1. Introduction
Bipolar disorder can be a debilitating illness with significant morbidity and mortality risk due to suicide. The risk of suicide attempts is 3.9% annually with a corresponding rate of completions of 1% annually (Baldessarini and Pompili, 2006a). This high lethality ratio, defined as the ratio of suicide attempts to completions, reflects the seriousness of all suicide attempts in bipolar disorder (Baldessarini and Pompili, 2006a).
Studies have focused on understanding the factors that increase suicide risk in an effort to curb the excessive mortality rate. Those results suggest that delayed or misdiagnosis, co-morbid substance abuse, and poor medication compliance contribute to less than optimal treatment (Goodwin and Jamison, 2007). Also, the misconception that bipolar type II is a less malignant form of bipolar illness may have led to an underestimation of suicide risk with this subtype (Novick et al., 2010). Studies of the clinical state of bipolar disorder have identified agitated depression or mixed affective states as being particularly high risk situations for suicide attempts and completions (McElroy et al, 2006).
An important area of research has been the impact of medications on suicide risk. Controlled, open-label, and retrospective studies have convincingly demonstrated that long term lithium treatment prevents suicide in bipolar disorder (both types I and II). Baldessarini (Baldessarini et al, 2006b) conducted a meta-analysis of all studies which provided information on suicidal behaviors during lithium treatment. Both open label and controlled trials, with and without a comparator treatment were included in this analysis.
In 31 studies of lithium treatment in subjects with affective illness, the risk of attempted or completed suicide was 5-fold lower during treatment with lithium (RR=4.91, 95% CI 3.82-6.31, p < 0.0001). The results were sustained when the groups were divided into diagnostic groups (bipolar versus other affective illness). He also found a reduction in the lethality index with lithium, with the ratio of attempts to suicides increasing 2.5 fold (6.94 %/year versus 2.79 %/year). A second meta-analysis (Cipriani et al, 2005) of 32 randomized controlled trials of lithium for mood disorders also demonstrated a significant reduction in both suicide (60% decrease) and in deliberate self harm (70% decrease) with lithium.
How do other medications used to treat bipolar disorder compared to lithium in terms of suicidal behavior? In a large retrospective study, Goodwin (Goodwin et al, 2003) found lithium to be more protective against suicide attempts and completion than divalproex in bipolar disorder. In a retrospective naturalistic study, Yerevanian (Yerevanian et al, 2007a) found no difference in attempted suicide rates between carbamazepine, divalproex, and lithium. A study of 372 patients by Bowden (Bowden, 2000) in a one year maintenance treatment study showed no statistical difference in suicide attempts between lithium and divalproex, with a trend toward a lower rate of attempt with divalproex. The data on carbamazepine are mixed. One study of patients with affective disorders or schizophrenia, showed a superior protective effect of lithium relative to carbamazepine in both attempts and completions (Thies-Flechtner et al, 1996) , while Yerevanian's study showed no difference as noted previously. Collins' study of 12,662 Medicaid patients demonstrated a protective effect of lithium for suicide attempts relative to anticonvulsants (Collins and McFarland, 2008). Baldessarini (Baldessarini and Tondo, 2009) reviewed 6 studies of suicide risk during long term treatment with lithium or anticonvulsants. Rates of suicidal acts were 2.86 times higher in the anticonvulsant treated group compared with the lithium group. Overall, it appears that lithium provides more protection against suicide attempts than anticonvulsants, but reports have shown mixed results.
The relationship between typical or first generation antipsychotics and suicide is complicated. Kerwin (Kerwin, 2003) noted that the 13-fold increase in suicide rates in schizophrenia was unaffected by the development of first generation antipsychotic medications. While the conventional antipsychotics did improve symptoms of schizophrenia, they also had the potential to cause depression and had side effect problems such as akathisia and akinesia that led to increased suicide attempts in some cases. Other studies have supported this finding (Drake and Ehrlich, 1985, Shear et al, 1983).
Atypical antipsychotics may help lower suicide risk in patients with schizophrenia. Altamura (Altamura et al, 2003) reported that the relative suicide risk was lower for atypical antipsychotics compared to typical antipsychotics in schizophrenia. Clozapine has demonstrated a reduction in suicide attempts and completion in schizophrenia (Meltzer and Okayli, 1995), and is the only atypical that is FDA labeled for lowering suicide risk in schizophrenia. A large multicenter prospective 2 year study in which schizophrenic subjects were randomized to clozapine or olanzapine (Meltzer et al, 2003) demonstrated lower suicidal behavior in clozapine subjects (hazard ratio=0.76) but no difference in completed suicides between the two groups. A small study comparing 44 chronic schizophrenic patients receiving either clozapine or haloperidol decanoate demonstrated a reduction of suicidality, impulsivity, and aggression in the clozapine group (Spivak et al, 2003). In a twenty eight week study comparing olanzapine and risperidone for schizophrenia and schizoaffective disorder (Tran et al, 1997), subjects on olanzapine had significantly lower suicide attempt rates. Two other studies compared olanzapine to haloperidol in the treatment of schizophrenia. Glazer (Glazer, 1998) found a 2.3 fold reduced risk of suicide in schizophrenic patients on olanzapine relative to haloperidol in a 1 year study, while Beasley and colleagues (Beasley et al, 1998) found no outcome difference in suicidal behavior between olanzapine and haldoperidol, but a decrease in suicidal thoughts in olanzapine subjects. In a six week study, Muller-Siecheneder (Muller-Siecheneder et al, 1998) compared risperidone to the combination of haldoperidol and amitriptyline in schizophrenic, schizoaffective, or psychotically depressed patients. There was no difference in suicidal ideation between the treatment groups. In a retrospective study, Barak and colleagues (Barak et al, 2004) reviewed patient records from 1998-2002. The index group for the study was schizophrenic patients with a previous suicide attempt and the control group was comprised of patients with schizophrenia with no previous suicide attempt, matched for gender and age. The protective effect (odds ratio) of treatment by second generation antipsychotics was significant at 3.54.
While used frequently to treat bipolar disorder as monotherapy or in combination with other mood stabilizers, the effect of atypical or second generation antipsychotics on suicide risk has been understudied. Several case reports of clozapine use in affective disorders note a possible anti-suicide benefit (Vangala et al, 1999, Ranjan and Meltzer, 1996, Suppes et al, 1999). There have been reports of a decrease on the suicide item on the Montgomery Asberg Depression Rating Scale in a bipolar depression study of quetiapine as well as a decrease on the suicidality item on the Hamilton Depression Scale with olanzapine (Houston et al, 2006). In contrast to the aforementioned reports, other studies have indicated an increase in suicidality in bipolar patients on atypical antipsychotics. In a retrospective study by Yerevanian (Yerevanian et al, 2007b), 405 veterans were followed naturalistically over a 3 year period. The rate of suicide attempts were 9.4 times greater during antipsychotic monotherapy compared with mood stabilizer (lithium, carbamazepine, divalproex) monotherapy. In addition the rate of suicide attempts during mood stabilizer plus antipsychotic treatment alone was 3.5 times greater than the rate on mood stabilizer monotherapy. Antipsychotic treatment was associated with a markedly increased rate of suicide attempts. Both first and second generation antipsychotics were used in this analysis and the study was limited by its retrospective design. In addition, clinical severity was not assessed, and patients on combinations of mood stabilizers and antipsychotics may have been more severely ill.
The purpose of this study was to extend the work of Goodwin (Goodwin et al, 2003) and Yerevanian (Yerevanian et al, 2007b), by retrospectively analyzing whether atypical antipsychotics when used alone or in combination with lithium or divalproex affect the suicide attempt rate. Given the high frequency of their use in bipolar disorder and the high lethality associated with this illness, it is important to understand the impact of atypical antipsychotics on suicide potential. Every treatment that is used in bipolar disorder ought to be tested not only for its ability to quell mania or ameliorate depression, but also for its ability to prevent suicide. The main hypothesis of this study was that the use of atypical antipsychotics in combination with lithium or divalproex may provide additional protection against suicide in bipolar patients.
2. Methods
Five VA hospitals (Milwaukee, Durham, Minneapolis, Cleveland, and Madison) participated in this study. Institutional Review boards at all sites approved all study procedures. The William S. Middleton VA (Madison) served as the coordinating center for data. We reviewed data on detailed treatments, suicide events and other study variables between Jan 1, 1999 and December 31, 2004 in this retrospective study. Specific inclusion criteria were: at least one outpatient diagnosis of bipolar disorder type 1 or 2, at least one prescription for lithium, divalproex or both during the study period. Exclusion criteria included: any diagnosis of schizophrenia, schizoaffective disorder, dementia, or any cognitive disorder.
Demographic variables including age, gender, bipolar type (I or II), age at diagnosis, duration of illness, and number of lifetime episodes of mania or depression (if available) were recorded. Medication exposure was calculated using computerized pharmacy records. The period of exposure was assumed to be the beginning dispensing date and continued for the duration of the prescription. For VA prescriptions, lithium, divalproex, and the atypical antipsychotics are dispensed in 30 day prescriptions. Each day was counted as a day of exposure to lithium, divalproex, lithium plus an atypical antipsychotic, divalproex plus an atypical antipsychotic, an atypical antipsychotic alone, or none of these medications. Thus, the same patient could contribute to data in any of the medication exposure groups. For the purposes of the analysis, data were subsequently analyzed by combinations of medications. Pharmacy records were also used to identify concomitant use of antidepressants, benzodiazepines, and other psychiatric medications. Information on other co-morbid psychiatric conditions was not collected, nor were there measures of disease severity. Suicide attempts were established through chart review of emergency room records, inpatient notes, and outpatient notes. Similarly, suicide completions were obtained by chart review of all deceased patients with bipolar disorder, including emergency room records, inpatient notes, and outpatient notes.
Clinical and demographic variables were summarized as frequencies and percentages (categorical variables) or means and standard deviations (continuous variables). A linear mixed effects model with subject specific random effects was used to compare the time spent on medications between medication groups. Suicide attempts were reported per 10,000 months of medication exposure. Crude rates of suicide attempts were reported for periods of treatment with lithium, divalproex and atypical antipsychotics. Furthermore, crude rates of suicide attempts were reported for various medication combinations, i.e., lithium alone, divalproex alone, atypical antipsychotics alone, lithium in combination with divalproex, lithium in combination with atypical antipsychotics, divalproex in combination with atypical antipsychotics, and lithium in combination with divalproex and atypical antipsychotics. A mixed-effects negative binomial model with subject specific random effects was used to evaluate the effects of lithium, divalproex and atypical antipsychotics alone or in combination on suicide attempt rates. A compound symmetry correlation structure was used to account for correlations between repeated measures within the same subject. All P values were 2-sided, and P < .05 was used to indicate statistical significance. Statistical analyses were performed using SAS software version 9.2. (SAS Institute, Cary, NC).
3. Results
Table 1 displays the basic demographic data for the study group. Most subjects were male and had bipolar type I disorder. There were a small number of subjects who were identified as bipolar type I and II during the six year study period. They are categorized in the table as bipolar I/II. The mean number of self-reported lifetime manic or depressive episodes was 5. Reported age of onset data was available for most subjects in the medical record.
Table 1. Demographic variables in study population.
| HOSPITAL | N | % | |
| Durham VA | 458 | 35.1 | |
| Cleveland VA | 26 | 2.0 | |
| Madison VA | 320 | 24.5 | |
| Milwaukee VA | 387 | 29.6 | |
| Minneapolis VA | 115 | 8.8 | |
| GENDER | |||
| Male | 1,151 | 88.1% | |
| Female | 155 | 11.9% | |
| BIPOLAR TYPE | |||
| I | 1,032 | 79.0% | |
| II | 203 | 15.5% | |
| I/II* | 71 | 5.4% | |
| N | Mean | SD | |
| ONSET AGE (yrs) | 1258 | 35.24 | 13.38 |
| TIME SINCE ONSET (yrs) | 1260 | 18.52 | 12.50 |
| Lifetime Number of Manic or Depressive Episodes | 658 | 5.02 | 3.45 |
Subjects were categorized as both type I and type II during the study period
Table 2 shows the characteristics of medication prescriptions that were filled for each patient, as well as the number and rate of suicide attempts by the type of prescriptions filled. Most patients (89%) experienced at least one period during which they were taking none of the three types of medication (lithium, divalproex, or atypical antipsychotics). On average, these patients spent a total of 2.3 separate periods, each lasting 19.8 (±20.8) months for a total of 44.8 (±21.5) months, during which they took none of these medications. Divalproex was the most commonly prescribed medication of the three types, while lithium was the least commonly prescribed. More than three-quarters (77%) of patients filled a prescription of divalproex during the six-year period covered by the study, while 57% filled at least one prescription of antipsychotics, and 42% filled at least one prescription of lithium. Though fewer patients ever used lithium, those who did spent more time on this medication (p<0.0001). In all, patients spent an average of 29.6 (±25.4) months on lithium, compared to 24.0 (±22.1) months on divalproex, and 18.7 (±18.9) months on antipsychotics.
Table 2. Suicide Attempt Data.
| # of Patients | Total time (mo.) | # of Periods | Each Period (mo.) | Suicide Attempts | Suicide Attempts Per 10,000 months | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | Mean | SD | Mean | SD | ||||
| Medications Prescribed | |||||||||
| None1 | 1165 | 89.2 | 44.77 | 21.53 | 2.26 | 19.82 | 20.75 | 69 | 13.2 |
| Lithium | 551 | 42.2 | 29.56 | 25.39 | 1.50 | 19.70 | ----- | 17 | 10.4 |
| Divalproex | 1000 | 76.6 | 24.00 | 22.08 | 1.49 | 16.11 | ------ | 24 | 10.0 |
| Atypical Antipsychotics | 745 | 57.0 | 18.74 | 18.92 | 2.04 | 9.20 | ------ | 28 | 20.1 |
| Medication Combinations | |||||||||
| Lithium only | 436 | 33.4 | 23.75 | 23.43 | 1.70 | 13.98 | 18.54 | 8 | 7.7 |
| Divalproex only | 821 | 62.9 | 19.17 | 19.68 | 1.81 | 10.60 | 15.45 | 11 | 7.0 |
| Atypical Antipsychotics only | 394 | 30.2 | 9.74 | 12.26 | 1.84 | 5.31 | 8.23 | 10 | 26.1 |
| Lithium and divalproex | 145 | 11.1 | 10.94 | 16.88 | 1.23 | 8.91 | 14.72 | 1 | 6.3 |
| Lithium and atypical antipsychotics | 238 | 18.2 | 14.47 | 16.71 | 1.59 | 9.11 | 12.77 | 6 | 17.4 |
| Divalproex and atypical antipsychotics | 464 | 35.5 | 12.44 | 15.58 | 1.81 | 6.87 | 11.89 | 10 | 17.3 |
| Lithium, divalproex and atypical antipsychotics | 99 | 7.6 | 9.13 | 12.91 | 1.37 | 6.65 | 10.32 | 2 | 22.1 |
Subjects not on lithium, divalproex or atypical antipsychotics
When the combination of medications is considered, more than three-fifths (63%) of the patients experienced at least one period taking only divalproex, while 11% spent at least one period taking both lithium and divalproex, 36% spent at least one period taking divalproex and antipsychotics, and 8% spent at least one period taking all three medications. About one-third (33%) of patients spent at least one period filling prescriptions for lithium alone, while an additional 18% experienced one period during which they took both lithium and an antipsychotic. Nearly one-fifth (18%) of patients filled at least one prescription for an antipsychotic during the study period when they were not taking either lithium or divalproex.
Patients took divalproex alone during an average of 1.8 periods with each period (on average) of 10.6 (±15.5) months, for an average total of 19.2 (±19.7) months. In addition, they took divalproex and lithium together during an average of 1.2 periods for 8.9 (±14.7) months each for an average 10.9 (±16.9) months, while they took divalproex and antipsychotics during 1.8 periods, each lasting 6.9 (±11.9) months, for a total of 12.4 (±15.6) months. Patients who took lithium alone did so for 1.7 periods, each lasting 14.0 (±18.5) months for a total of 23.8 (±23.4) months. They took lithium along with antipsychotics for 1.6 periods, each lasting 9.1 (±12.8) months, for a total of 14.5 (±16.7) months. Patients took antipsychotics alone for the shortest time; they took them over 1.8 periods of 5.3 (±8.2) months each for an average total of 9.7 (±12.3) months. Finally, the 8% of patients who took all three medications did so over an average of 1.4 periods, each lasting 6.7 (±10.3) months, for a total of 9.1 (±12.9) months.
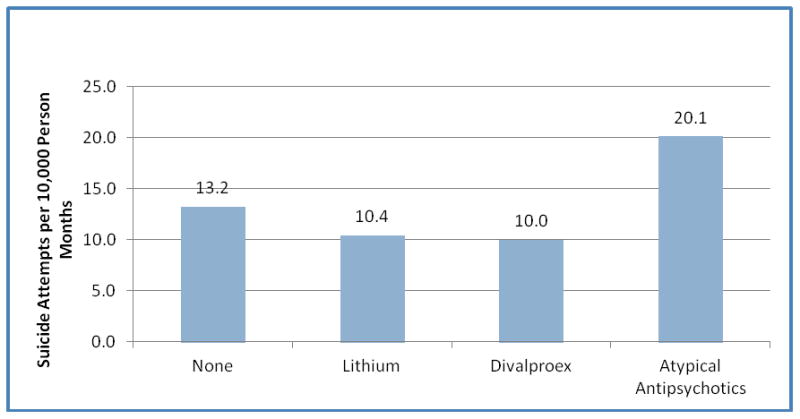
There were 117 suicide attempts over the six-year duration of the study. Nearly three-fifths (59%) of these attempts occurred when the patient was on no medication (i.e. not on lithium, divalproex, or atypical antipsychotic), while 15% occurred when the patient was taking lithium, 21% occurred when the patient was taking divalproex, and 24% occurred when the patient was taking an atypical antipsychotic. In 2 attempts, patients were taking other mood stabilizers (lamotrigine, topiramate, or carbamazepine). The aforementioned attempt rates do not take into account the length of exposure time for each medication. To assess this, we examined the rates of attempted suicide per 10,000 exposure months. As shown in Figure 1, patients experienced the fewest suicide attempts when they were taking divalproex or lithium; for every 10,000 divalproex exposure months patients made 10.0 attempts, while they made 10.4 attempts for every 10,000 lithium exposure months. In contrast, patients who were not taking any medications made 13.2 attempts per 10,000 exposure months. Patients experienced the highest rate of suicide attempts when they were taking antipsychotics: these patients made 20.1 suicide attempts for every 10,000 months they were exposed to antipsychotics.
Figure 1. Suicide Attempts by medication ever prescribed.
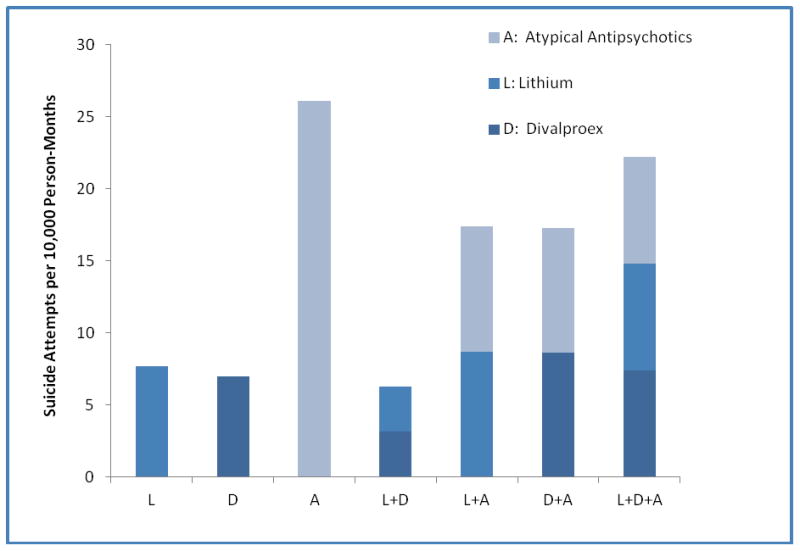
The above rates did not take into account that during many of these periods, the patient was on more than one medication. When the rates are examined by the combination of medications the patient was taking, most of these differences were preserved (Figure 2). The lowest suicide attempt rates occurred when the patient was taking both lithium and divalproex (6.3 attempts per 10,000 months of exposure), followed by taking only divalproex (7.0 attempts per 10,000 months of exposure), and only lithium (7.7 attempts per 10,000). In contrast, suicide attempt rates were more than double when the patient was taking an antipsychotic in addition to either lithium or divalproex (17.4 attempts per 10,000 months of exposure and 17.4 attempts per 10,000 months of exposure respectively). Patients who were only taking an antipsychotic experienced the highest suicide attempt rates (26.1 attempts per 10,000 months of exposure). Those who are taking all three types of medication (22.1 attempts per 10,000 months of exposure) had suicide attempt rates that are lower than those taking only antipsychotic, but higher than other combinations of any two mediations.
Figure 2. Suicide Attempts for Combinations of Medications.
The effects of lithium, divalproex, and antipsychotics were examined together in a mixed-effects negative binomial model (Table 3). The analysis was adjusted by time since onset of illness and age at onset of bipolar illness which were included as covariates in this model to function as a surrogate for illness severity. A significant increase in the odds or suicide attempts was observed for patients who took antipsychotics when compared to patients who did not take antipsychotics (odds ratio: 2.5; 95% CI: 1.5 – 3.9). No significant effects on suicide attempts were detected for lithium and divalproex in this regression analysis. There were 2 subjects that completed suicide during the study period, one on no medication, and the other on divaloproex.
Table 3. Mixed-Effects Negative Binomial Regression Model Results.
| Medication | OR† | Standard Error | 95% CI‡ | p-value* |
|---|---|---|---|---|
| Lithium | 1.03 | 0.27 | 0.61 – 1.73 | 0.934 |
| Divalproex | 1.08 | 0.25 | 0.66 – 1.68 | 0.746 |
| Antipsychotic | 2.45 | 0.57 | 1.55 – 3.86 | 0.001 |
Odds ratio for suicide attempt for drug exposure versus no exposure
95% confidence interval of OR
p-value for testing whether OR is different from one
4. Discussion
Medication adherence is the key to relapse prevention and potential suicide prevention. One notable finding of this study was the significant amount of time during which subjects were not on either lithium, divalproex, or an atypical antipsychotic. Nearly 90% of subjects spent an average of 45 months during the 6 year period on none of these medications. Most attempts (59%) occurred when veterans were on neither lithium, divalproex, nor an atypical antipsychotic. Clearly there is a need to focus on how to improve medication compliance in veterans with bipolar disorder.
In this study, divalproex was the most commonly prescribed medication. This finding in veterans is consistent with previous studies in the general population suggesting an uptrend of prescriptions for divaloproex and downtrend of lithium prescriptions over past 2 decades (Shulman et al, 2003). Although lithium was least commonly prescribed, patients on lithium spent significantly longer periods of time on this medication (14 months), compared to divalproex (11 months) and atypical antipsychotics (5 months).
Our study supports the protective effect of lithium and divalproex against suicide attempts, when used individually or in combination. Rates of suicide attempts per 10,000 months of exposure were 7.7(lithium), 7.0 (divalproex) and 6.3 (lithium plus divalproex) respectfully. This finding is consistent with reports from other studies (Baldessarini et al, 2006, Cipriani et al, 2005, Yerevanian et al, 2007a, Bowden, 2000).
Atypical antipsychotics are often used in clinical practice as a single agent for the treatment of bipolar illness. In this study, subjects only on an atypical antipsychotic had a high suicide attempt rate (26.2 per 10,000 months of exposure). While subject severity data were not directly available in this study, our mixed effects binomial model adjusted for both duration of illness and age of onset, with the assumption that these two variables may approximate overall severity of illness. In that analysis, subjects on atypical antipsychotics had a higher risk for suicide attempts compared to lithium or depakote.
Subjects on combinations of medications likely had more severe bipolar disorder. Indeed, those patients taking combinations of lithium or divalproex plus an atypical antipsychotic showed a higher rate of suicide attempts than either lithium or divalproex alone. The number of suicide attempts per 10,000 months of drug exposure was still highest when subjects were on atypical antipsychotics alone, even compared to lithium plus an atypical or divalproex plus an atypical antipsychotic, suggesting that it is lithium and divalproex that provide a protective effect against suicide attempts. The findings also suggest a possible negative effect of atypical antipsychotics on suicide risk in this population after taking into consideration the severity of bipolar disorder, as discussed above. These results are consistent with the findings of Yerevanian (Yerevanian et al, 2007b).
Subjects may have been on alternative mood stabilizers such as carbamazapine, topiramate, or lamotrigine during this time, or on no psychiatric medication. To address this issue, we analyzed the group of 74 subjects that was on other mood stabilizers (carbamazepine, topiramate or lamotrigine) and found that only 2 subjects on these alternative mood stabilizers had a suicide attempt. The issues of suicide attempts during switching of mood agents needs to be accounted for, as it is the transition from one agent to another is ordinarily a period of high risk for suicide. Only 5 out of 117 suicide attempts occurred during the transition from one medication to another in this study. Second, the addition of antidepressants to mood stabilizers may predispose a patient to mania, or a mixed state, thereby increasing the risk potential for a suicide attempt. Subjects on lithium, divalproex, or atypical antipsychotics were on antidepressants at different times and for varying durations. An analysis showed that the suicide attempt rate was 17.8 per 10,000 months of exposure when subjects were taking antidepressants in addition to lithium, divalproex, or an atypical antipsychotic. These subjects might have been at higher risk because of the antidepressant or may have been more severely ill.
There are limitations of this study. First, the study was purely retrospective, not prospective, and all information gathered was from detailed systematic chart review. Second, as noted earlier, the severity of illness was not measured directly. Subjects with more severe illness may have ended up on combinations of lithium or divalproex plus atypical antipsychotics, or on all three. It is impossible to completely understand the relationship between severity of illness and suicide with the current study design. This study did not track psychotic symptoms in subjects. The relationship between psychosis and suicide is unclear, with studies showing no difference in suicide risk and other studies finding an elevated risk (Goodwin and Jamison, 2007). In addition, the clinical state of subjects was not tracked, nor were co-morbid disorders such as substance abuse, which could have contributed to suicide risk. The possible different effect among individual antipsychotics on suicide risk were not studied due to sample size. In addition, information on medication exposure was obtained from pharmacy records only.
Future work needs to focus on improvement of medication compliance in our veteran population with bipolar disorder. This study found some differences between suicide attempt risk and type of medication in favor of the protective effect of lithium or divalproex relative to atypical antipsychotics. With regard to this relative risk, future studies should be prospective in design, include all mood stabilizers, ancillary psychiatric medications, psychotic symptoms, co-morbid conditions including substance abuse, and a measure of severity of illness to validate our preliminary findings.
Supplementary Material
References
- Altamura AC, Bassetti R, Bignotti S, Pioli R, Mundo E. Clinical variables related to suicide attempts in schizophrenic patients: A retrospective study. Schizophr Res. 2003;60:47–55. doi: 10.1016/s0920-9964(02)00164-0. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Pompili M. Suicide in bipolar disorder: Risks and management. CNS Spectrums. 2006;11:465–471. doi: 10.1017/s1092852900014681. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L, Davis P, Pompili M, Goodwin FK, Hennen J. Decreased risk of suicides and attempts during long-term lithium treatment: A meta-analytic review. Bipolar Disord. 2006;8:625–639. doi: 10.1111/j.1399-5618.2006.00344.x. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L. Suicidal risks during treatment of bipolar disorder patients with lithium versus anticonvulsants. Pharmacopsychiatry. 2009;42:72–75. doi: 10.1055/s-0028-1103291. [DOI] [PubMed] [Google Scholar]
- Barak Y, Mirecki I, Knobler HY, Natan Z, Aizenberg D. Suicidality and second generation antipsychotics in schizophrenia patients: A case-controlled retrospective study during a 5-year period. Psychopharmacology (Berl) 2004;175:215–219. doi: 10.1007/s00213-004-1801-2. [DOI] [PubMed] [Google Scholar]
- Beasley CM, Sayler ME, KGM, Potvin JH, Tollefson GD. Schizophrenia Research. 1998;29:28. [Google Scholar]
- Bowden CL. Efficacy of lithium in mania and maintenance therapy of bipolar disorder. J Clin Psychiatry. 2000;61(suppl 9):35–40. [PubMed] [Google Scholar]
- Cipriani A, Pretty H, Hawton K, Geddes JR. Lithium in the prevention of suicidal behavior and all-cause mortality in patients with mood disorders: A systematic review of randomized trials. Am J Psychiatry. 2005;162:1805–1819. doi: 10.1176/appi.ajp.162.10.1805. [DOI] [PubMed] [Google Scholar]
- Collins JC, McFarland BH. Divalproex, lithium and suicide among medicaid patients with bipolar disorder. J Affect Disord. 2008;107:23–28. doi: 10.1016/j.jad.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Drake RE, Ehrlich J. Suicide attempts associated with akathisia. Am J Psychiatry. 1985;142:499–501. doi: 10.1176/ajp.142.4.499. [DOI] [PubMed] [Google Scholar]
- Glazer WM. Formulary decisions and health economics. J Clin Psychiatry. 1998;19(59 suppl):23–29. [PubMed] [Google Scholar]
- Goodwin FK, Fireman B, Simon GE, Hunkeler EM, Lee J, Revicki D. Suicide risk in bipolar disorder during treatment with lithium and divalproex. JAMA. 2003;290:1467–1473. doi: 10.1001/jama.290.11.1467. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Jamison KR. Manic Depressive Illness: Bipolar disorders and recurrent depression. Oxford University Press; New York, NY: 2007. [Google Scholar]
- Houston JP, Ahl J, Meyers AL, Kaiser CJ, Tohen M, Baldessarini RJ. Reduced suicidal ideation in bipolar I disorder mixed-episode patients in a placebo-controlled trial of olanzapine combined with lithium or divalproex. J Clin Psychiatry. 2006;67:1246–1252. doi: 10.4088/jcp.v67n0811. [DOI] [PubMed] [Google Scholar]
- Kerwin R. Preventing suicide. Br J Psychiatry. 2003;182:366. doi: 10.1192/bjp.182.4.366. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Kotwal R, Kaneria R, Keck PE., Jr Antidepressants and suicidal behavior in bipolar disorder. Bipolar Disord. 2006;8:596–617. doi: 10.1111/j.1399-5618.2006.00348.x. [DOI] [PubMed] [Google Scholar]
- Meltzer HY, Okayli G. Reduction of suicidality during clozapine treatment of neuroleptic-resistant schizophrenia: Impact on risk-benefit assessment. Am J Psychiatry. 1995;152:183–190. doi: 10.1176/ajp.152.2.183. [DOI] [PubMed] [Google Scholar]
- Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A, Bourgeois M, Chouinard G, Islam MZ, Kane J, Krishnan R, Lindenmayer JP, Potkin S, International Suicide Prevention Trial Study Group Clozapine treatment for suicidality in schizophrenia: International suicide prevention trial (InterSePT) Arch Gen Psychiatry. 2003;60:82–91. doi: 10.1001/archpsyc.60.1.82. [DOI] [PubMed] [Google Scholar]
- Muller-Siecheneder F, Muller MJ, Hillert A, Szegedi A, Wetzel H, Benkert O. Risperidone versus haloperidol and amitriptyline in the treatment of patients with a combined psychotic and depressive syndrome. J Clin Psychopharmacol. 1998;18:111–120. doi: 10.1097/00004714-199804000-00003. [DOI] [PubMed] [Google Scholar]
- Novick DM, Swartz HA, Frank E. Suicide attempts in bipolar I and bipolar II disorder: A review and meta-analysis of the evidence. Bipolar Disord. 2010;12:1–9. doi: 10.1111/j.1399-5618.2009.00786.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranjan R, Meltzer HY. Acute and long-term effectiveness of clozapine in treatment-resistant psychotic depression. Biol Psychiatry. 1996;40:253–258. doi: 10.1016/0006-3223(95)00305-3. [DOI] [PubMed] [Google Scholar]
- Shear MK, Frances A, Weiden P. Suicide associated with akathisia and depot fluphenazine treatment. J Clin Psychopharmacol. 1983;3:235–236. doi: 10.1097/00004714-198308000-00006. [DOI] [PubMed] [Google Scholar]
- Shulman KI, Rochon P, Sykora K, Anderson G, Mamdani M, Bronskill S, Tran CT. Changing prescription patterns for lithium and valproic acid in old age: Shifting practice without evidence. BMJ. 2003;326:960–961. doi: 10.1136/bmj.326.7396.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spivak B, Shabash E, Sheitman B, Weizman A, Mester R. The effects of clozapine versus haloperidol on measures of impulsive aggression and suicidality in chronic schizophrenia patients: An open, nonrandomized, 6-month study. J Clin Psychiatry. 2003;64:755–760. doi: 10.4088/jcp.v64n0703. [DOI] [PubMed] [Google Scholar]
- Suppes T, Webb A, Paul B, Carmody T, Kraemer H, Rush AJ. Clinical outcome in a randomized 1-year trial of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry. 1999;156:1164–1169. doi: 10.1176/ajp.156.8.1164. [DOI] [PubMed] [Google Scholar]
- Thies-Flechtner K, Muller-Oerlinghausen B, Seibert W, Walther A, Greil W. Effect of prophylactic treatment on suicide risk in patients with major affective disorders. data from a randomized prospective trial. Pharmacopsychiatry. 1996;29:103–107. doi: 10.1055/s-2007-979553. [DOI] [PubMed] [Google Scholar]
- Tran PV, Hamilton SH, Kuntz AJ, Potvin JH, Andersen SW, Beasley C, Jr, Tollefson GD. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacol. 1997;17:407–418. doi: 10.1097/00004714-199710000-00010. [DOI] [PubMed] [Google Scholar]
- Vangala VR, Brown ES, Suppes T. Clozapine associated with decreased suicidality in bipolar disorder: A case report. Bipolar Disord. 1999;1:123–124. doi: 10.1034/j.1399-5618.1999.010210.x. [DOI] [PubMed] [Google Scholar]
- Walker AM, Lanza LL, Arellano F, Rothman KJ. Mortality in current and former users of clozapine. Epidemiology. 1997;8:671–677. doi: 10.1097/00001648-199710000-00010. [DOI] [PubMed] [Google Scholar]
- Yerevanian BI, Koek RJ, Mintz J. Bipolar pharmacotherapy and suicidal behavior. part I: Lithium, divalproex and carbamazepine. J Affect Disord. 2007;103:5–11. doi: 10.1016/j.jad.2007.05.019. [DOI] [PubMed] [Google Scholar]
- Yerevanian BI, Koek RJ, Mintz J. Bipolar pharmacotherapy and suicidal behavior part 3: Impact of antipsychotics. J Affect Disord. 2007;103:23–28. doi: 10.1016/j.jad.2007.05.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


