Abstract
Chronic debilitating pruritus is a cardinal feature of a topic dermatitis (AD). Little is known about the underlying mechanisms. Antihistamines lack efficacy in treating itch in AD, suggesting the existence of histamine-independent itch pathways in AD. Transient receptor potential ankyrin 1 (TRPA1) is essential in the signaling pathways that promote histamine-independent itch. In the present study, we tested the hypothesis that TRPA1-dependent neural pathways play a key role in chronic itch in AD using an IL-13 transgenic mouse model of AD. In these mice, IL-13 causes chronic AD characterized by intensive chronic itch associated with markedly enhanced growth of dermal neuropeptide-secreting afferent nerve fibers and enhanced expression of TRPA1 in dermal sensory nerve fibers, their dorsal root ganglia, and mast cells. Inhibition of TRPA1 with a specific antagonist in these mice selectively attenuated itch-evoked scratching. Genetic deletion of mast cells in these mice led to significantly diminished itch-scratching behaviors and reduced TRPA1 expression in dermal neuropeptide containing afferents in the AD skin. Interestingly, IL-13 strongly stimulates TRPA1 expression, which is functional in calcium mobilization in mast cells. In accordance with these observations in the AD mice, TRPA1 expression was highly enhanced in the dermal afferent nerves, mast cells, and the epidermis in the lesional skin biopsies from patients with AD, but not in the skin from normal subjects. These studies demonstrate a novel neural mechanism underlying chronic itch in AD and highlight the complex interactions among TRPA1+ dermal afferent nerves and TRPA1+ mast cells in a Th2-dominated inflammatory environment.
Introduction
AD is characterized by acute flare-ups and chronic eczematous skin lesions associated with refractory chronic itch. The pathophysiology of chronic itch (pruritoceptive) in AD is diverse and involves a complex network of cutaneous and neuronal cells and mediators. Antihistamines are often ineffective in treating chronic itch in AD, pointing to the existence of distinct pruritogens and histamine-independent itch pathways (1, 2). This lack of understanding of the mechanisms underlying itch in AD represents a serious unmet medical need. Little is known about how dermal itch sensory nerves interact with dermal immune cells and keratinocytes in the initiation or aggravation of itch.
Itch is broadly characterized as either histamine-dependent or -independent, both of which are relayed by subsets of dermal itch-sensitive C fiber-type nerves. Recent studies on the novel cation channel, the transient receptor potential ankyrin 1 (TRPA1) channel, have shown that TRPA1 functions in cells as a sensor for pain sensation, thermal sensitivity and neurogenic inflammation. The most recent study shows in a chemical-induced mouse model of itch that TRPA1 is an essential component of the signaling pathways that promote Mrgpr-dependent and histamine-independent itch (3). TRPA1 is activated by a series of by-products of oxidative/nitrative stress, produced under inflammatory conditions or in tissue damage, thus generating neurogenic inflammatory responses (4, 5). In addition, TRPA1 is activated downstream of G protein–coupled receptors (GPCRs), including the pro-algesicbradykin in receptor (6, 7). Histamine, serotonin, chloroquine and BAM8-22 all evoke itch by acting on GPCRs (8–10). TRPA1 is the primary transduction channel mediating non-histamine and endogenous pruritogen evoked signaling and itch-scratching behaviors (3). Thus, TRPA1 could be a candidate downstream transduction channel onto which multiple histamine-independent itch pathways converge. Little is known about the mechanisms underlying non-histaminergic itch in chronic inflammatory pruritic skin disease such as AD. Particularly, the role of TRPA1 in the pruritogenesis in AD has not been studied, despite the fact that the majority of chronic itch, such as that seen in AD, is mediated by non histaminergic mechanisms (1, 11,12).
Interleukin-13 (IL-13), a Th2 cytokine, is a critical mediator of human allergic disorders including asthma (13–15) and a topic dermatitis (16–20). We and others have shown that IL-13 plays a critical role in experimental models of asthma, allergic rhinitis (AR) and a topic dermatitis (AD) (21–29). IL-13 recently has been implicated in nerve repair in a transected rat spinal cord model (30). However, the role of IL-13 in pruritogenesis of AD has not been defined.
Mast cell–neuronal interactions are important in pruritic conditions (31, 32). Mast cells interact with neuronal cells through pruritogenic mediators such as tryptase, histamine, IL-31, neurotrophins and neuropeptides, including vasoactive intestinal peptide (VIP), calcitonin gene-related peptide (CGRP), substance P (SP) and endothelin-1, adding novel regulatory pathways for the modulation of itch (33–35). Mast cell-derived TNF can promote nerve fiber elongation in the skin during contact hypersensitivity in mice (31). Many of the mast cell mediators are involved in the elicitation of itch. Thus, mast cells are important in the cellular network of itch. Questions about how mast cells regulate the expression of TRPA1 and what role of mast cell related TRPA1 plays in itch in AD remain unanswered.
We hypothesized that chronic pruritus in IL-13 induced AD is mediated via a TRPA1 dependent neuronal inflammatory pathway. To test this hypothesis, we first characterized the expression of TRPA1 in the lesional skin from IL-13-induced AD and from patients with AD. We defined the relationships among the expression of TRPA1 in lesional AD skin correlating with itch–evoked scratching behavior, growth of dermal afferent sensory nerves and the severity of AD in transgenic mice in which skin-targeted IL-13 causes chronic pruritic AD and demonstrated that blockage of TRPA1 with a specific inhibitor significantly attenuated the itch in mice with AD and diminished TRPA1 in dermal afferent nerves and dermal cells in mast cell deficient AD mice. However, specific blockage of histamine receptor 1 did not. These studies demonstrated that IL-13 induces chronic pruritus via a novel TRPA1-dependent and histamine-independent pathway and that expression of TRPA1 in AD skin (dermal sensory nerves, mast cells and epidermis) is critical for the initiation and sustaining of chronic itch in AD.
Materials and Methods
Animals
The generation of K5-tTA-Tight-IL-13 mouse models of AD, the genotyping of these mice, and the activation of the IL-13 transgene were accomplished as we previously described (25, 27). Mast cell deficient IL-13 Tg mice were generated by crossbreeding c-Kit deficient KitW-sh/W-sh mice (The Jackson Laboratory, Bar Harbor, ME) on C57BL/6 genetic background with K5-tTA mice and TRE-Tight-IL-13 mice. K5-tTA-IL-13 Tg(+) mice carrying null mutation of c-Kit (Tg(+)/KitW-sh/W-sh) and K5-tTA-IL-13 Tg(+) mice carrying wild type c-Kit (Tg(+)/c-Kit+/+) were compared in the experiments. Skin mast cells in KitW-sh/W-sh mice usually disappear by the age of 13 weeks (36). To ensure that skin mast cells were absent in KitW-sh/W-sh mice, the activation of IL-13 transgene in the skin was initiated at the age of 15 weeks by withdrawing doxycycline from drinking water. Using Toluidine blue staining, mast cells were almost absent (one mast cell per ten HPFs) (Supplemental Figure 1). In all experiments, Tg(−) littermate controls received the same amount of Dox or no Dox for the same length of time. For the reversibility experiments, after development of AD, the Tg(+) mice were randomly assigned to receive Dox water to turn off the IL-13 transgene in vivo (the transgene On-Off group) or to receive normal drinking water to keep the IL-13 transgene on (the transgene On-On group). Both non lesional skin samples and lesional AD score-matched, anatomical site-matched skin samples were used in the reversibility experiments (Figure 5) and disease-kinetic experiments (Figure 1f, 1g, 1h, and 1i). Lesional AD skin samples were used for the rest of the experiments. Two differentTRPA1 deficient mouse strains were obtained. One strain was from Dr. David Julius (UCSF, Source A) and the other was purchased from the Jackson laboratory. Eight to 12 week-old mice were used for the experiments. The procedures involving animals in the present study were approved by the Institutional Animal Care and Use Committee of the Johns Hopkins University and Yale University.
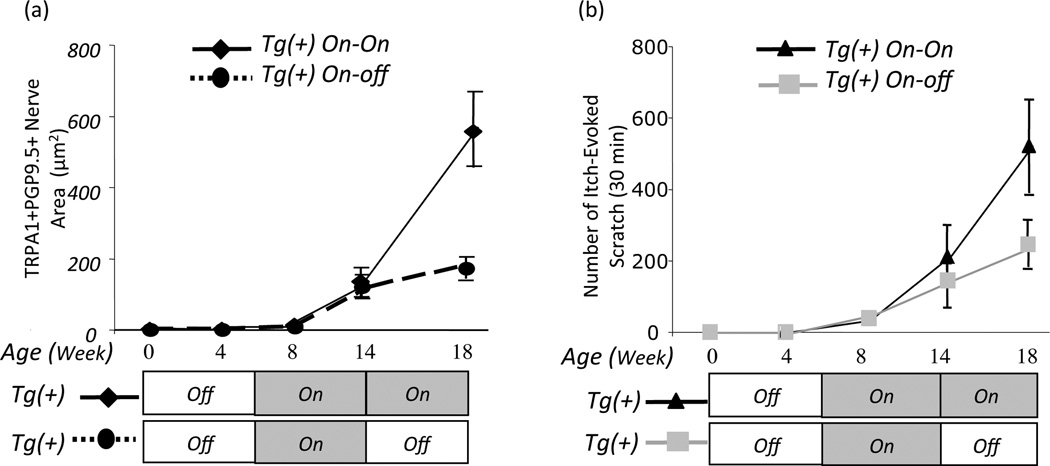
Figure 5. Inactivation of the IL-13 transgene in Tg(+) mice with AD over time led to diminished TRPA1 in lesional AD skin associated with diminished itch-induced scratching.
After withdrawal of Dox in the drinking water (the transgene was turned on) for 8 weeks, IL-13 was induced and Tg(+) mice began to develop AD (clinical score, 2). These mice were then randomly assigned to receive either Dox to inactivate the IL-13 transgene (IL-13 Tg(+) On-Off group) or normal water to keep the transgene on (IL-13 Tg(+) On-On group). Mice were sacrificed, and skin samples were obtained at the age of 18 weeks. (a) Significantly attenuated TRPA1+/PGP9.5+ afferent nerves in AD skin after the IL-13 transgene was turned off in the Tg(+) On-Off group (dotted line) compared to On-On group (solid line) in which the disease continued to worsen. (b) The number of itch-evoked scratching behaviors was diminished in Tg(+) On-Off group (gray line) compared to the Tg(+) On-On group (black line), (n=5 for each group).
Figure 1. Itch-evoked scratching correlates with the amount of cutaneous sensory afferent nerves, the number of dermal mast cells, and the severity of the disease in chronic AD of K5-tTA-IL-13 mice.
(a) Histology (H&E) of skin samples (20×), and (b) Fluorescent IHC staining with rabbit anti-PGP9.5 IgG (PGP9.5, Green), rabbit anti-CGRP IgG (CGRP, Green), DAPI (Nuclei, Blue), or control IgG (rabbit IgG) in Tg(−) or Tg(+) skin from the neck of mice with chronic AD. (c) Quantification of changes in dermal PGP9.5+ nerves (left) and CGRP+ nerves (right).(d) IHC with rabbit anti-c-Kit (c-Kit, White arrows) for mast cells. (e) Quantification of c-Kit+ mast cells per HPF in the skin (10 fields per skin sample per mouse; n=4–5 each group). Correlation of itch-evoked scratching with the dermal nerve growth CGRP+(f), PGP9.5+(g), c-Kit+ mast cells(h) and the severity of AD (i). In (a, b, and d), the lesional AD samples from the neck of Tg(+) mice were used and the data are pooled from three independent experiments, which gave similar results (Tg(−): n=4; Tg(+): n=5). In (c) and (e), ***P<0.001 versus values from Tg(−) skin. Original magnifications were 20× for(a), 40× for (b) and (d).
Histological analysis
Skin tissues from the same anatomical locations from each experimental group of mice were obtained and fixed with Shandon Glyo-Fixx (Thermo Fisher Scientific), embedded in paraffin, and stained with Toluidine blue (Sigma-Aldrich) to identify mast cells.
Clinical scores
After withdrawal of Dox from the drinking water to turn on the IL-13 transgene, Tg(+) mice were examined for skin lesions three times a week, and the clinical scores for disease severity were recorded as described previously with slight modifications (25, 37).
Itch evoked scratch
As an indicator of pruritus, the scratching behavior of mice was determined as described (25, 38). The spontaneous itching behavior of the mice was videotaped 30 minutes each time, and counted for hind limb and facial scratching as described previously with slight modification. The number of scratches was quantified by counting facial wiping and lifting of the hind limb directed towards the dermatitis area, regardless of the number of strokes (25, 38).
Fluorescent immunohistochemistry (IHC)
Mouse skin tissues were fixed with Shandon Glyo-Fixx (Thermo Fisher Scientific), embedded in paraffin, and sectioned at 4-µm thickness. The spinal column was opened and six to eight neck and/or thoracic dorsal root ganglia (DRG) along the whole vertebral column per mouse were dissected. The DRG were collected, cryoprotected in 20% sucrose, frozen in Tissu-Tek O.C.T. (Sakura Finetek), cryosectioned and mounted on slides. Fluorescent IHC was performed on deparaffinized mouse skin slides and on acetone-fixed frozen DRG sections. The slides were blocked with 10% donkey serum blocking solution (Sigma-Aldrich) for 1 hour. After washing, tissue sections were incubated at 4°C overnight wit h goat-anti-PGP9.5 (sc-23852, Santa Cruz Biotechnology), goat-anti-GRPR (sc-26836, Santa Cruz), rabbit-anti-CGRP (PC205L, Calbiochem), rabbit-anti-TRPA1 (NB110-40763, Novus Biologicals), rat-anti-CD3 (555273, BD bioscience), goat-anti-Langerin (sc-22620, Santa Cruz Biotechnology, Inc. Santa Cruz, CA), rat-anti-c-Kit (14-1172-81, eBioscience, Inc., San Diego, CA), rat-anti-F4/80 (14-4821-82, eBioscience), rat-anti-major basic protein (MBP) (a kind gift from Drs. Nancy and James J. Lee, Mayo Clinic, Scottsdale, AZ), and goat-anti-mast cell tryptase (MMCP6) (sc-32474, Santa Cruz Biotechnology).After rinsing, tissue sections were incubated with secondary antibodies, Alexa Fluor 488 or 594-conjugated donkey anti-rat IgG, Alexa Fluor 488 or 594-conjugated donkey anti-goat IgG, and/or Alexa Fluor 488 conjugated donkey anti-rabbit IgG (Invitrogen, Carlsbad, CA). Cell nuclei were detected by incubating the tissue sections with DAPI for 10 minutes. After washing, tissue sections were mounted using PermaFluor (Thermo-Fisher Scientific, Pittsburgh, PA) and examined using a fluorescence microscope.
Quantification of afferent nerves in the skin
The slides were evaluated using micrographs taken with a fluorescent microscope (Olympus BX-5; Olympus America, Inc, Center Valley, PA) equipped with a camera (Q-Imaging RetigaExi; Biovision Technologies, Inc, Exton, PA); a micrograph field of view of the entire stained section was taken. Imaging software (iVision; Biovision Technologies) was used to analyze areas of positive staining in each digitized micrograph where simple bi-level thresholding was performed. The total area of the dermal nerve are a was outlined by the observer and measured by the software. The software measurement of the positively stained nerve area within the dermal area was calculated as the percentage of the dermal area (positive nerve area divided by dermal area).
TRPA1 blockage and histamine blockage
The role of TRPA1 in AD was assessed by intraperitoneal (i.p.) administration of a selective TRPA1 antagonist, HC-030031 (100 mg/kg; Sigma-Aldrich, 100 mM HC-030031 stock in DMSO and 0.2% Tween 80 in saline) or vehicle control to AD mice (5 mice per group). The itch-scratching behavior was video recorded for 30 minutes before and for1 hour after the TRPA1 inhibitor injection. Scratching numbers were counted as above. Histamine receptors, H1, H3 and H4 are expressed in the skin and H1 and H4 appear to be key components in the induction of itch, whereas H3 is an inhibitory receptor of itch induction. The H1 receptor is reported to account for more than 95% of the histamine receptors in the skin (38). Specific H1 receptor antagonist Cetirizine (Pfizer, USA) 15 mg/kg and vehicle (PBS) were administered i.p. to IL-13 Tg(+) mice with AD. The itching behavior was recorded for 30 minute before injection. Immediately after administration of Cetirizine or vehicle control, scratching behavior was videotaped for 30 minutes (4 mice per group).
Measurement of cytokines in the skin
Protein samples were prepared as described previously (25). Briefly, frozen skin tissues were placed in liquid nitrogen, pulverized with a chilled mortar and pestle into powders and weighted. The skin protein was extracted by adding PBS with 0.25% Triton X-100 and stirring at 4°C overnight. Debris was removed by centrifugation at 3000×g for 15 minutes. Supernatants were stored in small aliquots at −80°C until assayed. Al l samples were normalized to weight. The expression of IL-13, IL-4, IFN-γ in the skin samples were measured using ELISA kits according to the manufacturer’s instruction (R&D Systems).
Bone marrow derived mast cell (BMMC) culture and flow cytometry
BMMC were obtained by in vitro differentiation of bone marrow cells obtained from femur and tibia of WT mice cultured in RPMI 1640 media (Invitrogen)containing 5 ng/mL of IL-3 (Peprotech, Rocky Hill, NJ) supplemented with 10% heat-inactivated FBS (Invitrogen), 100 µM 2-ME (Sigma-Aldrich, St. Louis, MO), 10 µM MEM nonessential amino acids solution, L-glutamine, sodium pyruvate, HEPES buffer (Sigma-Aldrich), and antibiotics. By 4 weeks in culture, the purity of BMMC was >98% as determined by positive Toluidine blue staining and FACS staining ofFcεRI and c-Kit (39). Mature BMMC between 5 and6 weeks in culture, with viability >95% by the trypan blue exclusion assay, were used for experiments. Cells were starved with 0.2% heat-inactivated FBS overnight and then incubated with IL-4 (10 ng/mL), IL-13 (10 ng/mL), IFN-γ (10 ng/mL), or H2O2 (10 nM) for 24 hours. Stimulated BMMC were harvested and stained for TRPA1 using rabbit anti-TRPA1 antibody and Alexa Flour 488 donkey anti-rabbit IgG (H+L) antibody, and analyzed by fluorescent IHC and flow cytometry.
Functional imaging of intracellular calcium mobilization
The effect of TPRA1 agonist in intracellular calcium mobilization was studied in murine mast cell line (C57.1). Cultured C57.1 cells were harvest, suspended at 107 cells/ml in complete medium, incubated with 3.5mM Calcium Sensor Dye eFluor® 514 (eBioscience, San Diego, CA) for 30 minutes at 37°C in the dark, and washed and analyze d by flow cytometry as unstimulated. After measuring basal level for 1 minute, cells were removed and TRPA1 agonist (100 µM, allylisothiocyanate, Sigma-Aldrich) was added for 30 minutes and analyzed by flow cytometry. The maximum intracellular calcium mobilization in cells exposed to treatment was measured, and histogram overlays are displayed as percentage of Max.
Human skin biopsy samples
De-identified skin biopsy samples from AD patients and normal subjects were described previously (40). After explanation of the nature of research and obtaining informed consent from patients, 3–5 mm punch biopsies were taken from the forearms of normal healthy individuals (n = 4) and from lesional or non lesional skin of AD patients (n = 3). Skin samples were immediately frozen in liquid nitrogen and stored at −80°C until analysis. The study was approved by the local ethics committee. Cryosectioned human skin samples were analyzed with immunofluorescence staining as above. Acetone-fixed frozen sections were blocked with 10% donkey serum (Sigma-Aldrich) for 1 hour, and incubated with goat-anti-PGP9.5 (sc-23852, Santa Cruz), rabbit-anti-TRPA1 (NB110-40763, Novus Biologicals, Littleton, CO) or mouse-anti-human mast cell tryptase (Chemic on International-Millipore, Billerica, MA) at 4°C overnight. The slides were rinsed and incubated with Alexa Fluor 594-conjugated donkey anti-goat IgG, Alexa Fluor 488 conjugated donkey anti-rabbit IgG and/or Alexa Fluor 594-conjugated donkey anti-mouse IgG (Invitrogen). Cell nuclei were stained with DAPI for 10 minutes. Images were obtained using a fluorescence microscope.
Statistical analysis of the data
Student’s t-test (two-tailed) or, for analysis of groups of data that were not normally distributed, Mann-Whitney U-test (two-tailed), was used for statistical evaluation of the results. Differences between samples in comparison with p < 0.05 were considered significant. Unless otherwise specified, all data are presented as Mean±SEM.
Supplemental materials
The changes in mast cells in the skin of KitW-sh/W-sh mice, TRPV1 expression in the skin, and the cytokine profiles in the skin of WT and IL-13 Tg(+) mice with or without c-Kit mutation, and TRPA1 expression in the wild type, IL-13 Tg(+) and TRPA1 deficient mice from two different sources are shown in the supplemental figures.
Results
Itch in IL-13-induced chronic AD correlated with the growth of calcitonin gene-related peptide (CGRP+), protein gene product (PGP9.5) afferent nerve, the number of cutaneous mast cells and the severity of AD
We previously demonstrated that transgenic expression of IL-13 causes chronic itch and AD in mice (25). To begin to understand the mechanisms in the pathogenesis of itch, fluorescent IHC of PGP9.5 and CGRP with anti-PGP9.5 antibody and anti-CGRP antibody was performed to determine whether IL-13 induces dermal afferent nerve growth. Lesional AD skin samples from the neck of Tg(+) mice shown in Figure 1a, 1b and 1d were taken after a 14-week induction of the IL-13 transgene. As we showed previously (25), remarkable inflammatory infiltrates were present in the epidermis and dermis of IL-13 Tg(+) mice as compared to normal skin of Tg(−) mice (Figure1a), and strikingly high amounts of both PGP9.5 and CGRP-immunore active nerves were shown in the epidermis ramifying into the dermis with variable staining intensity in IL-13 Tg(+) mice as compared to the scarce presence of these markers in the skin of Tg(−) mice (Figure 1b, 1c). These responses were associated with significantly increased c-Kit+ mast cells (White arrows) in the Tg(+) AD skin (Figure 1d, 1e). It is remarkable that itch-evoked scratching behavior in Tg(+) mice with AD correlated with the amount of both dermal CGRP+ (Figure 1f) and PGP9.5+ sensory C fibers (Figure 1g), with increased dermal c-Kit+ mast cells (Figure 1h), and with the severity of clinical AD (Figure 1i). These findings suggest potential roles for the PGP9.5 and CGRP dermal afferent nerves and mast cells in mediating itch in IL-13-induced AD.
Enhanced expression of TRPA1 in PGP9.5+ and CGPR+ dermal afferents, in dorsal root ganglia (DRG) and in mast cells in IL-13-induced AD skin
Although a role of TRPA1 has recently been implicated in chemical-induced acute itch, its role in chronic itch in AD has not been demonstrated. To understand the potential role of TRPA1 in neural pathogenesis of itch in AD, fluorescent IHC was first used to ascertain whether TRPA1 was expressed in lesional AD skin of Tg(+) mice as compared to that of Tg(−) mice. The expression of TRPA1 was markedly enhanced in the epidermal and dermal regions (Figure 2a) and in the CGRP+ and PGP9.5+ afferents of lesional skin of Tg(+) mice, and conversely, the expression of TRPA1 was almost absent in the skin of Tg(−) mice (Figure 2b,c). To characterize cutaneous cell types that expressed TRPA1, fluorescent IHC with cellular markers (MBP-eosinophils), (Langerins-Langerhans cells), (F4/80-macrophages), (CD3-T cells) and (c-Kitor mast cell-specific tryptase (MMCP6)-mast cells) for co-expression of TRPA1; the amount of co-expression of TRPA1+/c-Kit+was significantly higher in AD skin of Tg(+) mice compared to Tg(−) skin (Figure 2d). However, TRPA1 was minimally expressed or absent in eosinophils, Langerhans cells, macrophages, or T cells (Table 1), suggesting that TRPA1 expression may be mast cell-specific. The number of dual TRPA1+, c-Kit+ mast cells correlates with the number of itch-evoked scratch behaviors (Figure 2e). Moreover, the mast cell-specific tryptase MMCP6+ and/or c-Kit+cells were in close proximity to dermal PGP9.5 and CGRP+ nerve fibers (Figure 2f and data not shown), suggesting that mast cell–neuronal interactions may be important in itch in chronic AD. Interestingly, the vanilloid, TRPV1,co-localizing with the TRPA1 and important in histamine-induced itch, was not increased in the AD skin of Tg(+) mice (Supplemental Figure2).
Figure 2. Enhanced expression of TRPA1 in the AD skin from K5-tTA-IL-13 mice.
(a) Expression of TRPA1 in the epidermis and dermis of the lesional AD skin of the neck (arrows to the epidermis) was determined by fluorescent IHC with rabbit monoclonal anti-TRPA1 (TRPA1− Green, DAPI for nuclei-Blue) (10×). (b) Increased co-localization of TRPA1+ (Green)/CGRP+ afferent nerves (Red) in the AD skin, particularly in the dermis (40×), and (c) Quantification of TRPA1+/CGRP+ sensory nerves. (d) Enhanced co-expression of the dermal TRPA1+(Green)on c-Kit+(Red)mast cells in the AD skin (100×), and (e) increased TRPA1+/c-Kit+ mast cells correlated with itch-evoked scratching. (f) MMCP6+ mast cells (Red) by fluorescent IHC with rabbit polyclonal anti-MMCP6 are in close proximity to CGRP+ afferents (Green), DAPI (Blue for nuclei) in the dermal area of Tg(+) AD skin (100×). (g) Fluorescent IHC for TRPA1 of cryo-sections of cervical sensory DRG isolated from Tg(−) and Tg(+) mice showing markedly augmented expression of TRPA1 (Green) (DAPI for nuclei, Blue) in the sensory neurons, (10×). (g) Photos are representatives of DRG were from individual mice. Tg(−) and Tg(+) mice: n=5 for each group. (c) and (h) Data were pooled from three independent experiments with similar results (Tg(−) mice: n=5 and Tg(+) mice: n=8). (c) and (h), ***P<0.001 vs. corresponding values of Tg(−) skin. (a), (b), (d), (f) and (g), results shown are from one of 3 experiments with identical findings.
Table 1.
Enhanced Expression of TRPA1 in c-Kit+ Mast Cells in AD
| Skin Cells/TRPA1+ (HPF) |
Tg(−) (Mean±SEM) |
Tg(+) (Mean±SEM) |
P value |
|---|---|---|---|
| CD3+/TRPA1+ | 3.4 ± 0.21/0 | 14.5 ± 2.1/0 | ns |
| MBP+/TRPA1+ | 0.5 ± 0.03/0 | 9.4 ± 1.3/0 | ns |
| Langerin+/TRPA1+ | 3.7 ± 1.45/0 | 7.8 ± 0.99/0 | ns |
| F4/80+/TRPA1+ | 5.4 ± 2.1/0 | 12 ±1.1/0 | ns |
| c-Kit+/TRPA1+ | 10 ± 1.77/1.6 ± 0.4 | 37 ±3.9/36 ± 4.1 | 0.0012 |
Note: Skin samples from Tg(−) and IL-13 Tg(+) mice were fluorescent IHC stained for TRPA1 and with specific antibodies to CD3 (T cells), MBP (eosinophils), F4/80 (activated macrophages), Langer in (Langerhans cells), and c-Kit (mast cells). The data are pooled from 2 independent experiments with similar findings. (3 slides from each animal were stained. Eight to 10 HPFs per slide were blindly counted (Tg(−) mice: n=4 and Tg(+): n=6).
TRPA1 is expressed in a subpopulation of DRG neurons-the cell bodies of cutaneous sensory neurons and acts as a sensory receptor for oxidative mediators, hydrogen peroxide, produced endogenously during oxidative stress (5). However, TRPA1 expression in DRG neurons in chronic inflammatory skin diseases such as AD has not been well defined. We assessed the expression of TRPA1 in cervical DRG by IHC. TRPA1 expression was significantly increased in about 35–40% of DRG from Tg(+) mice with AD as compared to 8.5% in Tg(−) mice (Figure 2g, 2h). These studies show that IL-13 is a potent stimulator of TRPA1expression in dermal afferents, mast cells of AD skin and in the DRG neurons.
To assess the specificity of TRPA1 antibody using fluorescent IHC, skin samples from the neck of two different strains of TRPA1 deficient mice (see the method) were collected and compared to skin samples of Tg(−)mice. As shown in Supplemental Figure 4, increased TRPA+ dermal cells were seen in AD skin of Tg(+) animals compared to much fewer TRPA1+ cells in the dermis of wild type mice. In contrast, skin samples from TRPA1 KO mice of both sources failed to show any TRPA1+ cells.
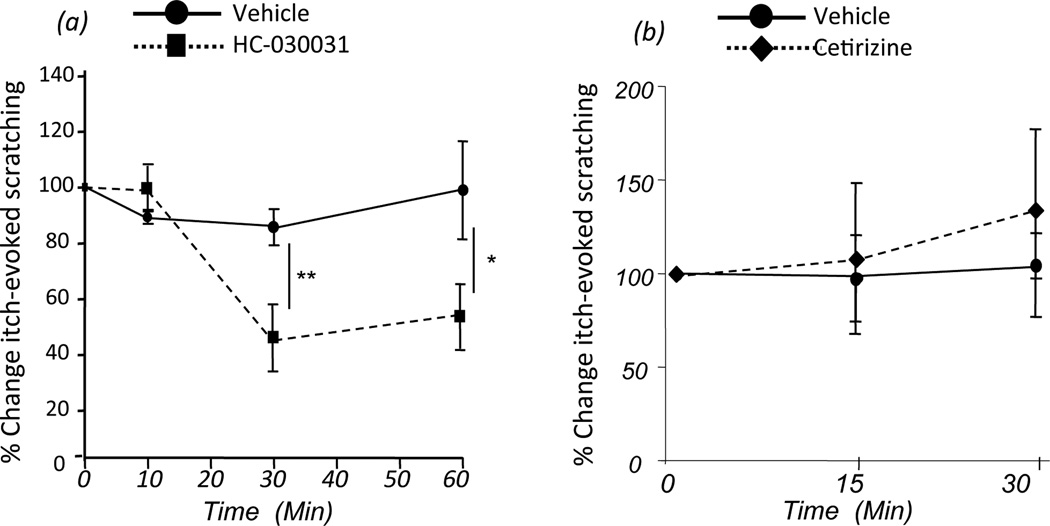
Blockade of TRPA1 attenuated itch-evoked scratching in AD
To investigate the function of TRPA1 in itch in AD, age- and AD clinic score-matched Tg(+) mice were randomly assigned to receive either a TRPA1-specific antagonist (HC-030031, 100 mg/kg, i.p.) or vehicle control. Behavior of itch-evoked scratching was video-recorded and counted blind to the treatment. The number of itch-evoked scratches was significantly attenuated starting3 minutes after administration of HC-030031 and the inhibitory effect lasted for 1 hour compared to unaltered itch-scratching in mice given vehicle control (Figure 3a). Conversely, behaviors of itch-scratching in Tg(+) mice that were administered (i.p.)a specific histamine receptor 1 antagonist (Cetirizine, 15 mg/kg) were not significantly altered compared to mice received control vehicle (PBS) (Figure 3b). These findings showed that TRPA1 antagonist specifically blocked itch-scratching, whereas histamine receptor 1 antagonist failed to do so, indicating that TRPA1 has a role in the pruritogenesis in AD, which is mediated through a histamine-independent pathway and, at least in part, a TRPA1-dependent pathway.
Figure 3. Blockade of TRPA1 attenuated itch-evoked scratching.
Age- and AD score-matched IL-13 Tg(+) mice were administered with TRPA1 specific antagonist HC-030031 (100 mg/kg, i.p., one dose) or vehicle control. Itch-evoked scratching activities were video recorded, counted, and compared between the two groups. (a) HC-030031 significantly inhibited itch-scratching behaviors in Tg(+) mice with AD. (b) Histamine receptor blocker (Cetirizine, 15 mg/kg, i.p.) failed to reduce itch-induced scratching. (a) and (b) Data were pooled from 2 independent experiments with similar results. (*p<0.05; **p<0.01; n=5 for each group).
Mast cells are essential for itch and expression of TRPA1 in dermal afferent nerves and DRG
Dermal afferents can both be affected by and contribute to inflammatory responses including those in the skin (41, 42) and the respiratory tract (32). As noted above (Figure 2), mast cells in AD lesions highly expressed TRPA1 and were in close vicinity to TRPA1+ nerve fibers, suggesting a functional role of mast cells in AD. To ascertain the role of mast cells in itch and in regulation of TRPA1 in AD, we generated mast cell-deficient IL-13 Tg mice by crossing IL-13 Tg mice with mast cell-deficient KitW-sh/W-sh mice (both on C57BL/6 genetic background). As previously reported (36), in KitW-sh/W-sh mice, few cutaneous mast cells were detected in the skin at the age of 12 weeks old. To ensure all cutaneous mast cells were absent in KitW-sh/W-sh mice, the IL-13 transgene was not activated in IL-13 Tg(+) mice with wild type c-Kit (Tg(+)/c-Kit+/+) or mutantKitW-sh/W-sh (Tg(+)/KitW-sh/W-sh) until the mice reached the age of 16 weeks when mast cells in c-Kit mutant skin were undetectable (Supplemental Figure 1). Compared to Tg(+)/c-Kit+/+ mice that developed AD, Tg(+)/KitW-sh/W-sh mice exhibited a very slow-onset disease and only 20% of the mice developed AD (Figure 4a, 4b). Tg(+)/KitW-sh/W-sh mice displayed much milder dermatitis associated with significantly fewer itch-scratching (Figure 4c). Furthermore, TRPA1+ cells in lesional AD skin of Tg(+)/KitW-sh/W-sh mice were barely seen (Figure 4d, 4f) and the expression of TRPA1 in the CGPR+ dermal afferent nerves was significantly diminished (Figure 4e, 4g). Consistently, the expression of TRPA1 in the cervical neurons of the dorsal root ganglia of Tg(+)/KitW-sh/W-sh mice was markedly reduced compared to Tg(+)/c-Kit+/+ mice (Figure 4h, 4i). These findings suggest that mast cells are important for the expression of TRPA1 on the dermal CGRP+ afferents and for the induction of itch in AD. Importantly, the level of IL-13 in the skin samples from Tg(+) mice was not significantly altered in mast cell deficient IL-13 Tg(+) mice (Supplemental Figure 3a), indicating that genetic deletion of mast cells in Tg(+) mice did not inhibit the IL-13 transgene expression.
Figure 4. Role of mast cells in itch-evoked scratching and TRPA1 expression in the epidermis, dermal cells and dermal sensory afferents and sensory neurons.
(a, b) Mast cell-deficient IL-13 Tg(+) mice exhibited slow onset, low incidence, and less severe AD and(c) markedly reduced itch-evoked scratching. Skin samples from upper portion of the back and sensory neurons from DRG collected from cervical region of IL-13 Tg(+) mice on c-Kit+/+ and KitW-sh/W-sh genetic background were fluorescent IHC stained for TRPA1 (Green), neuropeptide-releasing nerves-CGRP (Red), and DAPI (Blue for nuclei). (d) Attenuation and (f) Quantification of TRPA1 in the epidermis and dermis (20×). (e) Diminished dermal co-expression of TRPA1+/CGRP+ afferent sensory nerves (40×). (h, i) Harvested cervical ganglia (6–8 ganglia/mouse) from Tg(−)/c-Kit+/+, Tg(−)/KitW-sh/W-sh, Tg(+)/c-Kit+/+ and Tg(+)/KitW-sh/W-sh mice were stained for TRPA1 (Green), showing reduction of TRPA1 expression in the sensory neurons of DRG from Tg(+)/KitW-sh/W-sh mice as compared to Tg(+)/c-Kit+/+ mice (10×). Tg(+)/c-Kit+/+ mice: n=5, Tg(+)/KitW-sh/W-sh mice: n=5, Tg(−) groups n=4 for each. In (a), (b), and (c) Data are pooled from 5 independent experiments with similar results. Tg(−) mice: n=12 and Tg(+) mice: n=18. In (d), (e), and (h)Each is a representative of 3 independent experiments. Tg(+)/c-Kit+/+ mice: n=8 and Tg(+)/KitW-sh/W-sh mice: n=9. In (f), (g), and (i) Data are pooled from 3 experiments, n=4–7 for each group. (*p<0.05; **p<0.01; ***p<0.001).
Inactivation of IL-13 in vivo led to diminished growth of TRPA1+/PGP9.5+ afferent nerves
We then evaluated whether IL-13–up-regulated expression of TRPA1 in AD could be reversed after the IL-13 transgene was turned off in vivo. IL-13 Tg(+) mice with AD were randomly assigned to receive either Dox water to inhibit the IL-13 transgene (IL-13 Tg(+) On-Off group) or normal water to keep the transgene on (IL-13 Tg(+) On-On group) for 4 weeks. Expression of TRPA1 and itch-evoked scratching behavior were assessed and quantified. As show in Figure 5a,b, the mice that continued to receive normal water (the transgene On-On group) developed strikingly intense itch-scratch and enhanced growth of TRPA1+/PGP9.5+ nerve fibers in AD skin. In contrast, the expression of TRPA1+/PGP9.5+ in AD lesions and the number of itch-evoked scratching in the Tg(+) mice given Dox water to turn off the IL-13 transgene (the transgene On-Off group) were markedly diminished (Figure 5a, 5b). These findings suggest that pruritus in AD and the expression of TRPA1 are mainly dependent on IL-13.
Cytokine regulation of TRPA1 expression in cultured mast cells
To understand how TRPA1 is regulated by inflammatory cytokines important in AD, we obtained bone marrow derived mast cells (BMMC) from wild type C57BL/6 mice by culturing the cells in IL-3-containing medium for 6 weeks, at which time >98% of the cells are identified as mature mast cells by FACS for c-Kit/FcεRI (39). The BMMC were stimulated for 24 hours with various cytokines and H2O2, reactive oxygen species known to stimulate TRPA1.FACS analysis showed that the expression of TRPA1 was increased when stimulated by H2O2, IL-13 or IFN-γ. Among these, IL-13 showed the strongest stimulation. Interestingly, IL-4 down-regulated the expression of TRPA1 (Figure 6a). By fluorescent IHC, consistent with the FACS results, BMMC stimulated with IL-13 expressed significantly higher TRPA1 (14.7%) compared to H2O2 (4.1%) and IFN-γ (7%) stimulated cells, but IL-4 stimulated cells failed to do so (Figure 6b, 6c), despite the observation that the IL-4 levels in the AD skin were increased (Supplemental Figure 3). Taken together, these data demonstrated thatIL-13 is a potent stimulator of TRPA1 expression in cultured mast cells, where as IL-4 did not stimulate TRPA1 expression. Th1 cytokine IFN-γ modestly up-regulates the expression of TRPA1 in mast cells.
Figure 6. Cytokine regulation of TRPA1 expression in mast cells and functional calcium imaging of mast cells stimulated with TRPA1 agonist.
Bone marrow-derived mast cells (BMMC) were obtained by culturing bone marrow cells of wild type C57BL/6 mice in IL-3-containing medium for 4 to 6 weeks, when 98% of the cells were identified as mature mast cells by Toluidine blue staining and by flow cytometry for c-Kit and FcεRI as previously described (39). (a, b) BMMC were stimulated for 24 hours with H2O2 (10 nM), IL-13 (10 ng/ml),IL-4 (10 ng/ml), or IFN-γ (10 ng/ml). (a) Cultured BMMC were stained for TRPA1 using rabbit anti-TRPA1 antibody and Alexa Flour 488 dye labeled-donkey anti-rabbit IgG (H+L), and analyzed by flow cytometry. (b, c) Detection and quantification of TRPA1+ mast cells (Green) byfluore scent IHC. The data represent 4 independent experiments. (*P<0.05, **p<0.01 vs. Medium).Cultured mast cells (C57.1 cell line) were harvested, washed and loaded with Calcium Sensor Dye eFluor® 514 for 30 minutes at 37°C and t he cells were washed and analyzed by flow cytometry as unstimulated (d) and (e) stimulated with media (Red) and with 100 µM allylisothiocyanate (Blue) for 30 minutes. The maximum intracellular calcium mobilization in cells exposed to the agonist was measured, and histogram overlays are displayed as percentage of Max. Shown are representative of three independent experiments.
Mast cells express functional TRPA1 channel
It has been shown that neuronal sensitivity to allylisothiocyanate (mustard oil) correlates with TRPA1 expression in vivo and TRPA1 can be activated by increases in intracellular calcium (6). To determine whether TRPA1 has a functional role in mast cells, cultured mast cells (murine mast cell line C57.1), were loaded with Calcium Sensor Dye eFluor® 514 for 30 minutes at 37°C in the dark. The cells were then washed and analyzed by flow cytometry as unstimulated (Figure 6d). The cells were then washed and stimulated withTRPA1 agonist, allylisothiocyanate (100 µM, Blue histogram) (Figure 6e). The cells stimulated with allylisothiocyanate showed very strong calcium signals indicative of marked intracellular calcium mobilization. These data indicate thatTRPA1 plays a functional role in mast cells in response to allylisothiocyanate stimulation.
Markedly enhanced expression of TRPA1 in dermal afferent nerves and in mast cells in human AD skin
Although several neuropeptides have been implicated in the pathogenesis of human AD, expression of TRPA1 in human AD has not been characterized. We compared skin biopsy samples from chronic AD lesions of the forearms of AD patients and from the forearms of normal subjects for TRPA1 andPGP9.5 expression by fluorescent IHC. We found that in lesional AD skin, both cutaneous PGP9.5+ and TRPA1+/PGP9.5+ double positive afferent nerves were highly increased (Figure 7a,7b, 7c). In addition,TRPA1was markedly expressed in the dermal cells and keratinocytes in the lesional skin of AD patients, whereas minimal expression of TRPA1 was noted in the skin of normal subjects (Figure 7d). Furthermore, consistent with findings in the Tg(+) AD mice (Figure 2d), we found that tryptase+ mast cells were markedly increased in the AD skin (Figure7e) and that dermal TRPA1+ cells were co-localized with tryptase+ cells, indicating that TRPA1 is expressed in mast cells and the number of tryptase+/TRPA1+ cells was significantly increased and they were in very close proximity to dermal PGP9.5+ afferents (Figure 7f, 7g, close-up), suggesting a spatial relationship between mast cells and the afferent nerves in human skin lesions in AD. Taken together, these findings in human AD, consistent with those in the AD mouse models, suggest that augmented expression of TRPA1 and increased TRPA1+ mast cells may be important in the generation of itch in AD.
Figure 7. Increased dermal sensory nerve growth, TRPA1+ sensory afferent nerves, TRPA1+ epidermal and dermal cells and TRPA1+/Tryptase+ mast cells in chronic lesional skin biopsies from patients with AD.
Fluorescent IHC with rabbit monoclonal anti-TRPA1, anti-PGP9.5, and anti-human Tryptase was performed in skin biopsysamples from normal subjects (NS) and AD patients. The comparison was made between the skin biopsy samples from the forearms of normal subjects and chronic lesional AD biopsy samples from the forearms of AD patients.(a) Quantification of dermal PGP9.5+afferent nerves, and (b) TRPA1+ afferent nerves and (c) markedly increased TRPA+(Green)/PGP9.5+(Red) afferent nerves in AD skin. (d) Expression of TRPA1 (Green), DAPI (Blue) for nuclei, in the epidermis (keratinocytes) and dermal cells. (e) Increased Tryptase+ (Red) mast cells and (f) Co-expression of TRPA1+ (Green) and Tryptase+ (Red) mast cells and these TRPA1+/Tryptase+mast cells in proximity with TRPA1+ afferent nerves (Arrows). (g) Quantification of TRPA1+/Tryptase+mast cells. In (c), (d), (e), and (f), Each is a representative of 3–4 different sections of the skin from each patient. (g)Cells in 10–12 high power fields per slide were counted (Normal subject n=4 and AD patients n=3). (**p<0.01; ***p<0.001).
Discussion
Chronic itch, a hallmark of human AD, represents a huge burdensome clinical problem (43). There is no effective treatment for itch in patients with AD due to a lack of understanding of the mechanisms underlying chronic pruritus. Th2 cytokine IL-13 is a critical mediator in human a topic disorders including asthma and allergic rhinitis. It has a major role in the pathogenesis of both innate and adaptive immunity of AD. The present study was designed to enhance our understanding of the mechanisms of pruritogenesis in AD induced by Th2 cytokine IL-13 in a skin-selective transgenic model of chronic AD and to begin to characterize the relevance of neuronal abnormality to it chin human AD. Our studies demonstrated that IL-13 is a potent stimulator of pruritogenesis in AD and that the pruritogenic effects of IL-13 are mediated, in part, by a novel TRPA1-dependent mechanism. They also demonstrated that dermal expression of TRPA1is critical in mediating itch in IL-13 induced AD and that IL-13 stimulates expression of TRPA1 in mast cellsin vivo and in vitro. Importantly, we found that TRPA1 was highly expressed in the dermal cells, sensory afferents and keratinocytes and co-expressed in tryptase+ mast cells in lesional skin biopsies from patients with AD. To our knowledge, the findings represent the first evidence showing a novel TRPA1-dependent pathway in IL-13-induced itch in AD.
Anti-histamine therapy is often ineffective in treating itch in AD, suggesting that mediators other than histamine such as cytokines and neuropeptides may be involved. Many mediators such as IL-31, substance P and nerve growth factor (NGF) have been shown to have a pruritogenic role in AD (44, 45). We generated and used an externally inducible skin-specific IL-13 transgenic mouse model (K5-tTA-IL-13), as it recapitulates important aspects of human AD, including chronic pruritic dermatitis and systemic Th2 immunity (25, 27, 46). In these mice, we found that the number of mast cells and PGP9.5+ and neuropeptide secreting CGRP+ dermal afferent nerves were significantly increased in the AD skin and that these correlated with chronic itch-scratching behaviors. We showed strongly increased PGP9.5+ and CGRP+ dermal afferents in the skin ofIL-13 Tg(+) mice compared to Tg(−) mice (Figure 1b), although the intensity of immunofluorescent staining for both dermal PGP9.5 and CGRP nerve fibers was not as intense as seen in other studies where knock-in GFP was used as a tracer or colchicine was used to enhance CGRP accumulation before detection were employed (47–49).
Recent studies showed thatTRPA1 is an essential component of the signaling pathways that promote histamine-independent itch and is also a downstream transduction channel onto which multiple histamine-independent itch pathways converge (3). However, the role of TRPA1 in chronic itch associated with pathological conditions, such as AD has yet to be determined. In the present study we observed a markedly enhanced expression of TRPA1 in dermal c-Kit+ mast cells and in dermal CGRP+ afferents in the lesional AD skin, which were associated with increased numbers of TRPA1+ sensory neurons in the dorsal root ganglia and enhanced dermal levels of TRPA1. As a point of significance, these changes correlated with itch-induced scratching, highlighting the importance of TRPA1 in IL-13-induced chronic itch. Furthermore, when TRPA1 was blocked by a specific antagonist in mice with AD, itch-induced scratching was significantly attenuated; by contrast, non-sedating H1 histamine receptor blocker failed to inhibit it chin these mice, indicating that the chronic itch in AD-induced by IL-13 is, at least in part, through the TRPA1 pathway and not through the histamine-dependent pathway. It is possible that the effective blocking of itch-scratch by TRPA1 antagonist is through blocking itch signal transmission. Nevertheless, this indicates a contributing role for TRPA1 in the generation of itch in AD. It has been shown that TRPA1 is co-expressed in approximately 50% of TRPV1+ sensory neurons, which are known to transduce histamine-induced itch (50–54). In contrast to enhanced TRPA1 expression in the AD skin, TRPV1 was found minimally expressed in the AD skin and TRPV1 expression was comparable between WT skin and AD skin (Supplemental Figure 2), suggesting that TRPV1 may not be important in itch in AD induced by IL-13, despite previous findings that the level of histamine in AD lesions was elevated (25).
In chronic inflammatory skin such as AD, stimulated nerve fibers may activate local mast cells, which in turn can regulate local nerve functions (55, 56). In the present study, we demonstrated that in both lesional skin from mice with AD and lesional skin from AD patients, not only was the expression of TRPA1 markedly enhanced and the number of TRPA1+ mast cells significantly increased, but also these TRPA1+ mast cells were in close proximity to afferent fibers. Moreover, the number of TRPA1+ mast cells was correlated with itch-evoked scratching in mice with AD. These findings suggest that in the chronic inflammatory lesional skin, such as in AD, their close anatomical association may represent functionally important interactions between dermal TRPA1+ mast cells and TRPA1+ afferent nerves that could biologically be significant in the induction and maintenance of chronic itch in AD. For example, mast cells are found in close proximity to sensory nerves in inflammatory skin lesions from patients with psoriasis (57), AD (55) and contact dermatitis (31). Allergen-induced activation of tissue mast cells is associated with alterations in the phenotype or physiology of nearby primary afferent (sensory) nerves (58–62).
Interestingly, when mast cells were genetically deleted from IL-13 Tg mice, the onset of itch-evoked scratching behavior was markedly delayed and attenuated, and the expression of TRPA1 in the dermal nerves and epidermal and dermal cells in these mice were significantly diminished, indicating that mast cells are essential for the expression of TRPA1 in dermal sensory nerves and epidermal cells in the AD skin, an important but previously unrecognized role in the pathogenesis and pruritogenesis of AD induced by IL-13. In chronic inflammatory skin, stimulated sensory nerves can activate local mast cells, which in turn can influence local afferent nerve function. Indeed, other studies showed that neuropeptides released by cutaneous nerves, such as substance P, vasoactive intestinal peptide, and so matostatin can induce mast cells to release inflammatory mediators, such as histamine, tumor necrosis factor (TNF), and other inflammatory mediators (63–68). Afferent nerves express specific receptors for neuropeptides (69), prostaglandins (70), histamine (71), proteases (72), neurotrophins (73), and cytokines (74, 75). Levels of IL-13 in the skin samples from Tg(+)/c-Kit+/+ and Tg(+)/KitW-s/W-sh were comparable indicating that mast cell deficiency in K5-tTA-IL-13 mice did not affect the expression of theIL-13transgene and that changes in diminished TRPA1 expression and reduced AD severity in mast cell deficient Tg(+) mice were not caused by inhibition of the IL-13 transgene (Supplemental Figure 3a). Our present study suggests that mast cell deficiency in IL-13 Tg(+) mice leads to interruption of this positive feed-back loop of neuro-inflammation-itch, which may be TRPA1-dependent.
TRPA1 was reported to be expressed in different mammalian tissues, including brain, intestine and pancreas (76, 77), human skin keratinocytes (78, 79), and vestibular and auditory sensory epithelia (78, 80). However, functional activity of TRPA1 channels is most consistently characterized in sensory neurons and other cells with sensory functions. Functional TRPA1 has been reported in synoviocytes of joints (81) and endothelial cells (82). Our studies showed that IL-13, besides its immunomodulatory roles in both innate and adaptive immunity and in compromising the dermal barrier immune defense against microbial infections in AD (83) ((20, 84, 85), has a novel role in the pruritogenesis of AD. After the IL-13 transgene in vivo was turned off in Tg(+) mice that developed AD, the growth of TRPA1+/PGP9.5+ afferents and the expression of TRPA1+ cells in lesional AD skin were significantly diminished. Our in vitro data on cytokine regulation of TRPA1 expression in cultured mast cells demonstrated thatIL-13 is a potent stimulator of TRPA1 expression in mast cells. IFN-γ modestly increased TRPA1 expression in mast cells. Interestingly, IL-4, another Th2 cytokine, failed to up-regulate TRPA1 expression. Although Th2 cytokines IL-13 and IL-4, using the same IL-4 receptor type II (heterodimer of IL-4 receptor αand IL-13 receptor α1), share many biological activities, there is considerable evidence that IL-13 has some unique functions in vivo not seen with IL-4. IL-13 blockade abolished allergic inflammation independently of IL-4 (21, 22) and IL-13 expels helminthN. brasiliensis infection independently of IL-4 (86). Differences between IL-4 and IL-13 responses might be due to differences in their receptors and signaling pathways (87). In a contact dermatitis model, topical application of TRPA1 agonist, allylisothiocyanate, resulted in suppression of IL-4 production by local lymph nodes (88). The role of IL-4 in TRPA1 in chronic allergic dermatitis needs to be further studied. Importantly, cultured mast cells stimulated with TRPA1 agonist, Allylisothiocyanate showed markedly increased calcium signals indicating a functional role of TRPA1 in mast cells.
Importantly, in accordance with our findings in mice with AD, we found enhanced expression of TRPA1 in dermal mast cells, dermal afferent nerves and the epidermis in the lesional skin from patients with AD. The finding of increased mast cells in the AD skin biopsies was consistent with the findings that increased mast cells and degranulation have been shown in the lesional skin of AD patients (89, 90). The finding of heightenedTRPA1expression in the epidermis of lesional human AD skin suggests that TRPA1 in the epidermal cells including keratinocytes could also contribute to chronic itch in AD.
When viewed in combination, these novel observations show that TRPA1 expression in the lesional AD skin (keratinocytes, mast cells and dermal afferent nerve fibers) is essential for the pruritogenesis in AD and that mast cells positively regulate TRPA1 expression in dermal sensory nerves in AD skin and that IL-13 is a potent stimulator of TRPA1 expression in mast cells. It is important to point out, however, that TRPA1 antagonist, HC-030031 administration and the null mutation of c-Kit to delete mast cells, while markedly decreasing IL-13-induced AD associated itch and TRPA1 expression in AD skin, did not completely abrogate IL-13-induced itch responses. This suggests that mast cell-independent, TRPA1-independent mechanism(s), or other pruritogenic mediators or pathways also contribute to the pathogenesis of IL-13-induced itch in AD. The mechanisms that promote TRPA1 expression in dermal sensory afferents and the epidermis in the AD skin and those that diminish TRPA1 expression in the dermal sensory afferents in the AD skin from mast cell-deficient IL-13Tg mice remain to be fully defined in the future studies. Importantly, demonstration of enhanced expression of TRPA1 in dermal mast cells, dermal sensory nerves and in the epidermis in the chronic AD lesions in IL-13 transgenic mice was recapitulated in the findings from studies of the biopsy samples from patients with AD. Demonstration of increased TRPA1+ mast cells and cutaneous nerve growth in the lesional AD skin in the current studies highlights their relevance and importance in the cellular network of chronic itch.
In summary, our study revealed a novel neural mechanism underlying chronic itch in AD induced by IL-13. This mechanism is TRPA1-dependent, involves interactions between TRPA1+ dermal mast cells and TRPA1+ dermal afferent nerves in a Th2 dominated inflammatory environment, and is responsible for the pruritogenesis of chronic itch in AD. These studies also indicate a role for TRPA1 in the pruritogenesis of human AD.
Supplementary Material
Acknowledgments
We thank Dr. Yong-Jun Liu for providing human AD biopsy samples and Dr. David Julius (UCSF) for providing TRPA1 KO mice for this study.
This work was supported by NIH grants AI07502 to T Zhengand HL079349 and HL107151 to Z Zhu.
References
- 1.Yosipovitch G, Fleischer A. Itch associated with skin disease: advances in pathophysiology and emerging therapies. Am J Clin Dermatol. 2003;4:617–622. doi: 10.2165/00128071-200304090-00004. [DOI] [PubMed] [Google Scholar]
- 2.Twycross R, Greaves MW, Handwerker H, Jones EA, Libretto SE, Szepietowski JC, Zylicz Z. Itch: scratching more than the surface. QJM. 2003;96:7–26. doi: 10.1093/qjmed/hcg002. [DOI] [PubMed] [Google Scholar]
- 3.Wilson SR, Gerhold KA, Bifolck-Fisher A, Liu Q, Patel KN, Dong X, Bautista DM. TRPA1 is required for histamine-independent, Mas-related G protein-coupled receptor-mediated itch. Nat Neurosci. 2011;14:595–602. doi: 10.1038/nn.2789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baraldi PG, Preti D, Materazzi S, Geppetti P. Transient receptor potential ankyrin 1 (TRPA1) channel as emerging target for novel analgesics and anti-inflammatory agents. J Med Chem. 2010;53:5085–5107. doi: 10.1021/jm100062h. [DOI] [PubMed] [Google Scholar]
- 5.Trevisani M, Siemens J, Materazzi S, Bautista DM, Nassini R, Campi B, Imamachi N, Andre E, Patacchini R, Cottrell GS, Gatti R, Basbaum AI, Bunnett NW, Julius D, Geppetti P. 4-Hydroxynonenal, an endogenous aldehyde, causes pain and neurogenic inflammation through activation of the irritant receptor TRPA1. Proc Natl Acad Sci U S A. 2007;104:13519–13524. doi: 10.1073/pnas.0705923104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jordt SE, Bautista DM, Chuang HH, McKemy DD, Zygmunt PM, Hogestatt ED, Meng ID, Julius D. Mustard oils and cannabinoids excite sensory nerve fibres through the TRP channel ANKTM1. Nature. 2004;427:260–265. doi: 10.1038/nature02282. [DOI] [PubMed] [Google Scholar]
- 7.Bandell M, Story GM, Hwang SW, Viswanath V, Eid SR, Petrus MJ, Earley TJ, Patapoutian A. Noxious cold ion channel TRPA1 is activated by pungent compounds and bradykinin. Neuron. 2004;41:849–857. doi: 10.1016/s0896-6273(04)00150-3. [DOI] [PubMed] [Google Scholar]
- 8.Liu Q, Tang Z, Surdenikova L, Kim S, Patel KN, Kim A, Ru F, Guan Y, Weng HJ, Geng Y, Undem BJ, Kollarik M, Chen ZF, Anderson DJ, Dong X. Sensory neuron-specific GPCR Mrgprs are itch receptors mediating chloroquine-induced pruritus. Cell. 2009;139:1353–1365. doi: 10.1016/j.cell.2009.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parsons ME, Ganellin CR. Histamine and its receptors. Br J Pharmacol. 2006;147(Suppl 1):S127–S135. doi: 10.1038/sj.bjp.0706440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Julius D, MacDermott AB, Axel R, Jessell TM. Molecular characterization of a functional cDNA encoding the serotonin 1c receptor. Science. 1988;241:558–564. doi: 10.1126/science.3399891. [DOI] [PubMed] [Google Scholar]
- 11.Jeffry J, Kim S, Chen ZF. Itch signaling in the nervous system. Physiology (Bethesda) 2011;26:286–292. doi: 10.1152/physiol.00007.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun YG, Zhao ZQ, Meng XL, Yin J, Liu XY, Chen ZF. Cellular basis of itch sensation. Science. 2009;325:1531–1534. doi: 10.1126/science.1174868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berry MA, Parker D, Neale N, Woodman L, Morgan A, Monk P, Bradding P, Wardlaw AJ, Pavord ID, Brightling CE. Sputum and bronchial submucosal IL-13 expression in asthma and eosinophilic bronchitis. The Journal of allergy and clinical immunology. 2004;114:1106–1109. doi: 10.1016/j.jaci.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 14.Wills-Karp M. Interleukin-13 in asthma pathogenesis. Immunol Rev. 2004;202:175–190. doi: 10.1111/j.0105-2896.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- 15.Wynn TA. IL-13 effector functions. Annu Rev Immunol. 2003;21:425–456. doi: 10.1146/annurev.immunol.21.120601.141142. [DOI] [PubMed] [Google Scholar]
- 16.Hamid Q, Naseer T, Minshall EM, Song YL, Boguniewicz M, Leung DY. In vivo expression of IL-12 and IL-13 in a topic dermatitis. The Journal of allergy and clinical immunology. 1996;98:225–231. doi: 10.1016/s0091-6749(96)70246-4. [DOI] [PubMed] [Google Scholar]
- 17.Homey B, Steinhoff M, Ruzicka T, Leung DY. Cytokines and chemokines orchestrate atopic skin inflammation. The Journal of allergy and clinical immunology. 2006;118:178–189. doi: 10.1016/j.jaci.2006.03.047. [DOI] [PubMed] [Google Scholar]
- 18.Leung AK, Hon KL, Robson WL. Atopic dermatitis. Adv Pediatr. 2007;54:241–273. doi: 10.1016/j.yapd.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 19.Boguniewicz M, Leung DY. Recent insights into atopic dermatitis and implications for management of infectious complications. The Journal of allergy and clinical immunology. 2010;125:4–13. doi: 10.1016/j.jaci.2009.11.027. quiz 14–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Howell MD, Kim BE, Gao P, Grant AV, Boguniewicz M, DeBenedetto A, Schneider L, Beck LA, Barnes KC, Leung DY. Cytokine modulation of atopic dermatitis filaggrin skin expression. The Journal of allergy and clinical immunology. 2009;124:R7–R12. doi: 10.1016/j.jaci.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 21.Grunig G, Warnock M, Wakil AE, Venkayya R, Brombacher F, Rennick DM, Sheppard D, Mohrs M, Donaldson DD, Locksley RM, Corry DB. Requirement for IL-13 independently of IL-4 in experimental asthma. Science. 1998;282:2261–2263. doi: 10.1126/science.282.5397.2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wills-Karp M, Luyimbazi J, Xu X, Schofield B, Neben TY, Karp CL, Donaldson DD. Interleukin-13: central mediator of allergic asthma. Science. 1998;282:2258–2261. doi: 10.1126/science.282.5397.2258. [DOI] [PubMed] [Google Scholar]
- 23.Zhu Z, Homer RJ, Wang Z, Chen Q, Geba GP, Wang J, Zhang Y, Elias JA. Pulmonary expression of interleukin-13 causes inflammation, mucus hypersecretion, subepithelial fibrosis, physiologic abnormalities, and eotaxin production. J Clin Invest. 1999;103:779–788. doi: 10.1172/JCI5909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zheng T, Liu W, Oh SY, Zhu Z, Hu B, Homer RJ, Cohn L, Grusby MJ, Elias JA. IL-13 receptor alpha2 selectively inhibits IL-13-induced responses in the murine lung. J Immunol. 2008;180:522–529. doi: 10.4049/jimmunol.180.1.522. [DOI] [PubMed] [Google Scholar]
- 25.Zheng T, Oh MH, Oh SY, Schroeder JT, Glick AB, Zhu Z. Transgenic expression of interleukin-13 in the skin induces a pruritic dermatitis and skin remodeling. J Invest Dermatol. 2009;129:742–751. doi: 10.1038/jid.2008.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhu Z, Oh MH, Yu J, Liu YJ, Zheng T. The Role of TSLP in IL-13-Induced Atopic March. Sci Rep. 2011;1:23. doi: 10.1038/srep00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oh MH, Oh SY, Yu J, Myers AC, Leonard WJ, Liu YJ, Zhu Z, Zheng T. IL-13 induces skin fibrosis in atopic dermatitis by thymic stromal lymphopoietin. J Immunol. 2011;186:7232–7242. doi: 10.4049/jimmunol.1100504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu Z, Zheng T, Homer RJ, Kim YK, Chen NY, Cohn L, Hamid Q, Elias JA. Acidic mammalian chitinase in asthmatic Th2 inflammation and IL-13 pathway activation. Science. 2004;304:1678–1682. doi: 10.1126/science.1095336. [DOI] [PubMed] [Google Scholar]
- 29.Walter DM, McIntire JJ, Berry G, McKenzie AN, Donaldson DD, DeKruyff RH, Umetsu DT. Critical role for IL-13 in the development of allergen-induced airway hyperreactivity. J Immunol. 2001;167:4668–4675. doi: 10.4049/jimmunol.167.8.4668. [DOI] [PubMed] [Google Scholar]
- 30.Kuo HS, Tsai MJ, Huang MC, Chiu CW, Tsai CY, Lee MJ, Huang WC, Lin YL, Kuo WC, Cheng H. Acid fibroblast growth factor and peripheral nerve grafts regulate Th2 cytokine expression, macrophage activation, polyamine synthesis, and neurotrophin expression in transected rat spinal cords. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:4137–4147. doi: 10.1523/JNEUROSCI.2592-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kakurai M, Monteforte R, Suto H, Tsai M, Nakae S, Galli SJ. Mast cell-derived tumor necrosis factor can promote nerve fiber elongation in the skin during contact hypersensitivity in mice. Am J Pathol. 2006;169:1713–1721. doi: 10.2353/ajpath.2006.060602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bienenstock J, MacQueen G, Sestini P, Marshall JS, Stead RH, Perdue MH. Mast cell/nerve interactions in vitro and in vivo. Am Rev Respir Dis. 1991;143:S55–S58. doi: 10.1164/ajrccm/143.3_Pt_2.S55. [DOI] [PubMed] [Google Scholar]
- 33.Metz M, Grimbaldeston MA, Nakae S, Piliponsky AM, Tsai M, Galli SJ. Mast cells in the promotion and limitation of chronic inflammation. Immunol Rev. 2007;217:304–328. doi: 10.1111/j.1600-065X.2007.00520.x. [DOI] [PubMed] [Google Scholar]
- 34.Siebenhaar F, Magerl M, Peters EM, Hendrix S, Metz M, Maurer M. Mast cell-driven skin inflammation is impaired in the absence of sensory nerves. The Journal of allergy and clinical immunology. 2008;121:955–961. doi: 10.1016/j.jaci.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 35.Niyonsaba F, Ushio H, Hara M, Yokoi H, Tominaga M, Takamori K, Kajiwara N, Saito H, Nagaoka I, Ogawa H, Okumura K. Antimicrobial peptides human beta-defensins and cathelicidin LL-37 induce the secretion of a pruritogenic cytokine IL-31 by human mast cells. J Immunol. 2010;184:3526–3534. doi: 10.4049/jimmunol.0900712. [DOI] [PubMed] [Google Scholar]
- 36.Grimbaldeston MA, Chen CC, Piliponsky AM, Tsai M, Tam SY, Galli SJ. Mast cell-deficient W-sash c-kit mutant Kit W-sh/W-sh mice as a model for investigating mast cell biology in vivo. Am J Pathol. 2005;167:835–848. doi: 10.1016/S0002-9440(10)62055-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Akei HS, Brandt EB, Mishra A, Strait RT, Finkelman FD, Warrier MR, Hershey GK, Blanchard C, Rothenberg ME. Epicutaneous aeroallergen exposure induces systemic TH2 immunity that predisposes to allergic nasal responses. The Journal of allergy and clinical immunology. 2006;118:62–69. doi: 10.1016/j.jaci.2006.04.046. [DOI] [PubMed] [Google Scholar]
- 38.Rossbach K, Wendorff S, Sander K, Stark H, Gutzmer R, Werfel T, Kietzmann M, Baumer W. Histamine H4 receptor antagonism reduces hapten-induced scratching behaviour but not inflammation. Exp Dermatol. 2009;18:57–63. doi: 10.1111/j.1600-0625.2008.00762.x. [DOI] [PubMed] [Google Scholar]
- 39.Zhang L, Oh SY, Wu X, Oh MH, Wu F, Schroeder JT, Takemoto CM, Zheng T, Zhu Z. SHP-1 deficient mast cells are hyperresponsive to stimulation and critical in initiating allergic inflammation in the lung. J Immunol. 2010;184:1180–1190. doi: 10.4049/jimmunol.0901972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Soumelis V, Reche PA, Kanzler H, Yuan W, Edward G, Homey B, Gilliet M, Ho S, Antonenko S, Lauerma A, Smith K, Gorman D, Zurawski S, Abrams J, Menon S, McClanahan T, de Waal-Malefyt Rd R, Bazan F, Kastelein RA, Liu YJ. Human epithelial cells trigger dendritic cell mediated allergic inflammation by producing TSLP. Nat Immunol. 2002;3:673–680. doi: 10.1038/ni805. [DOI] [PubMed] [Google Scholar]
- 41.Steinhoff M, Stander S, Seeliger S, Ansel JC, Schmelz M, Luger T. Modern aspects of cutaneous neurogenic inflammation. Arch Dermatol. 2003;139:1479–1488. doi: 10.1001/archderm.139.11.1479. [DOI] [PubMed] [Google Scholar]
- 42.Steinhoff M, Bienenstock J, Schmelz M, Maurer M, Wei E, Biro T. Neurophysiological, neuroimmunological, and neuroendocrine basis of pruritus. J Invest Dermatol. 2006;126:1705–1718. doi: 10.1038/sj.jid.5700231. [DOI] [PubMed] [Google Scholar]
- 43.Boguniewicz M, Leung DY. Atopic dermatitis: a disease of altered skin barrier and immune dysregulation. Immunol Rev. 2011;242:233–246. doi: 10.1111/j.1600-065X.2011.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sonkoly E, Muller A, Lauerma AI, Pivarcsi A, Soto H, Kemeny L, Alenius H, Dieu-Nosjean MC, Meller S, Rieker J, Steinhoff M, Hoffmann TK, Ruzicka T, Zlotnik A, Homey B. IL-31: a new link between T cells and pruritus in atopic skin inflammation. The Journal of allergy and clinical immunology. 2006;117:411–417. doi: 10.1016/j.jaci.2005.10.033. [DOI] [PubMed] [Google Scholar]
- 45.Raap U, Wichmann K, Bruder M, Stander S, Wedi B, Kapp A, Werfel T. Correlation of IL-31 serum levels with severity of atopic dermatitis. The Journal of allergy and clinical immunology. 2008;122:421–423. doi: 10.1016/j.jaci.2008.05.047. [DOI] [PubMed] [Google Scholar]
- 46.Zhu Z, Oh MH, Yu J, Liu YJ, Zheng T. The Role of TSLP in IL-13-Induced Atopic March. Sci Rep. 2012;1:23. doi: 10.1038/srep00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McCoy ES, Taylor-Blake B, Zylka MJ. CGRP alpha-expressing sensory neurons respond to stimuli that evoke sensations of pain and itch. PloS one. 2012;7:e36355. doi: 10.1371/journal.pone.0036355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Conrath M, Taquet H, Pohl M, Carayon A. Immunocytochemical evidence for calcitonin gene-related peptide-like neurons in the dorsal horn and lateral spinal nucleus of the rat cervical spinal cord. Journal of chemical neuroanatomy. 1989;2:335–347. [PubMed] [Google Scholar]
- 49.Tie-Jun SS, Xu Z, Hokfelt T. The expression of calcitonin gene-related peptide in dorsal horn neurons of the mouse lumbar spinal cord. Neuroreport. 2001;12:739–743. doi: 10.1097/00001756-200103260-00025. [DOI] [PubMed] [Google Scholar]
- 50.Imamachi N, Park GH, Lee H, Anderson DJ, Simon MI, Basbaum AI, Han SK. TRPV1-expressing primary afferents generate behavioral responses to pruritogens via multiple mechanisms. Proc Natl Acad Sci U S A. 2009;106:11330–11335. doi: 10.1073/pnas.0905605106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zylka MJ, Dong X, Southwell AL, Anderson DJ. Atypical expansion in mice of the sensory neuron-specific Mrg G protein-coupled receptor family. Proc Natl Acad Sci U S A. 2003;100:10043–10048. doi: 10.1073/pnas.1732949100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Salas MM, Hargreaves KM, Akopian AN. TRPA1-mediated responses in trigeminal sensory neurons: interaction between TRPA1 and TRPV1. Eur J Neurosci. 2009;29:1568–1578. doi: 10.1111/j.1460-9568.2009.06702.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xiao B, Patapoutian A. Scratching the surface: a role of pain-sensing TRPA1 in itch. Nat Neurosci. 2011;14:540–542. doi: 10.1038/nn.2813. [DOI] [PubMed] [Google Scholar]
- 54.Andersson DA, Gentry C, Moss S, Bevan S. Transient receptor potential A1 is a sensory receptor for multiple products of oxidative stress. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2008;28:2485–2494. doi: 10.1523/JNEUROSCI.5369-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sugiura H, Maeda T, Uehara M. Mast cell invasion of peripheral nerve in skin lesions of atopic dermatitis. Acta Derm Venereol Suppl (Stockh) 1992;176:74–76. [PubMed] [Google Scholar]
- 56.Alving K, Sundstrom C, Matran R, Panula P, Hokfelt T, Lundberg JM. Association between histamine-containing mast cells and sensory nerves in the skin and airways of control and capsaicin-treated pigs. Cell Tissue Res. 1991;264:529–538. doi: 10.1007/BF00319042. [DOI] [PubMed] [Google Scholar]
- 57.Naukkarinen A, Jarvikallio A, Lakkakorpi J, Harvima IT, Harvima RJ, Horsmanheimo M. Quantitative histochemical analysis of mast cells and sensory nerves in psoriatic skin. J Pathol. 1996;180:200–205. doi: 10.1002/(SICI)1096-9896(199610)180:2<200::AID-PATH632>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 58.Greene R, Fowler J, MacGlashan D, Jr, Weinreich D. IgE-challenged human lung mast cells excite vagal sensory neurons in vitro. J Appl Physiol. 1988;64:2249–2253. doi: 10.1152/jappl.1988.64.5.2249. [DOI] [PubMed] [Google Scholar]
- 59.Riccio MM, Proud D, Undem BJ. Enhancement of afferent nerve excitability in the airways by allergic inflammation. Pulm Pharmacol. 1995;8:181–185. doi: 10.1006/pulp.1995.1024. [DOI] [PubMed] [Google Scholar]
- 60.Myers AC, Kajekar R, Undem BJ. Allergic inflammation-induced neuropeptide production in rapidly adapting afferent nerves in guinea pig airways. Am J Physiol Lung Cell Mol Physiol. 2002;282:L775–L781. doi: 10.1152/ajplung.00353.2001. [DOI] [PubMed] [Google Scholar]
- 61.Barbara G, Wang B, Stanghellini V, de Giorgio R, Cremon C, Di Nardo G, Trevisani M, Campi B, Geppetti P, Tonini M, Bunnett NW, Grundy D, Corinaldesi R. Mast cell-dependent excitation of visceral-nociceptive sensory neurons in irritable bowel syndrome. Gastroenterology. 2007;132:26–37. doi: 10.1053/j.gastro.2006.11.039. [DOI] [PubMed] [Google Scholar]
- 62.van Houwelingen AH, Kool M, de Jager SC, Redegeld FA, van Heuven-Nolsen D, Kraneveld AD, Nijkamp FP. Mast cell-derived TNF-alpha primes sensory nerve endings in a pulmonary hypersensitivity reaction. J Immunol. 2002;168:5297–5302. doi: 10.4049/jimmunol.168.10.5297. [DOI] [PubMed] [Google Scholar]
- 63.Piotrowski W, Devoy MA, Jordan CC, Foreman JC. The substance P receptor on rat mast cells and in human skin. Agents Actions. 1984;14:420–424. doi: 10.1007/BF01973842. [DOI] [PubMed] [Google Scholar]
- 64.Matsuda H, Kawakita K, Kiso Y, Nakano T, Kitamura Y. Substance P induces granulocyte infiltration through degranulation of mast cells. J Immunol. 1989;142:927–931. [PubMed] [Google Scholar]
- 65.Yano H, Wershil BK, Arizono N, Galli SJ. Substance P-induced augmentation of cutaneous vascular permeability and granulocyte infiltration in mice is mast cell dependent. J Clin Invest. 1989;84:1276–1286. doi: 10.1172/JCI114295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Niizeki H, Alard P, Streilein JW. Calcitonin gene-related peptide is necessary for ultraviolet B-impaired induction of contact hypersensitivity. J Immunol. 1997;159:5183–5186. [PubMed] [Google Scholar]
- 67.Ottosson A, Edvinsson L. Release of histamine from dural mast cells by substance P and calcitonin gene-related peptide. Cephalalgia. 1997;17:166–174. doi: 10.1046/j.1468-2982.1997.1703166.x. [DOI] [PubMed] [Google Scholar]
- 68.De Jonge F, De Laet A, Van Nassauw L, Brown JK, Miller HR, van Bogaert PP, Timmermans JP, Kroese AB. In vitro activation of murine DRG neurons by CGRP-mediated mucosal mast cell degranulation. Am J Physiol Gastrointest Liver Physiol. 2004;287:G178–G191. doi: 10.1152/ajpgi.00528.2003. [DOI] [PubMed] [Google Scholar]
- 69.Budai D, Larson AA. Role of substance P in the modulation of C-fiber-evoked responses of spinal dorsal horn neurons. Brain Res. 1996;710:197–203. doi: 10.1016/0006-8993(95)01384-9. [DOI] [PubMed] [Google Scholar]
- 70.Oida H, Namba T, Sugimoto Y, Ushikubi F, Ohishi H, Ichikawa A, Narumiya S. In situ hybridization studies of prostacyclin receptor mRNA expression in various mouse organs. Br J Pharmacol. 1995;116:2828–2837. doi: 10.1111/j.1476-5381.1995.tb15933.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ninkovic M, Hunt SP. Opiate and histamine H1 receptors are present on some substance P-containing dorsal root ganglion cells. Neurosci Lett. 1985;53:133–137. doi: 10.1016/0304-3940(85)90109-0. [DOI] [PubMed] [Google Scholar]
- 72.Steinhoff M, Neisius U, Ikoma A, Fartasch M, Heyer G, Skov PS, Luger TA, Schmelz M. Proteinase-activated receptor-2 mediates itch: a novel pathway for pruritus in human skin. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2003;23:6176–6180. doi: 10.1523/JNEUROSCI.23-15-06176.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Davies AM, Bandtlow C, Heumann R, Korsching S, Rohrer H, Thoenen H. Timing and site of nerve growth factor synthesis in developing skin in relation to innervation and expression of the receptor. Nature. 1987;326:353–358. doi: 10.1038/326353a0. [DOI] [PubMed] [Google Scholar]
- 74.Thier M, Marz P, Otten U, Weis J, Rose-John S. Interleukin-6 (IL-6) and its soluble receptor support survival of sensory neurons. J Neurosci Res. 1999;55:411–422. doi: 10.1002/(SICI)1097-4547(19990215)55:4<411::AID-JNR2>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 75.Stark B, Carlstedt T, Risling M. Distribution of TGF-beta, the TGF-beta type I receptor and the R-II receptor in peripheral nerves and mechanoreceptors; observations on changes after traumatic injury. Brain Res. 2001;913:47–56. doi: 10.1016/s0006-8993(01)02757-3. [DOI] [PubMed] [Google Scholar]
- 76.Garcia-Anoveros J, Nagata K. Trpa1. Handb Exp Pharmacol. 2007:347–362. doi: 10.1007/978-3-540-34891-7_21. [DOI] [PubMed] [Google Scholar]
- 77.Doihara H, Nozawa K, Kawabata-Shoda E, Kojima R, Yokoyama T, Ito H. TRPA1 agonists delay gastric emptying in rats through serotonergic pathways. Naunyn Schmiedebergs Arch Pharmacol. 2009;380:353–357. doi: 10.1007/s00210-009-0435-7. [DOI] [PubMed] [Google Scholar]
- 78.Anand U, Otto WR, Facer P, Zebda N, Selmer I, Gunthorpe MJ, Chessell IP, Sinisi M, Birch R, Anand P. TRPA1 receptor localisation in the human peripheral nervous system and functional studies in cultured human and rat sensory neurons. Neurosci Lett. 2008;438:221–227. doi: 10.1016/j.neulet.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 79.Atoyan R, Shander D, Botchkareva NV. Non-neuronal expression of transient receptor potential type A1 (TRPA1) in human skin. J Invest Dermatol. 2009;129:2312–2315. doi: 10.1038/jid.2009.58. [DOI] [PubMed] [Google Scholar]
- 80.Nagata K, Duggan A, Kumar G, Garcia-Anoveros J. Nociceptor and hair cell transducer properties of TRPA1, a channel for pain and hearing. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2005;25:4052–4061. doi: 10.1523/JNEUROSCI.0013-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kochukov MY, McNearney TA, Fu Y, Westlund KN. Thermosensitive TRP ion channels mediate cytosolic calcium response in human synoviocytes. Am J Physiol Cell Physiol. 2006;291:C424–C432. doi: 10.1152/ajpcell.00553.2005. [DOI] [PubMed] [Google Scholar]
- 82.Earley S, Gonzales AL, Crnich R. Endothelium-dependent cerebral artery dilation mediated by TRPA1 and Ca2+-Activated K+ channels. Circ Res. 2009;104:987–994. doi: 10.1161/CIRCRESAHA.108.189530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Leung DY, Boguniewicz M, Howell MD, Nomura I, Hamid QA. New insights into atopic dermatitis. J Clin Invest. 2004;113:651–657. doi: 10.1172/JCI21060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Howell MD, Gallo RL, Boguniewicz M, Jones JF, Wong C, Streib JE, Leung DY. Cytokine milieu of atopic dermatitis skin subverts the innate immune response to vaccinia virus. Immunity. 2006;24:341–348. doi: 10.1016/j.immuni.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 85.Howell MD, Fairchild HR, Kim BE, Bin L, Boguniewicz M, Redzic JS, Hansen KC, Leung DY. Th2 cytokines act on S100/A11 to downregulate keratinocyte differentiation. J Invest Dermatol. 2008;128:2248–2258. doi: 10.1038/jid.2008.74. [DOI] [PubMed] [Google Scholar]
- 86.Finkelman FD, Wynn TA, Donaldson DD, Urban JF. The role of IL-13 in helminth-induced inflammation and protective immunity against nematode infections. Current opinion in immunology. 1999;11:420–426. doi: 10.1016/S0952-7915(99)80070-3. [DOI] [PubMed] [Google Scholar]
- 87.Hershey GK. IL-13 receptors and signaling pathways: an evolving web. The Journal of allergy and clinical immunology. 2003;111:677–690. doi: 10.1067/mai.2003.1333. quiz 691. [DOI] [PubMed] [Google Scholar]
- 88.Maruyama T, Iizuka H, Tobisawa Y, Shiba T, Matsuda T, Kurohane K, Imai Y. Influence of local treatments with capsaicin or allyl isothiocyanate in the sensitization phase of a fluorescein-isothiocyanate-induced contact sensitivity model. International archives of allergy and immunology. 2007;143:144–154. doi: 10.1159/000099081. [DOI] [PubMed] [Google Scholar]
- 89.Irani AM, Sampson HA, Schwartz LB. Mast cells in atopic dermatitis. Allergy. 1989;44(Suppl 9):31–34. [PubMed] [Google Scholar]
- 90.Soter NA. Morphology of a topic eczema. Allergy. 1989;44(Suppl 9):16–19. doi: 10.1111/j.1398-9995.1989.tb04310.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.