Abstract
Background
There is a growing impetus to reorganize the hospital discharge process to reduce avoidable readmissions and costs. The aim of this study was to provide insight into hospital discharge problems and underlying causes, and to give an overview of solutions that guide providers and policy-makers in improving hospital discharge.
Methods
The Intervention Mapping framework was used. First, a problem analysis studying the scale, causes, and consequences of ineffective hospital discharge was carried out. The analysis was based on primary data from 26 focus group interviews and 321 individual interviews with patients and relatives, and involved hospital and community care providers. Second, improvements in terms of intervention outcomes, performance objectives and change objectives were specified. Third, 220 experts were consulted and a systematic review of effective discharge interventions was carried out to select theory-based methods and practical strategies required to achieve change and better performance.
Results
Ineffective discharge is related to factors at the level of the individual care provider, the patient, the relationship between providers, and the organisational and technical support for care providers. Providers can reduce hospital readmission rates and adverse events by focusing on high-quality discharge information, well-coordinated care, and direct and timely communication with their counterpart colleagues. Patients, or their carers, should participate in the discharge process and be well aware of their health status and treatment. Assessment by hospital care providers whether discharge information is accurate and understood by patients and their community counterparts, are important examples of overcoming identified barriers to effective discharge. Discharge templates, medication reconciliation, a liaison nurse or pharmacist, regular site visits and teach-back are identified as effective and promising strategies to achieve the desired behavioural and environmental change.
Conclusions
This study provides a comprehensive guiding framework for providers and policy-makers to improve patient handover from hospital to primary care.
Electronic supplementary material
The online version of this article (doi:10.1186/1472-6963-14-389) contains supplementary material, which is available to authorized users.
Keywords: Patient handoff, Patient discharge, Patient readmission, Intervention mapping, Adverse events
Background
Patients still experience needless harm and often struggle to have their voices heard, processes are not as efficient as they could be, and costs continue to rise at alarming rates while quality issues remain. A shorter length of hospital stay, the decrease in work-hours of health care providers, and the increasing number of patient transitions between departments and institutions requires effective patient handovers, especially those of frail patients with comorbidities [1]. Continuity of care at patient discharge from the hospital is a critical aspect of high quality patient care [2, 3]. Highly reliable care requires close cooperation between care providers across organisational boundaries, thereby establishing an interdisciplinary network [4]. Unfortunately, incomplete or incorrect information and communication errors between hospital care providers and the multiple receiving parties often increase the chance of adverse events. These may ultimately lead to life threatening situations, avoidable treatments, unplanned re-hospitalisations [5, 6], and extra costs [7–9].
Although studies have identified discharge problems in the social, organisational, linguistic and technical context [10–12], there is insufficient, evidence driven insights into more effective solutions. The effectiveness of most interventions is highly variable and limited in daily practice. Explanations for these disappointing results include the difficulty of changing providers behaviour and existing practices, non-optimal intervention strategies, inadequate resources devoted to evaluating the impact of interventions, and inadequate methods to design and evaluate interventions [13–15]. A systematic approach for translating discharge problems into customised solutions is lacking. Many clinical intervention developers select their strategies intuitively. Effective interventions need to be theory- and evidence based, and targeted at specific behavioural and environmental factors [16, 17].
The aim of our study was to systematically develop a guiding framework to more effective design of interventions that support care providers and policy-makers to improve patient handovers from the hospital to primary care.
Methods
Intervention mapping (IM) is a systematic, iterative six-step process that helps to develop an intervention, based on theoretical, empirical and practical information [18]. The steps are summarised in Table 1. IM was originally used effectively in the health promotion domain to develop programs for smoking cessatation [19], stroke prevention [20], asthma management [21], HIV prevention [22], and leg ulcer management [23]. We modified the IM terminology in order to apply it to the quality improvement domain.
Table 1.
Intervention mapping steps, objectives and methods*
| Steps | Objectives | Methods | |
|---|---|---|---|
| 1. | Problem analysis | ▪ Gain insight into health problem, quality of care, underlying causes and target population | ▪ Problem analysis using PRECEDE-PROCEED model; |
| ▪ Analysis based on: | |||
| - Literature research | |||
| - Individual interviews (n = 321) | |||
| - Focus group interviews (n = 26) | |||
| - Process maps (n = 5) | |||
| - Artifact analyses (n = 5) | |||
| - Ishikawa (fishbone) diagrams (n = 5) | |||
| 2. | Identify intervention outcomes, performance objectives and change objectives | ▪ State intervention outcomes | ▪ Use evidence from literature and empirical data from problem analysis (step 1) |
| ▪ Specify performance objectives | |||
| ▪ Select important and changeable determinants | ▪ Input from experts in the field of patient handover (healthcare providers, and organizational, social and health scientists) | ||
| ▪ Develop matrices with change objectives based on performance objectives and determinants of suboptimal hospital discharge | |||
| 3. | Select theory-based methods and strategies | ▪ Identify and select theoretical methods | ▪ Literature search on theory-based methods |
| ▪ Select evidence-based interventions and design of practical strategies | ▪ Input from experts (n = 220) | ||
| ▪ Ensure that interventions and strategies address change objectives | |||
| ▪ Systematic literature review on evidence based discharge interventions | |||
| ▪ Additional search for experience based practical strategies | |||
| ▪ Matching methods and practical strategies with determinants and performance objectives (step 1 and 2) | |||
| 4. | Develop an intervention | ▪ Provide suggestions for developing an intervention | ▪ Input from literature search and experts |
| 5. | Implementation | ▪ Provide suggestions for writing an implementation plan | ▪ Literature search of implementation strategies and tools |
| 6. | Evaluation | ▪ Provide suggestions for writing an evaluation plan | ▪ Literature search on methods for effect and process evaluation on complex interventions |
*Adapted from Bartholomew et al. [18].
Step 1: Problem analysis
We structured the problem analysis by using the PRECEDE PROCEED model [24] (see Additional file 1), to analyse and describe the scale, causes, and consequences of the health problem and to identify the target population.
Procedure and participants
A literature search on the frequency and consequences of ineffective hospital discharge problems was performed [25]. We performed a large qualitative study on patient handovers between acute care hospitals and primary care in five countries, i.e. The Netherlands, Spain, Poland, Sweden, and Italy, to identify the behavioural and environmental determinants influencing ineffective hospital discharge [10–12]. The study adhered to the RATS (Relevance, Appropriateness, Transparency, Soundness) guidelines for qualitative studies. Data collection and analysis consisted of multi-method qualitative research including individual and focus group interviews [26], process maps, artefact analyses [10–12], and Ishikawa diagrams [27] (Table 1). The discharged patients and their care providers were recruited using general and country-specific inclusion criteria (see Additional file 2). The study was approved by the ethics committee of the University Medical Center Utrecht — Medical Ethics Committee. Patients were asked for informed consent.
Step 2: Identify intervention outcomes, performance objectives and change objectives
In step 2, we identified the desired outcomes of the intervention and formulated specific performance objectives for the target population, such as writing a complete, accurate and timely discharge letter by the hospital physician. This resulted in a step-by-step checklist of what needs to be accomplished in order to obtain the desired outcomes [28].
It is important to identify what steps need to be tweaked in order to affect the performance objective, and ultimately the intervention outcome [28]. We identified the most important determinants (e.g., lack of knowledge and understanding between hospital and primary care providers) that need to be changed and combined these with performance objectives to formulate our change objectives. These change objectives specified who and what will change as a result of the intervention.
Procedure and participants
A literature search of the desired outcomes of the intervention was conducted [25]. The performance objectives and matrices of change objectives were discussed in a multidisciplinary study panel (n = 5) that included experts in health-, social- and organisational sciences. Members of the European HANDOVER Research Collaborative (n = 15 experts in the field of handover and health care providers) prioritised using a survey the large number of determinants of importance on a 5-point Likert scale.
Step 3: Selection of theory-based methods and strategies
We selected theory-based methods that relate to the change objectives in step 2. These methods were required to change the behavioural and environmental determinants of ineffective hospital discharge. Subsequently, these methods were translated into practical strategies.
Procedure and participants
Theory-based methods were identified from our literature search and mainly found in overviews provided by Bartholemew et al. [18], Achterberg et al. [29], and Grol et al. [30]. A total of 220 international researchers, policy-makers and regulators in the field of quality and safety in healthcare, healthcare providers and patient representatives were consulted about their experiences with successful strategies or promising ideas during three expert meetings in 2010–2011 [31]. A systematic review of randomised controlled trials (RCTs) of the effects of discharge interventions provided an overview of evidence-based strategies [32]. The systematic review was performed in accordance with the PRISMA guidelines. An additional literature search was performed to identify promising strategies that were not included in the systematic review (e.g., evaluated with a weaker study design than RCTs) or not evaluated yet (e.g., local initiatives). The strategies were selected by the study panel after 11 iterative discussion sessions based on the findings from the systematic review, the experiences of the experts and the additional literature search.
Step 4: Develop an intervention
In this step, we provide suggestions for the design of the intervention by considering the target group and local setting [18]. The intervention studies identified in step 3 were classified independently by two researchers (GH and MZ) according to the Oxford Centre for Evidence-Based Medicine - Levels of Evidence from 2009 onward [33].
Steps 5 and 6: Implementation and Evaluation
We made suggestions for developing an implementation plan for accomplishing program adoption, and for evaluating the effects and feasibility of the intervention program. The suggestions were based on literature regarding effective implementation strategies [17, 30, 34–36], existing implementation toolboxes [37, 38], and a literature review on methods to evaluate complex interventions in health care [35, 39, 40].
Results
Step 1: Problem analysis
The health problem and the underlying causes are presented in Figure 1. The published studies demonstrate that one in five patients experience an adverse event within 3 weeks after hospital discharge, of which one in three was considered preventable [41]. Three per cent of the adverse events led to permanent disability, including death. The one month unplanned readmission rates varied between 13% [42], and 20% [43]. Unnecessary hospital readmissions lead to considerable suffering, harm and extra costs. Friedman and Basu estimated hospital costs for preventable readmissions during 6 months at about $730 million [7]. Jencks estimated total hospital costs at $44 billion per year for rehospitalisations among Medicare patients within 30 days of hospital discharge [44].
Figure 1.
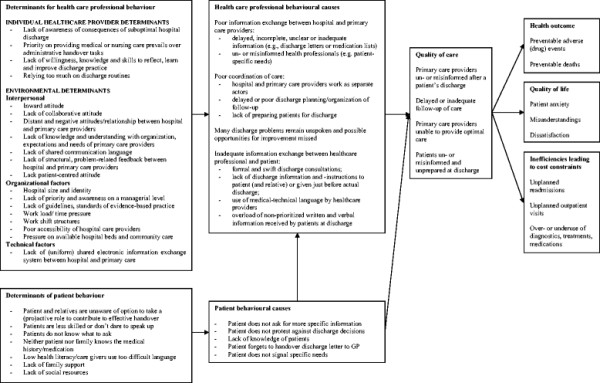
Model of suboptimal hospital discharge: overview of the health problem, causes and their determinants.
We found that ineffective handovers that lead to patient readmissions are caused by poor information exchange, poor coordination of care and poor communication between hospital and primary care providers, and between care providers and patients. The underlying causes include attitudinal and behavioural factors (e.g., lack of understanding of the needs of the counterpart, a distant relationship and a lack of collaborative attitude between hospital and primary care providers), organisational factors (e.g., lack of guidelines), technical factors (lack of a shared electronic information system) or patient factors (e.g., patients are less skilled or don’t dare to speak up). All the identified causes and their underlying factors are summarised in Figure 1.
Step 2: Matrices of change objectives
Intervention outcomes and performance objectives
Measurable and feasible endpoints to evaluate the discharge process are hospital readmission rates and adverse events rates after the hospital discharge.
All performance objectives are listed in Table 2. It is important for healthcare providers to transfer high-quality discharge information to primary care providers and patients. For example, using discharge letters that are complete (i.e., no redundant/irrelevant or missed information), accurate and understandable (i.e., structured presentation of information, explanation of abbreviations jargon), and patients being informed at discharge in plain language. Regarding coordination of care, healthcare providers are expected to have organised and accurate follow-up services at patient’s discharge in a timely manner and tailored to the patient’s preferences and psychosocial needs (e.g., assessment of home setting, social risks and support). Examples of performance objectives for discharge communication are hospital care providers being accessible for primary care providers or patients and exchanging discharge information in time to support primary care providers or patients.
Table 2.
Performance objectives for healthcare providers and patients
| Healthcare providers | |
| Discharge information | 1a. Complete discharge information |
| 1b. Clear discharge information | |
| 1c. Accurate discharge information | |
| Coordination of care | 2a. Ensure that follow-up services are being organized at actual discharge |
| 2b. Tailor follow-up care to patient needs and preferences | |
| 2c. Organize timely and accurate follow-up | |
| Discharge communication | 3a. Seek direct/personal contact with primary care counterpart |
| 3b. Discharge information easily accessible to counterpart care providers and patients (and relatives) | |
| 3c. Exchange discharge information on time to primary care counterparts | |
| 3d. Inform patient (and relatives) personally and in timely manner | |
| Patients | |
| Participation in discharge process | 4. Contribute, if capable, to the continuity of care in the discharge process |
| Awareness of health status and treatment | 5. Well aware about medical history and medication use, diagnosis/indication and (side) effects of the treatment, post discharge appointments, scheduled tests and (pending) test results |
Patients are, if capable, expected to contribute to the continuity of care by participating in the discharge process (e.g., by handing over a discharge letter to their GP after being discharged), and by being well aware of their health status (e.g., medical and medication history) and treatment plan.
Selected determinants and change objectives
The most important determinants (as perceived by experts in the field of patient handovers and described in step 2 of the methods) were classified according to the individual professional, interpersonal, organisational, technical and patient levels. Combining the performance objectives with the selected determinants resulted in two matrices with change objectives for healthcare providers and patients, which interventions need to target. The matrices are presented in Additional file 3.
Step 3: Selecting theory-based methods and strategies
Our literature review identified a raft of change methods, such as knowledge transfer, active listening and guided practice from the Social Cognitive Theory (SCT) [45], consciousness raising from the Transtheoretical Model [46, 47], shifting perspectives and interpersonal contact from the Intergroup Contact Theory [48] and standardised working processes from the SCT and Rational Decision-making theories [30] as influencers of the behavioural and environmental determinants of ineffective hospital discharge. Goal-setting and implementation intentions were derived from theories of Goal Directed Behaviour [49, 50], and multi-disciplinary collaboration and case management from theories of Integrated Care [51]. These theory-based methods were subsequently operationalised into practical strategies and corresponding activities and materials for the targeted population [52–76] as shown in Table 3.
Table 3.
Overview of change determinants, theory-based methods, strategies and practical applications, and evidence
| Determinants and change objectives | Theory-based methods | Examples of strategies/ practical applications | Examples of activities and materials | References* | Evidence† |
|---|---|---|---|---|---|
| Individual healthcare provider | |||||
| Aware of the consequences of suboptimal hospital discharge | Knowledge transfer/Active learning | Education in the medical and nursing curriculum | Lectures on patient handover and exercises with workbook and online materials (e.g., communication skills and discharge letter requirements) | 52 | 3a |
| Perceive handover administrative tasks as important part of patient discharge care and act accordingly | Stimulus control/ Reinforcement | Punishment by financial penalties; visual electronic reminders | Red, orange and green flags indicating status of discharge letter and planning; visualization of deadline for sending discharge letter | NF | NA |
| Interpersonal | |||||
| Outward focus by hospital-based care providers to ensure continuity of care after discharge | Integrated care | Post-discharge monitoring of follow-up | Standard post-discharge telephone call or home visit to the patient to evaluate follow-up, provide additional instructions and answer questions | 53 | 1a |
| Hospital and primary care provider collaborative during the discharge process | Integrated care/ Intergroup contact/ Case management | Case conference | Hospital or community-based face-to-face or telephone meetings between hospital and primary care providers | 54-57 | 1b |
| Liaison person | Designated care provider coordinating hospital discharge, follow-up care and the communication between hospital and primary care providers | 58-60 | 1b | ||
| Knowledge and understanding of the primary care organization, expectations and needs | Team building/ Intergroup contact/ Shifting perspective | Meetings between hospital and primary care providers to increase mutual understanding and respect between both parties | Focus group sessions, regular meetings and site visits to get to know each other, to learn each other’s organization and needs and to identify improvement opportunities | 61 | 1b |
| Structural, problem-related feedback between hospital and primary care providers | Stimulus control | Means to facilitate and stimulate structural feedback | Standard feedback form and return envelop along with discharge letter send to primary care providers | NF | NA |
| Patient-centered attitude | Modeling/ Individualization | Use of plain, patient-friendly, nonmedical language | Discharge summary in language that is understandable for patients and relatives | 62 | 1b |
| Active listening | Teach back | Care provider checks if patients received all discharge information needed and if they understood the received information | 63 | 2b | |
| Organizational | |||||
| Guidelines and standards of evidence-based practice | Standardized working processes | Standardized discharge letter (e.g. templates, formats) | Templates, formats, required (web-based) fields, clinical decision-support, pick lists | 64-66 | 1b |
| Standardized discharge planning | Guidelines, protocols, checklists for discharge planning, organizing follow-up | 67-68 | 1b | ||
| Medication reconciliation | Standardised medication reconciliation checklist/medication discrepancy tool/ reconciliation by (liaison) pharmacist | 54,57,65-67,69-71 | 1b | ||
| Technical | |||||
| Shared electronic information exchange system | Multi-disciplinarycollaboration | Shared electronic patient information system | Electronic notifications to primary care providers to inform them about patient hospital visits and to provide them (web-based) access to available discharge information | 65,66,71-73 | 1b |
| Patient and relative | |||||
| Participation in the discharge process | Self- management/ Guided practice | Encouraging and facilitating patients in self-management skills | Provide patient with discharge record (e.g., active problem list, medication, allergies, patient concerns) owned and maintained by the patient to facilitate cross-site information transfer | 62,74,75 | 1b |
| Skills and dare to speak up | Coaching/ Guided practice | Encouragement to assert a more active role during discharge | Question form for patients | 74 | 1b |
| Understanding of medical history and/or medication | Guided practice/ Knowledge transfer | Medication counseling at the hospital at discharge or at the patient’s home | Visits by a pharmacist counselor | 76 | 1b |
NF = not found; NA = not available.
*The majority of the references relate to interventions or a component of a studied intervention program with an aim to improve hospital discharge. Other types of interventions (e.g., improving clinical handovers within the hospital) were also used as references in case they were considered to be relevant and appropriate for improving hospital discharge.
†Grading of evidence, adapted and adjusted from the Oxford Centre for Evidence-based Medicine Levels of Evidence33: 1b = systematic review or meta-analysis of randomized controlled trials (RCTs); 1a = RCT of good-moderate quality or sufficient size and consistency; 3-4 = comparative trials (non-randomized, cohort studies, patient-control studies); 4 = non-comparative studies; 5 = Expert committee reports, opinions and/or clinical experience of respected authorities.
Step 4: Develop an intervention
We formulated a wide variety of change objectives at the individual clinician and patient levels, the interpersonal level, organisational and technical levels that need to be considered in order to tackle ineffective handovers at discharge more reliably (Additional file 3). Given these change objectives the intervention likely needs to be multi-faceted and needs to be tailored to the needs encountered in the local setting. Table 3 shows a framework with examples of strategies and related materials and activities guiding healthcare providers and policy makers in the development of their intervention. The list of all identified strategies and related materials, level of evidence and references are available upon request.
Many interventions were evaluated in well-designed studies. For example, the use of standardised discharge practices such as the use of discharge letter templates, discharge planning guidelines and medication reconciliation checklists are effective strategies [65–67, 70]. The use of a shared electronic patient information platform facilitates discharge communication between hospital and primary care providers [66, 71–73]. There is evidence demonstrating that the patient’s role in the discharge process is enhanced by the provision of written and verbal discharge information and by assistance and guidance in self-management (e.g., discharge counselling, follow-up calls or home-based visits and a patient discharge record or question form) [74, 76]. However, many promising interventions have not been evaluated properly or were tested using weak study designs. For example, the effects of lectures and exercises on discharge practice in the medical curriculum, and regular group discussions involving hospital and primary care providers are largely unknown [52].
Moreover, there is limited evidence on the effects of reinforcement by using discharge planning reminders, mandatory administrative tasks or financial incentives and penalties [77].
Insight also lacks into the effects of strategies to increase care provider reflections on discharge practices (e.g., use of a standardised feedback form, video reflection, role play or simulation of discharge consultations) [52] and regarding the use of teach-back to check the patient’s understanding of their medical and medication history [63, 78].
Steps 5 and 6: Implementation and evaluation
Commitment from and ownership by the target group is essential to successful implementation [79, 80]. The awareness among end users is enhanced when they are directly involved in the development or modification of the innovation, in mounting the implementation plan, and in selecting the implementation strategies to be used [35].
Moreover, uptake of policies and protocols, reimbursement and the consideration of patients’ preferences are necessary for a sustainable implementation [81].
Strategies that address the barriers to change are required to implement interventions in daily practice [36]. Most theories on implementing interventions in health care emphasise that an analysis of the barriers to change practice is a prerequisite to selecting or developing an effective implementation strategy [17]. An implementation plan should be developed specifically after selecting the implementation strategies to tackle the barriers. This plan should be compatible with the target group and settings in which the implementation will take place. Good management and planning of implementation activities (i.e., what, when, where, how and by whom) also appears to be a requisite for successful implementation of innovations in patient care [35].
Formative and summative effect evaluation should be carried out using hospital readmission and adverse events as defined patient outcome effects to evaluate whether the intervention led to the desired degree of change. The formulated performance objectives in step 2 can be operationalised in measurable process indicators, for example by assessing the proportion of patients discharged with a complete discharge letter and assessing the proportion of patients discharged after medication reconciliation.
A process evaluation should be performed to understand the effect, success or failure of the intervention and to get an impression of its feasibility, generalizability and its acceptability in the target population. The process evaluation gives insight into the black box of the implementation process and can explain the variation in results in evaluating interventions. The activities carried out as part of the intervention, the actual exposure of participants to these activities, and their experience of these activities should be studied [40].
Discussion
Effective hospital discharge and reducing patient readmission rates are influenced by the behaviours of care providers and patients and their environmental context. Our findings demonstrate the existence of a large number of determinants for (in)effective discharge that underscore the complexity of the discharge process. Therefore, improving hospital discharge requires a multi-component, multi-level intervention (“bundle”) instead of trying to find a “magic bullet” single intervention.
An extensive overview of theory-based methods and practical strategies suitable for improving patient handover skills and healthcare provider and patient behaviour in the discharge process was systematically created based on the scale, causes, and consequences of ineffective hospital discharge presented in our study. Most interventions were aimed at improving the organisational and technical aspects of the discharge process. There is a lack of evidence-based interventions on improving healthcare provider skills by means of handover training and evidence-based guidance. Moreover, effective interventions for changing the individual healthcare provider’s and patient’s competencies, awareness and attitudes (e.g., via education, reminders or teach-back), and the relationship between providers (e.g., via frequent informal meeting between hospital and primary care providers and reflexive feedback) are lacking. All this despite our overwhelming data demonstrating that awareness, attitudes and skills are key factors for improving hospital discharge. We found a gap between the discharge improvement needs and the evidence-based interventions that are suitable to address these needs. The lack of evidence about the effectiveness of interventions may be attributed to the difficulty of measuring attitudes and their effects on healthcare performance [82–84].
This study is supported by earlier research and discharge programs in the United States: i.e., the RED (“ReEngineerd Discharge”) project [69, 85], the Care Transitions Program [86] and BOOST (Better Outcomes for Older adults through Safe Transitions) [87]. An important strength of our study is the deliberate assessment of determinants and interventions that affect the discharge process. Qualitative input provides comprehensive insights into a variety of determinants. Our empirical data, results of a systematic literature review, theories of social behaviour and multiple consultation rounds of a broad group of 324 experts (researchers, policy-makers, inspectors) in the field of quality and safety in healthcare, healthcare providers and patient representatives [31], provided useful input for the selection of change methods, practical strategies and related evidence.
A limitation of the study is our focus on the micro-level excluding other key factors for change. The possible barriers and facilitators at a macro- and meso-levels, i.e., financial and legal obligations or constrains were not included. Moreover, the relationships between the identified determinants and theoretical-based methods and strategies were hypothetical.
However, the determinants were systematically and theory-driven and linked to practical strategies using the IM method and were not intuitively chosen.
Conclusions
This study provides a comprehensive overview of patient discharge problems and underlying causes. It provides a guiding framework including theory-based strategies and practical tools to support care providers and policy-makers in their efforts to select and implement interventions on a more rational basis. Intervention mapping is a powerful method for care providers and policy makers to assess and prioritise intervention strategies and tailor them to the needs of individual facilities and healthcare systems. The next step for care providers and policy-makers is to look carefully into the discharge problems in their own local settings and to select appropriate solutions for improving hospital discharge effectively.
Electronic supplementary material
Additional file 1: Modified model based on PRECEDE-PROCEED concept and the theory of planned behavior (DOCX 33 KB)
Additional file 2: Study Population Inclusion and Exclusion Criteria. (DOCX 15 KB)
Additional file 3: Matrix of change objectives. (DOCX 20 KB)
Acknowledgements
We thank the patients, relatives, physicians and nurses who participated in this study. We also thank the 220 expert meeting participants for their contributions to this study.
Financial support
This work was supported by a grant from the European Union, the Framework Programme of the European Commission (FP7-HEALTH-F2-2008-223409).
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GH and MZ designed and managed the study. GH, MF, ED-U, CO and GT collected the data. All authors (GH, MZ, MVD, PB, CK, MF, GÖ, MO, SB, CO, RS, GT, FV, EDU, LS, HW) were involved in the analysis and interpretation of the data. GH and MZ drafted the manuscript. All authors read the manuscript for important intellectual content and approved the final version.
Contributor Information
Gijs Hesselink, Email: gijs.hesselink@radboudumc.nl.
Marieke Zegers, Email: marieke.zegers@radboudumc.nl.
Myrra Vernooij-Dassen, Email: myrra.vernooij-dassen@radboudumc.nl.
Paul Barach, Email: pbarach@gmail.com.
Cor Kalkman, Email: c.j.kalkman@umcutrecht.nl.
Maria Flink, Email: maria.flink@karolinska.se.
Gunnar Ön, Email: gunnar.ohlen@karolinska.se.
Mariann Olsson, Email: mariann.olsson@karolinska.se.
Susanne Bergenbrant, Email: susanne.bergenbrant-glas@karolinska.se.
Carola Orrego, Email: corrego@fadq.org.
Rosa Suñol, Email: rsunol@fadq.org.
Giulio Toccafondi, Email: toccaf@gmail.com.
Francesco Venneri, Email: francesco.venneri@asf.toscana.it.
Ewa Dudzik-Urbaniak, Email: dudzik@cmj.org.pl.
Basia Kutryba, Email: kutryba@cmj.org.pl.
Lisette Schoonhoven, Email: lisette.schoonhoven@radboudumc.nl.
Hub Wollersheim, Email: hub.wollersheim@radboudumc.nl.
References
- 1.Halasyamani L, Kripalani S, Coleman E, Schnipper J, van Walraven C, Nagamine J, Torcson P, Bookwalter T, Budnitz T, Manning D. Transition of care for hospitalized elderly patients – development of a discharge checklist for hospitalists. J Hosp Med. 2006;1:354–360. doi: 10.1002/jhm.129. [DOI] [PubMed] [Google Scholar]
- 2.Clare J, Hofmeyer A. Discharge planning and continuity of care for aged people: indicators of satisfaction and implications for practice. Aust J Adv Nurs. 1998;16:7–13. [PubMed] [Google Scholar]
- 3.Hellesø R, Lorensen M, Sorensen L. Challenging the information gap–the patients transfer from hospital to home health care. Int J Med Inform. 2004;73:569–580. doi: 10.1016/j.ijmedinf.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 4.Cohen SG, Bailey DE. What makes teams work: group effectiveness research from the shop floor to the executive suite. J Manag. 1997;23:239–290. [Google Scholar]
- 5.Cheah LP, Amott DH, Pollard J, Watters DAK. Electronic medical handover: towards safer medical care. Med J Aust. 2005;183:369–372. doi: 10.5694/j.1326-5377.2005.tb07086.x. [DOI] [PubMed] [Google Scholar]
- 6.Simpson K. Handling handoffs safely. MCN Am J Matern Child Nurs. 2005;30:152. doi: 10.1097/00005721-200503000-00030. [DOI] [PubMed] [Google Scholar]
- 7.Friedman B, Basu J. The rate and cost of hospital readmissions for preventable conditions. Med Care Res Rev. 2004;61:225–240. doi: 10.1177/1077558704263799. [DOI] [PubMed] [Google Scholar]
- 8.Foekema H, Hendrix C. Fouten Worden Duur Betaald, Een Onderzoek Naar Medische Overdrachtsfouten (Deel 2) Amsterdam: TNS NIPO; 2004. Mistakes Are Expensive, An Investigation Into Medical Transcription Errors, (Part 2) [Google Scholar]
- 9.Leendertse AJ, Egberts AC, Stoker LJ, van den Bemt PM, HARM Study Group Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med. 2008;168:1890–1896. doi: 10.1001/archinternmed.2008.3. [DOI] [PubMed] [Google Scholar]
- 10.Hansagi H, Olsson M, Glas S, Flink M, Barach P, Ön G. Report on the Barriers And Facilitators To Effective Handovers In The Social, Linguistic And Technological Context In Which They Take Place. Utrecht, The Netherlands: Utrecht 383 Medical Center; 2010. [Google Scholar]
- 11.Johnson JK, Farnan JM, Barach P, Hesselink G, Wollersheim H, Pijnenborg L, Kalkman C, Arora VM, HANDOVER Research Collaborative Searching for the missing pieces between hospital and primary care: mapping the patient process during care transitions. BMJ Qual Saf. 2012;21(Suppl 1):i97–i105. doi: 10.1136/bmjqs-2012-001215. [DOI] [PubMed] [Google Scholar]
- 12.Hesselink G, Vernooij-Dassen M, Pijnenborg L, Barach P, Gademan P, Dudzik-Urbaniak E, Flink M, Orrego C, Toccafondi G, Johnson JK, Schoonhoven L, Wollersheim H, European HANDOVER Research Collaborative Organizational culture: an important context for addressing and improving hospital to community patient discharge. Med Care. 2012;51:90–98. doi: 10.1097/MLR.0b013e31827632ec. [DOI] [PubMed] [Google Scholar]
- 13.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, Medical Research Council Guidance Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–705. doi: 10.1001/jama.1995.03530090032018. [DOI] [PubMed] [Google Scholar]
- 15.Wensing M, van der Weijden T, Grol R. Implementing guidelines and innovations in general practice: which interventions are effective? Br J Gen Pract. 1998;48:991–997. [PMC free article] [PubMed] [Google Scholar]
- 16.van Bokhoven MA, Kok G, van der Weijden T. Designing a quality improvement interventions: a systematic approach. Qual Saf Health Care. 2003;12:215–220. doi: 10.1136/qhc.12.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, Robertson N: Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes (Review).Cochrane Database Syst Rev 2010., (3): CD005470 [DOI] [PMC free article] [PubMed]
- 18.Bartholomew LK, Parcel GS, Kok G. Planning Health Promotion Programs. An Intervention Mapping Approach. Third. San Francisco: Jossey-Bass; 2011. [Google Scholar]
- 19.Mullen PD, DiClemente CC, Bartholomew LK. Theory and Context In Project PANDA: A Program To Help Postpartum Women Stay Off Cigarettes. In: Bartholomew LK, Parcel GS, Kok G, Gottlieb NH, editors. Intervention Mapping: Designing Theory And Evidence-Based Health Promotion Programs. Mountain View, CA: Mayfield Publishing Co.; 2001. [Google Scholar]
- 20.Schmid AA, Andersen J, Kent T, Williams LS, Damush TM. Using intervention mapping to develop and adapt a secondary stroke prevention program in Veterans Health Administration medical centers. Implement Sci. 2010;5:97. doi: 10.1186/1748-5908-5-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fernandez ME, Bartholomew LK, Lopez A, Parcel G. 128th annual meeting of the American Public Health Association. 2000. Using Intervention Mapping In The Development Of A School-Based Asthma Management Intervention For Latino Children And Families: The FAMILIAS Project. [Google Scholar]
- 22.van Empelen P, Kok G, Schaalma HP, Bartholomew LK. An AIDS risk-reduction program for Dutch drug users: an intervention mapping approach to planning. Health Promot Pract. 2003;4:402–412. doi: 10.1177/1524839903255421. [DOI] [PubMed] [Google Scholar]
- 23.Heinen MM, Bartholomew LK, Wensing M, van de Kerkhof P, van Achterberg T. Supporting adherence and healthy lifestyles in leg ulcer patients: systematic development of the lively legs program for dermatology outpatient clinics. Patient Educ Couns. 2006;61:279–291. doi: 10.1016/j.pec.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 24.Green LW, Kreuter MW. Health Promotion Planning: An Educational And Ecological Approach. 3. Mountain View, CA: Mayfield Publishing Co.; 1999. [Google Scholar]
- 25.Yao GL, Novielli N, Manaseki-Holland S, Chen YF, van der Klink M, Barach P, Chilton PJ, Lilford RJ, European HANDOVER Research Collaborative Evaluation of a predevelopment service delivery intervention; an application to improve clinical handovers. BMJ Qual Saf. 2012;21:i29–i38. doi: 10.1136/bmjqs-2012-001210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Corbin J, Strauss A. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 1990;13:3–21. doi: 10.1007/BF00988593. [DOI] [Google Scholar]
- 27.Barach P, Gademan P, Kalkman C, Johnson JK, Pijnenborg L. Report on How Variations In Handover Processes Lead To Near Misses And Adverse Outcomes, And Identifying Standardized Elements Of Communication. Utrecht, The Netherlands: Utrecht Medical Center, for the European Union; 2010. [Google Scholar]
- 28.McEachan RR, Lawton RJ, Jackson C, Conner M, Lunt J. Evidence. Theory and context: using intervention mapping to develop a worksite physical activity intervention. BMC Public Health. 2008;8:326. doi: 10.1186/1471-2458-8-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Achterberg T, Huisman-de Waal GG, Ketelaar NA, Oostendorp RA, Jacobs JE, Wollersheim H. How to promote healthy behaviours in patients? An overview of evidence for behaviour change techniques. Health Promot Int. 2010;26:148–162. doi: 10.1093/heapro/daq050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grol RP, Bosch MC, Hulscher ME, Eccles MP, Wensing M. Planning and studying improvement in patient care: the use of theoretical perspectives. Milbank Q. 2007;85:93–138. doi: 10.1111/j.1468-0009.2007.00478.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kutryba B, Dudzik-Urbaniak E, Göbel AA, Pijnenborg L, Barach P. Dissemination of the HANDOVER project – Final Report. Utrecht, The Netherlands: Utrecht Medical Center, for the European Union; 2011. [Google Scholar]
- 32.Hesselink G, Schoonhoven L, Barach P, Spijker A, Gademan P, Kalkman C, Liefers J, Vernooij-Dassen M, Wollersheim H. Improving patient handovers from hospital to primary care. A systematic review. Ann Intern Med. 2012;157:417–428. doi: 10.7326/0003-4819-157-6-201209180-00006. [DOI] [PubMed] [Google Scholar]
- 33.Oxford Centre of Evidence-Based Medicine [http://www.cebm.net/index.aspx?o=1025
- 34.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 35.Grol R, Wensing M, Eccles M, Davis D. Improving Patient Care: The Implementation Of Change In Health Care. second. Wiley-Blackwell: Elsevier; 2013. [Google Scholar]
- 36.Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, Whitty P, Eccles MP, Matowe L, Shirran L, Wensing M, Dijkstra R, Donaldson C. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Tech Ass. 2004;8:1–72. doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]
- 37.Clarke CM, Persaud DD. Leading clinical handover improvement: a change strategy to implement best practices in the acute care setting. J Patient Saf. 2011;7:11–18. doi: 10.1097/PTS.0b013e31820c98a8. [DOI] [PubMed] [Google Scholar]
- 38.Australian Medical Association . Safe Handover: Safe Patients, Guidance On Clinical Handover For Clinicians And Managers. Canberra: AMA; 2006. [Google Scholar]
- 39.Brown C, Hofer T, Johal A, Thomson R, Nicholl J, Franklin BD, Lilford RJ. An epistemology of patient safety research: a framework for study design and interpretation. Part 2. Study design. Qual Saf Health Care. 2008;17:163–169. doi: 10.1136/qshc.2007.023648. [DOI] [PubMed] [Google Scholar]
- 40.Hulscher ME, Laurant MG, Grol RP. Process evaluation on quality improvement interventions. Qual Saf Health Care. 2003;12:40–46. doi: 10.1136/qhc.12.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 42.Halfon P, Eggli Y, van Melle G, Chevalier J, Wasserfallen JB, Burnand B. Measuring potentially avoidable hospital readmissions. J Clin Epidemiol. 2002;55:573–587. doi: 10.1016/S0895-4356(01)00521-2. [DOI] [PubMed] [Google Scholar]
- 43.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-services program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 44.Jencks SF. Defragmenting care. Ann Intern Med. 2010;153:757–758. doi: 10.7326/0003-4819-153-11-201012070-00010. [DOI] [PubMed] [Google Scholar]
- 45.Bandura A. Social Foundations Of Thought And Action. A Social Cognitive Theory. Englewood Cliffs, New Jersey: Prentice Hall; 1986. [Google Scholar]
- 46.Prochaska J, DiClimente C, Norcross J. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47:1102–1114. doi: 10.1037/0003-066X.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 47.Prochaska JO, DiClemente CC. The Transtheoretical Approach. In: Norcross JC, Goldfried MR, editors. Handbook of Psychotherapy Integration. 2. New York: Oxford University Press; 2005. [Google Scholar]
- 48.Pettigrew TF, Tropp LR. When Groups Meet: The Dynamics Of Intergroup Contact. New York: Psychology Press; 2011. [Google Scholar]
- 49.Locke EA, Latham GP. A Theory Of Goal Setting And Task Performance. Englewood Cliffs, NJ: Prentice-Hall; 1990. [Google Scholar]
- 50.Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation: a 35-year odyssey. Am Psychol. 2002;57:701–717. doi: 10.1037//0003-066x.57.9.705. [DOI] [PubMed] [Google Scholar]
- 51.Wagner EH. The role of patient care teams in chronic disease management. BMJ. 2000;320:569–572. doi: 10.1136/bmj.320.7234.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gordon M, Findley R. Educational interventions to improve handover in health care: a systematic review. Med Educ. 2011;45:1081–1089. doi: 10.1111/j.1365-2923.2011.04049.x. [DOI] [PubMed] [Google Scholar]
- 53.Chiu WK, Newcomer R. A systematic review of nurse-assisted case management to improve hospital discharge transition outcomes for the elderly. Professional Case Management. 2007;12:330–336. doi: 10.1097/01.PCAMA.0000300406.15572.e2. [DOI] [PubMed] [Google Scholar]
- 54.Caplan GA, Williams AJ, Daly B, Abraham K. A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department–the DEED II study. J Am Geriatr Soc. 2004;52:1417–1423. doi: 10.1111/j.1532-5415.2004.52401.x. [DOI] [PubMed] [Google Scholar]
- 55.Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, Schwartz JS. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 56.Rich MW, Vinson JM, Sperry JC, Shah AS, Spinner LR, Chung MK, Davila-Roman V. Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study. J Gen Intern Med. 1993;8:585–590. doi: 10.1007/BF02599709. [DOI] [PubMed] [Google Scholar]
- 57.Crotty M, Rowett D, Spurling L, Giles LC, Phillips PA. Does the addition of a pharmacist transition coordinator improve evidence-based medication management and health outcomes in older adults moving from the hospital to a long-term care facility? Results of a randomized, controlled trial. Am J Geriatr Pharmacother. 2004;2:257–264. doi: 10.1016/j.amjopharm.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 58.Preen DB, Bailey BE, Wright A, Kendall P, Phillips M, Hung J, Hendriks R, Mather A, Williams E. Effects of a multidisciplinary, post-discharge continuance of care intervention on quality of life, discharge satisfaction, and hospital length of stay: a randomized controlled trial. Int J Qual Health Care. 2005;17:43–51. doi: 10.1093/intqhc/mzi002. [DOI] [PubMed] [Google Scholar]
- 59.Avlund K, Jepsen E, Vass M, Lundemark H. Effects of comprehensive follow-up home visits after hospitalization on functional ability and readmissions among old patients. A randomized controlled study. Scand J Occup Ther. 2002;9:17–22. doi: 10.1080/110381202753505827. [DOI] [Google Scholar]
- 60.Shyu YI, Liang J, Wu CC, Su JY, Cheng HS, Chou SW, Chen MC, Yang CT, Tseng MY. Two-year effects of interdisciplinary intervention for hip fracture in older Taiwanese. J Am Geriatr Soc. 2010;58:1081–1089. doi: 10.1111/j.1532-5415.2010.02882.x. [DOI] [PubMed] [Google Scholar]
- 61.Rutherford A, Burge B. General practitioners and hospitals. Continuity of care Aust Fam Physician. 2001;30:1101–1107. [PubMed] [Google Scholar]
- 62.Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;23:1228–1233. doi: 10.1007/s11606-008-0618-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.White M, Garbez R, Carroll M, Brinker E, Howie-Esquivel J. Is “Teach-Back” Associated With Knowledge Retention and Hospital Readmission in Hospitalized Heart Failure Patients? J Cardiovasc Nurs. 2013;28:137–147. doi: 10.1097/JCN.0b013e31824987bd. [DOI] [PubMed] [Google Scholar]
- 64.van Walraven C, Laupacis A, Seth R, Wells G. Dictated versus database-generated discharge summaries: a randomized clinical trial. CMAJ. 1999;160:319–326. [PMC free article] [PubMed] [Google Scholar]
- 65.Schnipper JL, Kirwin JL, Cotugno MC, Wahlstrom SA, Brown BA, Tarvin E, Kachalia A, Horng M, Roy CL, McKean SC, Bates DW. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166:565–571. doi: 10.1001/archinte.166.5.565. [DOI] [PubMed] [Google Scholar]
- 66.Graumlich JF, Novotny NL, Nace GS, Aldag JC. Patient and physician perceptions after software-assisted hospital discharge: cluster randomized trial. J Hosp Med. 2009;4:356–363. doi: 10.1002/jhm.565. [DOI] [PubMed] [Google Scholar]
- 67.King TL. The impact of a nurse-driven evidence-based discharge planning protocol on organizational efficiency and patient satisfaction in patients with cardiac implants. 2008. [Google Scholar]
- 68.Bump GM, Bost JE, Buranosky R, Elnicki M. Faculty member review and feedback using a sign-out checklist: improving intern written sign-out. Acad Med. 2012;87:1125–1131. doi: 10.1097/ACM.0b013e31825d1215. [DOI] [PubMed] [Google Scholar]
- 69.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, Forsythe SR, O’Donnell JK, Paasche-Orlow MK, Manasseh C, Martin S, Culpepper L. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150:178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Koehler BE, Richter KM, Youngblood L, Cohen BA, Prengler ID, Cheng D, Masica AL. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medic. J Hosp Med. 2009;4(4):211–218. doi: 10.1002/jhm.427. [DOI] [PubMed] [Google Scholar]
- 71.Tripp JS. Development And Evaluation Of Notifications To Inform Primary Care Providers Of Summary Documentation For Their Patients’ Hospital Visits. 2009. [Google Scholar]
- 72.Chen Y, Brennan N, Magrabi F. Is email an effective method for hospital discharge communication? A randomized controlled trial to examine delivery of computer generated discharge summaries by email, fax, post and patient hand delivery. Int J Med Inform. 2010;79:167–172. doi: 10.1016/j.ijmedinf.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 73.Afilalo M, Lang E, Léger R, Xue X, Colacone A, Soucy N, Vandal A, Boivin JF, Unger B. Impact of a standardized communication system on continuity of care between family physicians and the emergency department. CJEM. 2007;9:79–86. doi: 10.1017/s1481803500014834. [DOI] [PubMed] [Google Scholar]
- 74.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 75.Krumholz HM, Amatruda J, Smith GL, Mattera JA, Roumanis SA, Radford MJ, Crombie P, Vaccarino V. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol. 2002;39:83–89. doi: 10.1016/S0735-1097(01)01699-0. [DOI] [PubMed] [Google Scholar]
- 76.Hugtenburg JG, Borgsteede SD, Beckeringh JJ. Medication review and patient counselling at discharge from the hospital by community pharmacists. Pharm World Sci. 2009;31:630–637. doi: 10.1007/s11096-009-9314-z. [DOI] [PubMed] [Google Scholar]
- 77.Kaiser Health News. Medicare To Penalize 2,217 Hospitals for Excess Readmissions [http://www.kaiserhealthnews.org/stories/2012/august/13/medicare-hospitals-readmissions-penalties.aspx]
- 78.Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, Leong-Grotz K, Castro C, Bindman AB. Closing the loop. Physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 79.Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Qual Saf. 2012;21:876–884. doi: 10.1136/bmjqs-2011-000760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Weiner BJ. A theory of organizational readiness for change. Implement Sci. 2009;4:67. doi: 10.1186/1748-5908-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: the importance of transitional care in achieving health reform. Health Aff (Millwood) 2011;30:746–754. doi: 10.1377/hlthaff.2011.0041. [DOI] [PubMed] [Google Scholar]
- 82.Parmelli E, Flodgren G, Beyer F, Baillie N, Schaafsma ME, Eccles MP. The effectiveness of strategies to change organisational culture to improve healthcare performance: a systematic review. Implement Sci. 2011;6:33. doi: 10.1186/1748-5908-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Scott T, Mannion R, Marshall M, Davies H. Does organisational culture influence health care performance? A review of the evidence. J Health Serv Res Policy. 2003;8:105–117. doi: 10.1258/135581903321466085. [DOI] [PubMed] [Google Scholar]
- 84.Gershon RR, Stone PW, Bakken S, Larson E. Measurement of organizational culture and climate in healthcare. J Nurs Admin. 2004;34:33–40. doi: 10.1097/00005110-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 85.Agency for Healthcare Research and Quality [http://www.ahrq.gov/professionals/systems/hospital/red/toolkit/index.html] [DOI] [PubMed]
- 86.Division of Health Care Policy and Research, University of Colorado Denver. The Care Transitions Program [www.caretransitions.org]
- 87.Society of Hospital Medicine. BOOSTing Care Transitions Resource Room. Philadelphia [www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm]
Pre-publication history
- The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6963/14/389/prepub
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Modified model based on PRECEDE-PROCEED concept and the theory of planned behavior (DOCX 33 KB)
Additional file 2: Study Population Inclusion and Exclusion Criteria. (DOCX 15 KB)
Additional file 3: Matrix of change objectives. (DOCX 20 KB)


