Abstract
This article describes the development, implementation, evaluation framework, and initial outcomes of a unique campus–community training initiative for community-based participatory research (CBPR). The South Carolina Clinical & Translational Research Center for Community Health Partnerships, which functions as the institution’s Clinical Translational and Science Award Community Engagement Program, leads the training initiative known as the Community Engaged Scholars Program (CES-P). The CES-P provides simultaneous training to CBPR teams, with each team consisting of at least one community partner and one academic partner. Program elements include 12 months of monthly interactive group sessions, mentorship with apprenticeship opportunities, and funding for a CBPR pilot project. A modified RE-AIM (Reach, Effectiveness, Adoption, Implementation, Maintenance) framework guides the process, impact, and outcome evaluation plan. Lessons learned include challenges of group instruction with varying levels of readiness among the CBPR partners, navigating the institutional review board process with community co-investigators, and finding appropriate academic investigators to match community research interests. Future directions are recommended for this promising and unique dyadic training of academic and community partners.
Keywords: community-based participatory research, health research, partnerships/coalitions, program planning and evaluation, training, college/community partnerships, university/college health
INTRODUCTION
Community-based participatory research (CBPR) is an approach to scientific inquiry that optimizes community engagement with partnerships between communities and academic organizations (Buchanan, Miller, & Wallerstein, 2007; Israel, Schulz, Parker, & Becker, 1998). CBPR strives for maximum feasible community engagement on a continuum, including identifying issues to be addressed, design and delivery of interventions, collection and evaluation of data, and dissemination of results (Minkler & Wallerstein, 2003; Viswanathan et al., 2004; Wallerstein & Duran, 2003). In an ideal CBPR model, academic researchers and community members work together as equal partners on issues relevant to the community, facilitate a transfer of expertise between partners, and generate new knowledge (Israel et al., 1998; Israel et al., 2003). An advantage of CBPR is that the processes are bidirectional, allowing researchers to use scientific knowledge of an identified health problem facing the community, and for the community to use their expertise of the cultural and social contexts of the health issue and potential solutions that may work locally (Andrews, Tingen, et al., 2012). More important, with an engaged and equitable partnership, research can contribute to decreasing local health inequities among disempowered communities and help build capacity for social change (Minkler & Wallerstein, 2003).
However, partnerships between communities and academic organizations often struggle with incongruent or inadequate CBPR knowledge and skills, resources, and leadership to support equitable mastery and ownership of research processes and products (Israel et al., 2003). Traditionally, there are disparities in the amount of CBPR training and resources that community members receive, as compared to their university member counterparts (Reardon, 1998). CBPR partnerships often require negotiation and compromise, which depends on dialogue and development of trust-based relationships (Martinez et al., 2012). Many CBPR partnerships are catalyzed by a new grant or funding opportunity with immediate deadlines and fail to lay the foundation for the transparent dialogue and trust that are needed for the CBPR partnership and product sustainability (Andrews, Newman, Meadows, Cox, & Bunting, 2012).
In response to these and other identified challenges, several institutions and organizations have developed training curricula designed to facilitate community members’ and academic researchers’ engagement and knowledge with CBPR. Although available training curricula share the common goal of providing instruction on the processes of CBPR, implementation strategies vary among programs. For example, most available CBPR training programs across the United States are targeted to either academic or community partners in separate courses or sessions (Allen, Culhane-Pera, Pergament, & Call, 2010; Jones & Wells, 2007; Rosenthal et al., 2009; University of North Carolina, n.d.). The well-established Community–Campus Partnerships for Health (CCPH) offers a web-based CBPR curriculum (CCPH, 2003) that is targeted to both audiences. The only known simultaneous intensive, face-to-face training programs for community and academic partner dyads have been limited to 3- to 5-day institutes or workshops (National Institutes of Health’s Office of Behavioral and Social Sciences Research, 2009).
The purpose of this article is to describe the development and implementation of the South Carolina Clinical & Translational Research’s Center for Community Health Partnerships (SCTR/CCHP) training program for dyadic teams of community and academic partners to build capacity for CBPR simultaneously. Contributing factors for the development of the Community Engaged Scholars Program (CES-P), a program description overview, and the CES-P implementation and evaluation framework are provided. We share lessons learned from our experiences and recommendations for future directions for dyadic CBPR partnership training.
BACKGROUND: PROGRAM HISTORY AND DEVELOPMENT
Formative Assessment
The SCTR/CCHP functions as the Community Engagement Core for the institution’s Clinical and Translational Science Award with a central mission to lead innovative, system-wide efforts to strengthen capacity for collaborative research relationships among academic investigators and community members, community-based clinicians, and local health care organizations. With a goal to implement a new CBPR training program at the university, a team of community and academic partners from the SCTR/CCHP participated in an intensive charrette training sponsored by the Campus Community Partnerships for Health in Chapel Hill, North Carolina in May 2008. The four-person team included representatives from the University President’s Office, College of Nursing, Cancer Center, and a community-based civil rights organization.
As part of the charette training session, the team completed a SWOT analysis (strengths, weaknesses, opportunities, and threats) to inform the development and components of a new CBPR training program offered by the university. Perceived strengths included a history of institutional commitment (i.e., hiring CBPR faculty, resource and time support) to community partnerships and projects, as well as increasing faculty interest and enthusiasm for institutionalizing a commitment to both the processes and products of CBPR (Magwood et al., in press). An assessment of weaknesses revealed that many academic investigators lacked awareness of CBPR models and principles (Israel et al., 1998; Israel et al., 2003; Minkler & Wallerstein, 2003) and conducted community “placed” or “based” research, instead of the preferred community engaged research. Research conducted in the local community typically had been submitted by the academic investigator who developed the grants, led the research implementation, and received the majority of funding. Community and academic partners identified both the need for and benefits of a mechanism to increase capacity among both academic and community members to address salient health issues in the community. Gaps in knowledge existed in how to promote partnership equity, how to optimize all partners’ contributions, and how to effectively operationalize CBPR principles and processes into action and results. The perceived opportunity, then, evolved with the development of an innovative CBPR training program for academic and community members that would address these needs.
Following the SWOT analysis, SCTR/CCHP staff conducted a comprehensive review of existing programs and curricula related to education and training on community-engaged research. Staff reviewed models for program structure and content and evaluated in concordance with our local needs. The SCTR/CCHP staff presented these data, along with the results of the SWOT analysis, to the SCTR/CCHP scientific and community advisory boards (see Newman et al., 2011 for further description of the SCTR/CCHP community advisory board). Both boards provided input and endorsed the design for the proposed CES-P to meet the needs of all partners and to produce long-term benefit to the community.
Program Overview
The 18-month CES-P provides interactive training, pilot funds, and apprentice-style mentorship for teams consisting of a community and academic partner who have interests in CBPR. At the time of writing, three cohorts consisting of 14 CBPR teams (with each team consisting of at least one community partner and one academic partner) have completed the CES-P.
The distinguishing factor of the CES-P is the focus on the dyad of community and academic partners. Rather than providing training to only the community or only the academic partner, the team is the focal entity for the CES-P from the initial submission of the CES-P application through completion of the program. This simultaneous training design promotes shared learning and maximizes opportunities for building capacity of both partners and the overall partnership. The goal of the training is to build a cadre of community–academic partnerships that are successful in securing extramural funding to conduct research and program initiatives that are meaningful, useful, and influence the health of participating communities. After successfully completing the CES-P, participating team members are expected to meet the following competencies:
understand the concepts and components of CBPR,
assess and leverage domains and key indicators of CBPR readiness for the partnership and potential research project,
integrate CBPR principles in grant proposals and research implementation,
communicate with audiences in both academic and community settings about CBPR principles and components,
implement a pilot CBPR initiative, and
build foundations for sustainability of the partnership and CBPR products.
PROGRAM IMPLEMENTATION
Marketing and Recruitment
We use multiple marketing strategies to reach potential community and academic partners. We release the call for applications on several established listservs with both academic and community audiences. In addition, we send information to community engagement “champions” within the academic departments on campus and various community leaders. Preapplication information sessions are held to provide further details about the CES-P to interested community members and faculty. Following the first cohort of scholars, we recognized that word of mouth is one of the most important sources of marketing and recruitment for the CES-P.
Although most of our team applicants have a partnership history, individuals (either from the community or campus) often have interest in the program and request assistance in identifying a potential partner match with mutual interests. In these instances, the SCTR/CCHP staff attempt to identify and introduce potential partners prior to the application process.
Selection Process
The process of selecting qualified teams for the CES-P involves multiple steps and stakeholders. A team is defined as consisting of at least one community and one academic partner meeting the following criteria:
Community partner: an individual(s) who maintains a primary affiliation, whether employed or volunteer, with a community organization. For the purpose of this program, community organization is defined as an organization that (a) has a documented interest in improving the health of the relevant community (e.g., a mission statement) and (b) has a history of serving the health needs and interests of the relevant community. These organizations may include, but are not limited to community practices, public schools, community-based organizations, faith-based organizations, and/or advocacy groups.
Academic partner: an individual(s) with a faculty appointment who has training and experience in research methods.
Additional inclusion criteria for participants are (a) ability to attend monthly didactic sessions at the academic medical center, (b) commitment to future research/initiatives as a team, and (c) release of time from employment to participate in the program.
The call for applications remains open for 3 months during which time applications are accepted from teams that meet inclusion criteria. Only one application is submitted per team. Should a community or academic investigator not have an identified or established partner, SCTR/CCHP staff use existing networks to facilitate an appropriate match. The application requires teams to respond to questions regarding partnership history, ability to carry out a project together, health topic/focus, and experience working with the project topic. Teams are asked to propose short-term goals related to the pilot project they plan to complete during the program, as well as long-term goals related to the partnership. These goals must specify the processes of partnership planned for the research and a commitment to working together on completion of the program.
In addition to the application, partners must complete a memorandum of understanding (MOU) confirming their commitment to the partnership team, the participatory research process, and the multiple components of the CES-P. The MOU is a common requirement of CBPR projects to ensure partnership commitment and success (CCPH, 2011; Newman et al., 2011). To ensure a release of time to fully participate in the CES-P, a supervisor consent form is required for all partners. This document clarifies to supervisors the time commitment, expectations, and funding regulations for CES-P participants. Thus, the application reflects the vision, experience, and commitment of the partnership team to address an identified need through CBPR.
A panel of both community and academic professionals conduct blinded reviews of all applications to provide a variety of perspectives and comprehensive assessment of applications. At least two community and two academic reviewers evaluate each application and score according to the criteria provided in Table 1. The SCTR/CCHP leadership makes final decisions on team selections based on the final scores. We limit cohorts to five to six teams per year because of funding restrictions and the desire to produce a cohesive group that provides a social network for creativity and support throughout the program.
TABLE 1.
Review Criteria for Community Engaged Scholars Program (CES-P) Applications
|
Program Design
The CES-P consists of three primary components: interactive training, apprentice-style mentorship, and pilot project implementation. Together these components provide comprehensive training in and application of the principles and processes of CBPR, while building partnership capacity for future success.
1. Interactive training
The training portion of the program is delivered in a group format in monthly, 3-hour sessions over a 12-month period. The methods used within each session are verbal and visual presentations, case studies, provocative partner questions, shared learning experiences, and open discussions. The date and time of the sessions are agreed on by all teams and set at the beginning of the program.
The early months of the program are dedicated to building partnership capacity by assessing partnership readiness, establishing operating guidelines, and setting a vision for the partnership. This training is enhanced with the CBPR Partnership Readiness Toolkit that is designed as a qualitative assessment promoting equal voice and transparent, bi-directional discussions among all partners (Andrews, Cox, Newman, & Meadows, 2011; Andrews, Newman, et al., 2012). The toolkit is formatted to direct individual partner assessments, followed by team assessments, discussions, and action plans to optimize the partnership goodness of fit, capacity, and operations to conduct CBPR. The experienced academic and community co-investigators who developed the toolkit lead these initial training sessions.
Subsequent sessions focus on the tenets of CBPR, including community assessment, implementation, evaluation and sustainability. Guest speakers with CBPR expertise from multiple academic and community organizations co-lead these sessions. While building knowledge, the monthly sessions also provide time for co-learning among the teams to share experiences and lessons learned. Table 2 describes the curriculum objectives for the monthly didactic sessions.
TABLE 2.
Training Sessions and Objectives
| Session Topic | Curriculum Objectives |
|---|---|
| History and definitions of community- | • Understand the origins and history of CBPR |
| based participatory research (CBPR) | • Understand the guiding principles of CBPR |
| Partnership Readiness I | • Describe the basics of partnership readiness and capacity |
| • Are We Ready? Toolkit Part I | |
| Partnership Readiness II | • Are We Ready? Toolkit Part II |
| CBPR panel | • Panel of CBPR teams for effective CBPR strategies, authentic |
| partnership, and lessons learned | |
| Community assessment and problem | • Describe components of community assessment |
| identification | • Understand community asset mapping |
| • Identify tools and methods for community assessment | |
| • Highlight selected methods in detail based on group projects | |
| Data collection and analysis | • Understand and differentiate between methods for data collection and |
| measurement | |
| • Identify methods for data analysis | |
| Evaluation Part I | • Provide overview of process evaluation |
| • Describe methods for process evaluation | |
| Evaluation Part II | • Provide overview of outcome/impact evaluation |
| • Describe methods for outcome/impact evaluation | |
| Academic–community partnerships | • Varied CBPR teams presentation |
| panel | |
| Dissemination and communication | • Identify key stakeholders for project dissemination |
| • Identify various modes of dissemination | |
| • Identify policy considerations for CBPR projects | |
| Sustainability for CBPR partnerships | • Understand and assess the effectiveness of the CBPR partnership |
| and projects | • Guidelines for assessing partnership research |
| Final session | • Group presentations |
2. Apprentice-style mentorship
Teams entering the CES-P have a broad range of research and partnership experience. The mentorship portion of the CES-P is intended to help guide partnerships through anticipated challenges and to assist with addressing gaps in knowledge and expertise. At the start of the program, each team identifies an experienced CBPR mentor that compliments and enhances the partnership. This mentor may be from either the academic or community sector, or both. Teams have the opportunity for apprenticeship learning with the mentor’s active CBPR study. For example, the CES-P team may wish to participate in the mentor’s CBPR study investigators meeting, attend mentor’s data collection session (i.e., focus group or survey administration), assist with a dissemination project, or attend a local policy session with the mentor.
3. Pilot projects
A substantial portion of the CES-P is the development and implementation of a pilot CBPR project for each team. While teams identify preliminary ideas for the project on the application, they develop the full pilot proposal over the first 6 months of the program, allowing time to build their partnership and further articulate project and partnership goals. The pilot project is then implemented in the final 12 months of the 18-month training program. The pilot proposal reflects sections found on typical federal grant applications and provides experience for the team with grantsmanship processes. CES-P staff review the proposals on measures related to goals, objectives, participatory methods, budget, evaluation, and sustainability. The team members perform a self-assessment of Green et al.’s (2003) Guidelines for Participatory Research to assess their incorporation of CBPR principles in the pilot grant. At the time the proposals are due, they must also be submitted to the institutional review board (IRB). Each team is awarded up to $10,000 for the pilot project, with the first half disbursed following IRB approval and the second half on adequate completion of a midterm progress summary. Adhering to the power sharing principles of CBPR, either the academic or community partner may accept the funds for the team. A midterm progress report (e.g., objectives met, budget expenditures, and plans for next steps) is due 6 months after proposal submission, and the final project summary is due after 12 months.
PROGRAM EVALUATION
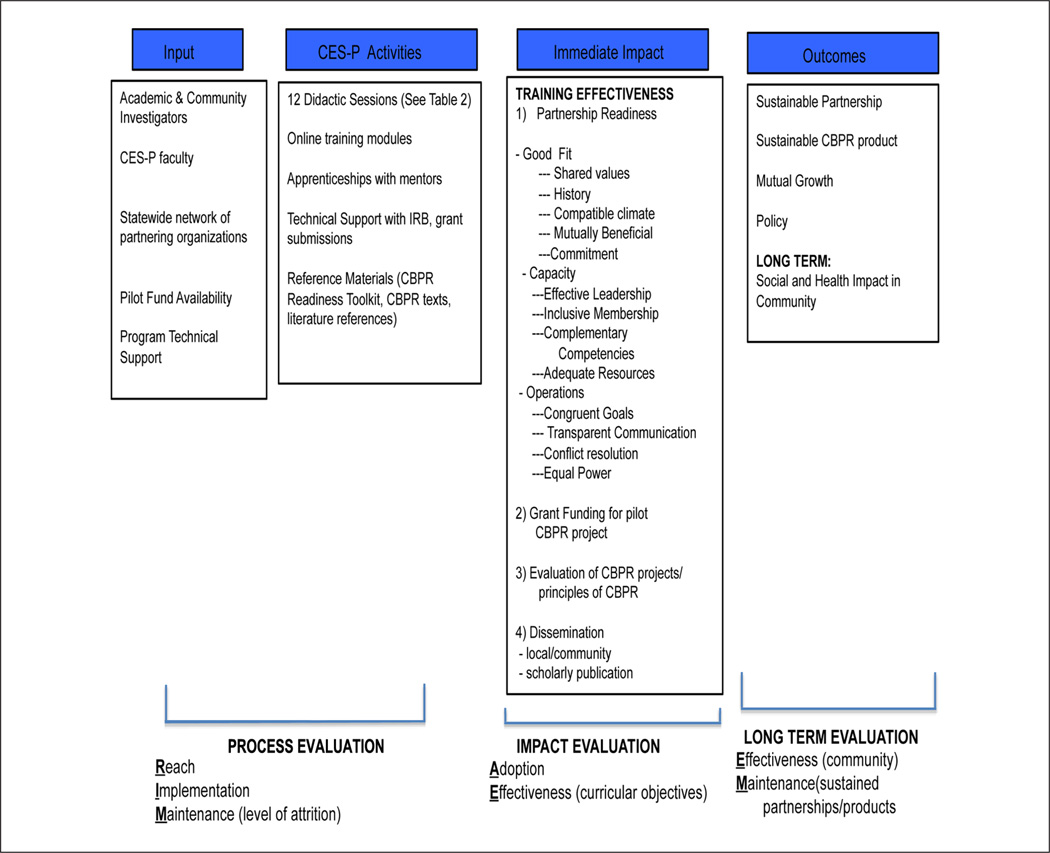
Evaluation of the CES-P is ongoing, incorporating process, impact, outcome, and partnership measures. We have continued to improve the evaluation process over time, and now use a modified RE-AIM (Reach, Effectiveness, Adoption, Implementation, Maintenance) framework (Glasgow, Klesges, Dzewaltowski, Estabrooks, & Vogt, 2006) to guide our evaluation. A logic model (Fielden et al., 2007; Sanchez, Carrillo, & Wallerstein, 2011; Sandoval et al., 2012; Scarinci, Johnson, Hardy, Marron, & Partridge, 2009) in Figure 1 summarizes the overall plan.
Reach: To evaluate reach of the CES-P, we monitor (a) number/types of participants that inquire about the program (via phone, e-mail, and/or information sessions) and their representative organizations; (b) number/types of participants that apply for the program and their representative organizations; and (c) types of participants that are selected, including organizations, areas of health interest, experience in CBPR, and previous history/ experience of the CBPR partnerships.
Effectiveness: To evaluate effectiveness of the CES-P, we use standardized evaluation tools for each training session (content, expertise of speakers, usefulness, etc.), a midterm evaluation, and an overall evaluation of the program (knowledge, attitudes, behaviors, usefulness, and satisfaction). Following program completion, we track teams’ progress with their partnership by documenting grant submissions, grant funding, and dissemination activities (both local and scholarly presentations, media, and publications). Although currently we assess CBPR Partnership Readiness (Andrews et al., 2011; Andrews, Newman, et al., 2012) with qualitative methods (focus groups and interviews), we are in the process of developing a quantitative scale for pretest and posttest measures.
Adoption: In the case of the CES-P, “adoption” is reflected in measures of impact effectiveness at the dyad level. We use Green et al.’s (2003) Guidelines for Participatory Research to review the CES-P teams’ pilot proposals. Second, the CES-P teams perform a self-assessment using a 27-item instrument developed by Braun et al. (2012) to assess operationalization of the nine CBPR principles in their partnership and CBPR product.
Implementation: Delivery of the CES-P components is evaluated using a program fidelity checklist, including training sessions, attendance, use of mentors, apprenticeship activities, and pilot grant implementation. At the end of the cohort session, we conduct interviews with CES-P faculty, partners, and participants on successes, challenges, barriers to the implementation, and recommendations for sustainability.
Maintenance: Maintenance is reflected at two levels: the dyad level and at the SCTR/CCHP program level. We monitor if adherence with the program components occurs over time and if the partners maintain their collaborative working relationship. We continue to request evaluative data from all our cohorts annually to track progress on intermediate- and long-term outcomes.
FIGURE 1. Logic Model Guided by RE-AIM Framework.
NOTE: RE-AIM = Reach, Effectiveness, Adoption, Implementation, Maintenance; CES-P = Community Engaged Scholars Program; CBPR = community-based participatory research.
Summary of Outcomes
The first 14 teams from the first three CES-P cohorts have produced relevant results that demonstrate effective strategies and future potential. Table 3 provides a summary of the teams and targeted health issues. Products of the CES-P teams to date have included 12 local/community presentations, 22 state/national presentations, 6 international presentations, 4 coauthored publications, 12 extramural grant submissions, and 8 funded extramural awards, including 2 from the National Institutes of Health and 1 from the Patient Centered Outcomes Research Institute.
TABLE 3.
Pilot Community Engaged Scholars Program (CES-P) Teams and Target Health Issues
| Community Partner | Academic Partner | Target Health Issue |
|---|---|---|
| Nonprofit (DisAbility Resource Center) |
Nursing | Persons with disabilities (needs assessment and development of peer navigator intervention) |
| Government Municipality (town of Hollywood, SC) |
Dental Medicine | Oral health needs of Gullah population and development of oral health navigator intervention |
| Federally Qualified Health Center (FQHC) |
Medicine | Prenatal care and outcomes of low–socioeconomic status women |
| Nonprofit (Pattison’s Academy) | Health Professions | School-based intervention for children with special care needs |
| Nonprofit (United Way) | Nursing | Adolescent suicide assessment and prevention intervention planning |
| Nonprofit (DAE Academy) and Chas Co Public Schools |
Medicine | Childhood obesity intervention in public elementary schools |
| Nonprofit (Low Country AIDS Association) and VA Outpatient Clinic |
Nursing | Community-based HIV screening and treatment programs for veterans |
| FQHC | Medicine | Missed appointments for patients with chronic diseases (hypertension, diabetes) |
| Nonprofit (Association of Personal Care Homes) |
Nursing | Nutrition in dementia patients and testing caregiver feeding intervention |
| Faith based (AME Churches) | Medicine | Cancer outreach programs delivered via churches |
| Nonprofit (AIDS organization) | Medicine | Transitional care program for incarcerated HIV+ women exiting prison |
| Nonprofit (Alpha 1 Community) | Nursing | Assess and prioritize sociopolitical needs of Alpha-1 community |
| Local Environmental Justice Organization |
Medicine | Identifying and addressing community priorities for environmental toxin exposures |
| Local nonprofit (Palmetto Project) |
Nursing | Integrated approach to diabetes management at food bank sites |
DISCUSSION
The CES-P uses multiple methods for training the dyad of community and academic partners to successfully conduct research. Interactive training sessions grounded in CBPR principles (Israel et al., 1998; Israel et al., 2003; Minkler & Wallerstein, 2003), mentorship by experienced CBPR investigators, and resources for a pilot CBPR project have been found by our team, and others (Rosenthal et al., 2009) as important components for CBPR training programs. However, unlike other training programs, the CES-P provides 18 months of simultaneous training and support with a focus on the partnership dyad, versus separate training courses for academic and community partners. Established strategies based on CBPR principles for equal contribution, decision making, and power between partners (Israel et al., 1998; Israel et al., 2003; Minkler & Wallerstein, 2003) should not only be proposed for the research process but also with the training process. Simultaneous CBPR training in a group format provides the opportunities for partners to learn CBPR principles and approaches together along with a forum for sharing with other CBPR teams. As others have identified (Rosenthal et al., 2009), a forum to discuss group interactions and share experiences is important for training diverse participants. We have observed that these strategies promote community “voice” and empowerment of community co-investigators to negotiate transactions and assume equitable power in the dyadic relationships. The group interactions, networking transparent communication, and shared resources (especially funding) collectively aid in maximizing strengths of the partners to foster greater collaboration and mutual ownership of the processes and products of research, and to build capacity to strengthen current and future CBPR projects.
We have learned several valuable lessons in the development and implementation of the CES-P that provide direction for future programs. First, the training of multiple community–academic teams simultaneously can present challenges. Some teams are new partnerships catalyzed by the application process, whereas others have worked together for several years with previous pilot data. The history, duration, and experiences of the partnerships contribute to varying degrees of readiness and training needs (Andrews, Newman, et al., 2012). Additionally, community and academic members often have different communication preferences, paces of work, and varied time commitment to the project. Use of the CBPR Partnership Readiness Toolkit (Andrews et al., 2011) during the first months of the program is necessary to address these issues. Additionally, adequate screening of all applicants and MOUs of accepted teams have been important to determine the presumed commitment of each partner during the training process and beyond, yet are not always predictive of actual commitment. Having experienced CBPR faculty who are flexible, can address diverse team needs, manage group interactions, and have opportunities and resources for apprentice learning have been critical for success of this training to date.
Like others, our teams have had challenges navigating the IRB process with CBPR studies at the university, especially with community members as co-investigators on the IRB application. Our SCTR/CCHP Co-Director now chairs an IRB group at our institution and has been instrumental in providing training to IRB administrators, faculty, and community partners on the IRB process for community-engaged research. Our Co-Director has worked with IRB administrators to implement a process to allow community partners access to the electronic IRB application and acknowledgement as a co– principal investigator, as well as instructional guidelines, templates, and algorithms to enhance the IRB navigation process. These efforts have shown promising early results and increased satisfaction by all stakeholders with this process.
Like other CBPR processes, flexibility has been essential from both the CES-P staff and participants. For example, one of the most recent cohort’s community partners are a virtual community organized by their rare health condition (alpha 1 deficiency), with CES-P team members across the United States. This prompted our staff to lead video-conferencing sessions to accommodate the CES-P participants. The staff and participants have embraced this use of technology, and other local participants who would have missed a session because of travel commitments, are now participating from distance sites when needed.
Over time, we have had more community interest in the program than academic interest, and on several occasions been unable to identify an appropriate academic match for a community partner. We have recognized the need to expand the reach of the program and to elicit other partners, such as the state’s Area Health Education Consortium, Historically Black Colleges and Universities, as well as community practices and organizations. We plan to expand our marketing across the state and to provide videoconferencing sessions with enhanced asynchronous online modules to provide additional accessibility for potential applicants. This may assist with increasing our pool to match partners and, ideally, to increase the network capacity to have a greater impact on state health outcomes.
CONCLUSION
There are various models for training community– academic teams to conduct CBPR. The comprehensive 18-month CES-P with 12 monthly interactive training sessions, mentorship with apprentice learning opportunities, and funds for a CBPR pilot project have yielded positive preliminary results with CBPR partnerships and products. Focusing on the dyadic partnership and simultaneous training of both types of partners—community and academic—seems a logical approach to meet the principles of CBPR. Dyadic training for busy partners with multiple roles has its challenges, yet has early promising outcomes as a potential model for CBPR training.
Acknowledgments
This research and development project was conducted by the Medical University of South Carolina and is made possible by a cooperative agreement that was awarded and administered by the U.S. Army Medical Research and Material Command (USAMRMC) and the Telemedicine & Advanced Technology Research Center (TATRC), Fort Detrick, Maryland 21702, under Contract Number: W81XWH-10–20–0057. This work was also supported by the South Carolina Clinical & Translational Research Institute, Medical University of South Carolina’s CTSA, NIH/NCRR Grant Number UL1RR029882 and NIH/NCATS UL1T R000062. The views, opinions and findings contained in this research are those of the Company/Laboratory/medical facility, etc., and do not necessarily reflect the views of the NIH, NCCR, or Department of Defense and should not be construed as an official DoD/Army policy unless so designated by other documentation.
REFERENCES
- Allen M, Culhane-Pera K, Pergament S, Call K. Facilitating research faculty participation in CBPR: Development of a model based on key informant interviews. Clinical and Translational Science. 2010;3:233–238. doi: 10.1111/j.1752-8062.2010.00231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews JO, Cox MJ, Newman SD, Meadows O. Development and evaluation of a toolkit to assess partnership readiness for community-based participatory research. Progress in Community Health Partnerships. 2011;5(2):183–188. doi: 10.1353/cpr.2011.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews JO, Newman SD, Meadows OM, Cox MJ, Bunting S. Partnership readiness for community-based participatory research. Health Education Research. 2012;27:555–571. doi: 10.1093/her/cyq050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews JO, Tingen MS, Jarriel SC, Caleb M, Simmons A, Brunson J, Hurman C. Application of a CBPR frame- work to inform a multi-level tobacco cessation intervention in public housing neighborhoods. American Journal of Community Psychology. 2012;50:129–140. doi: 10.1007/s10464-011-9482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun KL, Nguyen TT, Tanjasiri SP, Campbell J, Heiney SP, Brandt HM, Hébert JR. Operationalization of community based participatory research principles: Assessment of the National Cancer Institute’s Community Network Programs. American Journal of Public Health. 2012;102:1195–1203. doi: 10.2105/AJPH.2011.300304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan BR, Miller FG, Wallerstein NB. Ethical issues in community based participatory research: Balancing rigorous research with community participation in community intervention studies. Progress in Community Health Partnerships. 2007;1:153–160. doi: 10.1353/cpr.2007.0006. [DOI] [PubMed] [Google Scholar]
- Community-Campus Partnerships for Health. Developing and sustaining community–university partnerships for health research: Infrastructure requirements. National Institute of Health Report; 2003. Retrieved from www.ccph.info/ [Google Scholar]
- Community-Campus Partnerships for Health. MOUs/MOAs. 2011 Retrieved from http://depts.washington.edu/ccph/commbas.html#MOU.
- Fielden SJ, Rusch ML, Masinda MT, Sands J, Frankish J, Evoy B. Key considerations for logic model development in research partnerships: A Canadian case study. Evaluation and Program Planning. 2007;30:115–124. doi: 10.1016/j.evalprogplan.2007.01.002. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Klesges LM, Dzewaltowski DA, Estabrooks PA, Vogt TM. Evaluating the impact of health promotion programs: Using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Education Research. 2006;21:688–694. doi: 10.1093/her/cyl081. [DOI] [PubMed] [Google Scholar]
- Green LW, George AM, Daniel M, Frankish CJ, Herbert CP, Bowie WR, O’Neill M. Guidelines for participatory research in health promotion. In: Minkler M, Wallerstein N, editors. Community-research based participatory in health. San Francisco, CA: Jossey-Bass; 2003. pp. 419–428. [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Annual Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB, Allen AJ, Guzman R. Critical issues in developing and following community based participatory research principles. In: Minkler M, Wallerstein N, editors. Community based participatory research for health. San Francisco, CA: Jossey-Bass; 2003. pp. 53–76. [Google Scholar]
- Jones L, Wells K. Strategies for academic and clinician engagement in community partnered research. Journal of the American Medical Association. 2007;297:407–410. doi: 10.1001/jama.297.4.407. [DOI] [PubMed] [Google Scholar]
- Magwood G, Andrews JO, Zapka J, Cox M, Newman S, Stuart G. Institutionalization of community partnerships: Challenges for academic health centers. Journal of Health Care for the Poor and Underserved. doi: 10.1353/hpu.2012.0161. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez LS, Perea FC, Ursillo A, Weeks FH, Goldstein-Gelb W, Grugge D. A democratic university–community administrative body dedicated to expanding community-engaged research: The TUFTS Community Research Center (TCRC) Community Development. 2012 Advance online publication. doi:10.1080/ 15575330.2012.678873. [Google Scholar]
- Minkler M, Wallerstein N. Introduction to community-based participatory research. In: Minkler M, Wallerstein N, editors. Community-based participatory research for health. San Francisco, CA: Jossey-Bass; 2003. pp. 3–23. [Google Scholar]
- National Institutes of Health’s Office of Behavioral and Social Sciences Research. NIH Summer Institute on Community-Based Participatory Research Targeting the Medically Underserved. 2009 Retrieved from http://conferences.thehillgroup.com/si2009/
- Newman SD, Andrews JO, Magwood GS, Jenkins C, Cox MJ, Williamson DC. Community advisory boards in community-based participatory research: A synthesis of best processes. Preventing Chronic Disease. 2011;8(3):A70. [PMC free article] [PubMed] [Google Scholar]
- Reardon KM. Enhancing the capacity of community-based organizations in east St. Louis. Journal of planning Education and Research. 1998;17:323–333. [Google Scholar]
- Rosenthal MS, Lucas GI, Tinney B, Mangione C, Schuster MA, Wells K, Heisler M. Teaching community-based participatory research principles to physicians enrolled in a health services research fellowship. Academic Medicine. 2009;84:478–484. doi: 10.1097/ACM.0b013e31819a89e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez V, Carrillo C, Wallerstein N. From the ground up: Building a participatory evaluation model. Progress in Community Health Partnerships. 2011;5:45–52. doi: 10.1353/cpr.2011.0007. [DOI] [PubMed] [Google Scholar]
- Sandoval JA, Lucero J, Oetzel J, Avila M, Belone L, Mau M, Wallerstein N. Process and outcome constructs for evaluating community-based participatory research projects: A matrix of existing measures. Health Education Research. 2012;27:680–690. doi: 10.1093/her/cyr087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarinci IC, Johnson RE, Hardy C, Marron J, Partridge EE. Planning and implementation of a participatory evaluation strategy: A viable approach in the evaluation of community-based participatory programs addressing cancer disparities. Evaluation and Program Planning. 2009;32:221–228. doi: 10.1016/j.evalprogplan.2009.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of North Carolina. North Carolina Translational & Clinical Sciences Institute’s Community Engagement Program. (n.d.). Retrieved from http://tracs.unc.edu/obtain-education-training/obtain-education-training.html.
- Viswanathan M, Ammerman A, Eng E, Gartlehner G, Lohr KN, Griffith D, Whitener L. Community-based participatory research: Assessing the evidence. Rockville, MD: Agency for Healthcare Research and Quality; 2004. (Summary, Evidence Report/ Technology Assessment No. 99, AHRQ Publication 04-E0220–1. [PMC free article] [PubMed] [Google Scholar]
- Wallerstein N, Duran B. The conceptual, historical and practice roots of community based participatory research and related participatory traditions. In: Minkler M, Wallerstein N, editors. Community-research based participatory in health. San Francisco, CA: Jossey-Bass; 2003. pp. 27–52. [Google Scholar]