Abstract
Background
At least 17% of the population in Germany has been infected with the hepatitis E virus (HEV); thus, HEV infections are more frequent than was previously assumed. However, fewer than 500 HEV infections were reported to the Robert Koch Institute in 2013.
Method
Review of pertinent literature retrieved by a selective search in PubMed.
Results
Persons living in Germany generally acquire hepatitis E infection within the country by consuming infected and undercooked pork; in rare cases, hepatitis E infections are imported from the tropics. HEV can be transmitted via blood products, blood transfusions, and organ transplantation. More than 99% of HEV infections are asymptomatic and self-limiting, but there are also severe cases with acute liver failure. Immunosuppressed persons can develop chronic HEV infection, potentially leading, within a few years, to liver cirrhosis with life-threatening sequelae. Moreover, HEV infection may be associated with extrahepatic manifestations such as Guillain-Barré syndrome. In two retrospectively evaluated case series, ribavirin was found to be active against HEV and can be used to treat either acute or chronic HEV infection.
Conclusion
Hepatitis E must be considered in the differential diagnosis of elevated hepatic enzyme levels and of systemic and neurological conditions of uncertain origin. The infection is usually self-limiting but can take a severe course in immunosuppressed persons. In such cases, ribavirin can be used as an antiviral treatment.
It became evident in the 1970s that a second hepatitis virus with fecal–oral transmission must exist in the tropics alongside the hepatitis A virus. The Russian scientist M.S. Balayan succeeded in infecting himself with this virus by swallowing pooled extracts of fecal samples from a patient with non-A non-B hepatitis. He developed clinical hepatitis, and the hepatitis E virus (HEV) was demonstrated in his feces by electron microscopy. (1).
HEV is endemic to many tropical nations and is responsible for numerous outbreaks of hepatitis in these countries, particularly after major floods or in refugee camps (1, 2). It is estimated that the number of symptomatic HEV infections in the tropics exceeds 3 million annually, causing approximately -70 000 deaths each year (3). The disease may be particularly fulminant in pregnant women and in patients with chronic liver disease (1). HEV infection can cause symptoms of liver inflammation such as jaundice, pruritus, and upper abdominal pain. Furthermore, nonspecific and extrahepatic manifestations such as arthralgia and Guillain–Barré syndrome have been described in the course of HEV infection (4, 5).
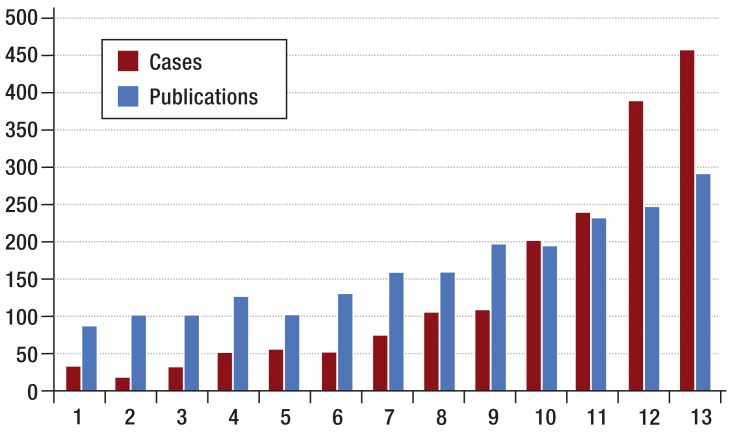
The perception and assessment of hepatitis E have undergone a transformation in recent years. An increase in the number of HEV infections acquired in Europe, together with the discovery of chronic hepatitis E in immunosuppressed individuals, has dispelled the notion of hepatitis E as merely an acute tropical illness, thus lending this infectious disease new importance in the industrialized nations (1). In Germany the number of cases reported to the Robert Koch Institute has risen sharply in recent years, as has the number of publications on HEV listed in PubMed (Figure 1), whereas the prevalence of antibodies to HEV in serum has remained constant since 1993 (6). This observation suggests that the increase in cases of hepatitis E reported to the Robert Koch Institute arises from increased awareness of this disease (6).
Figure 1.
Numbers of cases of hepatitis E reported in Germany (red; Robert Koch Institute) and numbers of publications on hepatitis E worldwide (blue; PubMed) in the period 2001 to 2013
Epidemiology and routes of transmission of hepatitis E virus
There are five genotypes of HEV. Genotypes 1 to 4 are human pathogens, while genotype 5 is found only in birds. The worldwide distribution of genotypes 1 to 4 is shown in Figure 2. Most cases of hepatitis E in Europe are caused by HEV genotype 3. This genotype is autochthonous, i.e., the HEV infections are acquired within Europe (7). Imported infections, in contrast, are mostly caused by HEV genotype 1 (7). With only occasional exceptions HEV genotypes 1 and 2 have been demonstrated only in humans, not in animals (1).
Figure 2.
Distribution of HEV genotypes
While in the tropics HEV is generally transmitted via contaminated drinking water, this pathway plays no part in the industrialized nations with their stringent quality requirements (1). Instead, zoonotic infections, i.e., infection by contact with living animals or with animal products contaminated with HEV, are likely of major importance in these countries (Table 1) (1). HEV genotypes 3 and 4 have been repeatedly detected in animals, for example in pigs and in commercially available pork (1). Heating to over 70 °C inactivates the virus, so that properly cooked meat is harmless (1).
Table 1. Transmission of hepatitis E virus.
| Infection source | Remarks | Literature |
|---|---|---|
| Drinking water | Principle route of transmission in the tropics; does not apply in industrialized nations owing to better hygiene | Emerson 2004 (40) |
| Pork meat | Thought to be principle route of transmission in industrialized nations (virus inactivated by heating to over 70 °C) | Banks 2004 (e5) |
| Blood products | Precise role in industrialized nations not yet conclusively clarified, but possible source of infection. Universal testing of blood products for HEV would eliminate this risk but has not yet been recommended by the responsible authorities. | Nelson 2014 (e6) |
| Sea food | For example as cause of an outbreak on a cruise ship (essential to avoid uncooked food) | Said 2009 (13) |
| Strawberries | Relevant source of infection particularly in children. Still unclear whether thorough washing reduces the risk. | Halac 2011 (e7) |
| Person-to-person transmission | Described in Uganda and, in isolated cases, in Europe (risk reduced by good hygiene) | Teshale 2011 (e8) |
| Transplanted organs | Described in individual cases. Universal testing of all transplants for HEV has not yet been recommended. | Schlosser 2011 (e9) |
HEV can also be transmitted via infected blood products. The role of this mode of transmission in the industrialized nations has not yet been clearly established. A recently published retrospective study showed that 79 (0.04%) of 225 000 blood donations in England contained HEV RNA. Forty-three of these blood products had already been transfused before the study results became known; 18 (42%) of the recipients developed signs of hepatitis E (8).
The question of whether blood products and transplants should always be tested for HEV is currently under debate. In 2009 the Blood Committee of the German Federal Ministry of Health decided not to recommend universal testing of blood products for HEV. The same body is now discussing this topic anew (9).
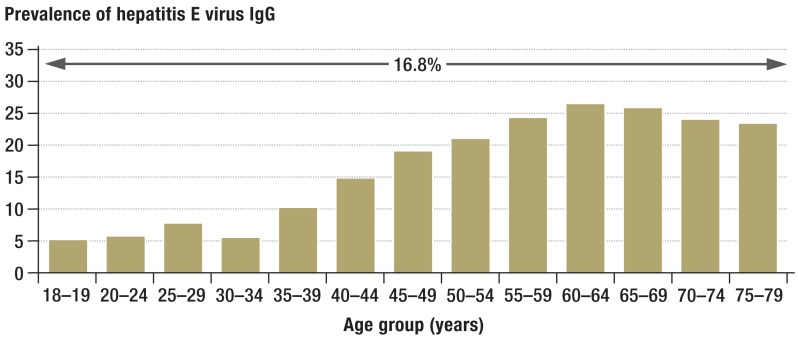
HEV infection was long thought to be rare in Germany. In the meantime, however, it has become clear that autochthonous HEV infections (i.e., infections acquired within Germany) are actually rather common. A recent study from the Robert Koch Institute found an anti-HEV prevalence of 16.8% in the adult German population (10) (Figure 3). We thus have to assume an annual rate of more than 100 000 infections, over 99% of which are clinically inapparent. Serologic studies on historic and current serum samples from Denmark (11), England (12), and Germany (6, e1) showed that the seroprevalence of anti-HEV in Europe has not increased in the past 20 years, but if anything decreased.
Figure 3.
Prevalence of anti-HEV antibodies by age group in Germany (detected by blot procedure [10])
Acute hepatitis E
In the immunocompetent, HEV infections are usually asymptomatic and have no consequences. Both a report of an outbreak of hepatitis E on a cruise ship and a large prospective vaccination study in China showed that fewer than 5% of those exposed to HEV develop signs of acute hepatitis E (1, 3, 13, 14). This is somewhat higher than the rate of 1% calculated for Germany and genotype 3. In children too, hepatitis E is very rarely symptomatic (1).
It has not yet been established why HEV infection is clinically inapparent in most cases and only a small proportion of persons have symptoms. If symptomatic hepatitis does develop, the first signs of illness are nonspecific—weakness, arthralgia, myalgia, or vomiting. These may be followed by symptoms more typical of hepatitis, such as jaundice, pruritus, colorless feces, and dark-colored urine. Clinical chemistry generally shows an increase in transaminases, more pronounced for ALT than for AST, as well as elevated bilirubin, alkaline phosphatase, and g-GT. The disease is generally self-limiting and harmless, but occasionally severe hepatitis E may progress to acute liver failure. Antiviral treatment is usually not necessary, but can be considered in individual cases of fulminant disease. Case reports have shown rapid normalization of liver synthesis and detoxification parameters in patients with acute hepatitis E following initiation of treatment with ribavirin (15, 16).
A fulminant course of hepatitis E is more frequent in pregnant women and patients with a previous history of liver disease (20 to 25%) (1, 3). In the former group, fulminant disease may be explained by increased expression of progesterone receptors or mutations in the MTHFR gene (17, 18). MTHFR (methylenetetrahydrofolate reductase) is an enzyme involved in numerous metabolic processes, and deficiency of MTHFR in pregnant women is associated with spina bifida. However, the precise role of MTHFR in the pathogenesis of hepatitis E has not yet been clarified (19).
Chronic hepatitis E
Since 2008 chronic hepatitis E has been repeatedly noted in immunosuppressed persons, organ transplant recipients, and HIV-positive patients (1). In the first such report, published in the New England Journal of Medicine, Kamar et al. described 14 cases of hepatitis E in recipients of kidney and liver transplants, in eight of whom the hepatitis did not resolve and became chronic (20).
A reduced HEV-specific T-cell response is associated with chronification of HEV infection. (21). Persisting viraemia can lead within a few years to liver cirrhosis with potentially life-threatening consequences; the natural course of the chronic liver inflammation seems to be more aggressive than in HBV and HCV infections (1). A retrospective analysis of 77 transplant recipients who acquired acute hepatitis E showed that the disease did not heal spontaneously in any of the patients who were viremic for more than 3 months (22). Therefore, persistence of the virus for more than 3 months seems to suffice as a definition for chronic hepatitis E (22). In a multicenter study, immune suppression with tacrolimus was associated with increased likelihood of chronification of hepatitis E (23). In contrast, administration of mycophenolate mofetil to heart transplant recipients was associated with a reduced risk of chronification (24). Indeed, it was recently shown that mycophenolate exerts an antiviral effect against HEV in vitro (25). The precise influence of various other immunosuppressants on HEV is being investigated in several ongoing studies. Ciclosporin and mTOR inhibitors, for example, seem to increase the replication of HEV (25, 26).
In several cohorts of transplant recipients in Europe, including stem cell transplants (e2, e3), chronic hepatitis E was found in around 1% of cases (24, 27– 29). In HIV patients, however, chronic HEV infection is much rarer and the risk is associated with the degree of immune deficiency (1).
Apart from a single report of a case involving HEV genotype 4 (30), chronification of HEV infections has been described exclusively for HEV genotype 3 (1). In contrast, HEV genotypes 1 and 2 do not seem to induce prolonged HEV viraemia. For example, chronic hepatitis E was found neither among 1 544 HIV-infected persons in Ghana and Cameroon (31) nor in 205 kidney transplant recipients in India (32).
Liver transplant recipients, lung transplant recipients, and persons infected with HIV are risk groups for chronification of HEV infection, but these groups‘ frequency of contact with the virus is no greater than that in the normal population. In contrast, a recent investigation showed that patients who had undergone heart surgery evinced much higher seroprevalence of anti-HEV antibodies (24). This was true not only for heart transplant recipients but also for patients treated with other cardiosurgical interventions. The reasons for this phenomenon have not yet been clarified, but may be connected with more frequent administration of blood and plasma products.
Extrahepatic manifestations
In both acute and chronic hepatitis E, involvement of organs other than the liver has been reported (Table 2), most commonly the nervous system and the kidney (1). The underlying mechanism has not been identified. Any viral infection can in principle induce autoimmune phenomena. It was recently shown that patients with autoimmune hepatitis display antibodies to HEV significantly more often than healthy controls (33). Whether this represents triggering of autoimmune hepatitis by HEV or mistaken diagnosis of autoimmune hepatitis remains to be clarified. A newly published case report describes symptomatic cryoglobulinemia in connection with hepatitis E (e4).
Table 2. Extrahepatic manifestations of hepatitis E.
| Disease | Remarks | Literature |
|---|---|---|
| Guillain-Barré syndrome (GBS) | Three of 201 GBS patients (1.5%) were viremic for HEV | van den Berg 2014 (5) |
| Neuralgic amyotrophy | Five of 47 patients (10.6%) were viremic for HEV | van Eijk 2014 (e10) |
| Glomerulonephritis | An accumulation of glomerulonephritides was observed in a cohort of 51 transplant recipients (liver or kidney) | Kamar 2012 (e11) |
| Meningitis, encephalitis, myopathy | Isolated cases | Kamar 2011 (e12) |
| Erythema and arthralgia | Single case report | Al-Shukri 2013 (4) |
| Cryoglobulinemia | Single case of cryoglobulinemic vasculitis in connection with chronic hepatitis E | Pischke 2014 (e4) |
HEV, hepatitis E virus
Diagnosis of hepatitis E
Every patient with hepatitis of uncertain origin should be investigated for signs of hepatitis E. There are both serologic and molecular genetic tests for HEV infection. None of these diagnostic procedures, however, has yet been licensed by the Food and Drug Administration (FDA) for use in the USA (1). In Germany both antibody tests and polymerase chain reaction (PCR)-based techniques for direct demonstration of HEV RNA are available. The PCR technique can be used on samples of blood or feces.
In patients who have chronic hepatitis E after receiving transplants, it may sometimes take months or even years before antibodies are produced to any measurable extent (27, 34). Therefore, suspicion of HEV infection in an immunosuppressed individual should always prompt direct investigation of HEV RNA by means of PCR. In the immunocompetent, on the other hand, widely available antibody tests are used, particularly because standardized PCR tests are not universally available and not all assays are optimized to various HEV genotypes. Improvements in molecular diagnosis can be anticipated in the next few years, because the World Health Organization (WHO) recently established an HEV standard that enables harmonization and comparability of PCR assays (35). Numerous international studies in the past few years have used a new serologic assay developed in China. This test yielded positive anti-HEV results much more frequently than other commercial assays (36, 37). Altogether, these studies show that earlier investigations often underestimated the seroprevalence of hepatitis E because of the insufficient sensitivity of the assays employed.
The diagnostic algorithm in suspicion of hepatitis E usually begins with testing for HEV antibodies. If the result is positive, the next step is determination of HEV RNA. Since antibody tests often yield false-negative results in immunosuppressed persons, PCR should be the primary diagnostic technique in this group of patents. Diagnostic confirmation of replicative HEV infection is important not only for establishing the cause of hepatitis of uncertain origin. Timely diagnosis is necessary so as to be able to give the patient the appropriate advice regarding hygiene, with the aim of preventing further infections. Finally, the confirmation of HEV replication can have direct therapeutic consequences, because the antiviral agent ribavirin has the potential to hinder progression of the disease.
Hepatitis E vaccination and antiviral treatment options
A vaccine for HEV that has been licensed in China since the beginning of 2012 has proved efficacious and safe in a large phase-III study embracing more than 100 000 probands (14). This study also showed that neither vaccine-induced anti-HEV antibodies nor those acquired in the context of a previous infection provide sterilizing immunity, although symptomatic hepatitis occurs much less often in anti-HEV-positive persons (38). It is not yet clear:
Whether this vaccine also protects against the European HEV genotype 3
When it will become commercially available in Europe
Whether it also offers secure protection to the risk group of transplant recipients.
A retrospective subgroup analysis of the data from the initial study (14) showed that this vaccine can be used safely and effectively to protect pregnant women (39).
Until recently no substances had been discovered that possess any significant antiviral activity against HEV. In 2010, however, the first case reports of a possible benefit of treatment with interferon-α or ribavirin were published (1). A retrospective single-center study from Germany with the largest number of patients worldwide up to that time then showed that ribavirin could represent a safe and efficient treatment for immunosuppressed persons with chronic hepatitis E (15). Ribavirin was also effective in an immunocompetent patient with severe acute hepatitis E, although the use of ribavirin in persons not in an immunosuppressed state is certainly indicated only in rare cases (15). A larger multicenter French study with 59 patients, published in the New England Journal of Medicine in March 2014, confirmed that ribavirin is effective against chronic hepatitis E in transplant recipients (16), although long-term elimination of the virus was not achieved in all patients. On the basis of the data from Germany and France, it seems advisable to administer ribavirin for at least 3 months in the attempt to eliminate chronic hepatitis E in immunosuppressed patients. If no HEV RNA negativity is achieved after 4 weeks, extension of the treatment period to at least 5 months should be considered. The dosage of ribavirin must be adjusted according to the individual patient‘s hemoglobin level and kidney function. The amount administered each day should not be below 600 mg because of the potential selection of HEV variants against which ribavirin has no sufficient action (15). It must be emphasized that no prospective standardized double-blind study of the efficacy of an antiviral substance against hepatitis E has yet been carried out.
Summary
Hepatitis E is a frequently under-reported infection. The number of cases reported to the Robert Koch Institute has increased more than tenfold since 2000. Only a minority of cases of hepatitis E in Germany are found in travelers; most infections are autochthonous with zoonotic transmission. Severe chronic disease has been described in immunosuppressed persons (Table 3). Furthermore, there are increasing signs that HEV infections may be associated with a broad spectrum of extrahepatic manifestations (Table 2). Hepatitis E should always be considered in patients with relevant symptoms.
Table 3. Studies on hepatitis E in Germany (not including case reports).
| Content | Literature |
|---|---|
| Sixty-six cases of acute hepatitis E in Germany (45 [68%] autochthonous, 21 [32%] associated with foreign travel), consumption of offal and wild boar meat risk factors for autochthonous hepatitis E | Wichmann 2008 (7) |
| Two hundred twenty-six liver transplant recipients, three patients viremic, two of them with chronic hepatitis E | Pischke 2010 (27) |
| One hundred twenty-three HIV patients, none of them chronically infected | Pischke 2010 (e13) |
| Demonstration of HEV RNA in 4% of commercially available pig livers | Wenzel 2011 (e14) |
| Twofold risk of anti-HEV positivity in persons with occupational contact with swine (compared with blood donors) | Krumbholz 2011 (e15) |
| Stable anti-HEV seroprevalence with simultaneous six-fold increase in number of reported cases of hepatitis E between 2001 and 2010 (2%; Abbott assay) | Pischke 2011 (6) |
| Up to 10% of the plasma pool for HEV testing contains HEV RNA (unclear what proportion infectious) | Baylis 2011 (e16) |
| No case of chronic hepatitis E in a cohort of 73 CVID patients | Pischke 2012 (e17) |
| One of 4525 units of donated plasma contains HEV RNA | Baylis 2012 (e18) |
| Heart transplant recipients are a risk group for contact with the hepatitis E virus; successful treatment with ribavirin is possible | Pischke 2012 (24) |
| Wide variation in anti-HEV seroprevalence rate among three assays (MP assay 4.5%, Mikrogen assay 18%, Wantai assay 30%) | Wenzel 2013 (36) |
| Ribavirin safe for treatment of acute and chronic hepatitis E, but usually not necessary in acute disease | Pischke 2013 (15) |
| Chronic hepatitis E also in lung transplant recipients; ribavirin as treatment option | Pischke 2014 (e19) |
| Much higher anti-HEV seroprevalence in patients with autoimmune hepatitis | Pischke 2014 (33) |
| Decrease in anti-HEV seroprevalence in southeastern Germany | Wenzel 2014 (e1) |
| Increased prevalence of anti-HEV antibodies in persons resident in areas with a high number of swine | Krumbholz 2014 (e20) |
HEV, hepatitis E virus; CVID, common variable immunodeficiency
Key Messages.
In Germany, hepatitis E is most commonly acquired by eating infected pork that has not been properly cooked.
Although hepatitis E virus (HEV) infection is asymptomatic and self-limiting in over 99% of cases, severe disease with liver failure does occur.
Immunosuppressed patients may suffer chronic HEV infection and liver cirrhosis can develop within a short time.
HEV infections have been associated with extrahepatic manifestations such as Guillain–Barré syndrome.
Ribavirin can be used as an antiviral agent in acute or chronic HEV infection.
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Prof. Jilg has received from Mikrogen payments for the preparation of scientific training courses and materials for a research project of his own conception.
Prof. Wedemeyer has received payments for consulting services from Abbott, Falk Foundation, Merck, Roche, Roche Diagnostics, and Siemens, as well as payments for his expert advice from Abbott, Roche, Roche Diagnostics, and Siemens.
Prof. Manns has received payments for consulting services from Abbott, Falk Foundation, Merck, and Roche.
PD Dr. Pischke has received payments for lectures from Falk Foundation, Merck, and Roche.
Prof. Bock and Dr. Behrendt declare that no conflict of interest exists.
References
- 1.Wedemeyer H, Pischke S, Manns MP. Pathogenesis and treatment of hepatitis E virus infection. Gastroenterology. 2012;142:1388–1397. doi: 10.1053/j.gastro.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention (CDC) Investigation of hepatitis E outbreak among refugees - Upper Nile, South Sudan, 2012-2013. MMWR Morb Mortal Wkly Rep. 2013;62:581–586. [PMC free article] [PubMed] [Google Scholar]
- 3.Rein DB, Stevens GA, Theaker J, Wittenborn JS, Wiersma ST. The global burden of hepatitis E virus genotypes 1 and 2 in 2005. Hepatology. 2011;55:988–997. doi: 10.1002/hep.25505. [DOI] [PubMed] [Google Scholar]
- 4.Al-Shukri> I, Davidson E, Tan A, et al. Rash and arthralgia caused by hepatitis E. Lancet. 2013;382 doi: 10.1016/S0140-6736(13)62074-7. [DOI] [PubMed] [Google Scholar]
- 5.van den Berg B, Annemick A, Van der Eijk A, et al. Guillain-Barré syndrome associated with preceding hepatitis E virus infection. Neurology. 2014 doi: 10.1212/WNL.0000000000000111. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 6.Pischke S, Heim A, Bremer B, et al. Hepatitis E: An emerging infectious disease in Germany? Z Gastroenterol. 2011;49:1255–1257. doi: 10.1055/s-0031-1273394. [DOI] [PubMed] [Google Scholar]
- 7.Wichmann O, Schimanski S, Koch J, et al. Phylogenetic and case-control study on hepatitis E virus infection in Germany. J Infect Dis. 2008;198:1732–1741. doi: 10.1086/593211. [DOI] [PubMed] [Google Scholar]
- 8.Hewitt PE, Ijaz S, Brailsford SR, et al. Hepatitis E virus in blood components: a prevalence and transmission study in southeast England. Lancet. 2014 doi: 10.1016/S0140-6736(14)61034-5. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Arbeitskreis Blut Untergruppe „Bewertung blutassoziierter Krankheitserreger“ Hepatitis E Virus. Transfus Med Hemother. 2009;36:40–47. [Google Scholar]
- 10.Faber MS, Wenzel JJ, Jilg W, et al. Hepatitis E virus seroprevalence among adults, Germany. Emerg Infect Dis. 2012;18:1654–1657. doi: 10.3201/eid1810.111756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christensen PB, Engle RE, Hjort C, et al. Time trend of the prevalence of hepatitis E antibodies among farmers and blood donors: a potential zoonosis in Denmark. Clin Infect Dis. 2008;47:1026–1031. doi: 10.1086/591970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ijaz S, Vyse AJ, Morgan D, et al. Indigenous hepatitis E virus infection in England: more common than it seems. J Clin Virol. 2009;44:272–276. doi: 10.1016/j.jcv.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 13.Said B, Ijaz S, Kafatos G, et al. Hepatitis E outbreak on cruise ship. Emerg Infect Dis. 2009;15:1738–1744. doi: 10.3201/eid1511.091094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu FC, Zhang J, Zhang XF, et al. Efficacy and safety of a recombinant hepatitis E vaccine in healthy adults: a large-scale, randomised, double-blind placebo-controlled, phase 3 trial. Lancet. 2010;376:895–902. doi: 10.1016/S0140-6736(10)61030-6. [DOI] [PubMed] [Google Scholar]
- 15.Pischke S, Hardtke S, Bode U, et al. Ribavirin treatment of acute and chronic hepatitis E: a single center experience. Liver International. 2013;33:722–726. doi: 10.1111/liv.12114. [DOI] [PubMed] [Google Scholar]
- 16.Kamar N, Izopet J, Tripon S, et al. Ribavirin for chronic hepatitis E virus infection in transplant recipients. N Engl J Med. 2014;370:1111–1120. doi: 10.1056/NEJMoa1215246. [DOI] [PubMed] [Google Scholar]
- 17.Bose PD, Das BC, Kumar A, et al. High viral load and deregulation of the progesterone receptor signaling pathway: Association with Hepatitis E-related poor pregnancy outcome. J Hepatol. 2011;54:1107–1113. doi: 10.1016/j.jhep.2010.08.037. [DOI] [PubMed] [Google Scholar]
- 18.Baruah B, Bose PD, Ray C, et al. Role of genetic alteration in MTHFR gene and homo-cysteine levles as critical factors influencing HEV related pregnancy outcome. Journal of Hepatology. 2012;56:32–33. [Google Scholar]
- 19.González Tallón AI, Moreira Vicente V, Mateos Lindemann ML, Achécar Justo LM. Chronic hepatitis E in an immunocompetent patient. Gastroenterol Hepatol. 2011;34:398–400. doi: 10.1016/j.gastrohep.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 20.Kamar N, Selves J, Mansuy JM, et al. Hepatitis E virus and chronic hepatitis in organ-transplant recipients. N Engl J Med. 2008;358:811–817. doi: 10.1056/NEJMoa0706992. [DOI] [PubMed] [Google Scholar]
- 21.Suneetha PV, Pischke S, Schlaphoff V, et al. Hepatitis E virus (HEV)-specific T-cell responses are associated with control of HEV infection. Hepatology. 2012;55:695–708. doi: 10.1002/hep.24738. [DOI] [PubMed] [Google Scholar]
- 22.Kamar N, Rostaing L, Legrand-Abravanel F, Izopet J. How should hepatitis e virus infection be defined in organ-transplant recipients? Am J Transplant. 2013;13:1935–1936. doi: 10.1111/ajt.12253. [DOI] [PubMed] [Google Scholar]
- 23.Kamar N, Garrouste C, Haagsma EB, et al. Factors associated with chronic hepatitis in patients with hepatitis e virus infection who have received solid organ transplants. Gastroenterology. 2011;140:1481–1489. doi: 10.1053/j.gastro.2011.02.050. [DOI] [PubMed] [Google Scholar]
- 24.Pischke S, Stiefel P, Franz B, et al. Chronic hepatitis e in heart transplant recipients. Am J Transplant. 2012;12:3128–3133. doi: 10.1111/j.1600-6143.2012.04200.x. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y, Zhou X, Debing Y, et al. Calcineurin inhibitors stimulate and mycophenolic acid inhibits replication of hepatitis E virus. Gastroenterology. 2014;146:1775–1783. doi: 10.1053/j.gastro.2014.02.036. [DOI] [PubMed] [Google Scholar]
- 26.Zhou X, Wang Y, Metselaar HJ, et al. Rapamycin and everolimus facilitate hepatitis E virus replication: Revealing a basal defense mechanism of PI3K-PKB-mTOR pathway. Journal of Hepatology. 2014 doi: 10.1016/j.jhep.2014.05.026. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 27.Pischke S, Suneetha PV, Baechlein C, et al. Hepatitis E virus infection as a cause of graft hepatitis in liver transplant recipients. Liver Transpl. 2010;16:74–82. doi: 10.1002/lt.21958. [DOI] [PubMed] [Google Scholar]
- 28.Haagsma EB, Niesters HG, van den Berg AP, et al. Prevalence of hepatitis E virus infection in liver transplant recipients. Liver Transpl. 2009;15:1225–1228. doi: 10.1002/lt.21819. [DOI] [PubMed] [Google Scholar]
- 29.Pas SD, de Man RA, Mulders C, et al. Hepatitis E virus infection among solid organ transplant recipients, the Netherlands. Emerg Infect Dis. 2012;18:869–872. doi: 10.3201/eid1805.111712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Geng Y, Zhang H, Huang W, et al. Persistent hepatitis e virus genotype 4 infection in a child with acute lymphoblastic leukemia. Hepat Mon. 2014;14 doi: 10.5812/hepatmon.15618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feldt T, Sarfo FS, Zoufaly A, et al. Hepatitis E virus infections in HIV-infected patients in Ghana and Cameroon. J Clin Virol. 2013;58:18–23. doi: 10.1016/j.jcv.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 32.Naik A, Gupta N, Goel D, et al. Lack of evidence of hepatitis E virus infection among renal transplant recipients in a disease-endemic area. J Viral Hepat. 2013;20:e138–e140. doi: 10.1111/jvh.12027. [DOI] [PubMed] [Google Scholar]
- 33.Pischke S, Gisa A, Suneetha PV, et al. Increased HEV seroprevalence in patients with autoimmune hepatitis. PLoS One. 2014;9 doi: 10.1371/journal.pone.0085330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Junge N, Pischke S, Baumann U, et al. Results of single-center screening for chronic hepatitis E in children after liver transplantation and report on successful treatment with ribavirin. Pediatr Transplant. 2013;17:343–347. doi: 10.1111/petr.12077. [DOI] [PubMed] [Google Scholar]
- 35.Baylis SA, Blumel J, Mizusawa S, et al. World Health Organization International Standard to harmonize assays for detection of hepatitis E virus RNA. Emerg Infect Dis. 2013;19:729–735. doi: 10.3201/eid1905.121845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wenzel JJ, Preiss J, Schemmerer M, Huber B, Jilg W. Test performance characteristics of Anti-HEV IgG assays strongly influence hepatitis E seroprevalence estimates. J Infect Dis. 2013;207:497–500. doi: 10.1093/infdis/jis688. [DOI] [PubMed] [Google Scholar]
- 37.Schnegg A, Burgisser P, Andre C, et al. An analysis of the benefit of using HEV genotype 3 antigens in detecting anti-HEV IgG in a European population. PLoS One. 2013;8 doi: 10.1371/journal.pone.0062980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang J, Zhang XF, Zhou C, et al. Protection against hepatitis E virus infection by naturally acquired and vaccine-induced immunity. Clin Microbiol Infect. 2013 doi: 10.1111/1469-0691.12419. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 39.Wu T, Zhu FC, Huang SJ, et al. Safety of the hepatitis E vaccine for pregnant women: a preliminary analysis. Hepatology. 2011;55 doi: 10.1002/hep.25522. [DOI] [PubMed] [Google Scholar]
- 40.Emerson SU, Purcell RH. Running like water-the omnipresence of hepatitis E. N Engl J Med. 2004;351:2367–2368. doi: 10.1056/NEJMp048285. [DOI] [PubMed] [Google Scholar]
- e1.Wenzel JJ, Sichler M, Schemmerer M, et al. Decline in hepatitis E virus antibody prevalence in Southeastern Germany, 1996-2011. Hepatology. 2014 doi: 10.1002/hep.27244. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- e2.le Coutre P, Meisel H, Hofmann J, et al. Reactivation of hepatitis E infection in a patient with acute lymphoplastic leucemia after allogenic stem cell transplantation. Gut. 2009;58:699–702. doi: 10.1136/gut.2008.165571. [DOI] [PubMed] [Google Scholar]
- e3.Versluis J, Pasch SD, Agteresch HJ, et al. Hepatitis e virus: an underestimated, opportunistic pathogen in recipientso of allogeneic hematopoietic stem cell transplantation. Blood. 2013, 122:1079–1086. doi: 10.1182/blood-2013-03-492363. [DOI] [PubMed] [Google Scholar]
- e4.Pischke S, Behrendt P, Manns MP, Wedemeyer H. HEV-associated cryoglobulinaemia and extrahepatic manifestations of hepatitis E. Lancet Infect Dis. 2014;8:678–679. doi: 10.1016/S1473-3099(14)70823-0. [DOI] [PubMed] [Google Scholar]
- e5.Banks M, Bendall R, Grierson S, et al. Human and porcine hepatitis E virus strains, United Kingdom. Emerg Infect Dis. 2004;10:953–955. doi: 10.3201/eid1005.030908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e6.Nelson KE. Transmission of hepatitis E virus by transfusion: what is the risk? Transfusion. 2014;54:8–10. doi: 10.1111/trf.12504. [DOI] [PubMed] [Google Scholar]
- e7.Halac U, Beland K, Lapierre P, et al. Chronic hepatitis E infection in children with liver transplantation. Gut. 2011;61:597–603. doi: 10.1136/gutjnl-2011-300708. [DOI] [PubMed] [Google Scholar]
- e8.Teshale EH, Grytdal SP, Howard C, et al. Evidence of person-to-person transmission of hepatitis E virus during a large outbreak in Northern Uganda. Clin Infect Dis. 2011;50:1006–1010. doi: 10.1086/651077. [DOI] [PubMed] [Google Scholar]
- e9.Schlosser B, Stein A, Neuhaus R, et al. Liver transplant from a donor with occult HEV infection induced chronic hepatitis and cirrhosis in the recipient. J Hepatol. 2011;56:500–502. doi: 10.1016/j.jhep.2011.06.021. [DOI] [PubMed] [Google Scholar]
- e10.van Eijk JJ, Madden RG, van der Eijk AA, et al. Neuralgic amyotrophy and hepatitis E virus infection. Neurology. 2014;82:498–503. doi: 10.1212/WNL.0000000000000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e11.Kamar N, Weclawiak H, Guilbeau-Frugier C, et al. Hepatitis E virus and the kidney in solid-organ transplant patients. Transplantation. 2012;93:617–623. doi: 10.1097/TP.0b013e318245f14c. [DOI] [PubMed] [Google Scholar]
- e12.Kamar N, Bendall RP, Peron JM, et al. Hepatitis E virus and neurologic disorders. Emerg Infect Dis. 2011;17:173–179. doi: 10.3201/eid1702.100856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e13.Pischke S, Ho H, Urbanek F, et al. Hepatitis E in HIV-positive patients in a low-endemic country. J Viral Hepat. 2010;17:598–599. doi: 10.1111/j.1365-2893.2009.01219.x. [DOI] [PubMed] [Google Scholar]
- e14.Wenzel JJ, Preiss J, Schemmerer M, et al. Detection of hepatitis E virus (HEV) from porcine livers in Southeastern Germany and high sequence homology to human HEV isolates. J Clin Virol. 2011;52:50–54. doi: 10.1016/j.jcv.2011.06.006. [DOI] [PubMed] [Google Scholar]
- e15.Krumbholz A, Mohn U, Lange J, et al. Prevalence of hepatitis E virus-specific antibodies in humans with occupational exposure to pigs. Med Microbiol Immunol. 2011;201:239–244. doi: 10.1007/s00430-011-0210-5. [DOI] [PubMed] [Google Scholar]
- e16.Baylis SA, Koc O, Nick S, Blumel J. Widespread distribution of hepatitis E virus in plasma fractionation pools. Vox Sang. 2011;102:182–183. doi: 10.1111/j.1423-0410.2011.01527.x. [DOI] [PubMed] [Google Scholar]
- e17.Pischke S, Horn-Wichmann R, Ernst D, et al. Absence of chronic hepatitis E in a German cohort of common variable immunodeficiency patients. Infect Dis Rep. 2012;4 doi: 10.4081/idr.2012.e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e18.Baylis SA, Gartner T, Nick S, Ovemyr J, Blumel J. Occurrence of hepatitis E virus RNA in plasma donations from Sweden, Germany and the United States. Vox Sang. 2012;103:89–90. doi: 10.1111/j.1423-0410.2011.01583.x. [DOI] [PubMed] [Google Scholar]
- e19.Pischke S, Greer M, Hardtke S, et al. Course and treatment of chronic hepatitis E virus infection in lung transplant recipients. Transpl Infect Dis. 2014;16:333–339. doi: 10.1111/tid.12183. [DOI] [PubMed] [Google Scholar]
- e20.Krumbholz A, Joel S, Dremsek P, et al. Seroprevalence of hepatitis E virus (HEV) in humans living in high pig density areas of Germany. Med Microbiol Immunol. 2014;203:273–282. doi: 10.1007/s00430-014-0336-3. [DOI] [PubMed] [Google Scholar]