Abstract
Background:
In most classifications of tibial plateau fractures, including one used most widely-Schatzker classification, fractures are described as a combination of medial and lateral condyle, primarily in the sagittal plane. Coronal component of these fractures, affecting the posterior tibial condyle is now well recognized. What is not described is anterior coronal component of the fracture, what we are calling “anterior tibial condyle fracture”. These fractures are often missed on routine antero-posterior and lateral knee X-rays due to an overlap between the fracture and the normal bone.
Materials and Methods:
Eight cases of anterior tibial condyle fractures with posterior subluxation of the tibia, six of which were missed by the initial surgeon and two referred to us early, are described. Two of the six late cases and both the early ones were operated. Reconstruction of the anterior condyle and posterior cruciate ligament reconstruction was done. Primary outcome measures such as union of the fracture, residual flexion deformity, range of motion and stability were studied at the end of 6 months.
Results:
All operated fractures united. There was no posterior sag in any. In those presenting late and were operated, the flexion deformity got corrected in all (average from 15° to 0°) and mean flexion achieved was 100° (range: 80-120°). In those presenting early and were operated, there was no flexion deformity at 6 months and a mean flexion achieved was 115° (range: 100-130°). None of the operated patients had instability.
Conclusion:
This article attempts to highlight that this injury is often missed. They should be suspected, diagnosed early and treated by reconstruction of anterior condyle, posterior cruciate ligament reconstruction.
Keywords: Anterior tibial condyle fracture, posterior subluxation tibia, tibial plateau fracture
MeSH terms: Fracture, tibial fractures, cruciate ligament
INTRODUCTION
Tibial plateau fractures are commonly described as a combination of fractures affecting medial, lateral or both condyles in the sagittal plane.1 Fractures of the posterior condyle of the tibia have been described in the literature,2,3 but we did not come across a description of anterior tibial condyle fracture on an extensive search of English literature.
We define anterior tibial condyle fractures as those affecting anterior one-third of the medial condyle, extending to a variable degree to the lateral side [Figure 1]. These are associated with variable degree of posterior cruciate ligament (PCL) injury. The importance of reporting this injury lies in the fact that it is likely to be missed by the initial treating doctor, as has happened in six out of eight cases in this series. Delay in treatment results in fixed posterior subluxation of the knee, making it technically difficult to treat at a later date. Persistent posterior subluxation results in early joint degeneration. We have described our technique of treating this injury.
Figure 1.
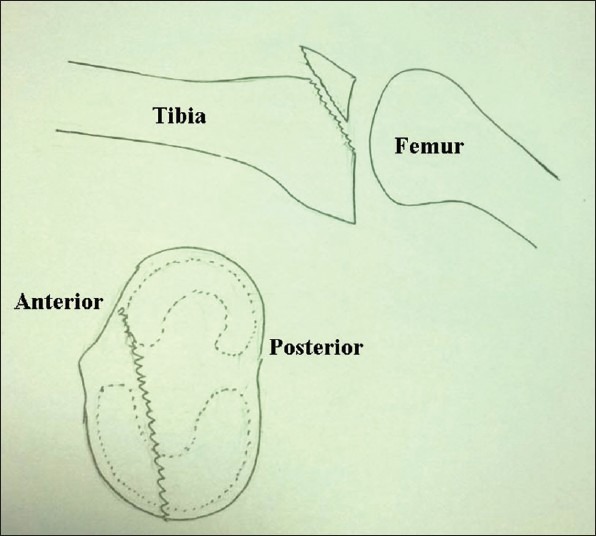
A line diagram showing anterior tibial condyle fracture
MATERIALS AND METHODS
We are reporting a total of eight cases, six presenting late (between 3 and 7 months) and two referred to us early (within 1 week, range: 2-6 days). They were in the age group of 21-45 years (mean 35 years). All patients had sustained the injury in road traffic accidents, the exact mechanism of injury could not be ascertained.
In all the cases presenting late, the fracture was missed by the initial treating doctor and they were treated as “soft-tissue injury”. All patients were treated for 3-6 weeks with immobilization in a plaster of Paris cast, followed by physiotherapy. They presented to us when they did not get desired results. They had either deformity or restriction of movements or both. A detailed clinical evaluation was done to record range of motion (ROM), deformity and stability. All patients had mild effusion with a posterior step off and posterior sag. Posterior subluxation was passively completely correctable in one and to a variable extent in others. They all had a flexion deformity in the range of 10-30°, with terminal loss of flexion of 30-40°. Two of the patients had common peroneal nerve palsy. The X-ray showed fracture of the anterior condyle of tibia with subtle posterior subluxation. X-rays and clinical picture of a representative case is as shown in Figure 2. Only 2 of the 6 patients in this late group accepted surgery. In one, the posterior subluxation was correctable whereas in the other, initial surgical mobilization of the tibial plateau was done from posteromedial approach to correct fixed posterior subluxation. Once the posterior subluxation was corrected, it was held in place with PCL reconstruction using hamstring graft. It was observed that with PCL reconstruction alone, the femoral condyle had a tendency to slide into the depressed malunited anterior tibial condyle. Hence, anterior tibial condyle was lifted by an open wedge osteotomy from front, stabilized by an osteochondral graft and a radius T-buttress plate anteriorly [Figure 3]. This improved the anteroposterior (AP) stability peroperatively. The patients were kept nonweight bearing for 4 weeks, with ROM exercises commencing on day 1. After 4 weeks, the patients were allowed to partially weight bear and full weight bear at the end of 12 weeks.
Figure 2.

Clinical photographs (a and b) showing posterior subluxation of tibia and x-rays knee joint anteroposterior and lateral views (c) showing anterior tibial plateau fracture of a typical case, presenting late
Figure 3.
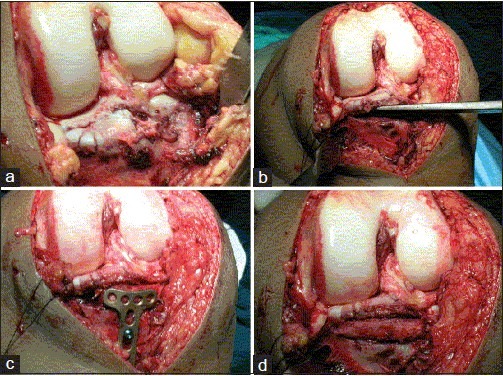
Intraoperative photographs showing (a) depression of anterior condyle (b) osteotomy to elevate the depressed condyle (c) insertion of cortico cancellous graft (d) buttressing the graft with plate
Two other cases who presented early (within the 1st week of injury) had hemarthrosis and the tibia was subluxated posteriorly. X-ray showed an anterior condyle fracture with posterior subluxation of the tibia. On opening the joint, we noticed that the femoral condyle was dipping into the depression caused by the depressed anterior tibial condyle. We did reconstruction of the anterior tibial condyle from front using the technique described above and PCL reconstruction. The fracture healed well and the subluxation was reduced.
The primary outcome measures of union of the fracture, deformity, ROM and stability were studied at the end of 6 months. Secondarily the complications were studied as well as the presence or absence of posterior step off. We also made note of any operative/nonoperative procedures such as manipulation under anesthesia, that were done on the patients.
RESULTS
The four patients who did not get operated (late un-operated group) continued to have flexion deformity of 20° (range 15-25°) and range of flexion of average 69° (range 60-80°). The common peroneal nerve injury in one of these four cases had not improved at the end of 6 months. All the fractures united with a posterior step off.
In the group that presented late and were operated upon (late operated group), the flexion deformity got corrected in all of the cases (from an average of 15-0°). Mean flexion achieved was 100° (range 80-120°) and there was no posterior sag. The common peroneal nerve palsy in one of the case in this group recovered partially in 6 months. One case needed manipulation under anesthesia 4 weeks after the surgery. Both cases showed union at the fracture site at the end of 6 months [Figure 4].
Figure 4.

(a) clinical photographs of a patient presented late showing posterior sagging of tibia (b) X-rays of knee joint anteroposterior and lateral views showing tibial plateau injury (c) Sagittal MRI of same patient showing anterior tibial plateau injury (d) immediate postoperative x-ray of knee joint anteroposterior and lateral views showing implant in situ with reduction achieved
In the group that presented early, there was no flexion deformity at the end of 6 months, the mean flexion achieved was of 115° (range: 100-130°). The knee was stable with no posterior sag and there was union at the fracture site at the end of 6 months. There were no complications.
DISCUSSION
The purpose of this paper is to report a hitherto not described injury - anterior tibial condyle fracture with posterior subluxation of tibia. We did not come across any reference to such an injury on extensive search of English literature. It seems that this fracture is missed often as is clear from our series where six out of eight cases were missed by the treating doctors.
This also raises a question on relevance of commonly used Schatzker's classification, which is based on considering the tibial plateau fracture a combination of medial and lateral pillars.1 Not much attention has been paid to the coronal component of these injuries. Moore identified that the medial condyle fracture is often posteromedial and not purely medial, for which they recommended posteromedial plating.4 There have been reports where the fracture is in the coronal plane alone, involving only the posterior part of the medial condyle.3 In such cases, the fractured condyle is displaced posteriorly, carrying with it the medial femoral condyle. Such fractures can be missed on AP X-ray, but can be diagnosed in lateral X-rays. Coronal bicondylar tibial plateau fracture involving the posterior condyles have also been reported.3 The relevance of recognizing the coronal component of these fractures lies in the fact that the buttress plate has to be put from behind.5
Lately, Luo et al. proposed, based on computed tomography (CT) evaluation, the concept of three-column in the treatment of tibial condyle fractures, where three columns were medial, lateral and posterior.6
It seems that inspite of such extensive work on tibial plateau fractures, the anterior condyle fractures have escaped attention. An anterior rim fracture detected on magnetic resonance imaging has been reported in radiology literature.7,8 This was only thought to be a useful indicator of associated PCL and posterolateral corner injuries. The anterior tibial plateau fractures reported by us are not merely that of the rim, but involve the anterior third of the tibial condyle. This fracture contributes along with PCL tear, to posterior subluxation of the knee. Whereas reconstruction of PCL would be required to keep the knee aligned in the sagittal plane, reconstruction of the anterior depressed tibial plateau fracture is mandatory not to let the femoral condyle slide into it. In our opinion, unless anterior bony stability is restored, an attempt at standalone PCL reconstruction may fail. We suspect that this fracture may be responsible for failure of PCL reconstruction in some cases where this fracture is co-existent and is not addressed too.
We highlight the importance of early diagnosis of these fractures as they were missed in six out of eight cases in this series. This happened apparently as these are difficult to see on AP and lateral X-rays due to overlap. In the absence of routine use of CT scan in treatment of these fractures, the only clue in plain X-rays is subtle posterior subluxation of the tibia. Once suspected, a CT will show the extent of injury clearly.
Early diagnosis and early surgery is critical in these cases as delay in treatment results in the tibia remaining in a posteriorly subluxated position. This causes significant deformity and limitation of knee movements. There are long term implications of leaving the knee subluxated as it will cause abnormal loading on the tibiofemoral and patella-femoral joint resulting in early degeneration. Attempt at late surgery is technically more demanding as one has to dissect behind the tibial condyles to mobilize the tibia. It is required to stabilize the anterior coronal fracture with an anterior plate, similar to posterior fixation of coronal fractures in the posterior plane. This was done in all the four cases using a radius plate.
We conclude that recognition of coronal component of the tibial condyle fracture, commonly posterior, but sometimes anterior, is important. Awareness that such an injury exists and suspecting it in a case with posterior subluxation of tibia, is the key to early diagnosis. Once diagnosed, an evaluation by CT scan and reconstruction of the depressed anterior condyle from front, in addition to PCL reconstruction is required.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968-1975. Clin Orthop Relat Res. 1979;138:94–104. [PubMed] [Google Scholar]
- 2.Bhattacharyya T, McCarty LP, 3rd, Harris MB, Morrison SM, Wixted JJ, Vrahas MS, et al. The posterior shearing tibial plateau fracture: Treatment and results via a posterior approach. J Orthop Trauma. 2005;19:305–10. [PubMed] [Google Scholar]
- 3.Carlson DA. Posterior bicondylar tibial plateau fractures. J Orthop Trauma. 2005;19:73–8. doi: 10.1097/00005131-200502000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Moore TM. Fracture-Dislocation of the knee. Clin Orthop Relat Res. 1981;156:128–40. [PubMed] [Google Scholar]
- 5.Lobenhoffer P, Gerich T, Bertram T, Lattermann C, Pohlemann T, Tscheme H. Particular posteromedial and posterolateral approaches for the treatment of tibial head fractures. Unfallchirurg. 1997;100:957–67. doi: 10.1007/s001130050218. [DOI] [PubMed] [Google Scholar]
- 6.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24:683–92. doi: 10.1097/BOT.0b013e3181d436f3. [DOI] [PubMed] [Google Scholar]
- 7.Bennett DL, George MJ, El-Khoury GY, Stanley MD, Sundaram M. Anterior rim tibial plateau fractures and posterolateral corner knee injury. Emerg Radiol. 2003;10:76–83. doi: 10.1007/s10140-003-0298-z. [DOI] [PubMed] [Google Scholar]
- 8.Cohen AP, King D, Gibbon AJ. Impingement fracture of the anteromedial tibial margin: A radiographic sign of combined posterolateral complex and posterior cruciate ligament disruption. Skeletal Radiol. 2001;30:114–6. doi: 10.1007/s002560000309. [DOI] [PubMed] [Google Scholar]


