Abstract
A 68-year-old man developed bilateral sequential non-arteritic anterior ischaemic optic neuropathy, each episode occurring with a close temporal relationship to influenza vaccination.
Key Words: Cardiovascular event, Bilateral sequential non-arteritic anterior ischaemic optic neuropathy, Influenza vaccination
Case Report
A 68-year-old man reported a 2-day history of reduced visual acuity 10 days after receiving the influenza vaccine. He reported no constitutional symptoms. His medical history included type 2 diabetes mellitus, previous transurethral resection of the prostate and erectile dysfunction treated with tadalafil. His ocular history included hypermetropia and left mild anisometropic amblyopia, with previous best-corrected visual acuities of 6/5 in his right eye and 6/12 in his left eye.
On examination, his visual acuities were 6/5 in the right eye and 6/60 in the left eye, improving to 6/36 with a pinhole. His colour vision was normal, with an Ishihara of 17/17 bilaterally. There was no relative afferent pupillary defect and no pain or diplopia on eye movements. Fundoscopy revealed bilateral crowded discs with evidence of disc swelling in the left eye. 24-2 Humphrey visual field testing identified an altitudinal visual field defect in the left eye.
The patient was diagnosed with anterior ischaemic optic neuropathy (AION) and laboratory studies were obtained to exclude giant cell arteritis. He had a normal full blood count, C-reactive protein of <4 mg/dl, and an erythrocyte sedimentation rate of 3 mm/h as well as normal blood pressure. The only abnormal finding was a raised cholesterol level of 6.1 mmol/l (normal, <5 mmol/l). Having refined the diagnosis to non-arteritic (NA) AION, he was commenced on aspirin 75 mg once daily, although the evidence for this is mixed [1, 2]. He also ceased the use of tadalafil. Subsequent MRI of his brain and orbits proved normal.
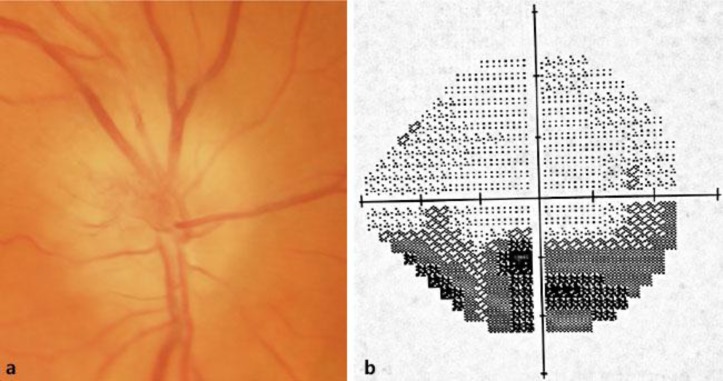
Over the next 3 months, his visual acuity in the left eye recovered to 6/36 with a persistent field defect. However, the following year, 6 days after receiving the influenza vaccine, he returned with a new-onset visual field defect in his right eye. His visual acuity remained good at 6/5 in the right eye and 6/36 in the left eye. Ocular findings were again normal apart from a swelling of the superior disc margin in the right eye, but 24-2 Humphrey visual field testing revealed an inferior altitudinal visual field defect in the right eye (fig. 1, fig. 2).
Fig. 1.
a Disc swelling in the superior segment of the disc, and b associated altitudinal field defect in the right eye following the second influenza vaccination.
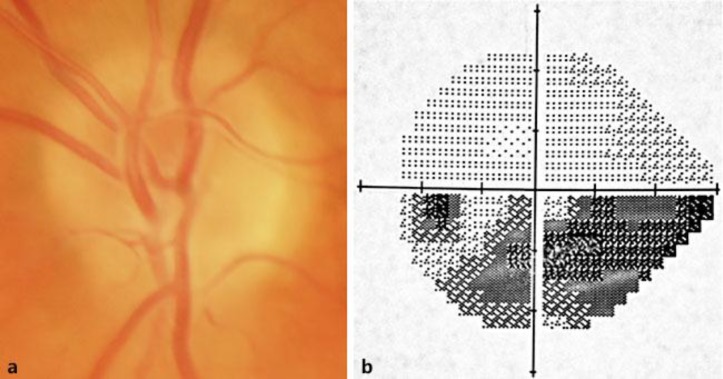
Fig. 2.
Fundus photography at the same time as figure 1 indicates resolution of disc swelling in in the left eye (a), but a persistent inferior visual field defect (b).
Laboratory studies again excluded giant cell arteritis but, given the temporal relation to his influenza vaccination, an immune-mediated component of the aetiology was considered, and he was treated with high-dose corticosteroid in the form of 80 mg prednisolone once daily. This was tapered off over 3 months and his visual acuity remained 6/5 in the right eye, although his inferior altitudinal visual field defect persisted.
Discussion
Ocular complications following influenza vaccination are rare but they have been recorded. Optic neuritis is well-described [3, 4, 5] and the proposed mechanism is immune-mediated optic nerve demyelination [4], which may be unilateral or bilateral. The majority of patients recover substantially without treatment.
Our case differs from the majority in that the clinical findings are consistent with a diagnosis of AION: an altitudinal visual field defect associated with segmental disc swelling. To our knowledge, there has been only 1 previous case reported in the literature of NA-AION following influenza vaccination [6]. In this case, the reported visual loss was bilateral and associated with systemic symptoms and raised serum inflammatory markers. The authors proposed an immune complex-mediated vasculopathy as a likely mechanism. Here, we report sequential NA-AION in one and the same patient, each event occurring with a close temporal relation to influenza vaccination.
Our patient was over 65, had a history of diabetes mellitus and was hypermetropic with small optic discs and taking tadalafil, all of which are known or potential risk factors for NA-AION [7, 8]. However, the close temporal relationship to vaccination does suggest the possibility of an inflammatory or immune-mediated element to the timing of its development. Nevertheless, the cumulative incidence of second-eye involvement in NA-AION is 18% at 1 year and 25% at 3 years [9]. Thus, our case probably represents a chance occurrence, especially as there is some evidence that within-season influenza vaccination leads to a reduced incidence of stroke and other cardiovascular events [10].
References
- 1.Beck RW, Hayreh SS, Podhajsky PA, Tan ES, Moke PS. Aspirin therapy in nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol. 1997;123:212–217. doi: 10.1016/s0002-9394(14)71038-4. [DOI] [PubMed] [Google Scholar]
- 2.Kupersmith MJ, Frohman L, Sanderson M, et al. Aspirin reduces the incidence of second eye NAION: a retrospective study. J Neuroophthalmol. 1997;17:250–253. [PubMed] [Google Scholar]
- 3.Perry HD, Mallen FJ, Grodin RW, Cossari AJ. Reversible blindness in optic neuritis associated with influenza vaccination. Ann Ophthalmol. 1979;11:545–550. [PubMed] [Google Scholar]
- 4.Hull TP, Bates JH. Optic neuritis after influenza vaccination. Am J Ophthalmol. 1997;124:703–704. doi: 10.1016/s0002-9394(14)70918-3. [DOI] [PubMed] [Google Scholar]
- 5.Rubinov A, Beiran I, Krasnitz I, Miller B. Bilateral optic neuritis after inactivated influenza vaccination. Isr Med Assoc J. 2012;14:705–707. [PubMed] [Google Scholar]
- 6.Kawasaki A, Purvin VA, Tang R. Bilateral anterior ischemic optic neuropathy following influenza vaccination. J Neuroophthalmol. 1998;18:56–59. [PubMed] [Google Scholar]
- 7.Escaravage GK, Jr, Wright JD, Jr, Givre SJ. Tadalafil associated with anterior ischemic optic neuropathy. Arch Ophthalmol. 2005;123:399–400. doi: 10.1001/archopht.123.3.399. [DOI] [PubMed] [Google Scholar]
- 8.Hayreh SS. Ischaemic optic neuropathy. Indian J Ophthalmol. 2000;48:171–194. [PubMed] [Google Scholar]
- 9.Beri M, Klugman MR, Kohler JA, Hayreh SS. Anterior ischemic optic neuropathy. VII. Incidence of bilaterality and various influencing factors. Ophthalmology. 1987;94:1020–1028. doi: 10.1016/s0161-6420(87)33350-0. [DOI] [PubMed] [Google Scholar]
- 10.Siriwardena AN, Asghar Z, Coupland CC. Influenza and pneumococcal vaccination and risk of stroke or transient ischaemic attack-matched case control study. Vaccine. 2014;32:1354–1361. doi: 10.1016/j.vaccine.2014.01.029. [DOI] [PubMed] [Google Scholar]