Abstract
[Purpose] This review article is designed to expose physiotherapists to a physiotherapy assessment of stress urinary incontinence (SUI) and the treatment and possibly preventive roles that they might play for women with SUI. Specifically, the goal of this article is to provide an understanding of pelvic floor muscle function and the implications that this function has for physiotherapy treatment by reviewing articles published in this area. [Methods] A range of databases was searched to identify articles that address physiotherapy for SUI, including the Cochrane Library, Medline, and CINAHL. [Results] According to the articles identified in our databases research, greater improvements in SUI occur when women receive a supervised exercise program of at least three months. The effectiveness of physiotherapy treatment is increased if the exercise program is based on some principles, such as intensity, duration, resembling functional task, and the position in which the exercise for pelvic floor muscles is performed. Biofeedback and electrical stimulation may also be clinically useful and acceptable modalities for some women with SUI. [Conclusion] We concluded that the plan for physiotherapy care should be individualized for each patient and include standard physiotherapy interventions.
Key words: Incontinence, Physiotherapy
INTRODUCTION
Urinary incontinence (UI) is defined by the International Continence Society as an “involuntary loss of urine which is objectively a demonstrable, social, and hygienic problem”1). There are three main types of urinary incontinence: stress, urge, and mixed.
Stress urinary incontinence (SUI) is the complaint of involuntary leakage on effort or exertion or on sneezing or coughing. During effort or exertion, the intra-abdominal pressure is raised, and the urethral sphincter is unable to maintain a pressure higher than that exerted on the bladder. Subsequently, urine leakage occurs during everyday activities such as lifting, laughing, jumping, sneezing, or coughing2, 3).
Urge urinary incontinence (UUI) is the complaint of involuntary leakage accompanied by or immediately preceded by urgency. During bladder filling, the bladder contracts abnormally, which creates a sensation of the need to urinate that becomes progressively stronger, is very difficult to ignore, and ultimately results in urine leakage. UUI may be associated with overactive bladder syndrome (OAB), a condition that denotes urgency, frequency, and nocturia, with or without UUI2, 3).
Finally, mixed urinary incontinence (MUI) is the complaint of involuntary leakage associated with urgency and also with exertion, effort, sneezing, or coughing2, 3).
UI is not only a serious medical condition in that it can lead to perineal rash, pressure ulcers, and urinary tract infections but also an undeniable social problem, creating embarrassment and negative self-perception. UI has been found to reduce both social interactions and physical activities4) and is associated with poor self-rated health5), impaired emotional and psychological well-being, impaired sexual relationships, decreased quality of life6), and depressive symptoms7). Women with UI are usually inactive and in the long term become isolated from community-based activities6, 8). There is also a risk of admission to a nursing house, specifically for older women with UI9).
UI affects approximately 20 million people in the United States, and the prevalence of UI in women ranges from 26–46%10). The economic costs of UI are substantial, comprising over $16 billion per year in the United States. Subak et al. reported that community-dwelling women spend nearly $750 per year out of pocket for incontinence management11).
Physiotherapists have become involved in the clinical management of UI in women, as the presumptive underlying impairments (i.e., decreased pelvic floor muscle strength and/or endurance, decreased awareness of bladder irritants) fall within the scope of physiotherapy practice according to the Guide to Physical Therapist Practice12). Consequently, there is a growing need to understand how physiotherapy interventions impact the UI symptoms, impairments, and functional limitations of women. This review article is designed to expose physiotherapists to a physiotherapy assessment of SUI and the treatment and possibly preventive roles that they might play for women with SUI.
Admission of an increased number of women with SUI into physiotherapy clinics convinced us that control of this condition to some extent, at least from the mechanical point of view, is associated with physiotherapy interventions. Reviewing a series of categories, including the anatomy of the pelvic floor and mechanism, pathophysiology, therapeutic modalities used in physiotherapy for SUI, preventive role of pelvic floor muscle (PFM) training, and some barriers to successful physiotherapy outcomes, may help physiotherapists to obtain an insight into how SUI may be controlled in a way to improve the quality of life of a sufferer of SUI. Although a number of physiotherapy treatments have been proposed for patients with SUI, there are sufficient uncertainties and some controversies concerning the effectiveness of physiotherapy modalities, particularly due to the different treatment strategies. Uncertainty and some possible barriers in performing physiotherapy treatments for SUI patients prompted a narrative review, which might be of interest to physiotherapists managing SUI patients. Therefore, in the present review article, we reviewed the recent physiotherapy treatments for women with SUI. Specifically, our main goal was to review exercise therapy methods for strengthening the pelvic floor muscles that mainly control continence.
METHODS
A range of databases, including the Cochrane Library, Medline, and CINAHL was searched to identify articles addressing physiotherapy for SUI. The search strategy involved entry of the word physiotherapy with a combination of other words such as physiotherapy, pelvic floor muscle, pelvic floor muscle training, pelvic floor muscle exercise, biofeedback, functional electrical stimulation, stress urinary incontinence, and women or female. This is a narrative review, and we were free to choose the related high-quality evidence based on our experience. So, we were confident that we would be able to find the main answers to our question.
RESULTS AND DISCUSSION
Anatomy of the pelvic floor and mechanism of incontinence
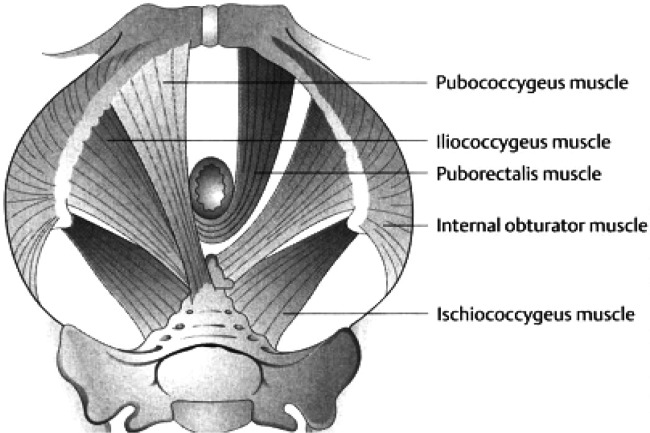
The continence mechanism is embedded within the pelvic floor structure. The pelvic floor is composed of striated muscles arranged in a dome-shaped sheet and is often described as a sling. These muscles are referred to as lying within either the deep or superficial pelvic floor. The fascia and muscles of the pelvic floor support the bladder, uterus, and rectum. Muscles specific to the deep pelvic floor include the levator ani (LA) and ischiococcygeus. The LA is composed of three muscle bellies, including the iliococcygeus, pubococcygeus, and puborectalis. The iliococcygeal and pubococcygeal muscles form a horizontal shelf or hammock that spans from one pelvic sidewall to the other and then attaches laterally to the ischial spines and arcus tendineus fascia. The puborectalis muscle arises from the pubic bone on either side and extends into a sling or U-shape around the posterior rectum, which attaches to the walls of the vagina, urethra, and rectum13, 14) (Fig. 1).
Fig. 1.
Levator ani muscles15)
Pelvic muscles and sphincters converge and attach at the perineal body. These include the anterior fibers of the LA, the transverses perinea superficialis and profundus, bulbospongiosus, external anal sphincters, and fibers from urinary sphincters13) (Fig. 1). The collective group of the LA and coccygeus muscles with the surrounding fascia is referred to as the diaphragm of the pelvis. Although it is poorly discussed, the pelvic floor has an important role in the function of core muscle stabilization. The core muscles are known as the muscles of the trunk (abdominals, quadrates lumborum, spinal muscles including the multifidus, and hip muscles), the diaphragm, and the pelvic floor. Essentially, the pelvic floor is the floor of the core14).
The opening between the LA through which the urethra, vagina, and rectum pass is the urogenital hiatus. The urogenital hiatus is anteriorly supported by the pubic bones and LA and posteriorly by the perineal membrane and external anal sphincter.
The perineal membrane is a dense triangular membrane located below the LA with a central opening through which the vagina and urethra pass. The deepest member of the perineal membrane is the external anal sphincter.
The anatomy of the continence system can be organized into those structures that provide normal support to the lower urinary tract, and those that determine urethral closure force. The structures that provide normal support include the three layers of the pelvic floor structure.
During bladder storage, activation of the sympathetic nervous system increases the tonic activity or contraction of the internal urethral sphincter to assist in preventing urine leakage.
The lower urinary tract is innervated by three sets of peripheral nerves including (i) pelvic parasympathetic nerves (S2-S4 segments) that excite the bladder, (ii) lumbar sympathetic nerves that inhibit the bladder and excite the internal urethral sphincter, and (iii) pudendal nerves that excite the external urethral sphincter and pelvic floor muscles13, 14).
Pathophysiology of SUI
The main anatomic hypotheses for development of SUI are as follows: 1) the loss of structural support, 2) the hammock, and 3) the neural hypotheses3).
Loss of structural support hypotheses: Supportive structures to the bladder neck and urethra are necessary to maintain urethral closure pressure. Intact attachments of the suburethral fascia to the fascia of the arcus tendineus and the LA construct a firm shelf that remains stable when faced with increased forces generated by a cough or sneeze14). Disruption of this shelf, such as weakness of the LA or damage to fascial attachments, as described in the loss of structural support hypotheses, could result in SUI. Aging and childbirth injury are considered the main etiological factors for LA weakness14).
The hammock hypotheses: In this hypothesis, the position of the urethra remains constant, but the compression of the pelvic floor muscles and fascia, which support the urethra, is decreased14). In a normal support system, intra-abdominal pressure pushes the urethra against the hammock-like supportive layer, and the urethral lumen closes, which in turn does not allow urine to pass. However, in the case of an abnormal supportive layer, the lumen is not closed completely, thus resulting in urine leakage13, 14).
The neural hypotheses: The main neural hypothesis for development of SUI is associated with the pudendal nerve injury. The pudendal nerve innervates the external urethral sphincter. So, any damage to the pudendal nerve (e.g., due to the recent vaginal delivery) results in SUI3).
In addition to the above mentioned hypothesis concerning UI, there are some risk factors that may result in the occurrence of SUI. These are as follows:
Childbirth15, 16), Age17), Decreased collagen content and elasticity18), Race and ethnicity15,16,17), Obesity17, 19), Smoking, chronic cough, respiratory diseases20), Pelvic surgery17), Chronic constipation20) , and Carbonated drinks19).
Furthermore, there are also some nonspecific risk factors, such as pelvic organ prolapse21), medications22), fluid intake23), fecal incontinence24), and pelvic pain20), that may result in SUI. It is worth mentioning that the coexisting pelvic symptoms might be as follows: dual incontinence and pelvic organ prolapse, constipation, sexual dysfunction, chronic pelvic pain, low back pain, and hip pain8).
Therapeutic modalities used in physiotherapy for SUI
Physiotherapy treatments for female SUI include pelvic floor physiotherapy, lifestyle and behavioral therapy, and medication8, 13, 25,26,27).
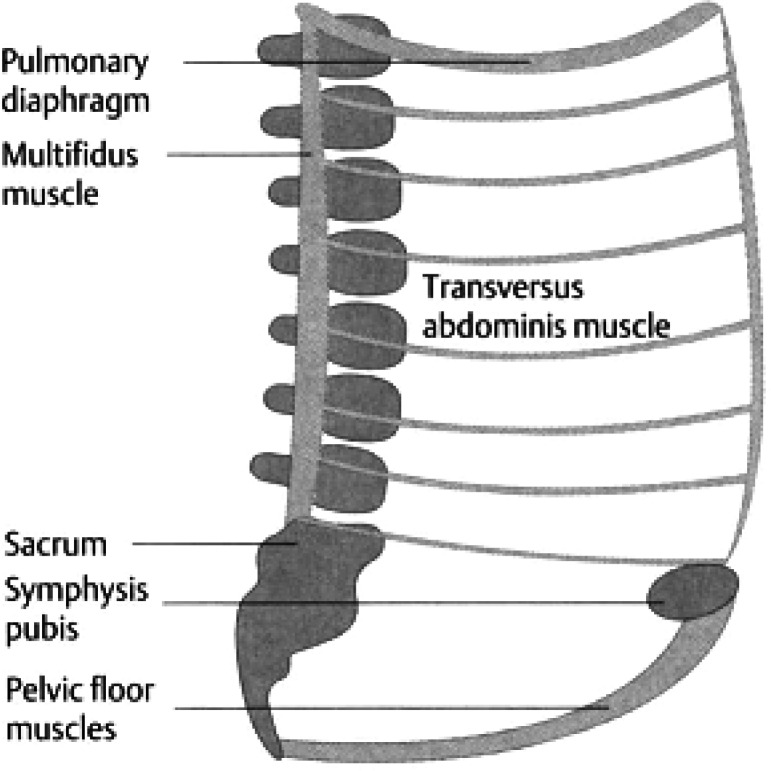
Pelvic floor physiotherapy: One of the most frequent treatments for SUI is pelvic floor muscle exercise (PFME) or specifically contraction of the LA muscle. The premise of this intervention is that strong LA muscle contraction will improve urethral closure and pelvic organ support. It is hypothesized that compression of the urethra by contraction of the pelvic floor muscle will stop urine leakage if the contraction is of sufficient force and properly timed8, 13, 25,26,27). It seems reasonable that LA muscle exercise could increase the compression function of the muscle. Since the LA muscle consists of both type I (slow twitch) and type II (fast twitch) muscle fibers, specific strength training exercises can affect type II muscle fiber size through hypertrophy. Thus, strengthening type II fibers of the LA muscle could aid the urethral sphincter in maintaining continence28). PFMEs such as Kegel exercises are taught either by verbal instruction or manual palpation, and produce contraction of the LA against intra-abdominal pressure. Specifically, strengthening and coordination of the motor control of muscles that form the abdominal cavity walls and function as primary stabilizing musculature of the lumbosacral spine (Fig. 2) are the main focus of PFME29, 30).
Fig. 2.
Abdominal cavity wall, which functions as the primary stabilizing musculature of the lumbosacral spine and as a functional unit15)
The effectiveness of PFME in women with SUI is determined by both the frequency and intensity of exercise. Performing 15 repetitions of 2 to 4 seconds of contraction in an exercise program with 3 sets per day for a period of 8 weeks, for instance, in women with mild to moderate SUI has been associated with a greater reduction in incontinence31). This exercise program was also accompanied by instruction of the “Knack” principle31). The Knack or counterbracing technique is taught by clinicians to prevent leakage during increases in abdominal pressure. The patient is taught to contract the pelvic floor muscle just prior to physical stresses such as sneezing. It is not clear, however, what contribution each intervention (PFME or behavioral training utilizing the Knack principle) made to the reduction in SUI in the patients. Another limitation of this study is associated with the short time period for muscle training. Normally, the maximal effect of strength training does not occur before 5 months of training31).
Studies in which women were trained longer and in which the effect of PFME alone on reduction of SUI was tested, reported favorable results. According to a Cochrane Review of PFME, greater improvements occur when women receive a supervised PFME program of at least three months8). It seems also likely that physiotherapy treatment effectiveness would be enhanced if the exercise prescription is based on sound physiological principles. The studies mentioned in this review are consistent in incorporating both PFM endurance and strengthening principles8).
It is worth mentioning that in addition to considering the intensity and duration of a PFME program, physiotherapists may also need to consider the body position in which the women with SUI exercise. Borello-France et al. compared the efficacy of a PFME progression that included practice in upright positions (i.e., sitting and standing) with the effectiveness of a PFME program that was performed only in the supine position in reducing SUI. They showed that the position used for PFME was not an important factor in performing exercise and the resulting reduction in SUI32). Further studies are needed to corroborate this finding concerning the positioning effects of PFME on SUI.
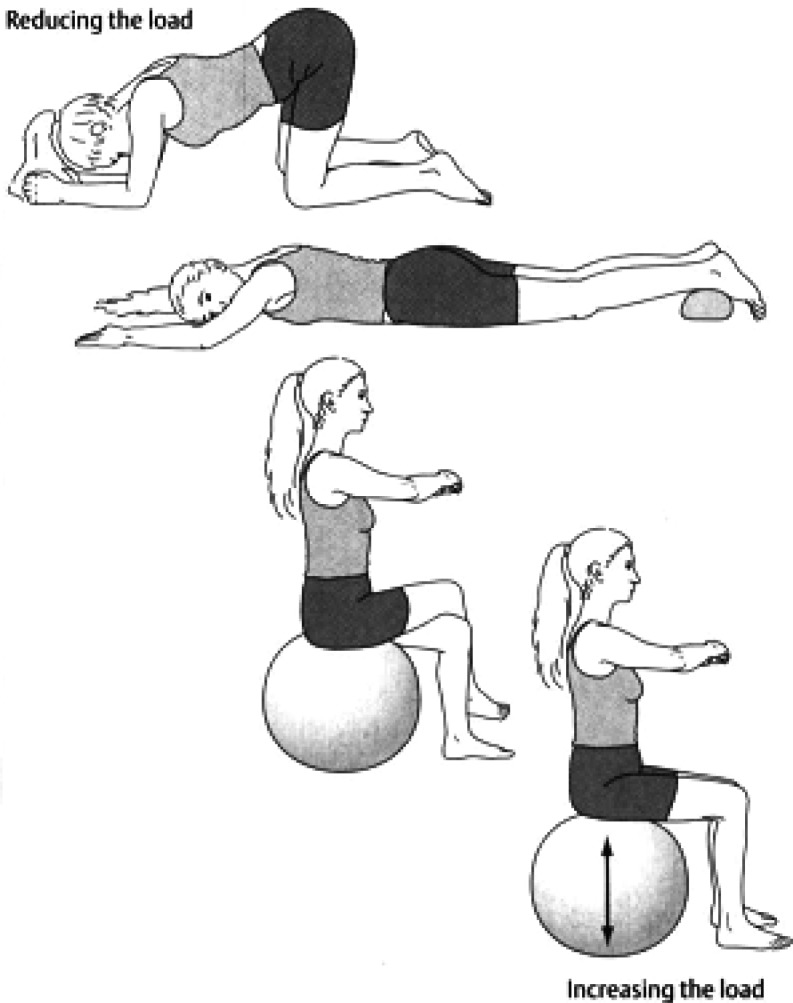
Clinically, physiotherapists utilize exercise progression from gravity-eliminated to anti-gravity positions and finally an unstable base of support such as Swiss ball exercise when strengthening the PFM (Fig. 3). We should also keep in mind that according to the specificity theory on motor tasks, greater gains in motor performance occur when practice resembles a functional task as much as possible8).
Fig. 3.
Examples of exercise progression (exercises progress from the top to bottom diagrams)15)
The main principles of therapeutic modalities used in physiotherapy for SUI can be summarized as follows:
• Pelvic floor muscle awareness is taught.
• The pelvic floor is assessed and exercised in functional positions.
• The use of anticipatory pelvic floor muscle contraction immediately prior to an activity that causes urine leakage (the “Knack” principle) is taught.
• A program of PFME is prescribed to individual patients and includes exercises for both fast and slow twitch muscle fibers.
• PFMEs are performed until the muscle fatigues, several times a day, and for 12 to 20 weeks.
• Patients are initially seen weekly, but their circumstances and/or the available resources may need to be taken into account.
• PFMEs are continued in a maintenance program25).
PFME along with Biofeedback: Correct contraction can be verified by biofeedback or manual palpation. In women, biofeedback can be obtained using small electrodes placed around the anus or by using an internal, vaginal electrode. Using biofeedback allows women to see almost instantly their muscle output during exercise.
Based on the literature, PFME with biofeedback is not more effective than PFME alone. However, PFME along with biofeedback may be a clinically useful and acceptable treatment for some women. A practical strategy may be to initiate PFME with biofeedback for those who might have difficulty in understanding how to contract or are unable to contract the PFM33). Biofeedback can also be used to teach correct PFME form.
PFME and electrical stimulation: Electrical stimulation (ES) is another intervention used by physiotherapists to reduce UI. The physiological objectives of ES are to produce muscle hypertrophy, to normalize the reflex activity of the lower urinary tract, and to increase circulation to muscles and the capillary system25, 27, 34). ES of the pudendal nerve improves urethral closure by activating the PFM. It may also increase conscious awareness of the action of these muscles to yield an improved ability to perform a voluntary muscle contraction.
With regard to a recent systematic review, ES did not differ from sham stimulation or PFME in terms of UI improvement35). However, ES is a priority for women with difficulty in contracting the PFM initially. Needless to say, substituting PFME alone for ES needs to be considered in the treatment protocol25, 27).
Cone therapy: Cone therapy can be a useful exercise and can be used as a biofeedback device using vaginal cones even in patients without a palpable voluntary contraction25).
Preventive role of PFM training
There are no studies, to our knowledge, applying PFM training for primary prevention of SUI. Theoretically, it is estimated that strengthening the PFM by specific training would have the potential to prevent SUI and pelvic organ prolapse. Strength training may increase the PFM volume and lift the levator plate to a more cranial level inside the pelvis. If the pelvic floor possesses certain amount of stiffness, it is likely that the muscles could counteract the increases in abdominal pressures that occur during physical exertion. The few studies published on prevention have concentrated on training during pregnancy or after childbirth26, 36, 37). The researchers showed that continent women had a significantly stronger PFM than incontinent women. Two other studies did not show any effect of PFM training during pregnancy or after childbirth38, 39). The interventions in these two studies were, however, weak, as the programs only consisted of one session with a midwife or a physiotherapist, respectively. There was no supervision or guiding of the training.
Barriers to successful physiotherapy outcomes
Normally, women with SUI receive physiotherapy treatment once a week for a period of 4 to 8 weeks. Instruction and performance of PFME at home are supplemented by a physiotherapy program. Thus, physiotherapy treatment when accompanied by a prescribed home exercise is likely to be successful for SUI treatment. Additionally, factors such as education, activity level, parity, smoking, child delivery type, and pelvic pain may affect the ability to correctly perform PFME38, 40).
Conclusion: From these observations, we concluded that the plan for physiotherapy care should be individualized for each patient and include standard physiotherapy interventions. As outlined in Table 1, these interventions include modalities to decrease pain, PFME with or without biofeedback and/or electrical stimulation to improve strength and coordination of the PFM, stabilization exercises to improve strength of abdominal and/or lumbar stabilizer muscles, and patient education including recommendations for bladder and/or bowel training, fluid management, and diet modification12).
Table 1. Intervention categories with evidence-based references of justification noted.
| Modalities | Heat41) |
| Ice41) | |
| PFM biofeedback33, 34) | |
| • To promote strength and endurance | |
| • To increase coordination | |
| • To promote muscle relaxation | |
| PFM electrical stimulation31, 34) | |
| • To improve PFM strength (if 2/5 PFM strength) | |
| • To promote sensory awareness due to sensory impairment | |
| • To reduce pain | |
| Manual physiotherapy procedures | Soft tissue mobilization to decrease soft tissue
restriction and improve range of motion42, 43) Joint mobilization to improve range of motion44) |
| Exercises | PFME32, 33, 45, 46) |
| • Manual facilitation | |
| • Gravity eliminated | |
| • Anti-gravity | |
| • During functional tasks | |
| • Down training | |
| Core stabilization47, 48) | |
| • Transverse abdominis muscle | |
| • Other abdominal muscles | |
| • Multifidus muscle | |
| • Functional exercises | |
| Flexibility | |
| • Hip41) | |
| • Lumbopelvic49) | |
| Education | Body mechanics/posture44) |
| Bladder/bowel schedule50) | |
| Diet modification | |
| • Caffeine reduction51) | |
| • Carbonated beverage reduction51) | |
| • Increase water intake52) | |
| • Decrease water intake53) | |
| • Fiber education52) | |
| Relaxation techniques to decrease muscle tension54) | |
| SUI strategies such as PFM contraction before increase in intra-abdominal pressure55) | |
| UUI strategies such as inhibition techniques to suppress bladder contractions56) | |
| Toilet strategies | |
| • For constipation such as toilet posture to promote bowel movement57) | |
| • Voiding without straining | |
| Soft tissue massage such as abdominal massage, scar massage, and self-stretching for introitus34, 43, 57) |
REFERENCES
- 1.Abrams P, Cardozo L, Fall M, et al. Standardisation Sub-committee of the International Continence Society: The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn, 2002, 21: 167–178 [DOI] [PubMed] [Google Scholar]
- 2.Wein AJ, Rovner ES: Definition and epidemiology of overactive bladder. Urology, 2002, 60: 7–12, discussion 12. [DOI] [PubMed] [Google Scholar]
- 3.Cannon TW, Damaser M: Pathophysiology of the lower urinary tract: continence and incontinence. Clin Obstet Gynecol, 2004, 47: 28–35 [DOI] [PubMed] [Google Scholar]
- 4.Wyman JF, Harkins SW, Fantl JA: Psychosocial impact of urinary incontinence in the community-dwelling population. J Am Geriatr Soc, 1990, 38: 282–288 [DOI] [PubMed] [Google Scholar]
- 5.Johnson TM, 2nd, Kincade JE, Bernard SL, et al. : The association of urinary incontinence with poor self-rated health. J Am Geriatr Soc, 1998, 46: 693–699 [DOI] [PubMed] [Google Scholar]
- 6.Temml C, Haidinger G, Schmidbauer J, et al. : Urinary incontinence in both sexes: prevalence rates and impact on quality of life and sexual life. Neurourol Urodyn, 2000, 19: 259–271 [DOI] [PubMed] [Google Scholar]
- 7.Dugan E, Cohen SJ, Bland DR, et al. : The association of depressive symptoms and urinary incontinence among older adults. J Am Geriatr Soc, 2000, 48: 413–416 [DOI] [PubMed] [Google Scholar]
- 8.Hay-Smith EJ, Dumoulin C: Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev, 2006, 25: CD005654 [DOI] [PubMed] [Google Scholar]
- 9.Hunskaar S, Burgio K, Diokno A, et al. : Epidemiology and natural history of urinary incontinence in women. Urology, 2003, 62: 16–23 [DOI] [PubMed] [Google Scholar]
- 10.Wilson L, Brown JS, Shin GP, et al. : Annual direct cost of urinary incontinence. Obstet Gynecol, 2001, 98: 398–406 [DOI] [PubMed] [Google Scholar]
- 11.Subak LL, Brubaker L, Chai TC, et al. Urinary Incontinence Treatment Network: High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstet Gynecol, 2008, 111: 899–907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Physiotherapy Association: Guide to Physical Therapist Practice, 2nd ed. American Physical Therapy Association.81. Alexandria, 2001 [Google Scholar]
- 13.Prather H, Dugan S, Fitzgerald C, et al. : Review of anatomy, evaluation, and treatment of musculoskeletal pelvic floor pain in women. PM R, 2009, 1: 346–358 [DOI] [PubMed] [Google Scholar]
- 14.Wei JT, De Lancey JO: Functional anatomy of the pelvic floor and lower urinary tract. Clin Obstet Gynecol, 2004, 47: 3–17 [DOI] [PubMed] [Google Scholar]
- 15.Pregazzi R, Sartore A, Troiano L, et al. : Postpartum urinary symptoms: prevalence and risk factors. Eur J Obstet Gynecol Reprod Biol, 2002, 103: 179–182 [DOI] [PubMed] [Google Scholar]
- 16.Waetjen LE, Liao S, Johnson WO, et al. : Factors associated with prevalent and incident urinary incontinence in a cohort of midlife women: a longitudinal analysis of data: study of women’s health across the nation. Am J Epidemiol, 2007, 165: 309–318 [DOI] [PubMed] [Google Scholar]
- 17.Minassian VA, Stewart WF, Wood GC: Urinary incontinence in women: variation in prevalence estimates and risk factors. Obstet Gynecol, 2008, 111: 324–331 [DOI] [PubMed] [Google Scholar]
- 18.Wong MY, Harmanli OH, Agar M, et al. : Collagen content of nonsupport tissue in pelvic organ prolapse and stress urinary incontinence. Am J Obstet Gynecol, 2003, 189: 1597–1599, discussion 1599–1600. [DOI] [PubMed] [Google Scholar]
- 19.Dallosso HM, McGrother CW, Matthews RJ, et al. Leicestershire MRC Incontinence Study Group: The association of diet and other lifestyle factors with overactive bladder and stress incontinence: a longitudinal study in women. BJU Int, 2003, 92: 69–77 [DOI] [PubMed] [Google Scholar]
- 20.Zhu L, Lang J, Liu C, et al. : The epidemiological study of women with urinary incontinence and risk factors for stress urinary incontinence in China. Menopause, 2009, 16: 831–836 [DOI] [PubMed] [Google Scholar]
- 21.Barber MD: Symptoms and outcome measures of pelvic organ prolapse. Clin Obstet Gynecol, 2005, 48: 648–661 [DOI] [PubMed] [Google Scholar]
- 22.Holroyd-Leduc JM, Straus SE: Management of urinary incontinence in women: scientific review. JAMA, 2004, 291: 986–995 [DOI] [PubMed] [Google Scholar]
- 23.Sutherland SE, Goldman HB: Treatment options for female urinary incontinence. Med Clin North Am, 2004, 88: 345–366 [DOI] [PubMed] [Google Scholar]
- 24.Markland AD, Richter HE, Kenton KS, et al. Urinary Incontinence Treatment Network: Associated factors and the impact of fecal incontinence in women with urge urinary incontinence: from the Urinary Incontinence Treatment Network’s Behavior Enhances Drug Reduction of Incontinence study. Am J Obstet Gynecol, 2009, 200: e1–e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laycock J: Clinical guidelines for the physiotherapy management of females aged 16–65 years with stress urinary incontinence. London: Chartered Society of Physiotherapy, 2001 [Google Scholar]
- 26.Bø K: Urinary incontinence, pelvic floor dysfunction, exercise and sport. Sports Med, 2004, 34: 451–464 [DOI] [PubMed] [Google Scholar]
- 27.Bernards ATM, Berghmans LCM, van Heeswijk-Faase IC, et al. : KNGF Guideline for physical therapy in patients with stress urinary incontinence. de Fysiotherapeut Royal Dutch Society for Physical Therapy, 2011, 121: 1–43.
- 28.Cammu H, Van Nylen M, Blockeel C, et al. : Who will benefit from pelvic floor muscle training for stress urinary incontinence? Am J Obstet Gynecol, 2004, 191: 1152–1157 [DOI] [PubMed] [Google Scholar]
- 29.Bo K, Berghmans B, Mørkved S, et al.: Evidence-Based Physical Therapy for the Pelvic Floor: Bridging Science and Clinical Practice. Churchill Livinsgtone, 2007 [Google Scholar]
- 30.Carriere B, Feldt C: The pelvic floor. New York: Georg Thieme Verlag, 2006 [Google Scholar]
- 31.Goode PS, Burgio KL, Locher JL, et al. : Effect of behavioral training with or without pelvic floor electrical stimulation on stress incontinence in women: a randomized controlled trial. JAMA, 2003, 290: 345–352 [DOI] [PubMed] [Google Scholar]
- 32.Borello-France DF, Zyczynski HM, Downey PA, et al. : Effect of pelvic-floor muscle exercise position on continence and quality-of-life outcomes in women with stress urinary incontinence. Phys Ther, 2006, 86: 974–986 [PubMed] [Google Scholar]
- 33.Mørkved S, Bø K, Fjørtoft T: Effect of adding biofeedback to pelvic floor muscle training to treat urodynamic stress incontinence. Obstet Gynecol, 2002, 100: 730–739 [DOI] [PubMed] [Google Scholar]
- 34.Sand PK, Richardson DA, Staskin DR, et al. : Pelvic floor electrical stimulation in the treatment of genuine stress incontinence: a multicenter, placebo-controlled trial. Am J Obstet Gynecol, 1995, 173: 72–79 [DOI] [PubMed] [Google Scholar]
- 35.Yamanishi T, Yasuda K, Sakakibara R, et al. : Pelvic floor electrical stimulation in the treatment of stress incontinence: an investigational study and a placebo controlled double-blind trial. J Urol, 1997, 158: 2127–2131 [DOI] [PubMed] [Google Scholar]
- 36.Oskouei Ali E, Ghaderi F: Physiotherapy management in prenatal and postnatal women with urinary incontinence. Iran J Reprod Med, 2012, 10: 95–96 [Google Scholar]
- 37.Hay-Smith J, Herbison P, Mørkved S: Physical therapies for prevention of urinary and faecal incontinence in adults (Review) Cochrane Database Syst Rev, 2002, 3: CD003191 [DOI] [PubMed] [Google Scholar]
- 38.Bø K, Owe KM, Nystad W: Which women do pelvic floor muscle exercises six months’ postpartum? Am J Obstet Gynecol, 2007, 197: e1–e5 [DOI] [PubMed] [Google Scholar]
- 39.Reilly ET, Freeman RM, Waterfield MR, et al. : Prevention of postpartum stress incontinence in primigravidae with increased bladder neck mobility: a randomised controlled trial of antenatal pelvic floor exercises. BJOG, 2002, 109: 68–76 [DOI] [PubMed] [Google Scholar]
- 40.Fine P, Burgio K, Borello-France D, et al. Pelvic Floor Disorders Network: Teaching and practicing of pelvic floor muscle exercises in primiparous women during pregnancy and the postpartum period. Am J Obstet Gynecol, 2007, 197: e1–e5 [DOI] [PubMed] [Google Scholar]
- 41.Prather H, Spitznagle TM, Dugan SA: Recognizing and treating pelvic pain and pelvic floor dysfunction. Phys Med Rehabil Clin N Am, 2007, 18: 477–496, ix. [DOI] [PubMed] [Google Scholar]
- 42.Weiss JM: Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J Urol, 2001, 166: 2226–2231 [DOI] [PubMed] [Google Scholar]
- 43.Oyama IA, Rejba A, Lukban JC, et al. : Modified Thiele massage as therapeutic intervention for female patients with interstitial cystitis and high-tone pelvic floor dysfunction. Urology, 2004, 64: 862–865 [DOI] [PubMed] [Google Scholar]
- 44.Prendergast SA, Weiss JM: Screening for musculoskeletal causes of pelvic pain. Clin Obstet Gynecol, 2003, 46: 773–782 [DOI] [PubMed] [Google Scholar]
- 45.Aukee P, Immonen P, Penttinen J, et al. : Increase in pelvic floor muscle activity after 12 weeks’ training: a randomized prospective pilot study. Urology, 2002, 60: 1020–1023, discussion 1023–1024. [DOI] [PubMed] [Google Scholar]
- 46.Bø K, Finckenhagen HB: Is there any difference in measurement of pelvic floor muscle strength in supine and standing position? Acta Obstet Gynecol Scand, 2003, 82: 1120–1124 [DOI] [PubMed] [Google Scholar]
- 47.Sapsford RR, Richardson CA, Maher CF, et al. : Pelvic floor muscle activity in different sitting postures in continent and incontinent women. Arch Phys Med Rehabil, 2008, 89: 1741–1747 [DOI] [PubMed] [Google Scholar]
- 48.Sapsford R: Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man Ther, 2004, 9: 3–12 [DOI] [PubMed] [Google Scholar]
- 49.Burgio KL, Goode PS, Locher JL, et al. : Predictors of outcome in the behavioral treatment of urinary incontinence in women. Obstet Gynecol, 2003, 102: 940–947 [DOI] [PubMed] [Google Scholar]
- 50.Subak LL, Quesenberry CP, Posner SF, et al. : The effect of behavioral therapy on urinary incontinence: a randomized controlled trial. Obstet Gynecol, 2002, 100: 72–78 [DOI] [PubMed] [Google Scholar]
- 51.Arya LA, Myers DL, Jackson ND: Dietary caffeine intake and the risk for detrusor instability: a case-control study. Obstet Gynecol, 2000, 96: 85–89 [DOI] [PubMed] [Google Scholar]
- 52.Shariati A, Maceda JS, Hale DS: High-fiber diet for treatment of constipation in women with pelvic floor disorders. Obstet Gynecol, 2008, 111: 908–913 [DOI] [PubMed] [Google Scholar]
- 53.Hashim H, Abrams P: How should patients with an overactive bladder manipulate their fluid intake? BJU Int, 2008, 102: 62–66 [DOI] [PubMed] [Google Scholar]
- 54.Fisher KA: Management of dyspareunia and associated levator ani muscle overactivity. Phys Ther, 2007, 87: 935–941 [DOI] [PubMed] [Google Scholar]
- 55.Miller JM, Perucchini D, Carchidi LT, et al. : Pelvic floor muscle contraction during a cough and decreased vesical neck mobility. Obstet Gynecol, 2001, 97: 255–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang AC, Wang YY, Chen MC: Single-blind, randomized trial of pelvic floor muscle training, biofeedback-assisted pelvic floor muscle training, and electrical stimulation in the management of overactive bladder. Urology, 2004, 63: 61–66 [DOI] [PubMed] [Google Scholar]
- 57.Harrington KL, Haskvitz EM: Managing a patient’s constipation with physical therapy. Phys Ther, 2006, 86: 1511–1519 [DOI] [PubMed] [Google Scholar]