Abstract
Reduction in the risk of abdominal dehiscence with application of interrupted method of laparotomy closure and comparison with risk of burst with continuous method of closure. Three hundred forty eight patients undergoing laparotomy (114–elective gynecology, 114–emergency gynecology, 120–emergency surgery) were randomized into three arms to undergo closure with continuous, interrupted-X, and Modified Smead-Jones suturing techniques. Burst abdomen occurring up to 4 weeks of operation. Twenty-nine (8.33 %) of 348 patients developed burst in the post-operative period. 19 (15.70 %) of 121 patients in continuous arm developed burst. Five of 110 (4.55 %) patients in Interrupted-X arm and 5 of 117 (4.27 %) patients in Modified Smead-Jones arm developed burst. Interrupted suturing was associated with significant reduction in risk of burst when compared with continuous closure. Important predictors of burst were Intraperitoneal sepsis, cough, uremia, and surgical site infection.
Keywords: Abdominal wound dehiscence, Burst abdomen, Interrupted X suture, Randomized trial, Emergency laparatomy, Gynecological surgery, Prof Hughes’ far & near suture
Introduction
There is a debate about the best method of closure of midline vertical abdominal wound following an emergency laparotomy. This debate has gained importance because one common complication of emergency laparotomy in Asia is burst abdomen or abdominal wound dehiscence, which is associated with high morbidity, mortality, and cost of care. There have been a number of studies evaluating various closure techniques [1] and suture materials. Studies carried out in the West have found no significant difference in the risk of burst between continuous and interrupted methods [2]. The choice of method of closure may not be very crucial in patients undergoing elective laparotomy with adequate nutritional status and no other risk factor for burst, but in developing countries such as Nepal, most patients present with one or more risk factors such as prolonged intraperitoneal sepsis and malnutrition. Hence, it is imperative for us to ascertain the safest method of closing the abdomen.
The present randomized clinical trial was launched to compare the risk of burst with continuous suturing method to that of two types of interrupted suturing at the Departments of Surgery and Gynecology at B. P. Koirala Institute of Health Sciences Hospital, Nepal.
The aim of the study was the following:
To apply (a) continuous suturing, (b) interrupted X-suturing, and (c) interrupted far-and-near suturing (Prof. Hughes double far-and-near method) for closure of midline laparotomy
To measure the risk of abdominal wound dehiscence for the above techniques
To calculate the relative risk of burst between continuous and interrupted methods
Methodology
Study Design
Double-blinded (the patient and the surgeon evaluating the outcome were blinded about the method of suturing) three-arm randomized controlled trial.
The study was undertaken at the Department of Surgery and Department of Obstetrics and Gynecology at B. P. Koirala Institute of Health Sciences (BPKIHS), Dharan, a tertiary care teaching hospital in Eastern Nepal. The trial was approved by the ethics committee of the BPKIHS.
Trial on General Surgical Patients
One hundred and twenty patients undergoing emergency laparotomy for acute abdominal conditions, namely, intestinal obstruction, peritonitis, and abdominal trauma, were included after signing an informed consent.
Patients having a previous laparotomy or burst abdomen or incisional hernia at presentation were excluded.
They were randomized to undergo continuous, interrupted X or interrupted far-and-near suturing techniques. The randomization was performed using codes obtained from www.randomization.com using permuted block design with a block size of six and allocation ratio of 1:1:1. The codes were kept in sealed numbered envelopes which were opened once the patient was deemed suitable for inclusion in the study and consent had been signed.
Suturing Techniques
Continuous Closure
It was performed using No. 1 Prolene suture (polypropylene, Johnson & Johnson Ltd., India), care being taken to place each bite 1.5–2 cm from the cut edge of linea alba and successive bites being taken 1 cm from each other. The edges of linea alba were gently approximated without strangulation with an attempt to keep a suture to wound length ratio of 4:1. The closure was performed by a consultant or a senior resident.
Interrupted Double-X Closure [1]
It was performed using No. 1 Prolene suture. A large bite was taken on the cut edge of linea alba from outside-in, 2 cm from edge. The needle emerged on the other side from inside-out diagonally 2 cm from the edge and 4 cm above or below the first bite. This strand was crossed or looped around the free end of suture and continued outside-in, diagonally at 90◦ to the first diagonal. The two ends were tied just tight enough to approximate the edges of linea alba taking care not to include bowel or greater omentum between the edges. The small free end of the suture was passed deep to the X behind linea alba and again tied to the other end of the suture. This method of tying four throws in front and four throws behind the X created two X-like crosses—one on the surface and another deep to linea alba. The central knot allowed fixation of four arms of the X like a pivot. The next X-suture was placed 1 cm away (above or below) from the previous one. Thus, in a 14 cm long wound, 3 X-sutures were applied (Fig. 1). The suture line was then palpated for any gap with the index finger. Any large gap permitting a finger was closed with a simple interrupted suture (see suturing technique on http://www.youtube.com/watch?v=_tZDd9DYBnw; http://www.youtube.com/watch?v=saevPuwMPcQ).
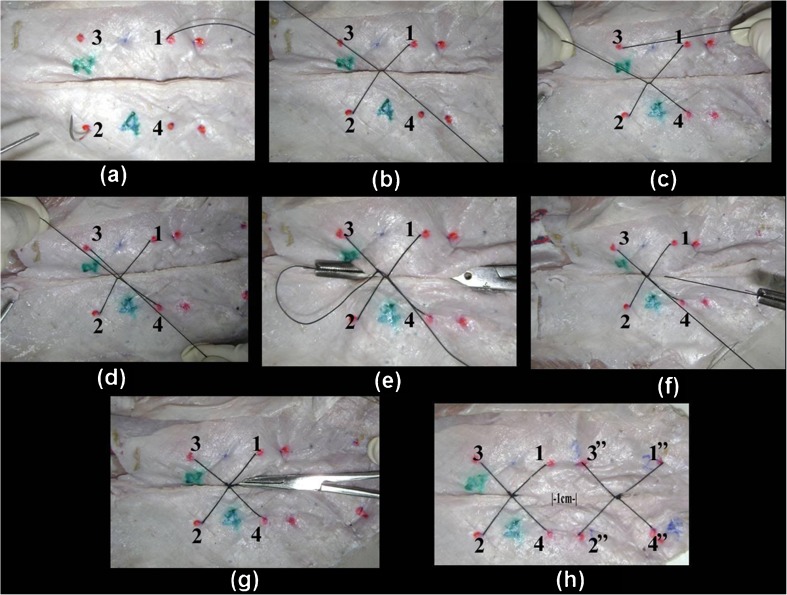
Fig. 1.
Interrupted X-suture. a A bite is taken at (1)—a point 2 cm from cut edge. The needle emerges at (2) another point 2 cm from cut edge, 4 cm cranial or caudal to (1). b The two ends of suture strand crossed. c The needle enters at (4) and comes out at (3). Point (3) is 4 cm away from (1) and 2 cm from cut edge. Point (4) is 4 cm away from (2) and 2 cm from cut edge. d The two ends of suture being tied in front of linea alba. e The small free end of suture pulled inside with an artery forceps or right angle forceps. f The small free end of suture tied with long strand of suture. g Knot being buried behind linea alba to prevent sinus formation. h Two interrupted X-sutures applied, 1 cm apart
Prof. Hughes Far-and-Near Interrupted Method [3]
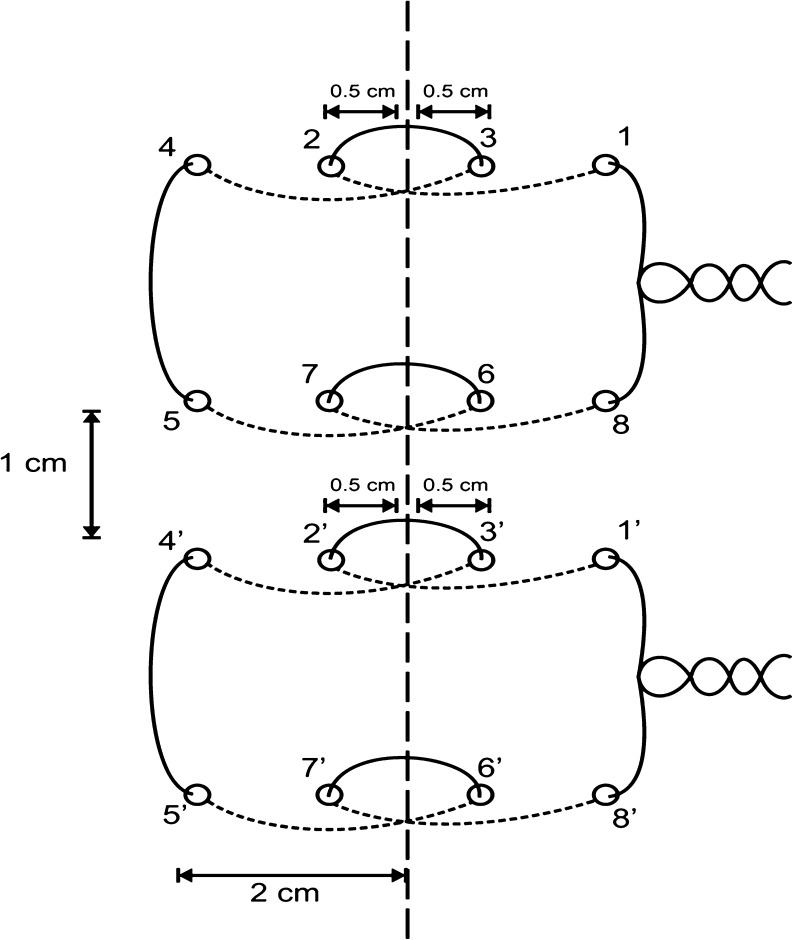
The patients in the third arm were treated by Professor Hughes modification of Smead-Jones far-and-near stitch. This comprised a far bite starting at 2 cm on the edge of linea from outside-in and then taking a near bite of 0.5 cm on the other side inside-out—a near bite on the same side outside-in and then a far bite on the other side inside-out. The suture was next converted to a horizontal mattress by taking a far bite 1 cm above or below the previous bite on the other side—near bite on the same side, near bite on the other side, and finally a far bite on the same side. The two ends of the suture were tied to approximate the edges of the linea alba (Fig. 2).
Fig. 2.
Far-and-near double horizontal mattress suture developed by Prof. L. E. Hughes at Cardiff [3]
Trial on Gynecological or Obstetric Patients
A similar trial was carried out in the Department of Obstetrics and Gynecology at BPKIHS on 228 (114 in elective and 114 in emergency surgeries) patients.
Inclusion Criteria
All patients scheduled to undergo a midline laparotomy for emergency or elective reasons such as cesarian section, ruptured ectopic pregnancy, total abdominal hysterectomy and bilateral salpingo-oophorectomy, ovariotomy, and myomectomy.
All patients giving written informed consent for enrollment in the study.
Exclusion Criteria
Patients younger than 18 years.
Patients who had undergone a previous laparotomy for any condition (or had an incisional hernia or burst abdomen at presentation).
The recruitment, randomization, and suturing techniques were similar to those of general surgical patients.
Measurement of Variables
The main outcome variable was presence of an abdominal wound dehiscence or burst. This was recorded as a binary variable—present/absent. A burst was considered present when intestine, omentum, or other viscera were seen in the abdominal wound up to 30 days from the date of operation. A consultant surgeon ascertained the occurrence of burst.
The following predictor variables were recorded:
Intra-peritoneal sepsis—coded as a binary variable, present/absent.
Coughing—present/absent.
Diabetes—coded as present/absent. Its presence was defined as fasting blood sugar >140 mg/dl or random blood sugar >200 mg/dl.
Abdominal distension—coded as a binary variable, present/absent.
Intra-abdominal malignancy—coded as binary variable, present/absent. If present the histological type of tumor was recorded.
Malnutrition—coded as binary variable, present/absent. Its presence was defined as weight <70 % of expected weight or serum albumin <3 g/dl.
Anemia—coded as binary variable, present/absent. Its presence was defined as hemoglobin less than 10 g/dl.
Steroid intake—coded as a binary variable, present/absent. If present, dose and duration of treatment was noted.
Hypoxia—coded as binary variable, present/absent. Its presence was defined as PaO2 less than 60 mmHg as recorded by an arterial blood gas at time of surgery or saturation less than 90 % on pulse oximetry immediately preoperatively on room air.
Uremia—coded as a binary variable, present or absent. Its presence was defined as blood urea greater than 50 mg/dl.
Jaundice—coded as a binary variable, present or absent. Its presence was defined as serum bilirubin greater than 2 mg/dl.
Method of suturing—coded as 0 for continuous; 1 for interrupted X method and 2 for Prof Hughes far-and-near method.
Statistical Analysis
The following statistical analyses were carried out:
Risk of burst: The risk (cumulative incidence) of burst was calculated as the number of burst abdomen patients in a group/total number of patients in that group. The point estimate and 95 % confidence intervals were calculated using STATA 10 software package (STATA Corporation, Texas). Fisher’s exact test or Mantel-Haenszel chi-square test was used for hypothesis testing. Two-tailed P values were used with α or type one error set at 0.05.
Relative risk of burst abdomen: The risk of dehiscence was similar with the two types of interrupted sutures (X and Prof Hughes far and near). Hence, the data of these groups were added together and named “interrupted suture” group. The relative risk of this interrupted group as the “exposure” was calculated against the continuous method as the “reference” category.
The data from both the above trials in surgery and gynecology were collated. The combined results are presented below.
Results
The trial recruited 348 patients.
Age Distribution
The mean age of the patients was 36.09 years (SD = 13.85) with a median of 32 years. The age ranged from 15 to 82 years.
Gender Distribution
There were 82 (23.56 %) males and 266 (76.44 %) females enrolled in the study.
Risk of Burst
Out of 348 patients, 29 (8.33 %) developed burst in the postoperative period.
Stratified analysis was performed for the significant predictors to better understand the efficacy of the three methods under different conditions.
Method of Suturing
Out of 348, 121 patients were randomized under the continuous method, 110 (32.43 %) under Interrupted X-suturing method, and 117 (34.23 %) under Prof Hughes far-and-near method. It was seen that 19 (15.70 %) of 121 patients in the continuous arm developed burst, while 5 (4.55 %) of 110 patients in the interrupted X arm developed burst and 5 (4.27 %) of 117 patients in the Prof Hughes far and near arm developed burst (P = 0.001) (Table 1).
Table 1.
Comparison of baseline characteristics among the three groups
| Characteristic | Continuous method N = 121 | Interrupted-X suture N = 110 | Prof Hughes’ suture N = 117 |
|---|---|---|---|
| Age (std. deviation) | 37.05 (14.10) | 36.46 (14.79) | 34.72 (12.64) |
| Gender (male/female) | 28/93 | 21/89 | 33/84 |
| Emergency/elective surgery | 83/38 | 72/38 | 79/38 |
| Serum albumin (std. dev.) | 3.0 (0.58) | 3.15 (0.56) | 3.15 (0.60) |
| BMI (std. dev.) | 22.45 (3.96) | 22.80 (4.18) | 21.57 (3.34) |
| Intra-peritoneal sepsis (%) | 33 (27.27) | 28 (25.45) | 39 (33.33) |
| Cough (%) | 9 (7.44) | 5 (4.55) | 3 (2.56) |
| Diabetes (%) | 3 (2.48) | 3 (2.73) | 3 (2.56) |
| Intra-abdominal malignancy (%) | 6 (4.96) | 4 (3.64) | 7 (5.98) |
| Anemia (%) | 35 (28.93) | 34 (30.91) | 33 (28.21) |
| Steroid intake (%) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Uremia (%) | 16 (13.22) | 9 (8.18) | 10 (8.62) |
| Jaundice (%) | 5 (4.13) | 1 (0.91) | 3 (2.56) |
| Intestinal obstruction (%) | 13 (28.89) | 6 (17.65) | 3 (7.32) |
There was no statistically significant difference in the risk of burst abdomen between interrupted X and Prof Hughes far-and-near techniques. Since these methods are two types of interrupted closure techniques, they were grouped under “interrupted method” for relative risk (RR) calculation as given below.
RR for burst abdomen with continuous method as “reference” category and interrupted method as “exposure” category was 0.280 (95 % CI 0.135–0.584; P = 0.0003). The prevented fraction was 71.94 % (95 % CI 41.59–86.52 %) (Table 2 and 3).
Table 2.
Showing relationship between methods of suturing and burst abdomen
| Burst abdomen | Method of suturing n (%) | Total | ||
|---|---|---|---|---|
| Continuous | Interrupted-X | Prof Hughes’ suture | ||
| Yes | 19 | 5 | 5 | 29 |
| (15.70) | (4.55) | (4.27) | (8.33) | |
| No | 102 | 105 | 112 | 319 |
| (84.30) | (94.45) | (95.73) | (91.67) | |
| Total | 121 | 110 | 117 | 348 |
| (100.00) | (100.00) | (100.00) | (100.00) | |
Pearson chi2(2) = 13.1924, Pr = 0.001
Table 3.
Showing relative risk of burst abdomen with continuous suturing as reference and interrupted suturing as exposure category
| Burst abdomen | Method of suturing | Total | |
|---|---|---|---|
| Interrupted suture | Continuous suture | ||
| Yes | 10 | 19 | 29 |
| No | 217 | 102 | 319 |
| Total | 227 | 121 | 348 |
| Risk of burst | 0.044 | 0.157 | 0.083 |
2-sided Fisher’s exact P = 0.0008
Relative risk of burst, Point estimate = 0.28, 95 % C.I.: 0.13 to 0.58
Prevented fraction for burst, Point estimate = 71.9 %, 95 % C.I.: 41.59 % to 86.52 %
This prevented fraction indicates that 71 % of bursts were prevented by application of interrupted suture that would have occurred if abdomen was sutured with a continuous suture.
Intraperitoneal Sepsis and Burst Abdomen
Intraperitoneal sepsis was present in 100 (28.73 %) cases. Seventeen (17 %) of these developed burst abdomen. On the other hand, out of the remaining 248 (71.21 %) cases where no contamination of the peritoneal cavity was observed, only 12 (4.84 %) of these developed burst. RRsepsis for burst = 3.51 (95 % CI 1.74–7.08; P = 0.0005).
Cough and Burst Abdomen
Presence of cough at the time of presentation was analyzed as a predictor in the outcome of burst abdomen. Out of 17 (4.88 %) cases who presented with cough preoperatively, 5 (29.41 %) went on to develop burst abdomen. Of those, not having preoperative cough, 24 (7.25 %) developed burst. RRcough = 4.05; 95 % CI 1.76–9.31; two-sided Fisher’s exact P = 0.0086. Evidence of chest infection was present in all these cases clinically as well as radiologically.
Diabetes and Burst Abdomen
Nine of the 348 patients included in the study were known diabetics. One (11.11 %) of these developed burst in the postoperative period. Of those not having diabetes, 28 (8.26 %) developed burst. RRdiabetes = 1.34; 95 % CI 0.20–8.83; two-sided Fisher’s exact P = 0.547.
Uremia and Burst Abdomen
Uremia was documented in 35 (10.05 %) cases preoperatively. Burst abdomen was seen in 13 (37.14) cases. RRuremia = 7.72 (95 % CI 4.01–14.87; P = 0.000). Presence of uremia was a highly significant factor in predicting wound dehiscence.
Jaundice and Burst Abdomen
Jaundice was present in 9 (2.58 %) cases but was not significant in the occurrence of burst abdomen. RRjaundice = 1.34; 95 % CI 0.20–8.83; two-sided Fisher’s exact P = 0.547.
Anemia and Intra-Abdominal Malignancy
Burst occurred in 10 (9.80 %) of 102 patients with anemia. Nineteen (7.72 %) of 246 patients without anemia had burst. Thus, anemia was not a detrimental factor (RRanemia = 1.27; 95 % C.I 0.61–2.63; two-sided Fisher’s exact P = 0.527) in the development of burst abdomen.
Presence of intra-abdominal malignancy in 17 (4.88 %) of 348 patients was also not associated with burst postoperatively (two-sided Fisher’s exact P = 0.379).
Surgical Site Infection and Burst Abdomen
Surgical site infection (SSI) was present in 57 (16.38 %) of 348 patients. Of these, 21 (36.84 %) developed burst in the postoperative period. Of those not having surgical site infection, 8 (2.75 %) developed burst abdomen postoperatively. RRSSI = 13.40 (95 % CI 6.25–28.75; P = 0.000). Thus, surgical site infection was a highly significant predictor of wound dehiscence.
Condition of the Linea Alba and Burst Abdomen
Per-operatively, the condition of linea alba was inspected and documented as healthy looking or necrotic. In 5 (1.43 %) cases, necrotic linea alba was encountered in which 4 (80.00 %) cases developed burst. RRnecrosis = 10.98 (95 % CI 6.15–19.57; two-sided Fisher’s exact P = 0.0002). Hence, linea alba necrosis was also significant in predicting the wound dehiscence.
Type of Surgery and Burst Abdomen
Inquest was made into the risk of burst abdomen among the elective and emergency surgical procedures using different suturing techniques.
Out of the total 114 elective operations performed, 3 (2.63 %) patients developed burst postoperatively.
Emergency Operations
Of the 234 emergency surgeries, 26 (11.11 %) patients developed burst.
The risk of burst in continuous arm was 19.28 % (16/83) as opposed to 6.94 % (5/67) in interrupted X arm and 6.33 % (5/74) in modified Smead-Jones arm.
Elective Operations
The risk of burst in continuous arm was 7.89 % (3/38). No bursts were reported in interrupted X or modified Smead-Jones arms.
Discussion
Abdominal wound dehiscence or burst abdomen remains a major cause of morbidity and mortality following laparotomy especially in the emergency setting.
Trials from Western countries have shown no significant difference in the risk of burst in the interrupted versus continuous methods of suturing [2].
In our trial, a statistically significant difference in the risk of burst was obtained between the continuous and interrupted arms. However, there was no significant difference in the risk of burst between the two types of interrupted methods, namely interrupted X and Prof Hughes far-and-near suture. In presence of certain factors (e.g., intraperitoneal sepsis, cough, uremia, and wound infection), the risk of burst increases manifold. It is in these cases that we need to apply the suturing method most effective in preventing burst. The occurrence of burst increases risk of chest infection due to inability to generate positive intra-abdominal pressure and expectorate the secretions. It also increases wound pain, duration of hospital stay, and cost of care due to need for re-suturing under general anesthesia and resources.
The patients following burst may require ventilatory support.
Conclusions
Intraperitoneal sepsis, cough, uremia, wound infection, and necrosis of linea alba are significant predictors of burst.
In presence of these symptoms, the risk of abdominal wound dehiscence can be reduced to less than one-third by using interrupted sutures.
Continuous closure gives good results in elective setting.
Jaundice, anemia, malnutrition, and intra-abdominal malignancy do not increase the risk of burst.
Acknowledgments
Recommendation
Interrupted suture techniques (Interrupted X or Prof. Hughes’ method) should be used in all emergency laparotomy cases and in elective laparotomy cases presenting with one or more risk factors for burst.
Limitations of study
We have not carried out long-term follow-up, and hence the risk of incisional hernia could not be calculated.
Footnotes
Source of Support: Nil
Contributor Information
Arpit Rao, Email: arpit.aiims@gmail.com.
Anurag Srivastava, Phone: +91-11-26594560, FAX: +91-11-26588663, Email: dr.anuragsrivastava@gmail.com.
References
- 1.Srivastava A, Roy S, Sahay KB, Seenu V, Kumar A, Chumber S, Bal S, Mehta SN. Prevention of burst abdominal wound by a new technique: a randomized trial comparing continuous versus interrupted X-suture. Ind J Surg. 2004;66(1):19–27. [Google Scholar]
- 2.Van’t Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J. Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg. 2002;89(11):1350–1356. doi: 10.1046/j.1365-2168.2002.02258.x. [DOI] [PubMed] [Google Scholar]
- 3.Hughes LE. Incisional hernia. Asian J Surg. 1990;13(2):69. [Google Scholar]