Abstract
Digital radiography (DR) technologies have the advantage of a wide dynamic range compared to their film-screen predecessors, however, this poses a potential for increased patient exposure if left unchecked. Manufacturers have developed the exposure index (EI) to counter this, which provides radiographers with feedback on the exposure reaching the detector. As these EIs were manufacturer-specific, a wide variety of EIs existed. To offset this, the international standardised EI has been developed by the International Electrotechnical Commission (IEC) and the American Association of Physicists in Medicine (AAPM). The purpose of this article is to explore the current literature relating to EIs, beginning with the historical development of the EI, the development of the standardised EI and an exploration of common themes and studies as evidenced in the research literature. It is anticipated that this review will provide radiographers with a useful guide to understanding EIs, their application in clinical practice, limitations and suggestions for further research.
Keywords: Deviation index, digital radiography, exposure index, image quality, radiography
Introduction
In medical imaging, radiography is the most frequently performed type of examination.1,2 Digital radiography (DR), which includes direct DR and computed radiography (CR) technologies,3 is now considered the accepted technology in most departments.4 Due to the wide exposure latitude and post processing capabilities associated with DR,5 resultant images will have similar appearances in terms of contrast and density when compared to film-screen technologies independent of the exposure, however, if images are underexposed increased quantum mottle will be evident in the image.6 DR technologies have been described as having the potential to reduce patient radiation dose,7,8 however, due to their large dynamic range inadvertent overexposure is possible,9 since underexposure rather than overexposure is more likely to affect image quality.10,11 Dose creep or dose drift are terms used to describe unintended overexposure to the patient,11 following the introduction of digital imaging technologies.12 This increase is driven, at least in part by a desire to reduce quantum mottle as radiologists tend to express concern about underexposed images.13,14 However, there is often less focus on overexposed images, unless saturation occurs.13 The literature supports this concept of overexposure to avoid noisy images14 and suggests that average exposures have a tendency to creep up over time if a clear exposure indicator is not provided and monitored routinely.13 This exposure indicator comes in the form of the exposure index (EI).
EIs were first developed for CR system technologies by Fujifilm with the introduction of the sensitivity ‘S’ number.13 The difference between the wide latitude of CR systems and the narrow exposure range emerging from the radiographic projection was the motivation to develop EIs, to estimate the detector exposure, to enable gain modification for the harvesting of the latent image and later to provide estimates to re-scale the digitised data in cassette-based systems.13 Since that time the EI has been further developed by DR manufacturers as a method of providing feedback to the radiographer on detector exposure.15 The EI is proportional to the signal to noise ratio squared (SNR2) and can be related to image quality.15 The EI, therefore, provides the radiographer with feedback as to the adequacy of each exposure, in the way that film density did with conventional radiography.15 The EI can be defined as a measure of a digital detector's response to radiation in the relevant image region (RIR) of an image acquired using DR.16
The wide variety of manufacturer-dependent EIs that were available, presented the opportunity for user confusion.13,15 These EIs were entirely manufacturer-specific and varied greatly in terminology, mathematical forms and calibration conditions.13 This can be seen in Figure 1 where, for example, the Carestream Health EI number has a logarithmic relationship to the detector exposure unlike the linear systems used by Philips and Siemens.17 Also some manufacturers offer a system whereby increasing EI values indicate increasing dose whereas for other manufacturer systems, the reverse is evident.18 This inconsistency between vendors was seen as a deterrent to effective EI implementation,13 and confusion was evident among professionals who experienced more than one vendor-specific system.13,18
Figure 1.
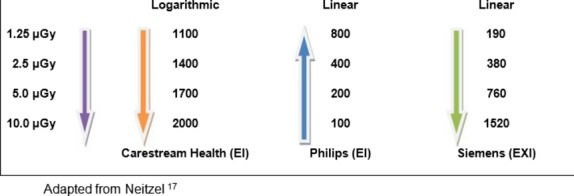
Sample of exposure index scales prior to exposure index standardisation.
To counter these inconsistencies an international standardised EI has been developed by the International Electrotechnical Commission (IEC),16 the American Association of Physicists in Medicine (AAPM)13 and internationally renowned diagnostic physicists in conjunction with DR system manufacturers.15 This new standardised EI is designed to present a linear relationship between the detector exposure and the index value.11,15 The details of the standardised EI will be considered further in the review.
Materials and Methods
Searches of the following databases were performed: Scopus, ScienceDirect, Proquest Central, Web of Knowledge and AIP Scitation. Multiple combinations of the following key words were searched: Exposure indicator; exposure index, deviation index, standardised exposure index, target exposure index (and/or) radiography, digital radiography, computed radiography, radiation dose, image quality, detector exposure.
Only full text journal articles published in English between 2008 and present day were included, with the exception of key historical papers relating to the topic.
IEC and AAPM Task Group 116 Solutions
The previously discussed EI options demonstrated the variability and potential for confusion that existed with manufacturer-dependent solutions. The IEC16 and the AAPM13 independently developed standardised terminology for EI.1 The standardised EI should be consistent between manufacturers and reflect the radiation incident on the detector and is based upon image noise levels.13 It is important to note that the EI does not reflect the radiation dose to the patient.13,15
In addition to a greater understanding and subsequent usage of EIs, the benefits of a standardised EI include the ability to monitor differences in exposures between digital systems in an institution, to compare techniques used between institutions and to estimate the quality of images produced using a particular system.13 The IEC indicates that care should be taken when comparing EI values from different imaging devices or for images acquired with different technique factors.16 The EI is heavily dependent on the RIR and the selection of RIR may differ between imaging systems.15,16 Values of interest (VOI) may be computed using the mean, median or mode, thus leading to differing VOIs, which could result in the same EIs being reported by different systems, with the actual exposure to the detector being very different.16 Also large variations in EI values may not necessarily indicate large differences in dose to the detectors of different systems.16 Further limitations of the EI are as a result of the response of differing systems to X-rays of different energies and differing angles of incidence.16 In addition to the standardised EI the deviation index (DI) has also been developed to serve as an indication of exposure appropriateness.13 The DI can be defined as presenting numerically the difference from the desired target EI and actual EI.16 The target EI is set for each examination type and may vary depending on the body part being examined and equipment used.11 Variations in the new standards are noted between the IEC and AAPM; the AAPM EI is reported in terms of microgray and reports the DI with one decimal of precision, whereas the IEC EI is reported without an assigned unit and multiplies the AAPM value by 100, also the IEC reports the DI with no specification of precision19 The calculation of DI based on a logarithmic scale of base 10 was deemed the most appropriate by the AAPM task group (TG) 116, as this provides appropriate information in terms of direction and magnitude.13 For example +1 is approximately 125% of the recommended exposure and −1 is 80% of the recommended exposure, therefore, requiring either −1 or +1 alteration in mAs or density steps on a properly calibrated DR system respectively.13 A DI value of 0.0 indicates that the appropriate exposure has been achieved.13,15 All this, however, relies on the availability of target values that have been established by users, vendors or professional societies and have taken into consideration the examination type, technique factors, filtration and the type of receptor used.20
The AAPM TG 116 also cautions against accepting an appropriate DI as evidence of optimal imaging, as poor collimation or the presence of prosthesis or gonad shielding may raise or lower the DI.13 It is essential, therefore, that good clinical practice should be assessed and monitored independently of DIs, such as evaluating image noise content rather than relying solely on the DI value to determine optimum practice.13 The complementary nature of EIs when establishing optimum practice has been emphasised.
The DI proposed by AAPM TG 116 has the potential for being an effective quality assurance (QA) tool. In particular, DI values belonging to rejected and repeated images along with exposure factors and selected projections should be stored on the system.13 Software should be made available to analyse these data so that for example, potential problems with particular examinations, issues with technology and specific educational and training requirements for radiographic personnel can be identified.13 By appropriate utilisation of EIs and DIs, inappropriate radiation levels will be automatically highlighted to the radiographer and corrective strategies can be employed as described by the AAPM.13 Radiographers should become familiar with the new standardised EIs in order to optimally use the new DR equipment.19 The Medical Imaging and Technology Alliance (MITA) issued a statement supporting the adoption of the IEC standardised EI in 2011.21
Common Themes
Common themes have appeared throughout the literature in relation to the EI such as image quality, exposure, radiographer education and optimisation of technique. These themes appear to be intrinsically linked.
With the widespread adoption of the standardised EI, it is anticipated that the confusion which existed as a result of proprietary terminology will be reduced.1 The new standardised EI has the potential to improve radiographer performance in terms of optimising technique.15 The Image Gently Campaign Back to Basics Initiative advocates measuring body part thickness; as this is the most important factor in determining correct technique,1 by virtue that X-ray absorption and transmission are dependent on body part thickness and composition.1 Although this article is based on the imaging of paediatric patients, many of the suggestions therein are also relevant to the imaging of adults. For example Mothiram et al. highlighted gender variation in terms of EI when imaging adults, with female patient radiographs recording significantly higher median EI values than males in a number of instances.22 Mothiram et al. have indicated that data on patient size and body part thickness could have provided useful information relating to the EI gender variations demonstrated in their study, as men and women have variations in tissue distribution,22 this would appear to validate a back to basics approach in terms of imaging adults utilising DR.
This point is further emphasised in the literature where it is indicated that the basics of radiographic practice are every bit as important today as they were previously.9 Radiographers knowledge of the attenuation processes and exposure factors when using DR technologies has been questioned, with the influence of these technical factors being eroded through post processing when using DR.23 This appears to imply that radiographers are gradually deskilling due to their dependence on the ability of DR to correct for exposure factor errors. A new paradigm of thinking in relation to how images are acquired, processed, stored and evaluated in DR is required.3
The standardised EI increases in a linear fashion when mAs increases, however, its response to alterations in kVp is not linear.24 The development of exposure charts based on patient size has been described as a method of preventing exposure creep along with the implementation of policies and procedures in accordance with ‘as low as reasonable achievable’ (ALARA) in order to vary protocols dependent on patient height and/or weight, lateral width and body mass index (BMI).14
To ensure the exposure of extraneous body parts is avoided the use of proper collimation to include only the body part to be examined has been reinforced.1,9 Changes in collimation and field size can alter the EI considerably and other factors that can affect the EI include the size of the detector, metal implants and gonadal shielding.18 The importance of monitoring EI and DI values when optimising radiation dose and ensuring correct use of equipment has been outlined.15 Don et al. suggest the monitoring of the appropriateness of technique based on the DI in association with noise levels present in images in order to avoid exposure creep.1 The use of EI to monitor the appropriateness of technique and exposure factor selection has also been discussed.25
The technical advances associated with DR have been described as having created challenges, which require the re-education of the workforce in order to prevent unnecessary radiation exposures.9 Martin and Sutton espouse that it is radiologists' and radiographers' professional responsibility to ensure that they are aware of the capabilities of their equipment and utilise the options available to them to achieve optimisation in terms of image quality and radiation dose.26 The use of digital technologies requires users to be up to date with their scientific knowledge concerning their use in radiography.27 This balance between radiation dose and image quality is ultimately affected by decisions made by the radiographer performing the examination,28 as the quantity of radiation used to acquire the image is based solely on the discretion of the radiographer.29 Radiographer education, in relation to CR and how the EI is related to patient dose, has been described as essential in assisting the radiography community in playing a vital role in dose reduction.30 When using DR, radiographers must be more aware of exposure factor selection and its effects on patient radiation exposures.31 Radiographer continuing education has been described as very important, as patient positioning, technique selection and collimation are all performed by the radiographer.2 Monitoring EIs and analysing the percentage over and under the recommended range can be used as a tool to educate radiographers, while also improving imaging quality in a department.1
Studies on EI
The studies reviewed for the purposes of this literature review have used phantoms and actual exposures and vary in terms of adult and paediatric radiography. These studies have yielded much useful information and some of the key findings are summarised below.
Manufacturer-recommended EIs may be set too high as images produced at lower EIs have been found to be clinically acceptable.32 Similarly, clinically acceptable images at lower EI levels were obtained in a study to optimise the use of CR in paediatric chest imaging using Agfa CR (here the Agfa EI is the logarithm of median exposure level “lgM”13), where the researchers found that a possible reduction by a factor of 2.5 in mean patient entrance surface dose (ESD) could be achieved in their centre.33 It has been suggested that CR manufacturers reassess their EI value recommendations.34 Additionally, it has been recommended that X-ray personnel optimise EIs (as opposed to accepting manufacturer recommended EIs) as a means to reduce patient dose.32,35 Minimisation of radiation exposures can also be achieved by using an optimised EI as a guideline for different medical imaging tasks, using a three-tier classification of image quality (high, medium and low).36 Here Zhang et al. found that different levels of image quality and thus EI are required for different imaging tasks when performing posterior-anterior chest radiography using DR.36 Cohen et al. indicated that when automatic exposure is used, the standardised EI will have a limited role in the imaging department37
Collimation was found to be an important factor affecting Fuji CR systems S-value in a study using an extremity phantom.38 Poorly collimated images achieved a low S-value, indicating a higher dose; however, the poor collimation resulted in the inclusion of extra areas of air, suggesting overexposure where in fact the images were underexposed.38 Although based on studies using a canine phantom, the results are applicable to human patients.
Possible causes of EI variations have been discussed, with these being based on working hours and patient gender differences. It has been reported that EI variations between examinations taken within hours and out of hours can occur, with higher EIs being recorded in the latter situation.22,32 This may be linked to staffing levels and levels of staff experience,22 with radiographers reluctant to have to repeat an exposure during these busy shifts.22,32 A survey of a cross section of the American Society of Radiologic Technologists (ASRT) members was undertaken to evaluate radiologic technologists' knowledge about image quality and dose management in paediatric DR examinations; they concluded that there is a need for comprehensive practical digital imaging technology education for technologists.3 It has also been found that exposure creep can be halted in the intensive and critical care unit (ICCU), by the effective recording and monitoring of individual patients chest X-ray (CXR) EIs along with radiographic technique factors used.12 Thereby providing the radiographer with a guide to optimal technique factors to use on subsequent CXRs on the same patient.12 Variation in EI values between genders has also been demonstrated with women often obtaining higher values compared to their male counterparts.22,39 The lack of an adequate exposure chart for female patients has been suggested as a possible cause of this gender variation.39 However, information on patient's size and body part thickness has been suggested as potentially providing useful information relating to EI gender variation.22 Zhang et al. established a method to set appropriate exposure parameters (mAs) to achieve a target EI based on a child's height and weight, thus enabling a significant reduction in dose–area product (DAP) and ESD in paediatric radiography.40 A similar approach to the imaging of adult patients could prevent the EI gender bias reported previously. Poletti, advocates the use of the points system in situations where the new DI values require corrections and for the establishment or correction of technique charts, however, the author also indicates that this would be most accurate and of most benefit in paediatric radiology.41
Many authors have published on the topic of dose and EI, Vano et al. used the EI to calculate paediatric entrance surface air kerma (ESAK) in CR42 but did not discuss the impact on EI degradation with CR processing delay, which has been demonstrated in the literature.38,43,44 This is problematic as value discrepancies of 8% occurring within the first hour of delay of CR plate processing have been reported,43 with increasing change occurring with increasing processing delay have been demonstrated.43,44 This would therefore call into question the validity of using the EI as a method to evaluate patient doses with CR. Certainly others have found that no relationship exists between patient radiation dose and EI31 although Butler et al. found that there is a correlation between ESD and EI.35 Interestingly, Silva and Yoshimura found that EI could be used as a dose estimator but that the relationship between EI and dose is dependent upon the projection.45 Cohen et al. found that the standardised EI and DI were excellent tools for monitoring the consistency of patient exposures in a study that was undertaken on neonatal portable chest radiographs.11 However, Butler et al. indicated that EIs can be unreliable with CR but entirely consistent in direct DR and therefore the utility of EI as a feedback mechanism for CR remains uncertain.5
The value of a reject analysis programme in conjunction with an exposure analysis programme in CR has been shown to be an effective QA and staff education tool when performed in association with DR technologies.46 With this in mind a number of studies have shown the usefulness of computer programs designed to extract data including EIs, as manual approaches can be very time consuming.47–49 Currently, new DR systems and software version upgrades for older systems are incorporating the IEC standardised EI.14
Conclusion
The value of the EI as a mechanism to provide feedback to radiographers as to the adequacy of their exposure technique has been highlighted, however, with manufacturer-specific EIs confusion existed. This confusion hindered effective EI implementation. The adoption of the new standardised EI and associated DI should encourage greater understanding and usage of the new EI.
The EI can be used as a QA tool to monitor correct use of equipment and observe variations in detector dose. In doing so caution should be exercised when examining any data generated from such a programme as the EI can be affected by a number of factors such as CR processing delay, collimation, detector size, presence of implants and patient habitus. Results from such QA programmes can be used to optimise exposures and provide radiographer continuing education and training in the use of DR.
Further research in relation to optimising adult technique charts based on patient body part thickness as opposed to gender is required. Careful consideration of time and date of exposure and use of specific types of technology can reveal important optimisation issues that require immediate, responsive and effective corrective action. Lessons can be learnt from each other's experiences, and the publication of such experiences with exposure indices is encouraged.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Don S, MacDougall R, Strauss K, et al. Image gently campaign back to basics initiative: Ten steps to help manage radiation dose in paediatric digital radiography. AJR Am J Roentgenol. 2013;200:W431–6. doi: 10.2214/AJR.12.9895. [DOI] [PubMed] [Google Scholar]
- 2.Tonkopi E, Daniels C, Gale MJ, Schofield SC, Sorhaindo VA, VanLarkin JL. Local diagnostic reference levels for typical radiographic procedures. Can Assoc Radiol J. 2012;63:237–41. doi: 10.1016/j.carj.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Morrison G, John SD, Goske MJ, et al. Pediatric digital radiography education for radiologic technologists: Current state. Pediatr Radiol. 2011;41:602–10. doi: 10.1007/s00247-010-1904-3. [DOI] [PubMed] [Google Scholar]
- 4.Shaefer-Prokop CM, De Boo DW, Uffmann M, Prokop M. DR and CR: Recent advances in technology. Eur J Radiol. 2009;72:194–201. doi: 10.1016/j.ejrad.2009.05.055. [DOI] [PubMed] [Google Scholar]
- 5.Butler ML, Rainford L, Last J, Brennan PC. Are exposure index values consistent in clinical practice? A multi-manufacturer investigation. Radiat Prot Dosimetry. 2010;139:371–4. doi: 10.1093/rpd/ncq094. [DOI] [PubMed] [Google Scholar]
- 6.Prokop M, Neitzel U, Schaefer-Prokop C. Principles of image processing in digital chest radiography. J Thorac Imaging. 2003;18:148–64. doi: 10.1097/00005382-200307000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Schaefer-Prokop C, Neitzel U, Venema HW, Uffmann M, Prokop M. Digital chest radiography: An update on modern technology, dose containment and control of image quality. Eur Radiol. 2008;18:1818–30. doi: 10.1007/s00330-008-0948-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uffmann M, Schaefer-Prokop C. Digital radiography: The balance between image quality and required radiation dose. Eur J Radiol. 2009;72:202–8. doi: 10.1016/j.ejrad.2009.05.060. [DOI] [PubMed] [Google Scholar]
- 9.Moore QT, Don S, Goske MJ, et al. Image gently: Using exposure indicators to improve pediatric digital radiography. Radiol Technol. 2012;84:93–9. [PubMed] [Google Scholar]
- 10.Aichinger H, Dierker J, Joite-Barfuß S, Säbel M. Chapter 9: Image Quality and Dose. In: Aichinger H, Dierker J, Joite-Barfuß S, Säbel M, editors. Radiation Exposure and Image Quality in X-Ray Diagnostic Radiology: Physical Principles and Clinical Applications. 2nd edn. Berlin, Heidelberg: Springer-Verlag; 2012. p. 87. [Google Scholar]
- 11.Cohen MD, Cooper ML, Piersall K, Apgar BK. Quality assurance: Using the exposure index and the deviation index to monitor radiation exposure for portable chest radiographs in neonates. Pediatr Radiol. 2011;41:592–601. doi: 10.1007/s00247-010-1951-9. [DOI] [PubMed] [Google Scholar]
- 12.Gibson DJ, Davidson RA. Exposure creep in computed radiography: A longitudinal study. Acad Radiol. 2012;19:458–62. doi: 10.1016/j.acra.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 13.Shepard SJ, Wang J, Flynn M, et al. An exposure indicator for digital radiography. College Park (MD): American Association of Physicists in Medicine; July 2009; 92 p. Report No: 116.
- 14.Andriole KP, Ruckdeschel TG, Flynn MJ, et al. ACR-AAPM-SIIM practice guidelines for digital radiography. J Digit Imaging. 2013;26:26–37. doi: 10.1007/s10278-012-9523-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seibert JA, Morin RL. The standardized exposure index for digital radiography: An opportunity for optimization of radiation dose to the pediatric population. Pediatr Radiol. 2011;41:573–81. doi: 10.1007/s00247-010-1954-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.International Electrotechnical Commission. Geneva, Switzerland: IEC; 2008. Medical electrical equipment – Exposure index of digital X-ray imaging systems- Part 1: Definitions and requirements for general radiography. International standard 62494-1. [Google Scholar]
- 17.Neitzel U. The Exposure Index and its Standardization 2006 [Internet]. Philips Medical Systems, Hamburg, Germany; Available from: http://www.dimond3.org/Trier_2006/Exposure_Index_Standardization.pdf [Accessed 2013 November 18]
- 18.Goske MJ, Charkot E, Herrmann T, et al. Image gently: Challenges for radiologic technologist when performing digital radiography in children. Pediatr Radiol. 2011;41:611–9. doi: 10.1007/s00247-010-1957-3. [DOI] [PubMed] [Google Scholar]
- 19.Don S, Whiting BR, Rutz LJ, Apgar BK. New exposure indicators for digital radiography simplified for radiologists and technologists. AJR Am J Roentgenol. 2012;199:1337–41. doi: 10.2214/AJR.12.8678. [DOI] [PubMed] [Google Scholar]
- 20.Don S, Goske MJ, John S, Whiting B, Willis CE. Image gently pediatric digital radiography summit: Executive summary. Pediatr Radiol. 2011;41:562–5. doi: 10.1007/s00247-010-1966-2. [DOI] [PubMed] [Google Scholar]
- 21.Vastagh S. Statement by MITA on behalf of the MITA CR-DR group of the X-ray section. Pediatr Radiol. 2011;41:566. doi: 10.1007/s00247-010-1961-7. [DOI] [PubMed] [Google Scholar]
- 22.Mothiram U, Brennan PC, Robinson J, Lewis SJ, Moran B. Retrospective evaluation of exposure index (EI) values from plain radiographs reveals important considerations for quality improvement. J Med Radiat Sci. 2013;60:115–22. doi: 10.1002/jmrs.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Walker S, Allen D, Burnside C, Small L. Determining the between exposure factors, dose and exposure index value in digital radiographic imaging. Synergy. 2011;10:14–7. [Google Scholar]
- 24.Rattan AS, Cohen MD. Removal of comfort pads underneath babies: A method of reducing radiation exposure to neonates. Acad Radiol. 2013;20:1297–300. doi: 10.1016/j.acra.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 25.Talaharla S. Exposure Index. Imaging & Therapy Practice. 2013;2:16–20. [Google Scholar]
- 26.Martin CJ, Sutton DG. Chapter 3: Radiation dose and image quality. In: Hayat MA, editor. Cancer Imaging: Lung and Breast Carcinomas. Vol. 1. London: Elsevier Academic Press; 2008. pp. 45–62. [Google Scholar]
- 27.Lança L, Silva A. Digital radiography detectors – A technical overview: Part 2. Radiography. 2009;15:134–8. [Google Scholar]
- 28.Willis CE. Optimizing digital radiography of children. Eur J Radiol. 2009;72:266–73. doi: 10.1016/j.ejrad.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 29.Johnston J, Comello RJ, Vealé BL, Killion J. Radiation exposure dose trends and radiation dose reduction strategies in medical imaging. J Med Imaging Radiat Sci. 2010;41:137–44. doi: 10.1016/j.jmir.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 30.Davidson R, Sim J. Computed radiography and dosimetry: Some practical tips for dose optimization procedures. J Med Imaging Radiat Sci. 2008;39:109–14. doi: 10.1016/j.jmir.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Fauber TL, Cohen TF, Dempsey MC. High kilovoltage digital exposure techniques and patient dosimetry. Radiol Technol. 2011;82:501–10. [PubMed] [Google Scholar]
- 32.Peters SE, Brennan PC. Digital radiography: Are the manufacturers' settings too high? Optimisation of the Kodak digital radiography system with aid of the computed radiography dose index. Eur Radiol. 2002;12:2381–7. doi: 10.1007/s00330-001-1230-0. [DOI] [PubMed] [Google Scholar]
- 33.Sanchez JacobR, Vano-Galvan E, Vano E, et al. Optimising the use of computed radiography in pediatric chest imaging. J Digit Imaging. 2009;22:104–13. doi: 10.1007/s10278-007-9071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsalafoustas IA, Blastaris GA, Moutsatsos AS, Chios PS, Efstathopoulos EP. Correlation of image quality with exposure index and processing protocol in a computed radiography system. Radiat Prot Dosimetry. 2008;130:162–71. doi: 10.1093/rpd/ncm493. [DOI] [PubMed] [Google Scholar]
- 35.Butler ML, Rainford L, Last J, Brennan PC. Optimization of exposure index values for the antero-posterior pelvis and antero-posterior knee examination. Proc. SPIE 7263, Medical Imaging 2009: Image Perception, Observer Performance, and Technology Assessment, 726302 (12 March 2009); doi: 10.1117/12.810748.
- 36.Zhang M, Zhao B, Wang Y, Chen W, Hou L. Dose optimization for different medical imaging tasks from exposure index, exposure control factor, and mAs in digital radiography. Health Phys. 2012;103:235–40. doi: 10.1097/HP.0b013e31824e71b6. [DOI] [PubMed] [Google Scholar]
- 37.Cohen MD, Markowitz R, Hill J, Huda W, Babyn P, Apgar B. Quality assurance: A comparison study of radiographic exposure for neonatal chest radiographs at 4 academic hospitals. Pediatr Radiol. 2012;42:668–73. doi: 10.1007/s00247-011-2290-1. [DOI] [PubMed] [Google Scholar]
- 38.Baker M. Investigation into factors influencing Fuji S-value using an extremity phantom. J Med Imaging Radiat Sci. 2012;43:34–7. doi: 10.1016/j.jmir.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 39.Lança L, Silva A. Evaluation of exposure index (IgM) in orthopaedic radiography. Radiat Prot Dosimetry. 2008;129:112–8. doi: 10.1093/rpd/ncn143. [DOI] [PubMed] [Google Scholar]
- 40.Zhang M, Liu K, Niu X, Liu X. A method to derive appropriate exposure parameters from target exposure index and patient thickness in pediatric digital radiography. Pediatr Radiol. 2013;43:568–74. doi: 10.1007/s00247-012-2555-3. [DOI] [PubMed] [Google Scholar]
- 41.Poletti J. The HVL in soft tissue and the AAPM and IEC exposure indices. Australas Phys Eng Sci Med. 2011;34:535–43. doi: 10.1007/s13246-011-0100-6. [DOI] [PubMed] [Google Scholar]
- 42.Vano E, Martinez D, Fernandez JM, et al. Paediatric entrance doses from exposure index in computed radiography. Phys Med Biol. 2008;53:3365–80. doi: 10.1088/0031-9155/53/12/020. [DOI] [PubMed] [Google Scholar]
- 43.Kowalczyk N, Comer E. Exposure indicator degradation from CR plate processing delays. Radiol Technol. 2009;80:401–9. [PubMed] [Google Scholar]
- 44.Butler ML, Brennan PC, Last J, Rainford L. The impact of processing delay on the exposure index value. Proc. SPIE 7622, Medical Imaging 2010: Physics of Medical Imaging, 76224X (March 23, 2010); doi: 10.1117/12.843233.
- 45.Silva TR, Yoshimura EM. Patient dose, gray level and exposure index with a computed radiography system. Radiat Phys Chem. 2014;95:271–3. [Google Scholar]
- 46.Jones AK, Polman R, Willis CE, Shepard SJ. One year's results from a server-based system for performing reject analysis and exposure analysis in computed radiography. J Digit Imaging. 2011;24:243–55. doi: 10.1007/s10278-009-9236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Källman H-E, Halsius E, Folkesson M, Larsson Y, Stenström M, Båth M. Automated detection of changes in patient exposure in digital projection radiography using exposure index from DICOM header metadata. Acta Oncol. 2011;50:960–5. doi: 10.3109/0284186X.2011.579622. [DOI] [PubMed] [Google Scholar]
- 48.Ng CKC, Sun Z. Development of an online automatic computed radiography dose data mining program: A preliminary study. Comput Methods Programs Biomed. 2010;97:48–52. doi: 10.1016/j.cmpb.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 49.Källman H-E, Halsius E, Olsson M, Stenström M. DICOM metadata repository for technical information in digital medical images. Acta Oncol. 2009;48:285–8. doi: 10.1080/02841860802258786. [DOI] [PubMed] [Google Scholar]


