Abstract
Background:
It is important to plan preoperatively when contemplating internal fixation following deformity correction. Surgeons often find it difficult to retain the achieved correction till the end of internal fixation. To maintain precise correction we used hybrid technique which uses both external and internal fixation. The objective of the study was to evaluate the effectiveness of this hybrid technique in achieving and retaining desired correction.
Materials and Methods:
In this retrospective study, we evaluated the magnitude of deformity with radiological parameters. We compared correction which was planned and correction which was achieved. The technique was used during surgery for corrective osteotomies. Before carrying out the osteotomy, rail fixator with two swivel clamps was applied. After osteotomy swivel clamps were loosened. Desired correction was achieved. While fixator held the fragments in corrected position, definitive internal fixation was carried out. External fixator was removed after completion of internal fixation. Position of mechanical axis ratio, mechanical lateral distal femoral angle and mechanical medial proximal tibial angle were measured before and 12 weeks after surgery. Student t-test was used to analyze the difference between correction which was planned and correction which was achieved.
Results:
There was no statistical difference between the desired correction and the correction achieved.
Conclusions:
Temporary use of external fixator while correcting angular deformities of lower limb allows to achieve accurate correction.
Keywords: Deformity correction, osteotomy, external fixation, internal fixation, hybrid fixation
MeSH terms: Fixation, osteotomy, knee joint, techniques
INTRODUCTION
Osteotomies are commonly used in orthopedics for a wide range of deformity correction. Preoperative planning is necessary to determine the level and magnitude of the deformity. Corrections can be performed acutely or gradually. After correction is achieved, the choice of fixation can be internal, external or a combination of both. Each of these methods has its own advantages and disadvantages. External fixator allows adjustments postoperatively while internal fixation does not permit such correction after surgery. When internal fixation is planned after correction, it is very important that preoperative planning is meticulous and is executed precisely till the fixation is completed. Under-correction or over-correction is possible while executing the procedure. While correcting the deformity in one plane, iatrogenic deformity in other planes may also develop. If such a deformity is significant, it may adversely affect the function or may lead to excessive loading on adjacent joints. In some cases, repeat surgery for further correction may be required to correct this residual or iatrogenic deformity.
Various options are available to surgeons for precision during the procedure. These include checking alignment during surgery using fluoroscopy marking each fragment before osteotomy to judge the rotation, passing wires in each fragment to check rotation and the use of computer navigation.1
One technique to facilitate precise correction is hybrid technique which uses both external and internal fixation.2,3,4,5,6,7,8,9 In this technique, external fixation is used to stabilize the fragments while getting the desired correction. Internal fixation is then applied to a fully corrected osteotomy. Once osteotomy is internally fixed, external fixator is removed.
Various types of fixators and plates have been reported for this hybrid technique.2,3,4,5,6,7,8,9 The purpose of this study is to present a technique in which a rail fixator is used to assist correction and reduce soft tissue trauma and operative time to achieve desired correction. We describe our results using this method of deformity correction. The objectives of the study were to find whether our technique helps to achieve the desired correction and the technique can prevent an iatrogenic deformity.
MATERIALS AND METHODS
20 lower limb segments in 14 patients operated to correct the deformities, between April 2010 and December 2012 were included in this retrospective study. Preoperative and postoperative radiographs were reviewed. Patients who required simultaneous correction of rotation were not included in the study. Two patients had bilateral deformity in femur and tibia.
Coronal plane deformity was measured on a standing anterior posterior (AP) long leg radiograph taken as described by Paley.10 Lateral radiographs were taken to measure the sagittal plane deformity. Rotational alignment of tibia was assessed clinically using the thigh foot angle. For femoral rotational alignment, trochanteric prominence method was used.11
Radiographic measurements
On standing long leg AP radiograph mechanical axis (MA) is drawn by a line joining the centre of the hip and center of the ankle. To overcome different magnification on radiographs, we measured the position of the mechanical axis ratio (PMAR) by dividing perpendicular distance of MA from the medial most point of tibial condyle with a width of tibial plateau [Figure 1]. For valgus deformity, PMAR will be more than 0.5 and for varus deformity this ratio will be less than 0.5. When the mechanical axis passes medial to medial border of the tibial condyle, negative value is denoted. Mechanical lateral distal femoral angle (mLDFA) and mechanical medial proximal tibial angle (mMPTA) were measured as per the method of Paley.12,13
Figure 1.
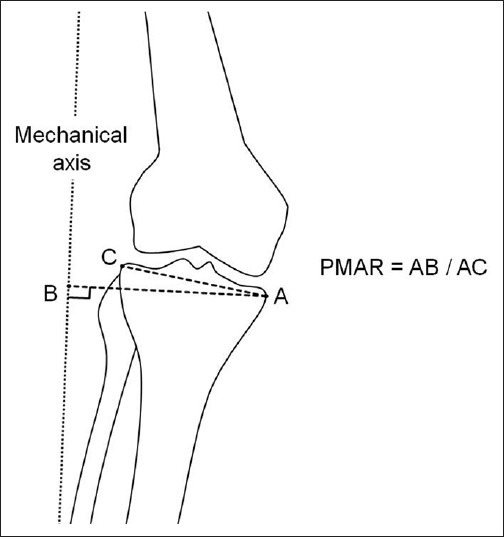
Method to see the mechanical axis ratio (PMAR). Dotted line is the mechanical axis. AB is the perpendicular distance from the medial most point of proximal tibial to the mechanical axis. AC is width of tibial plateau
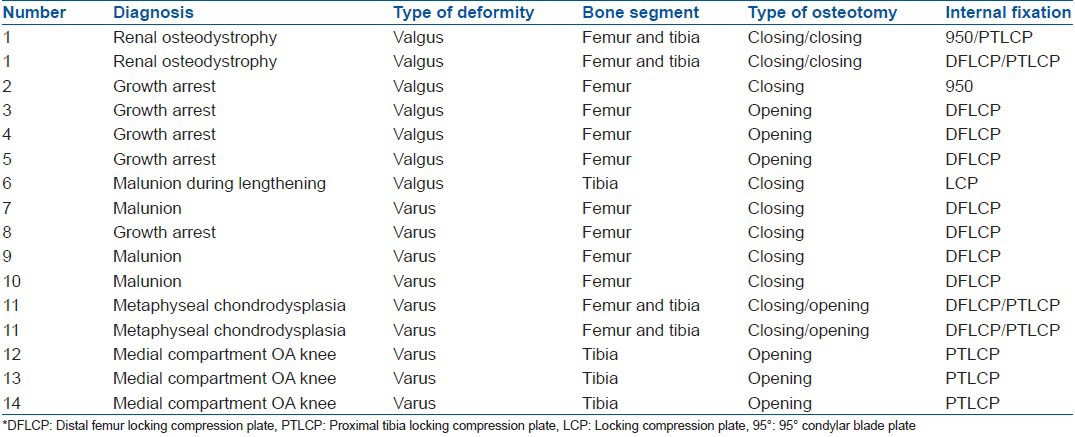
Data regarding underlying pathologies, type of deformities, osteotomy type and implants used for internal fixation are described in Table 1.
Table 1.
Patient details with deformity type, osteotomy type and implants used
Targeted correction
For young patients we planned that after surgery the MA passes from the center of the knee joint achieving a PMAR of 0.5. Three cases underwent proximal tibial opening wedge osteotomy for medial compartment osteoarthrosis (OA) of the knee joint. For this indication we intended to pass the postoperative MA through Fujisawa point achieving PMAR of 0.62.14 For cases other than OA of knee joint, we tried to achieve postoperative mLDFA and mMPTA values within a normal range of 85-90 degrees.12,13
Center of rotation of angulation (CORA) was identified by a method described by Paley.15 Correction was performed as close as possible to the CORA. Direction and level of osteotomy depended on the fixation device. When osteotomy hinge point was not at the CORA, displacement of mechanical axis was a likely occurrence. To overcome this displacement one of the fragments was displaced. From angulation observed on AP and lateral radiographs, the plane of deformity was calculated.16
Operative procedure
The plate length was marked on the skin. Rail fixator (Pitkar orthotools, Pune, India) with two swivel clamps was used in all cases. Plane of the fixator was parallel to plane of deformity. In cases where only coronal correction was required fixator was kept in a coronal plane. In case of oblique plane deformity, fixator was kept in an oblique plane. Two tapered pins were placed on either side of the planned osteotomy site. Pins were passed at a distance from the osteotomy so that they did not impede the subsequent internal fixation. Swivel clamps are aligned in such a way that full correction is possible. All pins were passed in one plane [Figure 2]. For deformity correction at distal femur, two pins were passed in the femoral diaphysis and two pins in the proximal tibia. For a proximal tibial deformity, two pins were passed in the distal femur and in the diaphysis of tibia.
Figure 2.

Clinical photograph showing rail fixator with two swivel clamps applied in the plane of deformity
After passing the pins, osteotomy site was exposed and osteotomy was carried out as planned.
Six patients had valgus deformity. Of these, four had deformity in femur, one in tibia and one patient had bilateral deformity in the femur and tibia, making a total of nine segments having valgus deformity (six femoral and three tibial). Three cases of femur underwent opening wedge osteotomy from lateral side and three underwent closing wedge for femur from medial side.17 Three tibial segments underwent closing wedge osteotomy from the medial side.
Eight patients had varus deformity. Of these, four had deformity in femur, three had deformity in tibia and one had bilateral deformity in femur and tibia making a total of 11 segments (6 femoral and 5 tibial). Femoral correction for varus deformity was by a closing wedge osteotomy from the lateral side and fixation was done on lateral side. Tibial correction for varus (5 segments) was by opening wedge osteotomy from medial side and fixation was done on medial side.
After osteotomy, swivel clamps were loosened and angular correction was achieved. Translation was carried out according to preoperative planning.16 Clamps were tightened. Coronal plane alignment was checked by a long metal rod [Figure 3]. Sagittal plane correction was checked clinically. If readjustment was required swivel clamps were loosened and further correction was carried out. Once desired correction was achieved, swivel clamps were tightened. Definitive internal fixation was carried out while external fixation held the fragments [Figure 4].
Figure 3.

Clinical photograph showing confirmation of the alignment
Figure 4.

Clinical photograph showing internal fixation is being carried out while external fixation ensures corrected position
For internal fixation our preference was tomofix plates (DePuy Synthes, Switzerland). For cases in which Tomofix inplants were not used, locking screw implants similar to Tomofix were used. In two cases such implants were not available for medial side of distal femur. We used 95° Condylar blade plate for these two cases.17 At least three screws having bicortical fixation were used for each fragment. Reduction clamps or plate holding clamps were not required in any case.
After the completion of internal fixation, external fixator was removed. Wound was closed over a negative suction tube. Postoperatively, partial weight bearing ambulation using a walker or crutches was started as soon as possible, usually on the second or third postoperative day. Full weight-bearing was permitted at 6 weeks after due x-ray evaluation.
Standing full length AP radiograph of lower limb was taken at 12 weeks after surgery. This radiograph was used for calculation of PMAR, mLDFA, and mMPTA. Sagittal plane alignment was evaluated by a lateral radiograph. Rotational alignment was also checked clinically at 3 months.
RESULTS
We used this technique in 20 lower limb segments (14 patients and 16 extremities). Surgery was performed on 12 femora and 8 tibias. 7 limbs had varus deformity and 9 extremities had valgus deformity. The osteotomy site was in the metaphysis in 18 segments and in the diaphysis in 2 segments. Two patients had bilateral deformity in the tibia and femur. These patients underwent surgery for ipsilateral tibial and femoral corrections in the same operative session. Tibial deformity was corrected first. Alignment was checked by a special device which helped to achieve mMPTA of 87 degrees. After internally fixing the tibial osteotomy, femoral deformity was corrected.
The number of screws placed in each segment varied from three to six. This was determined by the size of the patient and the quality of bone. Eighteen osteotomies were fixed with locking screw plate assembly. Autogenous bone grafting was used in two patients. These patients underwent opening wedge osteotomy of proximal tibia with a correction of more than 15°.
Corrections achieved
Difference of preoperative and targeted PMAR was 1.1 (range 0.59 to 2.31).
At 12 week postoperative evaluation, difference of targeted and post operative PMAR was 0.03 (range 0 to 0.07). Student's t test for targeted and actual post operative PMAR values showed a P value of 0.2569 which suggests there was no significant statistical difference between the targeted and actual postoperative PMAR values [Figure 5]. It confirmed that this technique ensured precision in osteotomy correction.
Figure 5.
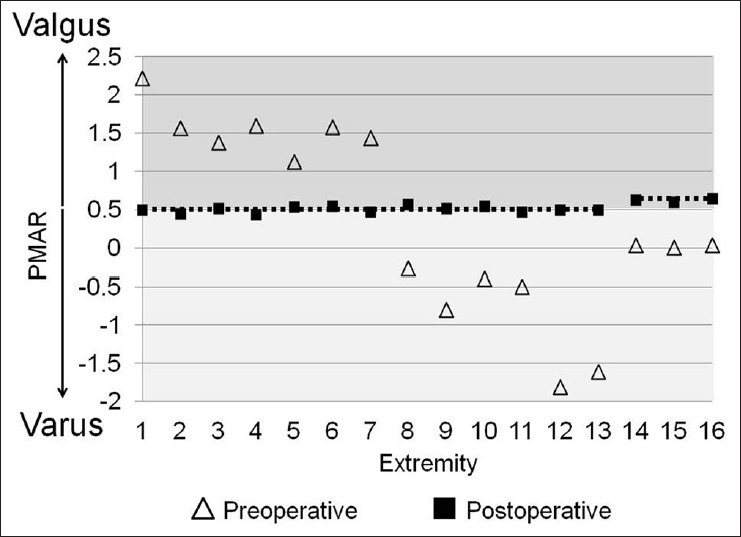
Preoperative and postoperative PMAR values of 16 limbs. Dotted line represents targeted PMAR of 0.5. Last three limbs were operated for medial compartment OA knees and had a targeted PMAR of 0.62
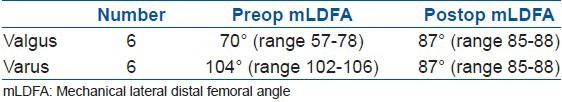
Of the 12 femoral corrections, 6 were for valgus and 6 were for varus. Preoperative mLDFA was outside the normal range in all patients. At 12 weeks, all patients had mLDFA within normal range (85° to 90°) [Table 2].
Table 2.
Preoperative and postoperative mechanical lateral distal femoral angle of 12 segments undergoing correction at distal femur
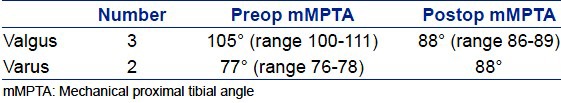
For mMPTA assessment, we did not include three patients in whom we carried out opening wedge osteotomy for OA of the knee joint. In OA of knee joint, our aim is to overcorrect mMPTA so that MA passes through Fugisawa point. In the remaining five patients, preoperative mMPTA was outside the normal range. At 12 weeks, all had mMPTA within normal range (85° to 90°) [Table 3].
Table 3.
Preoperative and postoperative mechanical proximal tibial angle of 5 segments § undergoing correction at proximal tibia. § 3 cases of proximal tibial osteotomy for medial compartment OA knee are excluded
None of the patients developed any iatrogenic deformity in other planes. No nerve releases were carried out. There were no cases of wound breakdown, infection or compartment syndrome. One patient who underwent simultaneous correction of distal femur and proximal tibial osteotomy for genu valgum developed lateral popliteal nerve palsy [Figures 6 and 7]. This recovered spontaneously by 12 weeks. Union was achieved in all segments at 12 weeks. All patients achieved preoperative knee range of motion at 12 week followup. Implants were not removed in any patient.
Figure 6.
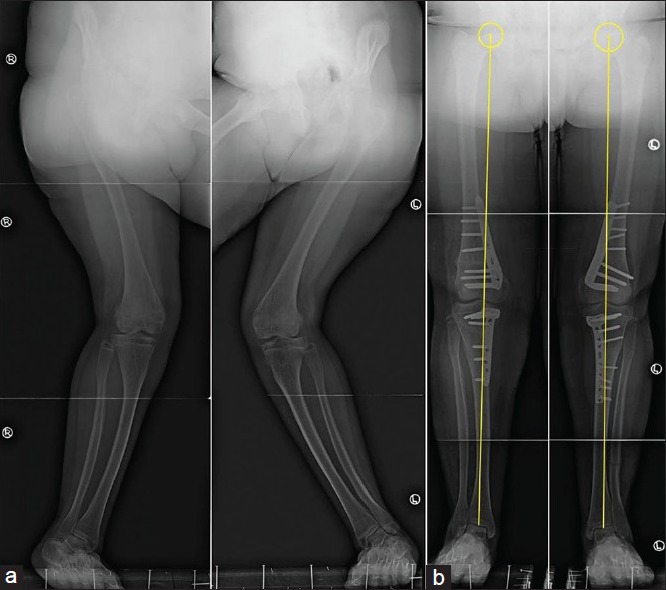
Pre and postoperative x-rays anteroposterior view (a and b) showing bilateral genu valgum due to renal osteodystrophy
Figure 7.

Pre and postoperative clinical photographs of the same patient showing correction of genu valgum
DISCUSSION
Acute correction of malalignment may be achieved with either closing or opening wedge osteotomy. After correction, osteotomy can be fixed internally or externally. It is crucial to fully correct the deformity at the time of surgery. External fixator allows correction even after surgery. However, external fixation is uncomfortable to the patient, tethers the soft tissues and is often associated with pin site irritation and infection.18 Due to these reasons stable internal fixation after deformity correction is preferred. When internal fixation is used, major challenge is in the difficulty in executing a precise deformity correction during surgery. After osteotomy bony fragments become unstable and are difficult to hold. If optimal correction is not achieved at the time of internal fixation then alignment cannot be achieved without additional surgery.
Hybrid techniques have been implemented to use the strengths and benefits of both internal and external fixation techniques.2,3,4,5,6,7,8,9 The external fixator is applied in the plane of deformity. The osteotomy is performed. The fixator is then used for controlled deformity correction. Intraoperative assessment is performed with fluoroscopy. The bony fragments are held stable during the process. Once the position is optimal, the internal fixation is carried out to maintain the corrected position. External fixator is removed peroperatively after internal fixation. Fixator-assisted nailing and plating has been described.2,3,4,5,6,7,8,9
Rogers described fixator-assisted plating with the hexapod external fixators.5 Hexapod external fixators such as the Taylor Spatial Frame (Smith and Nephew, Memphis, TN) and Multi axial Correction Frame (EBI/Biomet, Parsippany, NJ) which are designed specifically for deformity correction are well suited for this purpose. However, these fixators are not available particularly in a resource challenged set up. Bar-on et al. described a similar technique with tubular fixators.7 We used a rail fixator with a swivel clamps as an external fixator. Swivel clamps allow insertion of pins only in one plane or parallel planes. Two swivel clamps allow correction of angulation up to 80 degrees. It also allows translation of fragments. Axial compression at the osteotomy site can also be applied. Two pins in each fragment do not allow movement of fragment in other planes than the one in which they are passed.
Rail fixator has a disadvantage in comparison to a hexapod that rotational correction is not possible with rail fixator. We have modified the technique described in this paper for simultaneous correction of rotation but we have not included those cases in this study.
Holding the fragments with external fixator provide temporary stability before definitive internal fixation is carried out. Implants are applied to the bone manually without using reduction or plate holding forceps. This avoids soft tissue dissection. Actually time spent for applying the external fixator can be saved during this step of surgery.
Locked plating system has certain advantages over the nonlocking plate system. The plate functions like an internal fixator. It allows fixation even when the plate is away from the bone. This avoids unnecessary translation of bone. It reduces the possibility of loss of correction during and after surgery.19 For measuring the deformity we used PMAR. All radiographs have some element of magnification. To overcome this element we used PMAR. PMAR to overcome magnification element. The correction we achieved with our technique is also comparable with others.5,7 We had one complication of peroneal nerve palsy in a patient who underwent simultaneous femoral and tibial correction. Peroneal nerve palsy is a known complication of tibial osteotomy.20
The study has several limitations. The patient number is relatively small and they had varied etiologies. The fact that it was utilized successfully in such varied pathologies demonstrates the wide applicability of the technique. Followup period is short. A larger study with longer followup is required.
In conclusion, we believe that temporary use of external fixator while correcting angular deformities of lower limb allows one to achieve accurate correction. This technique can be used for both valgus and varus deformities of lower limb around knee.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Reising K, Strohm PC, Hauschild O, Schmal H, Khattab M, Südkamp NP, et al. Computer-assisted navigation for the intraoperative assessment of lower limb alignment in high tibial osteotomy can avoid outliers compared with the conventional technique. Knee Surg Sports Traumatol Arthrosc. 2013;21:181–8. doi: 10.1007/s00167-012-2088-1. [DOI] [PubMed] [Google Scholar]
- 2.Gugenheim JJ, Jr, Brinker MR. Bone realignment with use of temporary external fixation for distal femoral valgus and varus deformities. J Bone Joint Surg Am. 2003;85:1229–37. doi: 10.2106/00004623-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464–80. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Eralp L, Kocaoglu M, Yusof NM, Bulbul M. Distal tibial reconstruction with use of a circular external fixator and an intramedullary nail. The combined technique. J Bone Joint Surg Am. 2007;89:2218–24. doi: 10.2106/JBJS.F.01579. [DOI] [PubMed] [Google Scholar]
- 5.Rogers MJ, McFadyen I, Livingstone JA, Monsell F, Jackson M, Atkins RM. Computer hexapod assisted orthopaedic surgery (CHAOS) in the correction of long bone fracture and deformity. J Orthop Trauma. 2007;21:337–42. doi: 10.1097/BOT.0b013e3180463103. [DOI] [PubMed] [Google Scholar]
- 6.Kocaoglu M, Bilen FE. Fixator-assisted nailing for correction of long bone deformities. Oper Tech Orthop. 2011;21:163–73. [Google Scholar]
- 7.Bar-On E, Becker T, Katz K, Velkes S, Salai M, Weigl DM. Corrective lower limb osteotomies in children using temporary external fixation and percutaneous locking plates. J Child Orthop. 2009;3:137–43. doi: 10.1007/s11832-009-0165-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rozbruch SR. Fixator-assisted plating of limb deformities. Oper Tech Orthop. 2011;21:174–9. [Google Scholar]
- 9.Eidelman M, Keren Y, Norman D. Correction of distal femoral valgus deformities in adolescents and young adults using minimally invasive fixator-assisted locking plating (FALP) J Pediatr Orthop B. 2012;21:558–62. doi: 10.1097/BPB.0b013e328358f884. [DOI] [PubMed] [Google Scholar]
- 10.Paley D. 1st ed. New York: Springer; 2002. Principles of deformity correction; pp. 31–60. [Google Scholar]
- 11.Ruwe PA, Gage JR, Ozonoff MB, DeLuca PA. Clinical determination of femoral anteversion. A comparison with established techniques. J Bone Joint Surg Am. 1992;74:820–30. [PubMed] [Google Scholar]
- 12.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425–65. [PubMed] [Google Scholar]
- 13.Paley D. 1st ed. New York: Springer; 2002. Principles of deformity correction; pp. 1–18. [Google Scholar]
- 14.Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10:585–608. [PubMed] [Google Scholar]
- 15.Paley D. 1st ed. New York: Springer; 2002. Principles of deformity correction; pp. 99–154. [Google Scholar]
- 16.Paley D. 1st ed. New York: Springer; 2002. Principles of deformity correction; pp. 175–94. [Google Scholar]
- 17.Wang JW, Hsu CC. Distal femoral varus osteotomy for osteoarthritis of the knee. J Bone Joint Surg Am. 2005;87:127–33. doi: 10.2106/JBJS.C.01559. [DOI] [PubMed] [Google Scholar]
- 18.Rozbruch SR, Segal K, Ilizarov S, Fragomen AT, Ilizarov G. Does the Taylor Spatial Frame accurately correct tibial deformities? Clin Orthop Relat Res. 2009;468:1352–61. doi: 10.1007/s11999-009-1161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Slawski DP, Schoenecker PL, Rich MM. Peroneal nerve injury as a complication of pediatric tibial osteotomies: A review of 255 osteotomies. J Pediatr Orthop. 1994;14:166–72. doi: 10.1097/01241398-199403000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Smith WR, Ziran BH, Anglen JO, Stahel PF. Locking plates: Tips and tricks. J Bone Joint Surg Am. 2007;89:2298–307. doi: 10.2106/00004623-200710000-00028. [DOI] [PubMed] [Google Scholar]


