Abstract
Purpose
The present study investigated the psycho-physiological inter and intra-individual processes that mediate the linkage between childhood/adolescent socioeconomic adversities and adult health outcomes. Specifically, the proposed model examined the roles of youth depressive symptoms and BMI trajectories as mediators that explain the link between early adversity and young adults’ general health and physical illnesses after controlling for gender, race/ethnicity, and earlier general health reports.
Methods
Using a nationally representative sample of 12,424 from National Longitudinal Study of Adolescent Health (Add Health), this study used growth curve modeling to consider both the severity (initial level) as well as the change over time (deterioration or elevation) as psycho-physiological mediators, thereby acknowledging multiple facets of depressive symptoms and BMI trajectories as psych-physiological mediators of early adversity to adult health.
Results
Results provide evidence for (a) the influence of early childhood and early adolescent cumulative socioeconomic adversity on both the initial levels and changes over time of depressive symptoms and BMI and (b) the independent influences depressive symptoms and BMI trajectories on the general health and the physical illnesses of young adults
Conclusions
These findings contribute valuable knowledge to existing research by elucidating how early adversity exerts an enduring long-term influence on physical health problems in young adulthood; further, this information suggests effective intervention and prevention programs should incorporate multiple facets (severity and change over time) of multiple mechanisms (psychological and physiological).
Keywords: Early Socioeconomic Adversity, BMI, Depressive symptoms, Young adult health
Early adverse life experiences are ‘biologically imbedded’ and take their toll on health in the later stages of life.1,2,3 However, only a few studies have examined potential mediating life course processes, such as intra-individual trajectories of psycho-physiological attributes over adolescence and emerging adulthood (hereafter, early life course), that may link early socioeconomic adversity to later health in life. Delineating these long-term psycho-physiological mechanisms has important public health implications and warrants further investigation. The current study focuses on youth depressive symptoms and body mass index (BMI) as psycho-physiological mediators of early socioeconomic adversity and later health linkage because depressive symptoms and BMI have been shown to have (a) significant inter-individual variations in the early levels and individual changes over time, and (b) important health consequences in young adulthood,3,4,5,6 (c) operate as a concerted longitudinal process through their mutual association.7,8
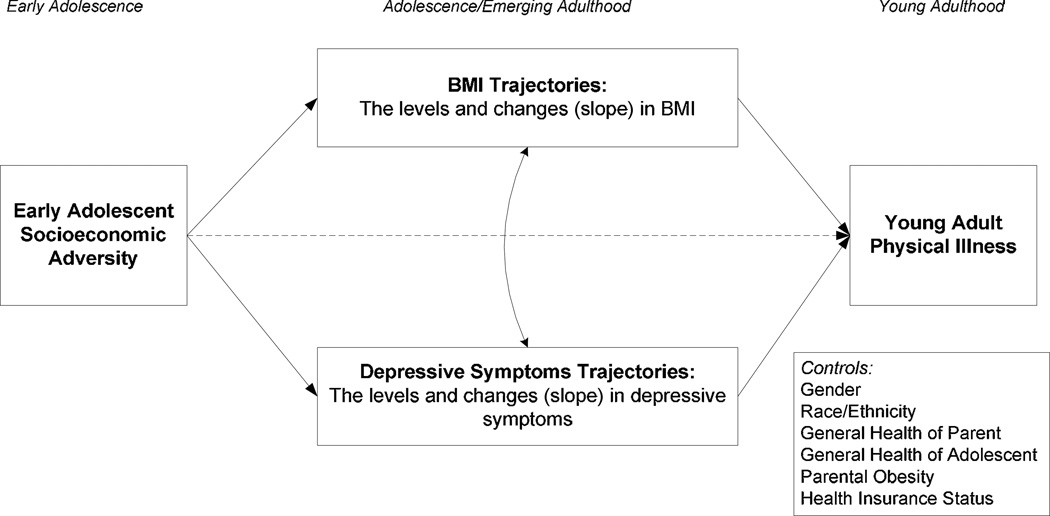
Early socioeconomic disadvantage may generate early physiological and cognitive deficits (e.g., low birth-weight, low stature, stunted organ growth) during infancy, childhood, and adolescence. These deficits may lead to irreversible consequences with long-term latent effects that manifest at a later stage in life.9, 10,11,12 Thus, in the present investigation, as shown in figure 1, we investigated the influence of early socioeconomic adversity on young adult health directly and indirectly through depressive symptoms and BMI trajectories. We capture the cumulative adversity (a composite index) by aggregating different dimensions of socioeconomic adversity (e.g., parental education, community family poverty rate).
Figure 1.
The theoretical modal.
Various dimensions of early socioeconomic adversity influence both the early levels and subsequent changes in depressive symptoms over time. We expect that adverse family characteristics, such as family economic hardship and low parental education, would influence depressive symptoms primarily through its impact on family stressful events (e.g., parental conflicts, stressful harsh and/or rejecting parenting).13 Particularly, resource deprivation (i.e., lack of materials, food, and clothing) generate depressive feelings in youths.13,14, 15 High overall levels of family stress are expected to increase adaptive challenges for an adolescent already dealing with the rapid biological, cognitive, and social changes that occur during this period of life.
Constant exposure to stressful family and community circumstances operate as a chronic stressor for adolescents which elevates depressive symptoms of adolescents. Psychobiological research has shown that stress responses (negative emotions including depressive symptoms) to chronic stressors evoke physiological processes such as activation of the hypothalamic-pituitary-adrenocortical (HPA) axis (secretes glucocorticoid), the sympathetic-adrenal-medullary (SAM) system (secretes cathacalmine), and immune function responses (i.e., chronic inflammation).16,17,18,19 These mechanisms results in physiological dysregulations (e.g., elevated levels of blood pressure, glucose, lipid, free fatty acids) and in turn contribute to physical illnesses such as heart risk and metabolic diseases.16,17 Furthermore, depressed mood indirectly contributes to physical illnesses through behavioral mechanisms (i.e., binge eating,20 substance use, risky sexual behaviors). Thus, as shown in figure 1, we expected that constant exposure to an adverse environment (e.g., family and community adversity) is a chronic stressor for youth that manifests as increased depressive symptoms and eventuates in later poor physical health.
Early Socioeconomic Adversity, Adolescent BMI Trajectories, and Young Adult Physical Illness
BMI increases with the transition from adolescence to adulthood with an increased rapidity in early adolescence and adulthood.21 Further, there is significant inter-individual variation in BMI trajectories during this period.9 As shown in the figure 1, we expected that early socioeconomic adversity to contribute to the variation in BMI trajectories.
Numerous studies have found that family economic hardship, low parental education, and adverse community characteristics influence adolescents’ BMI trajectories into young adulthood.6,9,10 Adolescents from poor families and single-parent families lack health resources(i.e., proper food/housing, access to recreation facilities and health services).9,20 This lack of environmental resources (i.e., recreational activities, availability/accessibility of health care) in disadvantaged communities contributes to the higher prevalence of adolescent obesity in disadvantaged communities. Further, socioeconomically disadvantaged parents may also model their unhealthy behaviors (e.g., unhealthy eating behaviors, lack of exercise) and risky lifestyles to their offspring.22
Chronic family stressors can lead to stress responses that can directly exacerbate adolescents’ metabolic processes resulting in an increased body weight.23 This physiologic process involves two stages.9,18 First, adrenaline is released from the “fight or flight response,” which triggers the release of stored energy and fat reserves. Second, the HPA axis is activated to release cortisol into the bloodstream in order to restore the energy reserves by prompting hunger and transforming food into fat reserves.
Obesity and being overweight contributes to an array of physical health problems (e.g., heart disease, gallstones, hypertension, diabetes, and certain cancers24) through adverse physiological mechanisms. For example, obesity contributes to elevated triglycerides, high blood pressure, and insulin resistance, all metabolic risk factors related to cardiovascular disease and diabetes.24 Also, obesity erodes self-esteem and contributes to psychological disorders (e.g., depression) which may in turn influence risk for risky sexual activities.25,26 Obesity, especially when experienced early in childhood and adolescence, is strongly linked to poor physical health outcomes in adulthood.27 Further, recent research indicates that BMI trajectories, rather than static BMI measures, are better predictors of mortality risk in later life.28 Thus, we expected both initial levels and slopes of BMI (i.e., trajectories) to contribute to young adult physical illness.
The Association between BMI and Depressive Symptoms Trajectories
The findings on the directional association between BMI and depressive symptoms are mixed.7 Some studies have shown that earlier depressive symptoms contribute to an increased BMI or an increased risk of high BMI later in life,29 whereas others have shown that BMI (i.e., being obese) contributed to increased levels of depressive symptoms.5 Yet others have shown that BMI trajectories and depressive symptom trajectories have a reciprocal relationship.8 Further the associations between BMI and depressive symptom trajectories may vary across race and gender.30
Gender and Race/Ethnicity
Existing research has shown BMI trajectories vary by gender. More specifically, women have been found to have lower initial BMI values than men, but women experienced a greater increase in BMI over time compared to men.9 Research has also indicated a high prevalence of obesity and increased levels of depressive symptoms among minority adolescents. Thus, gender and race/ethnicity was included as a covariate in this study.
Methods
Methodological concerns
Previous research has investigated life course models predicting health outcomes using traditional regression models. These models generally have not investigated intra-individual changes in health attributes over time. In the present study, we investigated individual trajectories of depressive symptoms and BMI as mediators because it allows interpretations of how early socioeconomic adversities influence not only the early levels (severity) and but also the subsequent individual changes or slopes (deteriorations or improvements) of these health attributes over 13 years.
Sample
Data for this study came from a nationally representative sample of adolescents participating in the National Longitudinal Study of Adolescent Health (Add Health; http://www.cpc.unc.edu/projects/Add Health). In 1995, baseline (Wave 1) data were derived from a complex stratified cluster-sampling of middle and high school students, yielding 20,745 respondents (Mage 15.5 years; range = 12 – 19 years at baseline) from 134 middle and high schools. The second and third waves of data were collected in 1996 and 2001 (N2=14,738; N2=15,100). We used in-home interview data from parents who responded to marital history questions in Wave 1 and adolescents who participated in Waves 1, 3, and 4 (young adulthood). Thus, the study sample size was 12,424. We used Wave 1 sample weights in the analyses. The final sample consisted of approximately 53% women, and 39% of respondents reported a minority racial/ethnic status with the largest percentages reporting for African American (15%), Hispanic (10%), Asian (6%), and Native American (2.8%), respectively. Female respondents who were pregnant at wave 2 or wave 3 were excluded from the sample.
We used Mplus (version 731) to impute data for all missing data in Waves 1 and Wave 3. Thus, the analytical sample included only non-imputed health outcome data in Wave 4 and marital history data in Wave 1. A total of 19.97% of the data were imputed. Attrition and missing data analysis showed that there was little difference between adolescents with missing data in our study sample and those with complete data.
Measures
Cumulative socioeconomic adversity
We constructed a composite index for cumulative socioeconomic adversity by summing standardized continuous indicators capturing different dimensions of adversity. These indicators included average parental education, family economic hardship, and U. S. Census measures of community adversity, and are further detailed in Table 1.
Table 1.
Indicators of Cumulative Socioeconomic Adversity
| Indicator (Wave of data used) |
Description of composite variable | Range of responses |
|---|---|---|
| Parental Education (Wave 1) | composite score of mothers’ and fathers’ education levelsa | 1 (Never went to school) to 10 (professional training beyond four-year college or university degree) |
| Economic Hardship (Wave 1) | Sum of 5 dichotomous items asking if household member received social service benefitsb (0 = no, 1 = yes) and 1 item on family poverty status | 0 to 6 |
| Community Adversity (Wave 1/ 1990 Census) (α = .78) | Sum of four U. S. Census based dichotomized indicators asking the community proportions of (1) families living in poverty, (2) single-parent families, (3) adults employed in the service industry, and (4) unemployed menc. | 0 to 4 |
Note.
For single-headed families (n = 79) with no available data from fathers, maternal education served as the indicator of parental education.
Specific items are whether any member of the household received the following social service benefits: social security, supplemental security income, aid to families with dependent children, food stamps, or housing subsidies.
Adapted from a previous study.37
Body mass index and obesity
Respondents’ BMI, the ratio of weight to height squared ([lbs*703]/inches2), was used to assess degree of being overweight. At wave 1, BMI was calculated using respondents’ self-reports of their height and weight. At waves 2, 3 and 4, BMI was calculated from height and weight measurements obtained by trained interviewers.
Depressive symptoms
At wave 1 (1995), wave 2 (1996), wave 3 (2001) and wave 4 (2008), five items from the Center for Epidemiological Studies of Depression Scale (CES-D32) were used to assess adolescent respondents’ distress feelings (e.g., felt depressed, sad, happy, enjoyed life, felt the blues) in the past week. Following Perreira and colleagues’33 recommendations, we used a composite of 5 items from the CES-D that has been shown to be comparable across racial/ethnic groups. Scale responses ranged from 0=never or rarely to 3=most/all of the time. Only 4 items of the suggested 5 items were available at Wave 3 (felt depressed, sad, enjoyed life, felt the blues). Items were reverse coded and averaged.. The scale had adequate internal reliability (α > .78 for all four waves).
Young adult physical illness
The young adult respondents’ physician-diagnosed physical illness at Wave 4 (2008) was comprised of a count of eight physician-diagnosed diseases and health problems within the past year. In the study sample, 0.2% (n=26) of the participants had been diagnosed with hepatitis, 1.5% (n=188) with cancer/leukemia, 3.2% (n=408) with diabetes, 0.9% (n=120) with heart disease, 17.3% (n=2153) with asthma/chronic bronchitis, 16.7% (n=2075) with migraines, 12.2% (n=1516) with high blood pressure, and 25.2% (n=3137) with any of 13 possible STIsa. 26% and 9.7% of participants reported either one or two or more physical illnesses, respectively. The composite count of young adult physical illness had a range with a minimum of 0 (no illness) and a maximum of 8 (8 counts of illness). The final count had a skewness of 2.19 (SE = .02).
Parent and adolescent general health
A single item of general health (i.e., how is your health on a scale from 1–‘excellent’ to 5–‘poor’) from wave 1 for both the parent respondent and the adolescent respondent were used as covariates. A parallel single item indicator of general health at wave 4 for the target respondent was assessed as a measure of global young adult health.
Race/ethnicity
At wave 1, adolescents reported their race/ethnicity. The variables were dummy-coded by dichotomizing the presence of African-American, Hispanic, Asian, Native-American, and Caucasian racial/ethnic statuses. Caucasians were used as a reference group. For multi-racial respondents, only the first choice of race/ethnicity category was considered.
Gender
Gender was coded as male (0) or female (1).
Biological parental obesity
Parental obesity assessed at wave 1 dichotomously (0-no, is not obese, 1-yes, is obese) for the target adolescents’ biological mother and biological father was included as a covariate. At wave 1, 18.5% of biological mothers were obese, and 10.3% of fathers were obese.
Health insurance
Target adolescent’s health insurance status assessed at wave 4 was included as a covariate using a single item determining the presence and type of health insurance (i.e., no insurance, Medicaid, parents’ health insurance, etc.) the individual currently had. At wave 4, 20.7% of participants did not have health insurance.
Biological proxy markers
At wave 4, dry blood spot biospecimen samples were collected and analyzed to determine cholesterol levels, hemoglobin A1C levels, and blood glucose levels. Systolic blood pressure (SBP), diastolic blood pressure (DBP), and pulse rate were obtained at the time of assessment. These biomarker proxies were analyzed separately as biological proxies related to the young adult physical illnesses (i.e., heart disease) that reflect physiological dysregulation. For more details on collection methods, please consult Add Health codebooks, which are available online (http://www.cpc.unc.edu/projects/addhealth/codebooks).
Analysis Plan
We tested the theoretical model in a bivariate parallel latent growth curve model (LGM) in a structural equation modeling (SEM) framework to estimate individual trajectories using Mplus (version731). Individual sample weights from Wave 1 were used to account for oversampling of smaller population groups.
We used the TYPE=COMPLEX analysis syntax in order to adjust for potential bias in standard errors and chi square computation due to the lack of individual independence between observations within schools in the Add Health data. Missing data were accounted for using the Full Information Maximum Likelihood (FIML) procedures.34 We used the Comparative Fit Index (CFI ≥ .90) and Root Mean Square Error of Approximation (RMSEA ≤ .06) to evaluate model fit.35
Results
Table 2 presents correlations among study variables, as well as descriptive statistics of main study variables. A slight positive skewness in physical illness at wave 4 was accounted for by using the weighted least squares mean adjusted (‘WLSM’-Type 5) estimator in MPlus.
Table 2.
Descriptives and correlations of study variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Parent Health a W1 b | -- | |||||||||||
| 2. Adolescent Health a W1 | .14** | -- | ||||||||||
| 3. Adolescent Health a W4 | .12** | .28** | -- | |||||||||
| 4. Physical Illness W4 c | .04** | .07** | .19** | -- | ||||||||
| 5. Early Adversity d | .34** | .11** | .15** | .03** | -- | |||||||
| 6. BMI W1–2 | .12** | .21** | .22** | .10** | .13** | -- | ||||||
| 7. BMI W3 | .11** | .18** | .26** | .10** | .13** | .75** | -- | |||||
| 8. BMI W4 | .11** | .16** | .30** | .12** | .16** | .69** | .81** | -- | ||||
| 9. Depression W1 | .12** | .25** | .15** | .06** | .12** | .05** | .04** | .03** | -- | |||
| 10. Depression W2 | .11** | .22** | .17** | .07** | .12** | .06** | .05** | .05** | .51** | -- | ||
| 11. Depression W3 | .07** | .12** | .15** | .06** | .06** | .04** | .01 | .03** | .25** | .29** | -- | |
| 12. Depression W4 | .07** | .12** | .26** | .11** | .09** | .04** | .03** | .02** | .25** | .28** | .32** | -- |
| Mean (SD) | 2.41 (1.03) | 2.13 (.91) | 2.34 (.91) | .51 (.89) | −.29 (2.13) | 22.86 (4.50) | 26.55 (6.15) | 29.15 (7.53) | 3.21 (2.82) | 3.15 (2.81) | 1.82 (2.18) | 2.80 (2.81) |
| Range | 1 – 5 | 1 – 5 | 1 – 5 | 0 – 8 | −4.05–10.59 | 11.21–54.23 | 13.46–63.83 | 15.40–97.40 | 0 – 15 | 0 – 15 | 0 – 12 | 0 – 15 |
Note.
General health.
W = Wave of data;
Young adult physical illness at Wave 4;
Early cumulative socioeconomic adversity.
p < .01
Table 3 includes growth parameter estimates from unconditional univariate latent growth curve (LGC) models of depressive symptoms and BMI. The unconditional LGC model of depressive symptoms showed adequate model fit and significant means and variances of the initial level and a linear decline, and significant means of a positive quadratic slope. Overall, youth in this sample showed a decline in depressive symptoms from adolescence to young adulthood.
Table 3.
Parameter estimates and model fit indices of Unconditional and Conditional LGC models of Young Adult Physical Illness
| Uncond BMI |
Uncond. DEP |
Multiple Allostatic Load Indicators | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (Variance) |
Mean (Variance) |
Physical Illness |
Global Health |
STIs | SBP | DBP | PR | High Cholesterol |
Hemoglobin A1C |
Blood Glucose |
||
| BMI Initial Level |
23.03*** (19.45***) |
-- | .02*** | .03*** | −.01*** | .59** | .36*** | .21*** | .01*** | .03*** | .79*** | |
| BMI Linear Slope |
.47*** (.14***) |
-- | .16*** | .51*** | −.03 | 8.76** | 5.58*** | 6.79*** | .05*** | .24*** | 4.81*** | |
| DEP Initial Level |
-- | 3.33*** (4.65***) |
.03* | .18*** | .13*** | −.37 | −.16 | .18 | .01 | .03 | 1.26 | |
| DEP Linear Slope |
-- | −1.59*** (2.98***) |
.06* | .22*** | .10*** | .09 | .51* | .22 | .01 | .02 | .77 | |
| DEP Quadratic Slope |
-- | .44*** (.05) |
.23*** | .51*** | .13** | .47 | 1.25** | .80 | .03 | .02 | .81 | |
| χ2 (df) | 62.71 (1) | 213.28 (1) | 1253.71 (63) |
1252.37 (63) |
1247.76 (63) |
1233.47 (63) |
1243.53 (63) |
1282.93 (63) |
1889.39 (63) |
1247.58 (63) |
1250.54 (63) |
|
| CFI | .99 | .98 | .94 | .95 | .90 | .95 | .95 | .95 | .92 | .95 | .95 | |
| RMSEA | .06 | .10 | .03 | .04 | .05 | .04 | .04 | .04 | .04 | .04 | .04 | |
Note.
Unstandardized parameter estimates shown. BMI = body mass index. DEP = depressive symptoms. STI= sexually transmitted illnesses. SBP = systolic blood pressure. DBP = diastolic blood pressure. PR = pulse rate.
p <. 05.
p < .01.
p < .0001.
BMI at waves 1 and 2 showed a very strong and significant correlation, indicating a very high stability which prevented us from estimating growth curves using both waves separately. Because only a 1 year period separated waves 1 and 2, the mean BMI from waves 1 and 2 were used as the baseline for the unconditional LGC of BMI, resulting in the three time points used in all subsequent analyses. This unconditional LGC model showed acceptable model fit, significant means and variances of the initial levels, and a slight linear increase in BMI over time. The significant variances of the linear slopes of both BMI and depressive symptoms suggest that some adolescents in this sample may have increased or decreased at a greater speed (steeper slopes) compared to others.
Influence of Cumulative Socioeconomic Adversity on Depression and BMI
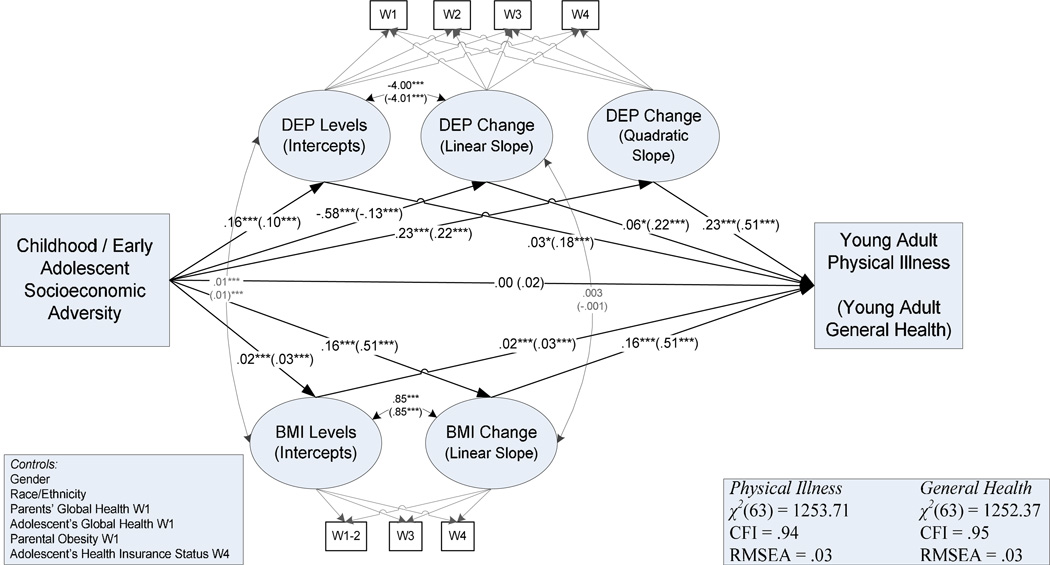
Figure 2 shows the conditional parallel latent growth curve (P-LGC) models of the influence of early adversity on young adult physical health and young adult global health with gender, race/ethnicity, parent general health at wave 1, adolescent general health at wave 1, parental obesity, and health insurance status at wave 4 as covariates. Model fit was acceptable: χ2(63) = 1253.69; CFI=.94; RMSEA=.03. Cumulative socioeconomic adversity positively influenced initial levels of depressive symptoms (β=.16, p<.001) and negatively influenced the linear slope of depressive symptoms (β= −.58, p<.001). This suggests that individuals who experienced extreme adverse conditions (i.e., very low parental education, high family economic hardship, and high community adversity) in early adolescence exhibited extremely high initial levels of depression compared to individuals who experienced less adversity. Further, individuals with high socioeconomic adversity (with high initial levels of depressive symptoms) showed a faster recovery over time (i.e., a faster rate of decline – regression to the mean) compared to individuals with lower levels of depressive symptoms. Cumulative adversity also influenced the curvilinear growth of depression positively.
Figure 2. Conditional P-LGC of cumulative early socioeconomic adversity depressive symptoms, BMI, and young adult physical illness vs. young adult general health.
Note. Standardized parameter coefficients shown. Modal estimates for young adult physical illness shown outside of parentheses, Modal estimates for young adult general health at wave 4 are shown in parentheses. Pathways of control variables not shown for the sake of clarity. Covariance of DEP levels and DEP quadratic slope not shown for clarity: r = 1.10*** (1.10***), DEP: Depressive Symptoms. W: Wave of data.
* p <.05. ** p <.001. *** p <.0001.
The positive influence of cumulative socioeconomic adversity on BMI trajectories suggested that greater socioeconomic adversity contributed to higher BMI levels initially (β = .02, p<.001), along with faster increases in BMI over time (β = .16, p<.001). This suggests that individuals who experienced more adversity in early childhood or early adolescence exhibited higher levels of BMI combined with faster linear growth.
Higher initial levels of BMI were positively associated with linear growth of BMI over time. That is, higher initial levels of BMI were associated with further increases in BMI over time. Initial levels and linear slopes of depression and BMI were uncorrelated, suggesting that depression and BMI changed over time independently.
Cumulative Adversity, Depression, BMI, and Young Adult Physical Illness
Higher initial levels of both depression (β=.03, p<.05) and BMI (β=.02, p<.001) contributed to higher counts of young adult physical illnesses. Further, faster growth of depression (β=.06, p<.05) and BMI (β=.16, p<.001) also contributed to higher counts of young adult physical illnesses. Thus, levels and slopes of depressive symptoms and BMI trajectories independently contributed to young adult physical illness.
We analyzed the same conceptual model predicting young adult general health at wave 4 (See Figure 2; estimates in parentheses). The model fit was acceptable: χ2(63) = 1252.37, p <.001; CFI= .95; RMSEA= .03. Importantly, BMI and depression trajectories similarly predicted young adult general health, emphasizing the importance of depressive symptom and BMI trajectories as valid mediators of the influence of early cumulative socioeconomic adversity on later young adult health. While early cumulative socioeconomic adversity did not directly influence young adult physical illnesses or young adult general health, trajectories of depression and BMI appear to carry over the influence of cumulative adversity.
Finally, to consider how the same pathway may influence independent biomarker proxies of the physical illnesses considered in the composite index of young adult physical health, we analyzed the model as predicting predict 6 additional indicators and 1 previously analyzed indicator separately (i.e., systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse rate, cholesterol level, hemoglobin A1C, blood glucose level, and STI count). The model fit indices for these models were acceptable (i.e., CFI >.90; RMSEA < .05) (Table 3). The linear and quadratic growth trajectories of depressive symptoms were predictive of STI count and DBP. However, the influences depressive growth symptoms trajectories on SBP, DBP, pulse rate, cholesterol level, hemoglobin A1C, or blood glucose level did not reach statistically significance. Linear BMI trajectories are positively associated with STI count, SBP, DBP, pulse rate cholesterol level, hemoglobin A1C, blood glucose levels, and the global health indicator.
Discussion
The present study examined a life course model, from adolescence to adulthood, of the contemporaneous development of depression and BMI in relation to socioeconomic adversities. The results show that early socioeconomic adversity potentiates the development of BMI and depressive symptoms through adolescence and young adulthood, culminating in the physical illness of participants over this period of the life course. A key element in this model involved depressive symptoms and BMI trajectories during this period as the psychophysiological vulnerabilities that mediate the longitudinal association between early adversity and later health. The investigation of individual trajectories of depressive symptoms and BMI allowed us to preserve the continuity of change in depressive symptoms and BMI, thereby treating these changes as processes that unfold over time.
An Investigation of a Life Course Mediational Model leading to Health Outcomes
Consistent with the life course perspective, the results showed that early adversity exerts a persistent maladaptive influence on physical health outcomes over the early life course indirectly through depressive symptoms and BMI trajectories. Early socioeconomic adversities contribute to elevated initial depressive symptom levels through the increase in adaptive challenges for adolescents already dealing with the stressful demands and circumstances that occur during this period. Similarly, early cumulative socioeconomic adversity plays an important role in initiating BMI trajectories as indicated by its effect on the initial BMI level. It seems that in addition to its structural disadvantages that directly influence BMI (i.e., lack of health resources, and educational, recreational and health facilities), early adversity may lead to stress responses that exacerbate metabolic processes resulting in increased body weight of adolescents.23
Importantly, the results showed that early socioeconomic adversity impacts the growth of both depressive symptoms and BMI trajectories as indicated by its effects on their linear slopes. Statistically, this effect corresponds to the interaction between early adversity and time. The cumulative influence of early adversity over the life course may be attributed to several mechanisms, such as (a) an increase in exposure to more stressors/disadvantages due to the proliferation of early stressors/disadvantages over the life course, (b) an increase in the susceptibility to stressors/disadvantages over the life course, and (c) an intensification of the impact of early psychophysiological damages in the later years. Future research should further elucidate these mechanisms.
The results suggest that the severity (as indicated by the initial levels of the trajectories) and the amount of growth or decline (deterioration or recovery) in depressive symptoms and BMI trajectories (i.e., psycho-physiological mediators) independently contribute to the subsequent physical health illnesses and general health in young adulthood. For example, the health consequences of an already obese adolescent who has experienced a sharp increase in BMI differs from the health consequences of an adolescent with an average BMI who has experienced the same amount of increase in BMI over the same period. The same may be true for depressive symptoms. Despite the strong mediating effects of BMI and depressive symptom trajectories in these findings, there may be other meaningful mediating processes. Additionally, the lack of association between the initial levels and changes over time of depressive symptoms and BMI suggests that depressive symptom trajectories and BMI trajectories take divergent paths over this period of the life course.
Several factors potentially limit the scope and the generalizability of the results. First, the present study used self-reports of BMI and physician diagnosed physical illnesses, which may contribute to measurement error. However, self-reported medical records may provide reliable and adequately valid information, a question that should be further examined empirically. Second, we did not examine potential moderating effects of youth academic and cognitive competencies.36 Third, although the analysis controlled for race and ethnicity, the investigated health processes may be unique to different races and ethnicities. Finally, individual genetic-make up would have additive and interactive influences on the study attributes. Thus, future investigations should be informed by individual genetic characteristics.
Despite these limitations, the present study makes a valuable contribution to existing research by elucidating how early adversity initiates an adverse developmental process over the early life course leading to physical health problems in young adulthood through individual psycho-physiological mechanisms in adolescence. The current findings support the salience of early adversity on later adult health1 and further highlights depressive symptoms and BMI trajectories as prime mediators of the early adversity—later health linkage. Accordingly, prevention or intervention programs should aim to reduce depressive symptoms and promote healthy eating habits in adolescence in an effort to prevent later life poor physical health stemming from early socioeconomic adversity.
Acknowledgements
This research is based on data from the Add Health project, a program project designed by J. Richard Udry (PI) and Peter Bearman, and funded by grant P01-HD31921 from the National Institute of Child Health and Human Development to the Carolina Population Center, University of North Carolina at Chapel Hill, with cooperative funding participation by the National Cancer Institute; the National Institute of Alcohol Abuse and Alcoholism; the National Institute on Deafness and Other Communication Disorders; the National Institute on Drug Abuse; the National Institute of General Medical Sciences; the National Institute of Mental Health; the National Institute of Nursing Research; the office of AIDS Research, NIH; the Office of Behavior and Social Science Research, NIH; the Office of the Director, NIH; the Office of Research on Women’s Health, NIH; the Office of Population Affairs, DHHS; the National Center for Health Statistics, Centers for Disease Control and Prevention, DHHS; the Office of Minority Health, Centers for Disease Control and Prevention, DHHS; the Office of Minority Health, Office of Public Health and Science, DHHS; the Office of the Assistant Secretary for Planning and Evaluation, DHHS; and the National Science Foundation. Persons interested in obtaining data files from The National Longitudinal Study of Adolescent Health should contact Add Health Project, Carolina Population Center, 123 West Franklin Street, Chapel Hill, NC27516-3997 (addhealthunc.edu).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Having any of 13 possible STIs (i.e., chlamydia, gonorrhea, trichomoniasis, syphilis, genital herpes, genital warts, hepatitis B, human papilloma virus, pelvic inflammatory disease, cervicitis, urethritis, vaginitis, or HIV/AIDs) was counted as a single count of a sexually transmitted infection.
Implications and Contribution
The present study illustrates how early adversity begins an adverse developmental process mediated by adolescent depression and BMI trajectories and resulting in poor young adult physical health. Preventive intervention health programs can identify at-risk adolescents and target factors associated with depressive symptoms and BMI in order to promote later health.
Contributor Information
K. A. S. Wickrama, Email: wickrama@uga.edu.
Josephine A. Kwon, Email: jkwon@uga.edu.
Assaf Oshri, Email: oshria@uga.edu.
Tae Kyoung Lee, Email: ltk501@uga.edu.
References
- 1.Hayward MD, Gorman BK. The long arm of childhood: The influence of early-life social conditions on men’s mortality. Demography. 2004;41(1):87–107. doi: 10.1353/dem.2004.0005. [DOI] [PubMed] [Google Scholar]
- 2.O’Rand AM, Hamil-Luker J. Processes of cumulative adversity: childhood disadvantage and increased risk of heart attack across the life course. J Gerontol B Psychol Sci Soc Sci. 2005;60:117–124. doi: 10.1093/geronb/60.special_issue_2.s117. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) The world health report: Reduce risks, promoting health life 2002. [Accessed October 2013]; http://www.who.int/whr/2002/en/whr02_en.pdf.
- 4.Crosnoe R. Gender, Obesity, and Education. Sociol Educ. 2007;80(3):241–260. [Google Scholar]
- 5.Merten MJ, Wickrama KAS, Williams AL. Adolescent obesity and young adult psychosocial outcomes: Gender and racial differences. J Youth Adolesc. 2008;37(9):1111–1122. [Google Scholar]
- 6.Wickrama KAS, O’Neal CW. Family of origin, race/ethnicity, and socioeconomic attainment: Genotype and intraindividual processes. J Marriage Fam. 2013;75:75–90. [Google Scholar]
- 7.De Wit LM, van Straten A, van Herten M, Penninx BW, Cuijpers P. Depression and Body Mass Index: A U-shaped Association. BMC public health. 2009;9(1):14–19. doi: 10.1186/1471-2458-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Konttinen H, Kiviruusu O, Huurre T, et al. Longitudinal associations between depressive symptoms and body mass index in a 20-year follow-up. Int J Obes (Lond) 2013 doi: 10.1038/ijo.2013.151. [DOI] [PubMed] [Google Scholar]
- 9.Burdette AM, Needham BL. Neighborhood Environment and Body Mass Index Trajectories from Adolescence to Adulthood. J Adolesc Health. 2012;50(1):30–37. doi: 10.1016/j.jadohealth.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 10.Shin SH, Miller DP. A longitudinal examination of childhood maltreatment and adolescent obesity: Results from the National Longitudinal Study of Adolescent Health (Add Health) Study. Child Abuse Negl. 2012;36(2):84–94. doi: 10.1016/j.chiabu.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 11.Conroy K, Sandel M, Zuckerman B. Poverty Grown Up: How Childhood Socioeconomic Status Impacts Adult Health. J Dev Behav Pediatr. 2010;31(2):154–160. doi: 10.1097/DBP.0b013e3181c21a1b. [DOI] [PubMed] [Google Scholar]
- 12.Ivanovic DM, Leiva BP, Perez HT, et al. Long-term Effects of Severe Undernutrition during the First Year of Life on Brain Development and Learning in Chilean High-School Graduates. Nutrition. 2000;16(11):1056–1063. doi: 10.1016/s0899-9007(00)00431-7. [DOI] [PubMed] [Google Scholar]
- 13.Conger RD, Schofiled TK, Conger KJ, Neppl TK. Economic Pressure, Parent Personality and Child Development: An Interactionist Analysis. Hist Soc Res. 2012;35(2):169–194. [PMC free article] [PubMed] [Google Scholar]
- 14.Wickrama KAS, Conger RD, Lorenz FO, Jung T. Family antecedents and consequences of trajectories of depressive symptoms from adolescence to young adulthood: a life course investigation. J Health Soc Behav. 2008;49(4):468–483. doi: 10.1177/002214650804900407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brooks-Gunn J, Peterson AC. Studying the Emergence of Depression and Depressive Symptoms during Adolescence. J Youth Adolesc. 1991;20(2):115–119. doi: 10.1007/BF01537603. [DOI] [PubMed] [Google Scholar]
- 16.Fagundes CP, Glaser R, Hwang BS, Malarkey WB, Keicolt-Glaser JK. Depressive Symptoms Enhance Stress-Induced Inflammatory Responses. Brain Behav Immun. 2012;31:172–176. doi: 10.1016/j.bbi.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kubzansky LD, Kawachi I. Going to the heart of the matter: do negative emotions cause coronary heart disease? J Psychosom Res. 2000;48(4):323–337. doi: 10.1016/s0022-3999(99)00091-4. [DOI] [PubMed] [Google Scholar]
- 18.McEwan BS. Protection and damage from acute and chronic stress: allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann N Y Acad Sci. 2004;1032:1–7. doi: 10.1196/annals.1314.001. [DOI] [PubMed] [Google Scholar]
- 19.Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative childhood stress and autoimmune diseases in adults. Psychosom Med. 2009;71(2):243–250. doi: 10.1097/PSY.0b013e3181907888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fitzgibbon ML, Spring B, Avellone ME, et al. Correlates of Binge Eating in Hispanic, Black, and White women. Int J Eat Disord. 1998;24(1):43–52. doi: 10.1002/(sici)1098-108x(199807)24:1<43::aid-eat4>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 21.Lee H, Lee D, Guo G, Harris KM. Trends in body mass index in adolescence and young adulthood in the United States: 1959–2002. J Adolesc Health. 2011;49(6):601–608. doi: 10.1016/j.jadohealth.2011.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wickrama KAS, Conger RD, Wallace LE, Elder GH. The intergenerational transmission of health-risk behaviors: adolescent lifestyles and gender moderating effects. J Health Soc Behav. 1999;40(3):258–272. [PubMed] [Google Scholar]
- 23.Dowd JB, Simanek AM, Aiello AD. Socioeconomic Status, Cortisol, and Allostatic Load: A Review of the Literature. Int J Epidemiol. 2009;38(5):1297–1309. doi: 10.1093/ije/dyp277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010;91(5):1499S–1505S. doi: 10.3945/ajcn.2010.28701B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wadden TA, Sarwer DB, Womble LG, et al. Psychosocial aspects of obesity and obesity surgery. Sug Clin North Am. 2001;81(5):1001–1024. doi: 10.1016/s0039-6109(05)70181-x. [DOI] [PubMed] [Google Scholar]
- 26.Ratcliff MB, Jenkins TM, Reiter-Purtill J, Noll JG, Zeller MH. Risk-taking behaviors of adolescents with extreme obesity: Normative or not? Pediatrics. 2011;127(5):827–834. doi: 10.1542/peds.2010-2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferraro KF, Kelley-Moore JA. Cumulative Disadvantage and Health: Long-Term Consequences of Obesity? Am Sociol Rev. 2003;68(5):707–729. [PMC free article] [PubMed] [Google Scholar]
- 28.Zheng H, Tumin D, Qian Z. Obesity and mortality risk: New findings from body mass index trajectories. Am J Epidemiol. 2013 doi: 10.1093/aje/kwt179. Advance online publication: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roberts RE, Duong HT. Obese youths are not more likely to become depressed, but depressed youths are more likely to become obese. Psychol Med. 2013;43:2143–2151. doi: 10.1017/S0033291712002991. [DOI] [PubMed] [Google Scholar]
- 30.Needham BL, Epel ES, Adler NE, Kiefe C. Trajectories of change in obesity and symptoms of depression: The CARDIA study. Am J Public Health. 2010;100(6):1040–1046. doi: 10.2105/AJPH.2009.172809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muthén LK, Muthén BO. Version 7.0. Los Angeles, CA: StatModel; MPlus. [Computer software] pp. 2008–2012. [Google Scholar]
- 32.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psyc Meas. 1977;1(3):385–401. [Google Scholar]
- 33.Perreira KM, Deeb-Sossa N, Harris KM, Bollen KA. What are we measuring? An evaluation of the CES-D across race/ethnicity and immigrant generation. Soc Forces. 2005;83(4):1567–1601. [Google Scholar]
- 34.Enders CK, Bandalos DL. The relative performance of full information likelihood estimation for missing data in structural equation models. Struct Equ Modeling. 2001;8(3):430–457. [Google Scholar]
- 35.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. [Google Scholar]
- 36.Wheaton B, Gotlib IH. Trajectories and turning points over the life course: Concepts and themes. In: Gotlib IH, Wheaton B, editors. Stress and adversity over the life course: Trajectories and turning points. New York: Cambridge University Press; 1997. pp. 1–25. [Google Scholar]
- 37.Wickrama KAS, Bryant C. Community context of social resources and adolescent mental health. J Marriage Fam. 2003;65:850–866. [Google Scholar]