Abstract
Objective
To examine correlates of Complementary and Alternative Medicine (CAM) use in a pediatric population with chronic pain. To determine if CAM use is positively correlated with adaptive coping skills.
Methods
We examined patient data from children ages 7–18 (n=1175) with chronic pain who completed the intake assessment at the time of initial evaluation at Boston Children’s multidisciplinary Pain Treatment Service between 2003–2011. The intake assessment included validated measures of anxiety, depression, pain coping skills and functional disability. Parents were also asked whether their child had tried CAM modalities in the past. We used a multivariable logistic regression model to determine correlates of CAM use and a multivariable linear regression model to determine the relationship between bio-behavioral CAM (relaxation training, hypnosis, and biofeedback) and accommodative coping.
Results
In our multivariable model, we found that female gender (OR 1.47, CI 1.07–2.01), parental education (OR 1.11 per year, CI 1.06–1.16), greater pain intensity (OR 1.06 per point on an 11-point numerical analog scale, CI 1.01–1.11), and more functional disability (OR 1.19 per 10 point increment on the Functional Disability Inventory, CI 1.06–1.34) were independently associated with CAM use. Bio-behavioral CAM was found to have a statistically significant correlation with accommodative coping skills (β 0.2 p-value .003).
Conclusion
In a pediatric chronic pain center, CAM users tended to have higher pain intensity, and greater functional disability. Exposure to bio-behavioral CAM techniques was associated with adaptive coping skills.
Keywords: Complementary and Alternative Medicine, Integrative Medicine, Pediatrics, Chronic Pain
Introduction
Chronic pain is a significant problem in pediatrics and the prevalence of chronic and recurrent pain in children has increased significantly in the last decade. In prior studies investigating pediatric chronic pain not associated with a specific disease, the prevalence of headache was 23%, and other pain types, including musculoskeletal pain, abdominal pain, and multiple pain complaints ranged from 11–38%.1 Unfortunately, there is little empirical support for the pharmacologic management of chronic pain in children outside of acute headaches, and most of the existing data are extrapolated from adult studies.2
Complementary and alternative medicine (CAM) is defined by the National Institutes of Health (NIH) as “a group of diverse medical and health care systems, practices, and products that are not generally considered to be part of conventional medicine.”3 There is a growing body of literature reporting promising results using certain CAM modalities for chronic pain. For example, guided imagery, biofeedback, hypnosis, mindfulness, massage, and acupuncture may be effective adjuncts to the treatment of chronic, acute, and recurrent pain for both pediatric and adult populations.4,5,6,7 Additionally, a recent systematic review by Rutten et al found that gut directed hypnotherapy for functional abdominal pain and irritable bowel syndrome in children was superior to standard medical care in children.8 Importantly, these therapies have few or no reported adverse effects.9, 10, 11
With the growing popularity of CAM and increasing research in this area, the percentage of children using CAM has also increased. Based on data from the 2007 National Health Interview Survey (NHIS), Barnes et al estimated that 11.8% of children in the United States use CAM.12 In a subsequent study using the same 2007 NHIS data, Birdee et al found that CAM use was high in children with gastrointestinal conditions, headaches, musculoskeletal conditions, and psychological conditions.13 In a recent study looking at CAM use in children with recurrent headaches, children who experience headaches are 2.1 times more likely to use CAM.14 Other studies have found that CAM use was higher in those with a chronic medical condition such as cancer, juvenile idiopathic arthritis and sickle cell anemia compared to the general population.15
Because there has been demonstrated efficacy for some CAM therapies, many tertiary pain centers in the United States have adopted a multidisciplinary approach to pain management that incorporates use of at least a subset of CAM modalities. In a 2005 survey of 43 pediatric anesthesiology fellowship programs, 38 reported that their clinical services to patients included one or more CAM modalities including: biofeedback (65%), guided imagery (49%), relaxation therapy (33%), massage (35%), hypnosis (44%), acupuncture (33%), art therapy (21%), and meditation (21%).16 There is some evidence that the longer a child experiences pain, the more likely s/he is to express an interest in trying CAM treatment approaches.17
Pain syndromes in childhood can have long-term negative consequences. As such, chronic pain in childhood, whether functional or organic, often leads to chronic pain with psychosocial co-morbidities in adulthood. However, studies have shown that increased coping mechanisms can potentially mediate the development of long-term co-morbidities. A recent longitudinal study by Walker et al. followed children with functional abdominal pain for nine years and evaluated differential health outcomes based on patient characteristics, including measures of coping. The authors report that children with the same intensity of pain, yet lower perceived pain coping efficacy, had higher levels of negative affect, increased pain catastrophizing, increased functional disability, and twice the prevalence of co-morbid chronic pain and psychiatric disorders compared to than their counterparts with higher coping efficacy. The children with lower coping efficacy were more likely to meet criteria for functional gastrointestinal disorder as adults.18
To our knowledge, only the Tsao study17 has focused specifically on CAM use in children presenting to a tertiary chronic pain center. This study reported on interest in CAM, but there have been no studies looking at correlates of actual CAM use in this population. The objective of our study is to examine correlates of current or prior CAM use in a pediatric population chronic pain, and to determine if CAM use is positively correlated with increased coping skills. We hypothesize that prior or current CAM use is correlated with longer pain duration, higher pain intensity, and more functional disability. We also hypothesize that CAM use is positively correlated with more accommodative coping skills.
Methods
Population Studied and Data Collected
We examined patient data (n=1175) collected from 2003 – 2011 of children ages 7–17 who completed the intake assessment battery at the time of initial clinical evaluation at Boston Children’s Hospital Pain Treatment Service multidisciplinary chronic pain outpatient clinic. This age range was selected based on the ages appropriate to complete the validated measures that are incorporated into the assessment battery. Patients and parents each completed a set of questionnaires as part of this initial evaluation. Questionnaires completed by child participants addressed pain characteristics (intensity, duration, and location), psychological functioning, pain coping skills, and functional disability. In addition parents were asked whether their child has tried various CAM modalities in the past for his/her pain.
Exposures and Their Measurement
Pain intensity was recorded using a self-reported numerical analog scale ranging from 0 = ”no pain” to 10 = ”worst pain imaginable.” Pain intensity was recorded as the intensity on the day of the initial evaluation.19 Father’s and mother’s highest levels of education was used as a proxy for socioeconomic status. Given the high correlation between the two, in multivariable analysis we included only father’s education. Anxiety was measured by the Revised Children’s Manifest Anxiety Scale (RCMAS) which is a 39-item child self-report questionnaire that assesses anxiety symptoms and is validated for children ages 8–19.20 Depressive symptoms were measured by the Children’s Depression Inventory (CDI), which is a 27-item child self-report assessing depressive symptoms experienced in the last two weeks. Higher scores indicate higher levels of depressive symptoms. The CDI is validated for children ages 7–17.21 Functional Disability was measured by the Functional Disability Inventory (FDI) which is a 15-item child self-report assessing difficulty in physical and psychosocial functioning due to their physical health. Higher scores indicate higher levels of functional disability. The FDI is validated for children ages 8–18.22
Outcomes and Their Measurement
Exposure to CAM modalities is measured by parent-report of whether the patient has used any of the following modalities for their pain: biofeedback, hypnosis, massage, and acupuncture and “other.” These techniques were then re-categorized to bio-behavioral - including biofeedback, relaxation training and hypnosis - acupuncture, massage and other CAM. We also combined all CAM modalities into a single dichotomous variable representing exposure to any of the above CAM techniques. Coping is measured by the Pain Response Inventory (PRI), which is a 60-item self-report assessing pain coping styles.23 The PRI generates scores for 3 coping styles: active – which involves taking action to change or influence stressful circumstances, passive - which involves orientation away from the stressor, and accommodative - which involves efforts to accept and/or adapt to the stressor. In this study we used the accommodative coping sub-scale as it is the most relevant indicator of a positive, adaptive coping style. The active coping sub-scale was not used given inconsistent patterns of associations found in previous studies. Some studies have found an association between the PRI’s active coping subscale and more pain and disability.24
Analysis
To determine correlates of CAM use, co-variates selected a priori (parent’s education, age, race, gender, pain duration, pain intensity, anxiety, depression, and functional disability) that had a p-value less than 0.05 in a bi-variable analysis, using a t-test, were entered into a multivariable logistic regression model. This strategy was repeated to determine correlates of each type of CAM use: bio-behavioral, massage, and acupuncture.
To determine the relationship between CAM and accommodative coping, co-variates selected a priori that had a p-value less than 0.05 in a bivariable analysis were entered into a multivariable linear regression model with accommodative coping as the outcome variable. This strategy was repeated to determine the relationship of bio-behavioral CAM and accommodative coping.
All analyses were performed using commercial software, SAS v9.3. The study was approved by Boston Children’s Hospital’s Institutional Review Board.
Results
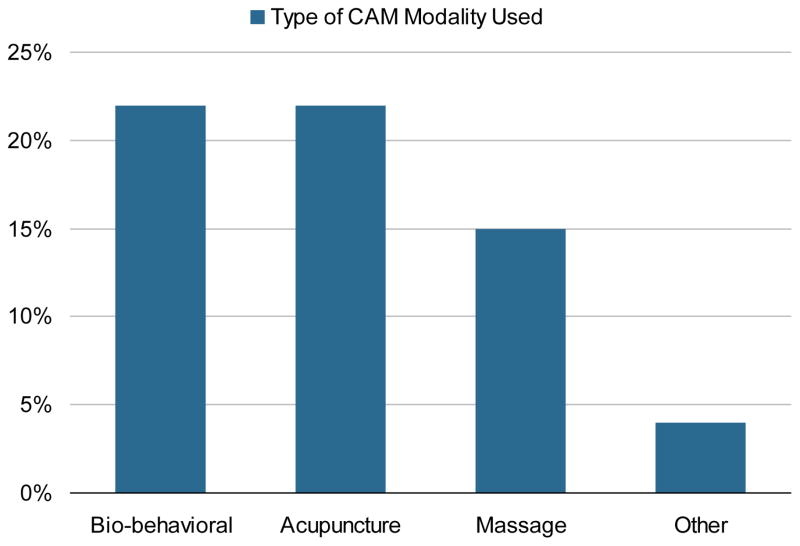
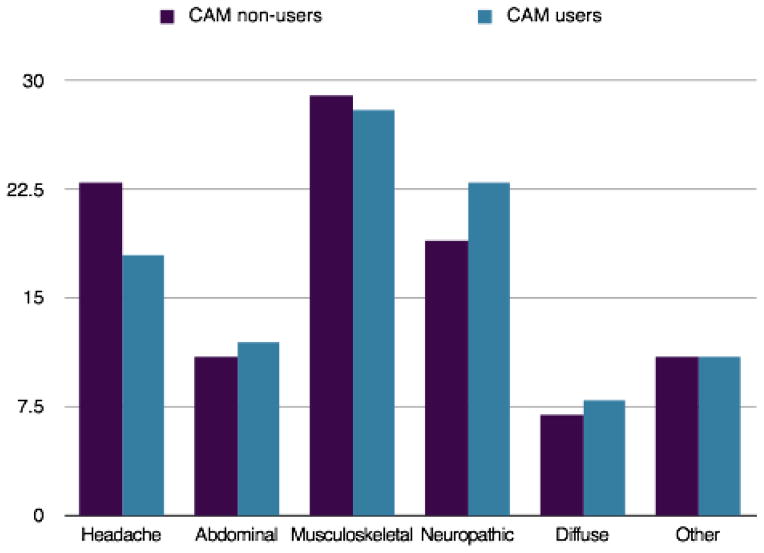
The mean (SD) age of our sample was 13.8 (2.5) years. Most common types of reported pain were musculoskeletal, neuropathic pain, and headache (Figure 1). In our sample, 497 (42%) reported exposure to CAM, most commonly acupuncture (22%), massage (22%), and bio-behavioral (15%), (Figure 2). The number of children who reported concurrent use of multiple CAM modalities was 182 (15.5%).
Figure 1. Type of CAM Modality Used in a Tertiary Pain Center (n=1175).
aBio-behavioral CAM includes: relaxation training, hynosis, and biofeedback
Figure 2.
Types of Pain at a Tertiary Pain Center (n=1175)
In Table 1, we report the socio-demographic characteristics, pain characteristics, functional disability, and psychosocial characteristics for CAM users and non-CAM users. Among both CAM users and non-users, mean scores on the functional disability measure fell within the moderately disabled range. Mean scores for the indicators of psychological distress (anxiety and depressive symptoms) were within the normative range for both groups. In our bivariable analysis, CAM use was higher in patients who were white, older, female, and had fathers with higher levels of education. Compared to non-users, CAM users reported significantly higher pain intensity and more functional disability.
Table 1.
Demographics of Children at a Tertiary Pain Center
| n= 1175 | CAM Non-User n=678 (58%) | CAM Users n=497 (42%) | P-value |
|---|---|---|---|
|
| |||
| Age, mean (SD), years | 13.8 (2.6) | 14.1(2.4) | 0.038 |
|
| |||
| Gender | |||
| Male | 27% (183/678) | 20% (97/497) | |
| Female | 73% (495/678) | 80% (400/497) | 0.003 |
|
| |||
| Race | |||
| White | 88% (593/671) | 92% (453/491) | |
| Non-White | 12% (78/671) | 8% (38/491) | 0.03 |
|
| |||
| Father’s Education, mean (SD), years | 15.1 (2.79) | 15.7 (2.71) | <.001 |
|
| |||
| Pain Duration, mean (SD), months | 25.0 (29.1) | 25.9 (28.5) | 0.61 |
|
| |||
| Pain Intensity, mean (SD)a | 4.3 (2.9) | 4.9 (2.9) | <.001 |
|
| |||
| Currently on Pain Medications | 73% (358/493) | 81% (329/407) | <.001 |
|
| |||
| Depression, mean (SD), CDIb | 50.7 (12.1) | 51.2 (12.1) | 0.51 |
|
| |||
| Anxiety, mean (SD), RCMASc | 48.6 (10.3) | 48.9 (9.6) | 0.59 |
|
| |||
| Functional Disability, mean (SD), FDId | 20.5 (12.2) | 23.5 (11.9) | <.001 |
Current pain on a 10 point numeric rating scale
Children’s Depression Inventory
Revised Children’s Manifest Anxiety Scale
Functional Disability Inventory
In an adjusted multivariable logistic regression model (Table 2), we found that female gender (OR 1.47, CI 1.07–2.01), more years of parental education (OR 1.11, CI 1.06–1.16), greater pain intensity on an 11 point numerical analog scale (OR 1.06, CI 1.01–1.11), and more functional disability (OR 1.19 per 10 point increment on the Functional Disability Inventory, CI 1.06–1.34) were independently associated with CAM use. Although CAM users were reported significantly higher pain medication use in our bivariable analysis, this was not added to the model due to the extent of missing data on pain medication use.
Table 2.
Correlates of CAM use in a Tertiary Pain Centera
| n=1175 | Odds Ratio | Confidence Intervals | P-value |
|---|---|---|---|
| Gender (Female) | 1.48 | 1.07–2.02 | 0.02 |
| Father’s Education | 1.11 | 1.06–1.16 | <.001 |
| Functional Disabilityb | 1.19 | 1.06–1.34 | 0.003 |
| Pain Intensity | 1.06 | 1.01–1.11 | 0.02 |
Multivariable model adjusted for age, race, and pain duration
Odds ratio for 10 point increment on the Functional Disability Inventory
In an adjusted linear multivariable model (Table 3) we found that although report of any CAM use was not significantly correlated with better accommodative coping skills, specific report of bio-behavioral CAM strategy use was statistically correlated with accommodative coping skills (β 0.2 p-value .004). Accommodative coping was associated with some of the demographic characteristics of the sample. Specifically, females reported greater use of accommodative coping skills compared to males (t-test, p-value <.05). Age was also positively correlated with greater use of accommodative coping skills (r = .13, p-value <.01).
Table 3.
Correlates of Accommodative Coping Skills in a Tertiary Pain Center Multivariable Modela
| n=612 | Beta | P-value |
|---|---|---|
| Any CAM | 0.1 | 0.17 |
| Bio-behavioral CAMb | 0.2 | 0.04 |
Multivariable model adjusted for age, gender, race, father’s education, current pain, functional disability, pain duration, depression, and anxiety
Bio-behavioral CAM includes: relaxation training, hypnosis, and biofeedback
Discussion
Tertiary chronic pain clinics are often viewed as the “last resort” for children suffering from chronic pain conditions. In a sample of children presenting for treatment in this setting with an average time since pain onset of more than two years, we found the prevalence of previous exposure to CAM to be 42%. CAM users in our sample were more likely to be, female, white, and from more highly educated families. They reported higher pain intensity and were more functionally disabled compared to children who reported no past experience with CAM. We also found that children who use bio-behavioral CAM endorse more adaptive coping mechanisms than non-CAM users and these children are more likely to be older and female.
Our results support those of the study by Birdee et al examining correlates of CAM use in the general pediatric population from the 2007 NHIS. This study also demonstrated that children who have tried CAM report greater pain chronicity, with more functional disability and higher pain intensity.13 Our sample, was predominately white and female, which is typical of pediatric pain centers.17
In our study females reported more accommodative coping skills, however, Walker et al, found that males and not females used more accommodative coping, therefore our findings are contradictory. However, there have been equivocal findings in terms of gender differences in the types of coping strategies used both specifically in coping with chronic pain and more generally in the general pediatric population. 25, 26, 27, 28
There is limited efficacy for drugs in treating pediatric chronic pain, and many studies demonstrate that certain CAM modalities have equal or better efficacy for certain types of pain, either in adjunct with standard of care, or as a stand-alone treatment,.4,5,6,7 However, in this patient population, after approximately 2 years of pain, the majority of patients had not tried a CAM modality, suggesting a potential missed opportunity for pursuing effective modalities as adjuncts to chronic pain management earlier in the course of chronic pain treatment.
Potential barriers to patients accessing CAM services prior to their care at a multidisciplinary pain center are a lack of general knowledge regarding referrals, lack of pediatrician exposure to CAM, and perceived cost. In 2001 a survey developed by the AAP found that most pediatricians are not comfortable discussing these therapies unless they have had a personal experience with them. Fewer than 5% of pediatricians surveyed felt knowledgeable about any CAM therapy, although 66% felt that CAM therapies could enhance recovery and help relieve symptoms.29
Following a recent Cochrane Review, gut-directed hypnosis has been recommended in recent guidelines for adult patients suffering from irritable bowel syndrome (IBS) 30, 31, 32 and in a recent systematic review, gut-directed hypnotherapy seemed superior to standard medical care in children with functional abdominal pain or IBS. 8 Thus, services may be accessible to patients if pediatricians can engage in better outreach to identify appropriate providers and provide this information to their patients.
Interestingly, many of these modalities, such as relaxation techniques, hypnosis, guided imagery, and biofeedback, are often performed by psychologists, and many are covered by insurance. Since CAM modalities have been shown to be used more in populations with higher income, providing this information to pediatricians could increase the use of bio-behavioral CAM in adjunct with standard treatments and reach a larger population of children who have chronic pain.
There are several limitations to our study. Because the study is cross-sectional, we are unable to determine causation and only report associations. Our database also is not a comprehensive inquiry of CAM and therefore several specific CAM modalities including: mediation, herbs, yoga, tai chi, and qi gong might not have been captured in “Other CAM.” We do not know the frequency of previous or current CAM use among the sample (single vs. multiple exposures). Parental self-report of CAM is an imperfect measure and therefore it is possible that the percentage of using CAM could be higher in this population. Additionally the Pain Treatment Service at Boston Children’s Hospital is a well-established tertiary service with a history of collaboration with CAM providers. Findings may not be generalizable to other clinics settings or to areas of the country where such services are more difficult to access. Nonetheless, this study provides valuable information regarding a difficult pediatric chronic pain population where pharmacological therapy is limited.
This study adds to the prior literature that suggests an interest in CAM in the pediatric pain population and more CAM exposure in those with greater disability and pain. This study also suggests that exposure to bio-behavioral CAM techniques is associated with adaptive coping skills and thus may play a role in modulating the development of psycho-social co-morbidities as these children reach adulthood. In CAM modalities such as acupuncture and massage, patients play a more passive role in their care, unlike bio-behavioral CAM where the patient must actively participate in their care. Perhaps this is why older children are more likely to use bio-behavioral CAM due to increased maturity and ability to understand the benefits of taking a self-management approach to their pain. Therefore, research should further investigate those modalities perceived to be helpful to patients, include randomized controlled efficacy trials, and seek to establish which specific CAM modalities may be best suited for certain chronic pain conditions. Further programs to educate pediatricians about evidence-based and cost-effective CAM approaches to pain are also needed.
What’s New.
Chronic pain is a growing problem in pediatrics and pharmacologic management is limited. There is growing interest in Complementary and Alternative Medicine (CAM) for pain, yet little is known about patterns of CAM use in youth with chronic pain.
Acknowledgments
Funding/Support: This research has been supported by the National Institutes of Health T32 grant and the Harvard Catalyst (ULI RR02575)
Footnotes
Conflicts of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Rachel Vinson, Boston Children’s Hospital, Boston MA. General Pediatrics.
Gloria Yeh, Beth Israel Deaconess Medical Center, Boston, MA. Internal Medicine.
Roger B. Davis, Beth Israel Deaconess Medical Center, Boston, MA. Internal Medicine.
Deirdre Logan, Boston Children’s Hospital, Boston, MA. Pain Treatment Service.
References
- 1.King S, Chambers CT, Huguet A, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. 2011;152(12):2729–2738. doi: 10.1016/j.pain.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 2.Eccleston C, Morley, Williams A, et al. Managing chronic pain in children and adolescents: we need to address the embarrassing lack of data for this common problem. BMJ. 2003;326(7404):1408–1409. doi: 10.1136/bmj.326.7404.1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Center for Complementary and Alternative Medicine. [Accessed April 2012]; http://nccam.nih.gov/sites/nccam.nih.gov/files/D347_05-25-2012.pdf.
- 4.Vlieger AM, Menko-Frankenhus C, Wolfkamp S, et al. Hypnotherapy for children with functional abdominal pain or irritable bowel syndrome: a randomized controlled trial. Gastroenterology. 2007;133(5):1430–1436. doi: 10.1053/j.gastro.2007.08.072. [DOI] [PubMed] [Google Scholar]
- 5.Van Tilburg AL, Chitkara DK, Palsson OS, et al. Audio-recorded guided imagery treatment reduces functional abdominal pain in children: a pilot study. Pediatrics. 2009;124(5):890–897. doi: 10.1542/peds.2009-0028. [DOI] [PubMed] [Google Scholar]
- 6.Palmero TM, Eccleston C, Lewandowski AS, et al. Randomized controlled trials of psychological therapies for management of chronic pain in children and adolescents: an updated meta-analytic review. PAIN. 2011;148(3):387–397. doi: 10.1016/j.pain.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cassileth BR, Vickers AJ. Massage therapy for symptom control: outcome study at a major cancer center. Journal of Pain and Symptom Management. 2004;28(3):244–249. doi: 10.1016/j.jpainsymman.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 8.Rutten J, Reitsma J, Vlieger A, et al. Gut-directed hypnotherapy for functional abdominal pain or irritable bowel syndrome in children: a systematic review. Arch Dis Child. 2013;98:252–257. doi: 10.1136/archdischild-2012-302906. [DOI] [PubMed] [Google Scholar]
- 9.Zeltzer L, Tsao JC, Stelling C, et al. A phase I study on the feasibility and acceptability of an acupuncture/hypnosis intervention for chronic pediatric pain. Journal of Pain and Symptom Management. 2002;24(4):437–446. doi: 10.1016/s0885-3924(02)00506-7. [DOI] [PubMed] [Google Scholar]
- 10.Chung Y, Dumont R. Complementary and alternative therapies: use in pediatric pulmonary medicine. Pediatric Pulmonology. 2011;46:530–544. doi: 10.1002/ppul.21426. [DOI] [PubMed] [Google Scholar]
- 11.Kohen DP. Integrative Pediatrics. New York: Oxford University Press; 2010. A pediatric perspective on mind-body medicine; pp. 267–301. [Google Scholar]
- 12.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. National Health Statistics Report. 2008 Dec 10; [PubMed] [Google Scholar]
- 13.Birdee GS, Phillips RS, Davis RB, et al. Factors associated with pediatric use of complementary and alternative medicine. Pediatrics. 2010;125(2):249–256. doi: 10.1542/peds.2009-1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bethell C, Kemper KJ, Gombojav N, et al. Complementary and conventional medicine use among youth with recurrent headaches. Pediatrics. 132(5):e1173–e1183. doi: 10.1542/peds.2013-1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kemper KJ, Fohra S, Walls R. The use of complementary and alternative medicine in pediatrics. Pediatrics. 2008;122(6):1374–1386. doi: 10.1542/peds.2008-2173. [DOI] [PubMed] [Google Scholar]
- 16.Lin Y, Lee A, Kemper KJ, et al. Use of complementary and alternative medicine in pediatric pain management service: a survey. American Academy of Pain Medicine. 2005;6(6):452–458. doi: 10.1111/j.1526-4637.2005.00071.x. [DOI] [PubMed] [Google Scholar]
- 17.Tsao JC, Meldrum M, Kim SC, et al. Treatment preferences for CAM in children with chronic pain. Evidenced Based CAM. 2007;4(3):367–374. doi: 10.1093/ecam/nel084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walker LS, Sherman AL, Bruehl S, et al. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain. 2012;153(9):1798–1806. doi: 10.1016/j.pain.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Von Baeyer CL, Spagrud LJ, McCormmick JC, et al. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children’s self-reports of pain intensity. Pain. 2009;143(3):223–227. doi: 10.1016/j.pain.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Reynolds CR, Richmond BO. What I think and feel: a revised measure of children’s manifest anxiety. J Abnorm Child Psychol. 1978;6(2):271–280. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- 21.Kovacs M. The Children’s Depression Inventory Manual. North Tanawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- 22.Walker LS, Green JU. The Functional Disability Inventory: measuring a neglected dimension of child health care status. J Pediatr Psychol. 1991;16(1):39–58. doi: 10.1093/jpepsy/16.1.39. [DOI] [PubMed] [Google Scholar]
- 23.Walker LS, Smith CA, Garber J, Deborah A. Development and validation of the Pain Response Inventory for children. Psychol Access. 1997;9(4):392–405. [Google Scholar]
- 24.Simons LE, Lewis Claar R, Logan DL. Chronic pain in adolescence: parental responses, adolescent coping, and their impact on adolescent’s pain behaviors. Journal of Pediatric Psychology. 2008;33(8):894–904. doi: 10.1093/jpepsy/jsn029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walker LS, Baber KF, Garber J, et al. A typology of pain coping strategies in pediatric patients with chronic abdominal pain. Pain. 2008;137(2):266–275. doi: 10.1016/j.pain.2007.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keogh E, Eccleston C. Sex differences in adolescent chronic pain and pain-related coping. Pain. 2006;123(3):275–284. doi: 10.1016/j.pain.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Compas BE, Malcarne VL, Fondacaro KM. Coping with stressful events in older children and young adolescents. Journal of Counseling and Clinical Psychology. 1998;56(3):405–411. doi: 10.1037//0022-006x.56.3.405. [DOI] [PubMed] [Google Scholar]
- 28.Wilson GS, Pritchard ME, Revalee B. Individual differences in adolescent health symptoms: The effects of gender and coping. Journal of Adolescence. 2004;28:369–379. doi: 10.1016/j.adolescence.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Kemper KJ, O’Connor KG. Pediatricians’ recommendations for complementary and alternative medical (CAM) therapies. Ambulatory Pediatrics. 2004;4(6):482–487. doi: 10.1367/A04-050R.1. [DOI] [PubMed] [Google Scholar]
- 30.Webb AN, Kukuruzovic RH, Catto-Smith AG, et al. Hypnotherapy for treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2007;17:CD005110. doi: 10.1002/14651858.CD005110.pub2. [DOI] [PubMed] [Google Scholar]
- 31.Spiller R, Aziz Q, Creed F, et al. Clinical services committee of the British society of gastroenterology. Guidelines on the irritable bowel syndrome: mechanisms and practical management. Gut. 2007;56:1770–1798. doi: 10.1136/gut.2007.119446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Layer P, Andresen V, Pehl C, et al. Irritable bowel syndrome: german consensus guidelines on definition, pathophysiology and management. Z Gastroenterol. 2011;49:237–223. doi: 10.1055/s-0029-1245976. [DOI] [PubMed] [Google Scholar]