Abstract
Several options exist for the treatment of osteochondral lesions of the talus. Particulated juvenile cartilage allograft transplantation (PJCAT) has become a viable treatment modality for osteochondral lesions of the talus that are not amenable to microfracture or for which microfracture has failed. Arthroscopic placement of this type of graft obviates the need for osteotomy or plafondplasty and does not prevent additional procedures from being performed through an anterior approach. Special instrumentation and setup are not required to perform this procedure. Our arthroscopic technique for placement of particulated juvenile cartilage into osteochondral lesions of the talus is described. Case series and outcomes after arthroscopic ankle PJCAT are currently not reported within the literature; however, it is believed that the outcomes are at least similar to those of open ankle PJCAT.
The term “osteochondral lesion of the talus” (OLT) refers to any pathology of the talar articular cartilage and corresponding subchondral bone. OLTs present a treatment challenge due to the innate inability of cartilage to heal. Ideally, OLTs could intrinsically heal from cell migration from the surrounding cartilage. However, it is believed that in vivo chondrocyte migration is limited because of the rigidity of the extracellular matrix.1-3 Therefore modern options to treat OLTs typically use methods to deliver autologous or allogeneic cells. Marrow stimulation (microfracture) attempts to deliver bone marrow cells by penetrating the subchondral plate. However, the fibrocartilage formed from this procedure has been shown to be biomechanically weaker than native hyaline cartilage.4 Osteochondral autograft transplantation transfers viable chondrocytes with native extracellular matrix and subchondral bone from the patient's own femoral condyle or talus into the OLT; however, donor-site morbidity, poor interface integration, the need for perpendicular access through an osteotomy, and the idiosyncratic 3-dimensional geometry of talar shoulder OLTs limit the application of this technique.5,6 Autologous chondrocyte implantation and matrix-induced autologous chondrocyte implantation have been successful in forming hyaline-like cartilage,7 but widespread use is limited because of the technical and financial burden of chondrocyte expansion and the need for 2 procedures.6 Bulk fresh osteochondral allografts have also shown success in treating OLTs,8 but this treatment option is limited by donor availability, the possible need for osteotomy, geometric contour discrepancies, and the uncertainty of delivering viable chondrocytes after allograft processing and impaction.
Particulated juvenile cartilage allograft transplantation (PJCAT) involves transplantation of multiple fresh juvenile cartilage allograft tissue pieces, containing live cells within their native extracellular matrix. Fibrin adhesive is used to secure the cartilage pieces inside the lesion. Currently, the only graft material available for this procedure is DeNovo NT Natural Tissue Graft (Zimmer, Warsaw, IN). The cartilage pieces of this product are obtained, in compliance with good tissue practice, from donors ranging in age from newborn to 13 years; however, it is typically obtained from neomorts aged younger than 2 years.9 No stillborn or fetal tissue is used.
Arthroscopic Technique
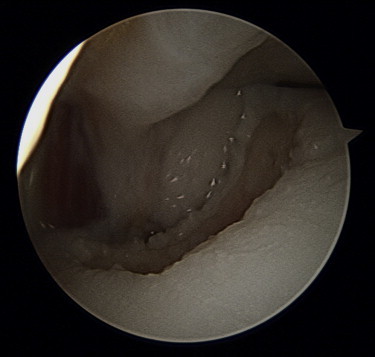
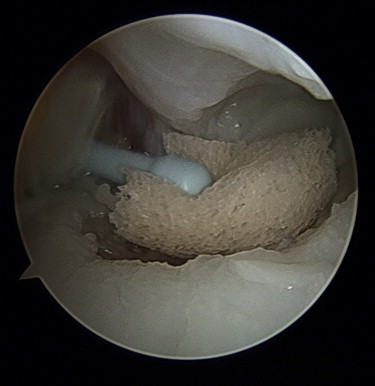
Routine anterior or posterior diagnostic ankle arthroscopy is performed. The synovium is debrided so as to prevent obstruction of the camera or passage of instruments. A probe is used to define the lesion (Fig 1, Video 1). The lesion is measured to ensure that there is adequate graft available. The lesion is then prepared with various cup and ring curettes (Fig 2). The cartilage is debrided back to a circumferential stable margin with vertical walls to contain the graft (Fig 3). Every attempt is made to leave a peripheral vertical wall for shoulder lesions.
Fig 1.
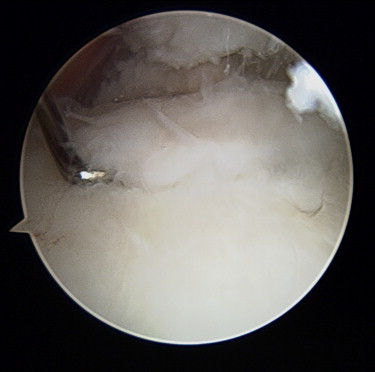
Right ankle with anterolateral OLT (viewed through medial portal).
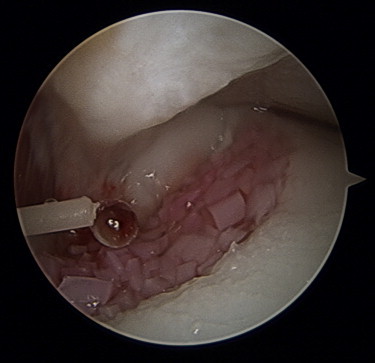
Fig 2.

Lesion preparation with ringed curette (viewed through medial portal). The curette is in the lateral portal.
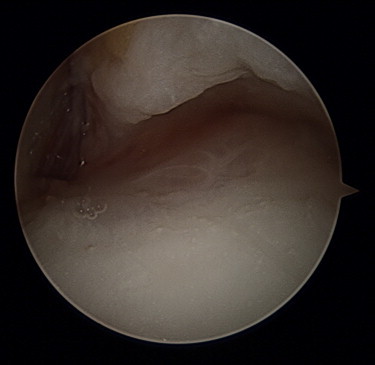
Fig 3.
Final lesion preparation (viewed through medial portal). Fluid has been evacuated from the joint. The distal fibula exposure, indicating that this is a shoulder lesion, should be noted.
The in-flow is temporarily shut off as graft delivery occurs in this setting. This allows the surgeon to assess for soft-tissue impingement at the working portal site that might interfere with graft insertion. The in-flow is restored for further soft-tissue debridement. The in-flow is again shut off, and the joint is evacuated with the use of a small suction catheter and an arthroscopic shaver. The lesion bed can be further dried with an epinephrine-soaked Weck-Cel sponge (Beaver Visitec, Waltham, MA) (Fig 4) or cotton-tipped applicator. Profuse bleeding at the base of the lesion can be addressed with a small amount of fibrin glue.
Fig 4.
Drying lesion base with Weck-Cel sponge (viewed through medial portal).
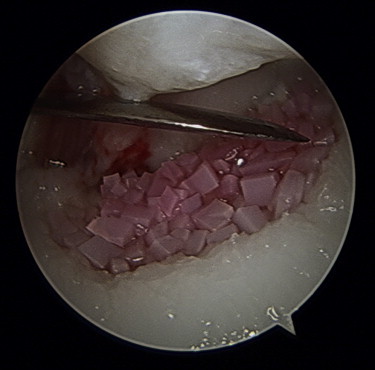
A 21-gauge, 1.5-inch needle and 5-mL syringe are used to aspirate the medium from the packaging of the De Novo NT Graft. One-half to one-third of the graft material is loaded in a retrograde fashion into the tip of a 2.7-mm arthroscopic cannula by use of a freer elevator and the cannula's corresponding trocar. The surgeon should not load all of the pieces at once. We routinely make 2 to 3 passes per package of DeNovo NT. The graft pieces are recessed into the cannula so that they are not exposed because they can become entrapped in soft tissue when introduced into the joint. The cannula, with the bevel down, is placed at the near edge of the lesion, and the pieces are slowly pushed into the lesion (Fig 5). The cannula is removed, and a freer or probe is inserted to distribute the graft uniformly throughout the lesion.
Fig 5.

Delivery of graft through lateral portal (viewed through medial portal). One should note that the bevel of the trocar is facing toward the lesion.
The fibrin glue tip is inserted through the arthroscopic portal, and a small amount of fibrin is applied (Fig 6). Occasionally, the tip provided with the fibrin glue is too short and an angiocatheter or its corresponding needle can be used. A freer elevator or probe is inserted to mold the pieces uniformly in the lesion (Fig 7) while the fibrin becomes more viscous. These steps should be repeated until the lesion is completely filled (Fig 8). The surgeon should allow the fibrin glue to set for 5 to 10 minutes until opaque (Fig 9).
Fig 6.

Application of fibrin to graft (viewed through medial portal).
Fig 7.
Graft distributed throughout lesion using a freer (viewed through medial portal).
Fig 8.
Additional fibrin is added once all the DeNovo graft has been implanted (viewed through medial portal).
Fig 9.
Final view of grafted defect (viewed through medial portal).
If cancellous bone graft is needed at the base of the lesion, it can be applied in the same manner as described for cartilage graft insertion. Bone graft can be obtained from the calcaneus with a trephine.
The arthroscopic portals are closed with nylon, and a well-padded splint is placed with the ankle in a position to fully contain the lesion under the tibial plafond.
Postoperative Management
The patient is kept in the splint, with no weight bearing, for 10 to 14 days. The sutures are removed at that point, and the patient is placed in a removable boot. The patient remains non–weight bearing except for range-of-motion exercises. A night splint should be used to keep the lesion contained while the patient is asleep. At 6 weeks postoperatively, the patient may progress to full weight bearing. The boot can be removed between weeks 6 and 12, and a lace-up ankle brace can be worn. Full range of motion is allowed during this time provided that there is no contraindication based on concomitant procedures performed. Physical therapy, strengthening exercises, stationary bicycling, and water activities may be initiated at 6 weeks. Impact activities are not started until 6 months.
Discussion
The advantages of the arthroscopic PJCAT technique are as follows: It is a technically simple procedure without the need for graft contouring (as is needed for osteochondral autograft or allograft transplantation), it does not require perpendicular access in the form of osteotomy or plafondplasty (as is often needed for osteochondral autograft/allograft transfer), it is a single-stage procedure, and there is no donor-site morbidity. By foregoing a medial or lateral arthrotomy, it does not preclude a subsequent midline approach for hemi-talus allograft or ankle arthroplasty. The disadvantages of this technique are the fact that it is a relatively new procedure with limited patient data; there is a limited supply of juvenile donor cartilage; it is a relatively expensive treatment option compared with other techniques; and as with any allograft tissue, disease transmission concerns exist.
Case series of open ankle PJCAT show promising results10,11; however, there are few reports in the literature on arthroscopic ankle PJCAT. Recently, Coetzee et al.12 presented a retrospective case series of 23 patients (24 ankles) treated with PJCAT at a mean follow-up of 16.2 months. Only 3 ankles in this cohort were managed in all-arthroscopic manner. No subgroup analysis was performed. The mean lesion surface size was 125 mm2 (range, 50 to 300 mm2), with a mean depth of 7 mm (range, 3 to 20 mm). Bone grafting was performed on lesions deeper than 5 mm. The mean postoperative 100-mm visual analog scale score for pain was 24 (range, 0 to 93), and the mean American Orthopaedic Foot & Ankle Society ankle-hindfoot score was 85 (range, 23 to 100). The mean Foot and Ankle Ability Measure for activities of daily living was 55.1 (range, 52 to 58), and the mean Foot and Ankle Ability Measure for sports was 63.4 (range, 52 to 75). The mean postoperative Short Form 12 physical composite score was 46.4 (range, 42 to 51). These outcomes scores are similar to published reports on patients who were treated with bone marrow stimulation, autologous chondrocyte implantation, and matrix-induced autologous chondrocyte implantation. Five patients required reoperation to remove symptomatic osteotomy hardware.
Kruse et al.13 presented 1 case of arthroscopically performed PJCAT for an OLT in a 30-year-old woman with a full-thickness posteromedial lesion that measured 7 mm × 5 mm. At 2 years after surgery, the patient was found to be pain free with no activity limitations.
When one is treating recalcitrant OLTs, diagnostic arthroscopy is often performed before definitive treatment. Proceeding with arthroscopic ankle PJCAT is a simple, effective technique for the delivery of graft into the lesion without special instrumentation. In addition, arthroscopic treatment does not require the use of osteotomy or plafondplasty. Portal incisions do not preclude further procedures about the anterior ankle. There are several key points to ensure that the procedure is performed in a smooth fashion (Table 1). The results of open ankle PJCAT are similar to those of other cartilage procedures in the ankle, and although we suspect at least similar results with arthroscopic ankle PJCAT, further research is needed.
Table 1.
Key Points
| 1. Ensure that enough anterior synovium is removed so that it does not impede graft passage during dry arthroscopy. |
| 2. Use a combination of suction and epinephrine-soaked Weck-Cel sponge to thoroughly dry the joint. |
| 3. Do not load the entire contents of the graft into the empty trocar. It is easier to accurately place and mold a smaller amount of graft into the joint as opposed to the entire contents of 1 package. |
| 4. Maximum plantar flexion of the ankle or noninvasive distraction is a useful technique to allow access to mid-body and posterior talar lesions. |
| 5. Have additional angiocatheters available for fibrin glue placement because these often become clogged. |
| 6. Ensure that the fibrin over the graft does not adhere to the anterior soft tissue or adjacent malleoli. |
Footnotes
The authors report the following potential conflict of interest or source of funding: S.B.A. receives support from Medshape, Regeneration Technologies Inc, Stryker, Harvest Terumo. S.G.P. receives support from Stryker, Solana, Integra, Nextremity, Biomet, Pacira, Orthohelix.
Supplementary Data
(1) Right ankle with anterolateral OLT, viewing from anteromedial portal. The lesion is defined with a nasal curette. (2) Preparation of the lesion is performed with a curette and shaver. (3) At the back table, the DeNovo NT suspension medium is aspirated from the packaging. (4) The DeNovo NT graft is loaded into an empty 2.7-mm cannula. (5) The graft is introduced into the ankle and delivered to the lesion, followed by application of fibrin. (6) The graft and fibrin are molded with a freer.
References
- 1.Giurea A., DiMicco M.A., Akeson W.H., Sah R.L. Development-associated differences in integrative cartilage repair: Roles of biosynthesis and matrix. J Orthop Res. 2002;20:1274–1281. doi: 10.1016/S0736-0266(02)00084-0. [DOI] [PubMed] [Google Scholar]
- 2.Hunziker E.B., Kapfinger E., Müller M.E. Removal of proteoglycans from the surface of defects in articular cartilage transiently enhances coverage by repair cells. J Bone Joint Surg Br. 1998;80:144–150. doi: 10.1302/0301-620x.80b1.7531. [DOI] [PubMed] [Google Scholar]
- 3.Qiu W., Murray M.M., Shortkroff S., Lee C.R., Martin S.D., Spector M. Outgrowth of chondrocytes from human articular cartilage explants and expression of α-smooth muscle actin. Wound Repair Regen. 2000;8:383–391. doi: 10.1111/j.1524-475x.2000.00383.x. [DOI] [PubMed] [Google Scholar]
- 4.Nehrer S., Spector M., Minas T. Histologic analysis of tissue after failed cartilage repair procedures. Clin Orthop Relat Res. 1999;365:149–162. doi: 10.1097/00003086-199908000-00020. [DOI] [PubMed] [Google Scholar]
- 5.McGahan P.J., Pinney S.J. Current concept review: Osteochondral lesions of the talus. Foot Ankle Int. 2010;31:90–101. doi: 10.3113/FAI.2010.0090. [DOI] [PubMed] [Google Scholar]
- 6.Lu Y., Dhanaraj S., Wang Z. Minced cartilage without cell culture serves as an effective intraoperative cell source for cartilage repair. J Orthop Res. 2006;24:1261–1270. doi: 10.1002/jor.20135. [DOI] [PubMed] [Google Scholar]
- 7.Peterson L., Minas T., Brittberg M., Nilsson A., Sjögren-Jansson E., Lindahl A. Two-to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop Relat Res. 2000;374:212–234. doi: 10.1097/00003086-200005000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Adams S.B. Midterm results of osteochondral lesions of the talar shoulder treated with fresh osteochondral allograft transplantation. J Bone Joint Surg Am. 2011;93:648–654. doi: 10.2106/JBJS.J.00141. [DOI] [PubMed] [Google Scholar]
- 9.Adams S.B., Jr., Yao J.Q., Schon L.C. Particulated juvenile articular cartilage allograft transplantation for osteochondral lesions of the talus. Tech Foot Ankle Surg. 2011;10:92–98. doi: 10.1016/j.fcl.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Schon L.C. 2013. Particulated juvenile cartilage allograft for treatment of osteochondral lesions in the ankle: The Medstar Union Memorial Hospital experience. Presented at the American Orthopaedic Foot and Ankle Society Annual Meeting, Hollywood, FL, July. [Google Scholar]
- 11.Bleazey S., Brigido S.A. Reconstruction of complex osteochondral lesions of the talus with cylindrical sponge allograft and particulate juvenile cartilage graft provisional results with a short-term follow-up. Foot Ankle Spec. 2012;5:300–305. doi: 10.1177/1938640012457937. [DOI] [PubMed] [Google Scholar]
- 12.Coetzee J.C., Giza E., Schon L.C. Treatment of osteochondral lesions of the talus with particulated juvenile cartilage. Foot Ankle Int. 2013;34:1205–1211. doi: 10.1177/1071100713485739. [DOI] [PubMed] [Google Scholar]
- 13.Kruse D.L., Ng A., Paden M., Stone P.A. Arthroscopic De Novo NT juvenile allograft cartilage implantation in the talus: A case presentation. J Foot Ankle Surg. 2012;51:218–221. doi: 10.1053/j.jfas.2011.10.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(1) Right ankle with anterolateral OLT, viewing from anteromedial portal. The lesion is defined with a nasal curette. (2) Preparation of the lesion is performed with a curette and shaver. (3) At the back table, the DeNovo NT suspension medium is aspirated from the packaging. (4) The DeNovo NT graft is loaded into an empty 2.7-mm cannula. (5) The graft is introduced into the ankle and delivered to the lesion, followed by application of fibrin. (6) The graft and fibrin are molded with a freer.


