Abstract
High tibial valgus osteotomy (HTO) is an established treatment for medial-compartment osteoarthritis of the knee. We have combined medial open and lateral closed-wedge HTO (hybrid closed-wedge HTO) to overcome the limitations of traditional closed-wedge HTO. Our new hybrid procedure has the following advantages: (1) the bone block removed is smaller in size; (2) the procedure yields optimal geometric characteristics for bone healing; (3) there is no step-off at the lateral osteotomy site; (4) the lateral cortex of the proximal and distal fragments is attached firmly by the oblique osteotomy; and (5) early full weight-bearing walking is possible. This procedure is effective in treating medial-compartment osteoarthritis accompanied by patellofemoral osteoarthritis. The indications for this procedure include a willingness and ability to comply with the postoperative rehabilitation program; a diagnosis of either medial-compartment osteoarthritis or complicated patellofemoral osteoarthritis; and preferably, an age of 70 years or younger, although this is not a strict constraint. Patients are permitted to stand using both legs on the day after surgery and walk with full weight bearing within 2 weeks of undergoing our novel HTO procedure. We describe the details of this surgical technique and the postoperative rehabilitation program for the patients who undergo this treatment.
High tibial valgus osteotomy (HTO) is an established surgical procedure to correct varus malalignment in patients with medial-compartment osteoarthritis (OA) of the knee.1,2 There are 2 main types of HTO surgery: lateral closed-wedge high tibial valgus osteotomy (CWHTO)3 and medial open-wedge high tibial valgus osteotomy (OWHTO).4 At present, an increasing number of surgeons use OWHTO because it is comparatively simpler. OWHTO is most effective during the early or middle stages of knee OA but is not expected to have a beneficial impact if the knee OA is accompanied by a severe deformity or in cases of patellofemoral joint OA.
There are several disadvantages to traditional CWHTO including lateral-offset increases due to horizontal osteotomy and loss of the large bone block below the lateral tibial plateau. Discrepancies in the leg length arise after CWHTO because the operative side is shortened.5,6 It also takes a relatively long time to achieve bone union at the osteotomy site after CWHTO because of discrepancies between the area on the proximal and distal fragments. This creates difficulties in maintaining alignment until bone union is acquired. Full weight bearing is also difficult until the osteotomy site is united, and a long leg cast or knee brace is thus needed for CWHTO patients.
Optimal postoperative rehabilitation after knee surgery is needed to enable walking with full weight without any support as soon as possible. This, in turn, will prevent the aggravation of osteoporosis, the deterioration of physical function, and the onset of deep vein thrombosis after surgery. We describe a new surgical procedure combining OWHTO and CWHTO (which we call a hybrid closed-wedge technique) that involves simple surgical techniques and facilitates full weight-bearing walking within 2 weeks after surgery without support other than perhaps a small cane (Table 1). Moreover, a good range of motion of the operated knee is acquired within a few days of this hybrid procedure.
Table 1.
Tips, Pearls, Pitfalls, Key Points, and Risks
| Tips |
| Patient can walk with full weight bearing within 2 wk after surgery |
| Pearls |
| Removed bone block size is smaller |
| Optimal geometric characteristics for bone healing |
| No step-off at lateral osteotomy site |
| Pitfalls |
| Precise preoperative planning |
| Key points |
| Lateral cortex of proximal and distal fragments are attached firmly by oblique osteotomy |
| Risks |
| Peroneal nerve palsy |
| Compartment syndrome |
Indications for Hybrid CWHTO Procedure
The inclusion criteria for our hybrid CWHTO procedure are as follows: (1) the patient has a willingness and ability to comply with the postoperative rehabilitation program; (2) the patient has a diagnosis of either medial-compartment OA or patellofemoral OA complication, especially a standing lateral angle between the femoral axis and tibial axis of more than 185°; and (3) an age of 70 years or younger is desirable for this procedure, although this is not a strict exclusion criterion at our hospital. The exclusion criteria are (1) both medial- and lateral-compartment OA of the knee, (2) infection of the knee, (3) acute or chronic osteomyelitis of the tibia, (4) severe OA with an Ahlbäck classification of grade 5,7 (5) a flexion contracture of over 30° and maximum flexion of less than 100°, and (6) patients who smoke.
Preoperative Planning
Because our hybrid CWHTO procedure provides greater correction of knee deformity with the removal of smaller wedges and release of medial soft-tissue tension because of a varus deformity increase, the site of osteotomy becomes stable. Moreover, the tibial fragments are fixed with a rigid locking compression plate (LCP) system. For the procedure, a proximal-lateral tibial plate (5 distal screw holes; Synthes, Solothurn, Switzerland) should be selected. This plate was developed for proximal tibial fracture repair, and plate bending is therefore necessary during presurgical planning.
It is vital to confirm the condition of the lateral meniscus and cartilage with magnetic resonance imaging before surgery. Surgical planning is important for an osteotomy. During planning, we obtained a radiograph of the anteroposterior view of the whole leg in the standing position, from which a tracing can be obtained (Fig 1A). Hybrid CWHTO is performed using this radiographic image of the leg as the postoperative weight-bearing line (WBL) passes through 63% laterally from the medial edge of the tibial plateau (Fig 1B). The WBL is detected by drawing a line from the center of the femoral head to the middle point of the proximal talar joint surface (broken line). The WBL ratio is calculated as the horizontal distance from the WBL to the medial edge of the tibial plateau (d), divided by the width of the tibial plateau (W): WBL ratio = d/W × 100%.
Fig 1.
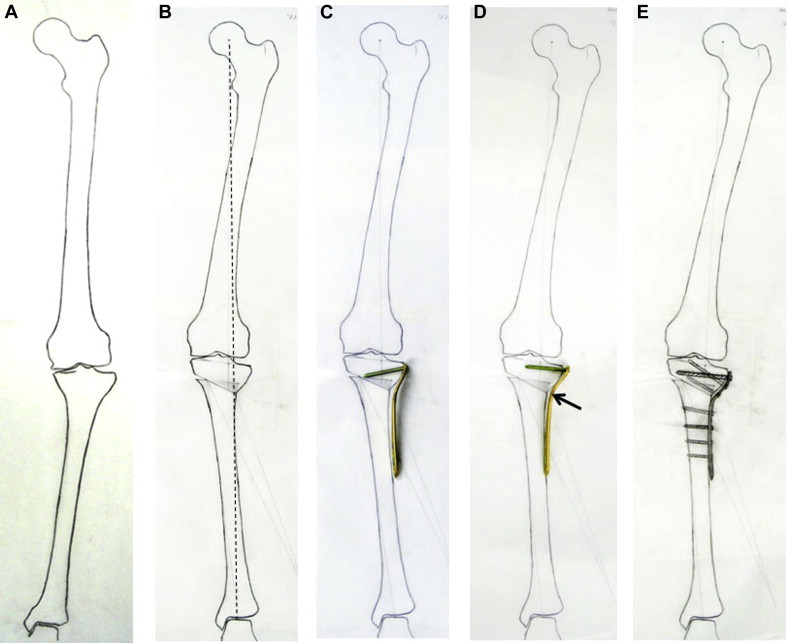
Preoperative planning in a left leg. (A) Preoperative tracing of anteroposterior view of entire leg in standing position from a radiograph. (B) Postoperative tracing of leg. (C) A lateral proximal tibial plate is developed for a tibial plateau fracture. The proximal screw directions are thus corrected according to the postoperative image. (D) Bending of the plate at the neck (arrow) is performed until the direction of the proximal screw is almost parallel to the tibial plateau. (E) Postoperative image of leg fixed with plate and screws.
Plate bending is needed until the insertion direction of the proximal screws becomes parallel to the tibial plateau (Figs 1C and 1D). Finally, an image of the leg and plate is obtained after surgery (Fig 1E).
Technique
The patient is placed in the supine position and the knee is positioned straight during surgery (Video 1). The lead surgeon stands on the lateral side of the patient, and the fluoroscopy unit is positioned on the medial side of the patient. Initial knee arthroscopy is performed in every patient in parallel with HTO surgery. After debridement of the degenerated meniscus and the cartilage on the joint surface, the large osteophytes of the medial femoral condyle or intercondylar space are removed. In cases of OA of the patellofemoral joint, lateral release of the lateral joint capsule and retinaculum is performed.
Before tibial osteotomy, the fibula undergoes osteotomy at its mid portion, and segmental resection is performed to remove a sufficient length of bone to enable tibial correction through a separate incision. The midportion osteotomy of the fibula is performed to avoid peroneal nerve palsy.
The operation is performed using the extension position of the knee. A 6-cm longitudinal lateral skin incision is first made on the anterior aspect of the knee at the lateral side of the tibial tuberosity. The retinaculum is then cut from the distal portion of the patella to the tibial tuberosity on the lateral side of the patellar ligament. The line of retinacular release is elongated, and the proximal part of the tibialis anterior muscle and periosteum at the osteotomy site of the tibia are elevated laterally with subperiosteal elevation of the iliotibial tract insertion (Gerdy tubercle). The posterior periosteum and soft tissue are released according to the osteotomy site. The knee is kept in a full-extension position during surgery (Figs 2A and 3A). Under fluoroscopy, the first Kirschner wire (2 mm in diameter) is inserted at a position 35 mm distally to the lateral proximal tibial joint surface (Figs 2B and 3B) to the medial target position (about 15 mm distally to the medial proximal tibial joint surface; this point is in the distal portion of the medial collateral ligament [MCL] deep layer attachment site) horizontally to the operating table. This is the proximal tibial osteotomy line. The proximal second Kirschner wire insertion point is posterior to the first Kirschner wire, perpendicular to the operating table and parallel to the first wire. The hinge point, which divides the proximal tibial osteotomy line by about 2 to 1, is then determined. A Kirschner wire is inserted at this hinge point from anterior to posterior percutaneously (Figs 2C and 3C). A special goniometer for CWHTO (Mizuho, Tokyo, Japan) is then set at this Kirschner wire inserted to the hinge point (Figs 2D and 4).
Fig 2.
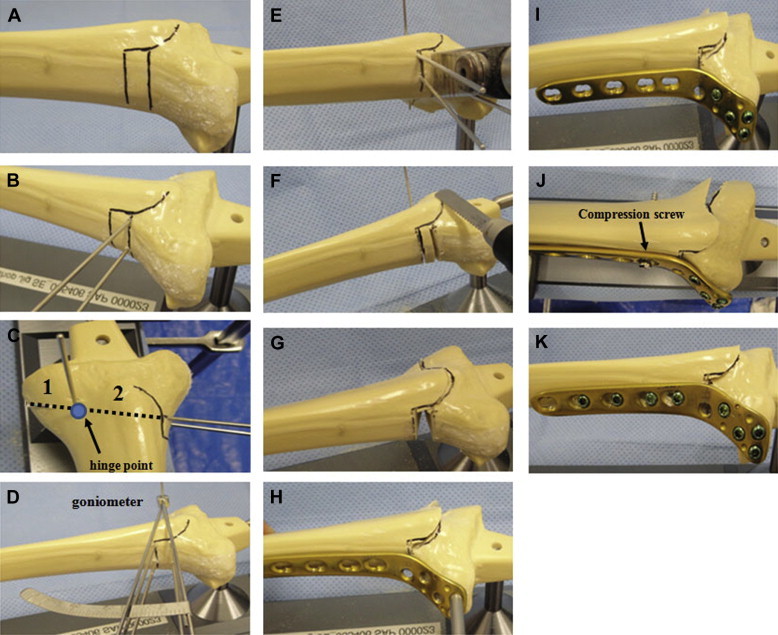
Hybrid CWHTO surgical process using a bone saw. (A) The black lines indicate the osteotomy lines. (B) Proximal Kirschner wires are inserted from lateral to medial obliquely to the tibial shaft. (C) A hinge point divides the proximal osteotomy line by about 2 to 1 from lateral to medial. (D) A special goniometer is set at the hinge point, and the distal osteotomy line is determined. (E) Osteotomy is commenced with a bone saw. (F) Biplanar osteotomy. (G) The bone block is removed and the osteotomy completed. (H) The proximal screw direction is determined in accordance with the preoperative planning. (I) The proximal part of the plate is fixed with 4 locking screws. (J) A distal fragment is attached to the plate using a compression screw technique. (K) The plate is typically fixed with 8 locking screws.
Fig 3.
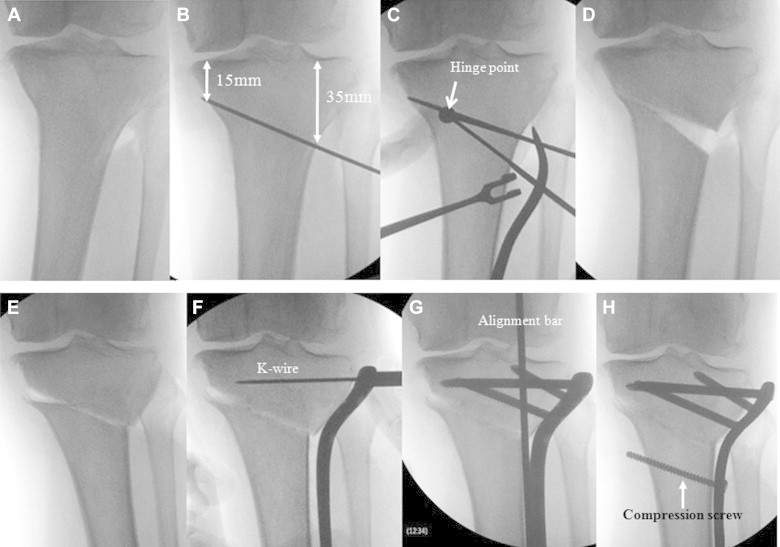
Hybrid CWHTO process examined under fluoroscopy. (A) The surgical position of the knee is at full extension with the patella upward. (B) A Kirschner wire is inserted obliquely from lateral to medial. The lateral point is 35 mm distal to the lateral tibial plateau, and the medial point is 15 mm distal to the medial tibial plateau. (C) A Kirschner wire is inserted percutaneously at the hinge point from anterior to posterior. A distal Kirschner wire is then inserted at the hinge point using a special goniometer. (D) The bone is cut, and the bone block is removed between the proximal and distal Kirschner wire guides. The medial cortex of the tibia is then cut completely. (E) Manual repositioning and completion of hybrid osteotomy (medial open and lateral closed). (F) The lateral proximal tibial plate is attached to the tibia. A Kirschner wire is then inserted from the proximal screw hole in the same direction as the screw guide on the preoperative planning image. (G) Limb alignment is confirmed using a long stainless steel rod from the center of the femoral head to the center of the ankle joint. (H) The distal fragment is pulled up to the plate shaft using a compression screw technique until both the proximal and distal lateral cortices are in firm contact. (K-wire, Kirschner wire.)
Fig 4.
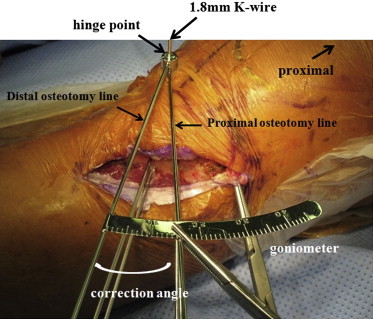
Determination of correction angle with a goniometer. The most important factor in the hybrid CWHTO procedure is the hinge point. A 1.8-mm-diameter Kirschner wire is inserted at this hinge point from anterior to posterior in the proximal tibia. A special goniometer for CWHTO is set at this wire. The distal osteotomy line is determined with the goniometer based on the correction angle. (K-wire, Kirschner wire.)
The distal osteotomy line is determined with the goniometer, and a third Kirschner wire (2 mm in diameter) is inserted from this point to the hinge point. Two Kirschner wires are used at the distal osteotomy site in the same manner as the proximal portion (Fig 2D). The first oblique osteotomy is started in accordance with the proximal Kirschner wires, and the second osteotomy is performed according to the distal Kirschner wires using a bone saw and chisels (Fig 2E). The third osteotomy is commenced from a point just proximal to the patellar tendon insertion toward the first osteotomy line, maintaining the thickness of the tibial tuberosity at 5 to 10 mm (biplanar osteotomy) (Fig 2F). The lateral closed-wedge bone block is then removed (Figs 2G and 3D), and the posterior surface of the tibial tuberosity is flattened. Finally, all Kirschner wires are removed, and the final osteotomy is performed according to the proximal osteotomy line. The medial cortex is then cut completely according to the proximal osteotomy line.
The salient point with regard to this new surgical procedure is that it is performed from the lateral site of the proximal tibia only. Thus the medial-side soft tissue including the MCL and periosteum is not released. After the osteotomy is completed, the proximal and distal fragments are approximated to correct any deformity (Figs 2H and 3E). The proximal and distal fragments rotate about the hinge point, the medial side is opened, and the lateral side is closed. In this way, the distal fragment is advanced proximally and anteriorly by the thickness of the flange (thickness of the tibial tuberosity).
Plate fixation is performed as follows: After repositioning of the fragments, the plate head is fixed to the proximal fragment. A Kirschner wire of 2 mm in diameter is then inserted from the proximal screw hole using a drill guide under fluoroscopy to ensure that the direction of the wire is parallel to the tibial plateau (with reference to preoperative planning) (Figs 2H and 3F). The proximal part of the plate is next firmly fixed with 4 screws (Figs 2I and 3G). Limb alignment is confirmed with a long stainless steel rod from the center of the femoral head to the center of the ankle joint under fluoroscopy, during which an axial load is applied to the sole to maintain the dorsiflexion position of the ankle joint as the WBL ratio becomes 63%. In most cases, the distal tibial shaft tends to dislocate medially compared with the proximal fragment. A compression screw technique is useful not only to attach the distal fragment of the tibia to the plate shaft but also to acquire a rigid contact force at the lateral proximal and distal cortex. A compression screw hole is made from the proximal normal screw hole at the first combination screw hole of the distal part of the plate by use of a 3.2-mm drill and drill guide. The drill direction is parallel or slightly distal to the repositioned osteotomy site. A normal cortical screw (4.2 mm in diameter) is inserted through this hole, and the distal fragment is moved to the plate (Figs 2J and 3H). Other plate holes are fixed with bicortical locking screws using another small skin incision with a minimally invasive technique. Finally, the former compression screw is changed to a locking screw (Fig 2K). The plate shaft is typically fixed with 4 screws (Fig 5). A drain is then inserted into the osteotomy site and removed the next day. The fascia of the tibialis anterior muscle is sutured in its original position, and the soft tissue is restored.
Fig 5.

Radiographs of left leg in a 63-year-old female patient with knee OA (Video 1). (A) Preoperative standing whole-leg radiograph. The WBL goes through the medial compartment of the knee. (B) Postoperative standing whole-leg radiograph. The WBL is shifted laterally.
Postoperative Rehabilitation
The day after surgery, after the drain is removed from the osteotomy site, active and passive range-of-motion and muscle-strengthening exercises are started. Standing on both legs and range-of-motion exercises with continuous passive motion are allowed as soon as possible on the same day. During the first week after surgery, patients are permitted partial (one-half) weight bearing with support equipment. Every patient commences full weight-bearing walking with a small cane within 2 weeks of the HTO procedure. Stair rise–and–fall training using a handrail or small cane is also permitted at 2 weeks after surgery.
Advantages of Hybrid CWHTO Procedure
There are many advantages of our hybrid CWHTO technique. First, a smaller bone wedge is removed from the lateral site of the osteotomy, and the leg length after this procedure is not reduced compared with traditional CWHTO. There is also no step-off at the lateral osteotomy site. In traditional CWHTO, the osteotomy is performed in parallel with the tibial plateau, and this causes a step-off of the proximal tibia shape. In addition, because of wedge removal in traditional CWHTO, there is a large bone block loss below the lateral tibial plateau with an increased lateral step-off, which could cause a difference in contact area between the proximal and distal osteotomy sites. The advantage of an oblique osteotomy is that the contact area of the osteotomy site is larger than that in conventional osteotomy.8 The oblique osteotomy used in our hybrid CWHTO procedure may increase shearing stress at the osteotomy site but prevents recurrence of varus deformities due to reductions in adduction moment at the osteotomy site after surgery. Shearing stress at the osteotomy site can be reduced by use of a rigid locking compression plate internal fixation device. Early full weight-bearing walking can be realized after surgery because the lateral cortices of the proximal and distal fragments are firmly attached. Bone healing at the medial open-wedge site is acquired in the early stages after surgery when using our hybrid procedure because the medial soft tissue at the osteotomy site is never released and thereby damaged. It is a potential concern with our method that there is higher tension in the medial soft tissue and pain will not be relieved because of the open medial osteotomy site. However, we believe that tension of the superficial bundle of the MCL decreases in varus knees accompanied by medial-compartment OA. It is our hypothesis that increasing the tension of the superficial bundle of the MCL again leads to improved stability of the medial-compartment joint and diminishes knee pain.
With our new method, the tibial tuberosity is cut using the biplanar osteotomy method and the patellar tendon insertion point is elevated anteriorly and repositioned proximally. The pressure on the patellofemoral joint is thereby diminished. Hence our procedure is effective for knees with medial-compartment OA accompanied by patellofemoral joint OA. Moreover, it is easy to change the tibial posterior slope during surgery using the hybrid CWHTO method. Lee and Byun9 have shown that the postoperative posterior tibial slope decreases compared with the preoperative slope in the sagittal plane after CWHTO. This phenomenon potentially decreases the in situ forces of tibial anterior translation with anterior cruciate ligament insufficiency. Complete cutting of the medial cortex does not lead to complications from CWHTO.10
In summary, the hybrid technique is easier to perform than other types of CWHTO. Patients treated with this method can be allowed to stand using both legs the day after surgery and commence full weight-bearing walking within 2 weeks of this HTO procedure. The development of a new plate system that is specific to this method is needed.
Acknowledgment
The authors acknowledge Dr. W. H. Jung of Murup Hospital for assisting with the wider adoption of the described procedure in South Korea.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
A 63 year old woman presented with right knee pain when walking and running. Her range of motion was an extension of 0 to a flexion of 130 degrees. She showed medial compartmental OA of the knee with an Ahlbäck classification of Grade 4. As her femoro-tibial angle (FTA) was 188 degrees and her correction angle was larger, we chose to perform hybrid CWHTO. An 18 degree correction valgus osteotomy was performed and her proximal tibia was fixed with a locking compression plate. The post-operative FTA in this patient was 170 degrees and she could start to walk with full wait bearing within one week of surgery with assistance from a small cane.
References
- 1.Hui C., Salmon L.J., Kok A. Long-term survival of high tibial osteotomy for medial compartment osteoarthritis of the knee. Am J Sports Med. 2011;39:64–70. doi: 10.1177/0363546510377445. [DOI] [PubMed] [Google Scholar]
- 2.Schallberger A., Jacobi M., Wahl P., Maestretti G., Jakob R.P. High tibial valgus osteotomy in unicompartmental osteoarthritis of the knee: A retrospective follow-up study over 13-21 years. Knee Surg Sports Traumatol Arthrosc. 2011;19:122–127. doi: 10.1007/s00167-010-1256-4. [DOI] [PubMed] [Google Scholar]
- 3.Efe T., Ahmed G., Heyse J.T. Closing-wedge high tibial osteotomy: Survival and risk factor analysis at long-term follow up. BMC Musculoskelet Disord. 2011;12:46. doi: 10.1186/1471-2474-12-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takeuchi R., Ishikawa H., Kumagai K. Fractures around the lateral cortical hinge following a medial opening wedge high tibial osteotomy: A new classification of lateral hinge fracture. Arthroscopy. 2012;28:85–94. doi: 10.1016/j.arthro.2011.06.034. [DOI] [PubMed] [Google Scholar]
- 5.Tunggal W.A.J., Higgins A.G., Waddell P.J. Complications of closing wedge high tibial osteotomy. Int Orthop. 2010;34:255–261. doi: 10.1007/s00264-009-0819-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atrey A., Morison Z., Tosounidis T., Tunggal J., Waddell P.J. Complications of closing wedge high tibial osteotomies for unicompartmental osteoarthritis of the knee. Bone Joint Res. 2012;1:205–209. doi: 10.1302/2046-3758.19.2000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahlbäck S. Osteoarthritis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 1968;(suppl 277):1–72. [PubMed] [Google Scholar]
- 8.Nakhostein M., Friedrich F.N., Müller W., Kentsch A. A special high tibial osteotomy technique for treatment of unicompartmental osteoarthritis of the knee. Orthopedics. 1993;16:1255–1258. doi: 10.3928/0147-7447-19931101-14. [DOI] [PubMed] [Google Scholar]
- 9.Lee C.D., Byun J.S. High tibial osteotomy. Knee Surg Relat Res. 2012;24:61–69. doi: 10.5792/ksrr.2012.24.2.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Raaij M.T., Brouwer W.R., de Vlieger R., Reijman M., Verhaar A.N.J. Opposite cortical fracture in high tibial osteotomy: Lateral closing compared to the medial opening wedge technique. Acta Orthop. 2008;79:508–514. doi: 10.1080/17453670710015508. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A 63 year old woman presented with right knee pain when walking and running. Her range of motion was an extension of 0 to a flexion of 130 degrees. She showed medial compartmental OA of the knee with an Ahlbäck classification of Grade 4. As her femoro-tibial angle (FTA) was 188 degrees and her correction angle was larger, we chose to perform hybrid CWHTO. An 18 degree correction valgus osteotomy was performed and her proximal tibia was fixed with a locking compression plate. The post-operative FTA in this patient was 170 degrees and she could start to walk with full wait bearing within one week of surgery with assistance from a small cane.


