDEC, and UZCHS. HEALZ is a one-year program of rigorous course work delivered face-to-face in three intensive week-long sessions. Content is based on the curriculum development training of David Kern and colleagues.6 During the first session, scholars learn to conduct a needs assessment and the basics of quantitative and qualitative research methods. Between the first and second sessions, scholars develop and implement the assessment in their areas of curricular interest. During the second session, they learn to analyze needs assessment data and develop their curriculum. Lessons on developing competencies, goals, and objectives; using educational strategies and learner assessments; and program evaluation are included. By the third session, scholars analyze their needs assessment data and develop draft curriculum. During the final session, they focus on project implementation, leadership skills, and change management. Scholars are expected to implement their curriculum through appropriate processes including assessing its effectiveness and acceptability. For ongoing support, scholars are assigned to a mentoring triangle consisting of a local and a distance mentor who provide content and methodology expertise. 7 Final projects are presented as posters at the HEALZ graduation ceremony.
To date, HEALZ scholars represent 20 of the 23 departments within UZCHS and one partner Zimbabwean university. The first cohort reported after each training week that they were “satisfied” or “extremely satisfied” with the professional development. Respondents believed they increased their knowledge and skills in key content and reported their intention to use this learning in other aspects of their professional work. After training the third cohort in the 2014-15 period, HEALZ is expected to have produced a critical mass of education leaders who will implement further curriculum reforms.
Mentored Clinical and Research Scholars Programs
Declining numbers of UZCHS faculty created a need to develop pipeline programs for future academic faculty. Two parallel mentored scholars programs were designed for postgraduate students to address this need. The Mentored Clinical Scholars Program (MCSP) provides training and mentoring in academic skills, including teaching, while the Mentored Research Scholars Program (MRSP) provides training and mentoring in research skills. These programs were developed in 2010 to augment existing training of MMed students hoping to increase interest in MMed programs and for future careers in academic medicine. The MCSP was offered to all postgraduate students. Six 4-day workshops were conducted three times between March 2012 and October 2013. Topics were selected by the MCSP committee, which comprised faculty from UZCHS and UCSOM (Table 1). Attendance increased from 22 postgraduate students in March 2012 to 49 students in October 2013.
Unlike the MCSP Program, the MRSP involves a competitive selection process based on the merits of each applicant's proposed research project. Currently, 28 MMed students have been selected. The MRSP holds monthly seminars to discuss research proposal development and to update research activities. To date, three participants have presented their findings at competitive national and regional conferences.
Competency-based curriculum review framework
One of NECTAR's aims is to revise the medical students' curriculum using a competency-based framework in HIV, TB, malaria, and other areas identified as priorities by the U.S. President's Emergency Plan for AIDS Research (PEPFAR). After reviewing multiple published competency frameworks, participants at a faculty development workshop in July 2011 developed competencies for Zimbabwe using CanMeds as a template.8 Following intense discussion, workshop participants agreed on seven patient-centered competency domains: medical expert, scholar/researcher, educator, community health advocate, communicator/relationship builder, manager/leader, and ethical professional. These domains were endorsed and adopted by the faculty before initiating a comprehensive UZCHS curriculum review process in July 2013. Currently, UZCHS is developing a curriculum map using these competencies, identifying gaps and redundancies, and developing new curricula to meet identified areas of need.
A 17-module HIV curriculum was subsequently developed to train MMed students in PEPFAR priority areas. These modules were delivered monthly during two- to three-hour sessions by facilitators from the college, the Ministry of Health, and other organizations. A 10-session HIV/TB curriculum was developed for undergraduate medical students and delivered using a modified team-based learning format to final-year students during their attachment in internal medicine.9 Visiting professors were invited to teach non-PEPFAR subjects where no faculty expertise existed, such as in genetics, pediatric haematology, and emergency medicine. This is a stopgap measure until sufficient faculty expertise develops.
Community-based education
Since 1970, community-based education (rural/field attachment) has been practiced at UZCHS. The need to ensure that medical graduates could work beyond the teaching hospitals has always been emphasized. The objectives of these attachments will be revised using a competency-based framework. A training program for district medical officers involved in supervising students on attachments is still in the planning phase.
Infrastructure Improvements
Research Support Center
The need for an administrative center to coordinate and facilitate research activities was recognized as a key component of the NECTAR and SACORE (Southern African Consortium for Research Excellence)10 programs. SACORE's goal is to increase the critical mass of researchers in the region. Both programs contributed to the resource mobilization and capacity building of the Research Support Center (RSC), which was established in 2010 using the model described by Exnevia Gomo and colleagues.11 This model provided a comprehensive modular framework for research capacity building suitable for UZCHS's needs.
Training in research administration was provided to strengthen this aspect of the research enterprise. An annual 25-week course in research methodology includes weekly one-hour sessions on research methodology, biostatistics, and research compliance. The sessions are usually well attended, averaging 50 participants per session. A multimedia announcement of research opportunities was also implemented. Between 2012 and 2013, individual and group support in grant writing and submission was instituted. With RSC assistance, six grant applications were submitted and three have been funded.
Technology-assisted learning (eLearning)
NECTAR has facilitated the upgrading of ICT facilities, including hardware (server capacity), bandwidth, and virtual private network (VPN) connections among the three primary teaching sites (Parirenyatwa Hospital, Parirenyatwa Annexe, and Harare Hospital). Access to online literature resources such as HINARI12 has improved. Regular training workshops on literature search and eLearning capacity are conducted for both students and staff. Through collaboration with other NECTAR partners, a wide range of electronic resources have been made available, including UpToDate, eGranary, REDCap, Claroline, SMILE, Mayo Clinic videos, and course materials from Khan Academy and Stanford University. The greatest challenge has been how to incorporate these resources into the toolkits of UZCHS faculty.
The eLearning capacity received a major boost in 2014 through the provision of tablet computers for students and staff by a local Internet and mobile network provider through its EcoSchool project.13 Initially, 2,000 students will benefit; the tablets are pre-loaded with core textbooks and other educational materials at minimal cost. The EcoSchool project will eventually be rolled out to the rest of UZ.
Program evaluation
An evaluation team, consisting of members from UZCHS and the Evaluation Center of the School of Education and Human Development has administered surveys and key stakeholder interviews as part of a comprehensive needs assessment. Exit interim surveys were administered at the end of every faculty development workshop, postgraduate training workshop, and other activity. Program performance data were collected annually through questionnaires, interviews, and key stakeholder in-depth interviews. Progress reports were presented to faculty, ministry officials, and partner institutions. Finally, the program evaluation team has participated extensively in faculty development aimed at increasing program evaluation capacity at UZCHS.
Achievements
Two of NECTAR's goals have been firmly achieved: Faculty numbers have increased substantially, from 122/314 (39%) in 2009 to 163/320 (51%) in 2013; and undergraduate first year medical student enrolment has nearly doubled, from 147 in 2010 to nearly 300 in 2013. Between 2010 and 2013 there was also a significant increase in postgraduate enrolment, from 113 to 213 students. Improved economic and political factors contributed to these improvements, but MEPI support played a leading role.
Questions of Sustainability
Establishing a Department for Health Professions Education
The University of Zimbabwe Teaching and Learning Center (UTLC) had been responsible for orienting all new university faculty members, but the center lacked the capacity to teach bedside/clinical techniques. The need for a Department for Health Professions Education (DHPE) became clear to strengthen faculty development. UZCHS had previously conducted one or two workshops per year through its Institute for Continuing Health Education. Now that DHPE has been established and faculty development and HEALZ are being transitioned to this key department, the sustainability of faculty development and curriculum reform is more secure. The DHPE is expected to institute health education specialist training to the doctoral level as well as establish a clinical skills training laboratory.14
Postgraduate training
Better-trained postgraduate students will ultimately be deployed as specialists in various parts of the country, where they will serve as role models, thus disseminating best practices in medical education. MSCP training will also continue under the auspices of the DHPE.
Electronic resources
MEPI has complemented the massive eLearning commitment by the UZ administration. These initiatives have included improvement of bandwidth, provision of computer hardware at low cost to staff and students, and the recently launched EcoSchool pilot project described above. Maintenance for the hardware and software needs and upgrades will be available through an existing computer center. UZCHS's strategic partnership with a local mobile service provider is expected to result in sustainable access to electronic resources.
Political and economic support
Support for NECTAR activities has been demonstrated through buy-in at the highest levels, including the vice-chancellor's office as well as the UZCHS administration. Furthermore, the Ministry of Higher Education has demonstrated commitment through financial support for the NECTAR program. National economic challenges, such as the hyperinflationary period up to 2009, are beyond our control.
Conclusion
Through various NECTAR innovations, such as enhanced faculty development programs and mentored postgraduate programs, UZCHS is hoping to develop a critical mass of academic health professionals trained in adult learning methodologies, curriculum development, program evaluation, and research. In the country's current stable environment, these transformative changes are likely to result in the expansion and retention of dedicated health professionals who provide high-quality teaching and service.15,16
Acknowledgments
Funding/Support: This publication has been supported by MEPI funding through NIH Grant No. TW008881. MEPI is funded by the Office of the United States Global AIDS Coordinator and jointly administered by the Fogarty International Center of the National institutes of Health and the HIV/AIDS Bureau of the Health Resources and Services Administration.
Footnotes
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Contributor Information
Chiratidzo E Ndhlovu, senior lecturer in the Department of Medicine, University of Zimbabwe, College of Health Sciences, Harare, Zimbabwe.
Kusum Nathoo, professor of pediatrics in the Department of Pediatrics, University of Zimbabwe College of Health Sciences, Harare, Zimbabwe.
Margaret Borok, associate professor of medicine in the Department of Medicine, University of Zimbabwe College of Health Sciences, Harare, Zimbabwe.
Midion Chidzonga, professor of oral and maxillofacial surgery in the Department of Dentistry, University of Zimbabwe College of Health Sciences, Harare, Zimbabwe.
Eva M. Aagaard, professor of medicine in the Department of Medicine, Division of General Internal Medicine at the University of Colorado School of Medicine, Aurora, Colorado.
Susan C. Connors, The associate director of The Evaluation Center, School of Education and Human Development, University of Colorado, Denver, Colorado.
Michele Barry, professor of medicine in the Department of Medicine, and senior associate dean for global health, Stanford University, Palo Alto, California.
Thomas Campbell, professor of medicine in the Department of Medicine, Division of Infectious Diseases, University of Colorado School of Medicine, Aurora, Colorado.
James Hakim, professor of medicine in the Department of Medicine, University of Zimbabwe College of Health Sciences, Harare, Zimbabwe.
References
- 1.Davidson L. Birmingham's baby:the beginning of medical education in Rhodesia. Med Educ. 1971;5(1):61–74. doi: 10.1111/j.1365-2923.1971.tb02153.x. [DOI] [PubMed] [Google Scholar]
- 2.Collins FS, Glass RI, Whitescarver J, Wakefield M, Goosby EP. Public health. Developing health workforce capacity in Africa. Science. 2010;330(6009):1324–5. doi: 10.1126/science.1199930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mullan F, Frehywot S, Omaswa F, Buch E, Chen C, Greysen SR, et al. Medical schools in sub-Saharan Africa. Lancet. 2011;377(9771):1113–21. doi: 10.1016/S0140-6736(10)61961-7. [DOI] [PubMed] [Google Scholar]
- 4.Ramani S, Leinster S. AMEE Guide no. 34: Teaching in the clinical environment. Med Teach. 2008;30(4):347–64. doi: 10.1080/01421590802061613. [DOI] [PubMed] [Google Scholar]
- 5.Sub-Saharan FAIMER Regional Institute. [Accessed April 17, 2014]; www.safri.faimerfri.org.
- 6.Kern DE, Thomas PA, Hughes MT. Curriculum Development for Medical Education: A Six-Step Approach. 2nd. Baltimore, MA: The Johns Hopkins University Press; 2009. [Google Scholar]
- 7.Johnson KS, Hastings SN, Purser JL, Whitson HE. The Junior Faculty Laboratory: an innovative model of peer mentoring. Acad Med. 2011 Dec;86(12):1577–82. doi: 10.1097/ACM.0b013e31823595e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Card SE, Snell L, O'Brien B. Are Canadian General Internal Medicine training program graduates well prepared for their future careers? BMC Med Educ. 2006;6:56. doi: 10.1186/1472-6920-6-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacob G, Fana GT, Campbell TB, Hakim JG, Borok MZ, Aagaard E. Feasibility and sustainability of an interactive team-based learning method for medical education during a severe faculty shortage in Zimbabwe. BMC Medical Education. doi: 10.1186/1472-6920-14-63. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Southern African Consortium for Research Excellence. [Accessed April 17, 2014]; www.sacoreresearch.org.
- 11.Gomo E, Kalilani L, Mwapasa V, Trigu C, Phiri K, Schmidt J, et al. Towards Sustainable Research Capacity Development and Research Ownership for Academic Institutes in Developing Countries. Journal of Research Administration. 2011;42(1):38–44. [Google Scholar]
- 12.HINARI. HINARI Access to Research in Health Program. [Accessed April 17, 2014]; www.who.int/hinari/
- 13.EcoSchool. [Accessed April 17, 2014]; www.EcoSchool.co.zw.
- 14.Akaike M, Fukutomi M, Nagamune M, Fujimoto A, Tsuji A, Ishida K, et al. Simulation-based medical education in clinical skills laboratory. J Med Invest. 2012;59(1-2):28–35. doi: 10.2152/jmi.59.28. [DOI] [PubMed] [Google Scholar]
- 15.Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Geneva: WHO; 2013. [Accessed April 17, 2014]. Transforming and scaling up health professionals' education and training:WHO education guidelines. http://www.who.int/hrh/resources/transf_scaling_hpet/en/ [PubMed] [Google Scholar]


