ABSTRACT
BACKGROUND
Little is known about whether more experience with an electronic health record (EHR) makes it easier for providers to meaningfully use EHRs.
OBJECTIVE
To assess whether the length of time that small practice providers have been using the EHR is associated with greater ease in performing meaningful use-related tasks and fewer EHR-related concerns.
DESIGN/PARTICIPANTS
We administered a web-based survey to 400 small practice providers in medically underserved communities in New York City participating in an EHR implementation and technical assistance project. We used logistic regression to estimate the association between the length of time a provider had been using the EHR (i.e., “live”) and the ease of performing meaningful use-related tasks and EHR-related concerns, controlling for provider and practice characteristics.
KEY RESULTS
Compared to providers who had been live 6 to 12 months, providers who had been live 2 years or longer had 2.02 times greater odds of reporting it was easy to e-prescribe new prescriptions (p < 0.05), 2.12 times greater odds of reporting it was easy to e-prescribe renewal prescriptions (p < 0.05), 2.02 times greater odds of reporting that quality measures were easy to report (p < 0.05), 2.64 times greater odds of reporting it was easy to incorporate lab results as structured data (p < 0.001), and 2.00 times greater odds of reporting it was easy to generate patient lists by condition (p < 0.05). Providers who had been live 2 years or longer had 0.40 times lower odds of reporting financial costs were a concern (p < 0.001), 0.46 times lower odds of reporting that productivity loss was a concern (p < 0.05), 0.54 times lower odds of reporting that EHR unreliability was a concern (p < 0.05), and 0.50 times lower odds of reporting that privacy/security was a concern (p < 0.05).
CONCLUSIONS
Providers can successfully adjust to the EHR and over time are better able to meaningfully use the EHR.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-014-2891-0) contains supplementary material, which is available to authorized users.
KEY WORDS: electronic health records, primary care, population health, physician satisfaction, vulnerable populations
INTRODUCTION
The majority of outpatient care is administered via small practices.1 Yet, as national electronic health record (EHR) adoption rates rise,2–4 small practice providers still lag behind large practices in rates of adoption. This is particularly true for practices that are located in underserved settings, are physician-owned, or run by solo practitioners.5–8
Recognizing that primary care providers in small practices serving the underserved are likely to have fewer resources to implement health information technology, New York City, through a mayoral initiative, subsidized the acquisition of eClinicalWorks™ software, a fully functional EHR with clinical decision support functionalities.9 This effort, known as the Primary Care Information Project (PCIP), has become one of the largest community-wide EHR implementation and technical assistance projects in the country. PCIP established NYC REACH, a Regional Extension Center (REC) that is designated by the Office of the National Coordinator for Health Information Technology (ONC) to assist small practice providers in the adoption and “meaningful use” of EHRs.10 Around the same time, the Centers for Medicare and Medicaid Services began to incentivize providers to adopt and use EHRs.11 Meaningful use refers to using the EHR to not only provide care, but to improve the quality of care.
Despite policy efforts to facilitate the adoption and meaningful use of EHRs, small practices face numerous barriers and challenges in using EHRs effectively to improve the quality of care and practice medicine more efficiently. Small practices have greater financial barriers and fewer resources to implement the required changes in information technology (IT) infrastructure.6,12 EHR implementation causes disruptions to practice workflow that are harder to adjust to in practices that have fewer administrative staff and less physical space.13,14 These challenges can undermine the successful adoption of EHRs and sustained meaningful use. Little is known about the learning curve for successful use of EHRs, particularly whether more experience with an EHR increases ease of use and improves providers’ ability to perform clinical tasks related to meaningfully using the EHR.
We assessed the relationship between how long small practice (ten or fewer) providers have used the EHR (time “live”) and their ease of use and challenges with the system. Our research questions were: Does more experience with the EHR ease providers’ ability to perform meaningful use-related tasks? What tasks do providers struggle with most? What are the biggest concerns for small practice providers after EHR adoption? Are there fewer concerns the longer a provider has been live on the EHR?
METHODS
Survey Development
We developed a 45-item provider survey (see Online Appendix). The survey assessed providers’ ease of use, satisfaction, and challenges with EHR implementation and use, satisfaction with PCIP/NYC REACH services, and provider and practice demographics. The survey was developed with input from field staff representatives who had worked closely with practices to implement the EHR. Where available, we modified questions from provider surveys PCIP had administered in the past.15 The survey was aligned with Meaningful Use concepts11,16(Table 2). Cognitive testing was performed with a provider champion and the survey was pilot tested internally and with members of PCIP’s Provider Advisory Board. The study was approved by the Institutional Review Board of the New York City Department of Health and Mental Hygiene.
Table 2.
Percent of Providers Who Reported that a Task Was Easy to Perform Using the EHR, Along with Odds Ratios Adjusting for Provider Characteristics (N =400)*
| Length of time live on EHR (unadjusted percentages) | Adjusted models† | |||||
|---|---|---|---|---|---|---|
| EHR task | 6–12 months (N =90) | 1–2 years (N =129) | 2+ years (N =181) | Overall | 1–2 years OR (95 % CI) | 2+ years OR (95 % CI) |
| Managing patient clinical information (%) | ||||||
| Record demographics | 69.9 % | 67.8 % | 72.9 % | 70.6 % | 0.93 (0.50, 1.74) | 1.36 (0.74, 2.51) |
| Maintain up-to-date problem list | 70.7 % | 71.2 % | 78.2 % | 74.3 % | 1.05 (0.56, 1.99) | 1.83 (0.97, 3.45) |
| Maintain an active medication list | 75.9 % | 72.0 % | 76.5 % | 74.9 % | 0.70 (0.36, 1.36) | 1.21 (0.63, 2.32) |
| Maintain an active allergy list | 80.7 % | 82.9 % | 81.8 % | 81.9 % | 1.14 (0.54, 2.40) | 1.25 (0.62, 2.52) |
| Record and chart changes in vital signs as structured data | 80.5 % | 83.8 % | 81.8 % | 82.1 % | 1.21 (0.57, 2.58) | 1.24 (0.61, 2.52) |
| Record smoking status for patients over 13 as structured data | 79.5 % | 79.7 % | 73.9 % | 77.1 % | 1.00 (0.49, 2.05) | 0.87 (0.45, 1.70) |
| Order lab/radiology tests as structured data | 51.8 % | 54.7 % | 64.1 % | 58.3 % | 1.08 (0.60, 1.93) | 1.90 (1.09, 3.33)‡ |
| Managing medications (%) | ||||||
| “E-prescribe” new prescriptions | 67.5 % | 78.8 % | 76.7 % | 75.3 % | 1.75 (0.90, 3.40) | 2.02 (1.07, 3.81)‡ |
| “E-prescribe” renewal prescriptions‡ | 61.0 % | 76.1 % | 73.7 % | 71.6 % | 1.87 (0.98, 3.56) | 2.12 (1.15, 3.91)‡ |
| Population health (%) | ||||||
| Report quality measures to CMS/state‡ | 21.3 % | 24.1 % | 36.2 % | 29.0 % | 1.09 (0.54, 2.21) | 2.02 (1.06, 3.85)‡ |
| Generate lists of patients by condition‡ | 32.1 % | 47.5 % | 47.6 % | 44.1 % | 1.94 (1.06, 3.56) ‡ | 2.00 (1.12, 3.57)‡ |
| Send reminders to patients for preventive/follow up care | 28.4 % | 27.1 % | 31.7 % | 29.5 % | 0.90 (0.47, 1.73) | 1.06 (0.58, 1.96) |
| Order preventive care services during visit | 48.8 % | 61.0 % | 60.8 % | 58.2 % | 1.73 (0.95, 3.14) | 1.97 (1.11, 3.48)‡ |
| Patient engagement (%) | ||||||
| Provide clinical summaries for each office visit | 56.8 % | 54.2 % | 58.7 % | 56.8 % | 0.90 (0.50, 1.61) | 1.05 (0.60, 1.82) |
| Provide patients with an electronic copy of their health information upon request and in a timely fashion | 61.0 % | 57.6 % | 62.7 % | 60.7 % | 0.86 (0.48, 1.54) | 1.11 (0.63, 1.94) |
| Care coordination (%) | ||||||
| Communicate referrals | 29.6 % | 29.7 % | 21.0 % | 25.7 % | 0.87 (0.46, 1.65) | 0.57 (0.30, 1.07) |
| Review referrals | 22.2 % | 25.6 % | 20.7 % | 22.7 % | 1.12 (0.56, 2.25) | 0.78 (0.39, 1.54) |
| Incorporate clinical lab test results as structured data§ | 43.4 % | 60.7 % | 64.5 % | 58.5 % | 2.05 (1.14, 3.69) ‡ | 2.64 (1.50, 4.65)‖ |
| Provide summary of care record for referrals | 30.0 % | 40.0 % | 40.4 % | 38.0 % | 1.50 (0.81, 2.78) | 1.53 (0.85, 2.74) |
| Billing (%) | ||||||
| Document CPT/ICD-9 codes as structured data | 70.7 % | 68.4 % | 70.3 % | 69.8 % | 0.87 (0.46, 1.63) | 1.12 (0.61, 2.05) |
*“Neutral”, “somewhat difficult”, “very difficult”, and “don’t know/NA” counted as “not easy”; “somewhat easy” and “very easy” counted as “easy”
†Number of patient encounters, number of providers, specialty (Pediatrics), receipt of a medical degree between 2000 and 2009, owning the practice, workload of > 50 h, and English as a first language are controlled for in the adjusted models; p values based on Chi-square statistic (unadjusted percentages) and logistic regression models. Reference group is being live on the EHR for 6–12 months
‡p < 0.05
§p < 0.01
‖p < 0.001
Study Design and Population
Our study uses a cross-sectional design based on a single survey administered to providers (physicians, nurse practitioners, and physician assistants). Providers were invited to complete the survey if they were PCIP members, worked in a small practice (generally ten or fewer providers) at least one full day a week, had been using the EHR for at least 6 months, and had a valid email address. The invited sample was extracted from Salesforce™, which is used for program administration. Extensive outreach efforts were made to obtain valid email addresses for at least 50 % of the providers at each practice.
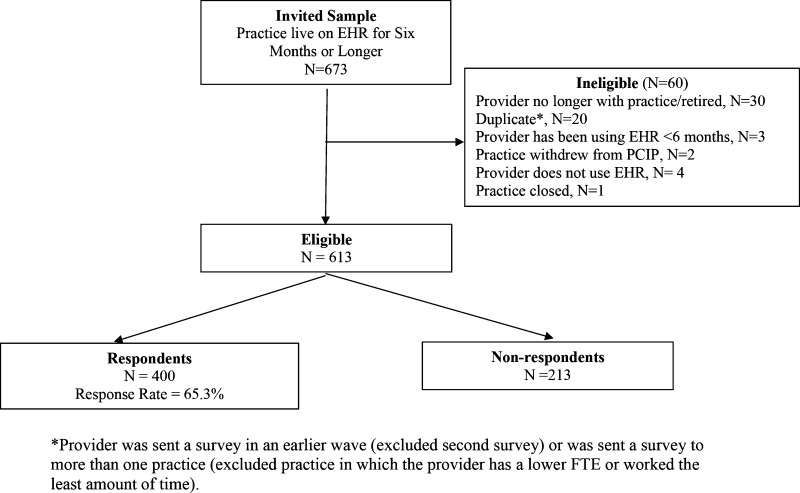
The survey was administered through SurveyGizmo™, a web-based survey tool. Survey administration spanned from November 2010 to October 2011. Because about half of the practices recently completed another major PCIP survey, it was administered in two stages in order to avoid survey fatigue. Email reminders were sent to non-responders and at least three reminder phone calls were conducted between seven (Wave 1) and 14 (Wave 2) weeks. Figure 1 shows a flow chart of the survey sample. If a non-provider (e.g., office manager) responded to the survey, or a provider reported using the EHR for less than 6 months, they were exited from the survey. Providers were offered a $25 Amazon electronic gift card for responding and Wave 1 respondents were also entered in a lottery for a REC membership ($600 value).
Figure 1.
Flow chart of survey sample.
Measures
The predictor variable was length of time live on the EHR. Providers indicated how long they had been using the EHR to document patient care (i.e., “live”): “between 6 and 12 months”, “more than 1 year but less than 2 years”, or “2 years or more.” Providers who responded “don’t know/remember”, or were missing data on the question (N =18) were included in the analysis and the length of time the practice was live on the EHR was calculated from the date the practice went live.
There were two sets of outcome variables. Providers were asked: “Please indicate the level of difficulty for you to do the following tasks using the EHR”, with a series of 20 items, e.g., “order laboratory and radiology tests as structured data (i.e., not free text)” (Table 2). To increase interpretability and focus on EHR ease of use,17 answer choices were dichotomized into not easy (“neutral”, “somewhat difficult”, “very difficult”, “don’t know,” “NA”) or easy (“somewhat easy”, “very easy”). For the second set of outcome variables, providers were asked: “At the present time, how much of a concern is each of the following in using or increasing your use of the EHR?” with ten concerns, e.g., “financial costs (start-up or ongoing costs, not enough return on investment or ‘ROI’)” (Table 3). Answer choices were dichotomized into whether providers were concerned (“major concern” or “minor concern”) or not concerned (“not a concern”, “no longer a concern”, “don’t know”, “NA”).
Table 3.
Percent of Providers Who Reported Item Was a Major or a Minor Concern in Using the EHR and Odds Ratios Adjusting for Provider Characteristics (N =400)*
| Length of time live on EHR (unadjusted percentages) | Adjusted models† | |||||
|---|---|---|---|---|---|---|
| EHR task | 6–12 months (N = 90) | 1–2 years (N = 129) | 2+ years (N = 181) | Overall | 1–2 years OR (95 % CI) | 2+ years OR (95 % CI) |
| Time constraints (to select, contract, and implement the EHR) | 51.8 % | 41.5 % | 37.4 % | 42.0 % | 0.66 (0.37,1.17) | 0.51 (0.29,0.88) |
| Financial costs (start-up or ongoing costs, not enough return on investment, or “ROI”)§ | 65.4 % | 47.9 % | 43.5 % | 49.7 % | 0.51 (0.27,0.94)‡ | 0.40 (0.22,0.72)§ |
| Loss of productivity during transition to the EHR system§ | 56.1 % | 46.2 % | 35.9 % | 43.7 % | 0.69 (0.39,1.23) | 0.46 (0.26,0.80)‡ |
| Lack of computer skills (your own, other providers, your staff) | 46.3 % | 43.2 % | 35.7 % | 40.5 % | 0.92 (0.52,1.64) | 0.66 (0.38,1.15) |
| Training issues (scheduling, time involved, staff turnover) | 61.0 % | 58.1 % | 51.8 % | 55.9 % | 0.88 (0.49,1.59) | 0.73 (0.42,1.27) |
| Unwillingness of other providers at the practice to use the technology | 24.4 % | 26.5 % | 21.2 % | 23.6 % | 1.07 (0.55,2.10) | 0.88 (0.46,1.68) |
| Not being able to rely on the EHR due to glitches/errors/crashing | 72.8 % | 61.5 % | 58.8 % | 62.8 % | 0.59 (0.32,1.09) | 0.54 (0.30,0.98)‡ |
| Vendor not responsive/poor technical support | 67.1 % | 59.0 % | 62.9 % | 62.6 % | 0.66 (0.36,1.21) | 0.81 (0.45,1.45) |
| Available EHR software does not meet the practice’s needs (e.g. not able to use the EHR with practice’s billing/claims submission system) | 37.4 % | 26.3 % | 27.1 % | 29.2 % | 0.58 (0.32,1.09) | 0.62 (0.34,1.10) |
| Privacy or security concerns‡ | 43.9 % | 30.5 % | 28.5 % | 32.6 % | 0.55 (0.30,1.01)‡ | 0.50 (0.28,0.89)‡ |
*“No longer a concern”, “not a concern”, and “don’t know” were counted as “not concerned”; “major concern” and “minor concern” counted as “concerned”
†Number of patient encounters, number of providers, specialty (Pediatrics), receipt of a medical degree between 2000 and 2009, owning the practice, workload of > 50 h, and English as first language are controlled for in the models; p values based on Chi-square statistic (unadjusted percentages) and logistic regression models. The reference group is being live on the EHR for 6–12 months
‡p < 0.05
§p < 0.001
Analysis
We examined the relationship between time live on the EHR and perception of clinical tasks and EHR-related concerns. We performed Pearson chi square tests to compare ease of use across the three time intervals. We then estimated logistic regression models to test the relationship between providers’ length of time live on the EHR and the two sets of outcomes, while controlling for the number of patient encounters, number of providers, specialty, the year they received a medical degree, whether they owned the practice or not, workload, and whether or not English was a first language. We report the resulting adjusted odds ratios. We also compared provider and practice characteristics of respondents and non-respondents. All analyses were conducted using SAS 9.2.18
RESULTS
Sample Characteristics
Four hundred providers responded, for a response rate of 65.3 %. Table 1 shows the practice and provider characteristics of the survey respondents. Providers varied with respect to how long they had been using the EHR (“live”): 22.5 % were live on the EHR for between 6 and 12 months, 32.3 % were live on the EHR for between 1 and 2 years, and 45.3 % were live on the EHR for longer than 2 years. Providers who had been live longer had more patient encounters per year: 8,570.2 for those live between 6 and 12 months, 9,750.6 for those live between 1 and 2 years, and 13,111.3 for those live 2 years or more (p < 0.05). Larger practices tended to have used the EHR longer (marginally significant). There were also more pediatricians and fewer family/internal medicine providers in the 6 to 12 month group (p < 0.05). The number of providers at the practice, provider type, year of graduation from medical school, whether or not the provider was a full or part owner of the practice, workload, and whether or not the provider’s first language is English were not associated with the length of time live on an EHR. There were no differences between respondents and non-respondents for number of providers, number of patient encounters, type of provider, specialty, or how long the practice had been live on the EHR (data not shown).
Table 1.
Provider and Practice Characteristics of Survey Respondents (N = 400)
| 6–12 months N =90 | 1–2 years N =129 | 2+ years N =181 | Overall N =400 | p value* | |
|---|---|---|---|---|---|
| Practice characteristics† | |||||
| Number of patient encounters per year, mean (SD) | 8,570.2 (10,692.5) | 9,750.6 (12,840.1) | 13,111.3 (15,871.3) | 10,962.7 (13,951.8) | 0.02 |
| Number of providers at practice, mean (SD) | 3.9 (7.3) | 4.2 (5.4) | 5.8 (8.2) | 4.8 (7.3) | 0.06 |
| Provider characteristics | |||||
| Provider type (%) | |||||
| MD, DO | 93.3 | 86.1 | 91.2 | 90.0 | 0.16 |
| NP, PA, Other | 6.67 | 14.0 | 8.8 | 10.0 | |
| Specialty | |||||
| Family/internal medicine | 51.1 | 69.0 | 70.2 | 65.5 | 0.02 |
| Pediatrics | 31.1 | 20.2 | 22.1 | 23.5 | |
| Other | 17.8 | 10.9 | 7.7 | 11.0 | |
| Year of graduation from medical school (%) | 0.58 | ||||
| 1979 or earlier | 13.3 | 22.5 | 19.3 | 19.0 | |
| 1980–1989 | 40.0 | 34.9 | 28.7 | 33.3 | |
| 1990–1999 | 22.2 | 20.9 | 24.3 | 22.8 | |
| 2000–2009 | 11.1 | 10.1 | 14.4 | 12.3 | |
| Missing‡ | 13.3 | 11.6 | 13.3 | 12.8 | |
| Full or part-owner of practice (%) | 68.9 | 65.1 | 66.9 | 66.8 | 0.86 |
| Missing (N =42) | 12.2 | 10.1 | 9.9 | 10.5 | |
| Work load in hours per week (%) | 0.33 | ||||
| Up to 15 | 7.8 | 7.0 | 3.3 | 5.5 | |
| More than 15, up to 30 | 22.2 | 14.7 | 19.3 | 18.5 | |
| More than 30, up to 50 | 31.1 | 42.6 | 33.2 | 35.8 | |
| More than 50 | 24.4 | 24.8 | 30.4 | 27.3 | |
| Missing (N =52) | 14.4 | 10.9 | 13.8 | 13.0 | |
| English is not a first language (%) | 21.3 | 37.8 | 40.9 | 31.8 | 0.44 |
| Missing (N =45) | 14.4 | 9.3 | 11.1 | 11.3 | |
*Comparisons were based on ANOVA for continuous items and chi-square for categorical variables. Bold indicates significance at p < 0.05
†Patient encounters per year, number of providers, provider type, and specialty are from administrative data. Providers’ length of time live on the EHR, number of years in practice, workload, and data on providers for whom English is not a first language are from the survey
‡Providers who graduated medical school in 2010 or later were not captured in the data
Performance of Meaningful Use-Related Tasks
As shown in Table 2, providers reported the greatest difficulty reviewing referral information from specialists (22.7 % reported ease performing the task), communicating referrals (25.7 %), and reporting quality measures to the state or the Centers for Medicare and Medicaid Services (CMS) (29.0 %). Providers also reported difficulty with panel management activities, such as sending patient reminders for preventive/follow-up care (29.5 % reported ease performing the task). Providers reported the least amount of difficulty recording changes in vital signs (82.1 % reported ease) and maintaining an active medication allergy list (81.9 % reported ease).
Length of time live on the EHR was significantly associated with improvement on several EHR tasks. After controlling for provider and practice characteristics in the logistic regression models, out of the 20 meaningful use-related tasks, seven showed increased ease of use with longer time live. Compared to providers who had been live for 6 to 12 months, providers who had been live 2 years or longer had 2.02 times greater odds of reporting that it was easy to e-prescribe new prescriptions (p < 0.05), 2.12 times greater odds of reporting that it was easy to e-prescribe renewal prescriptions (p < 0.05), 2.02 times greater odds of reporting that it was easy to report quality measures (p < 0.05), 2.64 times greater odds of reporting that it was easy to incorporate lab results as structured data (p < 0.001), and 2.00 times greater odds of reporting that it was easy to generate patient lists by condition (p < 0.05).
Time live on the EHR was most strongly associated with tasks associated with population health. For example, for generating patient lists, 32.1 % of providers live between 6 and 12 months reported ease in performing the task, whereas 47.6 % of providers live 2 years or more reported ease (p < 0.05).
Concerns with Using the EHR
Table 3 shows the concerns providers had with using (or increasing use) of the EHR, grouped by the three time intervals, as well as the adjusted odds ratios from the logistic regression models. The largest concerns were not being able to rely on the EHR due to glitches/errors/crashing (62.8 % overall) and poor technical support by the vendor (62.6 % overall).
Results from the logistic models show that length of time live on the EHR was significantly associated with fewer concerns related to using (or increasing use of) the EHR for four out of the ten items (Table 3). Compared to providers who had been live for 6 to 12 months, providers who had been live 2 years or longer had 0.40 times lower odds of reporting that financial costs were a concern (p < 0.001), 0.46 times lower odds of reporting that productivity loss was a concern (p < 0.05), 0.54 times lower odds of reporting that not being able to rely on the EHR due to glitches/errors/crashing was a concern (p < 0.05), and 0.50 times lower odds of reporting that privacy or security was a concern (p < 0.05).
Overall Evaluation of the EHR
Overall, providers would adopt the EHR again if they had another opportunity to do so. Out of the 357 providers who responded to this question, 88.0 % would recommend their current EHR to other providers. Sixty-three percent of providers felt their revenue would eventually increase. Out of 366 respondents, only seven planned to restart the EHR adoption process by switching to another EHR vendor in the next 12 months, and only two providers planned to return to paper charts due to a negative experience with their current EHR.
DISCUSSION
We found some evidence that time live on the EHR was significantly associated with meaningful use-related tasks and a general trend towards greater ease of use with longer durations on the EHR. After 2 years of being live on the EHR, the majority (over 70 %) of small practice providers in our study report being able to perform most (9 of the 17) tasks related to meaningful use. Not all tasks are equal. Our finding that providers struggle the most with population health and panel management activities is consistent with findings from national surveys.16,19 Managing patient clinical information and managing medications suggest an “easy win” for using EHRs. Providers reported facility with these tasks even at the 6-month mark.
There are some key areas in which providers have lingering concerns and challenges. These include not being able to rely on the EHR due to glitches/errors/crashing and poor technical support by the vendor. This finding is similar to other reported challenges encountered by Regional Extension Center (REC) providers.20 Many of the leading EHR systems were developed prior to meaningful use, so vendors have also been challenged by the requirements.21 While there has been quick progress in adapting to the regulations, some have argued that the vendors have not kept up with market demands,22,23 and EHR usability remains a primary concern for providers.24 Practices are overwhelmed with the choices of vendors and need guidance to select an appropriate system. To address this concern, the ONC has devised a standardized certification system to help providers choose a vendor. The 2014 certification standards further narrow the vendor and system options for newly adopting practices, but the product upgrade process for practices already using a system will create new challenges for vendors as well as practices.
Our findings consistently show that providers who have been live on the EHR longer than 2 years report fewer concerns with the EHR. The largest differences between providers who have been live 6 to 12 months and those live 2 years or more are for concerns about financial costs and loss of productivity. This is not surprising, since those live 2 years have had more time to recover the financial investment of an EHR and bounce back from any loss in productivity. Importantly, providers overwhelmingly had positive appraisals of the overall EHR experience. The majority (88.0 %) would recommend their EHR vendor to their peers, and only two providers would switch back to paper charts.
Limitations
Our results may not generalize to providers using EHRs in different settings. The experiences reported in this study represent small practice providers in New York City, whom may face greater challenges in pursuing CMS Meaningful Use incentives. However, these providers received substantial resources (e.g., subsidized software, technical assistance) from the city and state, and thus may be better equipped to meet Meaningful Use standards.
Our findings do not reflect the effect of EHR adoption alone. This study does not make any inferences about practices’ performance on quality measures–only their use and experiences in using an EHR. A recent study comparing PCIP and non-PCIP comparison practices in New York State using independent data found that performance on quality measures improved over time on the EHR, but only for practices that had intense technical assistance.25
We did not explore whether providers’ motivation to adopt an EHR was different for the earlier adopters in our sample. Early adopters of health IT tend to have greater motivation for quality improvement.26–29 However, we controlled for provider characteristics such as specialty in the regression models, and did not observe differences.
Our study is not longitudinal. We did not follow providers over time to determine whether time on the EHR predicts better perceived performance on the EHR. Therefore, we cannot infer that being live on the EHR longer caused improved performance or fewer concerns.
The survey was administered through an online tool and did not offer a paper option. Although we obtained a response rate of over 65 %, there is a potential response bias in that providers who are struggling more with the EHR and/or less technologically savvy may have been less likely to respond to the survey. Respondents may also be more likely to report positive experiences with the EHR than non-respondents. However, there were few differences between responders and non-responders in observable provider and practice characteristics (data not shown).
Implications
Our findings support the idea that practices can adapt to the EHR over time to more meaningfully use the EHR. This message is an optimistic one for providers, who are concerned about productivity and the return on investment.30 However, providers are still faced with considerable challenges in using EHRs effectively, including challenges posed by the technology itself. Our providers, even those that have used the EHR for 2 years or more, still have substantial concerns about vendor non-responsiveness and unreliability of the EHR.
As initiatives in the Affordable Care Act evolve to enhance primary care, additional data are needed to understand how small practices in underserved neighborhoods are adapting to the continuously changing policy landscape. Funding for RECs is finite (currently through 2014, although CMS plans to continue the Meaningful Use program through 2021) and meaningful use standards will get progressively harder to achieve. Stage 2 focuses on electronic health information exchange as well as using the EHR for panel management.31 The preponderance of rules and regulations can create a cumulative burden that can be detrimental to physician satisfaction.22 It is crucial to solicit provider’s experiences with major federal policies affecting them.32,33 It is important to continuously monitor providers’ challenges, successes, and potential unintended consequences in progressing towards higher quality care at a lower cost.
Electronic supplementary material
(DOC 342 kb)
Acknowledgments
The authors would like to thank those who served on the Survey Development Group at PCIP, including Sheila Anane and Rachel Helfont and Dr. Larry Casalino, Dr. Tara Bishop, and Dr. Amanda Parsons for guidance in designing the survey. Thanks to Samantha Catlett and Maryam Khan for assistance with data collection and Brent Stackhouse for help obtaining survey honoraria. Thanks to the many people who tested the survey, including members of our Provider Advisory Board and PCIP staff. We would like to thank Dr. Andrew Ryan for helpful comments on the paper.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Funding
The New York City Tax Levy and the Office of the National Coordinator (ONC) for Health Information Technology funded the survey and supported the salaries of staff to conduct this study.
Contributor Information
Mandy Smith Ryan, Phone: (347) 396-4869, Email: mandysoft@gmail.com
Sarah C. Shih, Phone: 347.396.4895, Email: sshih@health.nyc.gov.
REFERENCES
- 1.Hing E, Burt CW. Office-Based Medical Practices: methods and Estimates From the National Ambulatory Medical Care Survey. Adv Data, No 383. Hyattsville, MD: National Center for Health Statistics; 2007. [PubMed] [Google Scholar]
- 2.Hsiao CJ, Hing E, Socey TC, Cai B. Electronic Health Record Systems and Intent to Apply for Meaningful use Incentives Among Office-Based Physician Practices: United States, 2001–2011. NCHS Data Brief, No 79. Hyattsville, MD: National Center for Health Statistics; 2011. p. 2011. [PubMed] [Google Scholar]
- 3.King J, Patel V, Furukawa MF. Physician Adoption of Electronic Health Record Technology to Meet Meaningful use Objectives: 2009–2012. ONC Data Brief, No. 7. Washington, DC: Office of the National Coordinator for Health Information Technology; 2012. [Google Scholar]
- 4.Patel V, Jamoom E, Hsiao CJ, Furukawa MF, Buntin M. Variation in electronic health record adoption and readiness for meaningful use: 2008–2011. J Gen Intern Med. 2013;28:957–64. doi: 10.1007/s11606-012-2324-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simon SR, Kaushal R, Cleary PD, et al. Correlates of electronic health record adoption in office practices: a statewide survey. J Am Med Inform Assoc. 2007;14:110–7. doi: 10.1197/jamia.M2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rao SR, Desroches CM, Donelan K, Campbell EG, Miralles PD, Jha AK. Electronic health records in small physician practices: availability, use, and perceived benefits. J Am Med Inform Assoc. 2011;18:271–5. doi: 10.1136/amiajnl-2010-000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Decker SL, Jamoom EW, Sisk JE. Physicians in nonprimary care and small practices and those age 55 and older lag in adopting electronic health record systems. Health Aff (Millwood) 2012;31:1108–14. doi: 10.1377/hlthaff.2011.1121. [DOI] [PubMed] [Google Scholar]
- 8.Jamoom E, Beatty P, Bercovitz A, Woodwell D, Palso K, Rechtsteiner E. Physician Adoption of Electronic Health Record Systems: United States, 2011. NCHS Data Brief, No 98. Hyattsville: National Center for Health Statistics; 2011. p. 2012. [PubMed] [Google Scholar]
- 9.Mostashari F, Tripathi M, Kendall M. A tale of two large community electronic health record extension projects. Health Aff (Millwood) 2009;28:345–56. doi: 10.1377/hlthaff.28.2.345. [DOI] [PubMed] [Google Scholar]
- 10.Maxson E, Jain S, Kendall M, Mostashari F, Blumenthal D. The regional extension center program: helping physicians meaningfully use health information technology. Ann Intern Med. 2010;153:666–70. doi: 10.7326/0003-4819-153-10-201011160-00011. [DOI] [PubMed] [Google Scholar]
- 11.Blumenthal D, Tavenner M. The “Meaningful Use” regulation for electronic health records. N Engl J Med. 2010;363:501–4. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 12.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med. 2008;359:50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- 13.Lee J, Cain C, Young S, Chockley N, Burstin H. The adoption gap: health information technology in small physician practices. Health Aff (Millwood) 2005;24:1364–6. doi: 10.1377/hlthaff.24.5.1364. [DOI] [PubMed] [Google Scholar]
- 14.Landon BE, Normand ST. Performance measurement in the small office practice: challenges and potential solutions. Ann Intern Med. 2008;148:353–7. doi: 10.7326/0003-4819-148-5-200803040-00006. [DOI] [PubMed] [Google Scholar]
- 15.Messeri P, Khan S, Millery M, et al. An information systems model of the determinants of electronic health record use. Appl Clin Inform. 2013;4:185–200. doi: 10.4338/ACI-2013-01-RA-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DesRoches CM, Audet AM, Painter M, Donelan K. Meeting meaningful use criteria and managing patient populations: a national survey of practicing physicians. Ann Intern Med. 2013;158:791–9. doi: 10.7326/0003-4819-158-11-201306040-00003. [DOI] [PubMed] [Google Scholar]
- 17.Jamieson S. Likert scales: how to (ab)use them. Med Educ. 2004;38(12):1217–8. doi: 10.1111/j.1365-2929.2004.02012.x. [DOI] [PubMed] [Google Scholar]
- 18.SAS Institute. SAS Software version 9.2 Cary, NC: SAS Institute Inc; 2002–2008.
- 19.Hsiao CJ, Jha AK, King J, Patel V, Furukawa MF, Mostashari F. Office-based physicians are responding to incentives and assistance by adopting and using electronic health records. Health Aff (Millwood) 2013;32:1470–7. doi: 10.1377/hlthaff.2013.0323. [DOI] [PubMed] [Google Scholar]
- 20.Heisey-Grove D, Danehy LN, Consolazio M, Lynch K, Mostashari F. A national study of challenges to electronic health record adoption and meaningful use. Med Care. 2014;52(2):144–8. doi: 10.1097/MLR.0000000000000038. [DOI] [PubMed] [Google Scholar]
- 21.Government Health IT. EHR Makers Surprised by Stage 2 Complexity. Available at: http://www.govhealthit.com/news/vendors-struggle-mu-stage-2-EHR-ONC. Accessed 18 April 2014.
- 22.Friedberg MW, Chen PG, Van Busum KR, et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. 2013; RR-439-AMA. Available at http://www.rand.org/pubs/research_reports/RR439.html. Accessed 18 April 2014. [PMC free article] [PubMed]
- 23.Hsiao CJ, Decker SL, Hing E, Sisk JE. Most physicians were eligible for federal incentives in 2011, but few had EHR systems that met meaningful-use criteria. Health Aff (Millwood) 2012;31:1100–7. doi: 10.1377/hlthaff.2011.1315. [DOI] [PubMed] [Google Scholar]
- 24.Gold M, Hossain M, Charles DR, Furukawa MF. Evolving vendor market for HITECH-certified ambulatory EHR products. Am J Manage Care. 2013;19(11 Spec No. 10):SP353–61. [PubMed]
- 25.Ryan AM, Bishop TF, Shih S, Casalino LP. Small physician practices in New York needed sustained help to realize gains in quality from use of electronic health records. Health Aff (Millwood) 2012;32:53–62. doi: 10.1377/hlthaff.2012.0742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hysong SJ, Best RG, Pugh JA. Clinical practice guideline implementation strategy patterns in Veterans Affairs primary care clinics. Health Serv Res. 2007;42:84–103. doi: 10.1111/j.1475-6773.2006.00610.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen C, Garrido T, Chock D, Okawa G, Liang L. The Kaiser Permanente electronic health record: transforming and streamlining modalities of care. Health Aff (Millwood) 2009;28:323–33. doi: 10.1377/hlthaff.28.2.323. [DOI] [PubMed] [Google Scholar]
- 28.Gao J, Moran E, Almenoff PL, Render ML, Campbell J, Jha AK. Variations in efficiency and the relationship to quality of care in the Veterans Health System. Health Aff (Millwood) 2011;30:655–63. doi: 10.1377/hlthaff.2010.0435. [DOI] [PubMed] [Google Scholar]
- 29.Lee TH, Bothe A, Steele GD. How Geisinger structures its physicians’ compensation to support improvements in quality, efficiency, and volume. Health Aff. 2012;31:2068–73. doi: 10.1377/hlthaff.2011.0940. [DOI] [PubMed] [Google Scholar]
- 30.Fleming NS, Culler SD, McCorkle R, Becker ER, Ballard DJ. The financial and nonfinancial costs of implementing electronic health records in primary care practices. Health Aff (Millwood) 2011;30:481–9. doi: 10.1377/hlthaff.2010.0768. [DOI] [PubMed] [Google Scholar]
- 31.Office of the National Coordinator. Meaningful Use Stage 2. Available at: http://www.healthit.gov/policy-researchers-implementers/meaningful-use-stage-2. Accessed 18 April 2014.
- 32.El-Kareh R, Gandhi TK, Poon EG, et al. Trends in primary care clinician perceptions of a new electronic health record. J Gen Intern Med. 2009;24:464–8. doi: 10.1007/s11606-009-0906-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kanzaria HK, Brook RH. The silent physician. J Gen Intern Med. 2013;28:1389–91. doi: 10.1007/s11606-013-2525-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 342 kb)