Abstract
Chondral injuries of the hip joint are often symptomatic and affect patient activity level. Several procedures are available for addressing chondral injuries, including microfracture. Microfracture is a marrow-stimulating procedure, which creates subchondral perforation in the bone, allowing pluripotent mesenchymal stem cells to migrate from the marrow into the chondral defect and form fibrocartilaginous tissue. In the knee, microfracture has been shown to relieve pain symptoms. In the hip, microfracture has been studied to a lesser extent, but published studies have shown promising clinical outcomes. The depth, joint congruity, and geometry of the hip joint make microfracture technically challenging. The most common technique uses hip-specific microfracture awls, but the trajectory of impaction is not perpendicular to the subchondral plate. Consequently, the parallel direction of impaction creates poorly defined channels. We describe an arthroscopic microfracture technique for the hip using a flexible microfracture drill. The drill and angled guides simplify access to the chondral defect. The microfracture drill creates clear osseous channels, avoiding compaction of the surrounding bone and obstruction of the channels. Furthermore, this technique allows for better control of the angle and depth of the drill holes, which enhances reproducibility and may yield improved clinical outcomes.
Diagnosis and treatment of hip pathology offer many challenges for orthopaedic surgeons. With recent advances in the understanding of nonarthritic hip conditions, a number of hip pathologies are being addressed through the use of arthroscopic techniques, including chondral injuries. Ganz and colleagues1 described the concept of femoroacetabular impingement (FAI) to characterize the pathomechanical process in which subtle deformities in the acetabulum and proximal femur lead to repetitive injury to the chondrolabral junction. Often, focal chondral defects are identified at the time of surgery to address labral injury and deformities of the acetabulum and femoral head-neck junction. Depending on the size, location, and International Cartilage Repair Society grade, chondral injuries can be treated with arthroscopic debridement for partial-thickness lesions or microfracture for full-thickness lesions.
Microfracture
Microfracture techniques have primarily been used in the treatment of chondral injuries of the knee, whereas microfracture of the hip has been studied to a lesser degree.2 A literature search identified only 6 studies focusing specifically on microfracture of the hip, four of which focused on clinical outcomes of the procedure (Table 1). The procedure uses arthroscopic instruments to create perforations in the bone to provide a conduit for undifferentiated stem cells to migrate from the marrow into the area of the defect to form a clot. This clot provides the environment for the pluripotent and mesenchymal cells to differentiate and form fibrocartilaginous tissue filling the defect.2,7 Although the new fibrocartilage lacks the biomechanical properties of native hyaline articular cartilage, specifically in its ability to tolerate sheer stresses,8 it has been shown to relieve symptoms in 70% to 90% of patients undergoing knee microfracture.7
Table 1.
Outcome Studies of Arthroscopic Microfracture of Hip
| Authors | Year | Total No. of Patients | No. Receiving Microfracture | Mean Patient Age (range) (yr) | Follow-up (mo) | Outcomes |
|---|---|---|---|---|---|---|
| Byrd and Jones3 | 2002 | 9 | 3 | 51 (32-64) | Minimum, 24 | A mean MHHS improvement of 36 points occurred in the microfracture group compared with 2 points in the debridement group; only microfracture patients returned to activities beyond simple activities of daily living. |
| Haviv et al.4 | 2010 | 166 | 29 | 37 (14-78) | Mean, 22 | The NAHS was significantly better in patients who underwent microfracture. The NAHS improved by 20 points in the microfracture group (P < .001), as compared with 13 points in the debridement group (P = .003). |
| Karthikeyan et al.6 | 2012 | 20 | 20 | 37 (17-54) | Mean, 17 | Mean defect filling of 96% was observed in 19 of 20 patients on second-look hip arthroscopy, and the NAHS showed a mean improvement of 23 points. |
| Philippon et al.5 | 2008 | 9 | 9 | 37 (21-47) | Mean, 20 | Defect filling of 95%-100% was observed in 8 of 9 patients on second-look hip arthroscopy. |
NOTE. The studies by Byrd and Jones and Haviv et al. evaluated clinical outcomes of the procedure using the MHHS and NAHS, which were significantly improved in the microfracture group when compared with the debridement-only group at a mean of 23 months' follow-up. The studies by Karthikeyan et al. and Philippon et al. reported results from second-look arthroscopies 17 to 20 months after microfracture. Both studies reported 95% to 100% defect filling with fibrocartilage in most patients. One patient in each study had 20% to 25% filling—results that were attributed to severe osteoarthritis of the joints.
MHHS, Modified Harris Hip Score; NAHS, Non-Arthritic Hip Score.
The standard technique, adapted from the knee, uses longer microfracture awls to accommodate the hip joint. However, these instruments have limitations because of the direction of impaction of the awls. Because of the inherent constraints of the hip, drilling with curved guides has become an attractive alternative; this allows the drill to be directed perpendicular to the subchondral bone, allowing for more precise osseous channels.
Operative Technique
At our institution, hip arthroscopy is performed with the patient in the supine position, by use of traction, a well-padded perineal post, and fluoroscopy (Fig 1). The hip is distracted in neutral extension using adduction maneuvers. Three portals are used for this procedure: anterolateral portal, mid-anterior portal, and distal accessory anterolateral portal (4 cm distal to anterolateral portal) (Fig 1 and Table 2). These portals are created in standard fashion using cannulated instruments (spinal needle, guidewire, and metal trocars). Typically, the anterolateral portal is the viewing portal, and the distal accessory anterolateral portal is the working portal. Once the portals are established, a diagnostic arthroscopy is performed with a 70° arthroscope. The location of the focal chondral defects varies, but they are generally located in the anterosuperior quadrant of the hip joint.
Fig 1.

Operative setup. The patient is placed in the supine position. The hip is distracted in neutral extension by use of adduction maneuvers against a well-padded perineal post. Three portals are established in standard fashion using fluoroscopy and cannulated instruments, a spinal needle, a guidewire, and metal trocars. The procedure uses an anterolateral portal, mid-anterior portal, and accessory anterolateral portal (approximately 4 cm distal to anterolateral portal).
Table 2.
Technique Tips and Pearls: Step-by-Step Suggestions to Aid Microfracture Procedure Using Flexible Drill System
| Once the portals (anterolateral, mid-anterior, and distal accessory anterolateral) are established, the anterolateral portal is used as the viewing portal. The distal accessory anterolateral portal is the working portal to be used for the curettes, shaver, and drill. |
| The surgeon selects the depth cap and assembles it to the guide handle. Because the width of the cortical bone in the hip may be greater than that in the knee, in which 4 mm is an acceptable hole depth, we prefer to use a 7 mm depth cap to ensure proper access to bone marrow. |
| The surgeon places the guide mouth in the defect site, first drilling holes closest to the arthroscope and then systematically moving away. |
| The surgeon starts the drill on full forward speed before the drill bit makes contact with the bone. He or she drills through the guide continuously on full forward speed to a positive stop. He or she continues to drill on full forward speed while removing the drill. |
| The surgeon should hold both the drill guide and drill. This allows for an immediate instinctive reaction to stop drilling in case the guide should slip. |
Microfracture Technique
After the chondral lesion is identified, unstable flaps of cartilage are debrided with an arthroscopic shaver (Video 1). The rim of the cartilaginous defect is carefully prepared with arthroscopic curettes to create stable cartilage shoulders that are perpendicular to the subchondral surface. Vertical shoulders help contain the marrow clot and create a load-bearing transition zone. The length, width, and depth of the chondral defect are measured with an arthroscopic probe. Any labral pathology requires fixation before microfracture because the peripheral aspect of the focal chondral defect is bordered by the labrum (Fig 2). Next, arthroscopic curettes are used to remove the calcified cartilage layer, which improves clot adhesion. Care is taken not to disrupt the underlying subchondral plate. After preparation of the defect, a flexible arthroscopic microfracture drill is used to make multiple perforations in the exposed subchondral bone. We use the MicroFX OCD Osteochondral Drill System (Stryker, Kalamazoo, MI). Drill guides of varying angles (45°, 70°, 90°) are used to gain access to the lesion. We prefer to use the 70° curved drill guide. Depth caps (4 to 7 mm) are assembled to the guide handle to allow drilling to a predetermined depth. The drill guide is placed against the surface of the lesion at a 90° angle. The hole is made by drilling through the drill guide continuously on full forward speed to a hard stop at the depth allowed by the preselected depth cap. This eliminates the need to approximate the depth of drilling. Studies in the knee have shown that 2 to 4 mm of depth is sufficient to access the marrow elements,2 but there are no studies that have reported the required depth in the hip. Because the depth of the subchondral plate may be wider, we prefer to use 7 mm drill caps to ensure that the adequate depth is achieved. After the hard stop, the drill is removed while continuing on full forward speed. Drill holes are first made around the periphery of the defect. Next, additional holes are made to fill the defect, spaced at 3 to 4 mm from each other to avoid combining holes. As irrigation pressure is decreased, fat and blood droplets should be observed exiting the drill holes.2 Once the procedure is complete, the fluid is drained. The capsule and portals are closed in standard fashion.
Fig 2.
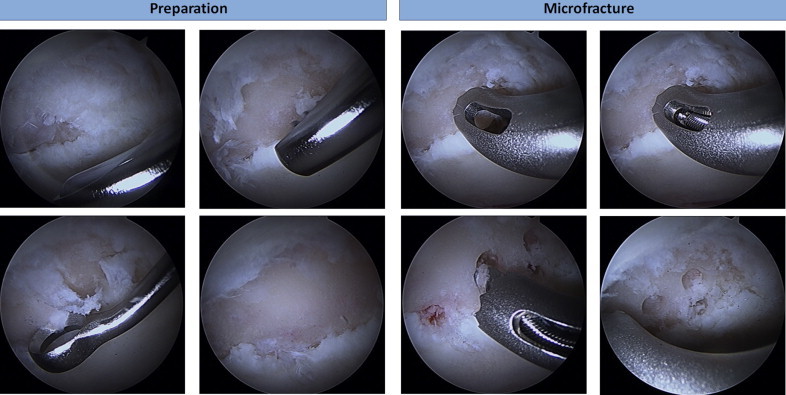
Intraoperative photographs taken with a 70° arthroscope. The left panel shows preparation of the cartilage defect before microfracture using an arthroscopic shaver to debride the frayed cartilage and curettes to create vertical shoulders and remove the calcified cartilage layer. The right panel shows the prepared microfracture site. A drill guide is inserted to establish an orthogonal angle with the bone surface, a flexible drill is threaded through the guide, and perforations are drilled in the bone following a standard pattern. For the purposes of this operation, we used the MicroFX OCD Osteochondral Drill System.
Discussion
Selection of appropriate patients is critical to the success of the operation. Younger patients with focal chondral defects and an otherwise normal articular surface may be good candidates for microfracture, but osseous deformities from FAI should also be addressed to protect the cartilage from repetitive microtrauma.9 Indications for microfracture include focal full-thickness articular cartilage loss in weight-bearing areas and lesions that are smaller than 2 to 4 cm in size.2 Contraindications include partial-thickness defects, lesions associated with bony defects, and cartilage injury induced by immune-mediated or systemic diseases.2
A study of microfracture in the hip by Byrd and Jones3 reported outcomes in 9 patients with acetabular chondral damage. At 2 years follow-up, only the 3 patients who underwent microfracture were able to return to activities beyond the simple activities of daily living. Recently, Karthikeyan et al.6 reported on the macroscopic and microscopic appearance of repair tissue after microfracture for acetabular chondral defects in FAI. At a mean of 17 months follow-up, 19 of 20 patients had mean filling of 96% of the chondral defect. Histologically, the tissue was primarily fibrocartilage. The mean Non-Arthritic Hip Score improved from 54 to 78 points. Philippon et al.5 reported similar results, with 8 of 9 patients achieving 95% to 100% coverage at 20 months. At that time, the appearance of the repaired lesions was consistent with Outerbridge grade I or II.
Hip arthroscopy remains technically demanding, with microfracture adding another layer of complexity. Current instrumentation with standard microfracture awls and curettes makes the procedure exceptionally difficult. Even with good joint visualization, the ability to obtain orthogonal holes in this deep concave surface remains an issue. The procedure described in this report provides several advantages in this respect. The use of a flexible drill with angled drill guides significantly improves our ability to create reproducible depths and organization of our microfracture perforations. The depth caps enable the surgeon to create perforations of adequate and equal depths. The fluted design of the drill tip extracts bone, instead of impacting it, creating a clear channel for the flow of the marrow components. An animal study by Chen et al.10 reported on osteochondral characteristics of tissue after drilling as compared with standard awl microfracture. The study showed that the awl technique fractured and compacted bone around holes, sealing off access to viable marrow, in contrast to drilling. Studies suggest that this may reduce the quality and quantity of repair cartilage. As a result, the use of the drill system may potentially improve the quality of the repair cartilage.
Increased osteocyte death from heat necrosis has been raised as a concern when using drill-based microfracture techniques. However, a recent animal study showed that drilling with cooled irrigation did not produce heat necrosis.10 Among the drawbacks of the technique is the possibility of equipment failure. In certain instances the drill bit may break if the drill is not on full forward speed when the drill contacts the bone. Therefore it is recommended to start the drill on full forward speed before making contact with the bone. In addition, there is a possibility of the drill guide skiving along the bone. Although the mouth of the drill guide has a toothed design to prevent skiving, it is recommended that the surgeon operate both the drill guide and drill to allow for an immediate reaction to stop drilling if the guide should slip.
Microfracture has proven to be an effective method of treating isolated chondral lesions of the knee. The procedure has been shown to produce significant improvement in the visual appearance of lesions and, more importantly, clinical symptoms. However, long-term outcome studies of both the awl-based and drill-based techniques will be needed to compare and contrast the two methods. Furthermore, such investigations will help clarify appropriate indications and contraindications for the procedure.
Footnotes
The authors report the following potential conflict of interest or source of funding: S.J.N. receives support from Stryker, Pivot Medical, Ossur. Research support—Stryker, Pivot Medical, AlloSource.
Supplementary Data
Intraoperative arthroscopic video demonstrating arthroscopic microfracture technique using flexible drill and angled guides. First, the curettes and shaver are used to debride the defect. The calcified cartilage layer is removed and vertical cartilage shoulders are created by use of curettes. Microfracture holes are created using angled guides through which the flexible drill is threaded to penetrate the subchondral plate at an orthogonal angle. Once the network of microfracture holes is created, the joint is drained and closed in standard fashion.
References
- 1.Parvizi J., Leunig M., Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15:561–570. doi: 10.5435/00124635-200709000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Crawford K., Philippon M., Sekiya J., Rodkey W., Steadman J.R. Microfracture of the hip in athletes. Clin Sports Med. 2006;25:327–335. doi: 10.1016/j.csm.2005.12.004. x. [DOI] [PubMed] [Google Scholar]
- 3.Byrd J.W., Jones K.S. Osteoarthritis caused by an inverted acetabular labrum: Radiographic diagnosis and arthroscopic treatment. Arthroscopy. 2002;18:741–747. doi: 10.1053/jars.2002.32837. [DOI] [PubMed] [Google Scholar]
- 4.Haviv B., Singh P.J., Takla A., O'Donnell J. Arthroscopic femoral osteochondroplasty for cam lesions with isolated acetabular chondral damage. J Bone Joint Surg Br. 2010;92:629–633. doi: 10.1302/0301-620X.92B5.23667. [DOI] [PubMed] [Google Scholar]
- 5.Philippon M.J., Schenker M.L., Briggs K.K., Maxwell R.B. Can microfracture produce repair tissue in acetabular chondral defects? Arthroscopy. 2008;24:46–50. doi: 10.1016/j.arthro.2007.07.027. [DOI] [PubMed] [Google Scholar]
- 6.Karthikeyan S., Roberts S., Griffin D. Microfracture for acetabular chondral defects in patients with femoroacetabular impingement: Results at second-look arthroscopic surgery. Am J Sports Med. 2012;40:2725–2730. doi: 10.1177/0363546512465400. [DOI] [PubMed] [Google Scholar]
- 7.Willams R.J., III, Harnly H.W. Microfracture: Indications, technique, and results. Instr Course Lect. 2007;56:419–428. [PubMed] [Google Scholar]
- 8.Xing L., Jiang Y., Gui J. Microfracture combined with osteochondral paste implantation was more effective than microfracture alone for full-thickness cartilage repair. Knee Surg Sports Traumatol Arthrosc. 2013;21:1770–1776. doi: 10.1007/s00167-012-2031-5. [DOI] [PubMed] [Google Scholar]
- 9.Shetty V.D., Villar R.N. Hip arthroscopy: Current concepts and review of literature. Br J Sports Med. 2007;41:64–68. doi: 10.1136/bjsm.2006.027755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen H., Sun J., Hoemann C.D. Drilling and microfracture lead to different bone structure and necrosis during bone-marrow stimulation for cartilage repair. J Orthop Res. 2009;27:1432–1438. doi: 10.1002/jor.20905. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intraoperative arthroscopic video demonstrating arthroscopic microfracture technique using flexible drill and angled guides. First, the curettes and shaver are used to debride the defect. The calcified cartilage layer is removed and vertical cartilage shoulders are created by use of curettes. Microfracture holes are created using angled guides through which the flexible drill is threaded to penetrate the subchondral plate at an orthogonal angle. Once the network of microfracture holes is created, the joint is drained and closed in standard fashion.


