Background: Heme oxygenase-1 (HO-1) is an inducible enzyme with pleiotropic immunomodulatory effects.
Results: Induction of HO-1 inhibits Th17-mediated responses in experimental colitis and switches the naive T cells to Tregs under Th17-skewing conditions in vitro.
Conclusion: HO-1 ameliorates dextran sulfate sodium (DSS)-induced colitis via blocking IL-6/IL-6R signaling to regulate Th17/Treg cell balance.
Significance: HO-1 may become a novel therapeutic target in IBD.
Keywords: Colitis, Heme Oxygenase, Inflammation, Inflammatory Bowel Disease (IBD), T Helper Cells, Th17, Treg, Heme Oxygenase-1
Abstract
Inflammatory bowel disease (IBD), including ulcerative colitis and Crohn's disease, is a group of autoimmune diseases characterized by nonspecific inflammation in the gastrointestinal tract. Recent investigations suggest that activation of Th17 cells and/or deficiency of regulatory T cells (Treg) is involved in the pathogenesis of IBD. Heme oxygenase (HO)-1 is a protein with a wide range of anti-inflammatory and immune regulatory function, which exerts significantly protective roles in various T cell-mediated diseases. In this study, we aim to explore the immunological regulation of HO-1 in the dextran sulfate sodium-induced model of experimental murine colitis. BALB/c mice were administered 4% dextran sulfate sodium orally; some mice were intraperitoneally pretreated with HO-1 inducer hemin or HO-1 inhibitor stannum protoporphyrin IX. The results show that hemin enhances the colonic expression of HO-1 and significantly ameliorates the symptoms of colitis with improved histological changes, accompanied by a decreased proportion of Th17 cells and increased number of Tregs in mesenteric lymph node and spleen. Moreover, induction of HO-1 down-regulates retinoic acid-related orphan receptor γt expression and IL-17A levels, while promoting Treg-related forkhead box p3 (Foxp3) expression and IL-10 levels in colon. Further study in vitro revealed that up-regulated HO-1 switched the naive T cells to Tregs when cultured under a Th17-inducing environment, which involved in IL-6R blockade. Therefore, HO-1 may exhibit anti-inflammatory activity in the murine model of acute experimental colitis via regulating the balance between Th17 and Treg cells, thus providing a possible novel therapeutic target in IBD.
Introduction
Inflammatory bowel disease (IBD)3 is a group of autoimmune diseases including two major clinical subtypes, ulcerative colitis (UC) and Crohn disease, characterized by chronic nonspecific inflammation in gastrointestinal tracts (1). Although the pathogenesis of IBD is still unclear, evidence has indicated that IBD is induced by abnormal T cell immune responses triggered by an inflammatory response to intestinal microorganisms in individuals with susceptible genes (2, 3). The abnormal immune response results in excessive activation of effector T cell subsets and/or deficiency of regulatory T cells (Treg), leading to persistent immune disorders and uncontrolled intestinal inflammation (4, 5).
Recent studies suggest that Th17 cells and related cytokines are critical factors in the pathogenesis of UC and Crohn disease, which have been novel targets of therapy in IBD (6–8). Th17 cells, as a recently discovered T cell subset involved in the pathophysiology of inflammatory disease, require specific cytokines and transcription factors for their differentiation, in which IL-6 and TGF-β are recognized as crucial factors (9). Moreover, retinoic acid-related orphan receptor γt (RORγt) is the key transcription factor modulating the Th17 lineage (10, 11). It has been reported that Th17 cells expressing RORγt can be isolated from peripheral blood and colon accompanied by elevated Th17-derived cytokine levels in IBD patients (12–14). Additionally, various investigations indicate that the Th17/Treg cell balance is considered to be critical for host immunity and the preservation of tolerance and that the imbalance in the development and function of Th17 cells and Tregs plays a crucial role in autoimmune diseases, including IBD (4, 15, 16). As one of the defense mechanisms developing in our immune system, Tregs are responsible for maintaining immune homeostasis and suppressing intestinal inflammation resulting from aberrant immune responses to self-antigens and commensal bacteria (17, 18). The expression of signature transcription factor forkhead box p3 (Foxp3) is indispensable to the anti-inflammatory function of Treg cells (15). Clinically, some patients with IBD display decreased tolerance and defects in their anti-inflammatory Treg function during active inflammation (19–21). Despite two distinct phenotypes, Th17 cells and Tregs can be interconverted and are reciprocally regulated during differentiation dependent on the cytokine milieu (22–24). Under proinflammatory conditions, Tregs may be able to differentiate into Th17 cells, which have unknown consequences for disease development and progression (18, 25). Therefore, regulation of Th17/Treg cell balance to enhance Tregs and suppress Th17 cells may be therapeutically effective in the treatment of IBD.
Heme oxygenase (HO)-1, as a rate-limiting enzyme for heme metabolism, catalyzes heme into carbon monoxide (CO), free iron, and biliverdin, and exerts a wide range of anti-inflammatory, anti-apoptosis, and immune regulatory effects in the body (26–28). Studies have demonstrated that hemin, a substrate of HO-1, significantly increases the expression of HO-1 protein as well as its activity and ameliorates inflammation in a variety of animal models (29–31). The competitive inhibitor Sn-protoporphyrin IX (SnPP) also induces the expression of HO-1 but blocks the enzymatic activity in both animal models and cultured cells, creating an opposite effect (32–35). Because HO-1 has pleiotropic immunomodulatory effects, there are already numerous illustrations of therapeutic applications of HO-1 in multiple experimental models of IBD mediated by various immune mechanisms (36–38). Additionally, our previous studies have suggested that induction of HO-1 attenuates the airway inflammation in a mouse asthma model through promoting Tregs in eosinophilic airway inflammation (39, 40) and inhibiting Th17 responses in non-eosinophilic airway inflammation (41). However, little is known about how HO-1 exerts immune regulatory effects under different inflammatory conditions. Thus, this study aims to further explore the protective effects of HO-1 and the underlying mechanisms involved in regulating the Th17/Treg cell balance in the dextran sulfate sodium (DSS)-induced murine model of acute experimental colitis.
EXPERIMENTAL PROCEDURES
Mice
Female BALB/c mice (6∼8 weeks old) were purchased from Shanghai SLAC Laboratory Animal Co., Ltd. and maintained in specific pathogen-free conditions in the Research Center for Experimental Medicine of Ruijin Hospital, affiliated with the Shanghai Jiao Tong University School of Medicine. All animal experiments were approved by and performed in compliance with the guidelines of the Ethics Committee of Ruijin Hospital (Shanghai Jiao Tong University School of Medicine).
Induction of Colitis and Administration of Hemin or SnPP
Mice were randomly divided into four groups, including the DSS, DSS+hemin, DSS+SnPP, and control groups (n = 6 in each group). Mice in the DSS, DSS+hemin, and DSS+SnPP groups were fed with 4% (w/v) DSS (MP Biochemicals) in drinking water and normal water in the control group from day 0. Mice were intraperitoneally administered 75 μmol/kg of hemin (Sigma-Aldrich) or 75 μmol/kg of SnPP (Porphyrin Products) on days −2 and −1 in the DSS+hemin and the DSS+SnPP groups, respectively. Hemin or SnPP was dissolved in 0.2 mol/liter NaOH, titrated to pH 7.4 with 0.2 mol/liter HCl, and then diluted with phosphate-buffered saline (PBS). We evaluated the severity of colitis by the daily monitoring of clinical manifestations such as weight loss, diarrhea, and rectal bleeding, and scoring disease activity index as described previously (Table 1) (38). Mice were anesthetized and sacrificed at the end of the experiment (day 7), and the colons, spleens, and mesenteric lymph node (MLN) were harvested for further assays.
TABLE 1.
The DAI scores
| Weight loss (%)a | Stool consistencyb | Occult bloodc | Score |
|---|---|---|---|
| 0 | Normal | Negative | 0 |
| 1∼5 | 1 | ||
| 5∼10 | Loose | Occult blood-positive | 2 |
| 10∼20 | 3 | ||
| >20 | Diarrhea | Gross bleeding | 4 |
a Five grades of weight loss (0, no loss or weight gain; 1, 1–5% loss; 2, 5–10% loss; 3, 10–20% loss; 4, >20% loss).
b Three grades of stool consistency (0, normal; 2, loose; and 4, diarrhea).
c Three grades of occult blood (0, negative; 2, occult blood-positive; and 4, gross bleeding).
Histopathology
Colons were fixed with 10% neutral buffered formalin and embedded in paraffin. Four-micrometer-thick sections were stained with H&E. Colonic inflammation was assessed under the light microscope (Olympus AX70) according to the degree of epithelial erosion, ulceration, vascular density, and leukocyte infiltration.
Western Blot Analysis
Colons were homogenized with ice-cold radioimmune precipitation assay buffer (Beyotime, Shanghai, China) containing protease inhibitors. The extracts containing 30 μg of proteins were separated on 12% SDS-PAGE and then transferred to polyvinylidene fluoride membranes. The membrane was blocked with Tris-buffered saline Tween 20 (TBST) buffer containing 5% skim milk and incubated with the following primary antibodies: rabbit anti-mouse RORγt IgG and rabbit anti-mouse Foxp3 IgG (1/1000 dilution, Santa Cruz Biotechnology, Santa Cruz, CA); mouse anti-mouse HO-1 IgG (1/1000 dilution, Cell Signaling). The samples were incubated overnight followed by addition of horseradish peroxidase-conjugated anti-rabbit or anti-mouse IgG secondary antibodies (1/5000 dilution, Cell Signaling). The signals were visualized via enhanced chemiluminescence using a Thermo ECL kit (Thermo Fisher Scientific, Waltham, MA) according to the manufacturer's instructions.
HO-1 Activity Assay
HO-1 enzyme activity was assessed by measuring bilirubin production as described previously with modifications (36). The colons were homogenized in 10 mmol/liter HEPES, 32 mmol/liter sucrose, 1 mmol/liter dithiotreitol (DTT), 0.1 mmol/liter EDTA, 10 μg/ml soybean trypsin inhibitor, 10 μg/ml leupeptin, and 2 μg/ml aprotinin and centrifuged at 18,000 × g for 30 min at 4 °C. The supernatant was used to measure HO activity. The reaction mixture, consisting of 200 μl of sample homogenate, 100 μl of normal liver cytosol (source of biliverdin reductase), 20 μmol/liter hemin, and 0.8 mmol/liter NADPH, was incubated at 37 °C for 1 h. The optical density (OD) was measured between 464 and 530 nm (extinction coefficient, 40 mmol/liter/cm for bilirubin) to assess bilirubin production once the reaction was terminated by putting samples in an ice bath. Values were expressed as pmol of bilirubin formed per hour per milligram protein.
Isolation and Culture of Mesenteric Lymph Node and Spleen Cells
MLNs and spleens were removed. Single-cell suspensions were prepared by passing the tissue through a nylon mesh (70-μm pore size). Erythrocytes were lysed with hypotonic buffer (0.15 mol/liter NH4Cl, 10 mmol/liter KHCO3, 0.1 mmol/liter Na2EDTA). Cells were washed twice with PBS and incubated in RPMI 1640 medium (HyClone) supplemented with 1% l-glutamine (0.2 mol/liter), 10% FCS, 100 international units/ml penicillin/streptomycin, 1% HEPES (1 mol/liter), 1% sodium hydrogen carbonate (100 mmol/liter), and 0.1% 2-β-mercaptoethanol (50 mmol/liter, Invitrogen) in the presence of anti-CD3 and anti-CD28 antibodies (eBioscience, San Diego, CA) for 48 h. Cells were collected and analyzed using flow cytometry (FCM). Cytokine production in culture supernatants was determined using enzyme-linked immunosorbent assay (ELISA).
Th17 Cell Differentiation in Vitro
Spleens from 8-week-old female BALB/c mice were removed and minced with a nylon mesh (70-μm pore size). After the cells were pelleted, erythrocytes were lysed with hypotonic buffer. Naive CD4+ T cells were purified via magnetic isolation (MiltenyiBiotec, Bergisch Gladbach, Germany) according to the manufacturer's instructions. Cells were seeded at a density of 1 × 106 per well in 48-well plates and cultured in RPMI 1640 medium (HyClone) supplemented with 1% l-glutamine (0.2 mol/liter), 10% FCS, 100 international units/ml penicillin/streptomycin, 1% HEPES (1 mol/liter), 1% sodium hydrogen carbonate (100 mmol/liter) and 0.1% 2-β-mercaptoethanol (50 mmol/liter, Invitrogen). The cells were activated with plate-bound anti-CD3 (2 μg/ml) and soluble anti-CD28 (2 μg/ml) antibodies (eBioscience). Th-neutral conditions (Th0) included no exogenous cytokines or anti-cytokines. For Th17 differentiation, cells were stimulated with TGF-β1 (5 ng/ml, Cell Signaling), IL-6 (50 ng/ml, R&D Systems), IL-23 (20 ng/ml, R&D Systems), anti-IFN-γ (10 μg/ml, Biolegend), and anti-IL-4 (10 μg/ml, Biolegend). Hemin and SnPP were dissolved in 0.2 mol/liter NaOH at a concentration of 50 μmol/ml and added to cultures at an appropriate concentration of 30 nmol/ml. After 5 days, cells were collected for FCM analysis and RNA extraction.
FCM
For detection of IL-6R, Th17, and Treg cells, cells were stimulated with lymphocyte activator mixture (phorbol 12-myristate 13-acetate/ionomycin/brefeldin A, BD Pharmingen, San Diego, CA) for 5 h and labeled with surface markers FITC anti-CD4 mAb, APC anti-CD25 mAb and PE anti-IL-6R mAb (eBioscience). After washing, fixing, and permeabilizing according to the manufacturer's instructions (eBioscience), cells were labeled intracellularly with PE-Cy7 anti-IL-17 mAb (Biolegend) or APC anti-IL-10 mAb and PE anti-Foxp3 mAb (eBioscience). All labeled cells were detected using FCM on the FACScan Flow Analyzer. The data were analyzed with FlowJo software (version 7.6).
ELISA
The concentrations of IL-17A and IL-6 (Biolegend, San Diego, CA) in colonic homogenates or cell culture supernatant were analyzed with ELISA kits in accordance with the manufacturers' instructions.
qRT-PCR
Colons and spleens were removed and cells cultivated in vitro were collected and homogenized to extract total RNA with TRIzol reagent (Invitrogen Invitrogen, Carlsbab, CA) according to the manufacturer's instructions. Reverse transcription was performed using PrimeScript reverse transcriptase (TaKaRa, Japan) to obtain cDNA samples. Quantitative real-time reverse transcription polymerase chain reaction (qRT-PCR) was performed using an ABI Prism 7300 (Applied Biosystems) with the following program: 95 °C for 10 s and 40 cycles of amplification at 95 °C for 5 s, 60 °C for 31 s, and 95 °C for 15 s, and finally, 60 °C for 30 s and 95 °C for 15 s. Relative levels of target mRNA were compared with β-actin using the 2−ΔΔCt method. All primers were synthesized by Shanghai Shengon Biotech Company (Shanghai, China). Sequences were as follows: β-actin, 5′-GGC TGT ATT CCC CTC CAT CG-3′ (forward) and 5′-CCA GTT GGT AAC AAT GCC ATG T-3′ (reverse); Foxp3, 5′-CAC AAT ATG CGA CCC CCT TTC-3′ (forward) and 5′-AAC ATG CGA GTA AAC CAA TGG TA-3′ (reverse); RORγt, 5′-GAC CCA CAC CTC ACA AAT TGA-3′ (forward) and 5′-AGT AGG CCA CAT TAC ACT GCT-3′ (reverse); IL-17A, 5′-TTT AAC TCC CTT GGC GCA AAA-3′ (forward) and 5′-CTT TCC CTC CGC ATT GAC AC-3′ (reverse); IL-6, 5′-TAG TCC TTC CTA CCC CAA TTT CC-3′ (forward) and 5′-TTG GTC CTT AGC CAC TCC TTC-3′ (reverse); IL-10, 5′-AGA AGC ATG GCC CAG AAA TCA-3′ (forward) and 5′-GGC CTT GTA GAC ACC TTG GT-3′ (reverse); IL-6R, 5′-TGA ATA GAG ATG CCC GTC AG-3′ (forward) and 5′-TGC TTG GAC TTT AGG AGT TCG-3′ (reverse); and HO-1, 5′-AAG CCG AGA ATG CTG AGT TCA-3′ (forward) and 5′-GCC GTG TAG ATA TGG TAC AAG GA-3′ (reverse).
Statistical Analysis
Data are presented as the mean ± S.D. The differences between mean values were calculated using an unpaired t test or nonparametric statistics. p < 0.05 was considered statistically significant.
RESULTS
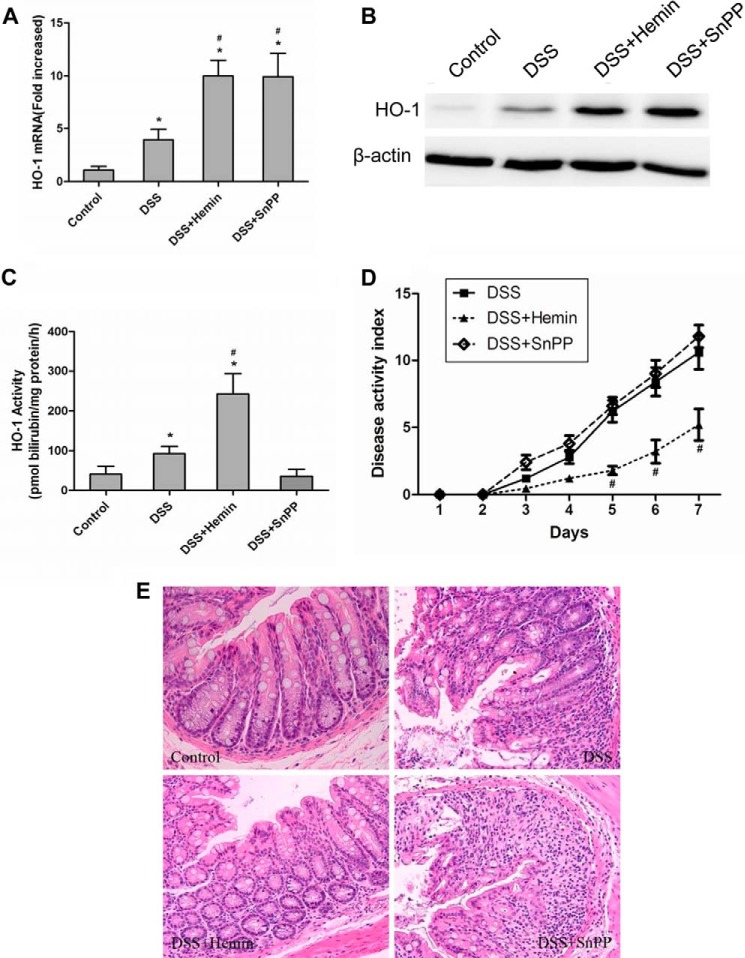
Colonic HO-1 Expression and Activity in DSS-induced Colitis
HO-1 is the inducible one of the three HO isozymes (42). The expression of HO-1 is up-regulated in response to cellular stress and by several factors, such as pro-oxidative stimuli, UV light, LPS, and heavy metals (28). We sought to determine whether DSS challenge could increase HO-1 expression in colons. After mice were sacrificed on day 7, the colons were taken for RNA and protein extraction. qRT-PCR and Western blot assays confirmed that the HO-1 mRNA expression and protein level were enhanced in the DSS group as compared with the control group (Fig. 1, A and B), accompanying the increase of HO-1 enzyme activity (Fig. 1C). Furthermore, the levels of HO-1 mRNA and protein in colon were significantly increased after administration of hemin and SnPP (Fig. 1, A and B). HO-1 activity was enhanced in the DSS+hemin group, but inhibited in the DSS+SnPP group (Fig. 1C).
FIGURE 1.
Induction of colonic HO-1 by hemin ameliorates DSS-induced colitis. Colitis was induced in BALB/c mice using DSS as described under “Experimental Procedures.” A, qRT-PCR analysis of HO-1 mRNA in colons isolated from four groups. Data are presented as mean ± S.D. B, Western blot analysis of HO-1 protein in colons extracted from four groups. β-Actin was used as loading control. C, the analysis of HO-1 activity in colons extracted from four groups. Data are presented as mean ± S.D. D, disease activity index scores of each group. Data are presented as mean ± S.D. E, histological analysis of colons isolated from each group. Paraffin-embedded colonic sections were stained with hematoxylin and eosin to observe inflammation (original magnification, × 200). Each symbol in the graph represents an individual mouse (n = 6; *, compared with control group; *, p < 0.05; #, compared with DSS group; #, p < 0.05). All results shown are representative of three independent experiments.
Induction of HO-1 by Hemin Ameliorates DSS-induced Colitis
The initial body weights did not differ among the four groups. Intake of DSS solution was monitored during the experiments to maintain the same dose in each group. Mice receiving DSS developed colitis, characterized by sustained weight loss, diarrhea, and rectal bleeding. Disease activity index scores evaluated by these symptoms were lower in the DSS+hemin group than in the DSS group, but were not reduced after treatment with SnPP (Fig. 1D). Histological study confirmed that administration of 4% DSS induced pathological changes in colons, including epithelial crypt loss, ulceration, prominent monocytic infiltration throughout the mucosa, and mucosal bleeding (Fig. 1E). In contrast, mice treated with hemin intraperitoneally for 2 days before DSS challenge showed less inflammatory cell infiltration, smaller erosions and mucosal integrity, thus remarkably improving the histological changes and ameliorating DSS-induced colitis, but SnPP administration did not exert any protective effects (Fig. 1E).
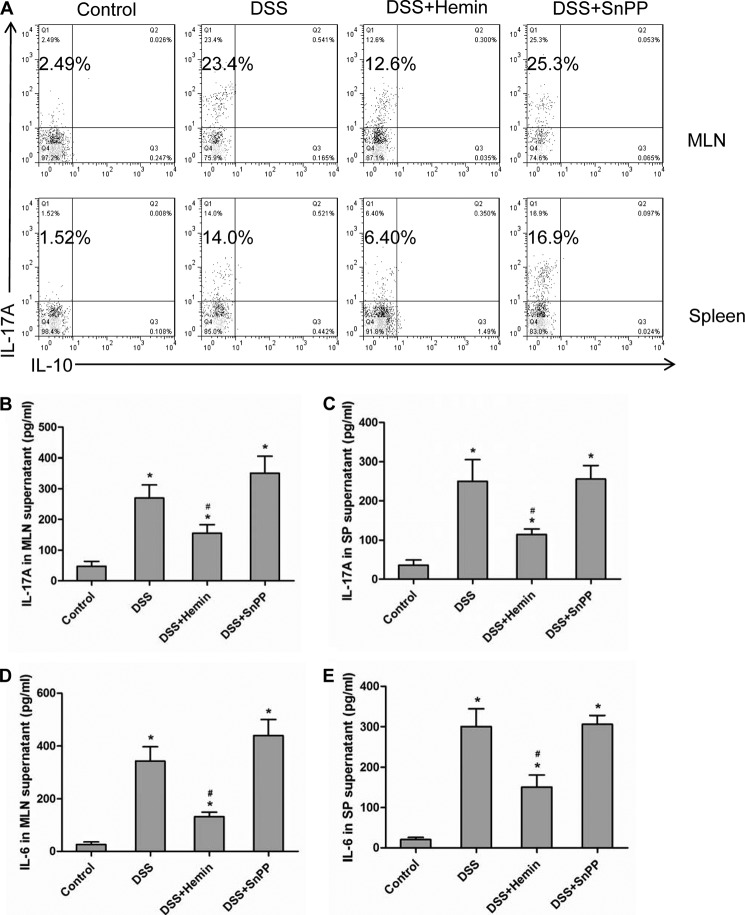
Hemin Treatment Inhibits Th17 Cell-mediated Responses in Vivo
Next, we evaluated the effect of HO-1 on Th17 response in DSS-induced colitis. The MLNs and spleens were isolated to prepare single-cell suspensions. Cells were cultured with anti-CD3 and anti-CD28 antibodies for 48 h. FCM results revealed that the proportions of CD4+ IL-17A+ T cells (Th17 cells) in MLNs and spleens were increased in the DSS and the DSS+SnPP groups in comparison with those in the control group (Fig. 2A). However, the percentage of Th17 cells in the DSS+hemin group was significantly lower than that in the DSS group (Fig. 2A). The levels of IL-17A and IL-6 in the cell culture supernatant, cytokines related to Th17 cells, were analyzed by ELISA. As shown in Fig. 2, B–E, IL-17A and IL-6 production in MLNs and spleens isolated from the DSS group exhibited higher levels than did those from the control group but were lower in mice treated with hemin. There was no significant difference in IL-17A or IL-6 levels between DSS and DSS+SnPP groups (Fig. 2, B–E).
FIGURE 2.
Hemin treatment inhibits Th17-mediated responses in MLNs and spleens. A, flow cytometric analysis of cells from MLNs and spleens of BALB/c mice cultured in the presence of anti-CD3 and anti-CD28 antibodies for 48 h. Numbers in upper left quadrants indicate the percentages of Th17 (CD4+ IL-17+) cells gated on CD4+ T cells. Each symbol in the graph represents an individual mouse (n = 6). B, ELISA analysis of IL-17A in supernatants of cultured MLN cells. Data are presented as mean ± S.D. C, ELISA analysis of IL-17A in supernatants of cultured spleen cells. Data are presented as mean ± S.D. D, ELISA analysis of IL-6 in supernatants of cultured MLN cells. Data are presented as mean ± S.D. E, ELISA analysis of IL-6 in supernatants of cultured spleen cells. Data are presented as mean ± S.D. (*, compared with control group; *, p < 0.05; #, compared with DSS group; #, p < 0.05). All results shown are representative of three independent experiments.
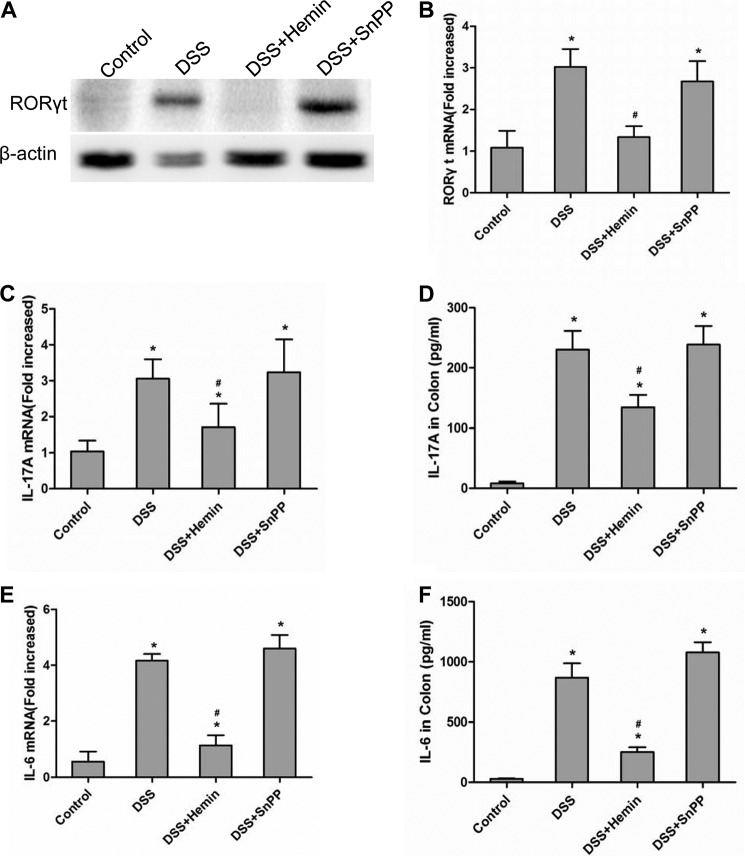
We further determined the expression of RORγt, the key transcription factor that regulates Th17 cell differentiation as well as IL-17A and IL-6 levels in colons. Western blot and qRT-PCR assays showed that the levels of RORγt protein and mRNA expression were significantly up-regulated in the DSS and the DSS+SnPP groups, but declined in the DSS+hemin group (Fig. 3A and B). Meanwhile, the levels of IL-17A and IL-6 protein and mRNA expression in colons were also determined by ELISA and qRT-PCR. Consistent with the results of RORγt protein and mRNA expression, the levels of both IL-17A and IL-6 and mRNA expression were higher in the DSS and the DSS+SnPP groups than those in the control group, but decreased in mice after hemin treatment (Fig. 3, C–F).
FIGURE 3.
Hemin treatment inhibits Th17-mediated responses in colons. A, Western blot analysis of RORγt protein expression in colons extracted from the four groups. β-Actin was used as loading control. B, QRT-PCR analysis of RORγt mRNA in colons isolated from four groups. Data are presented as mean ± S.D. C, QRT-PCR analysis of IL-17A mRNA in colons isolated from four groups. Data are presented as mean ± S.D. D, ELISA analysis of IL-17A in colons isolated from four groups. Data are presented as mean ± S.D. E, qRT-PCR analysis of IL-6 mRNA in colons isolated from four groups. Data are presented as mean ± S.D. F, ELISA analysis of IL-6 in colons isolated from four groups. Data are presented as mean ± S.D. (*, compared with control group, *, p < 0.05; #, compared with DSS group, #, p < 0.05). All results shown are representative of three independent experiments.
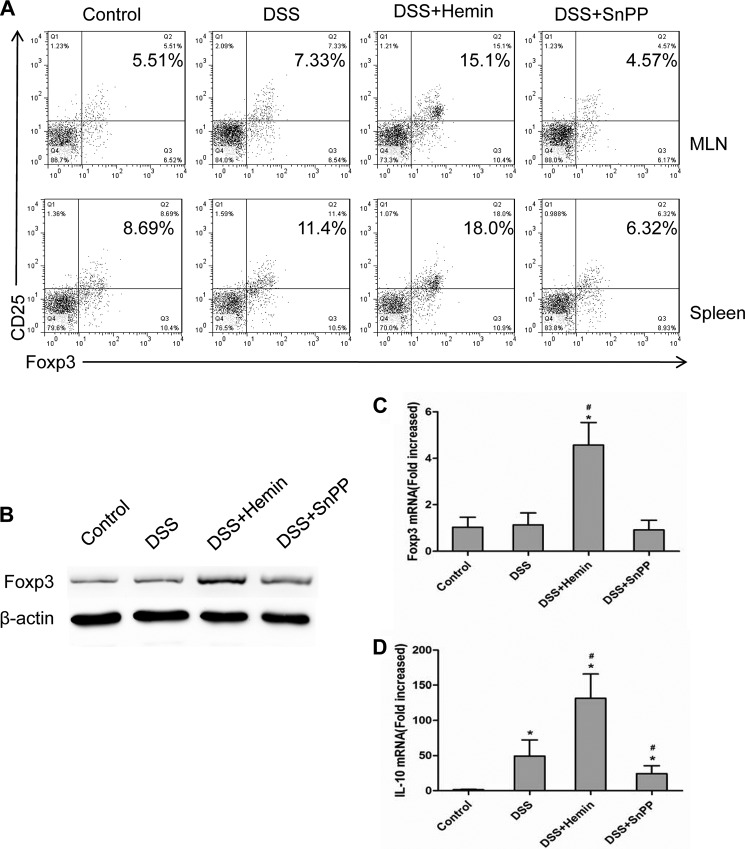
Hemin Treatment Promotes Treg Cell Development in Vivo
Tregs are considered important for immune homeostasis (15), and the imbalance of Th17 cells and Tregs plays a crucial role in IBD development (4, 16). We have previously reported that induction of HO-1 by hemin suppressed airway inflammation via up-regulating Tregs and IL-10 production (39, 40). Thus, we also investigated the changes in Tregs in DSS-induced colitis. As shown in Fig. 4A, FCM analysis indicated that DSS challenge slightly increased the percentages of CD4+ CD25+ Foxp3+ T cells (Tregs) in MLNs and spleens. There was a significant increase in Treg populations in the DSS+hemin group versus the DSS group, whereas inhibition of HO-1 enzymatic activity by SnPP led to a decline in Tregs (Fig. 4A). Foxp3 protein and mRNA levels in colon were further determined by Western blot and qRT-PCR, respectively. The results were in accordance with FCM, showing that the levels of Foxp3 protein and mRNA expression were significantly up-regulated by hemin treatment and were decreased in the presence of SnPP (Fig. 4, B and C). In addition, the mRNA expression of anti-inflammatory cytokine IL-10 in colon was also measured by qRT-PCR. The results demonstrated that IL-10 mRNA expression was markedly elevated in the DSS+hemin group but decreased in the DSS+SnPP group as compared with the DSS group (Fig. 4D).
FIGURE 4.
Hemin treatment promotes Treg cells in vivo. A, flow cytometric analysis of MLN and spleen cells isolated from BALB/c mice in the control, DSS, DSS+hemin, and DSS+SnPP groups. Numbers in upper right quadrants indicate the percentages of Tregs (CD4+ CD25+ Foxp3+) gated on CD4+ T cells. Each symbol in the graph represents an individual mouse (n = 6). B, Western blot analysis of Foxp3 protein expression in colons isolated from four groups. C, qRT-PCR analysis of Foxp3 mRNA in colons isolated from four groups. Data are presented as mean ± S.D. D, qRT-PCR analysis of IL-10 mRNA in colons isolated from four groups. Data are presented as mean ± S.D. (*, compared with control group, *, p < 0.05; #, with DSS group, #, p < 0.05). All results shown are representative of three independent experiments.
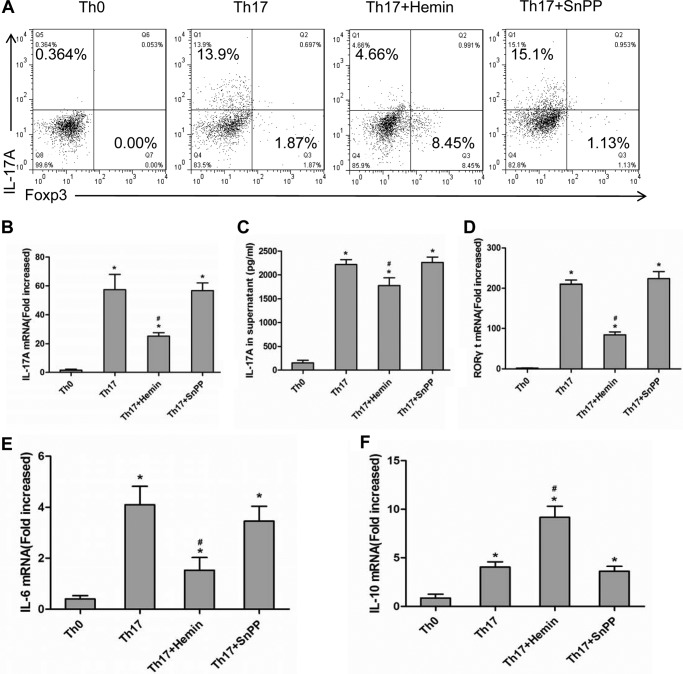
Induction of HO-1 Switched Naive T Cells to Treg Differentiation in Vitro
Because we observed that induction of HO-1 reduced Th17 cell populations but promoted Tregs in vivo, we further investigated the effect of HO-1 on Th17 cell differentiation in vitro. Purified naive CD4+ T cells from normal BALB/c mouse spleens were cultured under Th17-skewing conditions with or without hemin or SnPP. IL-17A and Foxp3 expression was determined by intracellular labeling, and the percentages of CD4+ IL-17A+ T cells (Th17 cells) and CD4+ Foxp3+ T cells (Tregs) were determined in CD4+ T cells by FCM. As shown in Fig. 5A, there was a significant inhibitory effect of hemin on Th17 cell differentiation at a concentration of 30 nmol/ml. Moreover, the population of CD4+ Foxp3+ T cells was increased, resulting in switching naive T cells to Treg differentiation. However, Th17 cell differentiation was not affected when 30 nmol/ml SnPP was added to the medium, a result quite opposite to the hemin effect (Fig. 5A). Meanwhile, the levels of RORγt, IL-17A, and IL-6 mRNA, as well as IL-17A level in supernatants were determined by qRT-PCR and ELISA, respectively. Consistent with the results from FCM analysis, hemin treatment reduced IL-17A mRNA expression and protein level (Fig. 5, B and C) and down-regulated RORγt mRNA expression (Fig. 5D). In addition, hemin also inhibited IL-6 mRNA expression (Fig. 5E) but increased IL-10 mRNA expression in cultured cells (Fig. 5F). However, SnPP did not exert the similar effect as hemin.
FIGURE 5.
Induction of HO-1 switched naive T cell differentiation from Th17 to Treg cells in vitro. A, flow cytometric analysis of magnetically purified naive T cells from spleens of BALB/c mice cultured under Th17-skewing conditions with or without hemin or SnPP (30 nmol/ml) for 5 days. Numbers in upper left quadrants indicate the percentages of Th17 (CD4+ IL-17+) cells gated on CD4+ T cells. Numbers in lower right quadrants indicate the percentages of Tregs (CD4+ Foxp3+) gated on CD4+ T cells. B, qRT-PCR analysis of IL-17A mRNA in cells cultured in vitro. Data are presented as mean ± S.D. C, ELISA analysis of IL-17A in supernatants of cultured cells. Data are presented as mean ± S.D. D, qRT-PCR analysis of RORγt mRNA in cultured cells in vitro. E, qRT-PCR analysis of IL-6 mRNA in cultured cells in vitro. Data are presented as mean ± S.D. F, qRT-PCR analysis of IL-10 mRNA in cultured cells in vitro. Data are presented as mean ± S.D. (*, compared with Th0 group, *, p < 0.05; #, with Th17 group, #, p < 0.05). All results shown are representative of three independent experiments.
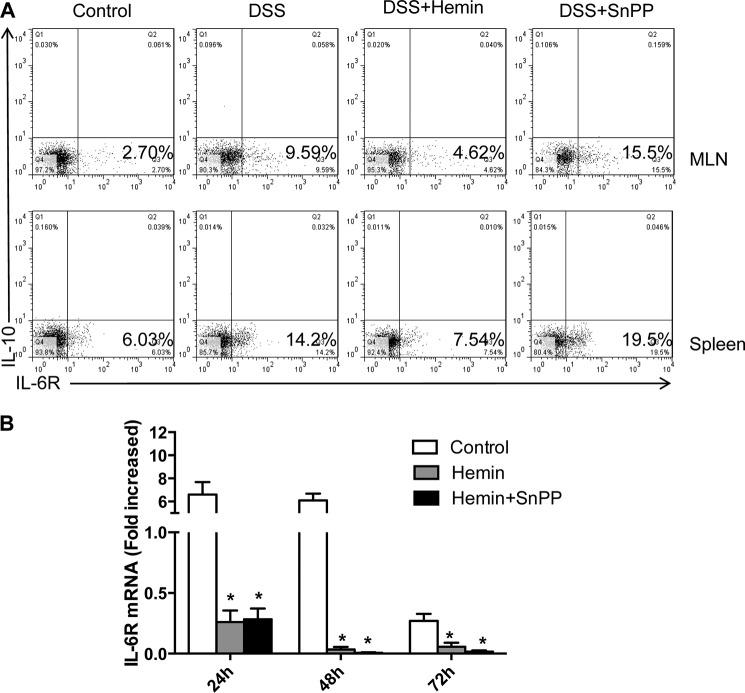
Hemin Treatment Down-regulated IL-6R Expression
IL-6 binds to a cognate membrane-bound receptor (IL-6R) to mediate many biological activities, which is necessary for the expression of multiple transcription factors involved in Th17 differentiation and directly regulates the RORγt and IL-17 expression. We supposed that HO-1 could blockade Th17 differentiation via affecting the expression of IL-6R on CD4+ T cells. Therefore, we detected IL-6R expression on CD4+ T cells and the level of IL-6R mRNA. FCM results showed that the expression of IL-6R on CD4+ T cells in MLNs and spleens was up-regulated in the DSS and the DSS+SnPP groups in comparison with the control group. But hemin treatment significantly down-regulated the expression of IL-6R on CD4+ T cells (Fig. 6A). Furthermore, splenocytes were isolated from BALB/c mice, and CD4+ T cells were activated in the presence of anti-CD3 and anti-CD28 in vitro for 72 h. The results also confirmed that the expression of IL-6R mRNA was significantly down-regulated by hemin at 24 and 48 h (Fig. 6B). We infer from these studies that HO-1 inhibits IL-6R expression and governs IL-6/IL-6R signaling to block Th17 cell differentiation.
FIGURE 6.
Hemin treatment inhibits IL-6R expression on CD4+ T cells. A, flow cytometric analysis of MLN and spleen cells isolated from BALB/c mice cultured in the presence of anti-CD3 and anti-CD28 antibodies for 48 h. Numbers in lower right quadrants indicate the percentages of IL-10+ IL-6R+ cells gated on CD4+ T cells. Each symbol in the graph represents an individual mouse (n = 6). B, qRT-PCR analysis of IL-6R mRNA in cultured cells with or without hemin or SnPP (30 nmol/ml) for 5 days in vitro. Data are presented as mean ± S.D. (*, compared with Th17 group, *, p < 0.05). All results shown are representative of three independent experiments.
DISCUSSION
In the present study, we use BALB/c mice to explore the consequences of DSS exposure on systemic and local inflammation and the effect of HO-1. DSS is a widely used chemical to induce a murine model of IBD, the clinical and pathological manifestations of which are found to resemble human UC (43–45). Thus, we fed the mice with 4% DSS for 7 days on the basis of pretreatment with or without hemin and SnPP according to our previous study (46) to observe the effect of HO-1 induction on DSS-induced colitis. The results demonstrate that the DSS-induced acute experimental colitis model increased the Th17 cell population and IL-17 production level. Furthermore, induction of HO-1 by hemin significantly ameliorates colitis in mice through inhibiting Th17 responses and down-regulating Th17-related transcription factors and cytokines, while increasing Treg numbers and promoting IL-10 production, to restore the Th17/Treg cell balance. These data suggest a possible role of HO-1 as a novel regulator of Th17/Treg cell balance to benefit the prognosis of colitis and improve the outcome of intestinal inflammation.
Although IBD is a multifactorial disease, involving genetic, immunological and environmental factors, the onset is characterized by an autoimmune inflammation that causes excessive production of proinflammatory cytokines to damage intestinal mucosa (47). Notably, it has been determined that HO-1 is prominently up-regulated in inflamed colon in the DSS-induced model of experimental colitis (46, 48, 49), corresponding with our observations in this study. As a rate-limiting enzyme of heme metabolism, HO-1 has been considered an attractive target for the prevention and treatment of a variety of diseases (50). It catalyzes heme into CO, free iron, and biliverdin and is inducible by several factors, including pro-oxidative stimuli, UV light, LPS, heat shock, and heavy metals (42). As an anti-inflammatory and immunoregulatory protein, HO-1 has been well studied in several autoimmune disease models involving different T cell subsets (26, 51). Pharmacological induction of HO-1 has a potential therapeutic role in IBD, partly attributable to the beneficial effects of its products such as biliverdin and CO (52, 53). In accordance, our data have indicated that hemin, a major substrate of HO-1, could induce colonic HO-1 expression and increase its enzymatic activity, significantly attenuating DSS-induced colitis. However, the competitive inhibitor SnPP did not have this protective effect, as it blocked the enzymatic activity of HO-1.
Accumulating evidence has demonstrated that Th17 cells associate closely with many autoimmune diseases, including IBD (6–8). IL-17A and IL-6 are two critical Th17 cell related cytokines. As a newly categorized T cell subset, Th17 cells are capable of producing IL-17A, which increases IL-6 and IL-8 levels, evoking recruitment of neutrophils and T cell proliferation and thus promoting inflammatory responses (54). IL-6, derived from several cell types such as T cells, dendritic cells, or macrophages activates the STAT3 (signal transducer and activator of the transcription 3) signal pathway to induce RORγt expression and determines Th17 cell differentiation (55). Th17 cells and the related cytokines are important factors in the pathogenesis of IBD, as IL-17A, IL-6 and IL-23 have been observed to increase remarkably in UC and Crohn disease patients. This is seen especially in UC, associating positively with disease activity and clinical grading (8). Research using animal models also has shown that IL-17/IL-23 is critical for IBD development (56, 57). Several studies have demonstrated that up-regulation of HO-1 has been found to ameliorate the symptoms of Th17 cell-mediated autoimmune disorders (58–60). In this experiment, our data show that both IL-17A and IL-6 production in spleen and MLN cell culture supernatants and colon were decreased by hemin administration. Furthermore, hemin suppressed RORγt expression and decreased the Th17 cell population. Thus, we suppose that the protective effect of HO-1 in DSS-induced colitis could be due to its inhibition of Th17 cell-mediated responses.
In contrast to Th17 cells, Tregs are indispensable for immune homeostasis. They inhibit autoimmunity and protect against tissue injury, and Foxp3 is regarded as the marker of active Tregs (17, 18). As an important anti-inflammatory cytokine, IL-10 can be secreted by Tregs and be involved in intestinal homeostasis, a defect of which causes spontaneous colitis in mice (61). In addition, the beneficial effect of Tregs is dependent on IL-10 in animal models of colitis, and IL-10+ Tregs are mainly observed in colonic lamina propria (62, 63). According to previous reports, HO-1 can exert an immune regulatory effect through modulating Tregs and IL-10 (39, 64). It has been proved that Tregs from humans or mice express HO-1 and that the function of Tregs is significantly inhibited when chemicals are added to suppress HO-1 activity in vitro (65, 66). Thus, we consider that the changes in the proportion of Tregs and expression of IL-10 in our current study may suggest that HO-1 induction is implicated in promoting Foxp3 expression, enhancing Treg number and secreting IL-10 production to attenuate colitis.
There is a dynamic balance between the development of Th17 and Treg cells, which is driven by the cytokine milieu. TGF-β and IL-6 are required for activating STAT3 and RORγt and initiating Th17 cell differentiation, whereas TGF-β also directs Foxp3 expression and induces the generation of Tregs and IL-10 (22, 55). Furthermore, Treg cell differentiation can be suppressed by IL-6 via inhibition of the expression of Foxp3 in a STAT3-dependent pathway, leading to immune pathology. Therefore, IL-6 is a key modulator of the STAT3-RORγt/Foxp3 signaling pathway which drives Th17 and Treg cell differentiation (67). An in vitro study suggests a regulatory role of HO-1 and its products in controlling T cell differentiation (68). CO produced by HO-1 suppresses T cell proliferation via inhibition of IL-2 production (69); biliverdin, as the ligand of the aryl hydrocarbon receptor, directs the development of CD4+ T cells toward Tregs or Th17 cells (70). Based on the above observations in vivo, we further explored the regulation of Th17/Treg cell balance by HO-1 through in vitro study, culturing naive T cells from spleens of BALB/c mice under Th17-skewing conditions with or without hemin or SnPP. Surprisingly, hemin interference decreased the percentage of CD4+ IL-17A+ cells while increasing that of CD4+ Foxp3+ cells, as well as suppressing RORγt, IL-17A, and IL-6 but enhancing IL-10 expression levels. It is evident that cytokine responses, including IL-6, are typically governed by specific membrane-bound receptor subunits. IL-6 signaling relies on its interaction with membrane-bound IL-6R. Thus, we examined IL-6R expression on CD4+ T cells in MLNs and spleens and the level of IL-6R mRNA from splenic T cell culture. Our results demonstrated that IL-6R expression significantly down-regulated after hemin treatment. These findings imply that induction of HO-1 may switch the naive T cell differentiation from Th17 toward Treg cells through blocking IL-6R expression and manipulate the homeostasis of T cell subsets. Therefore, the Th17/Treg cell balance can be restored by HO-1, which favors Tregs and inhibits Th17 cells in colitis. The anti-inflammatory mechanism of HO-1 may involve in IL-6/IL-6R signaling. This mediated kinetics of RORγt and Foxp3 expression and reconstructed Th17/Treg cell balance. However, further research is needed to interpret the exact mechanism of HO-1 in affecting the signaling events that underlie the fates of CD4+ T cells in forming distinct Th subsets.
In summary, our data indicate that HO-1 attenuated DSS-induced colitis in mice and was associated with a remarkable decrease in Th17 cells and increase in Tregs. In particular, TGF-β plus IL-6-induced Th17 cell differentiation is likely inhibited by HO-1 via blockading IL-6R and switching Th17 cell differentiation toward Treg development. Although further studies are warranted to determine the mechanisms involved in this phenomenon in more detail, HO-1 may have great potential as a novel therapeutic target, offering a promising alternative to our current approaches to management of IBD. Development of new agents that are capable of inducing HO-1 with more specific anti-inflammatory effects and less compromise of host defense might be of therapeutic value for treatment of additional autoimmune disorders.
Acknowledgment
We thank the flow cytometry core facility at Shanghai Jiaotong University School of Medicine for flow cytometric analysis.
This work was supported by National Natural Science Foundation of China Grants 81270084, 81070022, and 30871022 and Shanghai Municipal Science and Technology Commission Foundation Grants 13XD1402800 and 10410701000.
- IBD
- inflammatory bowel disease
- HO
- heme oxygenase
- UC
- ulcerative colitis
- DSS
- dextran sulfate sodium
- Th17
- T help cell 17
- Treg
- regulatory T cell
- SnPP
- stannum protoporphyrin IX
- MLN
- mesenteric lymph node
- RORγt
- retinoic acid-related orphan receptor γt
- Foxp3
- forkhead box p3
- qRT-PCR
- quantitative real-time reverse-transcription polymerase chain reaction
- IL-6R
- interleukin-6 receptor.
REFERENCES
- 1. Baumgart D. C., Carding S. R. (2007) Inflammatory bowel disease: cause and immunobiology. Lancet 369, 1627–1640 [DOI] [PubMed] [Google Scholar]
- 2. Boirivant M., Cossu A. (2012) Inflammatory bowel disease. Oral Dis. 18, 1–15 [DOI] [PubMed] [Google Scholar]
- 3. Kim J. M. (2010) [Inflammatory bowel diseases and enteric microbiota]. Korean J. Gastroenterol. 55, 4–18 [DOI] [PubMed] [Google Scholar]
- 4. Eastaff-Leung N., Mabarrack N., Barbour A., Cummins A., Barry S. (2010) Foxp3+ regulatory T cells, Th17 effector cells, and cytokine environment in inflammatory bowel disease. J. Clin. Immunol. 30, 80–89 [DOI] [PubMed] [Google Scholar]
- 5. Saruta M., Yu Q. T., Fleshner P. R., Mantel P. Y., Schmidt-Weber C. B., Banham A. H., Papadakis K. A. (2007) Characterization of FOXP3+CD4+ regulatory T cells in Crohn's disease. Clin. Immunol. 125, 281–290 [DOI] [PubMed] [Google Scholar]
- 6. Siakavellas S. I., Bamias G. (2012) Role of the IL-23/IL-17 axis in Crohn's disease. Discov. Med. 14, 253–262 [PubMed] [Google Scholar]
- 7. Kobayashi T., Okamoto S., Hisamatsu T., Kamada N., Chinen H., Saito R., Kitazume M. T., Nakazawa A., Sugita A., Koganei K., Isobe K., Hibi T. (2008) IL23 differentially regulates the Th1/Th17 balance in ulcerative colitis and Crohn's disease. Gut 57, 1682–1689 [DOI] [PubMed] [Google Scholar]
- 8. Olsen T., Rismo R., Cui G., Goll R., Christiansen I., Florholmen J. (2011) TH1 and TH17 interactions in untreated inflamed mucosa of inflammatory bowel disease, and their potential to mediate the inflammation. Cytokine 56, 633–640 [DOI] [PubMed] [Google Scholar]
- 9. Stockinger B., Veldhoen M. (2007) Differentiation and function of Th17 T cells. Curr. Opin. Immunol. 19, 281–286 [DOI] [PubMed] [Google Scholar]
- 10. O'Connor W., Jr., Zenewicz L. A., Flavell R. A. (2010) The dual nature of T(H)17 cells: shifting the focus to function. Nat. Immunol. 11, 471–476 [DOI] [PubMed] [Google Scholar]
- 11. Bedoya S. K., Lam B., Lau K., Larkin J., 3rd. (2013) Th17 cells in immunity and autoimmunity. Clin. Dev. Immunol. 2013, 986789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fujino S., Andoh A., Bamba S., Ogawa A., Hata K., Araki Y., Bamba T., Fujiyama Y. (2003) Increased expression of interleukin 17 in inflammatory bowel disease. Gut 52, 65–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kleinschek M. A., Boniface K., Sadekova S., Grein J., Murphy E. E., Turner S. P., Raskin L., Desai B., Faubion W. A., de Waal Malefyt R., Pierce R. H., McClanahan T., Kastelein R. A. (2009) Circulating and gut-resident human Th17 cells express CD161 and promote intestinal inflammation. J. Exp. Med. 206, 525–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu Z., Yadav P. K., Xu X., Su J., Chen C., Tang M., Lin H., Yu J., Qian J., Yang P. C., Wang X. (2011) The increased expression of IL-23 in inflammatory bowel disease promotes intraepithelial and lamina propria lymphocyte inflammatory responses and cytotoxicity. J. Leukoc. Biol. 89, 597–606 [DOI] [PubMed] [Google Scholar]
- 15. Tang Q., Bluestone J. A. (2008) The Foxp3+ regulatory T cell: a jack of all trades, master of regulation. Nat. Immunol. 9, 239–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bai A., Lu N., Guo Y., Liu Z., Chen J., Peng Z. (2009) All-trans retinoic acid down-regulates inflammatory responses by shifting the Treg/Th17 profile in human ulcerative and murine colitis. J. Leukoc. Biol. 86, 959–969 [DOI] [PubMed] [Google Scholar]
- 17. Huibregtse I. L., van Lent A. U., van Deventer S. J. (2007) Immunopathogenesis of IBD: insufficient suppressor function in the gut? Gut 56, 584–592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ueno A., Jijon H., Chan R., Ford K., Hirota C., Kaplan G. G., Beck P. L., Iacucci M., Fort Gasia M., Barkema H. W., Panaccione R., Ghosh S. (2013) Increased prevalence of circulating novel IL-17 secreting Foxp3 expressing CD4+ T cells and defective suppressive function of circulating Foxp3+ regulatory cells support plasticity between Th17 and regulatory T cells in inflammatory bowel disease patients. Inflamm. Bowel Dis. 19, 2522–2534 [DOI] [PubMed] [Google Scholar]
- 19. Li Z., Arijs I., De Hertogh G., Vermeire S., Noman M., Bullens D., Coorevits L., Sagaert X., Schuit F., Rutgeerts P., Ceuppens J. L., Van Assche G. (2010) Reciprocal changes of Foxp3 expression in blood and intestinal mucosa in IBD patients responding to infliximab. Inflamm. Bowel Dis. 16, 1299–1310 [DOI] [PubMed] [Google Scholar]
- 20. Ricciardelli I., Lindley K. J., Londei M., Quaratino S. (2008) Anti tumour necrosis-alpha therapy increases the number of FOXP3 regulatory T cells in children affected by Crohn's disease. Immunology 125, 178–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yu Q. T., Saruta M., Avanesyan A., Fleshner P. R., Banham A. H., Papadakis K. A. (2007) Expression and functional characterization of FOXP3+ CD4+ regulatory T cells in ulcerative colitis. Inflamm. Bowel Dis. 13, 191–199 [DOI] [PubMed] [Google Scholar]
- 22. Bettelli E., Carrier Y., Gao W., Korn T., Strom T. B., Oukka M., Weiner H. L., Kuchroo V. K. (2006) Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature 441, 235–238 [DOI] [PubMed] [Google Scholar]
- 23. Lee Y. K., Mukasa R., Hatton R. D., Weaver C. T. (2009) Developmental plasticity of Th17 and Treg cells. Curr. Opin. Immunol. 21, 274–280 [DOI] [PubMed] [Google Scholar]
- 24. Chen X., Oppenheim J. J. (2014) Th17 cells and Tregs: unlikely allies. J. Leukoc. Biol. 10.1189/jlb.1213633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Singh K., Gatzka M., Peters T., Borkner L., Hainzl A., Wang H., Sindrilaru A., Scharffetter-Kochanek K. (2013) Reduced CD18 levels drive regulatory T cell conversion into Th17 cells in the CD18hypo PL/J mouse model of psoriasis. J. Immunol. 190, 2544–2553 [DOI] [PubMed] [Google Scholar]
- 26. Xia Z. W., Zhong W. W., Meyrowitz J. S., Zhang Z. L. (2008) The role of heme oxygenase-1 in T cell-mediated immunity: the all encompassing enzyme. Curr. Pharm. Des 14, 454–464 [DOI] [PubMed] [Google Scholar]
- 27. Pae H. O., Lee Y. C., Chung H. T. (2008) Heme oxygenase-1 and carbon monoxide: emerging therapeutic targets in inflammation and allergy. Recent Pat. Inflamm. Allergy Drug Discov. 2, 159–165 [DOI] [PubMed] [Google Scholar]
- 28. Grochot-Przeczek A., Dulak J., Jozkowicz A. (2012) Haem oxygenase-1: non-canonical roles in physiology and pathology. Clin. Sci. 122, 93–103 [DOI] [PubMed] [Google Scholar]
- 29. Yoriki H., Naito Y., Takagi T., Mizusima K., Hirai Y., Harusato A., Yamada S., Tsuji T., Kugai M., Fukui A., Higashimura Y., Katada K., Kamada K., Uchiyama K., Handa O., Yagi N., Ichikawa H., Yosikawa T. (2013) Hemin ameliorates indomethacin-induced small intestinal injury in mice through the induction of heme oxygenase-1. J Gastroenterol. Hepatol. 28, 632–638 [DOI] [PubMed] [Google Scholar]
- 30. Hyvelin J. M., Maurel B., Uzbekov R., Motterlini R., Lermusiaux P. (2010) Hemin prevents in-stent stenosis in rat and rabbit models by inducing heme-oxygenase-1. J. Vasc. Surg. 51, 417–428 [DOI] [PubMed] [Google Scholar]
- 31. Hualin C., Wenli X., Dapeng L., Xijing L., Xiuhua P., Qingfeng P. (2012) The anti-inflammatory mechanism of heme oxygenase-1 induced by hemin in primary rat alveolar macrophages. Inflammation 35, 1087–1093 [DOI] [PubMed] [Google Scholar]
- 32. Almolki A., Guenegou A., Golda S., Boyer L., Benallaoua M., Amara N., Bachoual R., Martin C., Rannou F., Lanone S., Dulak J., Burgel P. R., El-Benna J., Leynaert B., Leynaert A. B., Aubier M., Boczkowski J. (2008) Heme oxygenase-1 prevents airway mucus hypersecretion induced by cigarette smoke in rodents and humans. Am. J. Pathol. 173, 981–992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chang T., Wu L., Wang R. (2008) Inhibition of vascular smooth muscle cell proliferation by chronic hemin treatment. Am. J. Physiol. Heart Circ. Physiol. 295, H999–H1007 [DOI] [PubMed] [Google Scholar]
- 34. Desbuards N., Rochefort G. Y., Schlecht D., Machet M. C., Halimi J. M., Eder V., Hyvelin J. M., Antier D. (2007) Heme oxygenase-1 inducer hemin prevents vascular thrombosis. Thromb. Haemost. 98, 614–620 [PubMed] [Google Scholar]
- 35. Wu J., Su W., Jin Y., Shi Y., Li C., Zhong W., Zhang X., Zhang Z., Xia Z. (2009) Targeted suppression of heme oxygenase-1 by small interference RNAs inhibits the production of bilirubin in neonatal rat with hyperbilirubinemia. BMC Mol. Biol. 10, 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Varga C., Laszlo F., Fritz P., Cavicchi M., Lamarque D., Horvath K., Posa A., Berko A., Whittle B. J. (2007) Modulation by heme and zinc protoporphyrin of colonic heme oxygenase-1 and experimental inflammatory bowel disease in the rat. Eur. J. Pharmacol. 561, 164–171 [DOI] [PubMed] [Google Scholar]
- 37. Sheikh S. Z., Hegazi R. A., Kobayashi T., Onyiah J. C., Russo S. M., Matsuoka K., Sepulveda A. R., Li F., Otterbein L. E., Plevy S. E. (2011) An anti-inflammatory role for carbon monoxide and heme oxygenase-1 in chronic Th2-mediated murine colitis. J. Immunol. 186, 5506–5513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Takagi T., Naito Y., Uchiyama K., Suzuki T., Hirata I., Mizushima K., Tsuboi H., Hayashi N., Handa O., Ishikawa T., Yagi N., Kokura S., Ichikawa H., Yoshikawa T. (2011) Carbon monoxide liberated from carbon monoxide-releasing molecule exerts an anti-inflammatory effect on dextran sulfate sodium-induced colitis in mice. Dig. Dis. Sci. 56, 1663–1671 [DOI] [PubMed] [Google Scholar]
- 39. Xia Z. W., Zhong W. W., Xu L. Q., Sun J. L., Shen Q. X., Wang J. G., Shao J., Li Y. Z., Yu S. C. (2006) Heme oxygenase-1-mediated CD4+CD25high regulatory T cells suppress allergic airway inflammation. J. Immunol. 177, 5936–5945 [DOI] [PubMed] [Google Scholar]
- 40. Xia Z. W., Xu L. Q., Zhong W. W., Wei J. J., Li N. L., Shao J., Li Y. Z., Yu S. C., Zhang Z. L. (2007) Heme oxygenase-1 attenuates ovalbumin-induced airway inflammation by up-regulation of foxp3 T-regulatory cells, interleukin-10, and membrane-bound transforming growth factor- 1. Am. J. Pathol. 171, 1904–1914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zhang Y., Zhang L., Wu J., Di C., Xia Z. (2013) Heme oxygenase-1 exerts a protective role in ovalbumin-induced neutrophilic airway inflammation by inhibiting Th17 cell-mediated immune response. J. Biol. Chem. 288, 34612–34626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bach F. H. (2002) Heme oxygenase-1 as a protective gene. Wien Klin. Wochenschr. 114, 1–3 [PubMed] [Google Scholar]
- 43. Waldner M. J., Neurath M. F. (2009) Chemically induced mouse models of colitis. Curr. Protoc. Pharmacol. 10.1002/0471141755.ph0555s46 [DOI] [PubMed] [Google Scholar]
- 44. Kim J. J., Shajib M. S., Manocha M. M., Khan W. I. (2012) Investigating intestinal inflammation in DSS-induced model of IBD. J. Vis. Exp. 10.3791/3678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Perše M., Cerar A. (2012) Dextran sodium sulphate colitis mouse model: traps and tricks. J. Biomed. Biotechnol. 2012, 718617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zhong W., Xia Z., Hinrichs D., Rosenbaum J. T., Wegmann K. W., Meyrowitz J., Zhang Z. (2010) Hemin exerts multiple protective mechanisms and attenuates dextran sulfate sodium-induced colitis. J. Pediatr. Gastroenterol. Nutr. 50, 132–139 [DOI] [PubMed] [Google Scholar]
- 47. Deban L., Correale C., Vetrano S., Malesci A., Danese S. (2008) Multiple pathogenic roles of microvasculature in inflammatory bowel disease: a Jack of all trades. Am. J. Pathol. 172, 1457–1466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wang W. P., Guo X., Koo M. W., Wong B. C., Lam S. K., Ye Y. N., Cho C. H. (2001) Protective role of heme oxygenase-1 on trinitrobenzene sulfonic acid-induced colitis in rats. Am. J. Physiol. Gastrointest. Liver Physiol. 281, G586–G594 [DOI] [PubMed] [Google Scholar]
- 49. Vijayan V., Mueller S., Baumgart-Vogt E., Immenschuh S. (2010) Heme oxygenase-1 as a therapeutic target in inflammatory disorders of the gastrointestinal tract. World J. Gastroenterol. 16, 3112–3119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Haines D. D., Lekli I., Teissier P., Bak I., Tosaki A. (2012) Role of haeme oxygenase-1 in resolution of oxidative stress-related pathologies: focus on cardiovascular, lung, neurological and kidney disorders. Acta Physiol. (Oxf) 10.1111/j.1748-1716.2011.02387.x [DOI] [PubMed] [Google Scholar]
- 51. Blancou P., Tardif V., Simon T., Rémy S., Carreño L., Kalergis A., Anegon I. (2011) Immunoregulatory properties of heme oxygenase-1. Methods Mol. Biol. 677, 247–268 [DOI] [PubMed] [Google Scholar]
- 52. Berberat P. O., A-Rahim Y. I., Yamashita K., Warny M. M., Csizmadia E., Robson S. C., Bach F. H. (2005) Heme oxygenase-1-generated biliverdin ameliorates experimental murine colitis. Inflamm. Bowel Dis. 11, 350–359 [DOI] [PubMed] [Google Scholar]
- 53. Hegazi R. A., Rao K. N., Mayle A., Sepulveda A. R., Otterbein L. E., Plevy S. E. (2005) Carbon monoxide ameliorates chronic murine colitis through a heme oxygenase 1-dependent pathway. J. Exp. Med. 202, 1703–1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Song X., Qian Y. (2013) The activation and regulation of IL-17 receptor mediated signaling. Cytokine 62, 175–182 [DOI] [PubMed] [Google Scholar]
- 55. Kimura A., Kishimoto T. (2010) IL-6: regulator of Treg/Th17 balance. Eur. J. Immunol. 40, 1830–1835 [DOI] [PubMed] [Google Scholar]
- 56. Abraham C., Cho J. (2009) Interleukin-23/Th17 pathways and inflammatory bowel disease. Inflamm. Bowel Dis. 15, 1090–1100 [DOI] [PubMed] [Google Scholar]
- 57. Toussirot E. (2012) The IL23/Th17 pathway as a therapeutic target in chronic inflammatory diseases. Inflamm Allergy Drug Targets 11, 159–168 [DOI] [PubMed] [Google Scholar]
- 58. Chora A. A., Fontoura P., Cunha A., Pais T. F., Cardoso S., Ho P. P., Lee L. Y., Sobel R. A., Steinman L., Soares M. P. (2007) Heme oxygenase-1 and carbon monoxide suppress autoimmune neuroinflammation. J. Clin. Invest. 117, 438–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Takeda Y., Takeno M., Iwasaki M., Kobayashi H., Kirino Y., Ueda A., Nagahama K., Aoki I., Ishigatsubo Y. (2004) Chemical induction of HO-1 suppresses lupus nephritis by reducing local iNOS expression and synthesis of anti-dsDNA antibody. Clin. Exp. Immunol. 138, 237–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kobayashi H., Takeno M., Saito T., Takeda Y., Kirino Y., Noyori K., Hayashi T., Ueda A., Ishigatsubo Y. (2006) Regulatory role of heme oxygenase 1 in inflammation of rheumatoid arthritis. Arthritis Rheum. 54, 1132–1142 [DOI] [PubMed] [Google Scholar]
- 61. Gomes-Santos A. C., Moreira T. G., Castro-Junior A. B., Horta B. C., Lemos L., Cruz D. N., Guimarães M. A., Cara D. C., McCafferty D. M., Faria A. M. (2012) New insights into the immunological changes in IL-10-deficient mice during the course of spontaneous inflammation in the gut mucosa. Clin. Dev. Immunol. 2012, 560817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Barada K. A., Mourad F. H., Sawah S. I., Khoury C., Safieh-Garabedian B., Nassar C. F., Tawil A., Jurjus A., Saadé N. E. (2007) Up-regulation of nerve growth factor and interleukin-10 in inflamed and non-inflamed intestinal segments in rats with experimental colitis. Cytokine 37, 236–245 [DOI] [PubMed] [Google Scholar]
- 63. Uhlig H. H., Coombes J., Mottet C., Izcue A., Thompson C., Fanger A., Tannapfel A., Fontenot J. D., Ramsdell F., Powrie F. (2006) Characterization of Foxp3+CD4+CD25+ and IL-10-secreting CD4+CD25+ T cells during cure of colitis. J. Immunol. 177, 5852–5860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Brusko T. M., Wasserfall C. H., Agarwal A., Kapturczak M. H., Atkinson M. A. (2005) An integral role for heme oxygenase-1 and carbon monoxide in maintaining peripheral tolerance by CD4+CD25+ regulatory T cells. J. Immunol. 174, 5181–5186 [DOI] [PubMed] [Google Scholar]
- 65. Pae H. O., Oh G. S., Choi B. M., Chae S. C., Chung H. T. (2003) Differential expressions of heme oxygenase-1 gene in CD25- and CD25+ subsets of human CD4+ T cells. Biochem. Biophys. Res. Commun. 306, 701–705 [DOI] [PubMed] [Google Scholar]
- 66. Choi B. M., Pae H. O., Jeong Y. R., Kim Y. M., Chung H. T. (2005) Critical role of heme oxygenase-1 in Foxp3-mediated immune suppression. Biochem. Biophys. Res. Commun. 327, 1066–1071 [DOI] [PubMed] [Google Scholar]
- 67. Korn T., Mitsdoerffer M., Croxford A. L., Awasthi A., Dardalhon V. A., Galileos G., Vollmar P., Stritesky G. L., Kaplan M. H., Waisman A., Kuchroo V. K., Oukka M. (2008) IL-6 controls Th17 immunity in vivo by inhibiting the conversion of conventional T cells into Foxp3+ regulatory T cells. Proc. Natl. Acad. Sci. U.S.A. 105, 18460–18465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Soares M. P., Marguti I., Cunha A., Larsen R. (2009) Immunoregulatory effects of HO-1: how does it work? Curr. Opin. Pharmacol. 9, 482–489 [DOI] [PubMed] [Google Scholar]
- 69. Pae H. O., Oh G. S., Choi B. M., Chae S. C., Kim Y. M., Chung K. R., Chung H. T. (2004) Carbon monoxide produced by heme oxygenase-1 suppresses T cell proliferation via inhibition of IL-2 production. J. Immunol. 172, 4744–4751 [DOI] [PubMed] [Google Scholar]
- 70. Quintana F. J., Basso A. S., Iglesias A. H., Korn T., Farez M. F., Bettelli E., Caccamo M., Oukka M., Weiner H. L. (2008) Control of T(reg) and T(H)17 cell differentiation by the aryl hydrocarbon receptor. Nature 453, 65–71 [DOI] [PubMed] [Google Scholar]