Abstract
Introduction
Digital technology has wider exposure latitude and post-processing algorithms which can mask the evidence of underexposure and overexposure. Underexposure produces noisy, grainy images which can impede diagnosis and overexposure results in a greater radiation dose to the patient. These exposure errors can result from inaccurate adjustment of exposure factors in response to changes in patient thickness. This study aims to identify all published radiographic exposure adaptation systems which have been, or are being, used in general radiography and discuss their applicability to digital systems.
Methods
Studies in EMBASE, MEDLINE, CINAHL and SCOPUS were systematically reviewed. Some of the search terms used were exposure adaptation, exposure selection, exposure technique, 25% rule, 15% rule, DuPont™ Bit System and radiography. A manual journal-specific search was also conducted in The Radiographer and Radiologic Technology. Studies were included if they demonstrated a system of altering exposure factors to compensate for variations in patients for general radiography. Studies were excluded if they focused on finding optimal exposures for an ‘average’ patient or focused on the relationship between exposure factors and dose.
Results
The database search uncovered 11 articles and the journal-specific search uncovered 13 articles discussing systems of exposure adaptation. They can be categorised as simple one-step guidelines, comprehensive charts and computer programs.
Conclusion
Only two papers assessed the efficacy of exposure adjustment systems. No literature compares the efficacy of exposure adaptations system for film/screen radiography with digital radiography technology nor is there literature on a digital specific exposure adaptation system.
Keywords: Exposure, radiography
Introduction
The transition from film/screen to digital technology for image acquisition in radiography departments has been progressing for 30 years.1 Digital radiography encompasses both computed radiography (CR) and direct digital radiography (DDR). There are many advantages of digital imaging that make it preferable to film/screen technology, including digital storage and transfer of images, non-chemical processing, reusability, wider exposure latitude and post-processing algorithms.2 Wider exposure latitude and post-processing algorithms adjust the image to a standard displayed optical density (OD) regardless of X-ray exposure, thereby disguising exposure errors.3,4
Optimal exposure is necessary for accurate diagnosis as well as adherence to the ALARA principle. Underexposed images results in increased quantum mottle, reduced image quality of the radiograph and may impede diagnosis.5,6 Overexposure reduces quantum mottle, improving image quality, and is less likely to be rejected by radiologists; thus there is a trend towards this technique.7,8 However, a higher exposure means an increase in dose to the patient. This trend to overexpose is known as dose creep' and is a growing concern with digital radiography.7,8
DDR, if used optimally, can provide equivalent image quality at a lower dose. Both CR and DDR can reduce the dose as the wider exposure latitude and post-processing algorithms minimise the need for repeats due to exposure selection errors.9 Compagnone et al. compared film/screen technology, CR and DDR, and found that CR needs a higher exposure to the patient to provide equivalent image quality to film/screen. However, the direct digital system was able to produce equivalent image quality to film/screen at lower dose, reduced by 13–66%.10
A well-defined system of exposure adaptation is required to allow accurate exposure selection for a variety of patients. Some research has gone into finding optimal exposure parameter settings for the ‘average patient’.11,12 However, the patients that radiographers encounter will deviate from the ‘average’ and exposures will need to be adjusted accordingly. The aim of the following review is to identify all published radiographic exposure adaptation systems which have been, or are being, used in general radiography and discuss their applicability to digital systems.
Methods
A search of Medline, Embase, CINAHL and Scopus databases was performed using the intervention terms combined with cohort terms, which are listed in Table 1. A wide range of intervention terms was used as there is no standard term for ‘exposure adaption system’ and the terminology for exposure parameters has changed over time. A variety of radiography-related terms were considered to ensure a complete search of the literature. The entire time period available was reviewed which ranged from 1949 to present. The search resulted in 3066 articles which were filtered down to 11 that satisfied the inclusion exclusion criteria. The search pathway is presented in Figure 1.
Table 1.
List of search terms used in database search.
| Intervention (all terms combined with ‘OR’) | Cohort | |
|---|---|---|
| Exposure determination | Fixed kvp | Radiography |
| Exposure adaptation | Fixed tube potential | Radiographer |
| Exposure modification | Fixed kilovoltage | Technician |
| Exposure parameter | Fixed kv | Radiologist |
| Exposure factor | Fixed peak kilovoltage | Radiologic technician |
| Exposure selection | Variable kvp | Technologist |
| Exposure adjustment | Variable tube potential | |
| Exposure decision | Variable kilovoltage | |
| Exposure alteration | Variable kv | |
| Exposure correction | Variable peak kilovoltage | |
| Exposure variation | System of exposure adaption | |
| Exposure technique | Bit system | |
| Exposimetry | Siemens point system | |
| Exposure calculation | 25% rule | |
| Exposure setting | 15% rule | |
| Exposure approach | Exposure chart | |
| Technique chart | ||
Figure 1.
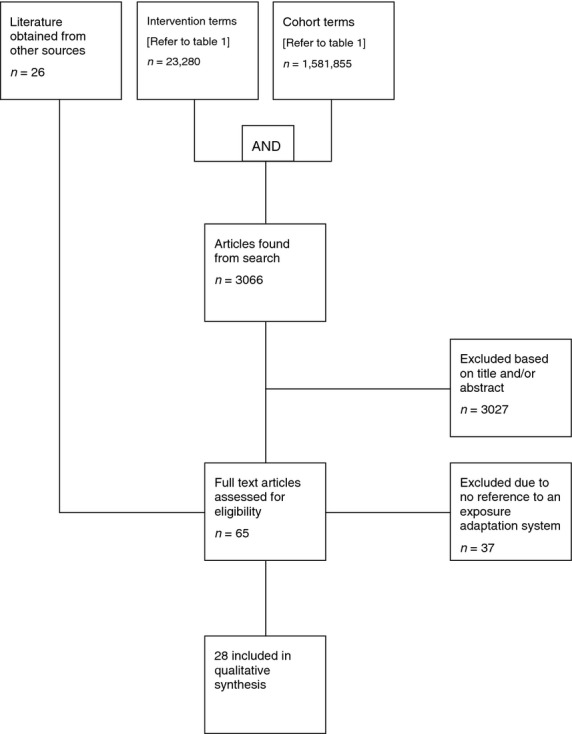
Search flow chart.
Studies that were included in this review were those that demonstrated a system of adjustment of multiple exposure factors which could be used in radiographic practice and those that were related to human general radiography, both film/screen and digital technology.
Studies that were excluded examined the optimum exposure factors for an examination of an average patient and those that focused on the relationship between exposure factors and dose.
Only 11 articles from the database search were accepted into this review. Another 13 articles were found through a journal specific search of the Radiologic Technology from 1961 to 2000 and The Radiographer from 1948 to 2000. These journals were selected as they were considered to be the most likely locations to find the articles related to exposure technique. All the literature found is summarised in Table 2. This study required no participants, thus no ethical approval was required.
Table 2.
The literature reviewed and a summary of the exposure adaptation systems described.
| Author/Paper | System | Study Design | Description | Limitations |
|---|---|---|---|---|
| Simon13 | 1. ‘Disc system’ | Description of the system(s) | 1. A system composed of concentric discs used to adjust exposure. Disc 1: Line up the parameters for an optimal exposure: tube current (mA), exposure time (s), tube potential (kVp), weight (lb). Turn the weight wheel to the desired weight and a set of optimal exposure parameters will be provided. If a certain kVp, mA or time is desired, turning the corresponding wheel will lead to compensation through adjustment of another factor. Disc 2: Same control as disc 1. The factors addressed are tube unit, grid, film/screen and tissue thickness combined into a density correction (DC) factor, SID (inches), kVp, mA and time. The mA and time adjustment based on linear logarithmic relationship with thickness. The kV scale based on the Bierman and Boldingh formula: (kV)5 × mAs = constant. |
1. None stated in article. |
| 2. Finding kilovolt peak (kVp) | 2. The radiographer needs to multiply the DC value (which includes anatomy thickness) by 2 then add 40 to find the kVp required for the anatomy being examined. | 2. None stated in article. | ||
| Gyss14 | 1. Optimum kilovoltage technique | Description of the system(s) | 1. All factors including kVp are fixed except time. Optimum time is found for an average patient. For a thicker than average patient, the time is doubled and for a thinner than average patient it is halved. | None stated in article. |
| 2. Variable kilovoltage technique | 2. The kVp is adjusted ‘to compensate … for part thickness … [and] radiopacity of the part.’ (p. 76) To adjust exposure for extremities that are imaged with a screen the kVp is adjusted 2 kVp per cm and without screen kVp is adjusted 3 kVp per cm. To adjust exposure because of radiopacity the patients are divided into three categories; hard to penetrate, normal and easy to penetrate. Hard to penetrate needs the addition of 4 kVp to the normal technique and easy to penetrate requires the subtraction of 4 kVp. |
2. ‘Radiographs of any given part will vary in contrast’. (p. 76) | ||
| Power15 | 1. Half value layer (HVL) | Description of the system(s) | 1. An ‘increase in thickness of body tissue of 3 cm. requires DOUBLE the exposure to achieve the same amount of film blackening’. (p. 16) [sic] | 1. None stated in article. |
| 2. 25% rule | 2. Every cm increase of patient thickness requires a 25% increase in milliampere-seconds (mAs). | 2. None stated in article. | ||
| Lyons16 | Optimum kilovoltage technique | Description of the system(s) | All factors including kVp are fixed except time. Optimum time is found for an average patient. For a thicker than average patient the time is doubled and for a thinner than average patient it is halved. | None stated in article. |
| Pinson17 | Unit step radiography | Description of the system(s) | Involves the use of a calliper which has been modified to have a scale of ‘units’ oppose to a centimetre scale. The values of the exposure parameters are also assigned ‘units’. Measure the anatomy to be imaged with this calliper and the ‘units’ is read. The correct exposure is when the sum of the ‘units’ of the set of exposure parameters matches the ‘units’ read off the calliper. | ‘The greatest error will occur when the calliper measurement is midway between a whole number and the next half unit’. (p. 9) |
| McDaniel18 | HVL | Water Bath Study Radiographs made each time there was an increase in 4 cm of water. Then for every 3.5 cm increase. Consistency of image density was observed when the exposure (time) was double in response to each increase. | For every 4 cm increase in patient thickness requires a doubling of exposure (time) in order to achieve an image of equal density. The study found slight density fluctuations when doubling exposure for every 4 cm increase in thickness and found more consistent density occurs when doubling exposure for every 3.5 cm increase in thickness. |
The more accurate value for HVL is between 3.3 cm and 3.8 cm but the use of 4 cm has a negligible effect and is suitable for practical use. |
| Funke19 | 1. Pegged kilovoltage technique | Description of the system(s) | 1. The kVps 44, 51, 57, 65, 75, 86, 100 and 120 are the only ones required for most radiologic examinations. Each step in this sequence delivers twice the exposure to the film than the preceding step. For each part of anatomy, set of one these values as optimum and only adjust mAs in response to an increase in patient thickness. | 1. Beyond certain limits it becomes impractical to increase the milliampere-seconds further because the limits of safe tube loading or acceptable exposure times cannot be exceeded. Thus, a change in kVp is required which alters the contrast of the image. |
| 2. HVL | 2. ‘The milliampere seconds should be doubled (or reduced by one half) for every three centimetres of tissue thickness’. (p. 207) [sic] | 2. This method fails when the anatomy thickness is greater than 30 cm, particular with high kVp and a HVL of 4 cm should be used. | ||
| Power20 | 1. ‘Rule of the thumb’ | Narrative review | 1. Time needs to be halved in order to achieve an image of equivalent density when the kVp is increased by 10 kVp. | 1. Only suitable for a kVp between 60 and 80 kVp. If the kVp is outside this range there is an error of 3–5 kVp. |
| 2. Siemen's point system | 2. Each region of anatomy is assigned points. The exposure parameters are also assigned points. If the sum of the points of the selected parameters matched the points of the anatomy being image then the exposure should be correct. | 2. It fails at the extreme ends of the kVp range (40 and 117 kVp). | ||
| 3. Unit step radiography | 3. Exposure parameters and patient thicknesses were assigned ‘units’ and an increase in one ‘unit’ equals a doubling of exposure. | 3. It fails at the extreme ends of the kVp range (40 and 117 kVp). | ||
| 4. Variable kVp technique | 4. The mAs is kept constant and the kVp is adjusted. An increase of 2 kVp is required for each centimetre increase in patient thickness. | 4. This technique causes a variation in contrast between different patient thicknesses | ||
| 5. Optimum kVp technique | 5. The kVp is ‘fixed at an optimum level of contrast’. (p. 11) The mAs value varies and is selected based on patient thickness. | 5. None stated in article. | ||
| 6. 25% rule | 6. Every cm increase of patient thickness requires a 25% increase in mAs. | 6. None stated in article. | ||
| Eastman21 | Body habitus factor | Description of the system(s) | The body habitus factor is found by dividing the patient's weight by their height. This value is then located on the chart provided in the article to find the appropriate exposure parameters. | None stated in article. |
| Eastman22 | Bit system of technic conversion | Description of the system(s) | ‘“Bits” are assigned to the factors controlling exposure such as kilovoltage and millampere-seconds’. (p. 75) ‘As long as the Bit totals remain constant, film density remains approximately constant’. (p. 76) |
None stated in article. |
| Kratzer23 | Supertech | Description of the system(s) | A system comprised of 3 charts. Chart A has a list of projections and a slider behind it. The slider is moved in order to display the measured thickness in the box next to the projection. Chart B provides correction factors for a change in FFD, grid, screen, aluminium filter, density and other minor factors. Chart C provides ‘200 combinations of kilovoltage, milliamperage, and time’. (p. 146) | The paper is not clear on how these three charts work to provide an adjusted exposure factor. |
| Atkins24 | 1. Bit system of technic conversion | Narrative review | 1. ‘Increasing one whole number in the Bit System, doubles the exposure, with a corresponding increase in density’. (p. 389) | 1. None stated in article. |
| 2. The thumb rule | 2. ‘As you double milliampere seconds, you reduce kilovoltage by 10 kilovolts’. (p. 389) | 2. This only applies when the kVp is decreased from 80 kVp to 70 kVp | ||
| 3. Variable kilovoltage technique | 3. ‘Milliampere seconds … are kept constant and kilovoltage is varied by 2 kvp. per centimeter of thickness’. (p. 389) | 3. A change in kVp also leads to a change in contrast. | ||
| 4. Optimum kilovoltage technique | 4. ‘When milliampere seconds and adequate kilovoltage values are established for the average patient, one half the milliampere-seconds value is then used for the small patient, and twice the milliampere-seconds value is used for the large patient’. (p. 389–390) | 4. None stated in article. | ||
| 5. Automatic exposure control (AEC) | 5. This technique involves employing a ‘fixed voltage and fixed milliamperage, with the time of exposure determined by the sensing device’. (p. 390) | 5. Incorrect centring leads to an incorrect exposure. | ||
| Stopford25 | Log10 technique chart | Description of the system(s) | Log10 factor is the value needed to increase the parameter per cm. Log10factor = [log10(of mAs for large) – log10(of mAs for small)]/(cm difference) Allows you to develop charts with mAs provided for each cm. The same can be done for kVp. |
None stated in article. |
| Markivee et al.26 | 1. AEC | Description of the system(s) | 1. ‘Terminates the X-ray beam when a preset level has been accumulated’. (p. 113) | 1. Errors in exposure occur when
|
| 2. Unit step radiography | 2. An exposure value scale (XVS) number is assigned to the centimetre thicknesses of body part and can be alter to suit the tissue composition. XVS numbers are also assigned to the values of the exposure parameters; kilovoltage, milliamperage and time. An accurate exposure comes from the selection of parameters whose XVS total matches the XVS of the anatomy to be imaged. Exposure parameters can also compensate for changes in ‘film speed, screen speed, target-to-film distance …, single phase or three phase power supplies, half wave or full wave rectification and the numerous patient variables’. (p. 114) |
None stated in article. | ||
| 3. Computer program | 3. Based on a modified version of unit step radiography to match the modern day techniques. It requires the input of ‘patient, equipment and other physical factors’ (p. 114) which leads to a total XVS number which in turn leads to a set of exposure parameters being displayed. Three sets are displayed which vary in kVp by 1 XVS number but all will produce the same density image. It is possible to adjust technique to different electrical powers and different amounts of filtration. |
3. Errors occur when the patient isn't properly measured. Using the system increases the time required per examination. Wide coverage of factors that influence exposure increase amount of input data required and thus increases length of each examination. |
||
| Horsington27 | Computer program | Description of the system(s) | It requires the input of a variety of factors to allow the calculation of a new exposure, which are tissue thickness, bucky or non-bucky, grid, SID, whether the lungs are in the region of interest and whether an intensifying screen is being used. Once all information has been collected, kVp and mAs will be displayed. The operator has the option of changing one of these values to get a different set of parameters. |
None stated in article. |
| Enright28 | Linear logarithmic relationship between mAs and patient thickness | Phantom Study Measure mAs need for varying patient thickness at each constant kVp. 60–120 kVp was tested at 5 kVp increments. Grid ratio used was not indicated. SID set at 100 cm | Using phantoms that represent the maximum and minimum thicknesses of the region and finding the optimal mAs and graphing a line between those two points to find appropriate mAs for thicknesses between the two thicknesses used. | This technique doesn't account for tissue composition. |
| Lewis29 | Computer program | Description of the system(s) | It requires the input of a variety of factors to allow the calculation of an appropriate set of exposure parameters that is displayed. The factors requested are body part, projection, intensifying screen, initial exposure factors and the exposure factor to be adjusted. |
None stated in article. |
| Kelly30 | 1. Half value layer (HVL) | Description of the system(s) | 1. ‘An increase in tissue thickness of 3 cm would require that the “Base” exposure be doubled to maintain the required film density’. (p. 19) | 1. None stated in article. |
| 2. 25% rule | 2. Every cm increase of patient thickness requires a 25% increase in mAs. | 2. Exceptions to the rule exist. i.e., for chest X-ray and thickness >25 cm a 25% increase in mAs per 1.5–2 cm increase in thickness. | ||
| 3. 15% rule | 3. A 15% increase in kVp requires a 50% decrease in mAs in order to achieve the same exposure. | 3. None stated in article. | ||
| Sterling31 | AEC | Description of the system(s) | The AEC ‘terminates the exposure when the proper level of radiation has been reached’. (p. 422) This allows the X-ray system to provide ‘consistent radiographic densities’. (p. 426) |
Incorrect positioning and/or chamber selection and/or bucky selection will lead to incorrect exposure. The desired exposure time needs to be greater than the minimum response time. The backup timer needs to be the maximum exposure required in case of malfunction The ‘AECs must be calibrated for the film screen combination in use’ (p. 425) and ‘to provide the required image density with the film screen combination in use’. (p. 426) |
| Artz3 | AEC | Description of the system(s) | A radiation detection device is place in front of or behind the image receptor and measures the residual X-ray beam. When sufficient X-rays have reached the detector the beam is stopped. | None stated in article. |
| Al-Balool and Newman32 | 1. 25% rule | Water bath used to simulate a patient. 50–150 kVp at 10 kVp increments was tested. Grid and non grid was tested for the whole kVp range. SID = 100 cm | 1. Every cm increase of patient thickness requires a 25% increase in mAs. | 1. The 25% rule only works well for most radiographic situations (low kVp with no grid and high kVp with a grid). |
| 2. 15% rule | 2. A 15% increase in kVp requires a 50% decrease in mAs in order to achieve the same exposure. | 2. The 15% rule is less reliable as the factors that affect the required mAs adjustment are patient thickness and the amount of mAs change required per kVp. | ||
| Carroll33 | 1. 15% rule | Description of the system(s) | 1. A 15% increase in kVp requires a 50% decrease in mAs in order to achieve the same exposure. | 1. None stated in article. |
| 2. Half value layer | 2. ‘Every four centimetres of thickness requires a change in mAs by a factor of two’ (p. 154). | 2. None stated in article. | ||
| 3. Optimum (fixed) kilovoltage technique | 3. A kVp is found for each part of anatomy that provides the best contrast and then is keep constant. The mAs is set as the maximum the desired focal spot size can accommodate. The optimal time is selected for an average patient. The time is double when a thicker an average patient is examined and halved for a smaller than average patient. | 3. None stated in article. | ||
| 4. Variable kilovoltage technique | 4. The optimal mAs needs to be found for each region and is then kept constant. The kVp is selected by multiplying the thickness of the anatomy of interest by 2 and adding 40. | 4. Altering kVp results in differences in contrast of images of the same region for different patient thicknesses or a change in contrast of images of the same region but differing projections. | ||
| 5. AEC | 5. A detector, either an ion chamber or photomultiplier tube, is the used to measure the exit beam that reaches the film/image plate. When a preset amount of radiation has reached the detector the exposure is stopped. | 5. It is not effective when imaging anatomy smaller than the detector, when the detector is not completely covered by anatomy, when positioning and/or centring are incorrect, when collimators are too wide increasing scatter radiation and when implants are covering the detector. | ||
| Schueler34 | 1. 10 kVp rule | Description of the system(s) | ‘An increase of 10kVp is equivalent to doubling the milliampere-seconds’. (p. 732) | It only works for a small range 60–100 kVp |
| McLean and Targett35 | 25%/cm rule | Water bath used to simulate a patient. The mAs needed for 1 cm increase in water depth was measured. No grid was used for 50–70 kVp and a grid used for 70–117 kVp SID = 100 cm. |
Every cm increase of patient thickness requires a 25% increase in mAs. | It works for most radiographic situations. Exact adjustment varies a few percent, which has a negligible effect on image quality |
| Fauber36 | 1. 15% rule | Description of the system(s) | 1. A 15% increase in kVp requires a 50% decrease in mAs in order to achieve the same exposure. | 1. None stated in article. |
| 2. AEC | 2. A radiation detection device is place in front of or behind the image receptor and measures the residual X-ray beam. When sufficient X-rays have reached the detector the beam is stopped. The AEC only controls the time factor so kVp and mA still need to be set. |
The AEC requires correct centring and detector selection, as incorrect centring and/or detector selection will result in an over- or under- exposed image. The AEC cannot distinguish between scatter and primary beam so wide collimation will lead to premature automatic cut-off. |
||
| Bontrager37 | 1. 15% Rule | Description of the System(s) | 1. A 15% increase in kVp requires a 50% decrease in mAs in order to achieve the same exposure. | 1. None stated in article. |
| 2. AEC | 2. ‘These systems provide automatic termination of exposure time when sufficient radiation (exposure) is received by the selected ionisation chamber’. (p. 36) | 2. None stated in article. | ||
| Eastman38 | 1. AEC | Summary | 1. The AEC uses ‘either a photocell or ionisation chamber … to terminate exposure when sufficient remnant radiation has reached the receptor’ (p. 202). | 1. None stated in article. |
| 2. Body habitus technique | 2. There is a chart for each body type (hypersthenic, sthenic, hypostenic, or asthenic) and the patient is categorised as one of these types and the corresponding chart is consulted. ‘Both kVp and mAs vary’ (p. 202). | 2. None stated in article. | ||
| 3. Variable kilovoltage technique | 3. The ‘mAs remains constant and the kVp changes according to the size of the anatomical part’. (p. 202) Increase the kVp by 2 for every centimetre increase in thickness. | 3. None stated in article. | ||
| 4. Fixed kilovoltage technique | 4. The ‘kVp remains constant and mAs is used to compensate for patient size’. (p. 202) The patient is classified as small, medium or large and the exposure is adjusted accordingly. | 4. None stated in article. | ||
| 5. High kilovoltage technique | 5. This is where the ‘fixed kVp technique … [is used] in the higher kilovolt peak range (100–150 kVp)’. (p. 203) | 5. None stated in article. | ||
| DuPont™39 | DuPont™ bit system | Exposure adaptation system chart | A ‘bit’ value is assigned to the values of each factor. The radiographer calculates the ‘total bit value’ for a ‘standard’ set of parameters. Whenever a factor changes from the ‘standard’ parameters, the radiographer needs to work out the new ‘total bit value’ and adjust the parameters in order to return to the value of the ‘standard’. A change of 1 ‘bit’ equals a doubling, or halving, of exposure. | None stated on system. |
Results
Patients that visit the radiology department naturally vary in thickness, tissue composition and pathology. The radiographic exposure parameters that are set for an examination should be selected with consideration of these variations. In order to clarify how this is achieved, several methods have been published over the years. Exposure adjustment systems can be categorised into simple techniques, which minimises the exposure adaptation steps, mathematical approaches, comprehensive charts and technological approaches which eliminate mental calculations and chart searching through the use of technology.
Simple techniques
The early approaches to exposure adjustment were designed to simplify the process for radiographers by keeping all factors constant but one. The ‘optimal kVp technique’, as described by Lyons, involves selecting a kVp which provides the best contrast for the anatomy being imaged and adjusting the mAs based on patient thickness; where it is doubled when the patient was deemed to be above average in thickness and halved when below.16 This makes selecting exposure relatively simple but the division of patients into three categories is arbitrary and is vulnerable to subjectivity.
An opposing technique is the ‘variable kVp technique’ which involves keeping all parameters constant except the kVp. This technique adjusts exposure factors for variations in patient thickness, where the kVp is increased by two for each centimetre increase in patient thickness.24 However, the variation in kVp for different patient thicknesses will lead to a variation in the contrast of radiographs of the same anatomy.
The pegged kilovoltage technique was developed as an improvement to the optimal kilovoltage technique. The pegged kilovoltage technique follows the same principle as the optimal kilovoltage technique, however there are specific kVp values that must be used (Table 2). The mAs is adjusted based on a half value layer (HVL) of 3 cm, where a change in thickness of 3 cm requires the mAs to be doubled or halved. This allows adaptation of exposure without a change in image contrast. This approach to mAs adjustment is more precise than the optimal exposure technique. Furthermore, a step in kVp corresponds to a 50% change in exposure (Table 2). This guideline allows the kVp to be adjusted instead of mAs when the mAs calculated goes beyond the tube limits or when a change in image contrast is required.19
Mathematical approaches
Mathematical approaches allow for the adjustment of factor(s) per centimetre making exposure selection more precise. The HVL refers to the thickness of a material required to produce an exit beam that is half the intensity of the primary beam. In the literature there is a discrepancy between the HVL of human tissue. In some papers, the HVL is 4 cm,33 while others state that it is 3 cm.15,30 McDaniel's water bath study found that the HVL lies between 3.3 and 3.8 cm so it is difficult to determine which of these is correct. A HVL of 3 cm provides the basis of the 25% rule.18
The 25% rule provides a method for adjusting mA, s, or mAs in response to variations in patient thickness. The 25% rule states that a 25% increase in mA, s, or mAs is required for each centimetre the patient is greater than the ‘average’.20,30 This is more of a guideline as it only works for radiographic situations (low kVp with no grid and high kVp with grid) and is an average of values that deviate from this by 2–5% depending on the kVp.32,35 Manufacturers incorporated this rule in the construction of their systems by making the time and/or mA factor(s) increase by a factor of 25% simplifying the job for the radiographer.30
The 15% rule describes the relationship between kVp and mAs. The 15% rule states that a 15% increase in kVp requires a 50% reduction in mAs to achieve the same exposure.33,37 This guideline only works for thicknesses of less than 15 cm and kVp less than 10032 and variation from this will result in a 5% error which is important as it amounts to ∼25% exposure difference. The 15% rule lacks accuracy across a wide range because the change in mAs required is affected by the mAs change per kVp and patient thickness.32
Enright devised a simple method for finding the mAs required for a range of patient thicknesses. It was based on the linear logarithmic relationship between mAs and anatomy thickness based on the 25% rule.28 Although this provides a quick method of producing exposure charts that cover a wide range of thicknesses, it fails to account for the variation of tissue composition. It is also limited by the fact that it only looks at adjustment of mAs.
Comprehensive charts
The 25% and 15% rules are useful guidelines for exposure adaptation but require some calculations in order to find the required values. Comprehensive systems have been developed in the form of charts, which adopt these rules as a basis for their systems of exposure adjustment and minimises the calculations required. These are the ‘disc system’, the unit step radiography and the DuPont™ Bit System.
The ‘disc system’ adjusts numerous exposure parameters providing a more comprehensive system of exposure adjustment. This system involves two discs, the first focuses on the adaptation of exposure parameters (kVp, mA, s) to the variation in patient weight as well as being able to compensate for a change in one of the parameters through a change in another. The second disc looks at the parameter required to produce a diagnostic image with a certain tube unit, grid, film/screen combination and patient thickness.13 This system is much better than those mentioned above as it looks at how different factors affect the exposure parameter required as well as how to compensate for a change in the exposure parameters.
Unit step radiography is an early system of exposure adjustment designed to adapt technique to changes in ‘film speed, screen speed, target-to-film distance, single-phase or three-phase power supplies, half wave or full wave rectification and the numerous patient variables’26 (p. 114). It adjusts exposure factors to compensate for changes in anatomy thickness by assigning each centimetre an exposure value scale (XVS) value as well as assigning the values of kVp, mA and time XVS values. An optimum exposure will be selected if the total XVS values of the exposure parameters equal the XVS value of the anatomy being imaged.26 However, this system fails at the extreme ends of the kVp range.20
The DuPont™ Bit System is another comprehensive exposure adaptation system. It covers most of the factors and parameter adjustments that the ‘disc system’ performs and also takes into account pathology. The Bit System assigns ‘bits’ to a wide range of values for each parameter that could affect the residual beam. A change in the bit value of one parameter can be compensated for by a change in another parameter(s) by the same number of bits to produce an image of equal OD.22 A change in 0.2 ‘bits’ corresponds to the change required in the parameter for a visible change in the image and a change in 1 ‘bit’ corresponds to a doubling or halving of the exposure.24
Technological approaches
There has also been the utilisation of technology in the selection of exposure parameters. Some of the systems, such as the unit step system described above, have been incorporated into the computer programs that speed up the exposure selection process. The X-ray system itself has also been improved through the addition of the automatic exposure control (AEC) system, which has direct control over the exposure being produced.
The AEC is designed to terminate the X-ray beam when a sufficient amount of exit beam is detected; this is determined by the mA and exposure time values. The AEC provides a quick and easy solution for adjusting radiographic exposure to patient thickness as it aims to give just enough exposure to produce the set image density. However, if the anatomy is not positioned over the AEC chambers, the wrong AEC chamber is selected or the wrong bucky selected, then the resultant image will be incorrectly exposed. Also the AEC is limited to bucky examinations and non-bucky examinations still require the use of manual exposures.3,36 The AEC is a good system of exposure adaptation as it accurately adjusts time in response to patient thickness if used optimally but still requires kVp and mA selection.3,36
Several articles26,27,29 described and provided the code for computer programs which use formulas to calculate exposure adjustment factors. It is designed to request information about the examination to be undertaken and then provide a set of exposure parameters in return. The program by Markivee et al. is based on a modified version of unit step radiography and his initial clinical testing found that it was well received by the radiographers.26
OD was a way to measure image quality in film/screen radiography. This value was also used as a way to determine the quality of the radiographs. An OD of 1.3–1.5 was deemed diagnostic and the techniques were assessed on their ability to produce or maintain this OD value.28,32 This measure of image quality is not applicable to digital radiography, particularly when viewing images on the monitor, so a new measure needs to be considered. Detector dose indices were developed for digital radiography which measures the amount of radiation that interacts with the detector and would provide a suitable substitute for OD.8
The systems described above are systems for exposure adaptation. These systems rely on the optimal parameters for an ‘average’ person as a baseline to work from. However, a problem arises when classifying an ‘average’ person, as the ‘average’ varies depending on the sample selected, such as the world population or only females.40 A considerable amount of research has gone into finding the set of parameters that provides a diagnostic image with minimal patient dose. This research is valuable for the construction of exposure charts that the exposure adaptation system works with, allowing selection of patient-specific exposure parameters. The DuPont™ Bit System could provide a good basis for the construction of a digital radiography-specific radiographic exposure adaptation system.
Discussion
Several different systems have been developed to assist radiographers for variations in patients. There is the 25% rule and 15% rule, which are basic systems as described by Kelly30 and Carroll.33 These rules were guidelines and have limitations as clinical radiographic exposures cover a wide range which the systems do not accurately cover. The more comprehensive exposure adaptation systems, such as the ‘disc systems’ and DuPont™ Bit System, use these guidelines as a basis for their construction and cover both a wider range of values for each parameter as well as many other factors that influence the exit beam.
The objectivity and completeness of the review could not be optimised due to the limitations faced. Time and resource restraints limited the review to literature published in journal articles and prevented exploration of unpublished works. Completeness is also compromised as over half the literature reviewed was not obtained through the databases listed but instead a journal-specific search. It is likely that the articles retrieved from Radiologic Technology and The Radiographer was not found by the databases as they were older than the year range available in the databases and needed to be found through a manual search. Other journals, such as Radiography, were not searched manually due to time restraints. Also some systems that were referenced in articles could not be obtained, thus preventing their inclusion into the review. The search was conducted by one person as distinct from a pair meaning that there was a risk of inherent subjectivity in article selection.
The literature uncovered concerning the systems of exposure adjustment was mostly descriptive, thus their efficacy is not known. The 15% and 25% rules were tested in two papers and found to be suitable for radiographic exposures used in clinical practice. However, these were water bath studies and their applicability to patients may not be accurate and phantom testing should be considered. The other systems, ‘disc system’ and DuPont™ Bit System, were not tested making it impossible to determine their efficacy and which system is most effective, which needs to be addressed particularly for digital.
Due to the lack of evidence proving a particular system is most effective, it is difficult to know which system would be most suitable in practice. All of these systems were developed for film/screen technology and their applicability to the digital systems is unknown as no literature was found. This is important because the materials used to construct the digital X-ray system, particularly the receptor phosphors differs from film/screen; thus there will be variations in their response to X-ray exposure.1 Since all of Australia and most of the developed world is now using digital radiography systems, there is a necessity for research in this field.
The literature has shown that it is possible to create a program that integrates a system of exposure adjustment so that radiographers can quickly input the factors known and get an optimal set of exposure parameters. Thus, once a digital-specific system of exposure adaptation has been developed, it should be extended into an electronic form allowing it to be easily accessible and increasing the likelihood that it will be used. It could be a useful tool both in the university, as a teaching tool and in the work place as a patient optimisation tool.1
Conclusion
There are no studies examining the efficacy of exposure adaptation systems designed for film/screen radiography with digital technology, nor is there any describing a system made for digital radiography. Film/screen radiography has been almost completely replaced by digital radiography creating a need for a suitable method of exposure adaptation. Thus, future research should test whether the existing comprehensive exposure adaptation systems are applicable to digital radiography.8
Conflict of Interest
The authors declare no conflict of interest.
References
- Compagnone G, Casadio Baleni M, Di Nicola E, et al. Optimisation of radiological protocols for chest imaging using computed radiography and flat-panel X-ray detectors. Radiol Med. 2013;118:540–54. doi: 10.1007/s11547-012-0892-8. [DOI] [PubMed] [Google Scholar]
- Willis CE. Computed radiography: a higher dose? Pediatr Radiol. 2002;32:745–50. doi: 10.1007/s00247-002-0804-6. [DOI] [PubMed] [Google Scholar]
- Artz DS. Computed radiography for the radiological technologist. Semin Roentgenol. 1997;32:12–24. doi: 10.1016/s0037-198x(97)80032-6. [DOI] [PubMed] [Google Scholar]
- Seibert JA, Shelton DK, Moore EH. Computed radiography X-ray exposure trends. Acad Radiol. 1996;3:313–8. doi: 10.1016/s1076-6332(96)80247-9. [DOI] [PubMed] [Google Scholar]
- Thakur Y, Bjarnason TA, Hammerstrom K, Marchinkow L, Koch T, Aldrich JE. Assessment of patient doses in CR examinations throughout a large health region. J Digit Imaging. 2012;25:189–95. doi: 10.1007/s10278-011-9390-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath R, England A, Ward A, et al. Digital pelvic radiography: increasing distance to reduce dose. Radiol Technol. 2011;83:20–8. [PubMed] [Google Scholar]
- Gibson DJ, Davidson RA. Exposure creep in computed radiography: a longitudinal study. Acad Radiol. 2012;19:458–62. doi: 10.1016/j.acra.2011.12.003. [DOI] [PubMed] [Google Scholar]
- Herrmann TL, Fauber TL, Gill J, et al. Best practices in digital radiography. Radiol Technol. 2012;84:83–9. [PubMed] [Google Scholar]
- Peer S, Peer R, Walcher M, Pohl M, Jaschke W. Comparative reject analysis in conventional film-screen and digital storage phosphor radiography. Eur Radiol. 1999;9:1693–6. doi: 10.1007/s003300050911. [DOI] [PubMed] [Google Scholar]
- Compagnone G, Baleni MC, Pagan L, Calzolaio F, Barozzi L, Bergamini C. Comparison of radiation doses to patients undergoing standard radiographic examinations with conventional screen–film radiography, computed radiography and direct digital radiography. Br J Radiol. 2006;79:899–904. doi: 10.1259/bjr/57138583. [DOI] [PubMed] [Google Scholar]
- Fauber TL, Cohen TF, Dempsey MC. High kilovoltage digital exposure techniques and patient dosimetry. Radiol Technol. 2011;82:501–10. [PubMed] [Google Scholar]
- Grondin Y, Matthews K, McEntee M, et al. Dose-reducing strategies in combination offers substantial potential benefits to females requiring X-ray examination. Radiat Prot Dosimetry. 2004;108:123–32. doi: 10.1093/rpd/nch015. [DOI] [PubMed] [Google Scholar]
- Simon M. Exposure factor selection by means of a new calculator. Br J Radiol. 1956;29:588–95. doi: 10.1259/0007-1285-29-347-588. [DOI] [PubMed] [Google Scholar]
- Gyss EE. A medical radiographic technique chart based on constants. X-ray Tech. 1957;29:76–80. [PubMed] [Google Scholar]
- Power KJ. A simple measuring device for the busy department. Radiographer. 1959;7:16–7. [Google Scholar]
- Lyons NJ. Optimum kilovoltage technique. X-ray Tech. 1962;33:398–401. [PubMed] [Google Scholar]
- Pinson A. Unit step radiography. Radiographer. 1963;10:6–10. [Google Scholar]
- McDaniel CT. Tissue absorption theory applied to formulation of radiographic technique resulting in time as the variable factor. Radiol Technol. 1965;37:51–5. [PubMed] [Google Scholar]
- Funke T. Pegged kilovolt technique. Radiol Technol. 1966;37:202–13. [PubMed] [Google Scholar]
- Power KJ. The evolution of radiographic exposures. Radiographer. 1967;13:6–15. [Google Scholar]
- Eastman TR. Chest technique through body habitus. Radiol Technol. 1969;41:80–4. [PubMed] [Google Scholar]
- Eastman TR. Measurement: the key to exposure with manual techniques. Radiol Technol. 1973;45:75–8. [PubMed] [Google Scholar]
- Kratzer B. A technique computer: scientific approach to radiologic technology. Radiol Technol. 1973;45:142–50. [PubMed] [Google Scholar]
- Atkins DF. Jerman memorial lecture: the image. Radiol Technol. 1974;45:385–95. [PubMed] [Google Scholar]
- Stopford JE. Log10 technique charts. Radiol Technol. 1979;51:331–3. [PubMed] [Google Scholar]
- Markivee CR, Edwards FM, Leonard P. Microcomputer controlled diagnostic X-ray exposure factors - A pilot study. Proc Annu Symp Comput Appl Med Care. 1980;3:113–6. [Google Scholar]
- Horsington G. An X-ray exposure calculator. Radiography. 1983;49:261–4. [PubMed] [Google Scholar]
- Enright M. A simple graphic method of exposure chart preparation for diagnostic radiography. Radiographer. 1984;31:43–7. [Google Scholar]
- Lewis S. Computer program for diagnostic X-ray exposure conversion. Radiography. 1984;50:266–70. [PubMed] [Google Scholar]
- Kelly A. Black or white? - Hit or miss. Radiographer. 1988;35:19–26. [Google Scholar]
- Sterling S. Automatic exposure control: a primer. Radiol Technol. 1988;59:421–7. [PubMed] [Google Scholar]
- Al-Balool G, Newman D. The relationships between kV, mAs and thickness in film-based radiography: 25% and 15% rules. OK? Radiography. 1998;4:129–34. [Google Scholar]
- Carroll QB. Fuchs's Radiographic Exposure, Processing, and Quality Control. 6th edn. Springfield, IL: Charles C. Thomas; 1998. [Google Scholar]
- Schueler BA. Clinical applications of basic X-ray physics principles. Radiographics. 1998;18:731–44. doi: 10.1148/radiographics.18.3.9599394. [DOI] [PubMed] [Google Scholar]
- McLean D, Targett C. Exposure determination: examining the validity of the 25%/cm rule. Radiographer. 2001;48:5–8. [Google Scholar]
- Fauber TL. Radiographic Imaging & Exposure. 3rd edn. St. Louis, MO: Mosby/Elsevier; 2009. [Google Scholar]
- Bontrager KL. Textbook of Radiographic Positioning and Related Anatomy. 7th edn. St. Louis, MO: Mosby/Elsevier; 2010. [Google Scholar]
- Eastman TR. Open forum. Exposure technique documentation. Radiol Technol. 2011;83:202–3. [PubMed] [Google Scholar]
- DuPont™ Photo Systems X-ray Technical Service. The Bit System Of Technique Management. 8th edn. Wilmington, DE: E.I. DuPont de Nemours & Co. (Inc.); , no date. [Google Scholar]
- Ruff C. Variation in human body size and shape. Ann Rev Anthropol. 2002;31:211–32. [Google Scholar]


