Abstract
Critical thinking, while highly valued as an ability of health care providers, remains a skill that many educators find difficult to teach. This review provides an analysis examining why current methods of teaching critical thinking to health care students (primarily medical and pharmacy students) often fail and describes a premise and potential utility of the Socratic method as a tool to teach critical thinking in health care education.
Keywords: critical thinking, Socratic method, pharmacy education
INTRODUCTION
As a result of increasing pressure from accrediting bodies and an evolving technical landscape, health care colleges and schools continue to place increasing emphasis on critical thinking skills rather than provision of facts and rote memorization.1,2 Additionally, the incorporation of competency-based education requires that students develop a deeper understanding of course material, which in turn necessitates new modes of content delivery and incorporation of new thought processes. A number of varying modalities intended to instill critical thinking have been attempted; however, in most cases these attempts have been reported to be only partially effective and often inconsistent in yielding positive results. This review will discuss the value of critical thinking among health care professionals and will re-visit the use of the Socratic method or Socratic questioning as a tool for modeling critical thinking.
CRITICAL THINKING
Numerous definitions of critical thinking have been described and reviewed elsewhere,3 but the concept is understood to have originated through the teachings of the classic Athenian philosopher Socrates (469-399 BCE). Often regarded as a founder of Western philosophy, Socrates observed that his students often lost their ability to justify their own preconceived thoughts and beliefs after a series of specific, targeted questions.4 Conversely, through appropriate and repeated questioning, Socrates observed that these same students eventually developed self-generated knowledge and the ability to regulate their own thoughts. The Art of Socratic Questioning describes 3 types of questions that, when used strategically by the questioner, can aid students in regulating their own thoughts. These questions are categorized as those of procedure, preference, and judgment.5 Questions of procedure are defined as those with correct answers, such as “Which of the following medications is a beta-blocker?” Alternatively, questions of preference are those with no correct answers, such as “How do you prefer to conduct patient counseling?” It is in the third type of question, however, where the Socratic definition of critical thinking can be found, as these types of questions are those with “best” answers, such as, “What is the most appropriate antibiotic for this patient?” Therefore, critical thinking within a Socratic paradigm might be described as the application and analysis of information requiring clarity, logical consistency, and self-regulation.
The ability to think critically is not only expected by employers but also almost unilaterally prescribed by accrediting bodies.6 The provision of high level care by pharmacists across all health care disciplines inherently requires the ability to think critically. As technology continues to make rote knowledge rapidly searchable, discoverable, and transferrable, the ability to think critically continues to gain importance. Tyreman states that all knowledge of suffering people is derived from two sources: previously treated patients with a similar disease course or changing medical knowledge.7 Therefore, the ability to relate current patient events to previous ones, while appreciating the innate limitations of this practice, is paramount to thinking critically.
In the clinical setting, the ability to think critically requires both an understanding of the “deep structure” of a question and the ability of the practitioner to relate that structure to similar experiences from his or her past.8 This “deep structure” refers to the question within the question (as opposed to its surface structure, which refers to the direct question at hand). For example, in a word problem using multiplication of rows and columns to count the number of vegetables in a garden, the deep structure relates to mathematics whereas the surface structure relates to farming, the latter of which is irrelevant to the problem’s solution. Chen et al. examined this construct in a 2004 study that evaluated 90 college students’ (60 American students’ and 30 Chinese students’) ability to propose a correct solution to each of two problems.9 The first problem was very similar to the story of Hansel and Gretel, where the correct solution related to leaving a trail of items to avoid getting lost; the second was very similar to a common Chinese tale called “Weigh the Elephant,” where the correct solution related to using water displacement to weigh an object too large for a scale. Nearly 80% of the American students answered the Hansel and Gretel question correctly compared to 25% of Chinese students (p<0.05); for the elephant question, success rates were flipped, with 69% of Chinese students answering correctly compared to 8% of American students (p<0.05). The disparity in correct responses suggests that ability to recognize and understand a question’s deep structure is paramount to the ability to think critically and apply previously-learned information to new situations. This, in concert with the statements by Tyreman,7 suggests that appropriate patient care requires the ability to critically analyze and apply information from previous patient cases and the available, albeit constantly changing, medical knowledge base.
An ability to think critically is also considered a foundational step in the development of expertise in a given content area or specialty. In his review, Tyreman analogizes being an expert versus a trainee to driving a car versus driving a motorcycle.7 Despite being able to appropriately drive a car, the ability to drive a motorcycle is not innate; he concludes that an expert is one who is, as compared to a novice, who is one who (merely) does. He subsequently elaborates saying an expert can apply himself “across a range of familiar and unfamiliar situations” and assess the context of a problem. Without the ability to recognize the deep structure of a question and apply it to previous scenarios, it is unreasonable to believe practitioners will be able to develop the skills necessary to ‘think like an expert.’
A common assumption is that health care ‘experts’ are inherently able to think more critically than their novice counterparts. Although the research presented below refutes this premise, the importance of critical thinking as an elemental skill of practitioners remains. In a 2004 study, Miller evaluated the ability of 66 pharmacy students to critically evaluate literature as an assessment of their ability to ‘think like experts.’10 Students were given three distinct trial summaries (one “well-designed” experimental study, one “well-done” case-control study, and one “poorly-designed” experimental study). All 3 research papers evaluated the ability of beta-carotene to prevent cervical cancer, and each produced negative results. Students were asked to use a visual analog scale to rate their confidence from 0 to 100 in the ability of beta-carotene to prevent cervical cancer both at baseline and after reading each study in random order. The authors then calculated student “likelihood ratios” (ie, the odds of believing vs not believing after reading each study divided by the same odds before reading any study), which were then compared to those of experts given the same task. The author found likelihood ratios more strongly correlated with level of evidence in the expert group than the student group, suggesting students were not able to critically evaluate literature as efficiently. The study found no correlations between scores on the California Critical Thinking Skills Test (CCTST) and students’ abilities to “think like experts.” There was, however, a correlation between CCTST scores and students’ final grades in the broader literature evaluation course within which the trial was conducted (r=0.45, p<0.001). This suggests that thinking like an expert is not akin to thinking critically, despite the intuitive assumption that the systematic approach to literature evaluation and critical thinking require thought regulation. Encouragingly, it appears health care courses and course examinations can be designed to test critical thinking.
This study had a number of limitations. First, the authors did not report CCTST scores at baseline, which subsequently does not allow for an a priori assessment of the course’s ability to teach critical thinking. Second, CCTST scores were collected as part of a separate study and correlated with examinations in the course; this might suggest that the course was not designed to teach critical thinking. Third, the authors note that students may have purposely placed little weight on each of the three studies based on what they thought the course instructor expected on the final examination, which may explain a lack of correlation between CCTST scores and likelihood ratios. Finally, experts were not given the CCTST examination for comparison. Although this study did not support a correlation between critical thinking and literature evaluation, the aforementioned limitations decrease the validity of this conclusion. Further the application of information, as previously reviewed, likely requires higher-level critical thinking skills. To the knowledge of the authors, this has not been formally evaluated in pharmacy education.
The challenges involved with teaching critical thinking are not new. Since as early as the 1950s, education has faced the issue of teaching critical thinking to students, and, with few exceptions, educators have failed to consistently document successes.11 Three key principles underlying critical thinking have been described for educators tasked with motivating students towards better thinking.8 First, critical thinking is not simply a skill that can be learned. Second, critical thinking is more likely in those learners with certain metacognitive strategies in place (eg, the forethought to consistently look for the deep structure in a question). Finally, the ability to think critically relies to some extent on domain knowledge and practice. In other words, one must not only recognize the deep structure of a question, but also be able to relate it to prior experiences. It therefore follows that one cannot think critically about an issue in which they have no point of reference.
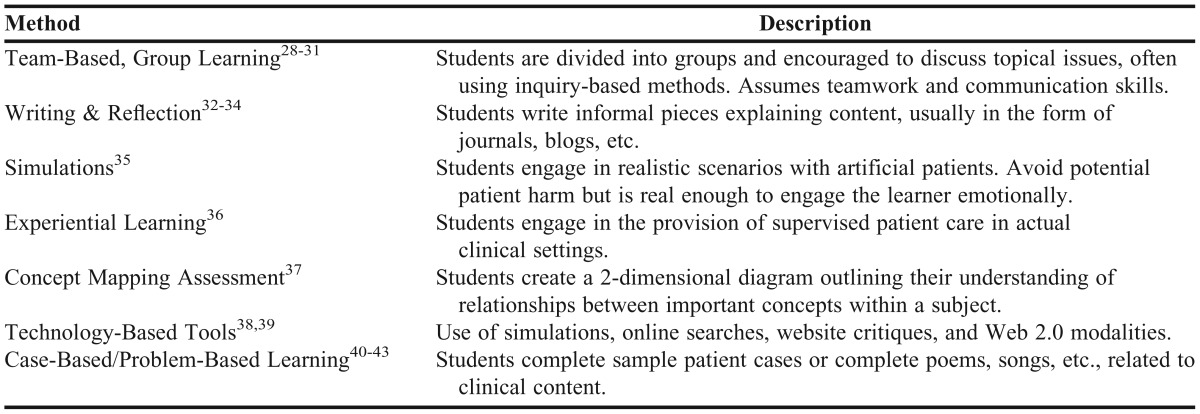
Despite the noted difficulty in teaching critical thinking, a number of methods have been proposed to aid educators charged with teaching critical thinking to student health care professionals. Among other methods, these variations can include group learning, problem-based learning, case-based learning, writing and reflection, concept mapping, and experiential education (Table 1). A complete discussion of these methods is beyond the scope of this paper as other authors have previously compiled comprehensive reviews in this regard.3 It should be noted, however, that few of the aforementioned methods focus on metacognition.
Table 1.
Examples of Activities Used to Encourage Critical Thinking
Unfortunately, many studies evaluating the ability to teach critical thinking have failed to produce overwhelmingly positive, reproducible results. In an effort to measure critical thinking skills throughout a curriculum, Miller evaluated CCTST and California Critical Thinking Dispositions Inventory (CCTDI) scores annually for 5 cohorts of pharmacy students at North Dakota State University. At the conclusion of data collection, information from each year was available for the first 2 cohorts (graduating classes of 1997 and 1998, n=60 students each).12 The study found a statistically significant increase in mean CCTST scores from professional year 1 through professional year 4 for each group (20.35 vs 18.15 for cohort 1, p=0.006; 21.71 vs 18.26 for cohort 2, p<0.001). However, it should also be noted that motivation to think critically, as assessed by the CCTDI decreased in both cohorts over the 4-year periods (mean composite score 307.7 vs. 303.8 for cohort 1, p=0.41; 305.8 vs. 300.4 for cohort 2, p=0.21), suggesting a decrease in inquisitiveness of pharmacy students as they progressed through the curriculum. Unfortunately, the author did not comment on specific attributes of the curriculum that could have caused the improvement in scores. Further, there was no comparison group, preventing analysis of whether changes in CCTST scores were attributable to the pharmacy curriculum or simply general maturation throughout matriculation. The authors also made note that students’ motivation to do well may have impacted results.
In another study conducted at Campbell University School of Pharmacy, Cisneros found no significant differences between critical thinking ability, as measured by the CCTST, both at the beginning and end of each professional year within a doctor of pharmacy degree program.13 Although the study was not designed to detect differences between classes, mean CCTST composite scores were not different between first and fourth professional year students (20.0 vs. 20.4, p=0.79), suggesting overall critical thinking ability did not change throughout the pharmacy curriculum. The authors mention the contribution of a possible “ceiling effect,” stating that the overall high scores at baseline seen in pharmacy students limited the possible increase in critical thinking ability as assessed by the CCTST. Other potential reasons for discrepancies between this study and others reporting improvement in thinking scores include a small sample size, unfamiliarity with this type of research at the institution, and limited follow-up.
Tiwari and colleagues compared problem-based learning (PBL) to traditional lectures in regard to their respective abilities to stimulate critical thinking in a cohort of 79 first-year undergraduate nursing students.14 Despite similar baseline mean composite scores on the CCTDI exam, these scores after 2 semesters were significantly higher in students enrolled in PBL-based courses as compared to traditional lectures (276.3 vs 263.1, p=0.02). Interestingly, the effect was not durable 2 years after completion of the course, as CCTDI scores were similar (271.4 vs. 262.2, p=0.11). This implies a continued need for reinforcement of critical thinking principles (or adoption of more durable techniques). The data presented was limited in that the CCTDI is a measure of disposition to think critically and is intended for use with the CCTST as a comprehensive measure of critical thinking skills.
Introduction to the Socratic Method and Socratic Questioning
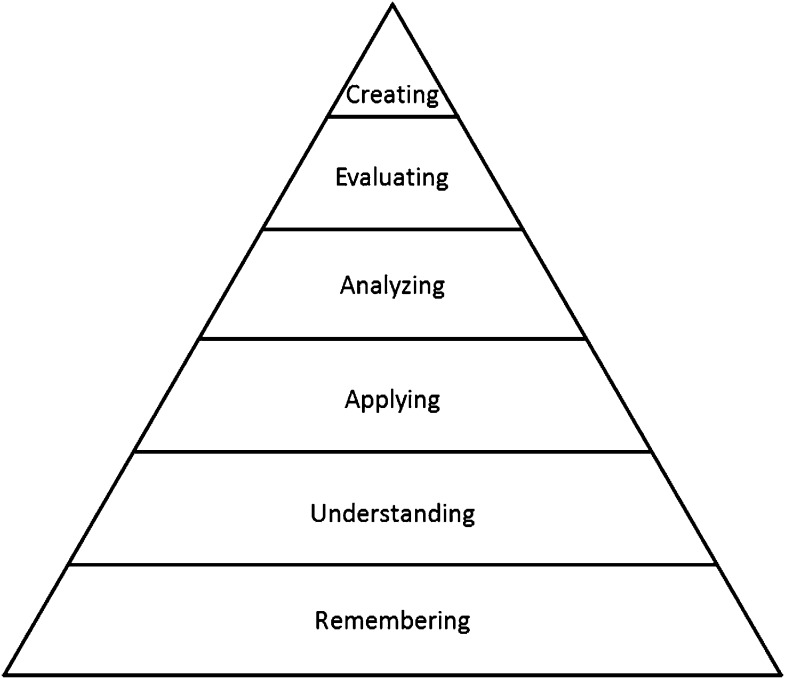
Given the shortcomings associated with many educational techniques aimed at instructing critical thinking and being cognizant that individual students may respond to differing approaches in varied manners, durable and reproducible means of motivating students to think critically are continually needed. The Socratic method is particularly intriguing as a means of motivation given its attention to deep structure and instillation of an inquisitive tendency. Critiqued by some and vigorously defended by others, the Socratic method is a time-tested means of teaching critical thinking to law students throughout the United States.15 Given the importance of critical thinking in the legal profession, the use of the Socratic method in health care education appears both logical and sound. As it focuses on higher orders of Bloom’s Taxonomy (Figure 1), it is likely that the Socratic method engages and encourages critical thinking.16 An example of an an abbreviated hypothetical Socratic session is provided in Appendix A.
Figure 1.
Bloom's Taxonomy (author's own rendition)
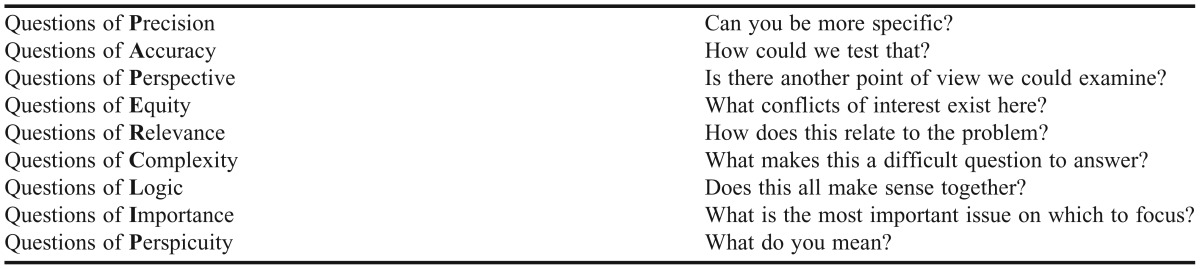
As previously mentioned, Socrates is widely regarded as the father of Western philosophy. Historians have come to appreciate the value he placed on self-generated knowledge, the use of questioning to evaluate others’ knowledge, and the teaching of implanted doubt. Given his predisposition to question, it is important to realize Socrates did not express unthinking skepticism.17 He used strategic, probing questions to evaluate the depth of others’ knowledge, focusing on evoking doubt and a constant tendency to question his students. His tactics’ propensity to stimulate discourse ultimately led to his state-sanctioned execution; however, his legacy lives on in contemporary education as the “Socratic method,” also referred to as “Socratic questioning.” The elements and hallmarks of Socratic questioning are outlined in Table 2. Through purposeful questioning aimed at these elements, it has been suggested that educators can more effectively invoke critical thinking in students.5 Critical thinking and Socratic questioning are intertwined in that critical thinking involves metacognition and regulation of one’s own thoughts, while Socratic questioning can be used as a tool to regulate one’s thoughts in the pursuit of true understanding. Examples of Socratic questions using the acronym “PAPER CLIP” can be found in Table 3.
Table 2.
Key Aspects of Socratic Questioning5
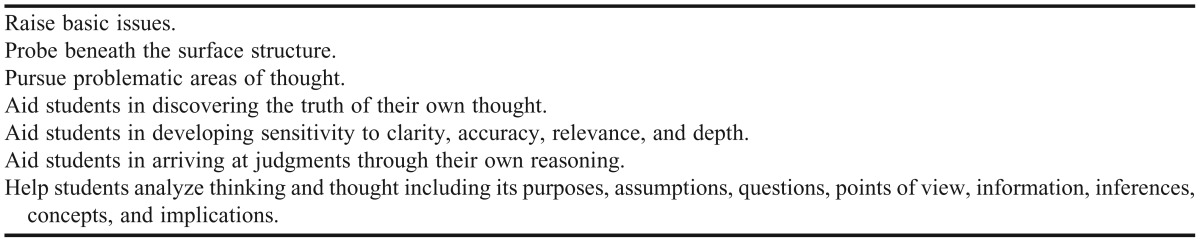
Table 3.
Types of Socratic Questions (PAPER CLIP)
Unlike Socrates who placed value in self-generated knowledge, the Eastern philosopher Confucius (551-479 BCE) valued effortful, pragmatic, respectful learning from those more experienced in a field.17 Similar to many traditional means of teaching (eg, didactic lectures), Confucian learning focuses on the purposeful acquisition of facts, rather than true knowledge and understanding. Socrates, however believed true knowledge was found only in the self and could not be translated by authority figures; in fact, he often considered himself ignorant, stating he could not be held accountable for his students’ beliefs because he never taught them anything.18 The ability to support opinions with facts, akin to evidence-based medicine, is heralded as the ultimate goal of Socratic questioning. However, it is important to note that just as students cannot be expected to critically analyze an issue without appropriate domain knowledge, the appropriate use of the Socratic method requires a foundational knowledge base, which may be acquired through Confucian methods. Therefore while these methods are fundamentally different, they are not mutually exclusive, and may be synergistic in developing competent practitioners.
Use of the Socratic Method in Health Care Education
Perhaps one of the most broad and well known methods of Socratic questioning is the practice of “pimping.” According to Brancati, pimping occurs when an attending physician or authority figure poses a series of very difficult questions to a student, intern, or other trainee.19 He goes on to state that, on the surface, the aim of pimping appears to be Socratic questioning; however, in its truest form, pimping often does not promote critical thinking. It may not inspire inquisitiveness in learners, and its motives are often largely political, reinforcing establishment of a “medical hierarchy,” which is much more consistent with Confucian philosophy. Given Socrates’ self-proclaimed ignorance, pimping is almost certainly not Socratic questioning. This is not to say pimping, as previously defined, has no role in the training of students in the health professions. The potential values of pimping, from the student, resident, and attending perspectives have been well-reviewed.19-21
While the effectiveness of Socratic questioning has not been formally evaluated, there are a number of reviews describing its merits in health care education. Oh described the value of Socratic teaching in a family medicine practice, with a specific focus on the need for the clinician to avoid rigidity of thought and respectfully question the “truths” of medicine.22 He goes on to discuss the importance of a safe learning environment in adult education, reinforcing the benefits of one-on-one teaching and avoidance of humiliation.
Not only does the Socratic method offer a theoretical advantage over didactic lectures, it may also be well-received by students. In a 2011 study, Zou et al. surveyed 74 upper-level medical students regarding their preferences for learning radiology.23 The students were invited to attend a 90-minute radiology conference. During the conference, the leader interchangeably taught using both didactic and Socratic methods. At the completion of the conference, students were given a voluntary 7-item survey assessing their preferences for learning. Of the 30 respondents who completed the survey (30% of the students who took the course), the vast majority indicated they preferred to learn using the Socratic method as opposed to the didactic approach (93.3 vs 6.7%, p<0.001). The authors did not hypothesize why students preferred to learn using the Socratic method, but an overall preference was found for active learning strategies, as they are generally regarded as more engaging.
Practical Considerations for Using the Socratic Method
The most concerning limitation of the Socratic method is the potential for educators to pose questions without purpose. As Rohrich highlighted, simply generating a list of questions is easy;24 however, Socratic questioning is targeted and directed with a beginning, middle, and end. Students should feel a sense of closure and resolution at the completion of an educational experience. Subsequently, effective Socratic questioning takes time, effort, and practice and ultimately may be more difficult for the educator than the student.
In a recent review, Tofade et al. provided “best-practice” strategies for effective questioning in pharmacy education.25 The authors described a number of practical considerations including clarity, safety, sequencing, and wait time and suggested that questions should be simple with limited action verbs to decrease the possibility for confusion. As previously mentioned, Socratic questioning is optimally performed in a safe environment, allowing the learner to say “I don’t know” without fear of consequence. Further, questions should be deliberately sequenced and balanced to avoid bombardment and allow for appropriate resolution. Finally, the “wait time” (ie, the amount of time between the end of a question and a subsequent response, either by the teacher or student) must be long enough to allow students to process information and formulate a response. Depending on the complexity of the question, wait times of less than 20 seconds or up to 1-2 minutes have been suggested.26,27
Given Socrates’ tendency to engage students “one-on-one,” use of the Socratic method in large groups such as full classrooms is a logical concern and potential limitation. Instruction using the Socratic method is recognized to be a more arduous task than typical traditional didactic teaching. An example use of the Socratic method with a group of students has previously been published.22 Even in instances when the Socratic method is employed, traditional lectures or other educational means may be required at least in part so that students may develop requisite domain knowledge. In the absence of sufficient domain knowledge, students may not be able to adequately process and answer Socratic questions,8 therefore the Socratic method may be difficult to implement as a stand-alone method of education.
A final limitation regarding the use of Socratic questioning is a lack of evidence-based research related to the use of this method within and across formal educational programs both inside and outside health care. Perhaps the greatest potential for the Socratic method may be its use within experiential settings; however, this too has yet to be validated in prospective, well-designed studies. Before the Socratic method can be widely accepted in pharmacy education, adequate research must be conducted. Initially, this research should focus on using validated measures of critical thinking (eg, the CCTST and CCTDI) to at least evaluate the validity of the Socratic method as a teaching tool in either didactic and/or experiential settings. If validated, subsequent research should then focus on delivery, training, and optimization of Socratic approaches, specifically in large groups such as classrooms.
Conclusions
While further research is needed to evaluate the ability of various modalities to effectively teach and test critical thinking in health care education, the Socratic method, if used appropriately, is an attractive “lost art” among the teacher’s instructional supplies. However, it is by no means stand-alone, as learners likely require foundational knowledge to be able to critically evaluate clinical concepts. For this reason, the Socratic method is likely more useful if incorporated later in a pharmacy curriculum. Given Socrates’ predilection for individual teaching, practice experience represents a natural place to incorporate the Socratic method in pharmacy education. However, introduction of the Socratic method into classroom settings may allow educators to instill the ability to recognize the deep structure of questions and begin the critical thinking process prior to practice experience. As Socrates described, understanding the fact of one’s ignorance perhaps holds the key to regulating thought, persevering in the pursuit of knowledge, and, ultimately, enhancing practice.
Appendix A
Abbreviated Example of Socratic Process and Questioning in the Classroom
-
Basic Tenants:
- The professor is not an antagonistic opponent in the learning experience nor is he or she an intentional “devil’s advocate.”
- The professor is an active participant in a dialogue and must be willing and open to learning from the pupil.
- The professor does not seek deference to his or her inherent authority but rather creates a culture of mutual respect.
- The professor does not seek to intimidate but rather to create intellectual discomfort when one’s beliefs do not withstand scrutiny.
Instructional Topic:
Clinical Toxicology and Lethal Injection
-
Objectives:
- Define lethal injection.
- Discuss the pros and cons of lethal injection as a means of execution.
- Discuss ethical issues surrounding the use of medications as a means of execution.
- Describe the mechanism of action of agents used as components of lethal injection.
Dialogue
Professor: What is lethal injection?
Pupil: Capital punishment using drugs.
Professor: Is lethal injection the only means of state-sanctioned execution in the US?
Pupil: No, some states still use the electric chair but most states now use lethal injection.
Professor: Why?
Pupil: It seems like most people think that lethal injection is easier on the prisoner or less cruel.
Professor: Do you think this is true?
Pupil: I’m not sure; it seems like it would be less harsh then being electrocuted or hung.
Professor: What drugs are used to perform lethal injection?
Pupil: Every state is different, but it seems like a combination of drugs is most common.
Professor: That seems odd, why does every state use a different set of drugs?
Pupil: Well no one really regulates what the prison system does and what drugs they can use.
Professor: Are medical professionals involved in the design or selection of these drugs/protocols?
Pupil: I’m not sure; seems like there may be ethical implications.
Professor: What do you mean?
Pupil: I am not sure what the code of ethics for various health professions says about lethal injection.
Professor: Do you think pharmacists should play a role in the development of lethal injection protocols?
Pupil: I am not sure. I will have to give it some thought and look at the code of ethics.
Professor: Do you think pharmacists should be involved in the compounding or administration of these agents to the condemned?
Pupil: I think it might be okay for a pharmacist to prepare a medication but not actually administer it.
Professor: What is the difference between compounding the medication and administering it?
Pupil: Well the pharmacist hasn’t actually “killed” the patient in so much as they prepared the drug but did not administer it.
Professor: Would the person administering the medication be able to do so if it were not properly prepared by the pharmacist?
Pupil: I’m not sure. I guess not.
Professor: What types of drugs are usually employed in lethal injection?
Pupil: Usually 3 drugs: a sedative, a paralyzing agent, and potassium.
Professor: Why are these 3 types of drugs used?
Pupil: Well it kind of makes sense in that the sedative will render the prisoner unconscious so they will not know what’s going on while the paralyzer will stop breathing and the potassium stops the heart.
Professor: Why would the government want the prisoner to be unconscious?
Pupil: I think this helps the whole concept of lethal injection be plausible in terms of not being cruel and unusual.
Professor: Why is it unacceptable for lethal injection or execution to be cruel and unusual?
Pupil: If it were deemed to be cruel and unusual then it would be unconstitutional.
Professor: So the fact that the prisoner is unconscious makes lethal injection acceptable?
Pupil: Well the fact that they are unaware and not in pain seems to make it acceptable.
Professor: How do we know the prisoner is unconscious and/or not in pain?
Pupil: I guess we really don’t know. I guess it’s assumed.
Professor: Why would we assume that the prisoner is unconscious?
Pupil: I guess because his eyes are closed after the sedative is administered and based on the doses they use.
Professor: What doses of sedatives are used?
Pupil: I don’t know. I don’t think most states let you know.
Professor: Then how can we be sure the prisoner is unconscious?
Pupil: I guess we can’t – we can only assume.
Professor: What would happen if the patient were not adequately sedated?
Pupil: Well the paralytic would stop them from breathing and the potassium would cause the heart to go into asystole.
Professor: Would they be aware that this was happening?
Pupil: If they were not sedated, yes.
Professor: Could they express their discomfort or tell officials what was happening?
Pupil: I don’t think so.
Professor: Why not?
Pupil: Because they would be paralyzed.
Professor: Could they feel pain?
Pupil: I am not sure.
Professor: How do paralytics work?
Pupil: They work by stopping skeletal muscle movement.
Professor: Right. So does that cause analgesia?
Pupil: No. So why don’t they give pain medications?
Professor: Should they give pain medications?
Pupil: Well, it’s a punishment, so I guess not. But at the same time, it still seems cruel.
Professor: More cruel than other methods?
Pupil: I suppose not.
Professor: Well that gets into another discussion altogether.
REFERENCES
- 1.Functions and structure of a medical school: standards for accreditation of medical education programs leading to the MD degree. Vol ED-62013:8. Washington, DC: Liaison Committee on Medical Education; 2013. http://www.lcme.org/publications/functions.pdf.
- 2.Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Vol 11.2. Chicago, IL: Accreditation Council for Pharmacy Education; 2006. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf.
- 3.Oderda GM, Zavod RM, Carter JT, et al. An environmental scan on the status of critical thinking and problem solving skills in colleges/schools of pharmacy: report of the 2009-2010 academic affairs standing committee. Am J Pharm Educ. 2010;74(10) doi: 10.5688/aj7410s6. Article S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.A brief history of the idea of critical thinking. The Critical Thinking Community; http://www.criticalthinking.org/pages/a-brief-history-of-the-idea-of-critical-thinking/408. Accessed September 19, 2013.
- 5.Paul R, Elder L. The Art of Socratic Questioning. Dilton Beach, CA: The Foundation for Critical Thinking; 2007. [Google Scholar]
- 6.Hart Research Associates, on behalf of the Association of American Colleges and Universities. It takes more than a major: employer priorities for college learning and student success. Liberal Education. 2013;99(2) [Google Scholar]
- 7.Tyreman S. Promoting critical thinking in health care; phronesis and criticality. Med Health Care Philos. 2000;3(2):117–24. doi: 10.1023/a:1009973021449. [DOI] [PubMed] [Google Scholar]
- 8.Willingham DT. Critical thinking: why is it so hard to teach? Arts Education Policy Review. 2008;109(4):21–32. [Google Scholar]
- 9.Chen Z, Mo L, Honomichi R. Having the memory of an elephant: long-term retrieval and the use of analogues in problem solving. J Exp Psychol Gen. 2004;133(3):415–33. doi: 10.1037/0096-3445.133.3.415. [DOI] [PubMed] [Google Scholar]
- 10.Miller DR. An assessment of critical thinking: can pharmacy students evaluate clinical studies like experts? Am J Pharm Educ. 2004;68(1) Article 5. [Google Scholar]
- 11.Provus M. Teaching critical thinking throughout history. The School Review. 1955;63(7):393–6. [Google Scholar]
- 12.Miller DR. Longitudinal assessment of critical thinking in pharmacy students. Am J Pharm Educ. 2004;67(4) doi: 10.5688/aj730466. Article 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cisernos RM. Assessment of critical thinking in pharmacy students. Am J Pharm Educ. 2009;73(4) doi: 10.5688/aj730466. Article 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tiwari A, Lai P, So M, Yuen K. A comparison of the effects of problem-based learning and lecturing on the development of students’ critical thinking. Med Educ. 2006;40(6):547–54. doi: 10.1111/j.1365-2929.2006.02481.x. [DOI] [PubMed] [Google Scholar]
- 15.Garrett E. Becoming lawyers: the role of the Socratic Method in modern law schools. The Green Bag. 1998;2D:199–208. [Google Scholar]
- 16.Forehand M. Bloom’s taxonomy. Orey M, editor. Emerging Perspectives on Learning, Teaching, and Technology. 2005 [Google Scholar]
- 17.Tweed RG, Lehman DR. Learning considered within a cultural context: Confucian and Socratic approaches. Am Psycholt. 2002;57(2):89–99. doi: 10.1037//0003-066x.57.2.89. [DOI] [PubMed] [Google Scholar]
- 18.Plato . The Apology. New York, NY: P.F. Collier & Son; 2001. [Google Scholar]
- 19.Brancati FL. The art of pimping. JAMA: The Journal of the American Medical Association. 1989;262(1):89–90. [PubMed] [Google Scholar]
- 20.Wear D, Kokinova M, Keck-McNulty C, Aultman J. Pimping: perspectives of 4th year medical students. Teach Learn Med. 2005;17(2):184–91. doi: 10.1207/s15328015tlm1702_14. [DOI] [PubMed] [Google Scholar]
- 21.Detsky AS. The art of pimping. JAMA: The Journal of the American Medical Association. 2009;301(13):1379–81. doi: 10.1001/jama.2009.247. [DOI] [PubMed] [Google Scholar]
- 22.Oh R. The Socratic Method in medicine: the labor of delivering medical truths. Fam Med. 2005;37(8):537–9. [PubMed] [Google Scholar]
- 23.Zou L, King A, Soman S, et al. Medical students’ preferences in radiology education: a comparison between the Socratic and didactic methods utilizing PowerPoint features in radiology education. AcadRadiol. 2011;18(2):253–6. doi: 10.1016/j.acra.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 24.Rohrich RJ, Johns DF. The Socratic Method in plastic surgery education: a lost art revisited. Plast Reconstr Surg. 2000;105(5):1803–5. doi: 10.1097/00006534-200004050-00030. [DOI] [PubMed] [Google Scholar]
- 25.Tofade T, Elsner J, Haines S. Best practice strategies for effective use of questions as a teaching tool. Am J Pharm Educ. 2013;77(7) doi: 10.5688/ajpe777155. Article 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rowe M. Wait time: slowing down may be a way of speeding up! Journal of Teacher Education. 1986;37(1):43–50. [Google Scholar]
- 27.Nicholl H, Tracey C. Questioning: a tool in the nurse educator’s kit. Nurse EducPract. 2007;7(5):285–92. doi: 10.1016/j.nepr.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 28.Powers M, Jones-Walker J. An interdisciplinary collaboration to improve critical thinking among pharmacy students. Am J Pharm Educ. 2005;69(4) Article 70. [Google Scholar]
- 29.Earl GL. Using cooperative learning for a drug information assignment. Am J Pharm Educ. 2009;73(7) doi: 10.5688/aj7307132. Article 132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Osftad W, Brunner LJ. Team-based learning in pharmacy education. Am J Pharm Educ. 2013;77(4):Article 70. doi: 10.5688/ajpe77470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sandahl SS. Collaborative testing as a learning strategy in nursing education. Nurse EducPerspect. 2010;31(3):142–7. [PubMed] [Google Scholar]
- 32.Austin Z, Gregory PA, Chiu S. Use of reflection-in-action and self-assessment to promote critical thinking among pharmacy students. Am J Pharm Educ. 2008;72(3) doi: 10.5688/aj720348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hobson EH, Schafermeyer KW. Writing and critical thinking: writing-to-learn in large classes. Am J Pharm Educ. 1994;58(4):423–7. [Google Scholar]
- 34.Wald HS, Borkan JM, Taylor JS, et al. Fostering and evaluating reflective capacity in medical education: developing the REFLECT rubric for assessing reflective writing. Acad Med. 2012;87(3):41–50. doi: 10.1097/ACM.0b013e31823b55fa. [DOI] [PubMed] [Google Scholar]
- 35.Al-Elq AH. Simulation-based medical teaching and learning. J Family Community Med. 2010;17(1):35–40. doi: 10.4103/1319-1683.68787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maudsley G, Strivens J. Promoting professional knowledge, experiential learning, and critical thinking for medical students. Med Educ. 2000;34(7):535–44. doi: 10.1046/j.1365-2923.2000.00632.x. [DOI] [PubMed] [Google Scholar]
- 37.West DC, Pomeroy JR, Park JK, et al. Critical thinking in graduate medical education: a role for concept mapping assessment? JAMA: The Journal of the American Medical Association. 2000;284(9):1105–10. doi: 10.1001/jama.284.9.1105. [DOI] [PubMed] [Google Scholar]
- 38.Kowalski SD, Louis MA. Using computer technology to teach critical thinking. Nurse Educ. 2000;25(5):210–12. doi: 10.1097/00006223-200009000-00009. [DOI] [PubMed] [Google Scholar]
- 39.Cain J, Fox BI. Web 2.0 and pharmacy education. Am J Pharm Educ. 2009;73(7) doi: 10.5688/aj7307120. Article 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chan ZC. Exploring creativity and critical thinking in traditional and innovative problem-based learning groups. J ClinNurs. 2013;22(15-16):2298–307. doi: 10.1111/jocn.12186. [DOI] [PubMed] [Google Scholar]
- 41.Thistlewaite JE, Davies D, Ekeocha S, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med Teach. 2012;34(6):e421–44. doi: 10.3109/0142159X.2012.680939. [DOI] [PubMed] [Google Scholar]
- 42.Krockenberger MB, Bosward KL, Canfield PJ. Integrated case-based applied pathology (ICAP): a diagnostic approach model for the learning and teaching of veterinary pathology. J Vet Med Educ. 2007;34(4):396–408. doi: 10.3138/jvme.34.4.396. [DOI] [PubMed] [Google Scholar]
- 43.Hoag K, Lillie J, Hoppe R. Piloting case-based instruction in a didactic clinical immunology course. Clin Lab Sci. 2005;18(4):213–20. [PubMed] [Google Scholar]