Abstract
Background
Parental concerns about their children’s development can be used as an indicator of developmental risk. We undertook a systematic review of the prevalence of parents’ concerns as an indicator of developmental risk, measured by the Parents’ Evaluation of Developmental Status (PEDS) and associated risk factors.
Methods
Electronic databases, bibliographies and websites were searched and experts contacted. Studies were screened for eligibility and study characteristics were extracted independently by two authors. A summary estimate for prevalence was derived. Meta-regression examined the impact of study characteristics and quality. Meta-analysis was used to derive pooled estimates of the impact of biological and psychosocial risk factors on the odds of parental concerns indicating high developmental risk.
Results
Thirty seven studies were identified with a total of 210,242 subjects. Overall 13.8% (95% CI 10.9 -16.8%) of parents had concerns indicating their child was at high developmental risk and 19.8% (95% CI 16.7-22.9%) had concerns indicating their child was at moderate developmental risk. Male gender, low birth weight, poor/fair child health rating, poor maternal mental health, lower socioeconomic status (SES), minority ethnicity, not being read to, a lack of access to health care and not having health insurance were significantly associated with parental concerns indicating a high developmental risk.
Conclusions
The prevalence of parental concerns measured with the PEDS indicating developmental risk is substantial. There is increased prevalence associated with biological and psychosocial adversity.
Trial registration
PROSPERO Registration: CRD42012003215.
Electronic supplementary material
The online version of this article (doi:10.1186/1471-2431-14-231) contains supplementary material, which is available to authorized users.
Keywords: Prevalence, Parental concerns, Parents Evaluation of Developmental Status (PEDS), Risk factors, Developmental risk, Child health
Background
Children at developmental risk, are those who have significant problems in at least one area of their development (e.g., motor, language, self-help, social, cognitive, behavioural) [1]. They include children who may be at risk of having a developmental disorder, or children who are functioning on the lower end of normal who may go on to struggle with the literacy, numeracy and socio-emotional demands of school and life [1]. Adverse childhood experiences including socioeconomic disadvantage, poor parental mental health, lack of stimulating early childhood experiences, and lack of access to services can contribute to developmental risk [2–6].
In order to develop a comprehensive public health response to optimise early childhood development, it is helpful if we are able to quantify the state of child development from a population perspective. Although not a comprehensive developmental assessment, measuring parental concerns about their children’s development can be done in a quick, standardised, systematic manner and has been used to estimate level of developmental risk in the general population and to identify high risk subpopulations [7, 8]. In addition, eliciting and addressing parental concern is a key component in the family centred practice of detecting individual children at developmental risk in well child health care so that they may have timely referral on for assessment and early intervention prior to starting school [9–12]. The Parents’ Evaluation of Developmental Status (PEDS) is a 10 − item parent completed standardised questionnaire, which has been used to elicit parental concerns around child development for children aged less than 8 years in populations, communities and clinical samples. The PEDS open ended questions cover expressive and receptive language, fine motor, gross motor, behaviour, socialisation, self care, and learning [13]. An estimate of developmental risk as high, moderate, low or no risk is derived from the parental concerns recorded and a clinical pathway is recommended. The PEDS has a sensitivity of 91-97% and specificity of 73-86% in recent validation studies from the USA for the accuracy of parental concerns in detecting children at high and/or moderate developmental risk [14]. The PEDS has been found to be useful in vulnerable disadvantaged populations, high, middle and low income countries, and has been translated in multiple languages [14, 15]. There is also a modified version of the PEDS, the Survey PEDS which has 12 close-ended questions that does not allow for further discussion of parental concerns and clinical decision making around these. It is less well validated than the clinical form of the PEDS but is used in telephone population surveys [7, 14, 16–18].
In order to better understand the current worldwide prevalence of parental concern measured by the PEDS that indicate developmental risk and associated risk factors, we undertook a systematic review to synthesize the available international evidence.
Methods
Search strategy
A protocol was developed and registered with the University of York Centre for Reviews and Dissemination (PROSPERO) on 6/11/2012 and updated on the 13/02/2014, registration number CRD42012003215(http://www.crd.york.ac.uk/PROSPERO/index.asp).
A systematic search of the literature was undertaken using the following inclusion criteria: primary observational studies (cohort study, cross-sectional studies) in geographically defined population or a community sample (including samples from primary health care services) of children aged under 8 years using the PEDS [15] with available prevalence data (Additional file 1). Studies using the modified “Survey PEDS” were also included in this review [14]. Electronic databases searched were Web of Science and Google Scholar, PubMed (Nov 2012), EMBASE (Nov 2012), Medline (Nov 2012), Psychinfo (Nov 2012), Global Health (Nov2012) CINAHL (Nov 2012), the Cochrane Library (Nov 2012), LILACS (Nov 2012), ERIC (Nov 2012), and Proquest (Nov 2012). Secondary searches of citations in review articles, requests to experts in the field and additional searches of the USA based PEDStest and RCH PEDS website for key studies were undertaken. Advice from the Cochrane Child Development, Psychosocial and Learning Groups was sought regarding search terms which were specific for early child development, developmental risk and the PEDS. There were no language limitations. Studies using specific clinical samples, for example, neonatal intensive care graduates or with participants who had a known developmental disorder were excluded.
The study titles, abstracts and full papers of “potentially relevant articles” were reviewed independently by two authors (SW&VE). Disagreements about inclusion were resolved through consensus and discussion with a third author (KW). Study characteristics, prevalence, and risk factors, were extracted independently by SW and VE on a data extraction form that was piloted and modified prior to use. Where insufficient data were reported, study authors were contacted. If no reply was forthcoming or full data not made available, data were included in analysis where possible. Methodological quality was assessed independently by SW and VE based on a validity of the study methods (design, sampling frame, sample size, outcome measures, measurement and response rate), interpretation of the results and applicability of the findings [19], a score of 6 or greater was rated by the reviewers as high quality.
Statistical analysis
Prevalence
Estimates of the prevalence of parental concerns on the PEDS indicating moderate or high risk with corresponding 95% confidence intervals were extracted from each study. If the confidence intervals were not provided, these were calculated using the Agresti and Coull method [20]. For longitudinal studies, cross-sectional estimates of prevalence were used to extract prevalence data at the first time point. We used an exact likelihood approach to obtain pooled estimates of prevalence. We used metaregression, a regression method that allows the examination of study-level factors on prevalence with the following pre-specified variables on prevalence: sample type; type of PEDS; study purpose; study quality; study age group, publication type and country income [21].
Risk factor analysis
We conducted a meta-analysis for risk factors for having parental concerns on the PEDS indicating high versus low/no developmental risk. We extracted odds ratios and 95% confidence intervals from each study. If odds ratio (OR) with a 95% confidence interval was not provided, we calculated the odds ratio and 95% confidence interval. We extracted adjusted odds ratios when possible, but we were unable to calculate these for studies in which they were not provided. We obtained pooled estimates of unadjusted odds ratios (uOR) using meta-analysis with random effects. Where studies presented adjusted odds ratios (aOR) for similar child and family variables these were combined in a separate meta-analysis.
Investigation of heterogeneity
For all meta‒analyses and meta‒regressions of prevalence, we modelled within-study variability using the binomial distribution [21]. We then examined heterogeneity through meta-regression models, as described in previous systematic reviews of prevalence [22]. We quantified the reduction in the between study variance from the inclusion of the study characteristics compared to the ‘base’ model (i.e., the model of prevalence without any covariates). This provides an estimate of the proportion of heterogeneity that is explained by that characteristic. For our meta-analysis of risk factors, the degree of heterogeneity was investigated by estimating the I2 statistic (which describes variation in the summary effect due to genuine variation rather than a sampling error as a percentage, a low I2 indicates low heterogeneity and high I2 indicates significant between study variability) and visual inspection of forest plots [22].
Results
Studies identified
The search strategy identified 17,272 titles (excluding duplicates). Seventy-eight articles underwent a text screen and 41 of these were excluded (Figure 1) [23].
Figure 1.
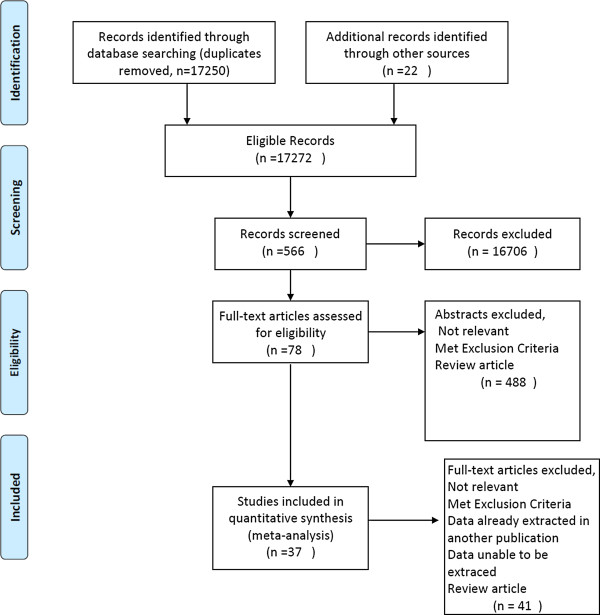
Search flow chart.
Included studies
The prevalence estimates of the 37 included studies are listed in Table 1 [7, 13–18, 24–56]. Twenty three studies were published in peer review journals, and the remainder were government/university reports, unpublished abstracts available on the PEDStest website, online population survey data and data from the PEDS Standardisation Manual (2013). There was one longitudinal cohort with data available on samples at two time points three years apart [39, 40, 57]. All other studies were cross sectional.
Table 1.
Included studies characteristics and prevalence rates*
| First author | Country | Age (months) | Sample size | Quality score/8 | High risk% (95% CI) | Moderate risk% (95% CI) | High and moderate risk% (95% CI) | Low/no risk% (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Armstrong [15] | Australia | 0-95 | 246 | 3 | 11.4 (8.0-16.0) | 21.9 (17.2-27.6) | 33.3 (27.7-39.5) | 66.7 (60.5-72.3) |
| Bethell [29] | USA | 10-71 | 22883 | 8 | 9.6(9.2-10.0) | 15.9 (15.5-16.4) | 25.5 (25.0-26.1) | 74.5 (73.9-75.0) |
| CHIS [50] | USA | 4-60 | 2884 | 7 | 25.6 (23.6-27.5) | 17.4 (15.6-19.2 | 43.0 (41.2-44.8) | 57.0 (55.2-58.8) |
| CHIS [49] | USA | 4-60 | 3029 | 7 | 19.9 (18.3-21.5) | 18.0 (16.4-19.6) | 37.9 (36.2-39.2) | 62.2 (60.4-63.9) |
| CHIS [48] | USA | 4-60 | 3058 | 7 | 26.3 (24.5-28.2) | 18.3(16.7-19.9) | 44.7 (72.9-46.4) | 55.3 (53.6-57.1) |
| CHIS [47] | USA | 4 to 60 | 3096 | 7 | 20.1 (17.6-22.5) | 19.7 (17.4-22.0) | 39.8 (38.1-41.5) | 60.2 (58.5-61.9) |
| Chuan [24] | Malaysia | 12-72 | 86 | 2 | 26 (17.5-35.8) | NA | NA | 17.0 (10.8-27.0) |
| Coghlan [28] | Australia | 18-69 | 262 | 3 | 9.2 (6.2-13.3) | 18.7 (14.4-23.9) | 27.9 (22.8-33.6) | 72.1 (66.4-77.2) |
| Davies [25] | UK | 0-24 | 76 | 5 | 2.6 (0.2-9.8) | 13.2 (7.2-22.8) | 15.8 (9.2-25.8) | 84.2 (74.2-90.8) |
| Glascoe [32] | USA | 24-84 | 408 | 5 | NA | NA | 34.6 (30.1-39.3) | 65.4 (60.7-69.9) |
| Glascoe [58] | USA | 3-93 (mean 46.5 SD 21.8) | 771 | 5 | 11.0 (9–13.4) | 26.0 (23.0-29.2) | 37.0 (33.6-40.4) | 63.0 (59.6-66.4) |
| Glascoe [33] | USA | mean 36 | 257 | 4 | 41.0 (35.0-47.0) | 40.0 (34.3-46.2) | 81.0 (75.6-85.3) | 19.0 (14.7-24.4) |
| Glascoe [33] | USA | mean 36 | 744 | 4 | 23.0 (20.1-26.2) | 26.0 (22.9-29.2) | 49.0 (45.4-52.5) | 51.0 (47.5-54.7) |
| Glascoe [14] | USA | 0.3-95 (mean 26 SD 20.6) | 47531 | 6 | 4.5 (4.3-4.7) | 13.7 (13.4-14.0) | 18.2 (17.9-18.6) | 81.8 (81.5-82.1) |
| Gustawan [59] | Indonesia | 3-12 | 170 | 3 | NA | NA | 31.0 (24.2-37.9) | 69.0 (62.1-75.8) |
| Ibironke [56] | USA | 6-71 (mean 38.5 SD 18.4) | 2381 | 7 | NA | NA | 21.4 (19.8-23.1) | 78.6 (76.9-80.2) |
| Kiing [41] | Singapore | 1-83 | 1806 | 3 | 7.5 (6.4-8.8) | 26.0 (24.1-28.1) | 33.5 (31.4-35.7) | 66.0 (64.3-68.6) |
| Kosht-Fedyshin [42] | Tanzania | 0-60 | 20 | 4 | 35.0 (18.1-56.9) | 0.0 | 35.0 (18.1-56.9) | 65.0 (43.1-81.9) |
| Limbos [43] | Canada | 12-60 | 331 | 5 | 13.9 (10.6-18.1) | 39.6 (34.5-45.0) | 53.5 (48.1-58.8) | 46.5 (41.2-51.9) |
| Malhi [44] | India | 24-60 | 79 | 2 | NA | NA | 39.2 (29.2-50.3) | 60.8 (49.7-70.8) |
| Matibag [45] | Philippines | 24-60 (mean 53.6) | 283 | 2 | 15.0 (11.2-19.5) | NA | NA | NA |
| McGookin [35] | USA | 9-24 | 385 | 3 | 5.2(3.4-8.0) | 17.4 (13.9-21.5) | 22.6 (18.7-27.1) | 77.4 (73.0-81.3) |
| Ng [18] | Canada | 0-83 (mean 46.1) | 419 | 6 | 9.3 (6.9-12.5) | 18.9 (15.4-22.9) | 28.2 (24.1-32.7) | 72.0 (67.3-75.9) |
| NSCH (2011/2012) [16] | USA | 4-60 | 28540 | 8 | 77.0 (10.1-11.9) | 15.2 (14.3-16.1) | 26.2(25.7-26.7) | 73.8 (72.7-75.0) |
| Oreto [46] | Philippines | 0-84 (means 53) | 318 | 4 | 15.1 (11.6-19.5) | 17.0 (13.3-21.5) | 32.1 (27.2-37.4) | 67.9 (62.6-72.8) |
| Palarca [51] | Philippines | 0.5-96 (means 52.6) | 421 | 3 | 9.0 (6.6-12.2) | 5.0 (3.3-7.6) | 14.0 (11.0-17.7) | 86.0 (82.3-89.0) |
| Restall (2009) [52] | Canada | 60 | 290 | 6 | 13.1 (9.7-17.5) | 32.4 (27.3-38.0) | 45.5 (39.9-51.3) | 54.5 (48.7-60.1) |
| Rose-Jacobs [37] | USA | 4-36 | 2010 | 5 | 13.8 (12.4-15.4) | NA | NA | NA |
| Roux [26] | USA | <60 | 2845 | 3 | 28.2 (26.6-29.9) | 27.5 (25.9-29.2) | 55.7 (53.9-57.5) | 44.3 (42.5-46.1) |
| Sarmiento Campos [31] | Spain | 6-42 | 1089 | 3 | 8.5 (7.0-10.4) | 23.0 (20.7-25.7) | 31.6 (28.9-34.4) | 68.4 (65.6-71.1) |
| Sices [38] | USA | 9-31 (means 17.6 SD 6.1) | 60 | 2 | 26.7 (17.1-39.1) | 10.0 (4.4-20.6) | 36.7 (25.6-49.4) | 63.3(50.6-74.4) |
| Stevens [7] | USA | 4.35 | 2068 | 6 | 23.4 (21.6-25.3) | 24.9 (23.1-26.8) | 48.3 (46.2-50.5) | 51.7 (49.5-53.9) |
| Theeranate [53] | Thailand | 0-72 | 216 | 3 | NA | NA | 4.2 (2.1-7.9) | 95.8 (92.1-97.9) |
| Tough [40] | Canada | Mean 38 (SD 8) | 792 | 4 | 10.8 (8.9-13.2) | 30.2 (27.1-33.5) | 41.0 (37.7-44.5) | 59.0 (55.5-62.3) |
| VSEHQ (2008) [54] | Australia | 60-83 | 54602 | 6 | 7.2 (7.0-7.4) | 16.5 (16.2-16.8) | 23.7 (23.3-24.0) | 76.3 (76.0-76.7) |
| Wake [55] | Australia | 63.4-90 | 853 | 3 | NA | NA | 35.0 (31.9-38.3) | 65.0 (61.7-68.1) |
| Zuckerman [34] | USA | <72 | 24933 | 7 | NA | NA | 22.4 (21.9-23.0) | 77.6 (77.05-78.1) |
*quality rating system as per quality rating tool developed by Public Health Agency in Canada [19].
Fifteen studies used the PEDS as a research tool to measure prevalence of developmental risk of which 12 were population surveys in high income countries and three were community samples. The remaining studies used the PEDS as a developmental surveillance tool in primary health care and early childhood education/early primary school settings [14, 24–28, 31–33, 35, 38, 41–46, 51, 53, 58, 59]. Eight of the studies were conducted in low and middle income countries [24, 42, 44–46, 51, 53, 59] and two studies were in socioeconomically disadvantaged communities in the USA [33].
Study sample sizes ranged from 20 to 54602 (median = 467). There were 210,242 subjects in total. Ages ranged from less than 1 month to 7 years and 11 months consistent with the age range for administration of the PEDS. Twenty seven of the studies used translated versions of the PEDS for at least part of their sample.
Study quality
Quality scores varied between studies (Table 2). Only 13 studies met 6 or more criteria and thus were deemed of high quality [7, 14, 16, 18, 29, 34, 47–50, 52, 54, 56]. Key areas of potential bias were lack of random selection of the sample (22/37), a biased sampling frame (20/37), less than 300 participants (11/37), less than 70% response rate and refusers not described (11/37); confidence intervals not given for prevalence results and lack of subgroup analysis (31/37).
Table 2.
Quality assessment of included studies*
| First author | Year | Random sample or whole population | Unbiased sampling frame (i.e. census data) | Adequate sample size (>300 subjects) | Measures were the standard | Outcomes measured by unbiased assessors | Adequate response rate (70%) and refusers described | Confidence intervals and subgroup analysis | Study subjects descirbed | Quality risk rating/8 |
|---|---|---|---|---|---|---|---|---|---|---|
| Bethell | 2011 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| NSCH | 2011/2012 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| CHIS | 2003 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| CHIS | 2005 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| CHIS | 2009 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| CHIS | 2007 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 7 |
| Ibironke | 2011 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 7 |
| Zuckerman | 2009 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 7 |
| Glascoe | 2013 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 6 |
| Stevens | 2006 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 6 |
| Ng | 2010 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 6 |
| Restall | 2009 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| VSEHQ | 2008 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 6 |
| Davies | 2009 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 5 |
| Glascoe | 1999 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 5 |
| Glascoe | 1997 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 5 |
| Rose Jacobs | 2008 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 5 |
| Glascoe | 2010 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 4 |
| Glascoe | 2010 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 4 |
| Kosht-Fedyshin | 2006 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 4 |
| Limbos | 2011 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 5 |
| Oreto | 2010 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 4 |
| Tough | 2008 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 4 |
| Armstrong | 2008 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 3 | |
| Campos | 2010 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 3 |
| Coghlan | 2003 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 3 |
| Kiing | 2012 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 3 |
| McGookin | 2011 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 3 |
| Palarca | 2008 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 3 |
| Roux | 2011 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 3 |
| Theeranate | 2005 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 3 |
| Wake | 2005 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 3 |
| Gustawan | 2010 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 3 |
| Chuan | 2012 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 2 |
| Mahli | 2002 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 2 |
| Matibag | 2008 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 2 |
| Sices | 2009 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 2 |
*Quality rating system as per quality rating tool developed by Public Health Agency in Canada [19].
Prevalence of developmental risk
The pooled estimate of the prevalence of parental concern on the PEDS indicating high developmental risk was 13.8% (95% CI 10.9-16.8%), meaning that almost 14% of parents raised concerns associated with a high risk for developmental problems (Figure 2). The pooled estimate of for moderate developmental risk was 19.8% (95% CI 16.7-22.9%). The pooled estimate for high or moderate developmental risk was 31.5%(95% CI 27.0-36.0%), meaning that more than 31% raised concerns associated with either high or moderate risk of developmental problems.
Figure 2.
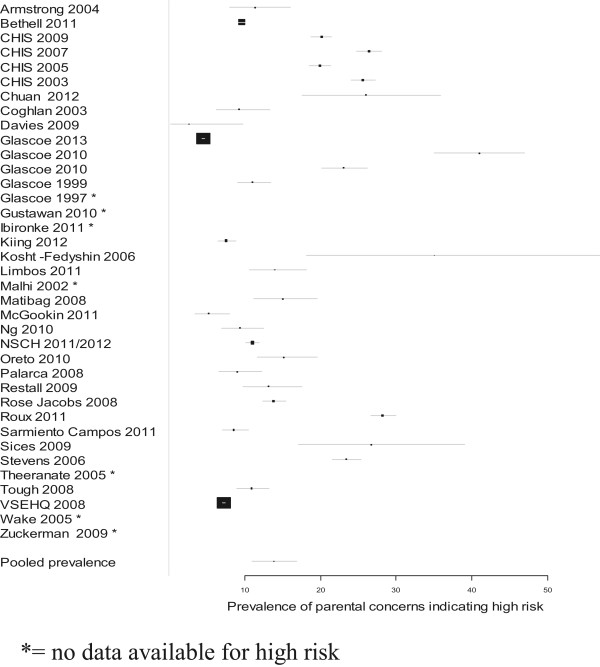
Prevalence of parental concerns indicating high developmental risk.
Meta-regression was conducted for study characteristics (Table 3). Peer reviewed publications had a significantly lower level of parental concerns indicating high developmental risk on the PEDS than unpublished sources (abstracts, reports and population survey data available on the internet). This variable contributed to 19% of the overall variance between studies. For the report of parental concerns on the PEDS indicating moderate developmental risk, studies done in high income countries reported a significantly higher rate than those done in low and middle income countries. This variable contributed to 29% of the overall variance between studies. All other variability in study characteristics did not have an impact.
Table 3.
Metaregression of included studies
| Study characteristics | Prevalence of high risk (%, 95% CI) | P value | Prevalence of moderate risk (%, 95% CI) | P value |
|---|---|---|---|---|
| All studies | 13.8 (10.9,16.8) | 19.9 (16.8,23.1) | ||
| Sample type | ||||
| Population survey | 13.5 (8.8,18.1) | 0.86 | 18.7 (14.3,23.1) | 0.47 |
| Community sample | 14.0 (10.2,17.8) | 21.0 (16.7,25.2) | ||
| Type of PEDS | ||||
| Survey PEDS | 17.9 (10.9,24.9) | 0.15 | 20.6 (16.9,24.3) | 0.50 |
| Clinical PEDS | 12.6(9.6,15.7) | 18.3 (12.9,23.7) | ||
| Study purpose | ||||
| Population risk measure | 14.5 (9.7,19.2) | 0.71 | 20.1 (15.4,24.9) | 0.92 |
| Developmental surveillance tool | 13.3 (9.6,17.1) | 19.8 (15.6,24.0) | ||
| Study quality | ||||
| High quality | 13.5 (8.8,18.1) | 0.86 | 18.7 (14.3,23.1) | 0.47 |
| Medium/low quality | 14.0 (10.2,17.8) | 21.0 (16.7,25.2) | ||
| Study age group | ||||
| 3 years and under | 14.5(8.9,20.2) | 0.76 | 22.9(16.7,29.1) | 0.25 |
| Includes over 3 years | 13.5(10.1,16.9) | 18.9 (15.4,22.3) | ||
| Publication type | ||||
| Peer review/Government report | 11(8.1,14.0) | 0.013 | 21.1(16.9,24.4) | 0.39 |
| Abstracts/website/manuals | 18.0(13.0,22.9) | 18.4(14.1,22.8) | ||
| Country income | High | |||
| High | 13.2(10.2,16.3) | 0.38 | 21.5(18.6,24.5) | 0.001 |
| Middle/low | 17.2(8.2,26.1) | 8.4(3.7,13.1) |
Pooled estimates for biological and psychosocial risk factors
As shown in Table 4, child sociodemographic variables predictive of parental concerns on the PEDS indicating high developmental risk included male gender [14, 16, 17, 27, 28, 30, 37, 40, 47–50, 52, 54], age 3 years and above [14, 27, 28, 47–50], low birth weight [17, 37], poor/fair child health [40, 47–50] or special health care needs [16, 30]. Family sociodemographic variables predictive of parental concerns on the PEDS indicating high developmental risk included poor maternal mental health [7, 37, 40], low family SES [7, 16, 30, 40, 47–50], being of African American [7, 14, 17, 30, 47–50], Hispanic [7, 16, 17, 30, 47–50], First Nations and Australian Aboriginal ethnicity [14, 47–50, 54], being from a Non English speaking household [30, 47–50]. Service level variables predictive of parental concerns on the PEDS indicating high developmental risk included not having a usual source of health care/medical home [16, 30, 37, 40, 47, 49, 50]; or having public/no health insurance [7, 16, 30, 37, 47–50]. Parents not completing high school [16, 27, 28, 30, 40, 50] and single parenthood [16, 40, 47–50, 54] were significant using unadjusted OR, however not significant as adjusted OR [17, 37]. Children not being read to daily was significant in the unadjusted analysis [40, 47–49], however this did not appear to be significant in the one study that included it in a multivariate analysis (p = 0.93) [40]. Family size (more than 6 people in household) was not significant [47–50]. Parents of children who did not attend formal childcare were less likely to have concerns on the PEDS that indicated high developmental risk [40, 47–49], however findings from multivariate analysis of NSCH 2007 data aOR =1.05 (CI 0.84,1.33) found a non -significant effect of childcare and that receiving more than 10 hours a week of care at another family’s home was a risk factor (aOR = 1.71, p < 0.05) [17].
Table 4.
Risk factors associated with parental concerns on PEDS indicating high developmental risk
| Risk factor | N studies | Summary effect OR (95% CI) | P value | Heterogeneity (I 2) |
|---|---|---|---|---|
| Child level | ||||
| Male gender | 11 | 1.68 (1.48,1.87) | <0.001 | 88.1% |
| Male gender (aOR) | 3 | 2.01 (1.38, 2.94) | <0.001 | 91.6% |
| >3 years of age | 7 | 1.83 (1.39,2.41) | <0.001 | 92.7% |
| Low birth weight | 2 | 1.95 (1.53,2.49) | <0.001 | 0.0% |
| Poor/fair child health status | 5 | 3.68 (2.66,5.08) | <0.001 | 68% |
| Special health care needs | 2 | 4.86 (2.81,8.38) | <0.001 | 98% |
| Family level | ||||
| Poor maternal mental health (aOR) | 3 | 1.61(1.31,1.99) | <0.001 | 0.0% |
| Low socioeconomic status | 8 | 2.12(1.65,2.72) | <0.001 | 93.9% |
| Low socioeconomic status (aOR) | 2 | 1.66 (1.08,2.53) | 0.019 | 0.0% |
| Less than high school education | 6 | 1.79 (1.14,2.79) | 0.011 | 95.5% |
| Less than high school education (aOR) | 3 | 1.94 (0.60,6.23) | 0.26 | 98.8% |
| Being read to less than daily | 4 | 1.47(1.28,1.67) | <0.001 | 30.6% |
| Family size (6 or more people in household) | 4 | 1.18(0.83,1.68) | 0.35 | 91.9% |
| Single parent | 7 | 1.46 (1.16,1.84) | 0.001 | 96.8% |
| Single parent (aOR) | 2 | 0.94(0.75, 1.17) | 0.57 | 0.0% |
| Ethnicity (vs White) | ||||
| African American | 7 | 1.95 (1.43,2.66) | <0.001 | 90.5% |
| African American (aOR) | 2 | 1.40 (1.10,1.78) | 0.006 | 0.0% |
| Indigenous | 6 | 1.98 (1.37,2.86) | <0.001 | 63.6% |
| Hispanic | 4 | 2.24(1.83,2.72) | <0.001 | 88.9% |
| Hispanic (aOR) | 2 | 1.54(1.16,2.04) | 0.03 | 0.0% |
| Language spoken | ||||
| English as a second language (all) | 5 | 1.61(1.12,2.33) | 0.01 | 94.2% |
| English as a second language (Spanish) | 5 | 1.48(0.87,2.53) | 0.15 | 96.5% |
| Service Level | ||||
| No Usual Health Care/Medical Home(USA) | 5 | 2.27(1.35,3.81) | 0.002 | 84.3% |
| No or Public Health Insurance | 4 | 1.85(1.45,2.37) | <0.001 | 95.2% |
| No Health Insurance (aOR) | 2 | 2.01(1.01,4.02) | 0.048 | 57.2% |
| Does not attend formal childcare | 4 | 0.88(0.77,0.99) | 0.040 | 0% |
aOR = adjusted OR.
Narrative summary of single studies, cumulative risk and life course analysis
A wide range of additional child, family, and service level factors were noted in single studies [36, 37, 39, 40, 56]. Child level factors were ear infections prior to age 2 (p < 0.001) [40], history of hospital admissions aOR 1.80 (95% CI 1.35–2.40) [37] and being underweight aOR 2.66 (95% CI 1.68–4.24) [37]. Family level factors were low scores on contentment/relaxation during pregnancy aOR 2.5 (95% CI 1.4 -4.2) [39], poor parenting morale when the child was 3 years old aOR 3.9 (95% CI 2.1- 7.3) [39], maternal history of domestic violence at pregnancy aOR 2.2 (95% CI 1.3- 3.7) [39, 40], household food-insecurity (aOR 1.76 (95% CI 1.26 - 2.46) [37], severe energy insecurity aOR 1.82 (95% CI 1.38 -2.39) [36], geographic site differences in the USA (p = 0.003) [37] and poor overall social support (p = 0.003) [39]. Service level factors were referral to early intervention (p < 0.001), speech pathology (p < 0.001) or audiology (p < 0.001) [40], lack of care coordination aOR 0.33 (95% CI 0.24–0.46), referrals aOR 0.40 (95% CI 0.25–0.65), family-centred care aOR 0.47 (95% CI 0.36–0.62) [30] and parental difficulty understanding the doctor uOR 3.35 (95% CI 2.1-5.4) [48].
Two studies reported a dose–response relationship between the number of risk factors and the increased likelihood of parental concerns on the PEDS indicating high developmental risk [7, 39, 40]. In one study having one risk factor was associated with an aOR 1.7 (95% CI: 1.20–2.38); two risk factors aOR 3.28, (95% CI: 2.27–4.73), three risk factors aOR 4.69 (CI: 2.84–7.73), and four risk factors aOR 14.58 (95% CI: 4.98–42.64) compared to a child with zero risk factors [7]. In addition, the greater the number of risk factors experienced by the child the more likely the child was to not receive comprehensive well child care [7].
The only longitudinal cohort in the review reported that at the second follow up when a child was 5 years of age male gender aOR 2.3 (1.3, 4.1), maternal history of abuse at pregnancy aOR 2.4 (1.3, 4.4) and poor parenting morale when the child was 3 years old aOR3.9 (2.1, 7.3) were predictors of parental concerns on the PEDS indicating high developmental risk [39].
Discussion
Prevalence and associated risk factors for parental concerns on the PEDSindicating developmental risk
This systematic review provides synthesised critically appraised evidence of the substantial global prevalence of parental concerns on the PEDS that indicate high and moderate developmental risk, which increases with biological and psychosocial adversity. This information is useful for researchers, service providers and clinicians to quantify the level of parental concern and to estimate the risk of children having developmental problems in the general population and to identify vulnerable subpopulations. Gender, low birth weight, poor maternal mental health, low family SES, minority ethnicity, speaking a language other than English and a lack of stimulation, such as a child not being read to, are all associated with adverse impacts on development in the literature and this was supported by the synthesised evidence [1, 60–63]. The increasing parental concerns with age of a child regardless of SES demonstrated in this review reflect the increasing developmental demands with age. The impact of child’s poor general health on developmental risk may reflect a true increase as some chronic illnesses and syndromes are associated with adverse developmental outcomes. However concerns about their child’s health may increase parental concerns generally [64, 65].
This review demonstrated that lack of access to usual and comprehensive health care in the USA and Canada was associated with an increased prevalence of parental concerns on the PEDS indicating high developmental risk. Interestingly the evidence for access to services such as early childhood education which has been found to particularly benefit children from disadvantaged backgrounds was not demonstrated [66–68].
Two studies demonstrated that parental concerns on the PEDS indicating high developmental risk increased with the number of risk factors a child was exposed to, consistent with our understanding of the burden of multiple risk factors on early childhood development [7, 39, 40, 62]. In addition, the “inverse care law” applied in one USA study, with the greater the number of risk factors, the less access to comprehensive health care [7, 69].
Comparison with other measures of developmental risk
The confidence intervals around the pooled prevalence estimates of high and moderate developmental risk using the PEDS (27.0-36.0%) is similar to rates using the Denver Developmental Screening Test (DDST) [70–72] but higher than those using the Australian Early Development Index (AEDI) [1], and Ages and Stages Questionnaire (ASQ) [38, 43, 52]. While the PEDS gives an estimate of high and moderate developmental risk based on parental concerns this is not synonymous with a comprehensive developmental assessment. The PEDS specificities of 73-86% for parental concerns indicating high and/or moderate developmental risk means that some children identified by parental concern will be false positives [14, 17]. If parental concerns indicating only high developmental risk are examined the specificity of the PEDS improves to 89%, reducing the number of false positives but the sensitivity drops substantially to less than 50% giving an unacceptable level of false negatives [38, 43]. Thus, the true prevalence of actual developmental problems indicated by parental concerns is likely to lie somewhere between the values indicating high and moderate developmental risk [38, 73]. This is reflected in how the PEDS is used in clinical practice with those children identified as at high developmental risk on parental concerns referred on for a comprehensive developmental assessments and those at moderate risk undergoing a secondary developmental screen with a tool such as the ASQ and if they fail that then being referred on for a comprehensive developmental assessment [38, 43, 52]. Systematic reviews of the diagnostic test accuracy (DTA) of the tools that measure developmental risk such as the PEDS in relation to the reference-standard diagnostic batteries in nationally representative samples with an inclusive analysis of vulnerable subpopulations would be useful in understanding how useful developmental risk is as a way to estimate the burden of developmental problems in a population. This systematic review only included studies which had used the PEDS. Prevalence and DTA systematic reviews of other tools such as the ASQ and AEDI would also be useful for further comparison.
Limitations
There was considerable variation in quality of the individual studies included in this systematic review. The major sources of bias were an inadequate sampling method, sampling frame, sample size and response rate and a lack of information to aid interpretation and applicability of the results including reporting of confidence intervals and subgroups. It is suggested that future research focus on designing studies that address these issues. Where community samples were used, parents most concerned about their children may be over-represented and this could lead to an overestimation of prevalence. However meta-regression using quality of the study as a variable did not find significant differences in pooled prevalence estimates. There were significant differences in pooled prevalence estimates of developmental risk between studies when the subgroups of publication type and country income were examined. We did not have individual patient data to undertake our own multivariate analysis. Although covariates were similar between studies, how these were measured and the breadth of variables measured varied. This highlights the need for agreed tools on measurement of psychosocial risk in research.
The cross sectional nature of the majority of papers in the review means that only associations of prevalence with risk factors can be examined not causality. In an attempt to address the issue of misclassification bias due to false positives we only examined the relationship between risk factors and high versus low/no developmental risk. Thus any significant relationship is likely to be an underestimate of the true strength of association [17].
Conclusions
This systematic review found that the prevalence of parental concerns indicating developmental risk on the PEDS is substantial. As with most systematic reviews there were methodological issues with many of the primary studies with variable quality in sampling, representativeness and reporting. Nevertheless, the level of parental concerns that indicate developmental risk highlights the need to support families and promote early childhood development. At the individual level, parents, especially those in disadvantaged communities, should be asked systematically about their concerns and service providers should respond to these concerns through advice, support and facilitating further assessment and early intervention as required [11, 74, 75]. At the population level families should have access to universal high quality early childhood services that optimise child development. Given the prevalence of parental concerns increased with biological and psychosocial adversity, the service response needs to be one of proportionate universalism where the greater the disadvantage, the more services available [68].
Electronic supplementary material
Additional file 1: Search strategy. (DOC 34 KB)
Acknowledgement
Many thanks to Professor Frances Glascoe and Associate Professor Sharon Goldfeld for consultation in regards to access to unpublished PEDS data.
What’s known on this subject?
Children at developmental risk are more likely to have long term adverse educational and health outcomes. Parental concerns about their child’s development measured by the Parents’ Evaluation of Developmental Status (PEDS) has been used as an indicator of developmental risk.
What this study adds
The prevalence of parental concerns measured with the PEDS that indicate developmental risk is substantial. There is increased prevalence associated with biological and psychosocial adversity.
Abbreviations
- PEDS
Parents Evaluation of Developmental Status.
Footnotes
Competing interests
“Financial Disclosure: The authors have no financial relationships relevant to this article to disclose”.
“Potential Non- financial Competing Interests: The authors have no non-financial competing interests relevant to this article to disclose”.
Authors’ contributions
SW conceptualized and designed the study, systematically searched the literature, excluded and included papers; designed the data collection form, extracted and analysed the data from the papers, assessed quality of the papers; drafted the initial manuscript and revised all subsequent versions of the manuscript. VE independently excluded and included papers from the systematic literature search assessed their quality and extracted data and reviewed and revised the manuscript. KW provided consensus for SW and VE when difference around exclusion/inclusion of papers and quality scoring and critically reviewed and revised the manuscript. AH undertook the data analysis of the prevalence data and supported SW in the data analysis of the risk factor data, critically reviewed the manuscript. NS supported SW in the design of the systematic review and critically reviewed and revised the manuscript. LK provided content expertise, supervised SW project management and critically reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Contributor Information
Susan Woolfenden, Email: susan.woolfenden@sesiahs.health.nsw.gov.au.
Valsamma Eapen, Email: v.eapen@unsw.edu.au.
Katrina Williams, Email: Katrina.Williams@rch.org.au.
Andrew Hayen, Email: a.hayen@unsw.edu.au.
Nicholas Spencer, Email: n.j.spencer@warwick.ac.uk.
Lynn Kemp, Email: l.kemp@unsw.edu.au.
References
- 1.Goldfeld S, O’Connor M, Sayers M, Moore T, Oberklaid F. Prevalence and correlates of special health care needs in a population cohort of australian children at school entry. J Dev Behav Pediatr. 2012;33:319–327. doi: 10.1097/DBP.0b013e31824a7b8e. [DOI] [PubMed] [Google Scholar]
- 2.Guralnick MJ. Effectiveness of early intervention for vulnerable children: a developmental perspective. Am J Ment Retard. 1997;102:319–345. doi: 10.1352/0895-8017(1998)102<0319:EOEIFV>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.King EH, Logsdon DA, Schroeder SR. Risk factors for developmental delay among infants and toddlers. Child Health Care. 1992;21:39–52. doi: 10.1207/s15326888chc2101_6. [DOI] [PubMed] [Google Scholar]
- 4.Zeanah CH, Boris NW, Larrieu JA. Infant development and developmental risk: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1997;36:165–178. doi: 10.1097/00004583-199702000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Patrianakos-Hoobler AI, Msall ME, Marks JD, Huo D, Schreiber MD. Risk factors affecting school readiness in premature infants with respiratory distress syndrome. Pediatrics. 2009;124(1):258–267. doi: 10.1542/peds.2008-1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sameroff A. The Transactional Model Of Development: How Children And Contexts Shape Each Other. (pp. 3–21). xiv, 290 pp. In: Sameroff AE, editor. The Transactional Model. Washington, DC, US: American Psychological Association; 2009. [Google Scholar]
- 7.Stevens GD. Gradients in the health status and developmental risks of young children: the combined influences of multiple social risk factors. Matern Child Health J. 2006;10:187–199. doi: 10.1007/s10995-005-0062-y. [DOI] [PubMed] [Google Scholar]
- 8.Zuckerman B, Stevens GD, Inkelas M, Halfon N. Prevalence and correlates of high-quality basic pediatric preventive care. Pediatrics. 2004;114:1522–1529. doi: 10.1542/peds.2004-0635. [DOI] [PubMed] [Google Scholar]
- 9.NH&MRC: Centre for Community Child Health (RCH) Child Health Screening and Surveillance: A Critical Review of the Literature. Canberra: National Health and Medical Research Council; 2002. [Google Scholar]
- 10.AAP Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006;118:405–420. doi: 10.1542/peds.2006-1231. [DOI] [PubMed] [Google Scholar]
- 11.Oberklaid F, Baird G, Blair M, Melhuish E, Hall D. Arch Dis Child. 2013. Children’s health and development: approaches to early identification and intervention. [DOI] [PubMed] [Google Scholar]
- 12.National Screening Committee: Child health sub-group report on developmental and behavioural problems.http://www.screening.nhs.uk/policydb_download.php?doc=144
- 13.Glascoe FP. Using parents’ concerns to detect and address developmental and behavioral problems. J Soc Pediatr Nurs. 1999;4:24–35. doi: 10.1111/j.1744-6155.1999.tb00077.x. [DOI] [PubMed] [Google Scholar]
- 14.Glascoe F. Collaborating with Parents: Using Parents’ Evaluation of Developmental Status (PEDS) to Detect And Address Developmental And Behavioral Problems. 2. Nolensville, TN: PEDSTest.com, LLC; 2013. [Google Scholar]
- 15.Armstrong M, Goldfeld S. Good Beginnings For Young Children And Families: A Feasibility Study. City of Wodonga: Centre for Community Child Health (RCH); 2004. pp. 1–106. [Google Scholar]
- 16.National Survey of Children’s Health, Data Resource Center for Child and Adolescent Health, Centre for Disease Controlhttp://childhealthdata.org/learn/NSCH accessed Sept2013
- 17.Simon AE, Pastor PN, Avila RM, Blumberg SJ. Socioeconomic disadvantage and developmental delay among US children aged 18 months to 5 years. J Epidemiol Community Health. 2013;67:689–695. doi: 10.1136/jech-2013-202610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ng W, Reynolds D, Kennedy E, Feightner K, Holowaty P, Wade K, Fleiszer P, Northrup D, Glascoe F. Measuring the prevalence of children at risk using; parents’ evaluation of developmental status in a telephone survey. Child Indicators Res. 2010;3:167–181. doi: 10.1007/s12187-009-9046-6. [DOI] [Google Scholar]
- 19.Loney PL, Chambers LW, Bennett KJ, Roberts JG, Stratford PW. Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Dis Can. 1998;19:170–176. [PubMed] [Google Scholar]
- 20.Agresti A, Coull B. Approximate is better than ‘exact’ for interval estimation of binomial proportions. Amer Statist. 1998;52:119–126. [Google Scholar]
- 21.Hamza T, van Houwelingen H, Stijnen T. The binomial distribution of meta-analysis was preferred to model within-study variability. J Clin Epidemiol. 2008;61:41–51. doi: 10.1016/j.jclinepi.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 22.Williams JG, Higgins JP, Brayne CE. Systematic review of prevalence studies of autism spectrum disorders. Arch Dis Child. 2006;91:8–15. doi: 10.1136/adc.2004.062083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, Altman D, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chuan LB, Hock TT, Bin Bujang MA, Haniff J, Chang WS, Abdullah MR, F.P G . Parents’ Evaluation Of Developmental Status – Validation And Feasbility Of Use Of Its Tranlsated Malay And Mandarin Version. 2012. [Google Scholar]
- 25.Davies S, Feeney H. A pilot of the Parents’ Evaluation of Developmental Status tool. Community Pract. 2009;82:29–31. [PubMed] [Google Scholar]
- 26.Roux A, Herrera P, Wold C, Dunkle M, Glascoe F, Shattuck P. Using 211 to Reach an Underserved Population with Developmental and Autism Screening. Washington University in St. Louis.http://www.pedstest.com/Research/tabid/91/articleType/CategoryView/categoryId/1/Articles-and-Abstracts.aspx accessed Jan 2013. 2011. [Google Scholar]
- 27.Armstrong MF, Goldfeld S. Systems of early detection in Australian communities: the use of a developmental concern questionnaire to link services. Aust J Adv Nurs. 2008;25:36–42. [Google Scholar]
- 28.Coghlan D, King J, Wake M. Parents’ Evaluation of Developmental Status in the Australian day-care setting:Developmental concerns of parents and carers. J Paediatr Child Health. 2003;39:49–54. doi: 10.1046/j.1440-1754.2003.00084.x. [DOI] [PubMed] [Google Scholar]
- 29.Bethell C, Reuland C, Schor E, Abrahms M, Halfon N. Rates of parent-centered developmental screening: disparities and links to services access. Pediatrics. 2011;128:146–155. doi: 10.1542/peds.2010-0424. [DOI] [PubMed] [Google Scholar]
- 30.Coker TR, Shaikh Y, Chung PJ. Parent-reported quality of preventive care for children at-risk for developmental delay. Acad Pediatr. 2012;12:384–390. doi: 10.1016/j.acap.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sarmiento Campos JA, Squires J, Ponte J. Universal developmental screening: preliminary studies in Galicia, Spain. Early Child Dev Care. 2011;181:475–485. doi: 10.1080/03004430903458007. [DOI] [Google Scholar]
- 32.Glascoe FP. The importance of discussing parents’ concerns about development: do Parents Express Concerns Spontaneously? Ambul Child Health. 1997;2:349–356. [Google Scholar]
- 33.Glascoe FP, Macias M, Herrera P, Brixey S, Simpson P, Li S: How do screening tests perform in settings serving at-risk populations?J Dev Behav Pediatr in press,2010 PEDStest website, http://www.pedstest.com/Research/tabid/91/articleType/CategoryView/categoryId/1/Articles-and-Abstracts.aspx accessed Jan 2013
- 34.Zuckerman KE, Boudreau AA, Lipstein EA, Kuhlthau KA, Perrin JM. Household language, parent developmental concerns, and child risk for developmental disorder. Acad Pediatr. 2009;9:97–105. doi: 10.1016/j.acap.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 35.McGookin E, D’Sa V. Developmental screening in a pediatric care practice. Med Health R I. 2011;94:194–196. [PubMed] [Google Scholar]
- 36.Cook JT, Frank DA, Casey PH, Rose-Jacobs R, Black MM, Chilton M, DeCuba SE, Appugliese D, Coleman S, Heeren T, Berkowitz C, Cutts DB. A brief indicator of household energy security: associations with food security, child health, and child development in us infants and toddlers. Pediatrics. 2008;122:e867–e875. doi: 10.1542/peds.2008-0286. [DOI] [PubMed] [Google Scholar]
- 37.Rose-Jacobs R, Black MM, Casey PH, Cook JT, Cutts DB, Chilton M, Heeren T, Levenson SM, Meyers AF, Frank DA. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. 2008;121:65–72. doi: 10.1542/peds.2006-3717. [DOI] [PubMed] [Google Scholar]
- 38.Sices L, Stancin T, Kirchner L, Bauchner H. PEDS and ASQ developmental screening tests may not identify the same children. Pediatrics. 2009;124:e640–647. doi: 10.1542/peds.2008-2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tough SC, Siever JE, Benzies K, Leew S, Johnston DW. Maternal well-being and its association to risk of developmental problems in children at school entry. BMC Pediatr. 2010;10:19. doi: 10.1186/1471-2431-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tough SC, Siever JE, Leew S, Johnston DW, Benzies K, Clark D: Maternal mental health predicts risk of developmental problems at 3 years of age: follow up of a community based trial.BMC Pregnancy Childbirth 2008.,8(16): [DOI] [PMC free article] [PubMed]
- 41.Kiing JS, Low PS, Chan YH, Neihart M. Interpreting parents’ concerns about their children’s development with the Parents Evaluation of Developmental Status: culture matters. J Dev Behav Pediatr. 2012;33:179–183. doi: 10.1097/DBP.0b013e31823f686e. [DOI] [PubMed] [Google Scholar]
- 42.Kosht-Fedeyshin M. Internet J Trop Med. 2006. Translation of the Parents’ Evaluation of Developmental Status (PEDS) Developmental Screening Tool for Identification of Developmental Delay in Children from Birth to Five Years of Age in the Karagwe District of Northwestern Tanzania, East Africa: a pilot study. [Google Scholar]
- 43.Limbos MM, Joyce DP. Comparison of the ASQ and PEDS in screening for developmental delay in children presenting for primary care. J Dev Behav Pediatr. 2011;32:499–511. doi: 10.1097/DBP.0b013e31822552e9. [DOI] [PubMed] [Google Scholar]
- 44.Malhi P, Singh P. Role of Parents’ Evaluation of Developmental Status in detecting developmental delay in young children. Indian Pediatr. 2002;39:271–275. [PubMed] [Google Scholar]
- 45.Matibag R, Navarro J. Use of Parents Evaluation of Developmental Status (PEDS) Questionnaire Among Pre-School Children aged 2–5 years old: Developmental Concerns of Parents and Teachers. 2008. [Google Scholar]
- 46.Oreto J, Navarro J, Tanchanco L. The use of the Filipino Parents’ Evaluation of Developmental Status (PEDS) Among Children aged 0–8 years old. 2010. [Google Scholar]
- 47.California Health Interview Survey 2009.http://healthpolicy.ucla.edu/chis/
- 48.California Health Interview Survey 2007.http://healthpolicy.ucla.edu/chis/
- 49.California Health Interview Survey 2005.http://healthpolicy.ucla.edu/chis/
- 50.California Health Interview Survey 2003.http://healthpolicy.ucla.edu/chis/
- 51.Palarca CT. The Role of Parents’ Evaluation of Developmental Status (PEDS) As A Screening Tool In The Early Detection Of Developmental Disabilities And Behavioural Disorders In Filipino Children Ages 0–96 Months Old In Gingoong City. 2008. [Google Scholar]
- 52.Restall G, Borton B. Parents’ concerns about their children’s development at school entry. Child Care Health Dev. 2010;36:208–215. doi: 10.1111/j.1365-2214.2009.01019.x. [DOI] [PubMed] [Google Scholar]
- 53.Theeranate K, Chuengchitraks S. Parent’s Evaluation of Developmental Status (PEDS) detects developmental problems compared to Denver II. J Med Assoc Thai. 2005;88(Suppl 3):S188–192. [PubMed] [Google Scholar]
- 54.VSEHQ . Outcomes For Victorian Children At School Entry. State And Local Findings From The School Entrant Health Questionnaire 2008. Melbourne, Victoria: Data Outcomes and Evaluation Division, Office for Children and Portfolio Coordination, Department of Education and Early Childhood Development; 2011. [Google Scholar]
- 55.Wake M, Gerner B, Gallagher S. Does parents’ evaluation of developmental status at school entry predict language, achievement, and quality of life 2 years later? Ambul Pediatr. 2005;5:143–149. doi: 10.1367/A04-162R.1. [DOI] [PubMed] [Google Scholar]
- 56.Ibironke JO, Friedman DS, Repka MX, Katz J, Giordano L, Hawse P, Tielsch JM. Child development and refractive errors in preschool children. Optom Vis Sci. 2011;88:181–187. doi: 10.1097/OPX.0b013e318204509b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tough S, Siever J, Benzies K, Leew S, Johnston DW. Calgary Children’s Initiative. 2006. Study Report: Screening For Developmental Problems Among Preschool-Aged Children. [Google Scholar]
- 58.Glascoe FP. A method for deciding how to respond to parents’ concerns about development and behavior… including commentary by Oberklaid F. Ambul Child Health. 1999;5:197–208. [Google Scholar]
- 59.Gustawan WI, Machfudz S. Validity of parents’ evaluation of developmental status (PEDS) in detecting developmental disorders in 3–12 month old infants. Paediatr Indones. 2010;50:6–10. [Google Scholar]
- 60.Mistry RS, Benner AD, Biesanz JC, Clark SL, Howes C. Family and social risk, and parental investments during the early childhood years as predictors of low-income children’s school readiness outcomes. Early Childhood Res Q. 2010;25:432–449. doi: 10.1016/j.ecresq.2010.01.002. [DOI] [Google Scholar]
- 61.Linver MR, Brooks-Gunn J, Kohen D. Parenting behavior and emotional health as mediators of family poverty effects upon young low-birthweight children’s cognitive ability. Ann N Y Acad Sci. 1999;896:376–898. doi: 10.1111/j.1749-6632.1999.tb08146.x. [DOI] [PubMed] [Google Scholar]
- 62.Walker SP, Wachs TD, Grantham-McGregor S, Black MM, Nelson CA, Huffman SL, Baker-Henningham H, Chang SM, Hamadani JD, Lozoff B, Gardner JM, Powell CA, Rahman A, Richter L. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011;378:1325–1338. doi: 10.1016/S0140-6736(11)60555-2. [DOI] [PubMed] [Google Scholar]
- 63.Braveman PA, Egerter SA, Woolf SH, Marks JS. When do we know enough to recommend action on the social determinants of health? Am J Prev Med. 2011;40:S58–66. doi: 10.1016/j.amepre.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 64.Smart D, Sanson A, Baxter J, Edwards B, Hayes A. Book Home-To-School Transitions For Financially Disadvantaged Children (Editor ed.^eds.) 2008. Home-To-School Transitions For Financially Disadvantaged Children. [Google Scholar]
- 65.Glascoe FP. The value of ‘parents’ evaluations of developmental status’ in detecting and addressing children’s developmental and behavioral problems. Assess Eff Interv. 1998;23:185–203. doi: 10.1177/073724779802300401. [DOI] [Google Scholar]
- 66.Anderson LM, Shinn C, Fullilove MT, Scrimshaw SC, Fielding JE, Normand J, Carande-Kulis VG. The effectiveness of early childhood development programs: a systematic review. Am J Prev Med. 2003;24:32–46. doi: 10.1016/S0749-3797(02)00655-4. [DOI] [PubMed] [Google Scholar]
- 67.Shonkoff JP. From neurons to neighborhoods: old and new challenges for developmental and behavioral pediatrics. J Dev Behav Pediatr. 2003;24:70–76. doi: 10.1097/00004703-200302000-00014. [DOI] [PubMed] [Google Scholar]
- 68.Marmot M. The Marmot Review. 2010. Fair Society, Healthy Lives. [Google Scholar]
- 69.Hart JT. The inverse care law. Lancet. 1971;1:405–412. doi: 10.1016/S0140-6736(71)92410-X. [DOI] [PubMed] [Google Scholar]
- 70.Miller JE. Developmental screening scores among preschool-aged children: the roles of poverty and child health. J Urban Health. 1998;75(1):135–152. doi: 10.1007/BF02344935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Moraes MW, Weber APR, Santos MCO, Almeida FA. Denver II: evaluation of the development of children treated in the outpatient clinic of Project Einstein in the Community of Paraisópolis. Einstein (Säo Paulo) 2010;8(2 pt 1):149–153. doi: 10.1590/S1679-45082010AO1620. [DOI] [PubMed] [Google Scholar]
- 72.Nair MK, George B, Padma K, Potti N, Elizabeth KE, Jeyaseelan L. Developmental Evaluation Clinic–CDC experience. Indian Pediatr. 2009;46(Suppl):s63–66. [PubMed] [Google Scholar]
- 73.Blanchard LT, Gurka MJ, Blackman JA. Emotional, developmental, and behavioral health of American children and their families: a report from the 2003 National Survey of Children’s Health. Pediatrics. 2006;117:e1202–1212. doi: 10.1542/peds.2005-2606. [DOI] [PubMed] [Google Scholar]
- 74.Kemp L, Harris E, McMahon C, Matthey S, Vimpani G, Anderson T, Schmied V, Aslam H, Zapart S. Child and family outcomes of a long-term nurse home visitation programme: a randomised controlled trial. Arch Dis Child. 2011;96:533–540. doi: 10.1136/adc.2010.196279. [DOI] [PubMed] [Google Scholar]
- 75.Zoritch B, Roberts I, Oakley A. Day care for pre-school children. Cochrane Database Syst Rev. 2000;3:CD000564. doi: 10.1002/14651858.CD000564. [DOI] [PubMed] [Google Scholar]
Pre-publication history
- The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2431/14/231/prepub
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Search strategy. (DOC 34 KB)


