Abstract
An internal brace is a ligament repair bridging concept using braided ultrahigh–molecular-weight polyethylene/polyester suture tape and knotless bone anchors to reinforce ligament strength as a secondary stabilizer after repair and return to sports, which may help resist injury recurrence. An internal brace may provide augmentation during knee medial and posteromedial corner anatomic repair. In patients with combined, chronic, symptomatic anterior cruciate ligament (ACL)–posteromedial corner laxity, combined ACL reconstruction with posteromedial corner reconstruction is indicated. Our ACL technique was previously published with video illustration in Arthroscopy and Arthroscopy Techniques. The purpose of this article is to describe, with video illustration, knee posteromedial corner reconstruction using anatomic repair with internal brace augmentation.
Symptomatic, combined knee ligament injuries require surgical stabilization.1,2 The relevant anatomic structures that contribute to posteromedial knee stability include the superficial and deep medial collateral ligaments (MCLs), the posterior oblique ligament (POL), and the semimembranosus. In cases of symptomatic laxity of the medial side of the knee, posteromedial corner anatomic reconstruction of the superficial MCL with or without reconstruction of the POL using soft-tissue grafts, bone sockets, and interference screw fixation has shown good biomechanical results.3,4 However, autografts have morbidity, allografts have risks,2 and bone tunnels with interference screws sacrifice bone stock, which may be of particular concern for multiligament reconstructive cases.
Alternatively, classic technique for treating the medial side of the knee laxity is posteromedial corner repair.5,6 In 2014, we propose that such a repair may be beneficially augmented with an internal brace. An internal brace is a tissue repair bridging concept using braided ultrahigh–molecular-weight polyethylene/polyester suture tape and knotless bone anchors to reinforce tissue strength.
An internal brace may provide augmentation during knee medial and posteromedial corner anatomic repair. Therefore we describe posteromedial corner repair in concert with augmentation ties. Video 1 demonstrates our technique for knee posteromedial corner repair with augmentation, described in this report, in a patient with chronic, severe knee posteromedial corner laxity combined with anterior cruciate ligament (ACL) insufficiency and anteromedial rotary instability. Our ACL technique has been previously published with video illustration.7,8 In this technical note, Video 1 focuses on the posteromedial reconstruction.
Surgical Technique
In this article, we illustrate knee posteromedial femoral-sided repair plus internal brace construction because femoral pathology is most common (Figs 1-3). (For tibial laxity, we recommend tibial-sided coronary [meniscotibial] ligament repair in combination with internal brace augmentation. The tibial technique is similar to the femoral technique described herein, except that placement of the primary anchor and the repair are performed at the tibial anatomic insertions and the internal brace is tensioned to a second anchor at the femoral anatomic insertion of the MCL.)
Fig 1.
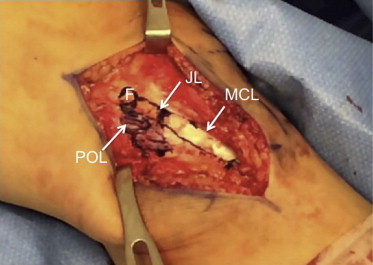
The skin incision forms a straight line when the knee is straight and extends from anterior to the medial epicondyle to 6 cm distal to the joint line (medial view of left knee, where patella is superior and hip is to left). The femoral origin of the MCL (F), superficial MCL, POL, and joint line (JL) are noted.
Fig 2.

A 4.75 mm SwiveLock anchor has been inserted at the femoral origin of the MCL (medial view of left knee, where patella is superior and hip is to left). The anchor is loaded with No. 0 FiberWire (upper and lower suture limbs) for MCL advancement and FiberTape (middle wider suture limbs) for internal brace construction. The POL is reflected for later advancement.
Fig 3.
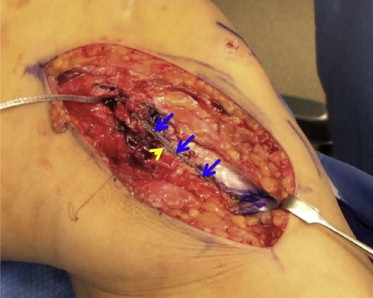
Internal brace (blue arrows) augments superficial MCL reconstruction (medial view of left knee, where patella is superior and hip is to left). The internal brace is sewn to the proximal tibial periosteum to augment the deep MCL (yellow arrow).
For knee posteromedial femoral-sided repair plus internal brace reconstruction, the skin incision should be straight when the knee is straight and should extend from anterior to the medial femoral epicondyle to a point 6 cm distal to the joint line, which represents the tibial attachment of the superficial MCL. When the knee is flexed, the incision will curve like a hockey stick, and because the skin flap is posterior, care is taken to avoid too posterior of an incision.
Deep surgical dissection is then required to identify the MCL and the POL throughout their full extent. Digital palpation can be helpful in identifying the femoral origin of the MCL because it lies just proximal and posterior to the medial femoral epicondyle. The POL courses from proximal and posterior to the MCL insertion in a posteroinferior direction. Relevant tibial anatomic landmarks include the tibial insertion of the semimembranosus, the pes anserinus, and the distal insertion of the superficial MCL, 6 cm distal to the joint line, just under the sartorius fascia of the pes.
Radiographic landmarks for the femoral MCL are of great value,9 but careful dissection also clearly delineates the MCL femoral insertion without fluoroscopy, even after femoral-sided injury. If there is doubt as to anatomy or isometry, a suture can be wrapped around guide pins and serve as an isometer during knee range of motion to ensure correct anatomic position.
After careful exposure of the femoral origin, MCL repair is performed5,6 with suture anchors (SwiveLock 4.75-mm-diameter PEEK [polyether ether ketone] anchors; Arthrex, Naples, FL) loaded with high-strength suture (FiberWire; Arthrex). In larger patients, 2 anchors are used, 1 for the MCL and 1 for the POL. The MCL and POL are advanced proximally to achieve maximal tissue tension and are repaired anatomically, after decortication of the medial femur. To complete the posteromedial repair and to achieve POL plication, it is vital to sew the anterior border of the POL to the posterior border of the MCL, advancing the POL from distal to proximal and from posterior to anterior.
The femoral anchor is placed in cancellous bone, so we simply punch, then tap, and then screw in the anchor. The tibial anchor is placed in cortical bone, so insertion requires placement of a 4.5-mm unicortical drill hole, then tapping to 4.75 mm, and then screwing in the 4.75 mm PEEK SwiveLock anchor. Tensioning of the MCL (and tensioning of the MCL internal brace) is performed at 30° of knee flexion with the knee held in varus to prevent gapping of the joint medially. Tensioning of the POL is performed with the knee in full extension with the knee held in varus.
To construct the internal brace, a high-strength suture structural tie (FiberTape; Arthrex) is loaded on the femoral anchor before anchor insertion, before completion of the femoral-sided repair. After the femoral-sided repair is complete, internal brace augmentation is performed by tensioning the FiberTape while inserting the tibial suture anchor at the MCL tibial footprint. The exact insertion point should be within the posterior fibers of the tibial superficial MCL, 6 cm distal to the joint line. Finally, to reconstruct the deep MCL, high-strength suture (FiberWire) is used to attach the MCL internal brace to the periosteum at the deep tibial MCL insertion, just distal to the joint line. Care is taken to minimize damage to the FiberTape internal brace during deep MCL suturing. (In larger patients, independent repair and internal brace reconstruction may be performed separately for the POL, using a second pair of anchors at the anatomic attachment points on the femur and tibia. An option in smaller patients is to use the second limb of femoral FiberTape to augment the POL.3)
In cases of severe, chronic, combined ACL-MCL laxity with associated anteromedial rotary instability, the dynamic stabilizer of the posteromedial corner–the semimembranosus musculotendinous unit–may also become lax. This is important because the semimembranosus, a knee flexor, is a dynamic, secondary stabilizer against knee anterior laxity (and anteromedial rotary instability), which is protective of the reconstructed ACL graft. The tendon may be identified at the posterior aspect of the tibia just distal to the joint line. The semimembranosus tendon may be advanced using a high-strength modified Bunnell suture (No. 0 FiberWire) to the tibial periosteal insertion of the tendon.
Discussion
The bridging concept using braided ultrahigh–molecular-weight polyethylene/polyester tape and knotless bone anchors has been shown to result in positive results with a low rate of complications for tendon repair in the shoulder rotator cuff10-13 and ankle Achilles tendon.14-16 These results may justify broadening of clinical indications to internal bracing of a ligament repair or reconstruction, with a goal of protecting a repaired ligament from noncompliant patient activity, secondary injury, or construct elongation and failure during early rehabilitation17,18 or as a secondary stabilizer after return to sport, particularly when patient compliance with external orthotics may be poor.19,20 However, future research is required to determine the results of ligament internal brace augmentation of a ligament repair or ligament autograft or allograft tissue reconstruction.
Footnotes
The authors report the following potential conflict of interest or source of funding: J.H.L. receives support from Arthrex, AANA, Breg, Donjoy, Smith & Nephew, Stryker, Taos MRI, Tornier, U&I, Ivivi, Taos Orthopaedic Institute, Taos Center for Sportsmedicine and Rehabilitation. Law firms not related to orthopaedic industry (i.e., medical malpractice defense, ski industry defense). Patents pending with Arthrex, not related to manuscript. G.M. receives support from Arthrex, only as part of consultant agreement for 1 day's research. Travel paid for 1 day's research/teaching as part of consultant agreement with Arthrex. InternalBrace. Royalties related to internal brace technology. B.G. receives support from Arthrex, Breg, Donjoy, Smith & Nephew, Stryker, Taos Center for Rehabilitation, Taos MRI, Tornier, U&I.
Supplementary Data
Surgical technique for posteromedial corner repair with internal brace augmentation includes repair of superficial MCL, repair and advancement of POL, advancement of semimembranosus, augmentation of deep MCL, and internal brace construction (medial view of left knee, where patella is superior and hip is to left). Our ACL technique has been previously published with video illustration7,8; hence only the posteromedial reconstruction is shown here.
References
- 1.Stannard J.P. Medial and posteromedial instability of the knee: Evaluation, treatment, and results. Sports Med Arthrosc. 2010;18:263–268. doi: 10.1097/JSA.0b013e3181eaf713. [DOI] [PubMed] [Google Scholar]
- 2.Levy B.A., Dajani K.A., Whelan D.B. Decision making in the multiligament-injured knee: An evidence-based systematic review. Arthroscopy. 2009;25:430–438. doi: 10.1016/j.arthro.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Coobs B.R., Wijdicks C.A., Armitage B.M. An in vitro analysis of an anatomical medial knee reconstruction. Am J Sports Med. 2010;38:339–347. doi: 10.1177/0363546509347996. [DOI] [PubMed] [Google Scholar]
- 4.Wijdicks C.A., Ewart D.T., Nuckley D.J., Johansen S., Engebretsen L., Laprade R.F. Structural properties of the primary medial knee ligaments. Am J Sports Med. 2010;38:1638–1646. doi: 10.1177/0363546510363465. [DOI] [PubMed] [Google Scholar]
- 5.Hughston J.C., Eilers A.F. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am. 1973;55:923–940. [PubMed] [Google Scholar]
- 6.Hughston J.C. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am. 1994;76:1328–1344. doi: 10.2106/00004623-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Lubowitz J., Ahmad C., Anderson K. All-inside anterior cruciate ligament graft-link technique: Second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;26:717–727. doi: 10.1016/j.arthro.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 8.Lubowitz J. All-inside anterior cruciate ligament graft link: Graft preparation technique. Arthrosc Tech. 2012;1:e165–e168. doi: 10.1016/j.eats.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wijdicks C.A., Griffith C.J., LaPrade R.F. Radiographic identification of the primary medial knee structures. J Bone Joint Surg Am. 2009;91:521–529. doi: 10.2106/JBJS.H.00909. [DOI] [PubMed] [Google Scholar]
- 10.Van der Meijden O., Wijdicks C., Gaskill T., Jansson K., Millett P. Biomechanical analysis of two tendon posterosuperior rotator cuff tear repairs: Extended linked repairs and augmented repairs. Arthroscopy. 2013;29:37–45. doi: 10.1016/j.arthro.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Mazzocca A.D., Millett P.J., Guanche C.A., Santangelo S.A., Arciero R.A. Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med. 2005;33:1861–1868. doi: 10.1177/0363546505279575. [DOI] [PubMed] [Google Scholar]
- 12.Vaishnav S., Millett P.J. Arthroscopic rotator cuff repair: Scientific rationale, surgical technique, and early clinical and functional results of a knotless self-reinforcing double-row rotator cuff repair system. J Shoulder Elbow Surg. 2010;19:83–90. doi: 10.1016/j.jse.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 13.Denard P.J., Jiwani A.Z., Lädermann A., Burkhart S.S. Long-term outcome of arthroscopic massive rotator cuff repair: The importance of double-row fixation. Arthroscopy. 2012;28:909–915. doi: 10.1016/j.arthro.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Greenhagen R.M., Shinabarger A.B., Pearson K.T., Burns P.R. Intermediate and long-term outcomes of the suture bridge technique for the management of insertional Achilles tendinopathy. Foot Ankle Spec. 2013;6:185–190. doi: 10.1177/1938640012473150. [DOI] [PubMed] [Google Scholar]
- 15.Fanter N.J., Davis E.W., Baker C.L., Jr. Fixation of the Achilles tendon insertion using suture button technology. Am J Sports Med. 2012;40:2085–2091. doi: 10.1177/0363546512453294. [DOI] [PubMed] [Google Scholar]
- 16.Witt B.L., Hyer C.F. Achilles tendon reattachment after surgical treatment of insertional tendinosis using the suture bridge technique: A case series. J Foot Ankle Surg. 2012;51:487–493. doi: 10.1053/j.jfas.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Acevedo J., Vora A. Anatomical reconstruction of the spring ligament complex: “Internal brace” augmentation. Foot Ankle Spec. 2013;6:441–445. doi: 10.1177/1938640013499404. [DOI] [PubMed] [Google Scholar]
- 18.Viens N.A., Wijdicks C.A., Campbell K.J., Laprade R.F., Clanton T.O. Anterior talofibular ligament ruptures, part 1: Biomechanical comparison of augmented Broström repair techniques with the intact anterior talofibular ligament. Am J Sports Med. 2014;42:405–411. doi: 10.1177/0363546513510141. [DOI] [PubMed] [Google Scholar]
- 19.Squyer E., Stamper D.L., Hamilton D.T., Sabin J.A., Leopold S.S. Unloader knee braces for osteoarthritis: Do patients actually wear them? Clin Orthop Relat Res. 2013;471:1982–1991. doi: 10.1007/s11999-013-2814-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ramírez N., Flynn J.M., Fernández S., Seda W., Macchiavelli R.E. Orthosis noncompliance after the Ponseti method for the treatment of idiopathic clubfeet: A relevant problem that needs reevaluation. J Pediatr Orthop. 2011;31:710–715. doi: 10.1097/BPO.0b013e318221eaa1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for posteromedial corner repair with internal brace augmentation includes repair of superficial MCL, repair and advancement of POL, advancement of semimembranosus, augmentation of deep MCL, and internal brace construction (medial view of left knee, where patella is superior and hip is to left). Our ACL technique has been previously published with video illustration7,8; hence only the posteromedial reconstruction is shown here.


