Abstract
Objective
We tested the hypothesis that among 3- to 5-year-old children attending Head Start, body mass index z score will decline during the academic year and increase during the summer.
Methods
We used retrospective longitudinal growth data collected over 5 academic years from 1914 children (51% boys, 62% white) enrolled in a Michigan Head Start program. Changes in body mass index (BMI) z score, calculated as annual rate of change, during 2 academic years and the intervening summer were assessed by piecewise linear regression analysis. Potential covariates were gender, single-parent status, program year, race/ethnicity, age at initial enrollment, and family income (divided by household size).
Results
Mean BMI z score at the start of Head Start enrollment was 0.52 (95% confidence interval [95% CI] 0.39 to 0.65). Mean annual rates of BMI z score change were: −0.07 (95% CI −0.28 to 0.14) during the first year of enrollment, 0.62 (95% CI −0.0005 to 1.23) over the summer, and −0.82 (95% CI −1.50 to −0.13) during the second year of enrollment. The effect was most robust among girls of minority race/ethnicity.
Conclusions
Head Start is associated with a shifting of BMI z scores toward the norm among low-income preschool-aged children, particularly among girls of minority race/ethnicity.
Keywords: child, child care, obesity, preschool
A recent study that used nationally representative data estimated the prevalence of obesity among 4-year-old children at 18.4%.1 Effective obesity intervention and prevention programs for low-income and minority preschool-aged children are needed. Head Start is a United States federally funded preschool program that is free to 3- to 5-year-old children living below the federal poverty line. To achieve its primary mission of improving school readiness among low-income children, federal regulations mandate nutritional and health services, adequate time and space for active play, and parental involvement.2,3 In a recent national survey, most Head Start programs reported practices and environments related to healthy eating and physical activity that exceed these federal regulations.4 Given its organized structure, standardized regulations, and expansive reach among low-income preschoolers, Head Start is an ideal venue for obesity intervention and prevention.
Although federal Head Start performance standards mandate that programs monitor children’s height and weight,5,6 there is no centralized national data bank of these measures, and the 2 large federal studies of Head Start7,8 have not included anthropometrics. Reports of obesity prevalence within Head Start programs regionally have consistently described a higher obesity prevalence9–12 as compared to same-aged children nationally.13,14 Only 3 published reports describe changes in weight status among individual Head Start enrollees longitudinally, but because longitudinal changes were not the focus of these studies, the reports provided insufficient detail to allow meaningful inferences.11,15,16
The preschool age range is the period of adiposity rebound, during which body mass index (BMI) declines to a nadir and then begins to increase. Typically growing children are therefore expected to have declining BMIs to at least age 4 years, with a subsequent gradual increase. A z score conveys the number of standard deviation units an individual child’s BMI is from the reference population mean as it shifts. A girl whose BMI tracks at the 85th percentile from age 3 to 6 years would have an absolute decline of 0.4 kg/m2 over 18 months, followed by an increase of about 0.2 kg/m2 over the next 18 months, but zero change in z score throughout this time period, having maintained a consistent z score of about 1.00 in comparison to the reference population.
To our knowledge, no published studies have described changes in BMI z score within academic years in Head Start and the intervening summer. This may be particularly important given that significantly more weight gain has been reported to occur during the summer months, compared to during the academic year, among 5- to 6-year-old children.17 The present study was therefore a retrospective analysis of existing anthropometric data from one Head Start program over 5 years that sought to determine changes in BMI z score within individual children during the academic year and summer while controlling for potential confounders. We hypothesized that children would show a decrease in BMI z score during the academic year and an increase during the summer.
METHODS
Sample
The sample was composed of all children enrolled in Head Start classrooms across 14 sites managed by the Jackson Community Action Agency serving both an urban and rural 3-county area in south central Michigan. Children’s environments were diverse in that some lived in urban public housing complexes, while others lived in very rural, remote areas miles from any markets, restaurants, or community playgrounds. Nearly all (94%) of the children in our sample had family incomes below the federal poverty line; the other 6%were eligible because they had a disability, 80%of whom had isolated language delay.
The present cohort included all children who entered the program between fall 2001 and fall 2006. The number of annual enrollees at this Head Start program has steadily increased to most recently approximately 800 children; of these, approximately 550 to 600 children each year are attending half-day classes 4 days per week and are the subject of the present analysis. Classes operated for half-days from either 8 to 11:30 am or 1 to 4:30 pm, 4 days a week (Monday through Thursday), from approximately September 1 to May 15. Classes included 15 to 17 children, one teacher, and one aide. For morning classes, shortly after arrival, children were provided breakfast, which typically consisted of a serving of dairy, meat, and fruit. Lunch was provided shortly before the children left for the day, and typically consisted of a serving of dairy, meat, vegetable, and fruit. For afternoon classes, children were provided lunch shortly after arrival. A snack was provided shortly before the children left for the day and typically consisted of a serving of dairy and meat or a serving of vegetable and meat. Children participated in 25 minutes of outside exercise, 15 minutes of music time with dancing and singing, and 60 minutes of free time to choose their own activities each day. Each Head Start site had an on-site playground. The Head Start program was not conducting any specific interventions for obesity or nutrition.
Data Collection and Measures
Parents reported basic demographic information at the time their child enrolled in Head Start. This study was deemed exempt by the University of Michigan Health Sciences Institutional Review Board because it was a retrospective review of deidentified data.
Measured weights and heights were obtained for all children within 90 calendar days of enrollment, as required by Head Start regulations.5,6 This particular Head Start program’s own policy required teachers to weigh and measure each child at the beginning and end of each academic year as part of efforts to monitor health and nutrition. Teachers were trained by Head Start health specialists (who were trained as licensed practical nurses or medical assistants) in how to perform the measurements, and they used the same equipment in a dedicated health room at both time points with shoes off and light clothing. Teachers obtained the measurements and provided them to the Head Start program’s clerical office, where staff entered them into a central database. At the time of measurement, the teachers did not have access to information that could have generated bias, including prior measurements or growth patterns or whether the measurements obtained equated to a categorization of the child’s BMI as obese, overweight, or underweight. Each child enrolled in Head Start is also required to provide documentation of an annual health maintenance examination from their health care provider, and these anthropometric data were also included in the database.
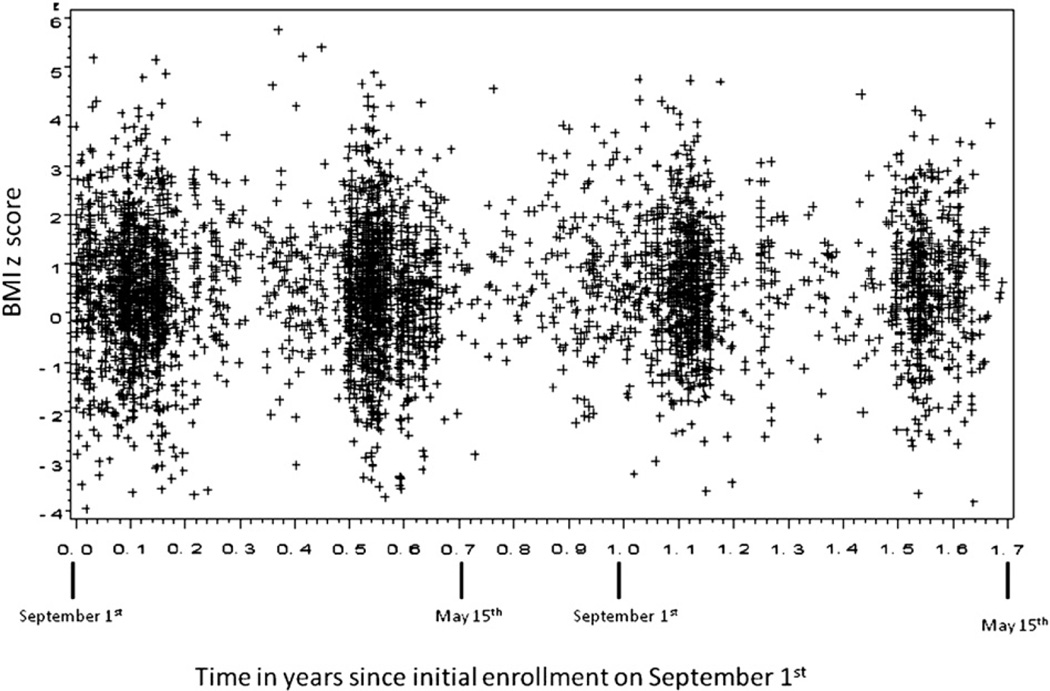
Figure 1 shows the timing of the measurements described above. The clusters of measurements in the fall and spring of each of the 2 years reflect the measurements taken by the teachers. Data points in the figure falling on the x-axis outside of these clusters represent the data points contributed from annual health maintenance exams at the outside health care providers’ offices. An individual child enrolled in Head Start for a full 2 years would therefore have up to 4 sets of anthropometric data obtained by Head Start staff and 2 sets of data obtained from their primary care provider’s office contributing to this data set. As can be seen in the figure, the majority of anthropometric data included in this analysis were measurements taken at Head Start by the teachers.
Figure 1.
Timing of measurements of body mass index (BMI) over 2 academic years in relation to initial enrollment on September 1.
BMI was calculated and BMI percentiles and z scores derived by using age- and gender-specific norms from the Centers for Disease Control growth charts.18 Obese was defined as a BMI ≥95th percentile, overweight as a BMI ≥85th percentile but <95th percentile, and underweight as a BMI <10th percentile. Normal weight was defined and examined in 2 alternate ways, as a BMI ≥10th percentile but <85th percentile as well as a BMI ≥5th percentile but <95th percentile. Children were excluded if they had a z score for BMI, weight or height less than −4; a height z score more than +4; changes in z score for BMI, weight, or height during the academic year >5 standard deviation units; or a significant decrease in height between measurements. Less than 5% of the original sample was excluded on the basis of these criteria, and there were no other exclusion criteria.
Statistical Analysis
We sought to determine whether there were changes in individual children’s BMI z score longitudinally over time. Initial examination of the data indicated that the change in BMI z score over time was not linear. Therefore, piecewise linear regression, which allows for different slopes for different time periods, was performed via repeated measures analysis by using mixed models with random intercept to evaluate changes in BMI z score across time. The PROC MIXED procedure in the SAS software package (SAS Institute, Cary, NC), a powerful statistical method that accounts for within-subject correlation and missing data, was used to complete this analysis, which included 4374 measurements on 1914 unique children. Slopes were individually defined within the following 3 windows: September 1 through May 15 of the first year of enrollment; May 15 through September 1 following the first year of enrollment (ie, summer); and September 1 through May 15 of the second year of enrollment. Sample sizes within each time frame are shown in Table 1. The slopes identified in these windows are annual rate of BMI z score change (as opposed to absolute change within the specified time period), to allow comparison of rates of change between the academic year and summer. A P value of .05 was used to determine statistical significance.
Table 1.
Sample Size by Study Interval
| Year in Head Start | |||||
|---|---|---|---|---|---|
| First Year | Second Year | ||||
| Characteristic | Total | Fall | Spring | Fall | Spring |
| No. of observations | 4374 | 1306 | 1479 | 1002 | 587 |
| No. of unique subjects | 1914 | 1091 | 1205 | 744 | 510 |
| Age at time BMI measured* | |||||
| 3 years | 454 | 716 | 461 | 85 | 0 |
| 4 years | 1128 | 368 | 635 | 646 | 297 |
| 5 years | 332 | 7 | 109 | 13 | 213 |
BMI = body mass index.
We included program year as a covariate a priori. We tested the inclusion of additional potential covariates known to have an association with weight status, which included gender (male vs female), single-parent status (single-parent vs 2-parent household), race/ethnicity (white vs minority), household income (divided by number of individuals living in the household), and initial age at enrollment. We tested interactions of each covariate with time period (first year of enrollment, summer, or second year of enrollment) and retained in the model only those covariates that had either significant main or interactive effects. We present the final adjusted model in the full sample, stratified by gender and race/ethnicity, as well as by weight status (obese, overweight, normal weight, and underweight) at the time of initial enrollment. We considered that changes in BMI could occur not only as a result of changes in rate of weight gain, but also as a result of changes in rate of linear growth. We therefore also repeated the piecewise linear regression, adjusting for covariates, predicting height z score as the outcome.
RESULTS
Characteristics of the sample are provided in Table 2. The sample was 51.2% boys, 62.5% white, 22.2% black, 7.2% multiracial, 6.7% Hispanic, and 1.4% another race. The final adjusted model is shown in Table 3. Neither income nor initial enrollment age had significant main or interactive effects on BMI z score and were therefore not included in the final model. As shown in the first column of Table 3 reporting results for the full sample, the mean BMI z score at the start of Head Start enrollment was 0.52 (95% confidence interval [95% CI] 0.39 to 0.65). Over the first academic year, mean BMI z score declined (nonsignificantly) by −0.07 (95% CI −0.28 to 0.14) BMI z score units per year, resulting in a mean BMI z score of 0.47 at the end of the first academic year. During the next summer, mean BMI z score increased (nonsignificantly) at a rate of 0.62 (95% CI −0.0005 to 1.23) units per year, resulting in a mean BMI z score at the start of the second academic year of 0.65. During the second academic year, mean BMI z score declined significantly at a rate of −0.82 (95% CI −1.50 to −0.13) units per year, resulting in a mean BMI z score of 0.07 by the end of the academic year. Thus, over the course of the 2 years, there was an overall shift in the distribution of BMIs within the Head Start sample toward the national population reference mean. Boys, children in single-parent families, and children of minority race/ethnicity had significantly higher BMI z scores over time. The results stratified by both gender and race/ethnicity are presented in the remaining columns of Table 3. Significant changes in BMI z score occurred only for minority girls. For this group, mean BMI z score significantly increased over the summer and declined during the second year of enrollment.
Table 2.
Characteristics of Study Sample
| Boys | Girls | ||||
|---|---|---|---|---|---|
| Characteristic | Total (N = 1914) | White (n = 635) | Minority (n = 345) | White (n = 561) | Minority (n = 373) |
| Single parent, n (%) | |||||
| Yes | 1058 (55.3) | 304 (47.9) | 233 (66.6) | 254 (45.3) | 267 (71.6) |
| No | 856 (44.7) | 331 (52.1) | 112 (33.4) | 307 (54.7) | 106 (28.4) |
| Weight status, n (%)*,† | |||||
| Obese | 252 (17.0) | 85 (17.1) | 55 (20.3) | 60 (14.0) | 52 (18.0) |
| Overweight | 240 (16.2) | 65 (13.1) | 39 (14.4) | 80 (18.7) | 56 (19.4) |
| Normal weight | 891 (60.0) | 313 (63.0) | 158 (58.3) | 252 (58.9) | 168 (58.1) |
| Underweight | 102 (6.9) | 34 (6.8) | 19 (7.0) | 36 (8.4) | 13 (4.5) |
| Program year, n (%) | |||||
| 2002 | 140 (7.3) | 44 (6.0) | 33 (9.6) | 39 (6.9) | 24 (6.4) |
| 2003 | 486 (25.4) | 169 (26.6) | 84 (24.3) | 144 (25.7) | 89 (23.9) |
| 2004 | 371 (19.4) | 122 (19.2) | 70 (20.3) | 117 (20.8) | 62 (16.6) |
| 2005 | 350 (18.3) | 121 (19.0) | 58 (16.8) | 116 (20.7) | 55 (14.7) |
| 2006 | 567 (29.6) | 179 (28.2) | 100 (29.0) | 145 (25.8) | 143 (38.3) |
| BMI z score, mean (SD)* | 0.53 (1.31) | 0.56 (1.38) | 0.67 (1.43) | 0.43 (1.22) | 0.62 (1.13) |
| Average income per household member, mean (SD)‡ | 3835 (2823) | 4021 (2911) | 3483 (2699) | 3967 (2902) | 3512 (2568) |
| Age, y, mean (SD)* | 3.77 (0.56) | 3.85 (0.56) | 3.73 (0.56) | 3.79 (0.57) | 3.68 (0.52) |
At enrollment; SD = standard deviation.
Sample size = 1485.
Sample size = 1803.
Table 3.
BMIz Change Across 3 Time Periods Stratified by Race/Ethnicity and Gender†
| Boys | Girls | ||||
|---|---|---|---|---|---|
| Characteristic | Full sample | White | Minority | White | Minority |
| No. of unique participants | 1914 | 637 | 347 | 562 | 374 |
| No. of observations | 4374 | 1446 | 816 | 1199 | 913 |
| BMIz at enrollment (Intercept) | 0.52 (0.39 to 0.65) | 0.67 (0.46 to 0.89) | 0.63 (0.35 to 0.92) | 0.53 (0.30 to 0.75) | 0.77 (0.56 to 0.98) |
| Annual rate of BMIz change | |||||
| First academic year | −0.07 (−0.28 to 0.14) | 0.11 (−0.27 to 0.49) | −0.10 (−0.63 to 0.43) | −0.04 (−0.42 to 0.34) | −0.38 (−0.77 to 0.02) |
| Summer | 0.62 (−0.00 to 1.23) | 0.10 (−1.04 to 1.23) | 1.52 (−0.57 to 2.46) | 0.12 (−1.03 to 1.27) | 1.69 (0.53 to 2.86)* |
| Second academic year | −0.82 (−1.50 to −0.13)* | −0.46 (−1.72 to 0.79) | −1.37 (−3.01 to 0.27) | −0.34 (−1.66 to 0.98) | −1.36 (−2.65 to −0.08)* |
| Male (vs female) | 0.12 (0.05 to 0.20)* | ||||
| Nonwhite (vs white) race/ethnicity | 0.16 (0.08 to 0.24)* | ||||
| Two parent (vs single) | −0.09 (−0.17 to −0.02)* | −0.27 (−0.41 to −0.14)* | 0.16 (−0.04 to 0.36) | −0.18 (−0.32 to −0.04)* | 0.19 (0.03 to 0.35)* |
P <.05.
Multivariate models showing slope and 95% confidence intervals for body mass index z score (BMIz) (standard deviation unit) change across each of 3 time periods (first academic year, summer, and second academic year) in full sample and stratified by race/ethnicity and gender.
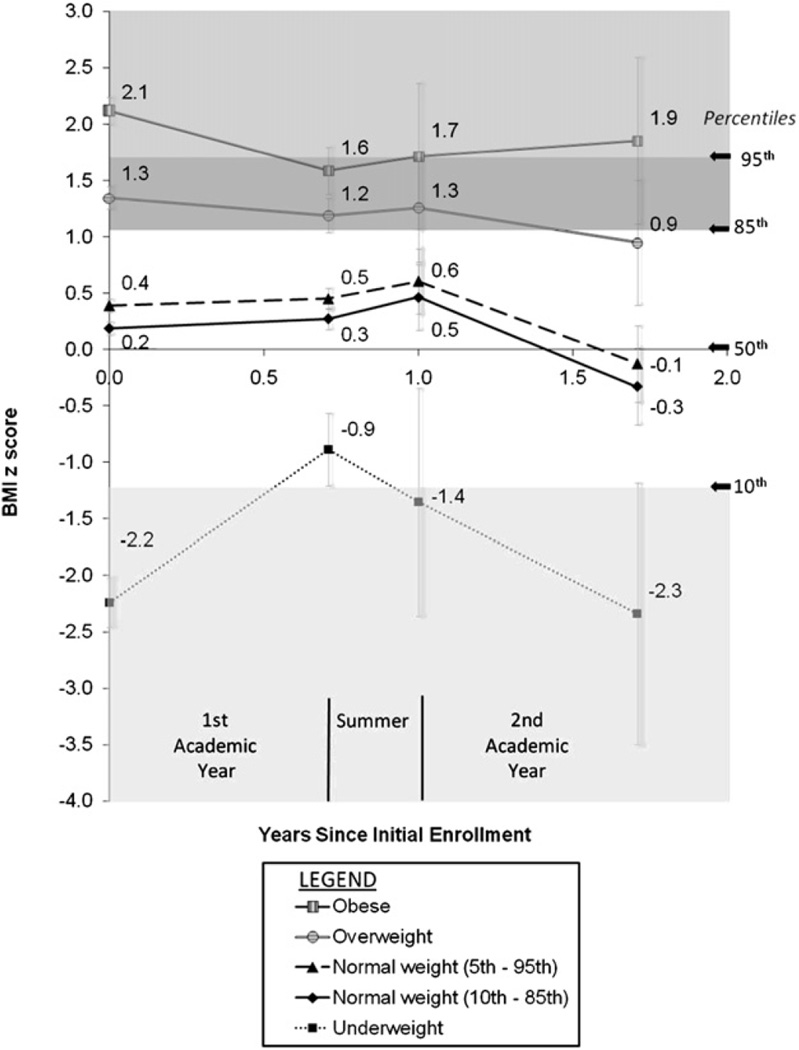
The results stratified by initial weight status at the time of enrollment are presented in Table 4. Figure 2 shows the mean z scores at the beginning and end of each time period that result from the annual rates of change described in Table 4 for children beginning Head Start with the specified weight status. The percentiles corresponding to the cutoffs for obese, overweight, and underweight are shown on the right-hand side of Figure 2 and signified by the shaded regions. As depicted by the dark triangles and diamonds in the figure, the starting BMI distribution of the sample of children who began Head Start in the normal weight range (by either definition) was shifted slightly upward from the Centers for Disease Control and Prevention reference mean (ie, z score = 0, or 50th percentile). The BMI distribution of this group of children remained shifted slightly above the reference mean through the first year of Head Start and began to shift further upward over the summer, to reach a new sample mean z score of 0.5 to 0.6. The BMI distribution of this group shifted downward over the subsequent academic year to meet the population reference mean. As shown in Table 4, significant shifts in BMI z score for the group of children starting Head Start in the normal weight range occurred during the second academic year only.
Table 4.
BMIz Change Across 3 Time Periods Stratified by Initial Weight Status†
| Normal Weight | |||||
|---|---|---|---|---|---|
| Characteristic | Obese | Overweight | Underweight | 10th to 85th Percentile | 5th to 95th percentile |
| No. of unique participants | 259 | 255 | 117 | 907 | 1173 |
| No. of observations | 606 | 566 | 278 | 2120 | 2774 |
| BMIz at enrollment (Intercept) | 2.12 (1.87 to 2.36) | 1.35 (1.16 to 1.54) | −2.04 (−2.47 to −1.60) | 0.19 (0.07 to 0.31) | 0.39 (0.27 to 0.51) |
| Annual rate of BMIz change | |||||
| First academic year | −0.74 (−1.14 to −0.34)* | −0.22 (−0.53 to 0.08) | 1.84 (1.20 to 2.49)* | 0.12 (−0.07 to 0.31) | 0.09 (−0.09 to 0.27) |
| Summer | 0.44 (−0.83 to 1.70) | 0.24 (−0.71 to 1.18) | −1.39 (−3.37 to −0.59)* | 0.65 (0.07 to 1.24)* | 0.53 (−.0.04 to 1.10) |
| Second academic year | 0.19 (−1.26 to 1.64) | −0.44 (−1.53 to 0.65) | −0.15 (−2.40 to 2.08) | −1.12 (−1.82 to −0.43)* | −1.03 (−1.70 to −0.36)* |
| Male (vs female) | 0.34 (0.18 to 0.49)* | 0.13 (0.01 to 0.25)* | 0.24 (−0.02 to 0.49) | −0.01 (−0.08 to 0.06) | −0.04 (−0.11 to 0.03) |
| Nonwhite (vs white) race/ethnicity | 0.13 (−0.02 to 0.29) | 0.07 (−0.05 to 0.19) | 0.34 (0.07 to 0.62)* | −0.04 (−0.11 to 0.04) | −0.002 (−0.74 to 0.74) |
| Two parent (vs single) | 0.05 (−0.11 to 0.21) | −0.13 (−0.25 to −0.01)* | −0.14 (−0.40 to 0.12) | −0.12 (−0.20 to −0.05)* | −0.12 (−0.19 to −0.05)* |
P <.05.
Multivariate models showing slope and 95% confidence intervals for body mass index z score (BMIz) (standard deviation unit) change across each of 3 time periods (first academic year, summer, and second academic year) stratified by initial weight status.
Figure 2.
Changes in body mass index (BMI) z score across each of 3 time periods (first academic year in Head Start, summer, and second academic year) by using piecewise regression, adjusted for gender, race/ethnicity, single-parent status, and program year stratified by weight status at enrollment (n = 1914 subjects). At right are the percentile equivalents of the z scores that mark the cutoffs for each weight status as well as the 50th percentile. The weight status described is the child’s weight status at enrollment (time zero). Normal weight is defined and shown in 2 different ways.
As denoted by the open circle symbol in Figure 2, the BMI distribution of the 255 children who began Head Start in the overweight range followed a similar pattern to that of the children beginning Head Start in the normal weight range, in that their BMI distribution remained shifted upward throughout the first year, shifted further upward over the summer, and then shifted downward toward the population reference mean during the second year of enrollment. As shown in Table 4, these changes did not, however, reach statistical significance. As denoted by the open square symbol in Figure 2, the BMI distribution of the 259 children who began Head Start in the obese range showed a significant downward shifting over the first year (P < .05, Table 4). There was some suggestion of a slow rebound, with a steady upward shifting over the summer and second academic year, but these changes were not statistically significant. Finally, as denoted by the dark square symbol in Figure 2, the BMI distribution of the 117 children who began Head Start in the underweight range showed a significant upward shifting over the first year (P < .05, Table 4), with a significant rebounding downward shift over the summer (P < .05, Table 4). Among the 22 children remaining in the sample during the second academic year, there was no significant change in z score.
There was no significant change in height z score during any of the 3 time periods: b = 0.05 (95% CI −0.14 to 0.23) for the first academic year, b = 0.03 (95% CI −0.52 to 0.57) for the summer, and b = 0.15 (95% CI −0.46 to 0.76) for the second academic year.
DISCUSSION
The pattern of findings in the present study suggests a beneficial effect of Head Start on children’s weight status, but the effect was modified by both the child’s sociodemographic characteristics and weight status at enrollment.
Shift of BMI Distribution Toward Population Reference Mean
The children in the present study began their Head Start experience with a distribution of BMIs significantly above the national Centers for Disease Control and Prevention reference means for children of the same age and gender, consistent with the prior reports of Head Start enrollees having a higher prevalence of obesity than same-aged children in the general US population.9–12 The central finding of the present study was that over the course of enrollment, there was a significant shift in the BMI distribution of the sample toward the population reference mean, such that at the conclusion of 2 years of Head Start exposure, this sample of low-income children had a distribution of BMIs no different from national norms defining healthy BMIs for children in this age range. There was the suggestion of a dose effect, such that the impact on BMI occurred more in the second year of enrollment. The observation that BMIs rebounded slightly over the summer also supports the hypothesis that Head Start had a causal role in the normalization of the children’s BMIs.
Moderation by Sociodemographic Characteristics
The shift in weight status toward the population reference norm was most robust for minority girls. It is possible that the moderating effect of race/ethnicity is rooted in differences between the home environment and Head Start specific to these groups. For example, feeding beliefs and practices,19–21 television viewing habits,22–24 and opportunities for physical activity25,26 may all be more obesity promoting in minority compared to white racial/ethnic groups. The significant effect in girls, but not boys, observed in our data may be related to the possibility that boys in this demographic could be given the opportunity to participate in active play at home more commonly than girls. In summary, the same Head Start environment may have a more robust effect in these groups because the differences between the home and Head Start environment are most pronounced.
Moderation by Starting Weight Status
The timing of the changes in BMI z score differed according to children’s weight status at enrollment. Children who began Head Start in the normal weight range (although notably still with a BMI distribution shifted upward relative to population reference norms) comprised the majority of the sample. For this group, the greatest shift in the BMI distribution toward the population reference mean occurred during the second year of enrollment, suggesting a “dose effect” of Head Start for this group. For children beginning Head Start in the overweight range, the timing of the change was similar, although it did not reach statistical significance. In contrast, the timing of the BMI change for the children beginning Head Start in the obese or underweight ranges differed significantly from those beginning in the normal weight range, in that the shift in their BMIs toward normal occurred much sooner, in the first year of enrollment. The fact that changes in BMI occurred sooner, with less time in Head Start, suggests that the home environments of these children with regard to nutrition and physical activity diverged more significantly from the norm than those of the other children. Therefore, exposure to the normative Head Start environment would have a more pronounced impact on the weight status of these children, translating to a more robust and immediate effect.
There were no significant changes in BMI z score for the initially obese or underweight during the second academic year, although the sample sizes were small and any inferences should be made with caution. However, the findings suggest that the impact of Head Start alone on normalization of weight status among obese and underweight children is limited, and the development of additional effective interventions for this group within the Head Start setting is an important goal.
Limitations
There are limitations to this study. We did not have data regarding maternal weight status or the child’s birth weight. The anthropometric measures contributing to this analysis were obtained by both Head Start staff and health care providers’ offices and not in a prospective fashion for this research study. However, the staff performing the measurements in both settings had similar training and used similar equipment, and there is no reason to suspect a systematic bias in measurements.
The study sample consisted of children from one Head Start program in one geographic area, and the replicability of these findings in other programs is uncertain. However, the nature of the Head Start regulations makes the quality and character of the Head Start environment much more consistent across programs than non–Head Start preschool settings. Absent any nationally representative Head Start data set to address the research question, the robust regulatory environment surrounding Head Starts nationally that engenders cross-program consistency allows one greater confidence in extrapolating the findings to other programs.
We considered that the decline in BMI z scores during the academic years resulted not from a slowing of excessive weight gain, but from an increase in height gain, given that gains in height among children are sometimes seen when environmental stressors are reduced,27 as may occur when more time is spent in Head Start as opposed to in the home. However, there were no significant changes in height z score, supporting the primary hypothesis that Head Start has beneficial effects on changes in weight.
Conclusions
Published work examining associations between child care experience and obesity risk continues to be conflicting, with some studies indicating a beneficial effect28 and others showing no effect.29 The effect of child care exposure on obesity risk may be moderated by age, such that it is a risk factor for children younger than 3 years,30,31 but a protective factor for children older than 3 years.28 The effect may be also be moderated by sociodemographic and anthropometric characteristics,32 as in our study.
The present study suggests beneficial effects of Head Start enrollment on the BMI of low-income preschool-aged children. Head Start has been shown to confer both social and educational advantages for low-income children,33 and healthy changes in BMI during the academic year may be one more benefit of enrolling children in Head Start.
ACKNOWLEDGMENT
We acknowledge grant support from the American Heart Association Fellow-to-Faculty Transition Award to Dr Lumeng, and the Robert Wood Johnson Foundation to Dr Frisvold. We thank Kyung Rhee, MD, MS, Deborah A. Frank, MD, Tiffany Cardinal, BS, and previous anonymous reviewers for helpful suggestions on earlier versions of this article. We also thank the Jackson Community Action Agency for providing the data for the present study.
REFERENCES
- 1.Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch Pediatr Adolesc Med. 2009;163:344–348. doi: 10.1001/archpediatrics.2009.18. [DOI] [PubMed] [Google Scholar]
- 2.Administration for Children and Families. Title 45, Chapter XIII—Office of Human Development Services, Department of Health and Human Services, Part 1304.23—Program Performance Standards for the Operation of Head Start Programs by Grantee and Delegate Agencies: Child nutrition. [Accessed August 6, 2007]; Available at: http://www.access.gpo.gov/nara/cfr/waisidx_05/45cfr1304_05.html.
- 3.Administration for Children and Families. Title 45, Chapter XIII—Office of Human Development Services, Department of Health and Human Services, Part 1304.21—Program Performance Standards for the Operation of Head Start Programs by Grantee and Delegate Agencies: Education and early childhood development. [Accessed August 6, 2007]; Available at: http://www.access.gpo.gov/nara/cfr/waisidx_05/45cfr1304_05.html.
- 4.Whitaker RC, Gooze RA, Hughes CC, Finkelstein DM. A national survey of obesity prevention practices in head start. Arch Pediatr Adolesc Med. 2009;163:1144–1150. doi: 10.1001/archpediatrics.2009.209. [DOI] [PubMed] [Google Scholar]
- 5.Office of Human Development Services, Department of Health and Human Services. Title 45, Chapter XIII, Part 1304: Performance Standards for the Operation of Head Start, Subpart b: Early Childhood Development and Health Services, Section 1304.20. [Accessed June 30, 2007];Child health and developmental services. Available at: http://edocket.access.gpo.gov/cfr_2007/octqtr/45cfr1304.20.htm.
- 6.Services Centers for Medicare and Medicaid. The State Medicaid Manual: Chapter 5—Early and Periodic Screening. [Accessed June 30, 2008]; Available at: http://www.cms.hhs.gov/Manuals/PBM/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=1&sortOrder=ascending&itemID=CMS021927.
- 7.US Department of Health and Human Services. Head Start Impact Study: First Year Findings. Washington, DC: Administration for Children and Families; 2005. [Google Scholar]
- 8.Office of Planning Research, and Evaluation. Head Start research: Head Start Family and Child Experiences Survey (FACES), 1997–2010. [Accessed June 30, 2008]; Available at: http://www.acf.hhs.gov/programs/opre/hs/faces/index.html.
- 9.Wiecha JL, Casey VA. High prevalence of overweight and short stature among Head Start children in Massachusetts. Pub Health Rep. 1994;109:767–773. [PMC free article] [PubMed] [Google Scholar]
- 10.Hernandez B, Uphold CR, Graham MV, Singer L. Prevalence and correlates of obesity in preschool children. J Pediatr Nurs. 1998;13:68–76. doi: 10.1016/S0882-5963(98)80033-X. [DOI] [PubMed] [Google Scholar]
- 11.Hu WT, Foley TA, Wilcox RA, et al. Childhood obesity among Head Start enrollees in Southeastern Minnesota: Prevalence and risk factors. Ethnic Dis. 2007;17:23–38. [PubMed] [Google Scholar]
- 12.Feese M, Franklin F, Murdock M, et al. Prevalence of obesity in children in Alabama and Texas participating in social programs. JAMA. 2003;289:1780–1781. doi: 10.1001/jama.289.14.1780-b. [DOI] [PubMed] [Google Scholar]
- 13.Ogden CL, Troiano RP, Briefel RR, et al. Prevalence of overweight among preschool children in the United States, 1971 through 1994. Pediatrics. 1997;99:e1. doi: 10.1542/peds.99.4.e1. [DOI] [PubMed] [Google Scholar]
- 14.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 15.Fitzgibbon ML, Stolley MR, Schiffer L, et al. Two-year follow-up results for Hip-Hop to Health Jr: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr. 2004;146:618–625. doi: 10.1016/j.jpeds.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 16.Fitzgibbon ML, Stolley MR, Schiffer L, et al. Hip-Hop to Health Jr for Latino preschool children. Obesity. 2006;14:1616–1625. doi: 10.1038/oby.2006.186. [DOI] [PubMed] [Google Scholar]
- 17.vonHippel PT, Powell B, Downey DB, Rowland NJ. The effect of school on overweight in childhood: gain in body mass index during the school year and summer vacation. Am J Pub Health. 2007;97:696–702. doi: 10.2105/AJPH.2005.080754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts. Advance Data. 2000;314:1–28. [PubMed] [Google Scholar]
- 19.Sherry B, McDivitt J, Birch LL, et al. Attitudes, practices, and concerns about child feeding and child weight status among socioeconomically diverse white, Hispanic, and African-American mothers. J Am Diet Assoc. 2004;104:215–221. doi: 10.1016/j.jada.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 20.Baughcum AE, Burklow KA, Deeks CM, Powers SW, Whitaker RC. Maternal feeding practices and childhood obesity. Arch Pediatr Adolesc Med. 1998;152:1010–1014. doi: 10.1001/archpedi.152.10.1010. [DOI] [PubMed] [Google Scholar]
- 21.Jain A, Sherman SN, Chamberlin LA, et al. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics. 2001;107:1138–1146. doi: 10.1542/peds.107.5.1138. [DOI] [PubMed] [Google Scholar]
- 22.Andersen R, Crespo C, Bartlett S, Cheskin L, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children: results from the third National Health and Nutrition Examination Survey. JAMA. 1998;279:938–942. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- 23.Certain L, Kahn R. Prevalence, correlates, and trajectory of television viewing among infants and toddlers. Pediatrics. 2002;109:634–642. doi: 10.1542/peds.109.4.634. [DOI] [PubMed] [Google Scholar]
- 24.Dennison B, Erb T, Jenkins P. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109:1028–1035. doi: 10.1542/peds.109.6.1028. [DOI] [PubMed] [Google Scholar]
- 25.Gordon-Larsen P, Adair LS, Popkin BM. Ethnic differences in physical activity and inactivity patterns and overweight status. Obesity. 2002;10:141–149. doi: 10.1038/oby.2002.23. [DOI] [PubMed] [Google Scholar]
- 26.Gordon-Larsen P, McMurray RG, Popkin BM. Determinants of adolescent physical activity and inactivity patterns. Pediatrics. 2000;105:e83. doi: 10.1542/peds.105.6.e83. [DOI] [PubMed] [Google Scholar]
- 27.Skuse D, Albanese A, Stanhope R, Gilmour J, Voss L. A new stress-related syndrome of growth failure and hyperphagia in children, associated with reversibility of growth-hormone insufficiency. Lancet. 1996;348(9024):353–358. doi: 10.1016/s0140-6736(96)01358-x. [DOI] [PubMed] [Google Scholar]
- 28.Lumeng JC, Gannon K, Appugliese D, Cabral HJ, Zuckerman B. Preschool child care and risk of overweight in 6- to 12-year-old children. Int J Obes Relat Metab Disord. 2005;29:60–66. doi: 10.1038/sj.ijo.0802848. [DOI] [PubMed] [Google Scholar]
- 29.Kimbro RT, Brooks-Gunn J, McLanahan S. Racial and ethnic differentials in overweight and obesity among 3-year-old children. Am J Public Health. 2007;97:298–305. doi: 10.2105/AJPH.2005.080812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim J, Peterson KE. Association of infant child care with infant feeding practices and weight gain among us infants. Arch Pediatr Adolesc Med. 2008;162:627–633. doi: 10.1001/archpedi.162.7.627. [DOI] [PubMed] [Google Scholar]
- 31.Benjamin SE, Rifas-Shiman SL, Taveras EM, et al. Early child care and adiposity at ages 1 and 3 years. Pediatrics. 2009;124:555–562. doi: 10.1542/peds.2008-2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maher EJ, Li G, Carter L, Johnson DB. Preschool child care participation and obesity at the start of kindergarten. Pediatrics. 2008;122:322–330. doi: 10.1542/peds.2007-2233. [DOI] [PubMed] [Google Scholar]
- 33.Zill N, Resnick G, Kim K, et al. Head Start FACES: Longitudinal Findings on Program Performance: Third Progess Report. [Accessed February 17, 2010]; Available at: http://www.acf.hhs.gov/programs/opre/hs/faces/reports/perform_3rd_rpt/meas_99_title.html.