Abstract
Background and Purpose
Dietary potassium has been associated with lower risk of stroke but there is little data on dietary potassium effects on different stroke subtypes or in older hypertensive and non-hypertensive women.
Methods
The study population consisted of 90,137 postmenopausal women aged 50–79 at enrollment, free of stroke history at baseline, followed prospectively for an average of 11 years. Outcome variables were total, ischemic, and hemorrhagic stroke, and all-cause mortality. Incidence was compared across quartiles of dietary potassium intake and hazard ratios were obtained from Cox proportional hazards models after adjusting for potential confounding variables, and in hypertensive and non-hypertensive women separately.
Results
Mean dietary potassium intake was 2611 mg/day. Highest quartile of potassium intake was associated with lower incidence of ischemic and hemorrhagic stroke, and total mortality. Multivariate analyses comparing highest to lowest quartile of potassium intake, indicated a hazard ratio (HR) for all-cause mortality of 0.90 (95% CI: 0.85 – 0.95), for all stroke of HR=0.88 (95% CI: 0.79 – 0.98), and for ischemic stroke of 0.84 (95% CI: 0.74 – 0.96). The effect on ischemic stroke was more apparent in non-hypertensive women among whom there was a 27% lower risk with HR of 0.73 (95% CI: 0.60 – 0.88), interaction p-value <.10. There was no association with hemorrhagic stroke.
Conclusions
High potassium intake is associated with a lower risk of all stroke and ischemic stroke as well as all-cause mortality in older women, particularly those who are not hypertensive.
Keywords: stroke, dietary potassium, hypertension, Women’s Health Initiative
Introduction
Stroke is the fourth leading cause of mortality in the United States, and women account for 60 percent of all US stroke cases1. Women also have a higher lifetime risk of stroke than men2. There is interest in studying lifestyle factors, such as diets rich in potassium, that may reduce stroke risk.
Evidence from prospective studies suggests that higher dietary potassium intake is associated with reduced risk of stroke3, 4,5. Three studies have specifically reported the effects of dietary potassium on risk of stroke in women. Khaw and Barret-Connor3 found that women consuming less than 49mmol (1911mg) of potassium had a relative risk of 4.8 (p = 0.01) as compared to women eating more than 49mmol of potassium. Iso6 found that women in the highest quintile of potassium intake (median of 3555mg) vs the lowest quintile (median of 2017mg) had a relative risk of 0.72 (95% CI, 0.51–1.01). Larsson7 in the Swedish Mammography Cohort, found that women with a history of hypertension had a relative risk of 0.64 (0.45–0.92) for all stroke types when comparing highest quintile of potassium intake to lowest quintile (mean = 3,845mg vs 2,363mg). In contrast, The EPIC-NL study (European Prospective Investigation into Cancer and Nutrition – Netherlands)8, found that potassium intake was not associated with stroke. Despite these useful contributions, it remains unclear whether higher dietary potassium intake is associated with reduced risk of all subtypes of stroke and whether these findings are especially relevant in specific population subgroups.
The Women’s Health Initiative Observational Study (WHI-OS), the largest prospective cohort study of post-menopausal women with long-term follow-up, was used to assess whether higher dietary potassium consumption is associated with reduced risk of total, ischemic or hemorrhagic stroke, and all-cause mortality. We also evaluated effects on ischemic stroke subtypes as determined by the TOAST, Trial of ORG 10172 Acute Stroke Trial, classification, which previous studies have not investigated.
Subjects and Methods
Study Population
A detailed description of the WHI-OS is published9. Briefly, between 1993 and 1998, 93,676 women aged 50 to 79 years were recruited from 40 states and followed prospectively for a mean of 11.1 years (range = 0.14 to 16.0 years). We excluded women with history of stroke at baseline (n = 1354), women with missing information on history of stroke (N=54), those with no information on dietary potassium (n=96). Finally, we also excluded as outliers n= 2035 women in the bottom 1% of caloric intake (less than 465 calories), whose potassium intake ranged from 0.07–1790mg, and women in the top 1% of caloric intake (more than 3931 calories) whose potassium intakes ranged from 1507–31,129mg. We therefore had an analytic cohort of 90,137.
Dietary Assessment of Potassium
Participants completed food frequency questionnaires (FFQ) at enrollment and Year 3 of follow-up. Details regarding diet assessment and the FFQs have been described elsewhere 9, 10. Briefly, participants completed questionnaires that reflected their dietary habits over the three months prior to enrollment. The questionnaire consisted of three sections: adjustment questions, food line items, and summary questions. The nineteen adjustment questions allowed for more detailed analysis of fat intake by asking participants how foods were prepared. The list of 122 food line items specified type and frequency of various foods and food group intake according to small, medium or large portion sizes. The four summary questions asked about intake of fruits, vegetables, and fat added to foods or in cooking. The FFQ nutrient database was derived from the University of Minnesota Nutrition Coordinating Center Nutrient Data for Scientific Research (NDSR) database for women in our analytic cohort.
Measurement properties of the WHI FFQ were evaluated in a sub-cohort of WHI, and found to be similar to other dietary assessments used in the WHI, such as dietary recalls10. The Pearson correlation coefficient between the FFQ and 8 days of dietary intake from combined 4 days of dietary recalls plus 4 days of food records was 0.58 for dietary potassium10. In our own analysis, the correlation between intake at baseline and intake at year 3 in the WHI Observational study was 0.63 indicating that potassium intake is fairly stable.
Ascertainment of Health Outcome
Ascertainment of death was determined based on the death certificate, medical records, or other records such as autopsy report11. Mortality cause was initially adjudicated by a local physician adjudicator at the Clinical Centers for the WHI, and then centrally adjudicated by two physicians. The two central adjudicators were required to review all deaths and come to agreement before closing the case.
Stroke was initially identified through self-report at annual visits, and medical records were then requested. Stroke was defined as rapid onset of neurologic deficit lasting more than 24 hours and without evidence of other causes. Outcomes were adjudicated by a local physician adjudicator who then assigned a diagnosis based on medical records and WHI criteria, which have been defined elsewhere12,13. More than 95% of WHI stroke classification was based on MRI or CT findings13. Neurologists then centrally adjudicated locally determined strokes. A comparison of adjudicated strokes in the WHI versus stroke events defined in Medicare data showed substantial agreement between the two for all stroke (kappa=0.69)14, suggesting that WHI stroke ascertainment is a valid measure of stroke outcome.
Stroke was classified as ischemic stroke if diagnosis revealed an occlusion of cerebral or pre-cerebral arteries with infarction (cerebral thrombosis, cerebral embolism, or lacunar infarction)12, 13. Central adjudicators then further classified ischemic stroke according to the TOAST (Trial of ORG 10172 Acute Stroke Trial) classification. The TOAST Classification is based on presumed underlying stroke etiology, and requires detailed investigation through brain imaging and methods described elsewhere12, 15. Stroke was classified as hemorrhagic if diagnosis revealed a subarachnoid hemorrhage, intracerebral hemorrhage, or other intracranial hemorrhage not resulting from a procedure12, 16.
Measurements of Covariates
Participants completed demographic and lifestyle questionnaires and physical measurements during baseline visits to a WHI Clinical Center. Demographic factors included date of birth and ethnicity (categories consistent with the 1990 US Census). Body mass index (BMI) was calculated by dividing weight in kilograms by the square of the height in meters. Past smokers were those who self-reported having smoked at least 100 cigarettes and were currently not smoking. Alcohol intake was defined as number of drinks in a given time. Women were classified as hypertensive if they were either taking anti-hypertensive medications or had a systolic blood pressure ≥ 140, or a diastolic blood pressure ≥ 90. Participants who had ever taken any aspirin containing medications were classified as aspirin users. Participants who took hormone therapy (HT) for more than three months but were not currently using HT were classified as past HT users. HT was based on estrogen and progesterone pill and patches only; creams and shots were excluded. Self-report of doctor diagnosis was used for diabetes (sugar related diabetes when not pregnant), for history of myocardial infarction (MI) and for having high cholesterol requiring pills. Recreational physical activity was assessed using information about frequency, duration and intensity of activity, and organized into categories of activity as described elsewhere9.
Statistical Methods/Analysis
Quartiles of dietary potassium were obtained. We examined the means and 95% confidence intervals (95%CI) of dietary potassium by demographic variables and by covariates that have been reported to increase the risk of stroke. All probability values for any differences across the various categories of each covariate were obtained by analysis of variance or chi-square. We also calculated the incidence of stroke and death per thousand person-years across quartiles of potassium intake and did linear trend analyses.
Hazard ratios (HRs) were estimated from Cox proportional hazards models comparing highest quartile to lowest quartile of potassium intake. We also considered an analysis of potassium per kilocalorie (K/Kcal) using quartile cutpoints of K/Kcal. However, since absolute potassium is more stably assessed with FFQ than are calories, an estimate of effect of nutrient density on stroke would not be as reliable. The correlation between potassium assessed by FFQ and 8 days of dietary records is 0.58, while the corresponding correlation for calories is 0.37 10. Since potassium intake may be related to blood pressure, and since hypertension may be in the pathway between potassium intake and stroke, and also because hypertension is a major risk factor for stroke, we considered hypertensive status a priori for stratified analyses. Follow up time was calculated in months from the date of enrollment to the date of first stroke, death, or end of the follow-up whichever came first. Model 1 is unadjusted, model 2 is adjusted for age, race and hypertension status, and model 3 is adjusted for model 2 variables plus smoking, recreational physical activity, history of diabetes, history of myocardial infarction (MI), hormone use, alcohol intake, aspirin use, high cholesterol requiring pills, and BMI. We examined each of these variables separately for interaction with potassium intake by including an interaction term of the variable and potassium intake in model 3 for ischemic stroke. When the interaction terms were significant with p<.10, we did stratified analyses for that variable. Statistical analyses were performed using SAS software (SAS Institute Inc, Cary, NC).
Results
The analytic cohort of 90,137 post-menopausal women with no history of stroke at baseline, had mean age 63.6 years at baseline, standard deviation (SD) 7.4 years. Mean dietary potassium intake was 2611 mg/day. Blacks, current smokers, and non-drinkers of alcohol reported lower dietary potassium intakes (Table 1). Those who reported 2 or more episodes of recreational physical activity a week had greater dietary potassium intake than those who reported limited or no activity.
Table 1.
Baseline potassium intake by characteristics
| Dietary Potassium (mg) | |||
|---|---|---|---|
|
| |||
| N | Mean (95% CI) | p value* | |
|
| |||
| Whole Cohort | 90137 | 2611 (2605 – 2618) | |
|
| |||
| Age | |||
| 50 – 59 | 28675 | 2589 (2578 – 2600) | <0.001 |
| 60 – 69 | 39739 | 2625 (2615 – 2634) | |
| 70–79+ | 21723 | 2616 (2603 – 2629) | |
|
| |||
| Ethnicity | |||
| White | 75842 | 2684 (2678 – 2691) | <0.001 |
| Black | 6848 | 2145 (2122 – 2168) | |
| Hispanic | 3301 | 2274 (2240 – 2309) | |
| Other | 3909 | 2304 (2274 – 2335) | |
|
| |||
| Education | |||
| 0–8 years or Some High School | 4353 | 2199 (2170 – 2228) | <0.001 |
| High School diploma - Some college | 47004 | 2519 (2511 – 2528) | |
| College graduate or Post-graduate | 38061 | 2772 (2763 – 2782) | |
|
| |||
| Income | |||
| < $20000 | 12897 | 2428 (2411 – 2446) | <0.001 |
| $20000 – $49999 | 36353 | 2609 (2599 – 2619) | |
| ≥ $50000 | 34334 | 2692 (2682 – 2702) | |
| Don’t know | 2608 | 2506 (2467 – 2545) | |
|
| |||
| Marital Status | |||
| Never | 4232 | 2655 (2624 – 2685) | <0.001 |
| Divorced or separated | 13991 | 2537 (2520 – 2553) | |
| Widowed | 15410 | 2560 (2544 – 2576) | |
| Presently married | 54619 | 2642 (2634 – 2650) | |
| Marriage like relationship | 1459 | 2591 (2542 – 2639) | |
|
| |||
| Smoking History | |||
| Current | 5441 | 2362 (2337 – 2387) | <0.001 |
| Past | 38194 | 2646 (2637 – 2656) | |
| Never | 45239 | 2613 (2603 – 2622) | |
|
| |||
| Alcohol Intake | |||
| None/Non-drinker | 9809 | 2429 (2409 – 2449) | <0.001 |
| Past Drinker | 16455 | 2527 (2511 – 2542) | |
| <1 drink per month | 10347 | 2537 (2519 – 2556) | |
| <1 drink per week | 18105 | 2608 (2594 – 2622) | |
| 1 – <7 drinks per week | 23371 | 2709 (2697 – 2721) | |
| 7+ drinks per week | 11474 | 2769 (2752 – 2785) | |
|
| |||
| Recreational Physical Activity | |||
| No activity | 11904 | 2341 (2324 – 2358) | <0.001 |
| Some activity of limited duration | 34071 | 2534 (2524 – 2545) | |
| 2 – < 4 episodes/wk | 16603 | 2679 (2665 – 2693) | |
| 4 episodes/wk | 26559 | 2791 (2779 – 2802) | |
|
| |||
| Hormone Use | |||
| Current | 43123 | 2630 (2621 – 2639) | <0.001 |
| Past | 18663 | 2604 (2590 – 2618) | |
| Never | 26732 | 2582 (2570 – 2594) | |
|
| |||
| Weight status, Body Mass Index (BMI, kg/m2) | |||
| Underweight (<18.5) | 1066 | 2550 (2491 – 2608) | 0.039 |
| Normal (18.5 – 24.9) | 35638 | 2616 (2606 – 2626) | |
| Overweight (25.0 – 29.9) | 30348 | 2606 (2596 – 2617) | |
| Obesity I (30.0 – 34.9) | 13859 | 2602 (2586 – 2619) | |
| Obesity II (35.0 – 39.9) | 5120 | 2628 (2600 – 2656) | |
| Extreme Obesity III (>= 40.0) | 3058 | 2610 (2574 – 2646) | |
|
| |||
| Systolic Blood Pressure | |||
| ≤120 | 36057 | 2633 (2623 – 2643) | <0.001 |
| 120–140 | 35947 | 2607 (2597 – 2617) | |
| >140 | 18011 | 2576 (2561 – 2590) | |
|
| |||
| Diastolic Blood Pressure | |||
| <90 | 84347 | 2616 (2610 – 2623) | <0.001 |
| ≥90 | 5649 | 2538 (2512 – 2564) | |
|
| |||
| Hypertension (if self-reported treatment or BP ≥140/90) | |||
| Yes | 34277 | 2573 (2563 – 2583) | <0.001 |
| No | 54635 | 2637 (2629 – 2645) | |
|
| |||
| High Cholesterol (requiring pills ever) | |||
| Yes | 12991 | 2574 (2557 – 2590) | <0.001 |
| No | 75171 | 2620 (2613 – 2627) | |
|
| |||
| Aspirin Use (Any) | |||
| Yes | 31768 | 2679 (2668 – 2689) | <0.001 |
| No | 58369 | 2575 (2567 – 2582) | |
|
| |||
| History of Diabetes | |||
| Yes | 4855 | 2558 (2529 – 2587) | <0.001 |
| No | 85205 | 2614 (2608 – 2621) | |
|
| |||
| History of MI | |||
| Yes | 2020 | 2534 (2490 – 2577) | <0.001 |
| No | 88056 | 2613 (2607 – 2619) | |
|
| |||
| History of Atrial Fibrillation | |||
| Yes | 4089 | 2624 (2594 – 2655) | 0.821 |
| No | 84603 | 2613 (2606 – 2619) | |
|
| |||
| History of CABG/PTCA | |||
| Yes | 1602 | 2535 (2486 – 2583) | <0.001 |
| No | 87121 | 2615 (2608 – 2621) | |
|
| |||
| History of CHD | |||
| Yes | 2871 | 2547 (2511 – 2584) | <0.001 |
| No | 85863 | 2616 (2609 – 2622) | |
p values were obtained from chi-square tests or analyses of variance across the various categories of each covariate.
Stroke Incidence
Incidence per 1000 person years was 3.10 for all stroke, 2.24 for ischemic stroke, 0.50 for hemorrhagic stroke and 11.60 for all-cause mortality. Those in the lowest quartile of estimated dietary potassium intake (<1925.5mg potassium) had higher estimated incidence than those in other quartiles across all outcomes (Table 2). There was a statistically significant linear trend for mortality (p=.0002) but the linear trend test did not reach statistical significance for the other outcomes.
Table 2.
All-cause mortality and stroke rates by quartiles of dietary potassium intake
| All-cause mortality | Stroke (all) | Stroke (no Hx of MI) | Ischemic Stroke | Hemorrhagic Stroke | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Quartiles of Dietary Potassium (mg) |
Participant number |
Event number |
Annualized rate* |
Event number |
Annualized rate* |
Event number |
Annualized rate* |
Event number |
Annualized rate* |
Event number |
Annualized rate* |
| Q1: < 1925.5 | 22534 | 3096 | 13.03 | 793 | 3.40 | 750 | 3.29 | 574 | 2.48 | 125 | 0.55 |
| Q2: ≥1925.5 – 2519.4 | 22534 | 2921 | 11.65 | 769 | 3.12 | 732 | 3.03 | 542 | 2.21 | 128 | 0.53 |
| Q3:>2519.4 – 3193.6 | 22535 | 2685 | 10.52 | 719 | 2.86 | 687 | 2.78 | 530 | 2.12 | 106 | 0.43 |
| Q4: >=3193.6 | 22534 | 2894 | 11.30 | 765 | 3.03 | 734 | 2.96 | 544 | 2.17 | 125 | 0.51 |
|
| |||||||||||
| Overall | 90137 | 11596 | 11.60 | 3046 | 3.10 | 2903 | 3.01 | 2190 | 2.24 | 484 | 0.50 |
p for trend for all cause mortality = .0002, no significance for other endpoints
Annualized rate is defined as number of events per 1000 person years
Dietary Potassium and Stroke Risk
Table 3 shows a statistically significant lower risk in all quartiles of potassium intake compared to lowest quartile, for all-cause mortality, all stroke, and ischemic stroke, in unadjusted, age-race -hypertension adjusted, and multivariate adjusted models (Table 3). In a sensitivity analysis excluding those with previous MI, the hazard ratios and confidence intervals were similar to those for all stroke (data not shown). The HR in the fully adjusted model comparing highest quartile (Q4) to the lowest quartile (Q1) of potassium intake, was 0.90 (95%CI 0.85–0.95) for all-cause mortality, 0.88 (95%CI 0.79–0.98) for all stroke, and 0.84, (95% CI 0.74–0.96) for ischemic stroke. There was no association with hemorrhagic stroke.
Table 3.
Hazard Ratios for All-cause mortality and Stroke by Quartiles of Potassium
| Quartiles of Potassium (mg) | ||||
|---|---|---|---|---|
|
| ||||
| Q1: < 1925.5 | Q2: ≥1925.5 – 2519.4 (HR, 95% CI) | Q3:>2519.4 – 3193.6 (HR, 95% CI) | Q4: >3193.6 (HR, 95% CI) | |
| All-Cause Mortality | ||||
| Model (1) | 1 | 0.87 (0.82 – 0.91) | 0.77 (0.74 – 0.82) | 0.83 (0.79 – 0.87) |
| Model (2) | 1 | 0.87 (0.82 – 0.91) | 0.78 (0.74 – 0.82) | 0.83 (0.79 – 0.87) |
| Model (3) | 1 | 0.91 (0.86 – 0.96) | 0.84 (0.79 – 0.89) | 0.90 (0.85 – 0.95) |
|
| ||||
| Stroke (all) | ||||
| Model (1) | 1 | 0.89 (0.81 – 0.99) | 0.82 (0.74 – 0.91) | 0.87 (0.79 – 0.96) |
| Model (2) | 1 | 0.90 (0.81 – 1.00) | 0.83 (0.75 – 0.92) | 0.88 (0.79 – 0.97) |
| Model (3) | 1 | 0.88 (0.79 – 0.98) | 0.85 (0.76 – 0.94) | 0.88 (0.79 – 0.98) |
|
| ||||
| Ischemic Stroke | ||||
| Model (1) | 1 | 0.88 (0.78 – 0.99) | 0.84 (0.74 – 0.94) | 0.85 (0.76 – 0.96) |
| Model (2) | 1 | 0.88 (0.78 – 0.99) | 0.85 (0.75 – 0.95) | 0.85 (0.76 – 0.96) |
| Model (3) | 1 | 0.85 (0.75 – 0.96) | 0.85 (0.75 – 0.97) | 0.84 (0.74 – 0.96) |
|
| ||||
| Hemorrhagic Stroke | ||||
| Model (1) | 1 | 0.95 (0.74 – 1.22) | 0.77 (0.60 – 1.00) | 0.91 (0.71 – 1.16) |
| Model (2) | 1 | 0.96 (0.75 – 1.23) | 0.75 (0.58 – 0.98) | 0.90 (0.70 – 1.16) |
| Model (3) | 1 | 0.91 (0.70 – 1.19) | 0.78 (0.59 – 1.03) | 0.92 (0.71 – 1.20) |
|
| ||||
| TOAST subtype* | ||||
| Large artery atherosclerosis | 1 | 0.95 (0.60 – 1.49) | 0.85 (0.53 – 1.35) | 0.69 (0.42 – 1.13) |
| Cardioembolism | 1 | 0.91 (0.70 – 1.17) | 1.01 (0.79 – 1.30) | 1.04 (0.81 – 1.32) |
| Small Vessel occlusion (lacune) | 1 | 0.82 (0.62 – 1.08) | 0.77 (0.59 – 1.03) | 0.83 (0.63 – 1.10) |
Model (1) unadjusted
Model (2) adjusted for Age, Race, and Hypertension status
Model (3) adjusted for Model 2 variables plus Smoking Status, Physical Activity, History of Diabetes, History of Atrial Fibrillation, History of Myocardial Infarction, Hormone Use, Alcohol Intake, Aspirin Use, High Cholesterol, and BMI
All adjusted for all variables in Model (3)
In accordance with our a priori analysis plan we present results for all outcomes of interest stratified by hypertension status (Table 4). Among non-hypertensive women, there was a lower risk of all-cause mortality, all stroke, and ischemic stroke across increasing quartiles for potassium. In particular, there was a 27% lower risk of ischemic stroke when comparing Q4 to Q1 in model 3 (HR 0.73, 95% CI 0.60–0.88), and no association for hemorrhagic stroke. Among hypertensive women, higher potassium intake was associated with lower all-cause mortality but there was no association with any stroke outcome.
Table 4.
Hazard Ratios for All-cause mortality and Stroke in Quartiles of Potassium by Hypertension Status
| Quartiles of Potassium (mg) | ||||
|---|---|---|---|---|
|
| ||||
| Q1: < 1925.5 | Q2: ≥1925.5 – 2519.4 (HR, 95% CI) | Q3:>2519.4 – 3193.6 (HR, 95% CI) | Q4: >3193.6 (HR, 95% CI) | |
| All-Cause Mortality | ||||
| hypertension | 1 | 0.92 (0.85 – 0.99) | 0.85 (0.79 – 0.92) | 0.89 (0.82 – 0.96) |
| no hypertension | 1 | 0.91 (0.84 – 0.98) | 0.84 (0.77 – 0.91) | 0.92 (0.85 – 1.00) |
|
| ||||
| Stroke (all) | ||||
| hypertension | 1 | 0.99 (0.86 – 1.13) | 0.93 (0.81 – 1.07) | 0.97 (0.84 – 1.12) |
| no hypertension | 1 | 0.75 (0.64 – 0.89) | 0.75 (0.64 – 0.89) | 0.79 (0.67 – 0.93) |
|
| ||||
| Ischemic Stroke | ||||
| hypertension | 1 | 0.96 (0.82 – 1.14) | 0.96 (0.81– 1.13) | 0.93 (0.79 – 1.10) |
| no hypertension | 1 | 0.71 (0.58 – 0.86) | 0.73 (0.60 – 0.88) | 0.73 (0.60 – 0.88) |
|
| ||||
| Hemorrhagic Stroke | ||||
| hypertension | 1 | 0.81 (0.56 – 1.18) | 0.85 (0.59 – 1.24) | 0.85 (0.58 – 1.24) |
| no hypertension | 1 | 1.02 (0.70 – 1.49) | 0.72 (0.48 – 1.09) | 1.01 (0.69 – 1.48) |
|
| ||||
| TOAST Subtype | ||||
|
| ||||
| Large artery atherosclerosis | ||||
| Hypertension | 1 | 1.13 (0.65 – 1.96) | 0.92 (0.51 – 1.65) | 0.66 (0.35 – 1.25) |
| No hypertension | 1 | 0.67 (0.30 – 1.49) | 0.74 (0.34 – 1.59) | 0.72 (0.33 – 1.57) |
|
| ||||
| Cardioembolism | ||||
| Hypertension | 1 | 0.99 (0.71 – 1.38) | 1.06 (0.76 – 1.48) | 1.17 (0.85 – 1.61) |
| No hypertension | 1 | 0.80 (0.54 – 1.19) | 0.95 (0.65 – 1.38) | 0.87 (0.60 – 1.28) |
|
| ||||
| Small Vessel occlusion (lacune) | ||||
| Hypertension | 1 | 1.11 (0.80 – 1.56) | 0.90 (0.63 – 1.28) | 0.95 (0.67 – 1.36) |
| No hypertension | 1 | 0.43 (0.26 – 0.71) | 0.60 (0.38 – 0.95) | 0.67 (0.43 – 1.04) |
Adjusted for Age, Race, Hypertension status, Smoking Status, Physical Activity, History of Diabetes, History of Atrial Fibrillation, History of Myocardial Infarction, Hormone Use, Alcohol Intake, Aspirin Use, High Cholesterol, and BMI
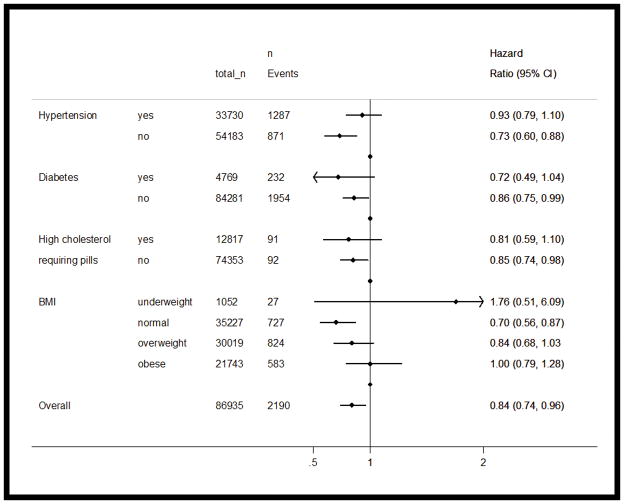
Interactions were observed for ischemic stroke between dietary potassium and hypertension (p<.10), diabetes (p <.05), high cholesterol requiring pills (p <.01) and BMI (p <.05). Figure 1 shows stratified analyses by these variables. For example, among the 35,227 women who had normal BMI, there were 727 ischemic stroke events. The HR comparing the highest quartile to the lowest quartile of potassium intake indicates that among those of normal weight, higher potassium intake was associated with a 30% lower risk of stroke (HR=0.70, 95% CI: 0.56–0.87).
Figure 1.
Hazard ratios comparing highest to lowest quartile of potassium intake (mg) for ischemic stroke stratified by hypertension, diabetes, high cholesterol and BMI
Hazard ratios adjusted for age, race, hypertension, smoking, physical activity, history of diabetes, history of atrial fibrillation, history of myocardial infarction, hormone use, alcohol intake, aspirin use, high cholesterol, and BMI. Variables that make up the strata are omitted when running Cox regressions in that stratum.
Subtypes of Ischemic Stroke According to TOAST Classification
Cox proportional hazards models were run for the predominant Trial of Org 10172 in Acute Stroke Treatment (TOAST) classes: large artery atherosclerosis, cardioembolism, and small vessel occlusion (lacunae). We compared each subtype to a reference group of no stroke. Power to detect effects was small for these subgroups. Nevertheless, higher potassium intake was associated with a lower risk of small vessel disease among those not hypertensive. Compared to the lowest quartile, Q2, Q3 and Q4 had HRs (95% CI) of 0.43 (0.26–0.71), 0.60 (0.38–0.95) and 0.67 (0.43–1.04), respectively.
Discussion
In the largest U.S. cohort study of over 90,000 post-menopausal women, we found an inverse association between self-reported dietary potassium intake and incidence of ischemic stroke. The lower risk of stroke associated with higher intake of potassium persisted after adjusting for multiple covariates. In particular, women consuming the highest quantity of potassium in our cohort (>3193.6mg) had a 12% lower risk of all-type stroke (HR 0.88, 95% CI 0.79–0.98), and a 16% lower risk of ischemic stroke (HR 0.84, 95%CI 0.74–0.96) as compared to women consuming less than 1925.5mg of potassium.
Non-hypertensive women tended to benefit the most from consuming diets higher in potassium. Women in the highest quartile of potassium intake had a 21% reduction in risk of all-type stroke (HR= 0.79, 95% CI 0.67–0.93) and a 27% reduction in risk of ischemic stroke (HR= 0.73, 95% CI 0.60–0.88). Women with hypertension had a lower total mortality risk with higher potassium intake but no lowered risk of stroke suggesting that higher potassium intake may be of more benefit before hypertension develops. This finding supports cell culture and animal model studies that have shown that higher potassium levels improve vascular endothelial function and promote nitric oxide release, thereby improving vascular flow 17, 18 In non-hypertensive women the correlation between systolic blood pressure and potassium intake was negligible at −.008, suggesting that in our data, the beneficial effect of potassium intake among non-hypertensives was not modulated by its effect on blood pressure. Instead, this particular result may be due to habitually higher intakes of dietary potassium that prevent arterial stiffness19. A small study of young men and women found that habitually low potassium intake was associated with increased arterial stiffness, measured by carotid-femoral pulse wave velocity, despite normal blood pressures. This suggests that dietary potassium may have an effect on blood vessels beyond its effects on blood pressure19. Further research to elucidate mechanisms is needed.
The US Department of Agriculture currently recommends that women eat at least 4700 mg of potassium daily20. In WHI only 2.8% of women met or exceeded this level. The World Health Organization recently amended its recommendation after conducting a meta-analysis of dietary potassium intake and cardiovascular disease, and advises that women eat at least 3510mg of potassium 21 per day22. In the WHI OS cohort, 16.6% of women met or exceeded this level. Overall, the mean reported dietary potassium intake was only 2611mg. Few postmenopausal women appear to reach the recommended levels of daily potassium intake.
Further, the National Health and Nutrition Examination Survey (NHANES) comparing the period from the 1988–1994 with the 2003–2008 survey, reports that mean dietary potassium intake declined among women aged 51–70 by 87mg to 2419mg and in those over 71 by 173mg to 2234mg23. This decline is predicted to continue unless major changes in the food environment provide more unprocessed meats, fruits and vegetables to consumers. Some foods rich in potassium are white and sweet potatoes, bananas, and white beans. Our results illustrate that consuming more potassium, even below recommended levels, is associated with a reduced risk of all-type stroke and ischemic stroke by over 20% in non-hypertensive women. With the general decline in potassium consumption, women may be at greater risk of suffering strokes. Health care providers therefore may wish to reinforce the importance of a potassium rich diet especially among postmenopausal women.
The difference between our results and those from the Swedish Mammography Cohort (SMC) and EPIC cohort studies can be explained in several ways. Our study was substantially larger than the SMC, and our measurement of hypertension was more robust than SMC, which relied on self-reported history of hypertension without subsequent validation7. This influenced their finding that an increase in potassium intake is more protective for hypertensive women. Our study looked exclusively at older women, unlike the EPIC-NL study which looked at a group of 36,094 men and women with a mean age of 498. The mean dietary potassium intake was also substantially lower in women from the WHI than in the EPIC-NL study participants (2611mg vs 3672mg). The generally higher potassium intakes in their analysis may have prevented them from finding an association with stroke.
There are some limitations to our study. First, this was an observational study rather than a clinical trial and therefore results must be interpreted with caution concerning causation. Secondly, our estimates of potassium intake come from food frequency questionnaires (FFQ) and may under- or over-estimate true intake. Thirdly, we only used baseline dietary potassium in assessing relationships to outcomes. WHI-OS participants also completed FFQs at Year 3 of follow up. In comparing the dietary potassium intake between baseline and year 3, there was a mean decrease in potassium intake of 79mg, with a correlation between baseline and year 3 of 0.63 Fourth, our analyses focus on potassium only, while corresponding sodium consumption may be an important covariate in determining hypertension 24 and cardiovascular disease21 risk. However, sodium consumption is not reliably estimated by the WHI FFQ, so analyses of potassium and sodium jointly in relation to these outcomes in the WHI OS needs to rely on biomarkers for sodium consumption25, which are not available on the entire cohort.
In summary, in the largest prospective study of older women with long-term follow-up, we found lower risk of ischemic but not hemorrhagic stroke associated with higher intakes of potassium, especially in non-hypertensive women, as well as lowered risk of all-cause mortality in all women. We also found that higher potassium intake is associated with lower risk of small vessel stroke subtype. Since dietary intake of potassium in the U.S. is well below the recommended intake, these findings are important in suggesting preventive dietary measures to lower the risk of stroke.
Acknowledgments
The authors thank the WHI investigators and staff for their dedication, and the study participants for making the program possible. A full listing of WHI investigators can be found at: http://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Short%20List.pdf
Funding Source:
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C.
Footnotes
Disclosures: None
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Executive summary: Heart disease and stroke statistics—2013 update: A report from the American Heart Association. Circulation. 2013;127:143–152. doi: 10.1161/CIR.0b013e318282ab8f. [DOI] [PubMed] [Google Scholar]
- 2.Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, et al. The lifetime risk of stroke: Estimates from the Framingham study. Stroke. 2006;37:345–350. doi: 10.1161/01.STR.0000199613.38911.b2. [DOI] [PubMed] [Google Scholar]
- 3.Khaw KT, Barrett-Connor E. Dietary potassium and stroke-associated mortality. A 12-year prospective population study. The New England Journal of Medicine. 1987;316:235–240. doi: 10.1056/NEJM198701293160502. [DOI] [PubMed] [Google Scholar]
- 4.Weng LC, Yeh WT, Bai CH, Chen HJ, Chuang SY, Chang HY, et al. Is ischemic stroke risk related to folate status or other nutrients correlated with folate intake? Stroke. 2008;39:3152–3158. doi: 10.1161/STROKEAHA.108.524934. [DOI] [PubMed] [Google Scholar]
- 5.Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: Systematic review and meta-analyses. BMJ. 2013;346:f1378. doi: 10.1136/bmj.f1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iso H, Stampfer MJ, Manson JE, Rexrode K, Hennekens CH, Colditz GA, et al. Prospective study of calcium, potassium, and magnesium intake and risk of stroke in women. Stroke. 1999;30:1772–1779. doi: 10.1161/01.str.30.9.1772. [DOI] [PubMed] [Google Scholar]
- 7.Larsson SC, Virtamo J, Wolk A. Potassium, calcium, and magnesium intakes and risk of stroke in women. American Journal of Epidemiology. 2011;174:35–43. doi: 10.1093/aje/kwr051. [DOI] [PubMed] [Google Scholar]
- 8.Sluijs I, Czernichow S, Beulens JW, Boer JM, van der Schouw YT, Verschuren WM, et al. Intakes of potassium, magnesium, and calcium and risk of stroke. Stroke. 2014;45:1148–50. doi: 10.1161/STROKEAHA.113.004032. [DOI] [PubMed] [Google Scholar]
- 9.Anderson GL, Manson J, Wallace R, Lund B, Hall D, Davis S, et al. Implementation of the Women’s Health Initiative study design. Annals of Epidemiology. 2003;13:S5–17. doi: 10.1016/s1047-2797(03)00043-7. [DOI] [PubMed] [Google Scholar]
- 10.Patterson RE, Kristal AR, Tinker LF, Carter RA, Bolton MP, Agurs-Collins T. Measurement characteristics of the women’s health initiative food frequency questionnaire. Annals of Epidemiology. 1999;9:178–187. doi: 10.1016/s1047-2797(98)00055-6. [DOI] [PubMed] [Google Scholar]
- 11.Curb JD, McTiernan A, Heckbert SR, Kooperberg C, Stanford J, Nevitt M, et al. Outcomes ascertainment and adjudication methods in the Women’s Health Initiative. Annals of Epidemiology. 2003;13:S122–128. doi: 10.1016/s1047-2797(03)00048-6. [DOI] [PubMed] [Google Scholar]
- 12.Outcome classifications: Cardiovascular outcomes. WHI Manual. 8(Section 5):5-12–15-13. [Google Scholar]
- 13.Chen JC, Brunner RL, Ren H, Wassertheil-Smoller S, Larson JC, Levine DW, et al. Sleep duration and risk of ischemic stroke in postmenopausal women. Stroke. 2008;39:3185–3192. doi: 10.1161/STROKEAHA.108.521773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lakshminarayan K, Larson JC, Virnig B, Fuller C, Allen NB, Limacher M, et al. Comparison of Medicare claims versus physician adjudication for identifying stroke outcomes in the Women’s Health Initiative. Stroke. 2014;45:815–21. doi: 10.1161/STROKEAHA.113.003408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldstein LB, Jones MR, Matchar DB, Edwards LJ, Hoff J, Chilukuri V, et al. Improving the reliability of stroke subgroup classification using the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) criteria. Stroke. 2001;32:1091–1098. doi: 10.1161/01.str.32.5.1091. [DOI] [PubMed] [Google Scholar]
- 16.Shimbo D, Newman JD, Aragaki AK, LaMonte MJ, Bavry AA, Allison M, et al. Association between annual visit-to-visit blood pressure variability and stroke in postmenopausal women: Data from the Women’s Health Initiative. Hypertension. 2012;60:625–630. doi: 10.1161/HYPERTENSIONAHA.112.193094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oberleithner H, Callies C, Kusche-Vihrog K, Schillers H, Shahin V, Riethmuller C, et al. Potassium softens vascular endothelium and increases nitric oxide release. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:2829–2834. doi: 10.1073/pnas.0813069106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rigsby CS, Pollock DM, Dorrance AM. Dietary potassium supplementation improves vascular structure and ameliorates the damage caused by cerebral ischemia in normotensive rats. Nutrition & Metabolism. 2008;5:3. doi: 10.1186/1743-7075-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lennon-Edwards S, Allman BR, Schellhardt TA, Ferreira CR, Farquhar WB, Edwards DG. Lower potassium intake is associated with increased wave reflection in young healthy adults. Nutrition Journal. 2014;13:39. doi: 10.1186/1475-2891-13-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoy MK, Goldman JD. Potassium Intake of the US Population: What We Eat In America, NHANES 2009–2010. USDA Agricultural Research Service; Sep 10, 2012. [27 July 2013]. http://ars.usda.gov/Services/docs.htm?docid=19476. [Google Scholar]
- 21.Cook NR, Obarzanek E, Cutler JA, Buring JE, Rexrode KM, Kumanyika SK, et al. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: The Trials of Hypertension Prevention follow-up study. Archives of Internal Medicine. 2009;169:32–40. doi: 10.1001/archinternmed.2008.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guideline: Potassium Intake for Adults and Children. Geneva: World Health Organization; 2012. Available from: http://www.ncbi.nlm.nih.gov/books/NBK132470/ [PubMed] [Google Scholar]
- 23.Cogswell ME, Zhang Z, Carriquiry AL, Gunn JP, Kuklina EV, Saydah SH, et al. Sodium and potassium intakes among US adults: NHANES 2003–2008. The American Journal of Clinical Nutrition. 2012;96:647–657. doi: 10.3945/ajcn.112.034413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Intersalt: An international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt cooperative research group. BMJ. 1988;297:319–328. doi: 10.1136/bmj.297.6644.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang Y, Van Horn L, Tinker LF, Neuhouser ML, Carbone L, Mossavar-Rahmani Y, et al. Measurement error corrected sodium and potassium intake estimation using 24-hour urinary excretion. Hypertension. 2014;63:238–244. doi: 10.1161/HYPERTENSIONAHA.113.02218. [DOI] [PMC free article] [PubMed] [Google Scholar]