Abstract
Objective. To determine the feasibility and effectiveness of adding a hand hygiene exercise in self-screening for Methicillin-Resistant Staphylococcus Aureus (MRSA) nasal colonization to a health care delivery course for first-year pharmacy (P1) students.
Design. About one month after students were trained in hand hygiene technique and indications, faculty members demonstrated how to self-screen for MRSA nasal colonization. Students were then asked to screen themselves during the required class time. Aggregated class results were shared and compared to prevalence estimates for the general population and health care providers.
Assessment. The 71 students present in class on the day of the self-screening exercise chose to participate. A survey comparing presecreening and postscreening responses indicated incremental improvements in student knowledge and awareness of health care associated infections and motivation to perform hand hygiene. On the written exam, student performance demonstrated improved knowledge compared to previous class years.
Conclusion. Self-screening for MRSA nasal colonization in a health care delivery course for P1 students increased students’ motivation to perform hand hygiene techniques and follow indications promulgated by the World Health Organization.
Keywords: hand hygiene, health care associated infection, prevention, MRSA, screening, colonization
INTRODUCTION
Methicillin-resistant Staphylococcus aureus (MRSA) is a common cause of health care associated infections, and the incidence of community-acquired infections has increased in recent years.1,2 Of the general population, about 1.5% are asymptomatic nasal carriers of MRSA, and the prevalence among health care workers is about 3 times as high (4.6%).3-6 The anterior nares serve as the main MRSA reservoir, but transient hand carriage and subsequent transmission is possible. Implementation of proper hand hygiene technique is effective in preventing person-to-person transmission of MRSA, and such programs have been associated with reduced prevalence of the infection.8-10 Despite the higher prevalence of the bacteria among health care workers, health care providers are rarely required to undergo screening for MRSA nasal colonization. Studies of the prevalence of MRSA carriage among health care professional students have not tested the feasibility of student screening or its impact on student knowledge and attitudes.11
In 2011, faculty members at the Wegmans School of Pharmacy began training all newly matriculated P1 students to follow the World Health Organization’s 8-step method for hand hygiene using alcohol-based products.11 Students were successful in mastering the skill for hand hygiene and reported greater motivation to perform hand hygiene after training.12
To make students more aware of the likelihood of MRSA exposure within their own classroom, we introduced a new active learning exercise in fall 2012: the MRSA nasal colonization self-screening. The purpose of this study was to determine the feasibility of having students participate in this invasive exercise and to assess the effects on student attitudes toward, knowledge of, and motivation to perform hand hygiene.
DESIGN
Newly matriculated doctor of pharmacy (PharmD) students received hand hygiene instruction within the context of a required 3-credit hour, semester-long lecture course titled Health Care Delivery. Hand hygiene instruction was a natural companion to the other introductory content presented in the course, which spanned what it means to be a health care professional, the various health care professions, health care settings, public health, the Triple Aim (lower cost, better health care quality, and improved patient outcomes), and interdisciplinary, patient-centered care. By providing this instruction at the start of the first semester of the P1 year and following it with MRSA self-screening one month later, we hoped to provide students with a clinical skill that they could use immediately and which, if performed regularly, could protect them throughout their experiential education. This study was reviewed and approved by the school’s Institutional Review Board (IRB).
Approximately one month after the P1 students completed their hand hygiene examination and skills assessment (evaluated using a rubric), we introduced the MRSA self-screening exercise during class. The flora sampling and reporting of MRSA nasal colonization incidence were designed to actively engage students in inquiry, reinforcing their interest and helping them make connections to hand hygiene. Thus, pedagogical components of this exercise (ie, teaching technique, providing evidence to support its importance) engaged students in an investigation that underscored the importance of hand hygiene.
Two faculty members from the biology department began the class by briefly reviewing MRSA microbiology and the history of contagion. This introduction consisted of a review of the importance of hand hygiene based on an 18th century case and a condensed tutorial on MRSA microbiology. Historical information regarding the history of hand washing and data demonstrating how hand washing improved mortality rates in clinical settings were presented to capture the students’ interest. The course instructor then reviewed the prevalence of health care-associated and community-acquired MRSA and introduced the exercise as a way to better understand the flora present in the classroom. At our institution, P1 students remain in the same classroom through the school year with instructors circulating through the room. Therefore, the flora of the classroom may more closely resemble that of the P1 students than classrooms in which many different students spend considerably less time.
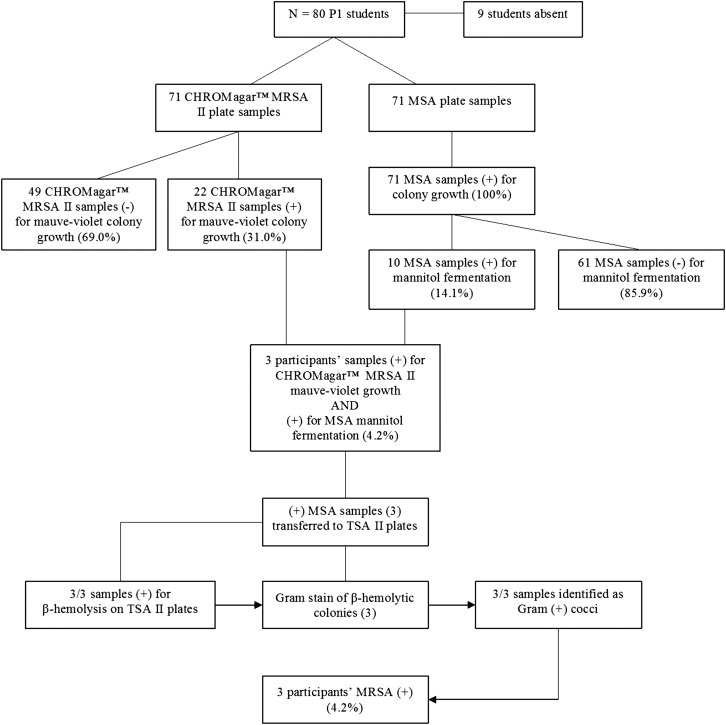
Techniques to properly gather anterior nasal specimens using a sterile, calcium alginate swab moistened with sterile saline were then described and demonstrated by the biology faculty member and course instructor, who collected their own samples in front of the class. The faculty members drew a specimen from each naris and transferred the first sample to a BBL CHROMagar MRSA II screening agar plate (Becton, Dickinson and Company, Sparks, MD), and the second sample to a mannitol salt agar (Becton, Dickinson and Company, Sparks, MD) plate. Plates were marked with a unique 6-digit identification number, which each participant was to record and retain to ensure anonymity. No personal or other identifying information was attached to the plates. Faculty members then distributed sample collection supplies to each student and instructed the class to self-collect specimens. The supplies were acquired by the Department of Biology for $15.44 per person. The introduction, demonstration, and student sampling took about 20 minutes. Immediately following specimen collection, plates were transferred to the laboratory and incubated according to manufacturer specifications for the recommended 24-hour time period at 37°C. After 24 hours, plates were evaluated for growth. Any CHROMagar MRSA II plates that had colony growth as indicated by a mauve-violet color were identified as preliminary positive results suggestive of MRSA presence. Any MSA plates that demonstrated a color change from baseline pink to bright yellow, which is indicative of a Staphylococcus species capable of fermenting mannitol, were identified as positive for pathogenic Staphylococcus growth. Each set of positive results was cross-referenced according to the unique 6-digit identifier on the plates. If a participant’s samples corresponded to positive results on both CHROMagar MRSA II and mannitol salt agar plates, further testing was performed. First, an isolated colony from the mannitol salt agar plate was extracted and placed on a BBL Trypticase Soy Agar with 5% Sheep Blood (TSA II; Becton, Dickinson and Company, Sparks, MD) plate according to manufacturer recommendations for a 24-hour incubation period at 37°C. Additionally, colony growth on TSA II plates exhibiting beta hemolysis after incubation was sampled for Gram staining. Results of the specimen plating exercise are represented in Figure 1.
Figure 1.
Schematic representation of the self-screening process and data collection and analysis protocols.
Approximately 2 weeks later, culture results (identified only by 6-digit plate numbers) were posted to Blackboard where students could view their results and those of the rest of the class. Although MRSA nasal colonization is not considered a condition requiring treatment, we recommended that students with a positive result see their health care provider or visit the campus wellness center. Health care providers have the option of repeating the test and treating any colonization with a regimen of mupirocin lotion applied topically by prescription, for example. During the next class period, we calculated the prevalence of MRSA nasal colonization in the class and compared it to the prevalence among the general population and among health care providers.
Two weeks after completing the screening exercise, after the MRSA screening results were shared with the class, students were asked to complete an anonymous survey during class to assess their knowledge, attitudes, and motivation regarding hand hygiene before and after completing the MRSA instruction. To measure incremental improvement in motivation and attitudes to perform hand hygiene after the MRSA exercise, many of the same survey items that we had used earlier in the semester to assess student knowledge of hand hygiene technique were used on the survey instrument. The survey design was based on our previously published work16,17 It included 17 questions with responses measured on a 4-point Likert scale (1=weak or disagree, 2=fair or somewhat disagree, 3=good or somewhat agree, 4=very good or agree) and each item had a prescreening and postscreening column in which to record their score. Participation in the survey was anonymous and voluntary. Analysis of students’ responses for prescreening vs postscreening was performed using the Wilcoxon signed ranks test. All analyses were conducted in SPSS, version 20, and repeated in STATA, version 10 (College Station, Texas).
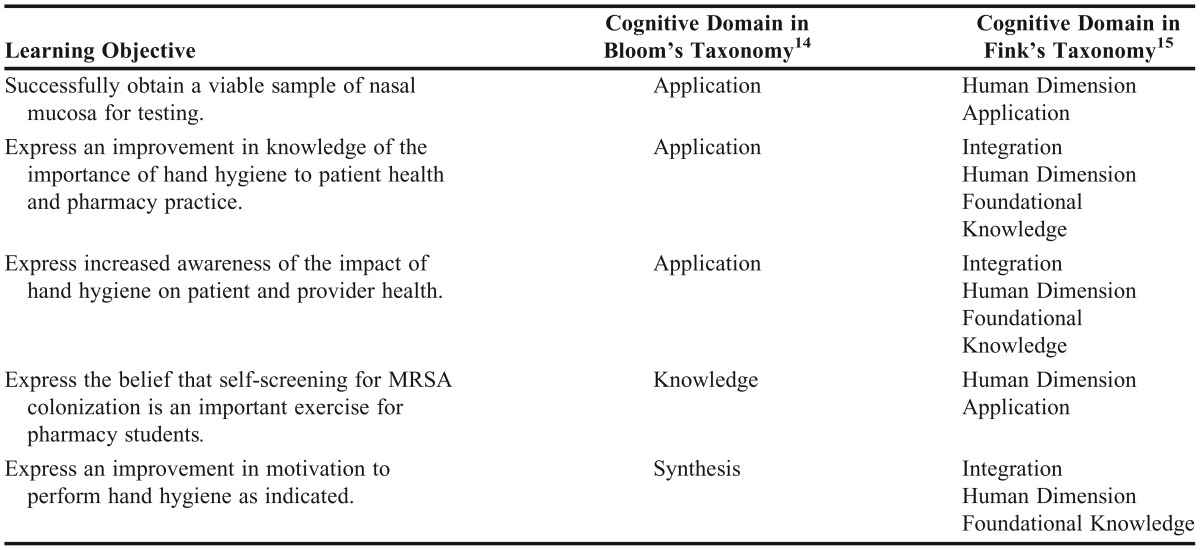
After completing the self-screening, reviewing the results, and calculating and comparing MRSA nasal colonization prevalence, students were expected to be able to meet several learning objectives incorporating the knowledge, application, and synthesis domains of Bloom’s Taxonomy and the human dimension, application, integration, and foundational knowledge domains of Fink’s Taxonomy (Table 1). For example, collection of samples (application skill) allowed for first-hand experience of the nasal specimen collection process and for observation of how the students, their classmates, and instructors reacted to the experience (human dimension [learning about oneself and others]). Through the sharing of anonymous results, students gained foundational knowledge about their personal flora and that of their classmates (human dimension). Students had the opportunity to synthesize information and experience from this and previous hand hygiene curriculum components to further enhance their knowledge and awareness of the importance of hand hygiene, as well as their motivation to perform proper hand hygiene.
Table 1.
Cognitive Domains of Learning Objectives According to Taxonomies of Learning for a Class Exercise on Self-Screening for Methicillin-Resistant Staphylococcus Aureus
EVALUATION AND ASSESSMENT
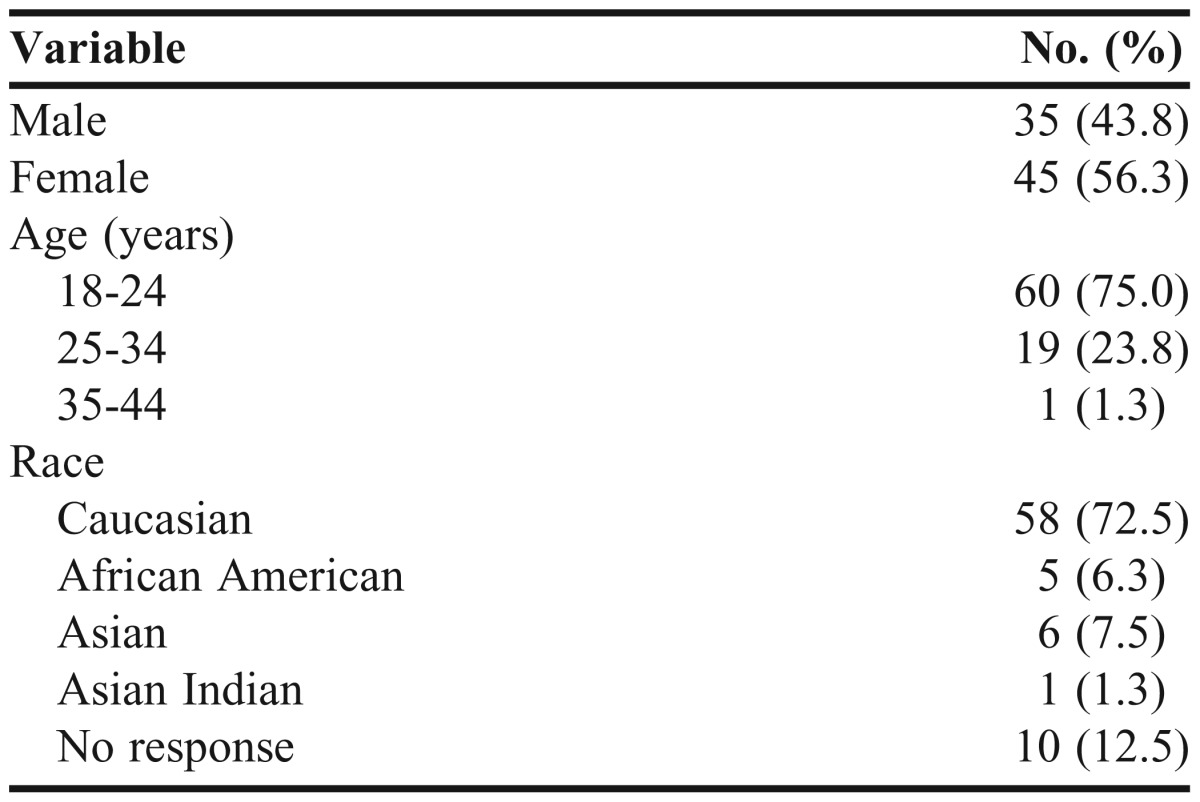
Matriculating P1 students in Fall 2012 were primarily Caucasian and between the ages of 18 and 24 (Table 2). Of the 80 students in the P1 class, 71 were present in class on the day of the self-screening exercise and all participated in the exercise. Of the 71 sets of plates, all samples yielded colony growth. Three (4.2%) plates screened positive for MRSA colonization. The Fisher exact test was used to determine if there was an association between the classroom prevalence and the general population prevalence. The difference between the groups was not significant (2-tailed, p=0.65), suggesting that the newly matriculating P1 class prevalence resembled that of the general population.
Table 2.
Demographics of First-Year Pharmacy Class Who Participated in an Exercise on Self-Screening for Methicillin-Resistant Staphylococcus Aureus (N=80)
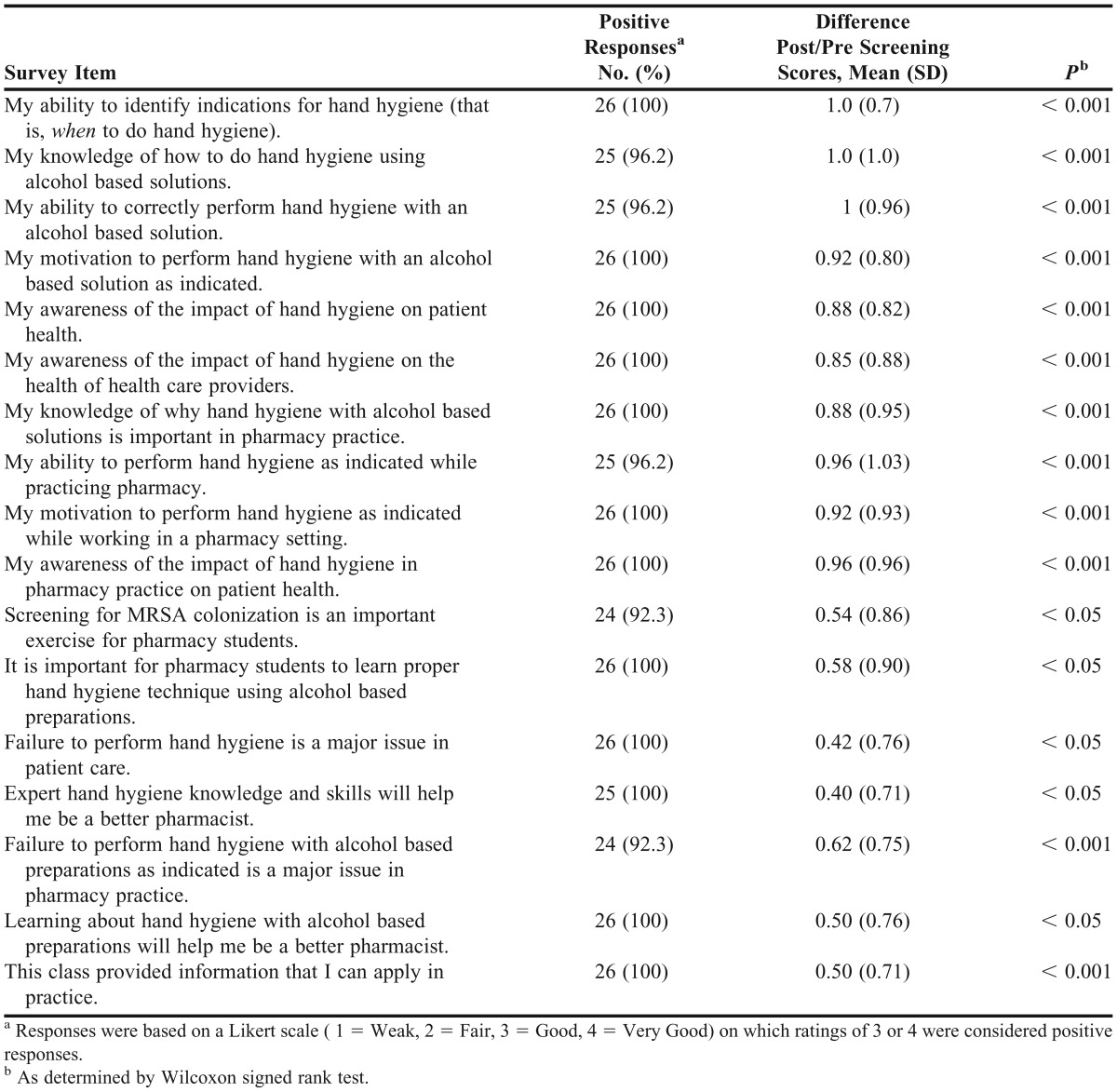
Twenty-six of the 71 students who had completed the exercise completed the survey instrument. Students’ scores on knowledge, awareness, and motivation to perform hand hygiene significantly improved following completion of the MRSA self-screening exercise (Table 3). Notably, 24 (92.3%) students responded positively to the statement: “Screening for MRSA colonization is an important exercise for pharmacy students.” All participants responded positively to the following statements: “Learning about hand hygiene with alcohol-based preparations will help me to be a better pharmacist” and “This class provided information that I can apply in practice.”
Table 3.
First-Year Pharmacy Students’ Responses on a Pre/Post Screening Survey Regarding Hand Hygiene and Health Care Associated Infections after Participating in a Self-screening Exercise to Detect Methicillin-Resistant Staphylococcus Aureus (N=26)
Class performance questions on hand hygiene and health care-associated infections on a written examination (worth 33% of the course grade) was compared to performance of the P1 class in the previous year, which had received the hand hygiene instruction but had not completed the MRSA nasal colonization self-screening exercise. For the test question, “Health care associated infections are a rare cause of death, true or false?” the number of students selecting the correct answer was significantly higher in the class that had completed the MRSA self-screening exercise (98.75% compared to 88.3% of the previous class with p<0.01). (The p-value associated with the chi-square test for a difference in proportions is p<0.01.) Student performance on test items specific to hand hygiene indications and technique were not significantly better than those of the previous class.
DISCUSSION
We assessed 3 broad questions in this study: (1) Is MRSA nasal colonization self-screening feasible and acceptable to students in a required course completed prior to clinical training? (2) Do students express an increased knowledge and awareness of health care-associated infections and the importance of hand hygiene after self-screening than after hand hygiene instruction alone? (3) Was the class performance on test questions related to health care-associated infections and hand hygiene better than that of the previous year’s class, which received the same instructions on hand hygiene technique and indications, but did not participate in the self-screening exercise?
The feasibility of adding the self-screening exercise was determined by the number of students who successfully obtained nasal samples by inserting a cotton swab to the very back of each side of their noses and swiping each swab onto a culture plate, one at a time. We anticipated that some students would feel uncomfortable sticking a swab up their nose, particularly in front of classmates. Others might not have wanted their samples tested and reported, even though samples were anonymous. Nevertheless, all 71 students (100%) present in class completed the exercise and every set of plates returned a viable result. In a relatively full classroom with faculty members participating, it may have been difficult for students to resist participation, particularly at this early stage in their training.
We concluded that self-screening for MRSA nasal colonization was feasible in this class of P1 students. The cultures demonstrated a prevalence of MRSA nasal colonization among the students in the class that was similar to that in the general population, and the pre/post screening survey responses suggested that this exercise resulted in achievement of learning objectives.
A limitation of the study was the relatively low survey response rate. Factors that may have contributed to the low response rate may include lower class attendance on the day the survey was administered and student fatigue. The pre/post screening survey used after the self-screening for MRSA nasal colonization was nearly identical to the pre/post survey students completed at the end of the hand rubbing skills training with alcohol based preparations. The instructor explained the purpose of the second survey, but fatigue, lack of time between classes, and competing demands likely had a negative effect on the response rate.
We expected to see modest improvements in students’ rating of incremental learning after completing the MRSA self-screening exercise but did not. Nevertheless, students reported significant improvements across all parameters, including improvements in their knowledge of hand hygiene even though the MRSA self-screening exercise did not address hand hygiene technique. Students may have assumed that self-screening for MRSA nasal colonization was a component of hand hygiene programs. Alternatively, students may have responded positively overall to the exercise and, therefore, tended to rate all of the survey items positively. Class performance on a test question related to health care-associated infections was significantly better than that of the previous class (which had received the same hand hygiene training but not the self-screening exercise), but scores on test questions related to hand hygiene were not higher than those of the previous class.
SUMMARY
Self-screening for MRSA nasal colonization in a first semester lecture course for P1 students appears to be a feasible method for reinforcing motivation to perform hand hygiene technique as promulgated by the World Health Organization. Future studies should examine the effects of such active learning on student hand hygiene behaviors and on retention of learned practice upon entering the health care workforce.
REFERENCES
- 1.Chambers HF, DeLeo FR. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat Rev Microbiol. 2009;7(9):629–641. doi: 10.1038/nrmicro2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Methicillin-resistant Staphylococcus aureus (MRSA) Infections. Centers for Disease Control and Prevention. http://www.cdc.gov/mrsa/health care/index.html. Accessed February 19, 2014.
- 3.Albrich WC, Harbarth S. Health-care workers: source, vector, or victim of MRSA? Lancet Infect Dis. 2008;8(5):289–301. doi: 10.1016/S1473-3099(08)70097-5. [DOI] [PubMed] [Google Scholar]
- 4.Jernigan J, Kallen A. Methicillin-resistant Staphylococcus aureus (MRSA) infections. Activity C: ELC prevention collaboratives. Division of health care quality promotion. Centers for disease control and prevention. http://www.cdc.gov/HAI/pdfs/toolkits/MRSA_toolkit_white_020910_v2.pdf. Accessed March 1 2013. [Google Scholar]
- 5.Elie-Turenne MC, Fernandes H, Mediavilla JR, et al. Prevalence and characteristics of Staphylococcus aureus colonization among health care professionals in an urban teaching hospital. Infect Control Hosp Epidemiol. 2010;31(6):574–580. doi: 10.1086/652525. [DOI] [PubMed] [Google Scholar]
- 6.Gorwitz RJ, Kruszon-Moran D, McAllister SK, et al. Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001-2004. J Infect Dis. 2008;197(9):1226–1234. doi: 10.1086/533494. [DOI] [PubMed] [Google Scholar]
- 7.Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet. 2000;356(9238):1307–1312. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]
- 8.Grayson ML, Russo PL, Cruickshank M, et al. Outcomes from the first 2 years of the Australian National Hand Hygiene Initiative. Med J Aust. 2011;195(10):615–619. doi: 10.5694/mja11.10747. [DOI] [PubMed] [Google Scholar]
- 9.Sroka S, Gastmeier P, Meyer E. Impact of alcohol hand-rub use on methicillin-resistant Staphylococcus aureus: an analysis of the literature. J Host Infect. 2010;74(3):204–211. doi: 10.1016/j.jhin.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 10.WHO guidelines on hand hygiene in health care. Geneva: World Health Organization; 2009. http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf. [Google Scholar]
- 11.Rohde RE, Rowder C, Patterson T, Redwine G, Vasquez B, Carranco E. Methicillin resistant Staphylococcus aureus (MRSA): an interim report of carriage and conversion rates in nursing students. Clin Lab Sci. 2012;25(2):94–101. [PubMed] [Google Scholar]
- 12.Lavigne JE. Paris: France; Schwartzmeyer C. Implementing World Health Organization standards for hand hygiene indications and methods using alcohol-based preparations at the Wegmans School of Pharmacy. International Forum on Quality & Safety in Health care. April, 2012. http://fisherpub.sjfc.edu/cgi/viewcontent.cgi?article=1015&context=pharmacy_facpub&sei-redir=1&referer=http%3A%2F%2Fwww.bing.com%2Fsearch%3Fq%3Dlavigne%2Bhand%2Bhygiene%2B2012%26qs%3Dn%26form%3DQBRE%26pq%3Dlavigne%2Bhand%2Bhygiene%2B2012%26sc%3D0-21%26sp%3D-1%26sk%3D%26cvid%3Defee68187d3d42869ac6fb3cf09a78d2#search=%22lavigne%20hand%20hygiene%202012%22. [Google Scholar]
- 13.Paule SM, Mehta M, Hacek DM, et al. Chromogenic media vs real-time PCR for nasal surveillance of methicillin-resistant Staphylococcus aureus: impact on detection of MRSA-positive persons. Am J Clin Pathol. 2009;131(4):532–539. doi: 10.1309/AJCP18ONZUTDUGAQ. [DOI] [PubMed] [Google Scholar]
- 14.Bloom BS, editor. Taxonomy of Educational Objectives. The Classification of Educational Goals. Handbook I: Cognitive Domain. New York, NY: McKay; 1956. [Google Scholar]
- 15.Fink LD. Creating Significant Learning Experiences. An Integrated Approach to Designing College Courses. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]
- 16.Gilligan AM, Myers J, Nash JD, et al. Educating pharmacy students to improve quality (EPIQ) in colleges and schools of pharmacy. Am J Pharm Educ. 2012;76(6):Article 109. doi: 10.5688/ajpe766109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lavigne J. Implementing “Educating Pharmacy Students and Pharmacists to Improve Quality” (EPIC) as a requirement at the Wegmans School of Pharmacy. Curr Pharm Teach Learn. 2012;4(3):212–216. [Google Scholar]