Abstract
Content
Violations of safety protocols are paths to adverse outcomes that have been poorly addressed by existing safety efforts. This study reports on nurses' self-reported violations in the medication administration process.
Objective
To assess the extent of violations in the medication administration process among nurses.
Design, Setting, & Participants
Participants were 199 nurses from two U.S. urban, academic, tertiary care, free-standing pediatric hospitals who worked in: a pediatric intensive care unit (PICU), a hematology-oncology-transplant (HOT) unit, or a medical-surgical (Med/Surg) unit. In a cross-sectional survey, nurses were asked about violations in routine or emergency situations in three steps of the medication administration process.
Main Outcome Measure
Self-reported violations of three medication administration protocols were made using a 7-point 0-6 scale from “not at all” to “a great deal.”
Results
Analysis of variance identified that violation reports were highest for emergency situations, rather than for routine operations, highest by HOT unit nurses, followed by PICU nurses, and then Med/Surge unit nurses, and highest during patient identification checking, followed by matching a medication to a medication administration record, and then documenting an administration. There was also a significant 3-way interaction among Violation Situation, Step in the process, and Unit, which is explained in detail in the Results.
Conclusions
Protocol violations occur throughout the medication administration process and their prevalence varies as a function of hospital Unit, Step in the process, and Violation Situation. Further research is required to determine whether these violations improve or worsen safety, and for those that worsen safety, how to redesign the system of administration to reduce the need to violate protocol in order to accomplish job tasks.
MESH Key Words: Patient safety, Compliance, Medication Administration, Violation
Keywords: Compliance, Human error, Human factors, Medical error, measurement/epidemiology, Patient safety
Introduction
Hospitalized patients may experience an average of one medication error per day.[1] Errors at the medication administration stage of the medication use process are especially likely to result in patient harm because, with the exception of high-risk medications, no independent health care provider checks a medication before it is administered.[2,3] To reduce errors in the medication administration process, protocols and technologies have been implemented.[1,4] However, the success of protocols and technologies depends on compliance. Non-compliance with protocols, here referred to as violations, represents a path to medical injury that requires further study.[5] Violations are actions that break rules, policies, protocols, or procedures.[6] In the case of medication administration, this would apply to any rule, policy, or procedure regarding how steps in the administration process should be carried out.
Violations in the medication administration process are known to occur,[7-9] but to date no quantitative data exist on the extent or prevalence of violations. This study of pediatric nurses in two hospitals is the first to examine the extent to which nurses knowingly violate medication administration protocols. Because the violations are self-reported, intentional violations and unintentional violations recognized as violations after the fact are captured. Intentional violations are those committed knowing that rules, policies, or norms are being broken.[10,11] This study is also the first to examine how violations vary between two hospitals, between three types of hospital units, between three specific steps in the medication administration process, and between violations committed routinely versus in emergency situations.
Methods
This study was conducted as part of a broader study to evaluate the impact of a bar coded medication administration (BCMA) system on medication administration errors and on end users (nurses, pharmacists, and pharmacy technicians). This study analyzes cross-sectional data from a paper survey administered at two hospitals before either one implemented BCMA. The study was approved by the University of Wisconsin-Madison IRB and by the IRBs of both study hospitals.
Setting and Sample
Two urban, academic, tertiary care, free-standing pediatric hospitals participated in the study. Hospital A had 222 beds and was located in the Midwest U.S. Hospital B had 162 beds and was located in the South U.S. Three units were studied in both hospitals: a pediatric intensive care unit (PICU), a hematology-oncology-transplant unit (HOT), and a general medical/surgical unit (Med/Surg).
Full-time nurses (24 hours per week or more) who provided patient care in the study units were eligible to participate. The sampling frame was 203 nurses from Hospital A and 144 from Hospital B. Surveys were distributed to all nurses in the sampling frame. Data were collected November–December, 2005, and March–May, 2006, at Hospitals A and B, respectively. Response rates of 59.6% and 54.2% were attained in Hospitals A and B, respectively. Descriptive statistics are provided in Table 1.
Table 1.
Descriptive statistics.
| Hospital A | Hospital B | |
|---|---|---|
| Response Rate | 59.6% (n=121) | 54.2% (n=78) |
| Gender (% female) | 97.5 | 96.2 |
| Race (% white, not Hispanic) | 93.4 | 94.9 |
| Education (% completing college) | 93.4 | 97.4 |
| Age* | ||
| 18-29 | 33.1 | 56.4 |
| 30-39 | 32.2 | 20.5 |
| 40-49 | 24.8 | 15.4 |
| 50+ | 9.9 | 7.7 |
| Shift | ||
| Day | 43.0 | 43.6 |
| Evening / Afternoon | 32.2 | 2.6† |
| Night | 24.8 | 37.2 |
| Other (e.g. weekends) | 10.7 | 16.7 |
| Mean (SD) | Mean (SD) | |
| Hours / week** | 31.3(7.8) | 37.3 (6.8) |
| Job tenure** | 8.9 (8.1) | 4.4 (5.7) |
| Unit tenure** | 8.1 (7.6) | 3.9 (5.4) |
| Employer tenure** | 9.2 (8.2) | 4.8 (5.9) |
| Occupation tenure** | 11.6 (9.4) | 7.7 (8.0) |
p ≤ 0.05 (Pearson chi-square)
p ≤ 0.05 (t-test, equal variances not assumed)
Hospital B had limited options for evening shifts; the majority of nurses were allowed only 12-hour shifts
Measures
The questions about violations were developed based on previous research,[10,12] and are provided in Table 2. Respondents were instructed to think of the past 30 days.
Table 2.
Questions and response scale used in study. Numbered Questions in Table 2 correspond to numbered Violation Situation / Steps in Table 3.
| Not at all | A little | Some | A moderate amount | Pretty much | Quite a lot | A great deal | Don't know | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | In actual practice, to what extent do you find yourself routinely having to break protocol for matching medications to the MAR/medication profile? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 0 | ||
| 2 | In actual practice, to what extent do you find yourself routinely having to break protocol for checking patient identification in order to administer medications? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 0 | ||
| 3 | In actual practice, to what extent do you find yourself routinely having to break protocol for documenting administered medications? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 0 | ||
| 4 | In an emergency situation, to what extent do you find yourself having to break protocol for matching medications to the MAR/medication profile? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 0 | ||
| 5 | In an emergency situation, to what extent do you find yourself having to break protocol for checking patient identification in order to administer medications? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 0 | ||
| 6 | In an emergency situation, to what extent do you find yourself having to break protocol for documenting administered medications? | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 0 | ||
Design and Procedures
Pretesting
Questionnaire items were evaluated using expert review and cognitive interviewing.[13] Expert reviews were completed by safety trained experts, nurse researchers, a pharmacist co-investigator, and two questionnaire design experts to assess readability, word choice, question clarity, and question content. Sixteen cognitive interviews were conducted with nurses at large teaching hospitals to appraise content validity.[14] Through these interviews, it was determined that nurses had a shared understanding of the protocols relevant to the questions and of the meaning of breaking protocol. In addition, nurses reported interpreting the response scale as one of frequency. That is, when asked, for example, “why did you choose to circle the 2 (“some”) instead of the 3 (“moderate”)” the nurses would respond that they only violated some of the time, not a moderate amount of the time.
Procedures
Publicity
The study team worked with nurse managers on the study units and with the research coordinators at each hospital to determine where to hang flyers advertising the study. One flyer provided information about the study; another listed “frequently asked questions” and answers to those questions. Some nurse managers sent emails to nursing staff encouraging them to participate in the study and/or made the PowerPoint presentation of the study available electronically.
Survey Administration
When possible, members of the research team attended staff meetings to speak with nurses and hand out surveys. All survey packets were delivered in personalized envelopes which contained the survey, an information sheet (consent form not requiring a signature), a stamped, addressed envelope in which to put the completed survey and mail it back to the survey processing center, and a $5 cash incentive. In addition to, or in lieu of, staff meetings, the research team presented the study to nurses during the report at the beginning of the nurse's shift or during informal inservices. When few surveys remained to be delivered, the research team attempted to find each nurse to provide an individual presentation of the study and to deliver that nurse's survey. Before giving surveys to subjects, the research team endeavored to speak with each of the subjects to tell them about the study, how to participate in the study, and about measures taken to ensure their confidentiality. After the presentation, time was left for subjects' questions. Then, subjects were given their survey packets. After survey distribution started, a series of three reminders was used to encourage nurses to complete the survey. To protect confidentiality, all nurses received identical-looking reminders.
Analysis
A four-factor mixed measures factorial model[15,16] was carried out in SPSS version 16.0 (Chicago, IL)[17] using a 2 (Hospital: Hospital A, Hospital B) by 3 (Unit: PICU, HOT, Med/Surg) by 3 (Step: matching the medication to the medication administration record [Match-MAR], checking patient identification [ChxID], and documenting administration of the medication [DOC]) by 2 (Violation Situation: Routine, Emergency) design. Step and Violation Situation were within-subjects variables. Hospital and Unit were between-subjects variables. Contrasts were run for significant interaction terms. The ANOVA was performed on the untransformed data and on the rank transformed data and very similar results were obtained. Therefore, based on Conover,[18] the results of the ANOVA with untransformed data are presented here.
Interaction contrasts were carried out using Graphpad Software.[19] A False Discovery Rate (FDR) approach was used to correct for family-wise error rate for numerous interaction contrasts. FDR is the expected proportion of false positive findings among all the rejected hypotheses. Compared to the typical approach (e.g., Bonferroni, Sidak, etc.), FDR is not as conservative and provides a good balance between discovery of statistically significant effects and limitation of false positive occurrences (see details elsewhere[20]).
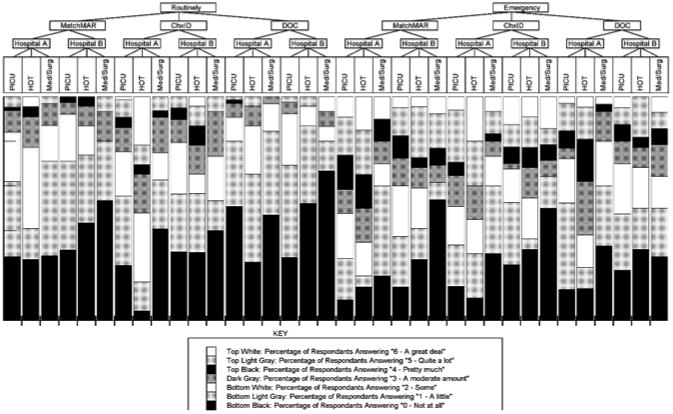
Results
Table 3 provides means and standard deviations for each Step of the medication administration process in each Hospital, each Unit within each hospital, overall for both hospitals, and for each type of unit across hospitals. Additionally, the percentage of nurses reporting ever violating (a response > 0) is reported. Appendix 1 shows the raw distributions of responses in a mosaic plot; the plot provides the complete distribution of responses on the 7-point response scale for: both Violation Situations, both Hospitals, the three types of Units, and the three Steps of the edication administration process.
Table 3.
Means, standard deviations, and percent self-reporting ever violating for questions about violations. Numbered Violation Situation / Steps in Table 3 correspond to numbered questions in Table 2.
| Violation Situation / Step |
Hospital A | PICU | HOT | Med/Surg | Hospital B | PICU | HOT | Med/Surg | Hospital A and B | PICU | HOT | Med/Surg | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Routine /Match-MAR | Mean (SD) | 1.39 (1.31) | 1.37 (1.30) | 1.73 (1.52) | 1.19 (1.17) | 1.04 (1.15) | 1.08 (1.00) | 1.00 (1.17) | 1.00 (1.51) | 1.25 (1.26) | 1.26 (1.20) | 1.36 (1.38 | 1.13 (1.28) |
| Percent | 71.6 | 71.4 | 72.7 | 71.0 | 60.5 | 68.4 | 56.5 | 46.7 | 67.2 | 70.3 | 64.4 | 63.0 | |
| 2. Routine /ChxID | Mean (SD) | 1.89 (1.74) | 1.69 (1.57) | 3.17 (1.92) | 1.38 (1.54) | 1.60 (1.59) | 1.49 (1.43) | 1.87 (1.89) | 1.47 (1.55) | 1.78 (1.69) | 1.62 (1.52) | 2.52 (2.00) | 1.40 (1.53) |
| Percent Mean (SD) | 75.0 | 75.4 | 95.7 | 59.4 | 67.5 | 69.2 | 69.6 | 60.0 | 72.1 | 74.4 | 71.8 | 59.6 | |
| 3. Routine /DOC | Mean (SD) | 0.89 (1.08) | 0.83 (1.11) | 1.30 (1.22) | 0.72 (0.81) | 0.97 (1.22) | 1.15 (1.06) | 0.74 (1.14) | 0.87 (1.68) | 0.92 (1.13) | 0.95 (1.10) | 1.02 (1.20) | 0.77 (1.15) |
| Percent | 55.0 | 49.2 | 73.9 | 53.1 | 57.1 | 71.8 | 47.8 | 33.3 | 55.8 | 57.7 | 59.2 | 46.8 | |
| 4. Emergency /Match-MAR | Mean (SD) | 2.72 (1.94) | 2.92 (1.87) | 3.30 (2.03) | 1.90 (1.84) | 2.28 (1.97) | 2.38 (1.79) | 2.36 (2.08) | 1.85 (2.38) | 2.55 (1.96) | 2.71 (1.85) | 2.81 (2.09) | 1.88 (1.99) |
| Percent | 87.0 | 90.8 | 85.0 | 80.0 | 74.7 | 85.0 | 78.7 | 46.2 | 82.1 | 88.6 | 78.6 | 69.8 | |
| 5. Emergency / ChxID | Mean (SD) | 2.55 (2.02) | 2.71 (1.95) | 3.15 (2.16) | 1.80 (1.94) | 2.20 (2.17) | 2.20 (2.14) | 2.41 (2.13) | 1.86 (2.41) | 2.41 (2.08) | 2.51 (2.03) | 2.76 (2.15) | 1.82 (2.07) |
| Percent | 81.7 | 84.6 | 90.0 | 70.0 | 68.4 | 75.0 | 68.2 | 50.0 | 76.4 | 81.0 | 78.6 | 63.6 | |
| 6. Emergency / DOC | Mean (SD) | 2.02 (1.71) | 2.03 (1.71) | 2.86 (1.77) | 1.40 (1.45) | 1.96 (1.81) | 1.98 (1.76) | 1.91 (1.87) | 2.00 (1.96) | 1.99 (1.75) | 2.01 (1.72) | 2.37 (1.86) | 1.59 (1.63) |
| Percent | 81.0 | 86.2 | 85.7 | 66.7 | 73.7 | 77.5 | 68.2 | 71.4 | 78.1 | 82.9 | 76.7 | 68.2 |
Significant Effects (Main Effects)
The main effects (testing for the effects of individual variables, without regard for interactions or moderating effects) for the variables of Unit (F (2, 1158) = 3.47, p<0.05), Step in the process (F (2, 1158) = 17.52, p<0.05) and Violation Situation (F (1, 1158) = 77.63, p<0.05) were significant. Effect sizes for significant effects, based on Cohen's D, were 0.26 for Unit, 0.26 for Step, and 0.49 for Violation Situation. For Unit, violations scores were highest for HOT, followed by the PICU, and then Med/Surg. For Step, violation scores were highest for ChxID, then Match-MAR, and finally DOC. The main effect for Violation Situation showed that violations scores were higher in emergency situations. The main effect for Hospital was not significant (F (1, 1158) = 2.80, p=0.096).
Significant Effects (Interaction Effects)
Interactions effects, which test the hypothesis that the effect of variable A on the outcome differs depending on the level of some variable B, are more illuminating than the main effects as they test whether and how main effect are moderated by another variable. The four-way interaction among the four main effects was not significant. There was a significant Unit by Step by Violation Situation interaction (F (4, 1158) = 3.24, p<0.05). To ease discussion of the three-way interaction, the two-way interaction between Unit and Step is discussed for each level of Violation Situation. Figures 1a and 1b show the 3-way interaction.
Figure 2.
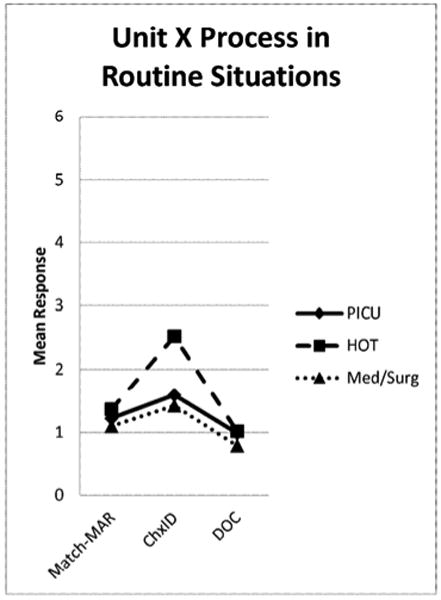
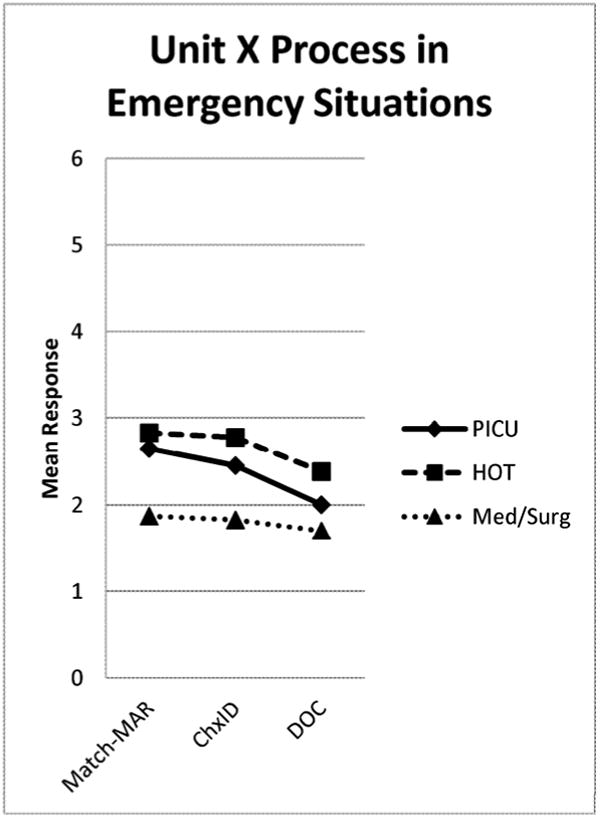
a and b show the 3-way interaction of Unit × Process × Situation. Figure 1a shows how Unit and Process vary within Routine Situations and Figure 1b shows how Unit and Process vary within Emergency Situations.
Routine Situations
Contrasts for the three-way interaction show that there were no differences among the three units for DOC or Match-MAR for routine violations (Figure 1a). However, for ChxID, the HOT units had significantly higher routine violation scores than the PICUs and Med/Surg units. In both the PICU and HOT units, routine violations in ChxID were reported more than violations in Match-MAR. Across units, significantly more violations were self-reported in ChxID than in DOC.
Emergency Situations
In emergency situations (Figure 1b), there were significant Unit differences for all three Steps of the medication administration process. For Match-MAR, the PICUs and HOT units had significantly higher emergency violation scores than the Med/Surg units. For ChxID, all three units significantly differed from each other; the HOT units had higher violation scores than the PICUs and Med/Surg units; the PICUs had significantly higher violation scores than the Med/Surg units. Finally, for DOC, the HOT units had significantly higher violations scores than both the PICUs and Med/Surg units.
Across units, there were no significant differences between reported violations in Match-MAR and ChxID. In both the PICUs and HOT units, there were fewer reported violations in DOC than in either Match-MAR or ChxID; in the Med/Surg units, there were no differences between steps.
Discussion
This study provided the first attempt at quantifying violations in the medication administration process. The results show that, based on nurses' self reports, depending on the Unit of care, the Violation Situation, and the Step of the medication administration process, violations were reported by as few as 33.3% to as many as 90.8% of nurses (defined as any non-zero response); reports of violations were not limited to one or two aberrant scenarios. This study also provided the first assessment of the extent to which violations vary by structure and process variables; violations do vary depending on the Violation Situation, the care Unit, and the particular Step of the medication administration process.
The study confirms findings from qualitative studies that show violations of protocols and technology use policies occur in the medication administration process.[7-9,21,22] This study extends prior findings by showing the extent of the violations and the structure and process variables that contribute to varying violation rates.
Significant Effects (Main Effects)
Main effects were found for Unit, Step, and Violation Situation, but not for Hospital. The null finding for Hospital is as important as the significant main effects. Not finding hospital differences demonstrates that our findings were not isolated to what might otherwise have been labeled a problematic hospital. Instead, we found similar self-reported violation levels at two highly regarded pediatric hospitals. We cannot say for sure if other pediatric hospitals have similar levels of violations, but our findings do not rule out that violations in medication administration are a systemic phenomenon.
The data also show that violations during emergency situations are more likely to be reported than routine violations, that violations are more likely to be reported in the hematology units (HOT), followed by the intensive care units (PICU), and then by medical-surgical units (Med/Surg), and that violations are more likely to be reported in the checking identification (ChxID) process, followed by matching medication to MAR (Match-MAR), and then by documentation (DOC). The significant 3-way interaction between Unit, Step, and Violation Situation provides a more accurate picture of those variables than the main effects, and is discussed next.
Significant Effects (Interaction Effects)
In routine situations, violations of the protocol for ChxID are reported more often on the HOT units than on the other two units. Greater reporting of ChxID violations in HOT compared to in other units may be partially explained by longer patient stays in HOT units due to the nature of those patients' diseases. Because patients are on the unit for a long time, nurses are better able to get to know the patients and may perceive that following the protocol for checking identification of these more familiar patients is less necessary. There may be a misunderstanding of the need for the identification check as per protocol: the check goes beyond verifying that the nurse knows the patient; it also ensures the medication in hand matches the patient. A nurse could accidentally take the wrong medication for the right patient, or have the “right” medication, but get distracted and go into the wrong patient's room—in both cases, simply recognizing the patient in the room may not prevent the misadministration.
In emergency situations, the picture is different. Typically, the HOT units had the highest reported levels of violations in emergency situations, followed by PICUs, and then Med/Surg. Why the HOT units had the highest reported levels requires further investigation. The reason for their reporting of higher levels of violations of Match-MAR may be related to patients having long lengths of stay, but it is not clear why violations of DOC would be higher.
Interestingly, in emergency situations, violations of Match-MAR were reported more than violations of ChxID and DOC in all units (though not significantly more in all cases). This differs from routine situations, in which violations of ChxID were most-reported. This may be because the MAR was located in a patient's chart and not necessarily available at bedside, unlike the patient identification. Another possibility is that the MAR may be less relevant during an emergency; emergency medications may be ordered and administered without first being entered into the MAR.
Violations in Healthcare Settings
Rules, policies, and procedures assume a work environment that is favorable to compliance. In contrast, healthcare delivery, especially in inpatient PICUs and HOT units, is characterized by time pressure, high acuity patients, and a need for problem solving. In those environments, medication administration is highly complex and filled with interruptions to manage and challenges to resolve.[23-26] When the reality of a clinical environment does not match the environment assumed by designers of rules or policies, violations are to be expected—because there is not enough time to comply with protocols, because the cost of compliance is perceived as higher than the cost of violating, or because different protocols may conflict.[5,8,27,28] The presence of conflicting goals is common in complex systems like health care[29] and makes it more likely that violations will occur regularly.
Importantly violations do not imply less safety; violations may reduce, have no impact on, or even improve safety.[10,30,31] While violations may increase the likelihood and severity of adverse events,[11,32] violations can also be necessary or even desired (by a patient or family) such as when compliance would slow down a process that requires speed to save a life.[33] In such cases, it is the clinician who, while technically violating a rule, might be in fact making “the difference between total disaster and a small accident, or no accident at all.”[34]
Limitations
This study has four main limitations. First, the questions captured self-reports of violations rather than the actual number of violations. Therefore, we cannot report actual rates of violations. Our data only give a sense of the extent of intentional violations that nurses were able and willing to self-report. Violations committed unknowingly would not have been captured in this analysis. While observing violations is possible, and may have provided a more accurate count of violations, differentiating between intentional and unintentional violations is impossible because the observer cannot know the subject's intentions. Further, nurses may choose not to violate while being observed because violations are socially undesirable.
Second, only two hospitals participated. This limits the generalization of the findings. However, most published patient safety studies have occurred in a single institution. The lack of a main effect for Hospital suggests that the extent of the violations is not limited to one hospital. A related point is that we did not adjust for the demographic differences between the hospitals so we do not know if any of the existing results could be explained by differences in, for example, job experience. This should be addressed in future research. Third, because of the question wording, we do not know the specific violation behaviors that respondents had in mind when they reported committing violations, generally. For example, we do not know if a reported violation of ChxID meant only checking one patient identifier instead of two, checking no identifier at all, or violating the protocol in some other way. Future research will need to obtain such specifics.
Fourth, there could be response bias. The response rates were acceptable, but we do not know how non-respondents differed from respondents. The response rate is high enough, however, that even if all non-respondents reported not violating at all, the data would show high levels of reported violations. Finally, though not a limitation per se, this study does not explain how to address violations. There exists general knowledge about violation causes in work domains,[27] and there is emerging evidence from healthcare,[7,8,22,35] but more research is needed.
Conclusion
This study demonstrates that violations occur in the medication administration process across Hospitals, Units, and Steps in the process. Importantly, factors such as the Unit in which a nurse works, whether or not a nurse is in an emergency Violation Situation, and the Step of the medication administration process all interact to influence intentional violations. This finding is important as it provides empirical evidence that structural and process variables influence intentional violations. Just as safety scientists urge a shift from blaming people for medical errors to studying the causes of errors, we strongly advocate not blaming clinicians for violations, but rather searching for a more systems-oriented causal explanation. It is, after all, the causes of violations that need remediation.
Acknowledgments
This study was funded in part by a grant from the Agency for Healthcare Research and Quality (R01 HS013610, Karsh PI). RJH was supported by a pre-doctoral training grant from the National Institutes of Health (1 TL1 RR025013-01) and a post-doctoral training grant from the Agency for Healthcare Research and Quality (5 T32 HS000083-11). The authors would like to thank Scot Barnett and Nancy DiCanio for their assistance editing this manuscript. The authors also thank the Barcode Study Team and the many nurses who participated in the Barcode Study and made this work possible.
Appendix
Footnotes
Competing Interest Statement: None of the authors have any competing interests.
Contributorship Statement: Alper: conception, design, acquisition, analysis, drafting, revising, and final approval
Holden: conception, design, acquisition, analysis, drafting, revising, and final approval
Scanlon: conception, design, acquisition, analysis, drafting, revising, and final approval
Patel: conception, design, acquisition, analysis, drafting, revising, and final approval
Kaushal: conception, design, revising, and final approval
Skibinski: conception, design, revising, and final approval
Brown: conception, design, analysis, revising, and final approval
Karsh: conception, design, acquisition, analysis, drafting, revising, and final approval
Data Sharing: No additional data are available.
Contributor Information
Samuel J. Alper, Exponent Failure Analysis Associates, Human Factors Practice; * Work completed at University of Wisconsin-Madison, Department of Industrial and Systems Engingeering
Richard J. Holden, University of Wisconsin-Madison, School of Medicine and Public Health; Royal Institute of Technology (KTH) Deparment, Division of Ergonomics
Matthew C. Scanlon, Medical College of Wisconsin, Pediatrics
Neal R. Patel, Vanderbilt University, Pediatrics
Rainu Kaushal, Weill Cornell Medical College, Departments of Pediatrics, Public Health, and Medicine
Kathleen A. Skibinski, St. Mary's Hospital, Pharmacy
Roger L. Brown, University of Wisconsin-Madison, School of Nursing and Department of Family Medicine
Ben-Tzion Karsh, University of Wisconsin-Madison, Department of Industrial and Systems Engineering
References
- 1.IOM. Preventing medication errors. Washington DC: The National Academic Press; 2007. [Google Scholar]
- 2.Kopp BJ, Erstad BL, Allen ME, et al. Medication errors and adverse drug events in an intensive care unit: Direct observation approach for detection. Crit Care Med. 2006;34:415–25. doi: 10.1097/01.ccm.0000198106.54306.d7. [DOI] [PubMed] [Google Scholar]
- 3.Leape LL, Bates DW, Cullen DJ, et al. Systems analysis of adverse drug events. JAMA. 1995;274(1):35–43. [PubMed] [Google Scholar]
- 4.Karsh B, Wetterneck T, Holden RJ, Rivera AJ, et al. Bar coding in medication administration. In: Yih Y, editor. Handbook of Healthcare Delivery Systems. CRC press; In Press. [Google Scholar]
- 5.Almaberti R, Vincent C, Auroy Y, Maurice GdS. Violations and migrations in health care: a framework for understanding and management. BMJ Qual Saf. 2006;15:66–71. doi: 10.1136/qshc.2005.015982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alper SJ, Karsh B. A systematic review of safety violations in industry. Accid Anal Prev. 2009 doi: 10.1016/j.aap.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 7.Carayon P, Wetterneck TB, Hundt AS, et al. Evaluation of nurse interaction with bar code medication administration technology in the work environment. J Patient Saf. 2007;3(1):34–42. [Google Scholar]
- 8.Koppel R, Wetterneck TB, Telles JL, et al. Workarounds to barcode medication administration systems: their occurrences, causes, and threats to patient safety. J Am Medl Inform Assoc. 2008 doi: 10.1197/jamia.M2616. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patterson ES, Rogers ML, Chapman RJ, et al. Compliance with intended use of bar code medication administration in acute and long-term care: an observational study. Hum Factors. 2006;48(1):15–22. doi: 10.1518/001872006776412234. [DOI] [PubMed] [Google Scholar]
- 10.Lawton R. Not working to rule: Understanding procedural violations at work. Saf Sci. 1998;28(2):75–95. [Google Scholar]
- 11.Reason J, Manstead A, Stradling S, et al. Errors and violations on the roads: a real distinction? Ergonomics. 1990;33(10/11):1315–32. doi: 10.1080/00140139008925335. [DOI] [PubMed] [Google Scholar]
- 12.Reason J. Human Error. Cambridge, UK: Cambridge University Press; 1990. [Google Scholar]
- 13.Presser S, Blair J. Survey Pretesting: Do Different Methods Produce Different Results? In: Marsden PV, editor. Sociological Methodology. Oxford: Basil Blackwell; 1994. pp. 73–104. [Google Scholar]
- 14.Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- 15.Box GEP, Hunter WG, Hunter JS. Statistics for Experimenters: An Introduction to Design, Data Analysis, and Model Building. New York, NY: John Wiley & Sons; 1978. [Google Scholar]
- 16.Keppel G, Wickens TD. Design and Analysis: a Researcher's Handbook. 4th. Prentice Hall; 2004. [Google Scholar]
- 17.SPSS [program] 16.0 version. Chicaco, IL: SPSS Inc; 2008. [Google Scholar]
- 18.Conover WJ. Practical nonparametric statistics. 2nd. New York: John Wiley and Sons; 1980. [Google Scholar]
- 19.Graphpad Software Inc. t-test calculator. 2005 [Google Scholar]
- 20.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Stat Soc B. 1995;57:289–300. [Google Scholar]
- 21.Sznelwar L, Mascia F, Montedo U, editors. Routine and situational violations during medication administration; 9th International Symposium on Human Factors in Organizational Design and Management; 2008; Guarujá, São Paulo, Brazil. [Google Scholar]
- 22.Patterson ES, Cook RI, Render ML. Improving patient safety by identifying side effects from introducing bar coding in medication administration. J Am Med Inform Assoc. 2002;9(5):540–53. doi: 10.1197/jamia.M1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Faye H, Carayon P, Karsh B, et al. ICU Nurse Medication Management: Decision-Making in a Complex Environment; 2nd International Conference on Healthcare Systems Ergonomics and Patient Safety; 2008; Strasbourg, France. [Google Scholar]
- 24.Holden RJ, Alper SJ, Scanlon MC, et al. Challenges and Problem-Solving Strategies During Medication Management: A Study of a Pediatric Hospital Before and After Bar-Coding; 2nd International Conference on Healthcare Systems Ergonomics and Patient Safety; 2008; Strasbourg, France. [Google Scholar]
- 25.Tucker AL. The impact of operational failures on hospital nurses and their patients. J Oper Manag. 2004;22(2):151–69. [Google Scholar]
- 26.Tucker AL, Spear SJ. Operational failures and interruptions in hospital nursing. Health Serv Res. 2006;41(3):643–62. doi: 10.1111/j.1475-6773.2006.00502.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alper SJ, Karsh B. A systematic review of safety violations in industry. Accid Anal Prev. 2009;41(4):739–54. doi: 10.1016/j.aap.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 28.Battman W, Klumb P. Behavioral economics and compliance with safety regulations. Saf Sci. 1993;16:35–46. [Google Scholar]
- 29.Vicente K. Cognitive Work Analysis : Toward Safe, Productive, and Healthy Computer- Based Work. Lawrence Erlbaum; 1999. [Google Scholar]
- 30.Dekker S. Failure to adapt or adaptations that fail: contrasting models on procedures and safety. Appl Ergon. 2003;34(3):233–38. doi: 10.1016/S0003-6870(03)00031-0. [DOI] [PubMed] [Google Scholar]
- 31.Reason J, Parker D, Lawton R. Organizational controls and safety: The varieties of rule- related behavior. J Occup Organ Psychol. 1998;71:289–304. [Google Scholar]
- 32.Parker D, Reason JT, Manstead ASR, et al. Driving errors, driving violations and accident involvement. Ergonomics. 1995;38(5):1036–48. doi: 10.1080/00140139508925170. [DOI] [PubMed] [Google Scholar]
- 33.Nascimento A, Falzon P. Safety management at the sharp end: Goals conflict and risky trade- offs by radiographers in radiotherapy; International Ergonomics Association 17th World Congress on Ergonomics; 2009 August 9-14; Beijing, China. [Google Scholar]
- 34.Hollnagel E. The Design of Fault Tolerant Systems - Prevention Is Better Than Cure. Reliab Eng Syst Saf. 1992;36(3):231–37. [Google Scholar]
- 35.Phillips DL, Parker D, Pals EJM, et al. Identifying violation-provoking conditions in healthcare. Ergonomics. 2008;51(11):1625–42. doi: 10.1080/00140130802331617. [DOI] [PubMed] [Google Scholar]


