Abstract
Background
Historically, women have been attended and supported by other women during labour. However, in hospitals worldwide, continuous support during labour has become the exception rather than the routine.
Objectives
Primary: to assess the effects of continuous, one-to-one intrapartum support compared with usual care. Secondary: to determine whether the effects of continuous support are influenced by: (1) routine practices and policies; (2) the provider’s relationship to the hospital and to the woman; and (3) timing of onset.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register (30 June 2012).
Selection criteria
All published and unpublished randomised controlled trials comparing continuous support during labour with usual care.
Data collection and analysis
We used standard methods of The Cochrane Collaboration Pregnancy and Childbirth Group. Two review authors independently evaluated methodological quality and extracted the data. We sought additional information from the trial authors. We used random-effects analyses for comparisons in which high heterogeneity was present, and we reported results using the average risk ratio (RR) for categorical data and mean difference (MD) for continuous data.
Main results
Twenty-two trials involving 15,288 women met inclusion criteria and provided usable outcome data. Results are of random-effects analyses, unless otherwise noted. Women allocated to continuous support were more likely to have a spontaneous vaginal birth (RR 1.08, 95% confidence interval (CI) 1.04 to 1.12) and less likely to have intrapartum analgesia (RR 0.90, 95% CI 0.84 to 0.96) or to report dissatisfaction (RR 0.69, 95% CI 0.59 to 0.79). In addition, their labours were shorter (MD −0.58 hours, 95% CI −0.85 to −0.31), they were less likely to have a caesarean (RR 0.78, 95% CI 0.67 to 0.91) or instrumental vaginal birth (fixed-effect, RR 0.90, 95% CI 0.85 to 0.96), regional analgesia (RR 0.93, 95% CI 0.88 to 0.99), or a baby with a low five-minute Apgar score (fixed-effect, RR 0.69, 95% CI 0.50 to 0.95). There was no apparent impact on other intrapartum interventions, maternal or neonatal complications, or breastfeeding. Subgroup analyses suggested that continuous support was most effective when the provider was neither part of the hospital staff nor the woman’s social network, and in settings in which epidural analgesia was not routinely available. No conclusions could be drawn about the timing of onset of continuous support.
Authors’ conclusions
Continuous support during labour has clinically meaningful benefits for women and infants and no known harm. All women should have support throughout labour and birth.
BACKGROUND
The first version of this Cochrane review was published in 1995 (Hodnett 2003), when the first systematic reviews in The Cochrane Collaboration Pregnancy and Childbirth Group Module were converted to the Cochrane review format. Thus, a formal Cochrane protocol was not initially published. Subsequently, the review author, Ellen Hodnett, completed a trial of labour support (Hodnett 2002) with a sample size larger than the entire sample in the prior version of the original review. As a protection against bias, she sought co-authors who were blind to the results of the new trial and who had special expertise that would enhance the quality of the review. Discussions among the authors led to decisions to modify the background and methods. The authors decided that the best approach would be to write a new protocol for the review. The new protocol was submitted through the peer review process of the Cochrane Pregnancy and Childbirth Group and has subsequently evolved into a review that has been updated.
Historically and cross-culturally, women have been attended and supported by other women during labour and birth. However, since the middle of the 20th century, in many countries as the majority of women gave birth in hospital rather than at home, continuous support during labour has become the exception rather than the routine. Concerns about dehumanisation of women’s birth experiences (in high-, middle-, and low-income countries) have led to calls for a return to continuous, one-to-one support by women for women during labour (Klaus 2002). Common elements of this care include emotional support (continuous presence, reassurance and praise), information about labour progress and advice regarding coping techniques, comfort measures (such as comforting touch, massage, warm baths/showers, promoting adequate fluid intake and output) and advocacy (helping the woman articulate her wishes to others).
Two complementary theoretical explanations have been offered for the effects of labour support on childbirth outcomes. Both explanations hypothesise that labour support enhances labour physiology and mothers’ feelings of control and competence, reducing reliance on medical interventions. The first theoretical explanation considers possible mechanisms when companionship during labour is used in stressful, threatening and disempowering clinical birth environments (Hofmeyr 1991). During labour, women may be uniquely vulnerable to environmental influences; modern obstetric care frequently subjects women to institutional routines, high rates of intervention, unfamiliar personnel, lack of privacy and other conditions that may be experienced as harsh. These conditions may have an adverse effect on the progress of labour and on the development of feelings of competence and confidence; this may in turn impair adjustment to parenthood and establishment of breastfeeding, and increase the risk of depression. The provision of support and companionship during labour may to some extent buffer such stressors.
The second theoretical explanation does not focus on a particular type of birth environment. Rather, it describes two pathways - enhanced passage of the fetus through the pelvis and soft tissues, as well as decreased stress response - by which labour support may reduce the likelihood of operative birth and subsequent complications, and enhance women’s feelings of control and satisfaction with their childbirth experiences (Hodnett 2002a). Enhanced fetopelvic relationships may be accomplished by encouraging mobility and effective use of gravity, supporting women to assume their preferred positions and recommending specific positions for specific situations. Studies of the relationships among fear and anxiety, the stress response and pregnancy complications have shown that anxiety during labour is associated with high levels of the stress hormone epinephrine in the blood, which may in turn lead to abnormal fetal heart rate patterns in labour, decreased uterine contractility, a longer active labour phase with regular well-established contractions and low Apgar scores (Lederman 1978; Lederman 1981). Emotional support, information and advice, comfort measures and advocacy may reduce anxiety and fear and associated adverse effects during labour.
Continuous support has been viewed by some as a form of pain relief, specifically, as an alternative to epidural analgesia (Dickinson 2002), because of concerns about the deleterious effects of epidural analgesia, including on labour progress (Anim-Somuah 2011). Many labour and birth interventions routinely involve, or increase the likelihood of, co-interventions to monitor, prevent or treat adverse effects, in a “cascade of interventions”. Continuous, one-to-one support has the potential to limit this cascade and therefore, to have a broad range of different effects, in comparison to usual care. For example, if continuous support leads to reduced use of epidural analgesia, it may in turn involve less use of electronic fetal monitoring, intravenous drips, synthetic oxytocin, drugs to combat hypotension, bladder catheterisation, vacuum extraction or forceps, episiotomy and less morbidity associated with these, and may increase mobility during labour and spontaneous birth (Caton 2002).
A systematic review examining factors associated with women’s satisfaction with the childbirth experience suggests that continuous support can make a substantial contribution to this satisfaction. When women evaluate their experience, four factors predominate: the amount of support from caregivers, the quality of relationships with caregivers, being involved with decision-making and having high expectations or having experiences that exceed expectations (Hodnett 2002a).
Clarification of the effects of continuous support during labour, overall and within specific circumstances, is important in light of public and social policies and programs that encourage this type of care. For example, the Congress in Uruguay passed a law in 2001 decreeing that all women have the right to companionship during labour. In several low- and middle-income countries (including China, South Africa, Tanzania and Zimbabwe); the Better Births Initiative promotes labour companionship as a core element of care for improving maternal and infant health (WHO 2010). In many low-income countries, women are not permitted to have anyone with them during labour and birth. Efforts to change policies in these settings have led to questions about the effectiveness of support from husbands/partners or other support people of the woman’s own choosing, particularly in settings where the cost of paid companions would be prohibitive.
In North America, the services of women with special training in labour support have become available. Most commonly known as doula (a Greek word for ‘handmaiden’), this new member of the caregiver team may also be called a labour companion, birth companion, labour support specialist, labour assistant or birth assistant. A number of North American organisations offer doula training, certification and professional support; according to one estimate more than 50,000 people have received this training to date (P Simkin, personal communication). Some North American hospitals have begun to sponsor doula services. In recent national surveys of childbearing women in the United States, 3% to 5% of respondents indicated that they had used doula services during their most recent labours (Declercq 2002; Declercq 2006). An association for doulas has been established in the UK (McGinnis 2001). Maternal healthcare systems in dozens of high- and low- to middle-income countries throughout the world are developing new traditions for supportive female companionship during labour (Pascali-Bonaro 2010).
Questions have arisen about the ability of employees (such as nurses or midwives) to provide effective labour support, in the context of modern institutional birth environments (Hodnett 1997). For example, nurses and midwives often have simultaneous responsibility for more than one labouring woman, spend a large proportion of time managing technology and keeping records, and begin or end work shifts in the middle of women’s labours. They may lack labour support skills or may work in short-staffed environments.
Companions from a woman’s social network, such as husbands/partners and female relatives, usually have little experience in providing labour support and are themselves in need of support when with a loved one during labour and birth. As they are frequently available to assume the role, often without extra cost to families or health systems, it is important to understand their effectiveness as providers of continuous labour support.
In addition to questions about the impact of the type of provider of labour support, there are other questions about the effectiveness of support, including its impact under a variety of environmental conditions, and whether its effects are mediated by when continuous support begins (early versus active labour).
Childbearing women, policy-makers, payers of health services, health professionals and facilities and those who provide labour support all need evidence about the effects of continuous support, overall and under specific conditions.
OBJECTIVES
The primary objective was to assess the effects, on mothers and their babies, of continuous, one-to-one intrapartum support compared with usual care, in any setting. Secondary objectives were to determine whether the effects of continuous support are influenced by the following.
- Routine practices and policies in the birth environment that may affect a woman’s autonomy, freedom of movement and ability to cope with labour, including:
- policies about the presence of support people of the woman’s own choosing;
- epidural analgesia; and
- continuous electronic fetal monitoring.
- Whether the provider is:
- a member of the staff of the institution (and thus has additional loyalties or responsibilities);
- not a staff member but not part of the woman’s social network and present solely for the purpose of providing continuous support; or
- a person chosen by the woman from family members and friends.
Whether the continuous support begins early or later in labour.
METHODS
Criteria for considering studies for this review
Types of studies
All controlled trials comparing continuous labour support by either a familiar or unfamiliar person (with or without healthcare professional qualifications) with usual care, in which there was random allocation to treatment and control groups, were considered for inclusion in the review.
Types of participants
Pregnant women, in labour.
Types of interventions
The form of care that was evaluated was continuous presence and support during labour and birth. The person providing the support could have qualifications as a healthcare professional (nurse, midwife) or training as a doula or childbirth educator, or be a family member, spouse/partner, friend or stranger with little or no special training in labour support. The control group received usual care, as defined by the trialists. In all cases, ‘usual care’ did not involve continuous intrapartum support, but it could involve other measures, such as routine epidural analgesia, to help women to cope with labour.
Types of outcome measures
Theoretically, continuous support can have many diverse physiological and psychosocial effects (both short- and long-term), and therefore, a larger than usual number of outcomes were considered.
Primary outcomes
Mother
Any analgesia/anaesthesia (pain medication).
Synthetic oxytocin during labour.
Spontaneous vaginal birth.
Postpartum depression (defined using a pre-specified cutoff score on a validated instrument).
Negative rating of/negative feelings about the birth experience.
Baby
Admission to special care nursery.
Breastfeeding at one to two months postpartum.
Secondary outcomes
Labour events
Regional analgesia/anaesthesia.
Labour length
Severe labour pain (postpartum report).
Birth
Caesarean birth.
Instrumental vaginal birth.
Perineal trauma (defined as episiotomy or laceration requiring suturing).
Newborn
Low five-minute Apgar score (as defined by trial authors).
Prolonged newborn hospital stay.
Longer-term maternal outcomes
Difficulty mothering.
Low self-esteem in the postpartum period.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co-ordinator (30 June 2012).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co-ordinator and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE;
weekly searches of EMBASE;
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE and EMBASE, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co-ordinator searches the register for each review using the topic list rather than keywords.
We did not apply any language restrictions.
Data collection and analysis
For this update we assessed one new trial (Yuenyong 2012) and added ‘postpartum depression’ outcome data from one existing trial report (Hofmeyr 1991), using the following methods.
Selection of studies
For the current update, three review authors (E Hodnett, J Hofmeyr, C Sakala) independently assessed for inclusion all potentially eligible studies. Had any disagreement occurred, we would have resolved it through discussion or, if required, we would have consulted a third member of the review team.
Data extraction and management
We designed a form to extract data. For eligible studies, data were independently extracted by two people (either two review authors or an author and an assistant), using the agreed form. We resolved discrepancies through discussion. We entered data into Review Manager software (RevMan 2011) and checked for accuracy. When information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
For each study, at least two review authors independently assessed risk of bias, using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We would have resolved any disagreement by discussion or by involving a third assessor.
(1) Sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non-random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal the allocation sequence, and determined whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non-opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3) Blinding (checking for possible performance and detection bias)
We described for each included study the methods used, if any, to blind personnel from knowledge of which intervention a participant received. Since women and care providers cannot be blinded as to whether continuous support was given, we considered blinding adequate if outcomes were recorded by outcome assessors who had no knowledge of the woman’s group assignment. We judged studies at low risk of bias if they were blinded, or if we judged that the lack of blinding could not have affected the results. We assessed blinding separately for different outcomes or classes of outcomes.
(4) Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. To be included in the review, data on a given outcome had to be available for at least 80% of those who were originally randomised.
For outcomes collected post-hospital discharge, we recognise that follow-up, particularly in low-income countries, can be very difficult. Therefore, we included data if the response rate was higher than 75% and there was no obvious imbalance in groups. Where sufficient information was reported, or could be supplied by the trial authors, we planned to include missing data in the analyses. We assessed methods as:
low risk of bias;
high risk of bias;
unclear risk of bias.
(5) Selective reporting bias
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found. We assessed the methods as:
low risk of bias (where it is clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre-specified outcomes have been reported; one or more reported primary outcomes were not pre-specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other sources of bias
We planned to describe for each included study any important concerns we had about other possible sources of bias, including, for example, whether the trial was stopped early due to a data-dependent process, there was evidence of extreme baseline imbalance, or there had been claims of fraud.
We assessed whether each study was free of other problems that could put it at risk of bias:
low risk of other bias;
high risk of other bias;
unclear whether there is risk of other bias.
(7) Overall risk of bias
We made explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses - see Sensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
All but one pre-specified outcome involved dichotomous data. For labour length, we used the mean difference because it was measured in the same way in the trials.
Unit of analysis issues
Cluster-randomised trials
Had we found cluster-randomised trials, we would have included them in the analyses along with individually-randomised trials. Our plan was as follows: we would adjust their sample sizes or standard errors using the methods described in the Handbook (Section 16.3.4 or 16.3.6) using an estimate of the intracluster correlation co-efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we had used ICCs from other sources, we planned to report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. In future updates of this review, if we identify both cluster-randomised trials and individually-randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely. We will also acknowledge heterogeneity in the randomisation unit and perform a separate meta-analysis.
Dealing with missing data
For included studies, we noted levels of attrition. We included data for a given outcome which occurred prior to hospital discharge only if the data were available for at least 80% of those originally randomised. For outcomes collected post-hospital discharge we included data if the response rate was higher than 75% and there was no obvious imbalance in groups.
For all outcomes we have carried out analyses, as far as possible, on an intention-to-treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta-analysis using the T2, I2 and Chi2 statistics. We regarded heterogeneity as substantial if the T2 was greater than zero and either the I2 was greater than 30% or there was a low P value (less than 0.10) in the Chi2 test for heterogeneity. In such cases we took the following steps:
a sensitivity analysis, in which methodological weak trials were removed from the analyses and results compared for the primary outcomes;
visual inspection of the forest plots for evidence of inconsistency in results; and
comparison of the results of fixed-effect and random-effects analyses.
Assessment of reporting biases
Had we suspected reporting bias, we would have attempted to contact study authors asking them to provide missing outcome data. If this were not possible, and the missing data were thought to introduce serious bias, we would not have included the outcome data from that trial.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2011). We used fixed-effect Mantel-Haenszel meta-analysis for combining data in the absence of heterogeneity, and random-effects analysis if substantial heterogeneity was detected and we considered that combining trials was meaningful. We defined heterogeneity as substantial if a given meta-analysis resulted in an I2 value greater than 30%, and there was inconsistency among trials in the direction or magnitude of effects (judged visually in the forest plot), or a low (less than 0.10) P value in the Chi2 test for heterogeneity.
Subgroup analysis and investigation of heterogeneity
We planned the following subgroup analyses.
A) Three subgroup analyses that concern characteristics of the childbirth environment
Trials in settings in which women were permitted to be accompanied by one or more support persons of their own choosing compared with trials in which accompaniment was not permitted.
Trials conducted in settings in which epidural analgesia was available compared with trials in settings in which it was unavailable.
Trials in which there was a policy of routine electronic fetal heart rate monitoring compared with trials in settings in which continuous electronic fetal monitoring was not routine.
(B) One subgroup analysis that concerns characteristics of the providers of labour support
Trials in which the caregivers were employees of the institution, compared with trials in which the caregivers were not employees and were not members of the woman’s social network, compared with trials in which the providers were not employees and were lay people chosen by the participants (e.g. husband/partner, friend, close relative).
(C) One subgroup analysis that concerns differences in the timing of onset of continuous support
Trials in which continuous labour support began prior to or during early labour (as defined by trial authors), compared with trials in which continuous support began in active labour.
Because few of the trial reports contained all of the information needed for the above subgroup analyses, we contacted the trial authors in an attempt to verify the presence/absence of routine electronic fetal monitoring (EFM), the presence/absence of epidural analgesia and timing of onset of continuous support. We excluded some studies included in the primary comparisons from the subgroup analyses concerning the use of EFM because their status regarding EFM use was unknown. For tests of differences between these subgroups, we recalculated the overall analysis by including only the studies in which EFM use was known.
The seven primary outcomes and one secondary outcome were used in the subgroup analyses. While normally, subgroup analyses are restricted to primary outcomes, we also included the outcome of caesarean delivery, because there is widespread concern about escalating caesarean rates worldwide, and subgroup analyses could be helpful to policy makers in decisions about the provision of continuous labour support. Thus the outcomes in the subgroup analyses were: any analgesia/anaesthesia, synthetic oxytocin during labour, spontaneous vaginal birth, caesarean birth, postpartum depression, negative ratings of the birth experience, admission to special care nursery, and breastfeeding at one to two months postpartum.
When I2 levels were high but the amount of heterogeneity in treatment effects was low (as happens when there are a large number of big trials and thus the amount of variation due to sampling error is extremely low), we compared the results of random-effects and fixed-effect analyses. In instances in which the conclusions were not materially different in both methods of analysis, we reported the results of fixed-effect, inverse variance meta-analysis, in order to be able to calculate a Chi2 for the purpose of exploring differences based on pre-specified subgroups. As a consequence the totals in the subgroup analysis tables are sometimes slightly different from those in the main comparison, since the main comparisons used the Mantel-Haenszel rather than the inverse variance method.
Sensitivity analysis
We performed sensitivity analyses, for the primary outcomes, in instances in which there was a high risk of bias associated with the quality of included trials.
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; Characteristics of ongoing studies.
Included studies
Please see Characteristics of included studies table. While 23 trials met the inclusion criteria, one trial (Thomassen 2003) provided no usable outcome data. We do not describe it here, but provide details in the Characteristics of included studies table.
All 22 trials (n = 15,288) that provided usable outcome data were conducted in hospitals. The trials were conducted in Australia, Belgium, Botswana, Brazil, Canada, Chile, Finland, France, Greece, Guatemala, Mexico, Nigeria, South Africa, Sweden, Thailand, and the United States, under widely disparate hospital conditions, regulations and routines. There was remarkable consistency in the descriptions of continuous support across all trials. In all instances the intervention included continuous or nearly continuous presence, at least during active labour. Twenty of the 22 trials that provided usable outcome data (all except Cogan 1988 and Dickinson 2002) also included specific mention of comforting touch and words of praise and encouragement.
In 11 trials (Breart - Belgium 1992; Breart - France 1992; Campbell 2006; Cogan 1988; Dickinson 2002; Gagnon 1997; Hemminki 1990a; Hemminki 1990b; Hodnett 1989; Hodnett 2002; McGrath 2008), hospital policy permitted women to be accompanied by their husbands/partners or other family members during labour, while in the other 11 trials, no additional support people were allowed. Epidural analgesia was not routinely available in seven trials (Breart - Greece 1992; Hofmeyr 1991; Kashanian 2010; Klaus 1986; Madi 1999; Morhason-Bello 2009; Yuenyong 2012). We were unsuccessful in obtaining information about the availability of epidural analgesia in one trial (Cogan 1988). Epidural analgesia was routinely available in the other 14 trials. Electronic fetal heart rate monitoring was not routine in eight trials (Bruggemann 2007; Hofmeyr 1991; Kashanian 2010; Klaus 1986; Langer 1998; Madi 1999; Morhason-Bello 2009; Yuenyong 2012). In nine trials (Campbell 2006; Dickinson 2002; Gagnon 1997; Hemminki 1990a; Hemminki 1990b; Hodnett 1989; Hodnett 2002; Kennell 1991; McGrath 2008) electronic fetal monitoring was used routinely. We were unsuccessful in obtaining information about the use of electronic fetal monitoring in five trials (Breart - Greece 1992; Breart - Belgium 1992; Breart - France 1992; Cogan 1988; Torres 1999).
It was not possible to categorise most of the trials according to the pre-specified subgroups of early versus active labour. In four trials (Cogan 1988; Hodnett 1989; Klaus 1986; Madi 1999), the support began in early labour. In the other 17 trials, the timing of onset of support was much more heterogenous, as were definitions of early and active labour, in instances in which these were defined. Women were in varying phases of labour, from elective induction to active labour.
In addition, the persons providing the support intervention varied in their experience, qualifications and relationship to the labouring women. In nine trials (Breart - Belgium 1992; Breart - France 1992; Breart - Greece 1992; Dickinson 2002; Gagnon 1997; Hemminki 1990a; Hemminki 1990b; Hodnett 2002; Kashanian 2010), the support was provided by a member of the hospital staff, for example, a midwife, student midwife or nurse. In seven trials the providers were not members of the hospital staff and were not part of the woman’s social network; they were women with or without special training, such as doulas or women who had given birth before (Hodnett 1989; Hofmeyr 1991; Kennell 1991; Klaus 1986; McGrath 1999): a childbirth educator (Cogan 1988), or retired nurses (Langer 1998). In six trials they were companions of the woman’s choice from her social network, with or without brief training -- a female relative or friend or the woman’s husband/partner (Bruggemann 2007; Campbell 2006; Madi 1999; Morhason-Bello 2009; Torres 1999; Yuenyong 2012).
Excluded studies
Sixteen trials were excluded altogether (Bender 1968; Bochain 2000; Brown 2007; Dalal 2006; Gordon 1999; Hemminki 1990c; Lindow 1998; McGrath 1999; Orenstein 1998; Pinheiro 1996; Ran 2005; Scott 1999; Sosa 1980; Trueba 2000; Tryon 1966; Zhang 1996). Seven trials were excluded as they were not randomised trials (Bender 1968; Dalal 2006; Ran 2005; Scott 1999; Sosa 1980; Trueba 2000; Tryon 1966). Five trials were excluded because the intervention was not continuous support (Bochain 2000; Brown 2007; Lindow 1998; Orenstein 1998; Zhang 1996). Two trials reported as abstracts provided insufficient information in order to assess eligibility (McGrath 1999; Pinheiro 1996). Two further trials were excluded because they did not provide any usable data (Gordon 1999; Hemminki 1990c). Please refer to table Characteristics of excluded studies for details.
Risk of bias in included studies
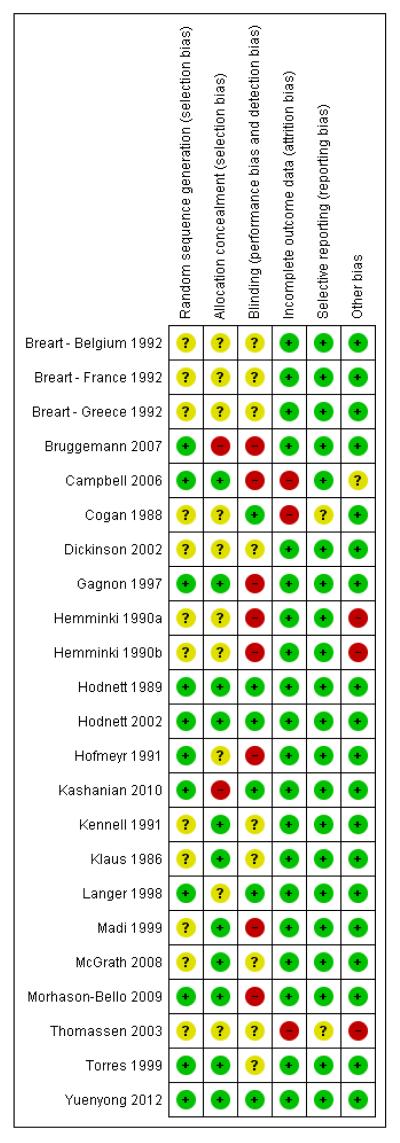
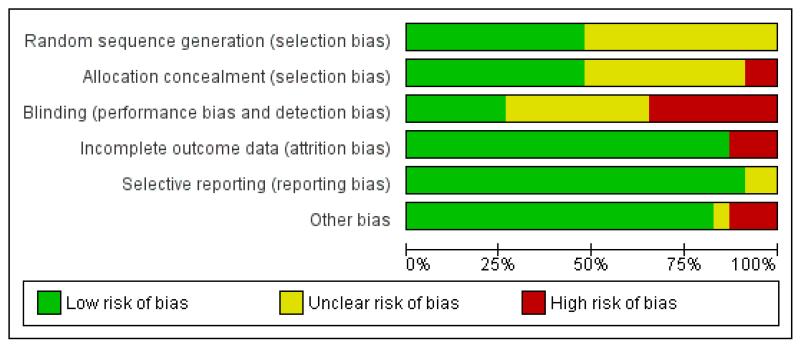
The trials were of generally good quality (Figure 1; Figure 2).
Figure 1.
Methodological quality summary: review authors’ judgements about each methodological quality item for each included study.
Figure 2.
Methodological quality graph: review authors’ judgements about each methodological quality item presented as percentages across all included studies
Allocation
Random sequence generation: Twelve trials were at unclear risk of bias (Breart - Belgium 1992; Breart - France 1992; Breart -Greece 1992; Cogan 1988; Dickinson 2002; Hemminki 1990a; Hemminki 1990b; Kennell 1991; Klaus 1986; Madi 1999; McGrath 2008; Thomassen 2003) because they did not describe the method of random assignment. Eleven trials described using a computer random number generator or referred to a random number table (Bruggemann 2007; Campbell 2006; Gagnon 1997; Hodnett 1989; Hodnett 2002; Hofmeyr 1991; Kashanian 2010; Langer 1998; Morhason-Bello 2009; Torres 1999; Yuenyong 2012) and were assessed as low risk of bias.
Allocation concealment: The risk of selection bias was high in two small trials (Bruggemann 2007; Kashanian 2010). In Bruggemann 2007, women picked their treatment allocation from an opaque container. In 11 trials (Campbell 2006; Gagnon 1997; Hodnett 1989; Hodnett 2002; Kennell 1991; Klaus 1986; Madi 1999; McGrath 2008; Morhason-Bello 2009; Torres 1999; Yuenyong 2012), risk of selection bias was low with allocation described as either using central allocation, e.g. Hodnett 2002 used a central, computerised randomisation service accessed by telephone or other trials described using sequentially numbered, opaque, sealed envelopes. In the remaining trials (Breart - Belgium 1992; Breart - France 1992; Breart - Greece 1992; Cogan 1988; Dickinson 2002; Hemminki 1990a; Hemminki 1990b; Hofmeyr 1991; Langer 1998; Thomassen 2003), risk of selection bias was unclear, e.g. one trial used methods that were centrally controlled but not concealed (Cogan 1988).
Blinding
Performance bias: neither those providing nor receiving care could be blinded to the presence/absence of a person providing continuous support. Hodnett 2002 provided evidence to discount contamination and co-intervention as serious threats to validity. In eight trials group assignment was known and no attempt to blind outcome assessment was apparent and so these were assessed as being at high risk of bias (Bruggemann 2007; Campbell 2006; Gagnon 1997; Hemminki 1990a; Hemminki 1990b; Hofmeyr 1991; Madi 1999; Morhason-Bello 2009).
Detection bias: in the trials which sought participants’ evaluations of their birth experiences, efforts were made to reduce response bias, through use of an interviewer blinded to the woman’s group allocation or self-administered questionnaires. Six trials were assessed as being at low risk of bias because some blinding of outcome assessment was performed (Cogan 1988; Hodnett 1989; Hodnett 2002; Kashanian 2010; Langer 1998; Yuenyong 2012). In the remaining trials, risk of bias for blinding (performance and detection bias) was unclear (Breart - Belgium 1992; Breart - France 1992; Breart - Greece 1992; Dickinson 2002; Kennell 1991; Klaus 1986; McGrath 2008; Thomassen 2003; Torres 1999).
Incomplete outcome data
Attrition bias: we did not include data for outcomes assessed in hospital in a comparison if there was more than 20% loss to follow-up; we did not include longer-term outcome data if there was more than 25% loss to follow-up. Based on these criteria, one trial (Thomassen 2003) provided no usable outcome data. Two trials further trials were assessed as being at high risk of bias for attrition bias (Campbell 2006; Cogan 1988).
Selective reporting
All outcomes appear to have been reported upon in the majority of trials. In two trials, it was unclear whether selective reporting had taken place (Cogan 1988; Thomassen 2003).
Other potential sources of bias
Three trials were assessed as being at high risk of other bias: in two trials the mothers had been told the purpose of the study differentially (Hemminki 1990a; Hemminki 1990b) and one trial was stopped early for ‘a range of largely organizational issues’ when only a quarter of the original sample size had been enrolled (Thomassen 2003). Risk of bias was unclear in one study (Campbell 2006) and no other sources of bias were apparent in the remaining trials.
Effects of interventions
Main comparison: continuous support versus usual care - all trials
We considered 17 outcomes. Between one and 22 trials contributed to the analyses of each outcome. Sensitivity analyses, conducted by removing the trials (all of which were small) with a high likelihood of selection bias (Bruggemann 2007; Hodnett 1989; Kashanian 2010) did not alter the conclusions. According to our pre-specified criteria, there was statistical heterogeneity in all but three outcomes (instrumental vaginal birth, low five-minute Apgar score, and low postpartum self-esteem). Inspection of the forest plots did not suggest sources of heterogeneity. For the two outcomes postpartum depression and difficulty mothering, this statistical heterogeneity confirmed our conclusion that based on clinical heterogeneity a summary statistic would not yield meaningful results (discussed further below). In all instances in which summary statistics are reported, the comparisons of fixed-effect and random-effects analyses did not yield substantive differences, nor alter conclusions. We report the results of fixed-effect analyses for instrumental vaginal birth, low five-minute Apgar score, and low postpartum self-esteem (the latter only contained one trial), and random-effects analyses for all other outcomes in which summary statistics were computed.
Primary outcomes
Women who had continuous, one-to-one support during labour were:
more likely to have
a spontaneous vaginal birth (19 trials, n = 14,119, average risk ratio (RR) 1.08, 95% confidence interval (CI) 1.04 to 1.12, I2 45%, ⊺ 2 0.00), Analysis 1.5;
less likely to have
any intrapartum analgesia/anaesthesia (14 trials, n = 12,283, average RR 0.90, 95% CI 0.84 to 0.96, I2 75%, ⊺ 2 0.01), Analysis 1.1;
reported negative rating of/negative feelings about childbirth experience (11 trials, n = 11,133, average RR 0.69, 95% CI 0.59 to 0.79, I2 63%, ⊺ 2 0.03), Analysis 1.13; and there was no apparent impact of continuous support on
use of synthetic oxytocin during labour (15 trials, n = 12,620, average RR 0.97, 95% CI 0.91 to 1.04, I2 65%, ⊺ 2 0.01), Analysis 1.3;
admission to the special care nursery (seven trials; n = 8897, average RR 0.97, 95% CI 0.76 to 1.25, I2 37%, ⊺ 2 0.03), Analysis 1.10;
breastfeeding at one to two months postpartum (three trials, n = 5363, average RR 1.01, 95% CI 0.94 to 1.09, I2 52%, ⊺ 2 0.00), Analysis 1.15;
and evidence of postpartum depression was a reported outcome in just two trials (Hodnett 2002; Hofmeyr 1991). Hodnett 2002 used the Edinburgh Postnatal Depression Inventory and reported the frequencies of scores greater than 12. Hofmeyr 1991 used the Pitt Depression Inventory and reported scores indicating mild (less than 20), moderate (20 to 34), and severe (greater than 34) depressive symptomatology. We combined the frequencies of moderate and severe depressive symptomatology, since Pitt scores greater than 19 have been considered indicative of postpartum depression (Avan 2010). The two trials were widely disparate in populations, the hospital conditions within which they were conducted, and the type of support provider. We concluded that combining them would not yield meaningful information. In both trials the direction of effect was the same. In Hofmeyr 1991, eight of 74 women in the group receiving continuous support had depressive symptomatology compared to 44 of 75 women in the control group; RR 0.18, 95% CI 0.09 to 0.36. In Hodnett 2002, 245 out of 2816 in the supported group had depressive symptomatology, compared to 277 out of 2751 in the control group; RR 0.86, 95% CI 0.73 to 1.02.
Secondary outcomes
Women who had continuous, one-to-one support were: more likely to have
shorter labours (12 trials, n = 5366, mean difference (MD) −0.58 hours, 95% CI −0.85 to −0.31, I2 45%, ⊺ 2 0.08), Analysis 1.4;
less likely to have
regional analgesia/anaesthesia (nine trials, n = 11,444, average RR 0.93, 95% CI 0.88 to 0.99, I2 81%, ⊺ 2 0.01), Analysis 1.2;
an instrumental vaginal birth (19 trials, n = 14,118, RR 0.90, 95% CI 0.85 to 0.96, fixed-effect), Analysis 1.6;
a caesarean birth (22 trials, n = 15,175, average RR 0.78, 95% CI 0.67 to 0.91, I2 53%, ⊺ 2 0.05), Analysis 1.7;
a baby with a low five-minute Apgar score (13 trials, n = 12,515, RR 0.69, 95% CI 0.50 to 0.95, fixed-effect), Analysis 1.9;
and there was no apparent impact of continuous labour support on
the likelihood of serious perineal trauma (four trials, n = 8120, average RR 0.97, 95% CI 0.92 to 1.01, I2 44%, ⊺ 2 0.00), Analysis 1.8;
severe labour pain (four trials; n = 2456, average RR 1.00, 95% CI 0.83 to 1.21, I2 78%, ⊺ 2 0.03), Analysis 1.12;
low postpartum self-esteem (one trial, n = 652, RR 1.00, 95% CI 0.77 to 1.30, fixed-effect), Analysis 1.17; and
prolonged neonatal hospital stay (three trials, n = 1098, average RR 0.83, 95% CI 0.42 to 1.65, I2 62%, ⊺ 2 0.15), Analysis 1.11.
Three trials reported results related to difficulty in mothering (Campbell 2006; Hofmeyr 1991; Hodnett 2002). As was the case with postpartum depression, the trials were widely disparate in populations, the hospital conditions within which they were conducted, and the type of support provider, and the forest plot supported our conclusion that combining them would not yield meaningful information. In Hofmeyr 1991, 41 out of 75 in the continuous support group reported difficulty mothering, compared to 67 out of 75 in the control group; RR 0.61, 95% CI 0.49, 0.76. In Hodnett 2002, 873 out of 2836 in the continuous support group reported difficulty mothering, compared to 853 out of 2765 in the control group; RR 1.00, 95% CI 0.92, 1.08. In Campbell 2006, 11 out of 292 in the continuous support group reported difficulty mothering, compared to 38 out of 265 in the control group; RR 0.26, 95% CI 0.14, 0.50.
Subgroup comparisons
We grouped the trials according to the following provider characteristics: 1) staff members of the hospital; 2) neither hospital employees nor part of the woman’s social network; and 3) chosen by the woman from her social network.
We have presented the results of the subgroup analyses below. While we made every effort to obtain the required information from trial authors, none of the subgroup comparisons are based on the total number of included trials for which usable data were available. Thus results must be interpreted with caution. The text below does not present the results for postpartum depression or breast-feeding at one to two months postpartum, because too few trials provided data. Only two trials contributed data about postpartum depression (Hodnett 2002; Hofmeyr 1991) and three about breastfeeding (Hodnett 2002; Hofmeyr 1991; Langer 1998).
We were unable to conduct the planned subgroup comparison based on timing of onset of labour support. It was not possible to categorise most of the trials according to the pre-specified subgroups of early versus active labour. In four trials (Cogan 1988; Hodnett 1989; Klaus 1986; Madi 1999), the support began in early labour. In the other 18 trials, both the definitions of early and active labour and the timing of onset of support were much more heterogenous, in instances in which they were defined. Women were in varying phases of labour, from elective induction to active labour.
As noted in Subgroup analysis and investigation of heterogeneity, totals in the subgroup analysis figures may differ slightly from those in the main comparisons, because a different method of analysis had to be used. All subgroup comparisons used fixed-effect, to allow computation of tests for differences between subgroups.
Outcome: any intrapartum analgesia/anaesthesia
Policies about the presence of companions during labour and birth: In seven trials (n = 9752) companions were permitted; RR 0.97, 95% CI 0.96 to 0.99, while in seven trials (n = 2598) companions were not permitted; RR 0.91, 95% CI 0.85 to 0.96. Chi2 for the subgroup comparison = 5.12, P = 0.02, Analysis 2.1.
Availability of epidural analgesia: In nine trials (n = 10,888), epidural analgesia was routinely available; RR 0.97, 95% CI 0.96 to 0.98. In five trials (n = 1462) epidural analgesia was not routinely available; RR 0.83, 95% CI 0.69 to 0.99. Chi2 for the subgroup comparison = 3.08, P = 0.08, Analysis 3.1.
Routine use of electronic fetal monitoring (EFM): in six trials (n = 8580), EFM was routine; RR 0.97, 95% CI 0.96 to 0.99. In six trials (n = 2186), EFM was not routine; RR 0.96, 95% CI 0.90 to 1.02. In two trials (n = 1579), the policy about routine EFM was unknown; RR 0.89, 95% CI 0.80 to 0.99. Chi2 for the subgroup comparison = 2.32, P = 0.31, Analysis 4.1.
Provider characteristics: in six trials (n = 9152) the support was provided by a member of the hospital staff; RR 0.97, 95% CI 0.96 to 0.99. In four trials (n = 1790), the support was provided by a woman who was not a member of the staff and was not part of the woman’s social network; RR 0.91, 95% CI 0.86 to 0.97. In four trials (n = 1408) the support was provided by a member of the woman’s social network; RR 0.94, 95% CI 0.88 to 1.00. Chi2 for the subgroup comparison = 4.84, P = 0.09, Analysis 5.1. Thus, the effects of continuous support on use of any intrapartum analgesia/anaesthesia appeared to be stronger in settings where companions were not permitted, but did not appear to be influenced by the availability of epidural analgesia, the use of routine EFM, or provider characteristics.
Outcome: synthetic oxytocin during labour
Policies about the presence of companions: in five trials (n = 9495) companions were permitted; RR 1.04, 95% CI 0.99 to 1.10. In 10 trials (n = 3125) companions were not permitted; RR 0.99, 95% CI 0.97 to 1.02. Chi2 for the subgroup comparison = 3.13, P = 0.08, Analysis 2.2.
Availability of epidural analgesia: in eight trials (n = 10,568) epidural analgesia was routinely available; RR 1.00, 95% CI 0.98 to 1.02. In seven trials (n = 2066), epidural analgesia was not routinely available; RR 1.02, 95% CI 0.93 to 1.11. Chi2 for the subgroup comparison = 0.24, P = 0.63, Analysis 3.2.
Use of routine EFM: in four trials (n = 8340) EFM was routine; RR 1.04, 95% CI 0.98 to 1.11. In seven trials (n = 1726) EFM was not routine; RR 0.99, 95% CI 0.96 to 1.01. In four trials (n = 2568) it is not known whether EFM was routine; RR 1.02, 95% CI 0.97 to 1.08. Chi2 for the subgroup comparison = 3.27, P = 0.19, Analysis 4.2.
Provider characteristics: in six trials (n = 9561), the support was provided by a member of the hospital staff; RR 1.06, 95% CI 1.01 to 1.11. In three trials (n = 1018), the support was provided by a woman who was not a member of the staff and was not part of the woman’s social network; RR 0.69, 95% CI 0.50 to 0.94. In six trials (n = 2041), the support was provided by a member of the woman’s social network; RR 0.99, 95% CI 0.96 to 1.01. Chi2 for the subgroup comparison = 11.46, P = 0.003, Analysis 5.2.
Thus the effects of continuous support on use of synthetic oxytocin during labour did not appear to be influenced by policies about the presence of companions, use of routine EFM, or availability of epidural analgesia. The effectiveness of continuous support in reducing the likelihood of intrapartum oxytocin seemed to be strongest when the provider was neither a staff member nor part of the woman’s social network.
Outcome: spontaneous vaginal birth
Policies about companions: In nine trials (n = 10,889) companions were permitted; RR 1.03, 95% CI 1.00 to 1.05. In ten trials (n = 3329) companions were not permitted; RR1.11, 95% CI 1.07 to 1.16. Chi2 for the subgroup comparison = 11.82, P < 0.001, Analysis 2.3.
Availability of epidural analgesia: In 13 trials (n = 12,672), epidural analgesia was routinely available; RR 1.04, 95% CI 1.01 to 1.06). In six trials (n = 1546) epidural analgesia was not routinely available; RR 1.11, 95% CI 1.06 to 1.17. Chi2 for the subgroup comparison = 6.59, P = 0.01, Analysis 3.3.
Routine use of EFM: In eight trials (n = 9717) EFM was routine; RR 1.03, 95% CI 1.01 to 1.06. In seven trials (n = 1913) EFM was not routine; RR 1.11, 95% CI 1.06 to 1.17. In four trials (n = 2561), the policy about routine EFM is not known; RR 1.07, 95% CI 1.01 to 1.13. Chi2 for the subgroup comparison = 8.56, P = 0.01, Analysis 4.3.
Provider characteristics: in nine trials (n = 10,813) the support was provided by a member of the hospital staff; RR 1.03, 95% CI 1.01 to 1.06. In five trials (n = 1935) the support was provided by a woman who was not part of the hospital staff nor part of the woman’s social network; RR 1.12, 95% CI 1.07 to 1.17. In five trials (n = 1470), the support was provided by a member of the woman’s social network; RR 1.07, 95% CI 0.99 to 1.15. Chi2 for the subgroup comparison = 9.97, P = 0.007, Analysis 5.3.
Thus the effectiveness of continuous support in increasing the likelihood of spontaneous vaginal birth appeared to be stronger when hospital policies did not permit companions, when epidural analgesia was not available, when EFM was not routine, and when the support provider was neither a staff member nor part of the woman’s social network.
Outcome: caesarean birth
Policies about companions: in 11 trials (n = 11,326) companions were permitted; RR 0.94, 95% CI 0.85 to 1.03. In 11 trials (n = 3849) companions were not permitted; RR 0.75, 95% CI 0.65 to 0.86. Chi2 for the subgroup comparison = 6.46, P = 0.01, Analysis 2.4.
Availability of epidural analgesia: in 14 trials (n = 13,064), epidural analgesia was routinely available; RR 0.93, 95% CI 0.86 to 1.02. In seven trials (n = 2077), epidural analgesia was not routinely available; RR 0.54, 95% CI 0.43 to 0.68. In one very small trial (n = 34), we were unable to determine if epidural analgesia was routinely available; RR 1.40, 95% CI 0.14 to 13.98. Chi2 for the subgroup comparison = 19.30, P < 0.0001,Analysis 3.4.
Routine use of EFM: in nine trials (n = 10,123), EFM was routine; RR 0.92, 95% CI 0.83 to 1.01. In eight trials (n = 2457) EFM was not routine; RR 0.66, 95% CI 0.55 to 0.79. In five trials (n = 2595), it is not known whether EFM was routine; RR 1.06, 95% CI 0.84 to 1.33. Chi2 for the subgroup comparison = 12.78, P = 0.002, Analysis 4.4.
Provider characteristics: in nine trials (n = 10,786), the support was provided by a member of the hospital staff; RR 0.95, 95% CI 0.85 to1.05. In seven trials (n = 2330), the support was provided by a woman who was not a member of the hospital staff and not part of the woman’s social network; RR 0.72, 95% CI 0.60 to 0.86. In six trials (n = 2059), the support was provided by a member of the woman’s social network; RR 0.83, 95% CI 0.69 to 1.01. Chi2 for the subgroup comparison = 6.88, P = 0.03, Analysis 5.4.
Thus the effectiveness of continuous support in reducing the likelihood of caesarean birth appeared to be stronger in settings where companions were not permitted, epidural analgesia was not routinely available and EFM was not routine, and when the provider was neither a staff member nor part of the woman’s social network.
Outcome: admission to special care nursery
Policies about companions: in two trials (n = 7328), companions were permitted; RR 0.99, 95% CI 0.84 to 1.17. In five trials (n = 1569), companions were not permitted; RR 0.91, 95% CI 0.71 to 1.17. Chi2 for the subgroup comparison = 0.28, P = 0.60, Analysis 2.5.
Availability of epidural analgesia: in five trials (n = 8380) epidural analgesia was routinely available; RR 0.98, 95% CI 0.85 to 1.13. In two trials (n = 517) epidural analgesia was not routinely available; RR 0.26, 95% CI 0.08 to 0.88. Chi2 for the subgroup comparison = 4.51, P = 0.03, Analysis 3.5.
Routine use of EFM: in three trials (n = 7740) EFM was routine; RR 0.97, 95% CI 0.84 to 1.11. In three trials (n = 729) EFM was not routine; RR 0.48, 95% CI 0.21 to 1.12. In one trial (n = 428), it is not known whether EFM was routine; RR 1.98, 95% CI 0.76 to 5.18. Chi2 for the subgroup comparison = 4.76, P = 0.09, Analysis 4.5.
Provider characteristics: in three trials (n = 7428), the support was provided by a member of the hospital staff; RR 0.99, 95% CI 0.84, 1.17. In two trials (n = 829), the support was provided by a woman who was not a member of the hospital staff and not part of the woman’s social network; RR 0.86, 95% CI 0.66 to 1.12. In two trials (n = 640) the support was provided by a member of the woman’s social network; RR 1.40, 95% CI 0.67 to 2.93. Chi2 for the subgroup comparison = 1.74, P = 0.42, Analysis 5.5.
Thus the effectiveness of continuous support in reducing the likelihood of admission of the newborn to a special care nursery appeared to be stronger in settings in which epidural analgesia was not routinely available, but effectiveness did not appear to be influenced by policies about companions or routine EFM, or by provider characteristics.
Outcome: negatives ratings of/negative views about the birth experience
Policies about companions: in five trials (n = 8639) companions were permitted; RR 0.70, 95% CI 0.62 to 0.78. In six trials (n = 2539) companions were not permitted; RR 0.62, 95%CI 0.56 to 0.69. Chi2 for the subgroup comparison = 2.03, P = 0.15, Analysis 2.7.
Availability of epidural analgesia: in nine trials (n = 10,404) epidural analgesia was routinely available; RR 0.70, 95% CI 0.64 to 0.77. In two trials (n = 774) epidural analgesia was not routinely available; RR 0.55, 95% CI 0.48 to 0.63. Chi2 for the subgroup comparison = 7.92, P 0.0005, Analysis 3.7.
Routine use of EFM: four trials (n = 7467) were conducted in settings with routine EFM; RR 0.67, 95% CI 0.60 to 0.76. Four trials (n = 1710) were conducted in settings in which EFM was not routine; RR 0.60, 95% CI 0.53 to 0.68. Three trials (n = 1977) were in settings in which the use of routine EFM is not known; RR 0.84, 95% CI 0.65 to 1.08. Chi2 for the subgroup comparison = 5.55, P = 0.06, Analysis 4.7.
Provider characteristics: in four trials (n = 8145) support providers were hospital staff; RR 0.87, 95% CI 0.73 to 1.03. In three trials (n = 1325) the providers were not hospital staff and not part of the woman’s social network; RR 0.66, 95% CI 0.57 to 0.77. In four trials (n = 1708), providers were part of the woman’s social network; RR 0.57, 95% CI 0.51 to 0.64. Chi2 for the subgroup comparison = 16.47, P = 0.0003, Analysis 5.7. Thus the effectiveness of continuous support in reducing the likelihood of dissatisfaction with or negative views of the childbirth experience appeared to be stronger in settings in which epidural analgesia was not routinely available, and when the provider was neither a staff member nor part of the woman’s social network.
DISCUSSION
This review summarises results of 22 trials involving 15,288 women, conducted in 16 countries under a wide variety of circumstances. Continuous one-to-one support was given by providers with a variety of experiences, through having given birth themselves and/or through education and practice as nurses, midwives, doulas or childbirth educators, or by the woman’s husband or partner, female relative or close friend. The methodological quality of the trials was generally good to excellent. For all outcomes in which summary statistics were computed, comparisons of fixed-effect and random-effects analyses did not yield material differences in the results. Thus neither the risk of bias nor heterogeneity should be of concern when interpreting results.
In the primary comparison, women who were allocated to continuous one-to-one support were more likely to have a spontaneous vaginal birth (risk ratio (RR) 1.08, 95% confidence interval (CI) 1.04 to 1.12) and less likely to have intrapartum analgesia (RR 0.90, 95% CI 0.84 to 0.96) or to report dissatisfaction (RR 0.69, 95% CI 0.59 to 0.79). In addition their labours were shorter (mean difference (MD) −0.58 hours, 95% CI −0.85 to −0.31), they were less likely to have a caesarean (RR 0.78, 95% CI 0.67 to 0.91) or instrumental vaginal birth (RR 0.90, 95% CI 0.85 to 0.96), regional analgesia (RR 0.93, 95% CI 0.88 to 0.99), or a baby with a low five-minute Apgar score (RR 0.69, 95% CI 0.50 to 0.95). The trial reports do not list any adverse effects. This form of care appears to confer important benefits without attendant risks. The results of earlier versions of this review prompted organisations in Canada, the UK and the USA to issue practice guidelines, advocating continuous support (AWHONN 2002; MIDIRS 1999; NICE Intrapartum Care 2007; SOGC 1995). The results of the primary comparison in the current review offer continued justification for such practice guidelines.
The subgroup analyses should be interpreted with caution. Individually each should be considered exploratory and hypothesis-generating, particularly when the sample size in one subgroup was much smaller than in another. However, taken in their totality, the consistency of the patterns suggests that the effectiveness of continuous intrapartum support may be enhanced or reduced by policies and practices in the birth setting and by the nature of the relationship between the provider and labouring woman.
We chose three aspects of the birth environment - routine use of electronic fetal monitoring (EFM), availability of epidural analgesia and policies about the presence of additional support people of the woman’s own choosing - as proxies for environmental conditions that may mediate the effectiveness of labour support. This review cannot answer questions about the mechanisms whereby settings with epidural analgesia limit the effectiveness of labour support. The impact of epidural analgesia may be direct (Anim-Somuah 2011) or indirect, as part of the ‘cascade of interventions’ described in the Background. The effects of a policy of routine EFM are less clear, most likely because we were unable to obtain information about EFM policies for several of the trials. However, continuous labour support in settings without routine EFM was associated with greater likelihood of spontaneous vaginal birth and lower likelihood of a caesarean birth. These results raise questions about the ability of labour support to act as a buffer against adverse aspects of routine medical interventions. Labour support appears to be effective in reducing the adverse consequences of the fear and distress associated with labouring alone in an unfamiliar environment. A report of a qualitative component of one of the included trials (Langer 1998), aptly titled “Alone, I wouldn’t have known what to do”, provides further justification for this argument.
Effects of continuous labour support appear to vary by provider characteristics. Divided loyalties, additional duties besides labour support, self-selection and the constraints of institutional policies and routine practices may all have played a role in the apparently limited effectiveness of members of the hospital staff. Childbirth environments influence the healthcare professionals who work in them as well as labouring women and their support people. Furthermore, while women want and benefit from the presence of selected members of their social network, the support of partners and others with whom they have a longstanding relationship is qualitatively different and more complex than that of a woman who is experienced and often trained to provide labour support and who has no other role other than to provide it. An early trial of labour support with partners present found that women received more support from their partners when a doula was present to guide them, and the partners themselves reported more support (Hodnett 1989). While continuous labour support appears to be more effective when it is provided by caregivers who are not employees of an institution (and thus have no obligation to anyone other than the labouring woman) and who have an exclusive focus on this task, support from a member of the woman’s social network is effective in improving women’s satisfaction with their birth experiences.
There remains relatively little information about the effects of continuous intrapartum support on mothers’ and babies’ health and well-being in the postpartum period.
AUTHORS’ CONCLUSIONS
Implications for practice
Continuous support during labour should be the norm, rather than the exception. Hospitals should permit and encourage women to have a companion of their choice during labour and birth, and hospitals should implement programs to offer continuous support during labour. Policy makers and hospital administrators in high-income countries who wish to effect clinically important reductions in inappropriately high caesarean rates should be cautioned that continuous support by nurses or midwives may not achieve this goal, in the absence of other changes to policies and routines. In many settings, the labour ward functions according to a risk-oriented, technology-dominated approach to care. Institutional staff are unlikely to be able to offer labouring women benefits comparable to non-staff members, in the absence of fundamental changes in the organisation and delivery of maternity care. Changes to the content of health professionals’ education and to the core identity of professionals may also be important. Policy makers and administrators must look at system reform and rigorous attention to evidence-based use of interventions that were originally developed to diagnose or treat problems and are now used routinely during normal labours. Given the clear benefits and absence of adverse effects of continuous labour support, policy makers should consider including it as a covered service for all women.
Every effort should be made to ensure that women’s birth environments are empowering, non-stressful, afford privacy, communicate respect and are not characterised by routine interventions that add risk without clear benefit. In most areas of the world, childbearing women have limited or no access to trained doulas. Where available, costs of doula services are frequently borne by childbearing families and may be a barrier to access. In areas where doulas are not available, a comprehensive guidebook for designated companions is available for those with good English literacy (Simkin 2007). The ‘Better Births Initiative’ is a structured motivational program which promotes humane, evidence-based care during labour. The program focuses on promoting labour companionship and avoiding unproven interventions such as routine starvation, supine position and routine episiotomy. The educational materials for the Better Births Initiative include a video presentation on childbirth companions which is available in the World Health Organization Reproductive Health Library (WHO 2010). It can be accessed free of charge on the Internet in Arabic, Chinese, French, English, Spanish, Russian and Vietnamese and is distributed on CD to health workers in resource-poor countries. The selection of Cochrane reviews in the Reproductive Health Library includes this review of continuous labour support.
Implications for research
There remains relatively little information about the effects of continuous intrapartum support on mothers’ and babies’ health and well-being in the postpartum period, and thus trials across all types of settings, which include a focus on longer-term outcomes for mother and baby, would be helpful. The trials in resource-constrained countries were relatively small, and additional, large trials may be required in such settings, where the cost of providing continuous support may compete with other resource priorities. Particular attention should be paid to outcomes that have been under-researched in resource-poor settings, but are causes of significant morbidity, including urinary and faecal incontinence, pain during intercourse, prolonged perineal pain and depression.
Trials of different models of training providers of labour support would help to inform decision makers about the most effective models in the context of their settings. All trials should include economic analyses of the relative costs and benefits.
PLAIN LANGUAGE SUMMARY.
Continuous support for women during childbirth
Continuous support in labour increased the chance of a spontaneous vaginal birth, had no harm, and women were more satisfied.
Historically women have been attended and supported by other women during labour and birth. However in many countries, as more women are giving birth in hospital rather than at home, continuous support during labour has become the exception rather than the norm. This may contribute to the dehumanisation of women’s childbirth experiences. Modern obstetric care frequently subjects women to institutional routines, which may have adverse effects on the progress of labour. Supportive care during labour may involve emotional support, comfort measures, information and advocacy. These may enhance physiologic labour processes as well as women’s feelings of control and competence, and thus reduce the need for obstetric intervention. The review of studies included 23 trials (22 providing data), from 16 countries, involving more than 15,000 women in a wide range of settings and circumstances. The continuous support was provided either by hospital staff (such as nurses or midwives), women who were not hospital employees and had no personal relationship to the labouring woman (such as doulas or women who were provided with a modest amount of guidance), or by companions of the woman’s choice from her social network (such as her husband, partner, mother, or friend). Women who received continuous labour support were more likely to give birth ‘spontaneously’, i.e. give birth with neither caesarean nor vacuum nor forceps. In addition, women were less likely to use pain medications, were more likely to be satisfied, and had slightly shorter labours. Their babies were less likely to have low five-minute Apgar scores. No adverse effects were identified. We conclude that all women should have continuous support during labour. Continuous support from a person who is present solely to provide support, is not a member of the woman’s social network, is experienced in providing labour support, and has at least a modest amount of training, appears to be most beneficial. In comparison with having no companion during labour, support from a chosen family member or friend appears to increase women’s satisfaction with their childbearing experience.
ACKNOWLEDGEMENTS
We are very grateful to the investigators who provided additional information: O Bruggemann, D Campbell, R Cogan, A Gagnon, E Hemminki, M Kashanian, J Kennell, M Klaus, A Langer, B Madi, S McGrath, G Trueba, E Kopplin, and S Yuengong. We thank Agnes Cho, Qian Xu and Jiang Huangye for translation of Chinese publications, and Qian Xu for contacting the trial author for additional details. Ellen Hodnett and Justus Hofmeyr also provided additional information about their trials. Tanya Webb performed the second data entry on the earlier version of the review, contacted trial authors for additional information and provided secretarial support. The Consumer Panel of the Pregnancy and Childbirth Group (of which Carol Sakala is a member) provided many helpful suggestions for both the protocol and earlier versions of the review.
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | RCT. | |
| Participants | 3 trials are reported separately, within 1 publication. Participants were nulliparous, healthy, in spontaneous labour, term, with singleton vertex presentations. Trial in Belgium: n = 264 (133 permanent support; 131 control) |
|
| Interventions | Permanent presence of a midwife compared to varying degrees of presence. Fathers were allowed to be present | |
| Outcomes | Oxytocin, epidural analgesia, labour length, mode of birth, Apgar scores, mothers’ views of their experiences | |
| Notes | Epidural analgesia was available and it is not known whether EFM was used routinely | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women were ‘randomly assigned’. The envelopes were prepared by the co-ordinating centre. No mention of the process of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No mention if they were opaque or consecutively numbered. The process of how the envelopes were opened was not described |
| Blinding (performance bias and detection bias) All outcomes |
Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Completion rate for medical record data and in-hospital questionnaire were 99.2% and 91.0% respectively |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | See Breart - Belgium. | |
| Participants | See Breart - Belgium. Trial in France: n = 1320 (656 continuous support; 664 control) |
|
| Interventions | See Breart - Belgium. Fathers were allowed to be present. | |
| Outcomes | See Breart - Belgium. | |
| Notes | Epidural analgesia was available and it is unknown whether EFM was routine | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women were ‘randomly assigned’. The envelopes were prepared by the co-ordinating centre. No mention of the process of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No mention if they were opaque or consecutively numbered. The process of how the envelopes were opened was not described |
| Blinding (performance bias and detection bias) All outcomes |
Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Completion rate for medical record data and in-hospital questionnaire was > 95%. There were some discrepancies in the total number enrolled. 2 reports show 656 in the permanent support group and 664 in the control group for a total of 1320. The table of results in 1 report shows 654 in the permanent support and 666 in control. The in-hospital questionnaire results are shown for 654 and 664 women (total 1318) but the authors state this is 95%of the sample, meaning the total is 1386. The n reported with each outcome was the one used in the data tables in this review |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | See Breart - Belgium. | |
| Participants | See Breart - Belgium. Trial in Greece: n = 569 (295 permanent support; 274 control) | |
| Interventions | See Breart - Belgium. Fathers/family members were not permitted to be present | |
| Outcomes | See Breart - Belgium, except that mothers’ views were not reported | |
| Notes | Epidural analgesia was not available. Not stated if EFM was used routinely | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women were ‘randomly assigned’. The envelopes were prepared by the co-ordinating centre. No mention of the process of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No mention if they were opaque or consecutively numbered. The process of how the envelopes were opened was not described |
| Blinding (performance bias and detection bias) All outcomes |
Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Completion rate for medical record data was 97%. No in-hospital questionnaire data were available |
| Selective reporting (reporting bias) | Low risk | All medical record outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 212 nulliparous women in active labour at term (105 support group, 107 control group) at a University-affiliated hospital in Sao Paulo, Brazil. To be eligible a companion of the woman’s choosing had to be available. 49.5% of the companions were present at enrolment and the others were phoned and asked to come to the hospital (4 failed to make it before delivery) | |
| Interventions | Support was ‘presence of a chosen companion during labour and delivery’. ‘The companions received verbal and written information on the activities involved in providing support, expected behaviour when confronted with signs of tiredness, anxiety, concern, crying, screaming and/or the woman’s feelings of inability to cope, compliance with regulations and the possibility of requesting information from staff’. in 47.6% of the sample the woman’s companion was her partner, for 29.5% it was her mother The control group received usual care where a companion during labour and delivery was not permitted For both groups labour and delivery care was provided ‘according to the routine protocol including active management of labour (early amniotomy, use of oxytocin, intermittent EFM and systematic analgesia)’ |
|
| Outcomes | Satisfaction with labour and delivery, perinatal and breastfeeding outcome in the 12 hours post delivery | |
| Notes | All women in labour at this hospital received epidural analgesia as a routine practice. Therefore, we did not include epidural analgesia data in the review EFM was not used routinely. |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘Computer generated sequence of random numbers.’ |
| Allocation concealment (selection bias) | High risk | ‘Individual assignment numbers were all placed in an opaque container to assure the concealment. The eligible women who had agreed to participate selected one of the numbers once, and were therefore allocated to either intervention group or control according to the list.’ This process was open to selection bias as women could have repicked another number from the container. No audit process is possible with this system of randomisation |
| Blinding (performance bias and detection bias) All outcomes |
High risk | Data collection by author, who knew group allocation. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Medical record data were collected and in-hospital questionnaires were completed for 100% of sample |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 600 nulliparous, low-income, under-insured pregnant women (300 doula group, 300 control group) booked for delivery at a hospital in New Jersey, USA were enrolled between 12 and 38 weeks’ gestation. They were considered low risk, with no contraindications to labour and had a female friend or relative willing to act as their lay doula. The doula was in addition to support people of their own choosing | |
| Interventions | Intervention: continuous support by a female friend or relative who had had 2, 2-hour sessions about labour support. The training sessions were conducted for nearly all of the lay caregivers when the participants were 34-36 weeks’ gestation Control group: support people of their own choosing. |
|
| Outcomes | Labour length, epidural analgesia, oxytocin augmentation, cervical dilation at epidural insertion, length of second stage labour, caesarean birth, 1-min Apgar score > 6, 5-min Apgar score > 6 | |
| Notes | Epidural analgesia was available and EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘Computer generated randomization scheme.’ |
| Allocation concealment (selection bias) | Low risk | Consecutively-numbered, sealed opaque envelopes contained treatment assignments. After obtaining consent, a research assistant opened the next envelope. It was unclear whether the research assistant enrolling the woman was the same one that opened the envelope |
| Blinding (performance bias and detection bias) All outcomes |
High risk | Medical record abstraction was done by the author who was not blinded. The 6-week questionnaire data collection was not blinded |
| Incomplete outcome data (attrition bias) All outcomes |
High risk | Medical record information was completed for 97.7% of the sample (82.3% in the intervention group and 94.3% in the control group). The differential rates are due to withdrawals from the intervention group for doula related reasons (incomplete training and not being present during labour). The 6-week questionnaire was completed for 82.3% of the sample. Only those women included in the study at delivery had the opportunity to complete the questionnaire and thus the differential completion rate between groups remained (76.3% in the intervention group and 88.3% in the control group). The differential withdrawals could introduce selection bias |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Unclear risk | The training of the doulas giving the intervention was done by the research assistant, who was herself a doula. This same research assistant enrolled all study participants |
| Methods | RCT. | |
| Participants | 34 women (primigravidas and multigravidas) at 26-37 weeks’ gestation in 2 Texas hospitals (20 to supported group and 14 to usual care). They were in early, uncomplicated preterm labour | |
| Interventions | Intervention: support provided by a Lamaze childbirth preparation instructor. Support included continuous presence, acting as a liaison with hospital staff, providing information, and teaching relaxation and breathing measures Usual care: intermittent nursing care. Family members allowed to be present |
|
| Outcomes | Fetal distress, caesarean birth, artificial oxytocin, labour length, Apgar scores, neonatal intensive care | |
| Notes | Not stated if epidural analgesia was available or if EFM was used routinely | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ‘Randomly assigned.’ No further details provided. |
| Allocation concealment (selection bias) | Unclear risk | Admitting nurse telephoned research assistant to obtain treatment allocation. No details about whether the research assistant had foreknowledge of the treatment allocation scheme |
| Blinding (performance bias and detection bias) All outcomes |
Low risk | Medical record information collected by ‘research assistants who did not know the group membership of the women’ |
| Incomplete outcome data (attrition bias) All outcomes |
High risk | Withdrawals occurred before analysis (6 (30%) in support group and 3 (21%) in control). This resulted in a follow-up rate of 73.5%. The withdrawals were done differentially in the support group, i.e. some women were withdrawn because of an event that occurred before the support person arrived. Women in the control group with the same event were not withdrawn. We were able to re-create the original study groups for 1 outcome only, caesarean birth, and therefore it is included in the analysis table |
| Selective reporting (reporting bias) | Unclear risk | No outcomes were stated a priori. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT, stratified by induced or spontaneous labour at trial entry | |
| Participants | 992 nulliparous women at term (499 to continuous support and 493 to control), cephalic fetal presentation, cervical dilatation < 5 cm, in a hospital in Perth, Western Australia | |
| Interventions | Group 1: continuous physical and emotional support by midwifery staff, and women were encouraged to use pharmacologic and nonpharmacologic alternatives to epidural analgesia. Group 2: continuous midwifery support was not provided and women were encouraged to have epidural analgesia as their primary method of pain relief in labour |
|
| Outcomes | Labour length (expressed as median and interquartile range), epidural analgesia, mode of delivery, 5 min Apgar score < 7, arterial cord pH | |
| Notes | The stated purpose was to compare the effects of intrapartum analgesic techniques on labour outcomes. Continuous midwifery support was conceptualised as an analgesic technique. Both groups had access to opioids and nitrous oxide. No data were presented about the number of women who used no pharmacologic analgesia. Because the type of analgesia used was a measure of compliance rather than an outcome, no data on analgesic outcomes are included in this review It was not stated if other support person was allowed. epidural analgesia was available and EFM was used routinely |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details about how the blocks of treatment allocations were produced |
| Allocation concealment (selection bias) | Unclear risk | Randomisation on presentation in the labour and delivery unit, “by selection from a blocked group of eight sealed opaque envelopes, replenished from blocks of 12”. No further details about process |
| Blinding (performance bias and detection bias) All outcomes |
Unclear risk | Not noted. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | There was 100% follow-up for medical record data and in-hospital survey. A 6-month questionnaire was completed by 64. 7% of the sample and these data were not used |
| Selective reporting (reporting bias) | Low risk | All main outcomes were reported. Effects on breastfeeding were not analysed by treatment group and thus the results could not be included in the review |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 413 women admitted to an intrapartum unit at a tertiary care teaching hospital in Montreal, Canada, were randomly allocated to experimental (n = 209) or control (n = 204) groups. All but 3 in the experimental group and 6 in the control group were accompanied by a spouse, relative or friend during labour. All participants were nulliparous, with singleton fetuses, > 37 weeks’ gestation, and in labour | |
| Interventions | Experimental: 1-to-1 nursing care from randomisation until 1 hour postbirth. Care was provided by on-call nurses who were hired specifically for the study and had received a 30-hour training program and quarterly refresher workshops. The training program included critical reviews of the literature concerning the effects of intrapartum medical and nursing practices, as well as discussions of stress and pain management techniques. The nurse provided the usual nursing care plus physical comfort, emotional support, and instruction on relaxation and coping techniques. The nurse took meal breaks and brief rest breaks Women in the comparison group received usual nursing care by the regular unit staff, consisting of intermittent support and monitoring |
|
| Outcomes | Caesarean birth, caesarean birth for cephalopelvic disproportion or failure to progress, post-randomisation artificial oxytocin augmentation, post-randomisation analgesia/anaesthesia, instrumental vaginal delivery (forceps or vacuum extraction), NICU admission, perineal trauma, mean duration of labour post-randomisation, postpartum urinary catheterisation | |
| Notes | The participants had been admitted to the unit for an average of 5 hours (SD = 4 hours) prior to randomisation. 36 women in the experimental group and 41 in the control group had epidural analgesia prior to randomisation. 55 women in the experimental group and 45 in the control group had intravenous oxytocin augmentation of labour prior to randomisation. Mean duration of labour post-randomisation was 9.2 hours (SD = 4.3) Epidural analgesia was available but it was not stated if EFM was used routinely |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘Randomized using a list of computer generated random numbers.’ |
| Allocation concealment (selection bias) | Low risk | ‘Randomized in blocks of eight.’ ‘Group assignments were placed in sequentially numbered, sealed, opaque envelopes.’ |
| Blinding (performance bias and detection bias) All outcomes |
High risk | Data collectors were not blinded as they read nurses notes to collect data |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | 100% follow-up. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | 2 RCTs reported in the same publication. The Zelen method was used: only those participants randomised to the experimental group were told the true purpose of the trial and asked for consent. The participants in the control group were told about the study in the introduction letter for the postpartum questionnaire and they were told it was ‘a study on factors influencing birth’ | |
| Participants | Healthy nulliparous and parous women in labour at a hospital in Finland. 86 women were enrolled in Trial A. The actual number enrolled to each group was not noted but medical record data were collected for 79 women (41 in the support group and 38 in the control group). These 79 women represented 91.9% of the total sample | |
| Interventions | Trial A: in 1987, the intervention was 1:1 support by midwifery students from enrolment until transfer to the postpartum ward. The midwifery students volunteered, were not specially trained in support and responsible for the other routine intrapartum care The control group ‘was cared for according to the normal routine of the midwife and by a medical student, if s(he) was on duty’ Over 70% of fathers were present. |
|
| Outcomes | Labour length, medical interventions, complications (mother and baby), pharmacologic pain relief, method of birth, mothers’ evaluations of their experiences | |
| Notes | Not stated if epidural analgesia was available or if EFM was used routinely | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Nomention of how the allocation sequence was produced. |
| Allocation concealment (selection bias) | Unclear risk | ‘Randomization coding was done in blocks of 6 and put into non-transparent envelopes. The envelope was opened at the reception ward when it was decided to transfer mother to labour ward.’ It was not stated if the envelopes were consecutively numbered |
| Blinding (performance bias and detection bias) All outcomes |
High risk | Medical record outcome were collected unblinded. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Medical record data were collected on 91. 9% of the sample. A questionnaire was administered at 2-3 days postpartum. This was completed by only 70% of the sample and thus the data were not used |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | High risk | Mothers were told the purpose of the study differentially (see methods for Trial A above) |
| Methods | See Hemminki 1990a. | |
| Participants | See Hemminki 1990a. 161 women were enrolled in Trial B (81 in the support group and 80 in control) | |
| Interventions | Trial B: in 1988, the intervention was support by a new group of midwifery students. All students were involved in the trial, not just volunteers. The students were permitted to leave their participants to witness other interventions and deliveries The control group ‘was cared for according to the normal routine of the midwife’ and by a medical student as enrolment was limited to days when medical students were on duty Slightly less than 70% of fathers were present. |
|
| Outcomes | See Hemminki 1990a. | |
| Notes | Not stated if epidural analgesia was available or if EFM was used routinely | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided. |
| Allocation concealment (selection bias) | Unclear risk | The block size was reduced from the first study. ‘To lessen the frustration resulting from opening a code for a control mother, randomisation envelopes contained a maximum of two similar codes in sequence (not told in advance)’. ‘Put into non-transparent envelopes’. The envelope was opened in the labour ward. It was not stated if the envelopes were consecutively numbered |
| Blinding (performance bias and detection bias) All outcomes |
High risk | Medical record outcome were collected unblinded. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Medical record data were collected on 100% of the sample. A questionnaire was administered at 2-3 days postpartum and completed by 93.7% of the sample |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | High risk | Mothers were told the purpose of the study differentially (see methods for Trial A above) |
| Methods | RCT, stratified by type of prenatal classes (Lamaze vs general) | |
| Participants | 145 nulliparous women (72 to support group and 73 to control) in the last trimester of a healthy pregnancy, booked for delivery at a Toronto, Canada, hospital | |
| Interventions | Support provided by a monitrice (community ‘lay’ midwife or midwifery apprentice) compared with usual hospital care, defined as the intermittent presence of a nurse. Support described as including physical comfort measures, continuous presence, information, emotional support, and advocacy. The monitrice met with the woman twice in the latter weeks of pregnancy, to discuss her birth plans Comparable prenatal attention was provided to the controls. All but 1 woman also had husbands or partners present during labour. Support began in early labour at home or in hospital and continued through delivery |
|
| Outcomes | Intrapartum interventions, perceived control, method of delivery | |
| Notes | Epidural analgesia was available and EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer-generated table of random numbers. |
| Allocation concealment (selection bias) | Low risk | Randomisation done over the phone by a third party who had no knowledge of the participant, but used the open table of random numbers |
| Blinding (performance bias and detection bias) All outcomes |
Low risk | All participants blinded to the intervention. Control participants received prenatal and postpartum support (after the end of data collection); experimental participants received prenatal and intrapartum support Initial collection of medical record data was not blinded. ‘Duplicate abstraction was done by a second research assistant blind to the subject’s study group assignment, on a random sample of 20 records. Interrater agreement of over 95% was obtained for all categories of intervention and physical outcomes.’ In-home interview at 2-4 weeks postpartum was blinded |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Method of delivery outcome available on 88.3% of sample. Other outcomes collected on only 71% of the sample and thus not used |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | Multi-centre RCT with prognostic stratification for parity and hospital | |
| Participants | 6915 nulliparous and parous women in labour at 13 hospitals in the USA and Canada (3454 to continuous labour support and 3461 to usual care). Eligibility criteria: live singleton fetus or twins, no contraindications to labour, in labour. Women were excluded if gestational age was < 34 weeks or if they were so high risk that a 1:1 patient-nurse ratio was medically necessary | |
| Interventions | Experimental: continuous support from staff labour and delivery nurses who had volunteered for and received a 2-day training workshop in labour support. Prior to the trial, the support nurses had opportunities to practice their skills. They also had opportunities to continue learning from each other and the labour support trainer, throughout the trial. The nurses with training were part of the regular staffing complement of the unit and they provided care to the continuous support group but not to the usual care group Usual care: intermittent support from a nurse who had not received labour support training | |
| Outcomes | Intrapartum interventions, method of birth, immediate complications (mother or baby), complications (mother or baby) in the first 6-8 weeks postpartum, perceived control, postpartum depression, breastfeeding at 6-8 weeks, relationship with partner and with baby, likes and dislikes about birth experience and future preferences for labour support | |
| Notes | Other support person(s) were allowed, epidural analgesia was available and EFM was used routinely | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation program. |
| Allocation concealment (selection bias) | Low risk | ‘Randomization was centrally controlled with the use of a computerized randomization program at the data co-ordinating centre, accessible by means of a touch-tone telephone.’ |
| Blinding (performance bias and detection bias) All outcomes |
Low risk | Data collectors were not blinded as they read nurses’ notes to collect data about type of nursing care provided. However random chart audits yielded no errors in reporting study outcomes |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Medical record data were collected on 100% of the sample. In-hospital questionnaires were completed by 96.4% and 6-8 week questionnaires by 81% of the sample |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 189 nulliparous women (92 to support and 97 to control) in active labour at a community hospital serving low-income women in South Africa | |
| Interventions | Intervention group: support by carefully trained, volunteer lay women, for at least several hours (supporters not expected to remain after dark) Control group: intermittent care on a busy ward. Husbands/family members were not permitted |
|
| Outcomes | Intrapartum interventions, method of birth, complications (mother and baby), anxiety, pain, mothers’ perceptions of labour, breastfeeding | |
| Notes | Epidural analgesia was not available and EFM was not used routinely. While scores on an instrument measuring postpartum depression were reported in categories of “low”, “moderate,“ and ‘high”, the authors stated that categorization was not appropriate as a clinical diagnostic definition of depression. To achieve the latter, the change in score must be reported, and these data were not collected | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random. |
| Allocation concealment (selection bias) | Unclear risk | “Randomly ordered cards in sealed opaque envelopes”. Not stated if consecutively numbered |
| Blinding (performance bias and detection bias) All outcomes |
High risk | Data collectors were not blinded as they asked questions about support received in labour |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Medical record data were collected on 100% of the sample and questionnaires within 24 hours postpartum were completed by 99%. The 6-week follow-up interviews were completed by 78. 8% of the sample, no imbalances existed between groups and thus the data were included in the analysis. At 1-year interviews were complete for 46% of the sample and data from these were not used. Nikodem reported on a larger sample of women with 1-year follow-ups but the completion rate was still only 50% of the original number enrolled |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 100 nulliparous women at term (50 to support and 50 to routine care) in active labour at a university hospital in Tehran, Iran from March to September 2003 | |
| Interventions | ‘Women allocated to the intervention group were shown to an isolated room and were supported by an experienced midwife. The women were free to choose their position, and able to eat and walk about freely. During labor, the midwife explained the process of labor and the importance of body relaxation. Midwife-led support included close physical proximity, touch, and eye contact with the labouring women, and teaching, reassurance, and encouragement. The midwife remained with the woman throughout labor and delivery, and applied warm or cold packs to the woman’s back, abdomen, or other parts of the body, as well as performing massage according to each woman’s request.’ ‘Women allocated to the routine care group were admitted to the labor ward (where 5-7 women labour in the same room), did not receive continuous support, and followed the routine orders of the ward. They did not have a private room, did not receive one-to-one care,were not permitted food, and did not receive education and explanation about the labor process. The only persons allowed in the delivery room were nurses, midwives, and doctors.’ |
|
| Outcomes | Duration of labour, caesarean delivery, oxytocin use, Apgar score at 5 mins | |
| Notes | EFM was not used routinely and epidural analgesia was not available | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | From personal communication - equal numbers of envelopes were produced for each letter (see below) and put into a box. No list of treatment allocations was created |
| Allocation concealment (selection bias) | High risk | ‘Allocated to one of two groups using 4-part, block randomization’. Used ‘sealed envelopes labelled A, B, C, and D: envelopes A and C (intervention group) and B and D (routine care group). Patients then chose an envelope, which was opened by the investigator’ Further details from personal communication - the women picked from all the envelopes produced. Once an envelope was picked it was discarded This process was open to selection bias as women previously in the trial may have shared knowledge of which envelope contained which group with women not yet enrolled in the study |
| Blinding (performance bias and detection bias) All outcomes |
Low risk | From personal communication - ‘The co worker of investigator collected the outcome data and she was blind for the study group.’ |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Medical record information was collected on 100% of the sample |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT of continuous support vs usual care with an ‘inconspicuous observer’ plus a retrospective non-random control group. This review is restricted to comparisons of the outcomes of the participants who were randomly assigned | |
| Participants | 412 nulliparous women (212 in support group and 200 in observed group) were part of the RCT. They were aged 13-34, with singleton, term, healthy pregnancies, many not English-speaking, in active labour at a public hospital in Texas which provides care for low-income patients | |
| Interventions | The description of the setting, the participants, and the type of care echo developing world conditions. All women laboured in a large 12-bed room For the women in the support group a doula stayed by their bedside and gave continuous support For those in the observed group they had the routine intermittent presence of a nurse and continuous presence of an ‘inconspicuous observer’ who ‘kept a record of staff contact, interaction and procedures’. The observer was away from the beside and never spoke to the labouring woman |
|
| Outcomes | Analgesia/anaesthesia, labour length, artificial oxytocin use, method of birth, complications (mother and baby), neonatal health, number of women who rated their experience as negative | |
| Notes | In instances in which outcome data (such as analgesia/anaesthesia use) in the published report were only provided for subgroups, the primary author was contacted and he provided complete outcome data for all women who were originally randomised Family members were not allowed to be present. Epidural analgesia was available and EFM was used routinely |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as random. |
| Allocation concealment (selection bias) | Low risk | ‘Randomly assigned’ is stated in the report. In the protocol for the trial it states ‘numbered opaque envelopes’ would be used. The envelopes ‘would contain the random assignments of the women to control or treatment groups and would be numbered sequentially’ |
| Blinding (performance bias and detection bias) All outcomes |
Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | There is some discrepancy in the number of women enrolled in the study. The report states 412 were enrolled and reports outcome data on all 412 women. But it also states that ‘14 women that agreed to participate were not included in the study.’ The reasons for not including them seem to be events that would happen after randomisation - e.g. transferred due to staffing limitations, withdrew, undetected breech, interrupted observations, etc., and thus the sample appears to have numbered 426. Data are reported for 412 women (96.7% of 426) |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. Purposefully enrolled more women to the control group. See ‘Risk of bias’ table below | |
| Participants | 465 healthy nulliparous women (186 to support group and 279 to control) in labour at the Social Security Hospital in Guatemala | |
| Interventions | Support group: continuous emotional and physical support by a doula Control group: usual hospital routines (described as no consistent support) | |
| Outcomes | Labour length, use of artificial oxytocin, method of birth, problems during labour and birth, fetal distress, Apgar scores, transfer to neonatal intensive care nursery | |
| Notes | No family members permitted to be present. epidural analgesia was not available and EFM was not used routinely | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ‘Enrolled using randomised design’. ‘Pool of envelopes contained more control group to ensure similar sized groups with uncomplicated labours and deliveries.’ They anticipated more complications in control group based on an earlier study (Sosa 1980). No information on how allocation sequence was generated. |
| Allocation concealment (selection bias) | Low risk | ‘Randomly assigned according to contents of a sealed opaque envelope. Each envelope was numbered sequentially.’ |
| Blinding (performance bias and detection bias) All outcomes |
Unclear risk | Not noted. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | ‘Mother-infant pairs were excluded when the mother developed a complication during labour, delivery, or post partum that required special care, if the baby’s weight was below 5.5 lbs or above 8 lbs, if there were twins or congenital malformations.’ This occurred for about 10% of cases in both groups resulting in reported outcomes for 89.6% of those randomised. Unpublished data on the excluded women were provided by the author Labour length data were only available for 48.4% of the sample (225 of 465) and thus not included |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported on. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 724 women (361 to support and 363 to control) admitted for delivery at a large social security hospital in Mexico City, who met the following criteria: singleton fetus, no previous vaginal delivery, < 6 cm cervical dilatation, and no indications for an elective caesarean delivery | |
| Interventions | Support group: continuous support from1 of 10 women who had received doula training (6 were retired nurses), throughout labour, birth, and the immediate postpartum period. Support included: emotional support, information, physical comfort measures, social communication, ensuring immediate contact between mother and baby after birth, and offering advice about breastfeeding during a single brief session postnatally Control group: women received ‘routine care’. |
|
| Outcomes | The main outcomes were exclusive and full breastfeeding at 1 month postpartum. Other outcomes included labour length, epidural anaesthesia, forceps birth, caesarean birth, meconium staining, and Apgar scores, as well as mothers’ perceived control during childbirth, anxiety, pain, satisfaction, and self-esteem | |
| Notes | Partners and family members were not permitted. Epidural analgesia was available but it was not stated if EFM was used routinely | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘Computer generated random number list’. ‘The treatment sequence was kept at a central level.’ |
| Allocation concealment (selection bias) | Unclear risk | ‘Opaque envelopes with the assignment were locked in a cabinet to which only a social worker exclusively in charge of randomisation and the principal investigator had access. An envelope with a paper inside showing to which group each woman was assigned was opened by the social worker immediately after recruitment in the labour and delivery unit. Not stated if envelopes were sequentially numbered |
| Blinding (performance bias and detection bias) All outcomes |
Low risk | Data were collected by 2 ‘blinded social workers’. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Medical record data and in-hospital interview data were collected for 100% of the sample. A in-home interview was completed at 1 month postpartum for 92.2% of the sample |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 109 Black women from Botswana (53 in support group and 56 in usual care group), mean age 19 years, 80% unmarried, mostly students, who had met the following criteria: nulliparous, in labour, pregnancy at term, no history of pregnancy complications, cephalic presentation, normal spontaneous labour with cervical dilation 1-6 cm, female relative present who was willing to remain with the woman for the duration of labour | |
| Interventions | Support group: continuous presence of female relative (usually her mother) in addition to usual hospital care Congrol group: usual hospital care, which involved staff:patient ratios of 1:4, and no companions permitted during labour |
|
| Outcomes | Spontaneous vaginal birth, vacuum extraction, caesarean birth, analgesia, amniotomy, artificial oxytocin during labour, Apgar scores (1- and 5-min) | |
| Notes | Epidural analgesia was not available and it was not stated whether EFM was used routinely | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ‘Randomly allocated.’ No other details provided. |
| Allocation concealment (selection bias) | Low risk | ‘Selection of an opaque, numbered, sealed envelope from a box of envelopes that were shuffled in the woman’s presence. When opened the envelope revealed a code indicating her group.’ An assistant that was not involved in the recruitment process shuffled the envelopes |
| Blinding (performance bias and detection bias) All outcomes |
High risk | The researcher, who was involved in the recruitment of participants, collected the medical record data |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Medical record data were collected on 100% of the sample. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. Enrollment occurred at childbirth education classes and randomisation occurred when the woman arrived at hospital in labour | |
| Participants | 420 nulliparous middle and upper class women (224 on doula group and 196 in control group) were enrolled in the third trimester of an uncomplicated pregnancy in Cleveland, Ohio. All women expected to be accompanied during labour by their male partner | |
| Interventions | Experimental group: a doula met the couple at the hospital as soon as possible after random assignment (typically within an hour of their arrival at the hospital) and remained with them throughout labour and delivery. The central component of doula support was the doula’s continuous bedside presence during labour and delivery, although her specific activities were individualised to the needs of the labouring woman. Doula support included close physical proximity, touch, and eye contact with the labouring woman, and teaching, reassurance, and encouragement of the woman and hermale partner. All doulas completed training requirements that were equivalent to the DONA International doula certification Control group: routine obstetric and nursing care which included the presence of a male partner or other support person |
|
| Outcomes | Caesarean delivery, epidural anaesthesia, oxytocin use, labour length, mode of delivery, fever during labour, satisfaction at 6 weeks postpartum | |
| Notes | Epidural analgesia was available and EFM was used routinely. The author has been contacted for data split by study group and questionnaire data for the control group |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details stated. |
| Allocation concealment (selection bias) | Low risk | ‘When the research co-ordinator was informed that an enrolled woman had arrived at the hospital in early active labor, she opened the next sequentially numbered opaque envelope to determine random assignment to the doula or control group’. The research co-ordinator was off-site and called by the staff or the study participant |
| Blinding (performance bias and detection bias) All outcomes |
Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Medical record data were collected on 100% of the sample. The in-hospital and 6-week questionnaires were completed by 87.9% and 87.5% of the doula group. No information was provided for the control group |
| Selective reporting (reporting bias) | Low risk | The primary outcomes of caesarean birth and epidural anaesthesia were reported for each study group. Other labour and delivery outcomes were reported for the full sample only (not split by group). The in-hospital and 6-week questionnaire data were only reported for the doula group.The author has been contacted for these missing details |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 603 women from Ibadan, Nigeria with anticipated vaginal delivery were enrolled between 30 and 32 weeks’ gestation at an antenatal clinic (305 to intervention and 298 to control) from November 2006 to March 2007 | |
| Interventions | Those in the experimental group were informed to bring someone of their choice to act as a companion during labour. On arrival in labour the accompanying companions were provided with an information leaflet that explained their responsibilities. These included: gentle massage of the woman’s back during contraction, reassuring words, spiritual support inform of prayers and also acting as intermediary between the woman and healthcare team. After studying the leaflets, they were allowed to seek clarifications. The information leaflet was also interpreted for those that are not literate. The attending midwife allowed and ensured companions performed their expected duties throughout. The companions were told to offer continuous support - they were to be by the patient’s side except for feeding and use of toilet until two hours after childbirth. Husbands were the most common support person (65.4%) The women in the control group had only routine care where relatives of patients are usually barred from the labour ward |
|
| Outcomes | Caesarean section rate, active phase of labour duration, pain score, need for analgesia, need for oxytocin augmentation, time from delivery to initiation of breastfeeding and the emotional experience during labour | |
| Notes | Epidural analgesia was not available and it was not stated whether EFM was used routinely. We have requested further details from the authors The randomisation process was well done, but resulted in an imbalance in socioeconomic status between the groups. Women in the experimental group tended to be more educated (82% vs 48% with tertiary level) and skilled workers (78% vs 39%). This imbalance was noted and discussed by the authors |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘The randomisation sequence was generated using a table of random numbers’ |
| Allocation concealment (selection bias) | Low risk | ‘Random permuted blocks of size four were used to ensure a balanced design.’ ‘Based on the sequence of treatments generated using this method, treatment groups (A and B) were written on pieces of cardboard paper and put into sealed opaque envelopes. Each of the opaque envelopes had a serial number on it.’ ‘Two trained research assistants (RAs) non-medical staff, supervised the randomisation procedure at every clinic. On each clinic day, consented women that met the inclusion criteria were given serial numbers with allotted treatment group based on their arrival time.Only the statistician and RAs had access to the list of numbers used to prevent clinicians’ influence on the randomisation. Each participant opened the opaque envelope in the presence of an RA, and the assigned treatment group was recorded on the woman’s medical record file.’ |
| Blinding (performance bias and detection bias) All outcomes |
High risk | How data collection was done was not noted. The treatment group was noted in the chart so it is likely that the data collectors were unblinded |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Follow-up was completed for 97% of the sample. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT, no details regarding method of random assignment. | |
| Participants | 144 ‘healthy’ women having their first baby booked for delivery at a Swedish hospital (72 to doula group and 72 to usual care). Participants were enrolled at 36 weeks’ gestation | |
| Interventions | Continuous presence by a doula who had met the woman during pregnancy, compared to usual care | |
| Outcomes | Emergency caesarean birth and epidural analgesia. | |
| Notes | The trial author reported that the information about randomisation method and outcomes of those lost to follow-up are no longer available Epidural analgesia was available. It was not stated if other support person(s) were allowed or if EFM was used routinely |
|
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ‘Randomized’ - no further details provided or available. |
| Allocation concealment (selection bias) | Unclear risk | No details provided or obtained. |
| Blinding (performance bias and detection bias) All outcomes |
Unclear risk | Not noted. |
| Incomplete outcome data (attrition bias) All outcomes |
High risk | Medical record data collected on 70.1% of sample. No usable outcome data, due to serious risk of attrition bias. Outcomes are reported for 55/72 (76%) of the intervention group and 46/72 (64%) of the control group. Reason for the 41 “dropouts” were preterm birth, induction, or caesarean section “for medical reasons”, and participant withdrawal. No numbers are given for individual reasons, or by group, but it is clear that some “dropouts” were prior to labour and others were during labour. Numbers in the report show the number of dropouts was actually 43 |
| Selective reporting (reporting bias) | Unclear risk | Sample size was based on caesarean section rate. The only outcome reported was emergency caesarean |
| Other bias | High risk | Trial was stopped early for ‘a range of largely organizational issues’ when only 1/4 of the original sample size had been enrolled |
| Methods | RCT. | |
| Participants | 435 women (217 in companion group, 218 in control group) with a singleton pregnancy and considered to be low-risk at University Hospital in Santiago, Chile. Enrolled at 34-36 weeks’ gestation | |
| Interventions | Intervention group: psychosocial support during labour from a companion chosen by the pregnant woman. The companions were trained by trial staff to provide emotional support, promote physical comfort and encourage progress of labour, without interfering with the activities of the obstetricians or midwives. They were with the labouring woman continuously from admission to delivery. Women were encouraged to pick a companion who had experienced a vaginal birth Control group did not have companion. Both groups laboured in a room with other women where curtains were pulled for privacy |
|
| Outcomes | Caesarean section, exclusive breastfeeding, duration of labour, mode of delivery, use of oxytocics, presence of meconium, regional anaesthesia, birth asphyxia, Apgar scores, level of neonatal care, maternal satisfaction | |
| Notes | Epidural analgesia was available. It was not stated if EFM was used routinely. Authors have been contacted for further details | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer-generated list of random numbers. |
| Allocation concealment (selection bias) | Low risk | Used blocks of 6. Group assignment used sealed opaque envelopes numbered consecutively. A member of the trial team enrolled women and did not know in advance the content of each envelope |
| Blinding (performance bias and detection bias) All outcomes |
Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | Medcial record data were collected for 100% of the sample and in-hospital surveys were completed by 95.8%. A 6-week phone interview was completed for 71.2%of the sample and thus these data were not used |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT | |
| Participants | 120 nulliparous women, ages 18-30, at least 36 weeks’ gestation, singleton fetus with cephalic presentation, able and willing to have a close female relative with them during labour and birth, booked to give birth at a regional teaching hospital in Thailand | |
| Interventions | Experimental group: close female relative who attended a 2-hour preparation class on labour routines and supportive actions, and provided continuous support during the active portion of hospital labour. The institution required that the researcher remain in order to monitor the relative’s activities. Control group: usual care by health professionals, which included intermittent support. Family members were not permitted to stay with the woman | |
| Outcomes | Oxytocin during labour, analgesia, labour length, spontaneous birth, assisted vaginal birth, caesarean birth, Apgar Scores, perceived control | |
| Notes | Epidural analgesia was not available and continuous EFM was not used | |
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number sequence generated by a software program. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes were used. Envelopes were consecutively-numbered on the outside |
| Blinding (performance bias and detection bias) All outcomes |
Low risk | Women, investigator, and providers could not be blinded to the presence of the female relative. Research assistant blinded to group assignment collected satisfaction data |
| Incomplete outcome data (attrition bias) All outcomes |
Low risk | 5% lost to follow-up: 2 in the experimental group and 4 in the control group |
| Selective reporting (reporting bias) | Low risk | Appears complete. |
| Other bias | Low risk | 6 women (10%) in experimental group did not receive continuous support |
EFM: electronic fetal monitoring
min: minutes
NICU: neonatal intensive care unit
RCT: randomised controlled trial
SD: standard deviation
vs: versus
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Bender 1968 | 2 studies are reported, n = 12 in the first study and n = 30 in the second. Neither one was an RCT. Both employed alternate allocation that was neither centrally controlled nor concealed. The researcher delivered the intervention and collected outcome data. In the first study the researcher also enrolled participants. No usable outcome data are reported |
| Bochain 2000 | The intervention was not continuous labour support. It was a short nursing intervention (taking approximately 1 hour) administered in early labour for women undergoing Misoprostol induction |
| Brown 2007 | The intervention was not continuous labour support. It was an educational intervention to promote childbirth companions in hospital deliveries. A cluster-RCT was undertaken at 10 South African state maternity hospitals |
| Dalal 2006 | Not an RCT. 100 randomly-selected mothers who had a birth companion were compared with 50 randomly-selected mothers who did not have one. Mothers were matched for age and socioeconomic status |
| Gordon 1999 | 30% of those enrolled were excluded post-randomisation, 73/232 in the doula group and 69/246 in the control group. A letter was sent to the first author, asking for data on the excluded participants that would permit an intent-to-treat analysis. If and when a response is received, we will evaluate the trial report again |
| Hemminki 1990c | Third study in the same report as Hemminki 1990aand Hemminki 1990b. This was a small pilot RCT of support by lay women that was ‘stopped for economic and other practical reasons’. 31 women were enrolled but 7 dropped out (all from the intervention group). Very little data were reported and it was not separated by treatment group and thus unusable |
| Lindow 1998 | Support was not continuous, and was quite brief in duration. 16 women in active labour were randomised to either 1 hour with a supportive companion or 1 hour without. The only outcome was maternal oxytocin level for 16 minutes post-support or control period |
| McGrath 1999 | An abstract outlining a study of 531 women in Houston, Texas. Insufficient details to permit evaluation of the quality of the trial, and insufficient details regarding results. Thus far, attempts to locate a full report of the trial have been unsuccessful |
| Orenstein 1998 | Not a randomised trial. Women chose to either have a doula or have Lamaze preparation for childbirth |
| Pinheiro 1996 | An abstract of a paper presented at the Xth World Congress of Psychiatry in Madrid, 1996. Preliminary results were reported. Efforts to locate a published report of the full trial have been unsuccessful. The abstract provides insufficient details regarding methods, to permit evaluation of the quality of the trial. The purpose was to compare the effectiveness of female vs male doulas vs routine care without doulas. The doulas were medical and psychology students |
| Ran 2005 | Not an RCT. Translated personal communication from the author stated “I randomly sampling allocated the patient, did not use any random tool” |
| Scott 1999 | Not a trial. A review of selected studies of intrapartum support |
| Sosa 1980 | Strong evidence of selection bias. “A woman was removed from the study if labor was false or prolonged; if fetal distress necessitated an intervention such as oxytocin, caesarean delivery, or forceps”; or if the infant was asphyxiated or ill at birth, etc. “If a woman was removed, her group assignment was inserted at random into the pool of unused assignments. Women were enrolled in the study until there were 20 in the control group and 20 in the experimental group.” The total study sample of 127 mothers includes 95 in the control group and 32 in the experimental group. Thus assignment was not random |
| Trueba 2000 | Direct contact with investigator revealed that randomisation was not used. On arrival at the hospital, women were asked if they wanted to have a doula. If they accepted, a doula was assigned to them. Also support was not continuous throughout active labour for most women, since admission to the labour ward (and assignment of a doula) did not usually occur until 8 cm |
| Tryon 1966 | Not an RCT. “After a random start, the matched groups were alternately assigned to experimental and control groups.” Women who developed severe complications in labour (number not specified), such as fetal distress, were dropped from the study |
| Zhang 1996 | Not a trial of continuous 1-to-1 support. On admission to the labour ward, women received instruction about normal labour, non-pharmacological methods to ease pain, and how to push in second stage, from a team of physicians and nurses. Support was continuous, depending on the women’s needs, but not 1-to-1 |
EFM: electronic fetal monitoring
RCT: randomised controlled trial
vs: versus
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract - insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Unclear. |
| Outcomes | Insufficient details. |
| Notes | Communication sent to author regarding details of randomisation process, the nature of the intervention, and information to allow classification for analysis subgroups |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract - insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract - insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract - insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract - insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract - insufficient details to permit classification. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Janssen. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Starting date | Insufficient details. |
| Contact information | Insufficient details. |
| Notes |
DATA AND ANALYSES
Comparison 1.
Continuous support versus usual care - all trials
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any analgesia/anaesthesia | 14 | 12283 | Risk Ratio (M-H, Random, 95% CI) | 0.90 [0.84, 0.96] |
| 2 Regional analgesia/anaesthesia | 9 | 11444 | Risk Ratio (M-H, Random, 95% CI) | 0.93 [0.88, 0.99] |
| 3 Synthetic oxytocin during labour | 15 | 12620 | Risk Ratio (M-H, Random, 95% CI) | 0.97 [0.91, 1.04] |
| 4 Labour length | 12 | 5366 | Mean Difference (IV, Random, 95% CI) | −0.58 [−0.85, −0.31] |
| 5 Spontaneous vaginal birth | 19 | 14119 | Risk Ratio (M-H, Random, 95% CI) | 1.08 [1.04, 1.12] |
| 6 Instrumental vaginal birth | 19 | 14118 | Risk Ratio (M-H, Fixed, 95% CI) | 0.90 [0.85, 0.96] |
| 7 Caesarean birth | 22 | 15175 | Risk Ratio (M-H, Random, 95% CI) | 0.78 [0.67, 0.91] |
| 8 Perineal trauma | 4 | 8120 | Risk Ratio (M-H, Random, 95% CI) | 0.97 [0.92, 1.01] |
| 9 Low 5-minute Apgar score | 13 | 12515 | Risk Ratio (M-H, Fixed, 95% CI) | 0.69 [0.50, 0.95] |
| 10 Admission to special care nursery | 7 | 8897 | Risk Ratio (M-H, Random, 95% CI) | 0.97 [0.76, 1.25] |
| 11 Prolonged neonatal hospital | 3 | 1098 | Risk Ratio (M-H, Random, 95% CI) | 0.83 [0.42, 1.65] |
| 12 Postpartum report of severe labour pain | 4 | 2456 | Risk Ratio (M-H, Random, 95% CI) | 1.00 [0.83, 1.21] |
| 13 Negative rating of/negative feelings about birth experience | 11 | 11133 | Risk Ratio (M-H, Random, 95% CI) | 0.69 [0.59, 0.79] |
| 14 Difficulty mothering | 3 | Risk Ratio (M-H, Fixed, 95% CI) | Totals not selected | |
| 15 Breastfeeding at 1-2 months postpartum | 3 | 5363 | Risk Ratio (M-H, Random, 95% CI) | 1.01 [0.94, 1.09] |
| 16 Postpartum depression | 2 | Risk Ratio (M-H, Fixed, 95% CI) | Totals not selected | |
| 17 Low postpartum self-esteem | 1 | 652 | Risk Ratio (M-H, Fixed, 95% CI) | 1.00 [0.77, 1.30] |
Comparison 2.
Continuous support versus usual care - policy regarding presence of companion
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any analgesia/anaesthesia | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Other support permitted | 7 | 9752 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.99] |
| 1.2 Other support not permitted | 7 | 2598 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.85, 0.96] |
| 2 Synthetic oxytocin during labour | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Other support permitted | 5 | 9495 | Risk Ratio (IV, Fixed, 95% CI) | 1.04 [0.99, 1.10] |
| 2.2 Other support not permitted | 10 | 3125 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.97, 1.02] |
| 3 Spontaneous vaginal birth | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Other support permitted | 9 | 10889 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [1.00, 1.05] |
| 3.2 Other support not permitted | 10 | 3329 | Risk Ratio (IV, Fixed, 95% CI) | 1.11 [1.07, 1.16] |
| 4 Caesarean birth | 22 | Risk Ratio IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Other support permitted | 11 | 11326 | Risk Ratio IV, Fixed, 95% CI) | 0.94 [0.85, 1.03] |
| 4.2 Other support not permitted | 11 | 3849 | Risk Ratio IV, Fixed, 95% CI) | 0.75 [0.65, 0.86] |
| 5 Admission to special care nursery | 7 | Risk Ratio IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Other support permitted | 2 | 7328 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.84, 1.17] |
| 5.2 Other support not permitted | 5 | 1569 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.71, 1.17] |
| 6 Postpartum depression | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Other support permitted | 1 | 5567 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.73, 1.02] |
| 6.2 Other support not permitted | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.18 [0.09, 0.36] |
| 7 Negative rating of/negative feelings about birth experience | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Other support permitted | 5 | 8639 | Risk Ratio (IV, Fixed, 95% CI) | 0.70 [0.62, 0.78] |
| 7.2 Other support not permitted | 6 | 2539 | Risk Ratio (IV, Fixed, 95% CI) | 0.62 [0.56, 0.69] |
| 8 Breastfeeding at 1-2 months postpartum | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Other support permitted | 1 | 4559 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.92, 1.02] |
| 8.2 Other support not permitted | 2 | 804 | Risk Ratio (IV, Fixed, 95% CI) | 1.05 [0.98, 1.13] |
Comparison 3.
Continuous support versus usual care - availability of epidural analgesia
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any analgesia/anaesthesia | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Epidural analgesia routinely available | 9 | 10888 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.98] |
| 1.2 Epidural analgesia not routinely available | 5 | 1462 | Risk Ratio (IV, Fixed, 95% CI) | 0.83 [0.69, 0.99] |
| 2 Synthetic oxytocin during labour | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Epidural analgesia routinely available | 8 | 10568 | Risk Ratio (IV, Fixed, 95% CI) | 1.00 [0.98, 1.02] |
| 2.2 Epidural analgesia not routinely available | 7 | 2066 | Risk Ratio (IV, Fixed, 95% CI) | 1.02 [0.93, 1.11] |
| 3 Spontaneous vaginal birth | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Epidural analgesia routinely available | 13 | 12672 | Risk Ratio (IV, Fixed, 95% CI) | 1.04 [1.01, 1.06] |
| 3.2 Epidural analgesia not routinely available | 6 | 1546 | Risk Ratio (IV, Fixed, 95% CI) | 1.11 [1.06, 1.17] |
| 4 Caesarean birth | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Epidural analgesia routinely available | 14 | 13064 | Risk Ratio (IV, Fixed, 95% CI) | 0.93 [0.86, 1.02] |
| 4.2 Epidural analgesia not routinely available | 7 | 2077 | Risk Ratio (IV, Fixed, 95% CI) | 0.54 [0.43, 0.68] |
| 4.3 Unknown availability of epidural analgesia | 1 | 34 | Risk Ratio (IV, Fixed, 95% CI) | 1.4 [0.14, 13.98] |
| 5 Admission to special care nursery | 7 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Epidural analgesia routinely available | 5 | 8380 | Risk Ratio (IV, Fixed, 95% CI) | 0.98 [0.85, 1.13] |
| 5.2 Epidural analgesia not routinely available | 2 | 517 | Risk Ratio (IV, Fixed, 95% CI) | 0.26 [0.08, 0.88] |
| 6 Postpartum depression | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Epidural analgesia routinely available | 1 | 6915 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.75, 1.05] |
| 6.2 Epidural analgesia not routinely available | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.18 [0.09, 0.36] |
| 7 Negative rating of/negative feelings about birth experience | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Epidural analgesia routinely available | 9 | 10404 | Risk Ratio (IV, Fixed, 95% CI) | 0.70 [0.64, 0.77] |
| 7.2 Epidural analgesia not routinely available | 2 | 774 | Risk Ratio (IV, Fixed, 95% CI) | 0.55 [0.48, 0.63] |
| 8 Breastfeeding at 1-2 months postpartum | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Epidural analgesia routinely available | 2 | 5214 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.95, 1.03] |
| 8.2 Epidural analgesia not routinely available | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 1.15 [0.95, 1.40] |
Comparison 4.
Continuous support versus usual care - policy about routine EFM
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any analgesia/anaesthesia | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1. 1 Setting had routine EFM | 6 | 8580 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.99] |
| 1.2 Setting did not have routine EFM | 6 | 2186 | Risk Ratio (IV, Fixed, 95% CI) | 0.96 [0.90, 1.02] |
| 1.3 Policy about routine EFM not known | 2 | 1579 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.80, 0.99] |
| 2 Synthetic oxytocin during labour | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Setting had routine EFM | 4 | 8340 | Risk Ratio (IV, Fixed, 95% CI) | 1.04 [0.98, 1.11] |
| 2.2 Setting did not have routine EFM | 7 | 1726 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.96, 1.01] |
| 2.3 Policy about routine EFM not known | 4 | 2568 | Risk Ratio (IV, Fixed, 95% CI) | 1.02 [0.97, 1.08] |
| 3 Spontaneous vaginal birth | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Setting had routine EFM | 8 | 9717 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [1.01, 1.06] |
| 3.2 Setting did not have routine EFM | 7 | 1913 | Risk Ratio (IV, Fixed, 95% CI) | 1.11 [1.06, 1.17] |
| 3.3 Policy about routine EFM not known | 4 | 2561 | Risk Ratio (IV, Fixed, 95% CI) | 1.07 [1.01, 1.13] |
| 4 Caesarean birth | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Setting had routine EFM | 9 | 10123 | Risk Ratio IV, Fixed, 95% CI) | 0.92 [0.83, 1.01] |
| 4.2 Setting did not have routine EFM | 8 | 2457 | Risk Ratio IV, Fixed, 95% CI) | 0.66 [0.55, 0.79] |
| 4.3 Policy about routine EFM not known | 5 | 2595 | Risk Ratio IV, Fixed, 95% CI) | 1.06 [0.84, 1.33] |
| 5 Admission to special care nursery | 7 | Risk Ratio IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Setting had routine EFM | 3 | 7740 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.84, 1.11] |
| 5.2 Setting did not have routine EFM | 3 | 729 | Risk Ratio (IV, Fixed, 95% CI) | 0.48 [0.21, 1.12] |
| 5.3 Policy about routine EFM not known | 1 | 428 | Risk Ratio (IV, Fixed, 95% CI) | 1.98 [0.76, 5.18] |
| 6 Postpartum depression | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Setting had routine EFM | 1 | 6915 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.75, 1.05] |
| 6.2 Setting did not have routine EFM | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.18 [0.09, 0.36] |
| 7 Negative rating of/negative views about birth experience | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Setting had routine EFM | 4 | 7467 | Risk Ratio (IV, Fixed, 95% CI) | 0.67 [0.60, 0.76] |
| 7.2 Setting did not have routine EFM | 4 | 1710 | Risk Ratio (IV, Fixed, 95% CI) | 0.60 [0.53, 0.68] |
| 7.3 Policy about routine EFM not known | 3 | 1977 | Risk Ratio (IV, Fixed, 95% CI) | 0.84 [0.65, 1.08] |
| 8 Breastfeeding at 1-2 months postpartum | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Setting had routine EFM | 1 | 4559 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.92, 1.02] |
| 8.2 Setting did not have routine EFM | 2 | 804 | Risk Ratio (IV, Fixed, 95% CI) | 1.05 [0.98, 1.13] |
Comparison 5.
Continuous support versus usual care - variations in provider characteristics
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any analgesia/anaesthesia | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Support people were hospital staff | 6 | 9152 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.99] |
| 1.2 Support people were not hospital staff and not chosen by woman | 4 | 1790 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.86, 0.97] |
| 1.3 Support people were not hospital staff and were chosen by woman | 4 | 1408 | Risk Ratio (IV, Fixed, 95% CI) | 0.94 [0.88, 1.00] |
| 2 Synthetic oxytocin during labour | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Support people were hospital staff | 6 | 9561 | Risk Ratio (IV, Fixed, 95% CI) | 1.06 [1.01, 1.11] |
| 2.2 Support people were not hospital staff and not chosen by woman | 3 | 1018 | Risk Ratio (IV, Fixed, 95% CI) | 0.69 [0.50, 0.94] |
| 2.3 Support people were not hospital staff and were chosen by woman | 6 | 2041 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.96, 1.01] |
| 3 Spontaneous vaginal birth | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Support people were hospital staff | 9 | 10813 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [1.01, 1.06] |
| 3.2 Support people were not hospital staff and were chosen by woman | 5 | 1470 | Risk Ratio (IV, Fixed, 95% CI) | 1.07 [0.99, 1.15] |
| 3.3 Support people were not hospital staff and not chosen by woman | 5 | 1935 | Risk Ratio (IV, Fixed, 95% CI) | 1.12 [1.07, 1.17] |
| 4 Caesarean birth | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Support people were hospital staff | 9 | 10786 | Risk Ratio (IV, Fixed, 95% CI) | 0.95 [0.85, 1.05] |
| 4.2 Support people were not hospital staff and not chosen by woman | 7 | 2330 | Risk Ratio (IV, Fixed, 95% CI) | 0.72 [0.60, 0.86] |
| 4.3 Support people were not hospital staff and were chosen by woman | 6 | 2059 | Risk Ratio (IV, Fixed, 95% CI) | 0.83 [0.69, 1.01] |
| 5 Admission to special care nursery | 7 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Support people were hospital staff | 3 | 7428 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.84, 1.17] |
| 5.2 Support people were not hospital staff and not chosen by woman | 2 | 829 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.66, 1.12] |
| 5.3 Support people were not hospital staff and were chosen by woman | 2 | 640 | Risk Ratio (IV, Fixed, 95% CI) | 1.40 [0.67, 2.93] |
| 6 Postpartum depression | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Support people were hospital staff | 1 | 5567 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.73, 1.02] |
| 6.2 Support people were not hospital staff and not chosen by woman | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.17 [0.09, 0.33] |
| 6.3 Support people were not hospital staff and were chosen by woman | 0 | 0 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Negative rating of/negative feelings about birth experience | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Support people were hospital staff | 4 | 8145 | Risk Ratio (IV, Fixed, 95% CI) | 0.87 [0.73, 1.03] |
| 7.2 Support people were not hospital staff and not chosen by woman | 3 | 1325 | Risk Ratio (IV, Fixed, 95% CI) | 0.66 [0.57, 0.77] |
| 7.3 Support people were not hospital staff and were chosen by woman | 4 | 1708 | Risk Ratio (IV, Fixed, 95% CI) | 0.57 [0.51, 0.64] |
| 8 Breastfeeding at 1-2 months postpartum | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only |
REFERENCES
References to studies included in this review
- Breart - Belgium 1992.* Breart G, Garel M, Mlika-Cabanne N. Evaluation of different policies of management of labour for primiparous women. Trial B: Results of the continuous professional support trial. In: Kaminski M, editor. Evaluation in Pre-, Peri-, and Post-Natal Care Delivery Systems. INSERM; Paris: 1992. pp. 57–68. [Google Scholar]; Breart G, Mlika-Cabane N, Kaminski M. The evaluation of different policies for the management of labour. Proceedings of 3rd European Health Services Research Meeting; London, UK. 1991 Dec 13-14.1991. [Google Scholar]; Breart G, Mlika-Cabane N, Kaminski M, Alexander S, Herruzo-Nalda A, Mandruzzato P, et al. Evaluation of different policies for the management of labour. Early Human Development. 1992;29:309–12. doi: 10.1016/0378-3782(92)90183-h. [DOI] [PubMed] [Google Scholar]; Breart G, Mlika-Cabane N, Thornton J, Trakas D, Alexander S, Mandruzzato P, et al. European trials on artificial rupture of membranes and professional support during labour. Journal of Perinatal Medicine. 1992;20(Suppl 1):37. [Google Scholar]
- Breart - France 1992.* Breart G, Garel M, Mlika-Cabanne N. Evaluation of different policies of management of labour for primiparous women. Trial B: Results of the continuous professional support trial. In: Kaminski M, editor. Evaluation in Pre-, Peri-, and Post-natal Care Delivery Systems. INSERM; Paris: 1992. pp. 57–68. [Google Scholar]; Breart G, Mlika-Cabane N, Kaminski M. The evaluation of different policies for the management of labour. Proceedings of 3rd European Health Services Research Meeting; London, UK. 1991 Dec 13-14.1991. [Google Scholar]; Breart G, Mlika-Cabane N, Kaminski M, Alexander S, Herruzo-Nalda A, Mandruzzato P, et al. Evaluation of different policies for the management of labour. Early Human Development. 1992;29:309–12. doi: 10.1016/0378-3782(92)90183-h. [DOI] [PubMed] [Google Scholar]; Breart G, Mlika-Cabane N, Thornton J, Trakas D, Alexander S, et al. European trials on artificial rupture of membranes and professional support during labour. Journal of Perinatal Medicine. 1992;20(Suppl 1):37. [Google Scholar]
- Breart - Greece 1992.* Breart G, Garel M, Mlika-Cabanne N. Evaluation of different policies of management of labour for primiparous women. Trial B: Results of the continuous professional support trial. In: Kaminski M, editor. Evaluation in Pre-, Peri-, and Post-Natal Care Delivery Systems. INSERM; Paris: 1992. pp. 57–68. [Google Scholar]; Breart G, Mlika-Cabane N, Kaminski M. The evaluation of different policies for the management of labour. Proceedings of 3rd European Health Services Research Meeting; London, UK. 1991 Dec 13-14.1991. [Google Scholar]; Breart G, Mlika-Cabane N, Kaminski M, Alexander S, Herruzo-Nalda A, Mandruzzato P, et al. Evaluation of different policies for the management of labour. Early Human Development. 1992;29:309–12. doi: 10.1016/0378-3782(92)90183-h. [DOI] [PubMed] [Google Scholar]; Breart G, Mlika-Cabane N, Thornton J, Trakas D, Alexander S, et al. European trials on artificial rupture of membranes and professional support during labour. Journal of Perinatal Medicine. 1992;20(Suppl 1):37. [Google Scholar]
- Bruggemann 2007.Bruggemann OM, Parpinelli MA, Osis MJD, Cecatti JG, Neto ASC. Support to woman by a companion of her choice during childbirth: a randomized controlled trial. Reproductive Health. 2007;4:5. doi: 10.1186/1742-4755-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell 2006.Campbell D, Scott KD, Klaus MH, Falk M. Female relatives or friends trained as labor doulas: outcomes at 6 to 8 weeks postpartum. Birth. 2007;34(3):220–7. doi: 10.1111/j.1523-536X.2007.00174.x. [DOI] [PubMed] [Google Scholar]; * Campbell DA, Lake MF, Falk M, Backstrand JR. A randomized control trial of continuous support in labor by a lay doula. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2006;35(4):456–64. doi: 10.1111/j.1552-6909.2006.00067.x. [DOI] [PubMed] [Google Scholar]
- Cogan 1988.Cogan R, Spinnato JA. Social support during premature labor: effects on labor and the newborn. Journal of Psychosomatic Obstetrics and Gynaecology. 1988;8:209–16. [Google Scholar]
- Dickinson 2002.Dickinson JE, Paech MJ, McDonald SJ, Evans SF. Maternal satisfaction with childbirth and intrapartum analgesia in nulliparous labour. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2003;43:463–8. doi: 10.1046/j.0004-8666.2003.00152.x. [DOI] [PubMed] [Google Scholar]; * Dickinson JE, Paech MJ, McDonald SJ, Evans SF. The impact of intrapartum analgesia on labour and delivery outcomes in nulliparous women. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2002;42(1):59–66. doi: 10.1111/j.0004-8666.2002.00065.x. [DOI] [PubMed] [Google Scholar]; Henderson JJ, Dickinson JE, Evans SF, McDonald SJ, Paech MJ. Impact of intrapartum epidural analgesia on breast-feeding duration. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2003;43:372–7. doi: 10.1046/j.0004-8666.2003.t01-1-00117.x. [DOI] [PubMed] [Google Scholar]
- Gagnon 1997.Gagnon A, Waghorn K. One-to-one nurse labor support of nulliparous women stimulated with oxytocin. Journal of Obstetric, Gynecologic and Neonatal Nursing. 1999;28:371–6. doi: 10.1111/j.1552-6909.1999.tb02005.x. [DOI] [PubMed] [Google Scholar]; * Gagnon A, Waghorn K, Covell C. A randomized trial of one-to-one nurse support of women in labor. Birth. 1997;24:71–7. [PubMed] [Google Scholar]
- Hemminki 1990a.Hemminki E, Virta AL, Koponen P, Malin M, Kojo-Austin H, Tuimala R. A trial on continuous human support during labor: feasibility, interventions and mothers’ satisfaction. (Trial A - Pilot study with volunteered midwifery students) Journal of Psychosomatic Obstetrics and Gynaecology. 1990;11:239–50. [Google Scholar]
- Hemminki 1990b.Hemminki E, Virta AL, Koponen P, Malin M, Kojo-Austin H, Tuimala R. A trial on continuous human support during labor: feasibility, interventions and mothers’ satisfaction. (Trial A - Pilot study with volunteered midwifery students) Journal of Psychosomatic Obstetrics and Gynaecology. 1990;11:239–50. [Google Scholar]
- Hodnett 1989.Hodnett ED, Osborn RW. A randomized trial of the effects of monitrice support during labor: mothers’ views two to four weeks postpartum. Birth. 1989;16:177–83. doi: 10.1111/j.1523-536x.1989.tb00893.x. [DOI] [PubMed] [Google Scholar]; * Hodnett ED, Osborn RW. Effects of continuous intrapartum professional support on childbirth outcomes. Research in Nursing and Health. 1989;12:289–97. doi: 10.1002/nur.4770120504. [DOI] [PubMed] [Google Scholar]
- Hodnett 2002.* Hodnett ED, Lowe NK, Hannah ME, Willan AR, Stevens B, Weston JA, et al. Effectiveness of nurses as providers of birth labor support in North American hospitals. A randomized controlled trial. JAMA. 2002;288(11):1373–81. doi: 10.1001/jama.288.11.1373. [DOI] [PubMed] [Google Scholar]; Muir HA, Hodnett ED, Hannah ME, Lowe NK, Willan AR, Stevens B, et al. The influence of continuous labor support on the choice of analgesia, ambulation and obstetric outcome [abstract] Anesthesiology. 2002;96(Suppl 1):P44. [Google Scholar]
- Hofmeyr 1991.Chalmers B, Wolman WL, Hofmeyr GJ, Nikodem C. Companionship in labour: effect on the mother-infant relationship. Proceedings of the International Conference on Primary Care Obstetrics and Perinatal Health; Utrecht, The Netherlands. 1991.1991. p. 50. [Google Scholar]; Chalmers B, Wolman WL, Hofmeyr GJ, Nikodem C. Companionship in labour and the mother-infant relationship: preliminary report of a randomised trial. Proceedings of the 9th Conference on Priorities in Perinatal Care; Johannesburg, South Africa. 1990 March.1990. pp. 139–41. [Google Scholar]; Gulmezoglu AM, Chalmers BE, Nikodem VC, Wolman WL, Hofmeyr GJ. Companionship in labour: do the personality characteristics of labour supporters influence effectiveness?. Proceedings of the 11th Conference on Priorities in Perinatal Care in South Africa; Caledon, South Africa. 1992 March.1992. pp. 115–6. [Google Scholar]; Hofmeyr GJ, Nikodem C, Gulmezoglu M, Wolman WL. Companionship to modify the clinical birth environment: long-term effects on mother and child. Proceedings of the 11th Conference on Priorities in Perinatal Care in South Africa; Caledon, South Africa. 1992 March.1992. pp. 113–4. [Google Scholar]; Hofmeyr GJ, Nikodem C, Gulmezoglu M, Wolman WL. Companionship to modify the clinical birth environment: long-term effects on mother and child. Proceedings of the 26th British Congress of Obstetrics and Gynaecology; Manchester, UK. 1992 July 7-10.1992. p. 34. [Google Scholar]; Hofmeyr GJ, Nikodem VC, Chalmers BE, Kramer T. Clinically orientated care during labour reduces the chance of successful breastfeeding. Proceedings of the 10th Conference on Priorities in Perinatal Care in South Africa; Eastern Transvaal, South Africa. 1991 March 12-15.1991. pp. 107–9. [Google Scholar]; Hofmeyr GJ, Nikodem VC, Mahomed K, Gulmezoglu AM, Lawson M, Van Der Walt LA, et al. Companionship to modify the clinical birth environment: no measurable effect on stress hormone levels. Journal of Obstetrics and Gynaecology. 1995;15:178–81. [Google Scholar]; * Hofmeyr GJ, Nikodem VC, Wolman WL, Chalmers BE, Kramer T. Companionship to modify the clinical birth environment: effects on progress and perceptions of labour, and breastfeeding. British Journal of Obstetrics and Gynaecology. 1991;98:756–64. doi: 10.1111/j.1471-0528.1991.tb13479.x. [DOI] [PubMed] [Google Scholar]; Nikodem VC, Nolte AG, Wolman W, Gulmezoglu AM, Hofmeyr GJ. Companionship by a lay labour supporter to modify the clinical birth environment: long-term effects on mother and child. Curationis. 1998;21(1):8–12. doi: 10.4102/curationis.v21i1.596. [DOI] [PubMed] [Google Scholar]; Trotter C, Wolman WL, Hofmeyr J, Nikodem C, Turton R. The effect of social support during labour on postpartum depression. South African Journal of Psychology. 1992;22(3):134–9. [Google Scholar]; Wolman WL, Chalmers B, Hofmeyr J, Nikodem VC. Postpartum depression and companionship in the clinical birth environment: a randomized, controlled study. American Journal of Obstetrics and Gynecology. 1993;168:1388–93. doi: 10.1016/s0002-9378(11)90770-4. [DOI] [PubMed] [Google Scholar]
- Kashanian 2010.Kashanian M, Javadi F, Haghighi MM. Effect of continuous support during labor on duration of labor and rate of cesarean delivery. International Journal of Gynecology & Obstetrics. 2010;109(3):198–200. doi: 10.1016/j.ijgo.2009.11.028. [DOI] [PubMed] [Google Scholar]
- Kennell 1991.* Kennell J, Klaus M, McGrath S, Robertson S, Hinkley C. Continuous emotional support during labor in a US hospital. JAMA. 1991;265:2197–201. [PubMed] [Google Scholar]; Kennell J, Klaus M, McGrath S, Robertson S, Hinkley C. Medical intervention: the effect of social support during labour. Proceedings of Annual Meeting of the American Pediatric Society/Society for Pediatric Research; USA. 1988 May.1988. [Google Scholar]; Kennell J, McGrath S, Klaus M, Robertson S, Hinkley C. Labor support: what’s good for the mother is good for the baby. Pediatric Research. 1989;25:15A. [Google Scholar]; Martin S, Landry S, Stellman L, Kennell J, McGrath S. The effect of doula support during labor on mother-infant interaction at 2 months. Infant Behaviour and Development. 1998;21(Supp1):556. [Google Scholar]
- Klaus 1986.Klaus MH, Kennell JH, Robertson SS, Sosa R. Effects of social support during parturition on maternal and infant morbidity. British Medical Journal. 1986;293:585–7. doi: 10.1136/bmj.293.6547.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer 1998.Campero L, Garcia C, Diaz C, Ortiz O, Reynoso S, Langer A. “Alone, I wouldn’t have known what to do”: a qualitative study on social support during labor and delivery in Mexico. Social Science and Medicine. 1998;47:395–403. doi: 10.1016/s0277-9536(98)00077-x. [DOI] [PubMed] [Google Scholar]; * Langer A, Campero L, Garcia C, Reynoso S. Effects of psychosocial support during labour and childbirth on breastfeeding, medical interventions, and mothers’ wellbeing in a Mexican public hospital: a randomised clinical trial. British Journal of Obstetrics and Gynaecology. 1998;105:1056–63. doi: 10.1111/j.1471-0528.1998.tb09936.x. [DOI] [PubMed] [Google Scholar]
- Madi 1999.Madi BC, Sandall J, Bennett R, MacLeod C. Effects of female relative support in labor: a randomized controlled trial. Birth. 1999;26:4–8. doi: 10.1046/j.1523-536x.1999.00004.x. [DOI] [PubMed] [Google Scholar]
- McGrath 2008.McGrath SK, Kennell JH. A randomized controlled trial of continuous labor support for middle-class couples: effect on cesarean delivery rates. Birth. 2008;35(2):92–7. doi: 10.1111/j.1523-536X.2008.00221.x. [DOI] [PubMed] [Google Scholar]
- Morhason-Bello 2009.Morhason-Bello IO, Adedokun BO, Ojengbede OA. Social support during childbirth as a catalyst for early breastfeeding initiation for first-time Nigerian mothers. International Breastfeeding Journal. 2009;4:16. doi: 10.1186/1746-4358-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]; * Morhason-Bello IO, Adedokun BO, Ojengbede OA, Olayemi O, Oladokun A, Fabamwo AO. Assessment of the effect of psychosocial support during childbirth in Ibadan, south-west Nigeria: a randomised controlled trial. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2009;49(2):145–50. doi: 10.1111/j.1479-828X.2009.00983.x. [DOI] [PubMed] [Google Scholar]; Ojengbede O, Morhason-Bello I, Adedokun B, Becker S, Oni G, Tsui A. Psycho-social support in labour, as a catalyst for contraceptive uptake in Nigeria: preliminary analysis of a randomised controlled trial. International Journal of Gynecology & Obstetrics. 2009;107(Suppl 2):S623–S624. [Google Scholar]
- Thomassen 2003.Thomassen P, Lundwall M, Wiger E, Wollin L, Uvnas-Moberg K. Lakartidningen. Doula--a new concept in obstetrics [Doula—-ett nytt begrepp inom forlossningsvarden] Lakartidningen. 2003;100(51-52):4268–71. [PubMed] [Google Scholar]
- Torres 1999.Kopplin E, Torres-Pereyra J, Peña V, Salinas R. Impact of psychosocial supports during childbirth: the decrease of caesarean and bonuses of the process. Pediatric Research. 2000;47:834. [Google Scholar]; * Torres J, Kopplin E, Pena V, Klaus M, Salinas R, Herrera M. Impact of emotional support during labour in the decrease of caesarean sections and satisfaction with the process [Impacto del apoyo emocional durante el parto en la disminucion de cesareas y gratificacion del proceso] Revista Chilena de Obstetricia y Ginecologia. 1999;64(5):405–12. [Google Scholar]
- Yuenyong 2012.Yuenyong S, O’Brien B, Jirapeet V. Effects of labor support from close female relative on labor and maternal satisfaction in a Thai setting. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2012;41(1):45–56. doi: 10.1111/j.1552-6909.2011.01311.x. [DOI] [PubMed] [Google Scholar]
- Bender 1968.Bender B. A test of the effects of nursing support on mothers in labor. ANA Regional Clinical Conferences 1967 Philadelphia/Kansas City; New York: Appleton-Century-Crofts; 1968. pp. 171–9. [PubMed] [Google Scholar]
- Bochain 2000.Bochain SS. Induced labor intervention for self-efficacy: a nursing intervention for women prone to an unpredictable labor pattern [thesis] University of Rhode Island; Rhode Island: 2000. [Google Scholar]
- Brown 2007.Brown H, Hofmeyr GJ, Nikodem VC, Smith H, Garner P. Promoting childbirth companions in South Africa: a randomised pilot study. BMC Medicine. 2007;5:7. doi: 10.1186/1741-7015-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalal 2006.Dalal R, Rathnakumar Santamani. Birth companion and mother - a preliminary report [abstract]. 49th All India Congress of Obstetrics and Gynaecology; Kerala State, India. 2006 Jan 6-9; 2006. p. 140. [: 8E10.0007M] [Google Scholar]
- Gordon 1999.Gordon NP, Walton D, McAdam E, Derman J, Gallitero G, Garrett L. Effects of providing hospital-based doulas in health maintenance organization hospitals. Obstetrics & Gynecology. 1999;93:422–6. doi: 10.1016/s0029-7844(98)00430-x. [DOI] [PubMed] [Google Scholar]
- Hemminki 1990c.Hemminki E, Virta AL, Koponen P, Malin M, Kojo-Austin H, Tuimala R. A trial on continuous human support during labor: feasibility, interventions and mothers’ satisfaction. (Trial C - Pilot study with lay women) Journal of Psychosomatic Obstetrics and Gynaecology. 1990;11:239–50. [Google Scholar]
- Lindow 1998.Lindow SW, Hendricks MW, Thompson JW, van der Spuy ZM. The effect of emotional support on maternal oxytocin levels in labouring women. European Journal of Obstetrics & Gynecology and Reproductive Biology. 1998;79:127–9. doi: 10.1016/s0301-2115(98)00073-6. [DOI] [PubMed] [Google Scholar]
- McGrath 1999.McGrath S, Kennell J, Suresh M, Moise K, Hinkley C. Doula support vs epidural analgesia: impact on cesarean rates. Pediatric Research. 1999;Vol. 45(issue 4):16A. [Google Scholar]
- Orenstein 1998.Manning Orenstein G. A birth intervention: the therapeutic effects of doula support versus Lamaze preparation on first-time mothers’ working models of caregiving. Alternative Therapies in Medicine. 1998;4(4):73–81. [PubMed] [Google Scholar]
- Pinheiro 1996.Pinheiro RT, Sousa PLR, Horta B, de Souza RM, de Sousa MGR, de Sousa FR. Male and female young doulas - effective on labour? [abstract]. Xth World Congress of Psychiatry; Madrid, Spain. 1996 August 23-28.1996. [Google Scholar]
- Ran 2005.Ran KQ, He AM, Han QR, Tang ZL, Lei FH. Comfortable nursing and the mental state in parturient women. Chinese Journal of Clinical Rehabilitation. 2005;9(32):62–3. [Google Scholar]
- Scott 1999.Scott KD, Klaus PH, Klaus MH. The obstetrical and postpartum benefits of continuous support during childbirth. Journal of Women’s Health & Gender-Based Medicine. 1999;8(10):1257–64. doi: 10.1089/jwh.1.1999.8.1257. [DOI] [PubMed] [Google Scholar]
- Sosa 1980.Sosa R, Kennell J, Klaus M, Urrutia J. The effect of a supportive woman on mothering behavior and the duration and complications of labor. Pediatric Research. 1979;13:338. [Google Scholar]; * Sosa R, Kennell JH, Klaus MH, Robertson S, Urrutia J. The effect of a supportive companion on perinatal problems, length of labor, and mother-infant interaction. New England Journal of Medicine. 1980;303:597–600. doi: 10.1056/NEJM198009113031101. [DOI] [PubMed] [Google Scholar]
- Trueba 2000.Trueba G, Contreras C, Velazco MT, Lara EG, Martinez HB. Alternative strategy to decrease cesarean section: support by doulas during labor. Journal of Perinatal Education. 2000;9(2):8–13. doi: 10.1624/105812400X87608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tryon 1966.Tryon PA. Use of comfort measures as support during labor. Nursing Research. 1966;15(2):109–18. [PubMed] [Google Scholar]
- Zhang 1996.Zhang CL, Yu ZJ, Feng AH. Study of psychological nursing to ease pain during labour. Chinese Journal of Nursing. 1996;31(6):311–3. [PubMed] [Google Scholar]
- Dong 2009.Dong X, Qi H, Hu L, Luo X, Zhu Y, Cai J. The effects of air sac combined with nitrous oxide and Doula companying delivery in vaginal delivery. International Journal of Gynecology and Obstetrics. 2009;107:S158–S159. [Google Scholar]
- Huang 2003.Huang XH, Xiang XY, Shen RG, Shang Q, Zhu LP, Qian X, et al. Study on intrapartum service model during normal labor. Chung-Hua Fu Chan Ko Tsa Chih [Chinese Journal of Obstetrics & Gynecology] 2003;38(7):385–7. [PubMed] [Google Scholar]
- Orbach-Zinger 2012.Orbach-Zinger S, Ginosar Y, Sverdlik J, Treitel C, Mackersey K, Bardin R, et al. Partner’s presence during initiation of epidural labor analgesia does not decrease maternal stress: a prospective randomized controlled trial. Anesthesia and Analgesia. 2012;114(3):654–60. doi: 10.1213/ANE.0b013e318241f4f3. [DOI] [PubMed] [Google Scholar]
- Riley 2012.Riley L, Hutchings Y, Lieberman E. The effect of doula support on epidural use among nulliparous women in tertiary care centers. American Journal of Obstetrics and Gynecology. 2012;206(Suppl 1):S70–S71. [Google Scholar]
- Sangestani.Sangestani G. [accessed 10 March 2012];The influence of doula on the parturient anxiety in delivery ward. 2011 http://www.irct.ir/searchresult.php?id=6827&number=2
- Shen.Shen XF. [accessed 7 March 2012];Doula combined latent phrase epidural analgesia in primiparous women (DCLEAP) http://clinicaltrials.gov/ct2/show/record/NCT00664118
- Wan 2011.Wan H, Hu S, Thobaben M, Hou Y, Yin T. Continuous primary nursing care increases satisfaction with nursing care and reduces postpartum problems for hospitalized pregnant women. Contemporary Nurse. 2011;37(2):149–59. doi: 10.5172/conu.2011.37.2.149. [DOI] [PubMed] [Google Scholar]
- Janssen.Janssen P. [accessed 15 February 2012];Impact of doula support on intrapartum outcomes for women undergoing a vaginal birth after cesarean (vbac) http://clinicaltrials.gov/ct2/show/record/NCT01216098
- Anim-Somuah 2011.Anim-Somuah M, Smyth RMD, Jones L. Art. No.: CD000331. Epidural versus non-epidural or no analgesia in labour. Cochrane Database of Systematic Reviews. 2011;(Issue 12) doi: 10.1002/14651858.CD000331.pub3. [DOI: 10.1002/14651858.CD000331.pub3] [DOI] [PubMed] [Google Scholar]
- Avan 2010.Avan B, Richter LM, Ramchandani PG, Norris SA, Stein A. Maternal postnatal depression and children’s growth and behaviour during the early years of life: exploring the interaction between physical and mental health. Archives of Disease in Childhood. 2010;95(9):690–5. doi: 10.1136/adc.2009.164848. [DOI] [PubMed] [Google Scholar]
- AWHONN 2002.Association of Women’s Health, Obstetric, Neonatal Nurses [accessed 2002];Professional nursing support of laboring women. http://www.awhonn.org
- Caton 2002.Caton D, Corry MP, Frigoletto FD, Hopkins DP, Lieberman E, Mayberry L, et al. The nature and management of labor pain: executive summary. American Journal of Obstetrics and Gynecology. 2002;186(5):S1–S15. doi: 10.1016/S0002-9378(02)70178-6. [DOI] [PubMed] [Google Scholar]
- Declercq 2002.Declercq ER, Sakala C, Corry MP, Applebaum S, Risher P. Listening to mothers: report of the first national US survey of women’s childbearing experiences. Maternity Center Association; New York: Oct, 2002. [Google Scholar]
- Declercq 2006.Declercq GD, Sakala C, Corry MP, Applebaum S. Listening to mothers: report of the second national U.S. survey of women’s childbearing experiences. Childbirth Connection; New York: 2006. [Google Scholar]
- Higgins 2011.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; [updated March 2011]. 2011. Available from www.cochrane-handbook.org. [Google Scholar]
- Hodnett 1997.Hodnett E. Are nurses effective providers of labor support? Should they be? Can they be? Birth. 1997;24:78–80. [PubMed] [Google Scholar]
- Hodnett 2002a.Hodnett ED. Pain and women’s satisfaction with the experience of childbirth: a systematic review. American Journal of Obstetrics and Gynecology. 2002;186(5):S160–S172. doi: 10.1067/mob.2002.121141. [DOI] [PubMed] [Google Scholar]
- Klaus 2002.Klaus MH, Kennell JH, Klaus PH. The doula book: how a trained labor companion can help you have a shorter, easier and healthier birth. 2nd Edition Perseus Books; Cambridge, MA: 2002. [Google Scholar]
- Lederman 1978.Lederman RP, Lederman E, Work BA, Jr, McCann DS. The relationship of maternal anxiety, plasma catecholamines, and plasma cortisol to progress in labor. American Journal of Obstetrics and Gynecology. 1978;132(5):495–500. doi: 10.1016/0002-9378(78)90742-1. [DOI] [PubMed] [Google Scholar]
- Lederman 1981.Lederman E, Lederman RP, Work BA, Jr, McCann DS. Maternal psychological and physiologic correlates of fetal-newborn health status. American Journal of Obstetrics and Gynecology. 1981;139(8):956–8. doi: 10.1016/0002-9378(81)90967-4. [DOI] [PubMed] [Google Scholar]
- McGinnis 2001.McGinnis S. On being a doula. MIDIRS Midwifery Digest. 2001;11(3):362–4. [Google Scholar]
- MIDIRS 1999.MIDIRS and the NHS Centre for Reviews and Dissemination . Support in labour: informed choice for professionals leaflet. Midwives Information and Resource Service; Bristol, England: 1999. [Google Scholar]
- NICE Intrapartum Care 2007.National Collaborating Centre for Women’s and Children’s Health . Section 4.3. Support in labour. Intrapartum Care: Care of Healthy Women and Their Babies During Childbirth. RCOG press; London: Sep, 2007. pp. 73–5. [PubMed] [Google Scholar]
- Pascali-Bonaro 2010.Pascali-Bonaro D. Global labor support trends. Jun 5, 2010. Personal communication.
- RevMan 2011.The Nordic Cochrane Centre, The Cochrane Collaboration . Review Manager (RevMan). 5.1. The Nordic Cochrane Centre, The Cochrane Collaboration; Copenhagen: 2011. [Google Scholar]
- Simkin 2007.Simkin P. The Birth Partner: A Complete Guide to Childbirth for Dads, Doulas, and Other Labor Companions. 3rd Edition Harvard Common Press; Boston: 2007. [Google Scholar]
- SOGC 1995.Society of Obstetricians and Gynaecologists of Canada SOGC policy statement: fetal health surveillance in labour. SOGC News. 1995;41:5. [Google Scholar]
- WHO 2010. [accessed 2010];Labour companionship: every woman’s choice. WHO Reproductive Health Library. http://apps.who.int/rhl/videos/en/index.html
- Hodnett 2003.Hodnett ED, Gates S, Hofmeyr GJ, Sakala Continuous support for women during childbirth. Cochrane Database of Systematic Reviews. 2003;(Issue 3) doi: 10.1002/14651858.CD003766. [DOI: 10.1002/14651858.CD003766] [DOI] [PubMed] [Google Scholar]
- Hodnett 2011.Hodnett ED, Gates S, Hofmeyr GJ, Sakala C, Weston J. Continuous support for women during childbirth. Cochrane Database of Systematic Reviews. 2011;(Issue 2) doi: 10.1002/14651858.CD003766.pub3. [DOI: 10.1002/14651858.CD003766.pub3] [DOI] [PubMed] [Google Scholar]
- *Indicates the major publication for the study