Abstract
Background
The objective of this pilot study was to evaluate cartilage T1ρ and T2 relaxation times and knee mechanics during walking and drop-landing for individuals with anterior cruciate ligament reconstruction (ACL-R).
Methods
Nine patients (6 men and 3 women, Age 35.8±5.4 years, BMI 23.5±2.5 kg/m2) participated 1.5±0.8 years after single-bundle two-tunnel ACL reconstruction. Peak knee adduction moment (KAM), flexion moment (KFM), extension moment (KEM), and peak varus were calculated from kinematic and kinetic data obtained during walking and drop-landing tasks. T1ρ and T2 times were calculated for medial femur (MF), and medial tibia (MT) cartilage and compared between subjects with low KAM and high KAM. Biomechanical variables were compared between limbs.
Results
The high KAM group had higher T1ρ for MT (p = 0.01), central MT (p = 0.05), posterior MF (p = 0.04), posterior MT (p = 0.01); and higher T2 for MT (p = 0.02), MF (p = 0.05) posterior MF (p = 0.002) and posterior MT (p = 0.01). During walking, ACL-R knees had greater flexion at initial contact (p =0.04), and lower KEM (p = 0.02). During drop-landing, the ACL-R knees had lower KAM (p = 0.03) and KFM (p = 0.002).
Conclusion
Patients with ACL-R who have higher KAM during walking had elevated MR relaxation times in the medial knee compartments. These data suggest that those individuals who have undergone ACL-R and have higher frontal plane loading, may be at a greater risk of knee osteoarthritis.
Keywords: T1ρ, T2, gait, drop-landing, knee adduction moment
INTRODUCTION
Over 50% of individuals with an anterior cruciate ligament (ACL) injury and reconstruction develop post-traumatic osteoarthritis (PTOA).1–3 Multiple studies have shown that individuals with ACL-reconstruction (ACL-R) continue to demonstrate abnormal walking mechanics of the reconstructed knee when compared to the contralateral knee and compared to control subjects.4–6 It has been hypothesized that abnormal gait mechanics may contribute to altered cartilage loading and subsequent PTOA following an ACL-R.7 Specifically, higher external knee adduction moment (KAM) and dynamic knee varus during walking have been implicated in the pathogenesis of knee OA.8–11 These metrics, along with static varus deformity,12 are associated with an increase in frontal plane knee loading predisposing the medial knee cartilage to greater loading and subsequent degeneration.8, 13, 14 Furthermore, abnormal movement patterns for the reconstructed knee have also been demonstrated for other activities including running,4 stair climbing,5, 7 and drop landing.15–17 However, there are also studies that report no difference in KAM7 or lower KAM in the ACL-R knees. 5 Hence, it is possible that considerable variability in movement patterns exists post ACL-R between individuals. Those who have movement patterns characterized with high KAM may have greater risk of cartilage degeneration compared to those who do not have such movement patterns. Although, some recent work has shown an association between abnormal knee sagittal kinematics during walking, and cartilage morphology in individuals with ACL-R, 18 no studies have been performed to evaluate the relationship between frontal plane knee mechanics and early cartilage degeneration in individuals with ACL-R. Therefore, it is important to evaluate if cartilage composition post ACL-R is different between individuals who have high KAM vs. those who have low KAM.
Early changes in knee OA consist of loss of proteoglycans (PG) and increase in water content of the articular cartilage, along with loosening, disorganization and loss of collagen matrix 19. Loss of PG and collagen disruption hampers the load bearing ability of cartilage leading to further cartilage degeneration.19 These biochemical changes can be detected using non-invasive quantitative MR imaging techniques of T1ρ and T2 relaxation times which are sensitive to loss of PG and collagen disruption respectively, and are promising biomarkers of early disease 20–24. An increase in T1ρ and T2 relaxation times indicates loss of PG and disruption of collagen matrix, which is invisible to conventional radiography and morphologic MR imaging 20, 23–26. It has been shown that in people with ACL injuries, or knee OA, there is an increase in these MR relaxation times showing cartilage degeneration 20, 23–26.
Abnormal knee mechanics following an ACL-R, especially greater KAM, may be related to accelerated medial knee cartilage degeneration. However, association of these MR relaxation time parameters with frontal plane knee mechanics in individuals with ACL-R has not been performed. If abnormal frontal plane mechanics are associated with early cartilage degeneration in individuals with ACL-R, it may allow for development of early intervention programs targeted at training healthier movement patterns. Hence, the objective of this pilot study was to evaluate the articular cartilage T1ρ and T2 relaxation times, and knee mechanics during walking and drop-landing for individuals with ACL-R. Specifically, we evaluated the differences in medial articular cartilage global and sub-regional T1ρ and T2 relaxation times between individuals with high vs. low KAM during walking post ACL-R.
METHODS
Subjects
Nine patients (6 men and 3 women, Age 35.8±5.4 years, BMI 23.5±2.5 kg/m2) were referred by their orthopaedic surgeon 1.5±0.8 years after single-bundle two-tunnel ACL reconstruction. Six patients had isolated ACL repair with either posterior tibialis allograft (from cadaver) or hamstring autograft (from self), one patient had concurrent partial lateral meniscectomy with hamstring autograft, one patient had concurrent partial medial meniscectomy with posterior tibialis allograft and one patient had concurrent medial meniscus repair with posterior tibialis allograft. The study was performed in accordance with the rules of our institution’s Committee on Human Research. Informed consent was obtained from each patient after the nature of the study had been explained.
Motion Analysis
Three-dimensional kinematic data were collected at 250 Hz using a passive 10-camera system (VICON, Oxford Metrics, UK), and kinetic data were collected at 1000 Hz from two embedded force platforms (AMTI, Watertown, MA). Fourteen millimeter spherical retro-reflective markers were placed on bony landmarks of bilateral lower extremities for identification of joint centers and rigid clusters placed on the lateral surface of the subject's thighs, legs and heel shoe counters were used to track segment motions 27. Each subject performed a walking task and a drop jump task. For the walking task, patients were instructed to walk at a pace of 1.3±0.07 m/s. A trial was considered acceptable when there was clean foot-strike on any of the force platforms and the speed was within ± 5% of the defined speed. Three good trials were collected from both lower extremities. The drop jump task, as described by Pollard et al 28, involved the patient standing on a 30.5cm platform and stepping off with one foot landing on each of the force plates. The subjects were instructed to land with both feet contacting the ground simultaneously, and then immediately jump “as high as possible”. A successful trial was defined as one where the patient stepped off the platform (as opposed to jumping off or lowering themselves down), landed with both feet simultaneously with one foot on each force plate and immediately performed a maximal vertical jump. Three drop jump trials were collected.
Kinematic and kinetics were calculated using Visual3D (C-motion, Georgetown, MD). All net joint moments are expressed as external moments and normalized to body mass (Nm/kg). Variables were calculated for the stance phase when the foot was in contact with ground and included – peak KAM (early stance), peak external knee flexion moment (KFM) (early stance during walking, not present during drop-landing), peak external knee extension moment (KEM) (late stance during walking), and peak adduction angle (peak varus). 1st peak KAM (early stance) was selected to stratify the subjects into high-KAM and low-KAM groups because it has been shown to be related to progression of knee OA and medial cartilage and meniscus damage in earlier studies.9, 29, 30
MR Imaging
Imaging for the ACL-R knee was performed using a 3T GE Signa HDx MR Scanner (General Electric, Milwaukee, WI, USA) and an 8-channel phased-array knee coil (Invivo, Orlando, FL, USA) with the patient in a supine position. The imaging protocol included clinical T2-weighted FSE images (TR/TE=4300/51ms, FOV = 14cm, matrix=512x256, 2 mm slice thickness), sagittal 3D fat-saturated high-resolution spoiled gradient-echo (SPGR) images (TR/TE=15/6.7ms, FOV = 14cm, matrix =512x512, 1mm slice thickness) and 3D T1ρ/T2 quantification sequence developed previously in our lab31 (TR/TE=9.1/3.3ms, TSL: 0/10/40/80 msec, spin-lock frequency: 500Hz, FOV= 14cm, matrix=256x128, 4 mm slice thickness; for T2: preparation TE = 0/13.7/27.3/54.7 msec; total acquisition time = 9 min 30 sec).
Medial femoral condyle (MF), and medial tibia (MT) cartilage compartments were segmented on multiple slices semi-automatically in high resolution SPGR images using the in-house software developed with Matlab (Mathworks, Natick, MA, USA) based on edge detection and Bezier splines 32. These compartments were further divided into sub-regions as shown in Figure 1. T1ρ and T2 maps were reconstructed by fitting the T1ρ- and T2- weighted images pixel-by-pixel to the equations below using in-house developed software:
T1ρ and T2 maps were rigidly registered to SPGR images and cartilage contours generated from SPGR images after segmentation were overlaid to the registered T1ρ and T2 maps. Mean T1ρ and T2 values were calculated in defined regions. To reduce artifacts caused by partial volume effects with synovial fluid, pixels with relaxation time greater than 130 ms in T1ρ or 100 ms for T2 maps were removed from the data used for quantification.
Figure 1.
Statistical Analysis
Patients were divided into two groups using median peak KAM during walking: Group A) low KAM, and Group B) high KAM. Mean and standard deviation for all variables were calculated. Group comparisons were made using independent samples t-tests for MF and MT T1ρ and T2 relaxation time parameters. Paired t-tests were used to compare the sagittal plane metrics, peak KAM, peak varus angle during the walking and drop-landing tasks between the ACL-R and contralateral knees. All statistical analyses were done using SPSS (SPSS Inc. Chicago, IL) with one-tailed significance level set at p ≤ 0.05.
RESULTS
Motion Analysis
Frontal plane analyses showed no significant differences between the ACL-R and contralateral knees for peak KAM (Mean ± SD - ACL-R: 0.53±0.20 Nm/kg vs. contralateral: 0.58±0.19 Nm/kg, p = 0.12) and peak varus angle (Mean ± SD - ACL-R: 2.64±3.09 vs. contralateral: 2.86±2.86°, p = 0.39) during walking. Sagittal plane analyses showed that during walking, the ACL-R patients made initial contact with greater knee flexion (Mean ± SD - ACL-R: 4.3±4.3° vs. contralateral: 3.0±3.9°, p =0.04), had a lower peak external extension moment (Mean ± SD - ACL-R: −0.44±0.12 Nm/kg vs. contralateral: −0.50±0.11 Nm/kg, p = 0.02), and a close to significance lower peak external flexion moment (Mean ± SD - ACL-R: 0.44±0.11Nm/kg vs. contralateral: 0.53±0.20 Nm/kg, p = 0.06).
During drop-landing, the ACL-R knees had lower peak KAM Mean ± SD - (ACL-R: 0.23±0.18 vs. contralateral: 0.32±0.18 Nm/kg, p = 0.03) but the peak varus angle was no different (Mean ± SD - ACL-R: 5.0±7.5 vs. contralateral: 3.6±4.4°, p = 0.13). In the sagittal plane, the ACL-R knees had lower peak external knee flexion moment (Mean ± SD - ACL-R: 1.68±0.36 vs. contralateral: 2.12±0.40 Nm/kg, p = 0.002).
Medians for the peak KAM during walking was calculated to be 0.367 Nm/kg. Patients were stratified into those with KAM below the median (Group A: Low KAM, n = 5) and those with KAM greater than the median (Group B: High KAM, n = 4). (Table 1).
Table 1.
ACL-reconstructed patients grouped by knee biomechanics
| A: Low KAM (n = 5) |
B: High KAM (n =4) |
p-value | |
|---|---|---|---|
| Age | 29.0±17.0 | 36.9±2.2 | 0.20 |
| BMI | 22.7±1.7 | 24.4±3.3 | 0.17 |
| Peak KAM during walking (Nm/kg) | 0.30±0.05 | 0.54±0.12 | <0.01 |
MR Relaxation Times
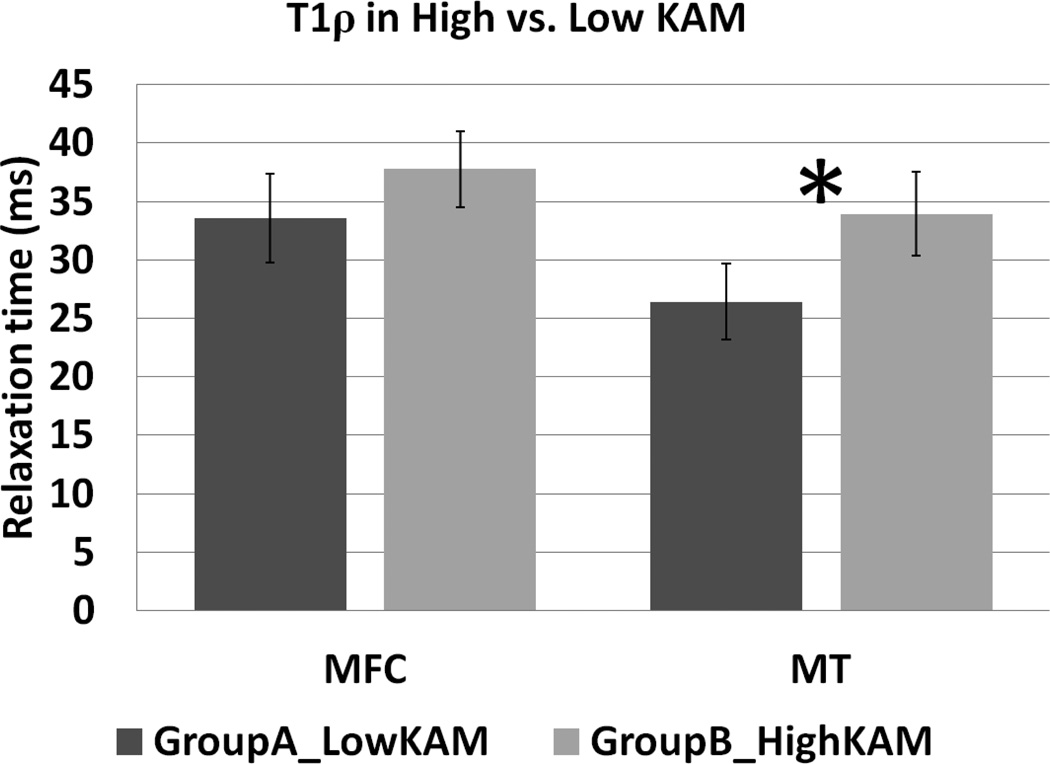
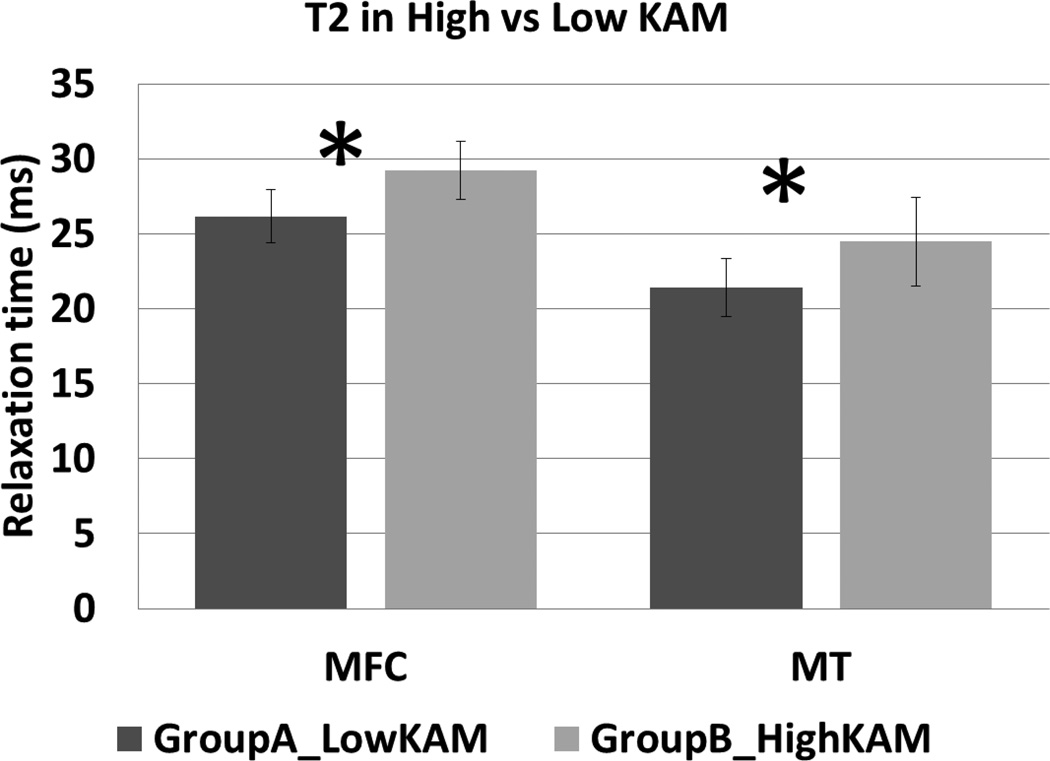
Table 2, and Figures 2–3 show that data for MR relaxation times for the two groups. On comparing the MR relaxation times for the reconstructed knee between the two groups, it was seen that Group B had higher T1ρ relaxation times for MT (p = 0.01, Figure 2) and for MF (p = 0.06, Figure 2) with a difference close to significance. Sub-compartment analyses (Table 2) showed that the Group B had higher T1ρ relaxation times for central MT (p = 0.05), posterior MF (p = 0.04), posterior MT (p = 0.01). For T2 relaxation times, Group B had higher values for MT (p = 0.02, Figure 3) and MF (p = 0.05). Sub-compartmental analyses (Table 2) showed higher T2 times for posterior MF (p = 0.002) and posterior MT (p = 0.01).
Table 2.
Mean ± Standard Deviation for Sub-compartment T1ρ and T2 relaxation times for the two groups.
| A: Low KAM (n = 5) |
B: High KAM (n = 4) |
p-value | ||
|---|---|---|---|---|
| T1ρ relaxation times (msec) | ||||
| Femur | cMF-a | 41.8±7.8 | 38.3±9.6 | 0.28 |
| cMF-c | 34.6±3.9 | 36.8±5.1 | 0.23 | |
| cMF-p | 29.8±6.1 | 35.3±8.5 | 0.15 | |
| pMF | 33.4±4.7 | 38.9±2.3 | 0.04 | |
| Tibia | MT-a | 30.6±7.1 | 28.9±6.2 | 0.36 |
| MT-c | 29.4±2.3 | 32.4±2.4 | 0.05 | |
| MT-p | 21.4±4.7 | 32.8±6.8 | 0.01 | |
| T2 relaxation times (msec) | ||||
| Femur | cMF-a | 31.1±5.3 | 29.1±6.3 | 0.31 |
| cMF-c | 28.1±2.6 | 26.9±4.5 | 0.32 | |
| cMF-p | 23.2±3.3 | 27.7±6.3 | 0.11 | |
| pMF | 25.4±0.9 | 30.4±2.6 | 0.002 | |
| Tibia | MT-a | 27.0±4.7 | 22.6±2.4 | 0.07 |
| MT-c | 23.3±4.2 | 25.5±2.6 | 0.20 | |
| MT-p | 19.0±1.8 | 26.4±4.9 | 0.01 | |
Figure 2.
Figure 3.
DISCUSSION
This goal of this pilot study was to explore the relationship between key frontal plane loading metrics which are known to be a risk factor for knee OA, and medial knee articular cartilage MR relaxation times, in individuals with ACL-R. The key finding from this study was that people with ACL-R who demonstrate high KAM show elevated articular cartilage MR relaxation times in the medial knee compartments compared to those with low KAM. KAM is a considered a surrogate measure of medial knee loading during functional activities 8, 13, 14. It has been shown to be a risk factor for progression of knee OA 9. Individuals with knee OA who have greater frontal plane loading have a higher rate of cartilage loss 29, increased incidence of medial knee cartilage lesions 33, and medial meniscus extrusion 30. Earlier work has also shown that KAM during drop-landing is related to medio-lateral T1ρ relaxation times ratio in young healthy adults 27. Hence, higher frontal plane loading and medial cartilage overload may lead to changes in medial knee cartilage composition as assessed using MR relaxation time parameters. Based on these data individuals with ACL-R who move with patterns that may lead to higher frontal plane loading may be at greater risk of PTOA. These individuals may benefit from a screening and targeted interventions to change these movement patterns and potentially prevent PTOA.
Current interventions for preventing the onset or progression of idiopathic knee OA or PTOA have been shown to be ineffective 34. People with ACL-R are at a particularly high risk of PTOA 2, 3. It has been hypothesized that abnormal gait mechanics may contribute to altered cartilage loading and subsequent PTOA following an ACL-R 7. Multiple studies have shown that individuals with ACL-reconstruction (ACL-R) continue to demonstrate abnormal walking mechanics of the reconstructed knee when compared to the contralateral knee and compared to control subjects 4–6. Higher KAM in the ACL-R knees compared to control knees has been reported 6, 35. However, other studies have reported no difference in KAM 7 or even lower KAM in the ACL-R knees 5. We also did not find a statistically significant difference in KAM between the ACL-R and contralateral knees. These results suggest that there may be significant variability in the movement patterns in individuals post ACL-R 35. This is supported by the observation of higher KAM in women with ACL-R compared to men with ACL-R 36. Hence future studies should consider studying sub-groups of individuals with ACL-R who demonstrate higher frontal plane loading longitudinally. This approach may allow for identification of risk factors specific to the sub-group that walks with greater frontal plane loading.
Earlier studies have also reported increased knee flexion at initial contact and lower sagittal plane moments in knees with ACL-R compared to contralateral or control knees 5, 18, 37. We also found higher knee flexion at initial contact and lower sagittal plane moments during walking. These sagittal plane patterns have been thought to be related to altered cartilage loading and subsequent degeneration. Greater knee flexion at initial contact was recently shown to be related with cartilage morphology 18. The authors found significant correlation between knee flexion angle at initial contact and region of thickest femoral cartilage. However, they did not find a significant difference in the region of thickest femoral cartilage between the ACL-R and contralateral knees even though the ACL-R knees landed with greater flexion. They concluded that in the ACL-R knees, thinner cartilage areas may experience higher loading, potentially leading to degeneration.
MR relaxation times allow for non-invasive and early detection of cartilage degeneration. An increase in T1ρ and T2 relaxation times indicates an increase in water, loss of proteoglycans and disruption of collagen matrix 20, 21, 23, 38–40. Numerous studies have shown that people with knee OA have higher T1ρ and T2 relaxation times compared to healthy control subjects 20, 21, 24. Earlier studies also report higher T1ρ and T2 relaxation times in ACL-R knees compared to the contralateral and control knees 41, 42. Cartilage composition as assessed using MR relaxation times could be related to the loading experience by the cartilage during daily activities. A recent study reported significant associations between sagittal, frontal, and transverse plane kinetics during hopping and drop-landing tasks, and T1ρ and T2 relaxation times 27. The results from this pilot study suggest that in individuals with ACL-R, higher frontal plane loading may be related to early cartilage degeneration, and MR relaxation times may be related to differences in movement patterns. Biomechanical studies have shown that following ACL-R the contact mechanics and contact area do not return to normal. 37, 43 The medial contact area was smaller following ACL-R at 0° and 15° of flexion compared to normal knees along with greater cartilage deformation.37 Also, the cartilage contact was located relatively more posteriorly and laterally on tibial plateaus in people with ACL-R during a weight-bearing knee flexion activity. Although, direct correlation between our data and these previous findings is not possible, our findings of higher MR relaxation times in central and posterior compartments could be related to these altered mechanics. However, future studies with larger samples and longer follow-up are needed to confirm these findings.
One major limitation of our study is the small number of patients. Also, our cohort was not homogenous in terms of the types of grafts, and concomitant injuries. Hence, the results need to be confirmed with larger samples. Also, we did not have information on the activity levels of these patients. It is plausible that amount of daily activity may be related to cartilage composition. This should be evaluated in future studies as well. KAM during walking could be affected by lower extremity alignment,12 angle of toe-out,44, 45, step width,46 and the type of shoes worn.47 The angle of toe-out and step-width were not different between the high KAM and low KAM groups in our cohort for both tasks (data not shown). However, we did not account for these and other variables in our analyses considering the preliminary nature of the work and future studies with larger samples and a control group are needed to investigate these associations. Finally, this study followed patients over an average period of 1.5 years following ACL-R. Considering the chronic nature of OA, longer follow-up is needed to evaluate these changes further.
To conclude, we found that people with ACL-R who have movement patterns characterized by higher KAM during walking had elevated MR relaxation times in the medial knee compartments. These data suggest that it may be possible that those individuals who have undergone ACL-R and have higher frontal plane loading, may be at a greater risk of PTOA. Hence, screening for these potentially harmful movement patterns may offer opportunities to develop targeted interventions for this subgroup of patients with ACL-R. Future studies with larger cohorts and longitudinal follow-up will be needed to confirm these preliminary findings.
Highlights.
9 patients 1.5 years following ACL reconstruction participated.
Evaluated medial knee cartilage MR relaxation times.
Evaluated the mechanics of walking and drop-landing.
High T1ρ and T2 in patients with high knee adduction moment during walking.
ACKNOWLEDGEMENTS
UCSF Dean’s Student Research Fellowship, K25 AR053633 and AR053633-S.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST
None of the authors report any conflicts of interest.
REFERENCES
- 1.Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med. 1999;27:143–156. doi: 10.2165/00007256-199927030-00001. [DOI] [PubMed] [Google Scholar]
- 2.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 3.Lohmander LS, Roos H. Knee ligament injury, surgery and osteoarthrosis. Truth or consequences? Acta Orthop Scand. 1994;65:605–609. doi: 10.3109/17453679408994613. [DOI] [PubMed] [Google Scholar]
- 4.Noehren B, Wilson H, Miller C, Lattermann C. Long-term gait deviations in anterior cruciate ligament-reconstructed females. Med Sci Sports Exerc. 2013;45:1340–1347. doi: 10.1249/MSS.0b013e318285c6b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zabala ME, Favre J, Scanlan SF, Donahue J, Andriacchi TP. Three-dimensional knee moments of ACL reconstructed and control subjects during gait, stair ascent, and stair descent. J Biomech. 2013;46:515–520. doi: 10.1016/j.jbiomech.2012.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Butler RJ, Minick KI, Ferber R, Underwood F. Gait mechanics after ACL reconstruction: implications for the early onset of knee osteoarthritis. Br J Sports Med. 2009;43:366–370. doi: 10.1136/bjsm.2008.052522. [DOI] [PubMed] [Google Scholar]
- 7.Hall M, Stevermer CA, Gillette JC. Gait analysis post anterior cruciate ligament reconstruction: knee osteoarthritis perspective. Gait Posture. 2012;36:56–60. doi: 10.1016/j.gaitpost.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Kumar D, Manal KT, Rudolph KS. Knee joint loading during gait in healthy controls and individuals with knee osteoarthritis. Osteoarthritis Cartilage. 2013;21:298–305. doi: 10.1016/j.joca.2012.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang A, Hochberg M, Song J, Dunlop D, Chmiel JS, Nevitt M, et al. Frequency of varus and valgus thrust and factors associated with thrust presence in persons with or at higher risk of developing knee osteoarthritis. Arthritis Rheum. 2010;62:1403–1411. doi: 10.1002/art.27377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang AH, Chmiel JS, Moisio KC, Almagor O, Zhang Y, Cahue S, et al. Varus thrust and knee frontal plane dynamic motion in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2013;21:1668–1673. doi: 10.1016/j.joca.2013.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Halder A, Kutzner I, Graichen F, Heinlein B, Beier A, Bergmann G. Influence of limb alignment on mediolateral loading in total knee replacement: in vivo measurements in five patients. The Journal of bone and joint surgery American volume. 2012;94:1023–1029. doi: 10.2106/JBJS.K.00927. [DOI] [PubMed] [Google Scholar]
- 13.Andriacchi TP, Mundermann A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr Opin Rheumatol. 2006;18:514–518. doi: 10.1097/01.bor.0000240365.16842.4e. [DOI] [PubMed] [Google Scholar]
- 14.Sharma L, Hurwitz DE, Thonar EJ, Sum JA, Lenz ME, Dunlop DD, et al. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum. 1998;41:1233–1240. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 15.Delahunt E, Sweeney L, Chawke M, Kelleher J, Murphy K, Patterson M, et al. Lower limb kinematic alterations during drop vertical jumps in female athletes who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012;30:72–78. doi: 10.1002/jor.21504. [DOI] [PubMed] [Google Scholar]
- 16.Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17:258–262. doi: 10.1097/JSM.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- 17.Tsai LC, McLean S, Colletti PM, Powers CM. Greater muscle co-contraction results in increased tibiofemoral compressive forces in females who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012;30:2007–2014. doi: 10.1002/jor.22176. [DOI] [PubMed] [Google Scholar]
- 18.Scanlan SF, Favre J, Andriacchi TP. The relationship between peak knee extension at heel-strike of walking and the location of thickest femoral cartilage in ACL reconstructed and healthy contralateral knees. J Biomech. 2013;46:849–854. doi: 10.1016/j.jbiomech.2012.12.026. [DOI] [PubMed] [Google Scholar]
- 19.Lohmander LS. Articular cartilage and osteoarthrosis. The role of molecular markers to monitor breakdown, repair and disease. J Anat. 1994;184(Pt 3):477–492. [PMC free article] [PubMed] [Google Scholar]
- 20.Li X, Benjamin Ma C, Link TM, Castillo DD, Blumenkrantz G, Lozano J, et al. In vivo T(1rho) and T(2) mapping of articular cartilage in osteoarthritis of the knee using 3 T MRI. Osteoarthritis Cartilage. 2007;15:789–797. doi: 10.1016/j.joca.2007.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mosher TJ, Dardzinski BJ. Cartilage MRI T2 relaxation time mapping: overview and applications. Semin Musculoskelet Radiol. 2004;8:355–368. doi: 10.1055/s-2004-861764. [DOI] [PubMed] [Google Scholar]
- 22.Xia Y. Relaxation anisotropy in cartilage by NMR microscopy (muMRI) at 14-microm resolution. Magn Reson Med. 1998;39:941–949. doi: 10.1002/mrm.1910390612. [DOI] [PubMed] [Google Scholar]
- 23.Akella SV, Regatte RR, Gougoutas AJ, Borthakur A, Shapiro EM, Kneeland JB, et al. Proteoglycan-induced changes in T1rho-relaxation of articular cartilage at 4T. Magn Reson Med. 2001;46:419–423. doi: 10.1002/mrm.1208. [DOI] [PubMed] [Google Scholar]
- 24.Regatte RR, Akella SV, Lonner JH, Kneeland JB, Reddy R. T1rho relaxation mapping in human osteoarthritis (OA) cartilage: comparison of T1rho with T2. J Magn Reson Imaging. 2006;23:547–553. doi: 10.1002/jmri.20536. [DOI] [PubMed] [Google Scholar]
- 25.Pulido L, Parvizi J. Femoroacetabular impingement. Semin Musculoskelet Radiol. 2007;11:66–72. doi: 10.1055/s-2007-984413. [DOI] [PubMed] [Google Scholar]
- 26.Rauscher I, Stahl R, Cheng J, Li X, Huber MB, Luke A, et al. Meniscal measurements of T1rho and T2 at MR imaging in healthy subjects and patients with osteoarthritis. Radiology. 2008;249:591–600. doi: 10.1148/radiol.2492071870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Souza RB, Fang C, Luke A, Wu S, Li X, Majumdar S. Relationship between knee kinetics during jumping tasks and knee articular cartilage MRI T1rho and T2 relaxation times. Clin Biomech (Bristol, Avon) 2012;27:403–408. doi: 10.1016/j.clinbiomech.2011.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pollard CD, Sigward SM, Ota S, Langford K, Powers CM. The influence of in-season injury prevention training on lower-extremity kinematics during landing in female soccer players. Clin J Sport Med. 2006;16:223–227. doi: 10.1097/00042752-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Bennell KL, Bowles KA, Wang Y, Cicuttini F, Davies-Tuck M, Hinman RS. Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann Rheum Dis. 2011;70:1770–1774. doi: 10.1136/ard.2010.147082. [DOI] [PubMed] [Google Scholar]
- 30.Vanwanseele B, Eckstein F, Smith RM, Lange AK, Foroughi N, Baker MK, et al. The relationship between knee adduction moment and cartilage and meniscus morphology in women with osteoarthritis. Osteoarthritis Cartilage. 2010;18:894–901. doi: 10.1016/j.joca.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 31.Li X, Wyatt C, Rivoire J, Han E, Chen W, Schooler J, et al. Simultaneous acquisition of T and T quantification in knee cartilage: Repeatability and diurnal variation. J Magn Reson Imaging. 2013 doi: 10.1002/jmri.24253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carballido-Gamio J, Bauer JS, Stahl R, Lee KY, Krause S, Link TM, et al. Inter-subject comparison of MRI knee cartilage thickness. Med Image Anal. 2008;12:120–135. doi: 10.1016/j.media.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Creaby MW, Wang Y, Bennell KL, Hinman RS, Metcalf BR, Bowles KA, et al. Dynamic knee loading is related to cartilage defects and tibial plateau bone area in medial knee osteoarthritis. Osteoarthritis Cartilage. 2010;18:1380–1385. doi: 10.1016/j.joca.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 34.Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18:476–499. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 35.Sanford BA, Zucker-Levin AR, Williams JL, Mihalko WM, Jacobs EL. Principal component analysis of knee kinematics and kinetics after anterior cruciate ligament reconstruction. Gait Posture. 2012;36:609–613. doi: 10.1016/j.gaitpost.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 36.Webster KE, McClelland JA, Palazzolo SE, Santamaria LJ, Feller JA. Gender differences in the knee adduction moment after anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2012;46:355–359. doi: 10.1136/bjsm.2010.080770. [DOI] [PubMed] [Google Scholar]
- 37.Hosseini A, Van de Velde S, Gill TJ, Li G. Tibiofemoral cartilage contact biomechanics in patients after reconstruction of a ruptured anterior cruciate ligament. J Orthop Res. 2012;30:1781–1788. doi: 10.1002/jor.22122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li X, Cheng J, Lin K, Saadat E, Bolbos RI, Jobke B, et al. Quantitative MRI using T1rho and T2 in human osteoarthritic cartilage specimens: correlation with biochemical measurements and histology. Magn Reson Imaging. 2011;29:324–334. doi: 10.1016/j.mri.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dunn TC, Lu Y, Jin H, Ries MD, Majumdar S. T2 relaxation time of cartilage at MR imaging: comparison with severity of knee osteoarthritis. Radiology. 2004;232:592–598. doi: 10.1148/radiol.2322030976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Menezes NM, Gray ML, Hartke JR, Burstein D. T2 and T1rho MRI in articular cartilage systems. Magn Reson Med. 2004;51:503–509. doi: 10.1002/mrm.10710. [DOI] [PubMed] [Google Scholar]
- 41.Li X, Kuo D, Theologis A, Carballido-Gamio J, Stehling C, Link TM, et al. Cartilage in anterior cruciate ligament-reconstructed knees: MR imaging T1{rho} and T2--initial experience with 1-year follow-up. Radiology. 2011;258:505–514. doi: 10.1148/radiol.10101006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Su F, Hilton JF, Nardo L, Wu S, Liang F, Link TM, et al. Cartilage morphology and T1rho and T2 quantification in ACL-reconstructed knees: a 2-year follow-up. Osteoarthritis Cartilage. 2013;21:1058–1067. doi: 10.1016/j.joca.2013.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carpenter RD, Majumdar S, Ma CB. Magnetic resonance imaging of 3-dimensional in vivo tibiofemoral kinematics in anterior cruciate ligament-reconstructed knees. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2009;25:760–766. doi: 10.1016/j.arthro.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 44.Guo M, Axe MJ, Manal K. The influence of foot progression angle on the knee adduction moment during walking and stair climbing in pain free individuals with knee osteoarthritis. Gait Posture. 2007;26:436–441. doi: 10.1016/j.gaitpost.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 45.Marcus-Harel T, Silverstone BZ, Seelenfreund M, Schurr D, Berson D. Retinal detachment with high myopia in the Rubinstein-Taybi syndrome. Metabolic, pediatric, and systemic ophthalmology. 1991;14:53–56. [PubMed] [Google Scholar]
- 46.Paquette MR, Zhang S, Milner CE, Klipple G. Does increasing step width alter knee biomechanics in medial compartment knee osteoarthritis patients during stair descent? The Knee. 2014;21:676–682. doi: 10.1016/j.knee.2014.02.020. [DOI] [PubMed] [Google Scholar]
- 47.Kutzner I, Stephan D, Dymke J, Bender A, Graichen F, Bergmann G. The influence of footwear on knee joint loading during walking--in vivo load measurements with instrumented knee implants. J Biomech. 2013;46:796–800. doi: 10.1016/j.jbiomech.2012.11.020. [DOI] [PubMed] [Google Scholar]