Abstract
Purpose
We aimed to elucidate the effects of two epigenetic inhibitors, 5-aza-2’-deoxycytidine (5-aza-dC) and trichostatin A (TSA), on several key secretory mediators of diabetic retinopathy (DR) in human retinal endothelial cells (HRECs) and human retinal pigment epithelial (HRPE) cells treated with high glucose or interleukin-1β (IL-1β).
Methods
HRECs and HRPE cells were incubated in 30 mM D-glucose or 10 ng/ml IL-1β with or without the presence of various concentrations of 5-aza-dC or TSA. The production of pigment epithelium derived factor (PEDF), vascular endothelial cell growth factor (VEGF), intercellular cell adhesion molecule-1 (ICAM-1), IL-1β, and matrix metalloproteinase 2 (MMP2) was evaluated at the mRNA and protein levels using real-time PCR and enzyme-linked immunosorbent assay (ELISA), respectively.
Results
In the 30 mM D-glucose and the 10 ng/ml IL-1β condition, the expression of VEGF, ICAM-1, IL-1β, and MMP2 was induced in the HRECs and the HRPE cells. PEDF was downregulated in the HRPE cells but upregulated in the HRECs. However, the PEDF-to-VEGF ratio, which is thought to be critical in DR, was downregulated in both cell types. 5-aza-dC dose-dependently alleviated VEGF, ICAM-1, IL-1β, and MMP2 and reversed PEDF or the PEDF/VEGF ratio in both cell types. TSA had similar effects as 5-aza-dC on the target mediators. However, ICAM-1 production was aggravated in the HRECs while remaining unchanged in the HRPE cells after TSA was administered.
Conclusions
Our results demonstrated that 5-aza-dC and TSA enhance the protective PEDF and the PEDF/VEGF ratio and ameliorate the adverse effects of diabetic stimuli in vitro, suggesting that these two drugs may be of potential therapeutic value in DR.
Introduction
Diabetic retinopathy (DR), characterized by diabetic macular edema and retinal neovascularization, is a common microvascular complication of diabetes and a leading cause of adult blindness. Over the last several years, multiple mechanisms and pathological processes including oxidative stress, inflammation, and extracellular matrix remodeling have been implicated in the development and progression of DR. The molecular mechanisms involved in these processes are complex, including proper cellular signal coordination and interactions of various growth factors, cytokines, and enzymes produced by the retinal cells. Effective blockage or readjustment of the cytokines involved in these processes with protective factors can reverse the pathological states of the retina [1].
In recent years, epigenetic modifications, including DNA methylation and histone acetylation, have been recognized as playing significant roles in regulating cellular activity. In this system, DNA methylation and histone acetylation are regulated by DNA methyltransferases (DNMTs) and histone deacetylases (HDACs), respectively. DNA methylation and histone acetylation imbalances have been shown to contribute to the pathogenesis of cancers, cardiovascular diseases, neural degenerative diseases, metabolic diseases, etc. [2]. 5-aza-2'-deoxycytidine (5-aza-dC) and trichostatin A (TSA), which can non-selectively inhibit DNMTs and HDACs, respectively, have been shown to have therapeutic effects in several pathological conditions [3,4]. Since the roles of 5-aza-dC and TSA in retinal cells under diabetic condition have not been investigated, our objective in this study was to determine whether 5-aza-dC and TSA affect the critical and representative mediators under high glucose or interleukin-1β (IL-1β) circumstances in human retinal endothelial cells (HRECs) and human retinal pigment epithelial (HRPE) cells.
Methods
Cell culture
All experiments were conducted according to the tenets of the Declaration of Helsinki for Research Involving Human Subjects and the ARVO statement on human subjects and approved by the Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou, China. Eight eyes (from four donors) were obtained after the corneas had been removed for transplantation from the Eye Bank of Zhongshan Ophthalmic Center (Guangzhou, China).
Primary cultured HRECs and HRPE cells were prepared and cultured as previously described [5,6]. Briefly, the eyes were cut circumferentially 3 mm posterior to the limbus, and the retinas were harvested. The retinas were then minced gently, digested in 2% trypsin for 20 min followed by 0.1% collagenase for 20 min at 37 °C. The homogenate was centrifuged, and the pellet was resuspended and grown in fibronectin-coated flasks and maintained in human endothelial-serum free medium (HE-SFM; Gibco, Grand Island, NY) supplemented with 10% fetal bovine serum, 5 ng/ml recombinant human β-endothelial cell growth factor (β-ECGF; R&D Systems, Minneapolis, MN), and 1% insulin-transferrin-selenium (ITS; Gibco). After the vitreous and the retina were removed, the RPE cells were mechanically harvested, separated by digestion with 0.25% trypsin and 0.02% EDTA, and then maintained in Dulbecco’s Modified Eagle’s Medium (DMEM; Gibco) containing 10% fetal bovine serum, penicillin G (100 U/ml), streptomycin sulfate (100 mg/ml), and amphotericin B (2.5 mg/ml; Gibco) and were characterized by the typical hexagon shape with epitheloid morphology and pigment granules. Cells were incubated at 37 °C in a humidified atmosphere containing 5% CO2. HRECs at passages 3–5 and HRPE cells from passages 6–8 were used in all experiments.
Cell treatment
Cells were seeded in six-well plates. After 24 h synchronization in HE-SFM or DMEM containing 1% serum, the sub-confluent cells were incubated in 5 mM D-glucose (normal physiologic glucose, NG), 30 mM D-glucose (high glucose, HG), or 10 ng/ml human recombination IL-1β with or without the presence of various concentrations of 5-aza-dC (5 μM, 10 μM) or TSA (0.2 μM, 0.5 μM, 1 μM) for 24 h (the IL-1β group) or 48 h (the HG group). The experiment was repeated at least three times.
Evaluation of gene expression using quantitative real-time PCR
Total RNA from the cells was extracted using TRIzol (Invitrogen Life Technologies, Grand Island, NY), and the RNA was reverse transcribed with the TaKaRa First Strand Synthesis kit (TaKaRa, Dalian, China). Real-time quantitative PCR was run on an ABI Prism 7000 system with the SYBR Green PCR kit (TaKaRa, Dalian, China). PCR was performed by denaturing at 95 °C for 5 min, followed by 40 cycles of denaturation at 95 °C, annealing at 60 °C, and extension at 72 °C for 10 s, respectively. One microgram of each RNA and 2 μl of each cDNA was used to measure the target genes. The primers used are summarized in Table 1.
Table 1. primers used in real-time PCR.
| Gene (human) | Forward primers | Reverse primers | Product length (bp) |
|---|---|---|---|
| PEDF |
TGAGAAGAAGCTGCGCATAA |
ACCGAGAAGGAGAATGCTGA |
196 |
| VEGF |
AAGGAGGAGGGCAGAATCAT |
ATCTGCATGGTGATGTTGGA |
226 |
| ICAM-1 |
CAGAGGTTGAACCCCACAGT |
CCTCTGGCTTCGTCAGAATC |
196 |
| IL-1β |
GGACAAGCTGAGGAAGATGC |
TCCATATCCTGTCCCTGGAG |
246 |
| MMP2 |
GATACCCCTTTGACGGTAAGGA |
CCTTCTCCCAAGGTCCATAGC |
112 |
| β-actin | CATGTACGTTGCTATCCAGGC | CTCCTTAATGTCACGCACGAT | 250 |
Evaluation of protein levels using enzyme-linked immunosorbent assay
At the end of the incubation, the supernatants of the cells were harvested to analyze cytokine secretions using double monoclonal antibodies sandwich enzyme-linked immunosorbent assay (ELISA) assay kits according to the manufacturer's protocol. Pigment epithelium derived factor (PEDF), vascular endothelial cell growth factor (VEGF), intercellular cell adhesion molecule-1 (ICAM-1), IL-1β, and matrix metalloproteinase 2 (MMP2) ELISA kits were purchased from ExCellBiology (Shanghai, China).
Statistical analysis
The experiments presented in the figures represent three or more different repetitions. All data are expressed as mean±standard deviation (SD) and analyzed with SPSS 15.0 software (SPSS Inc., Chicago, IL). One-way ANOVA was used to compare differences among groups. A value of p<0.05 was considered statistically significant.
Results
Effect of 5-aza-dC and TSA on target mediators in the NG condition
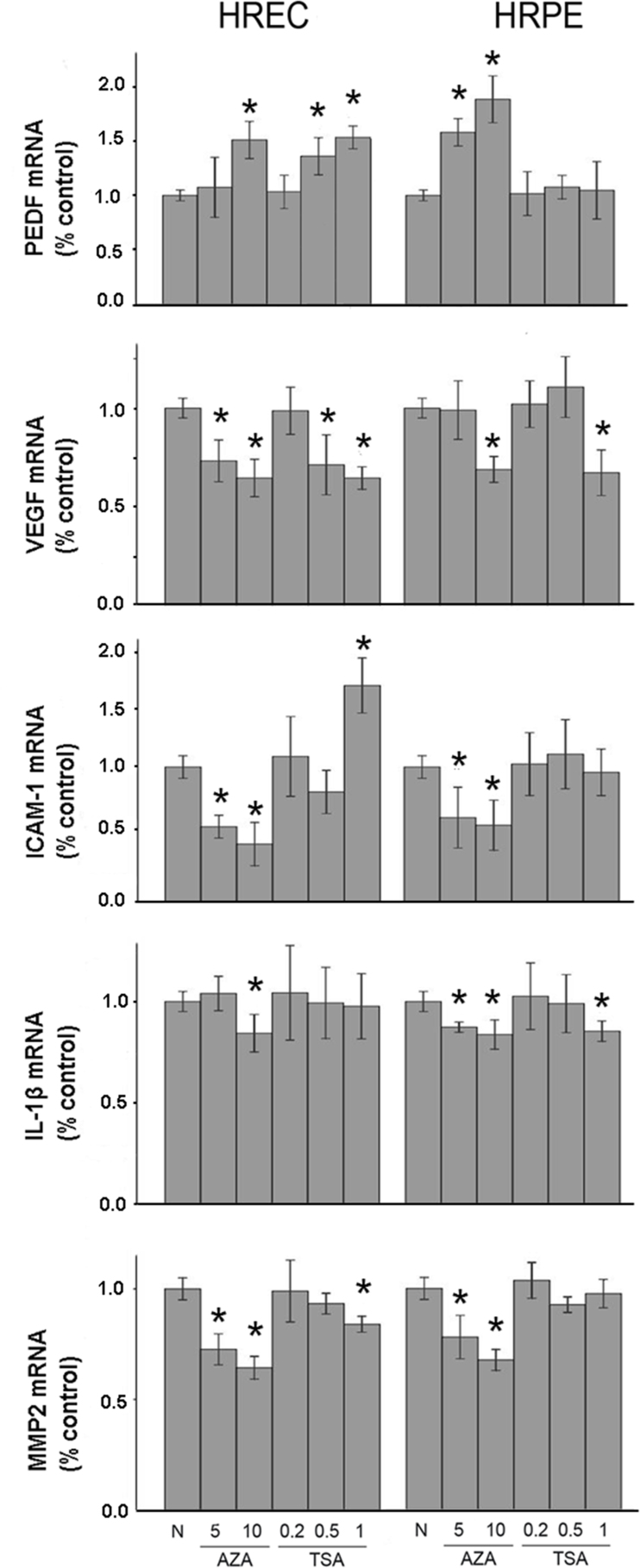
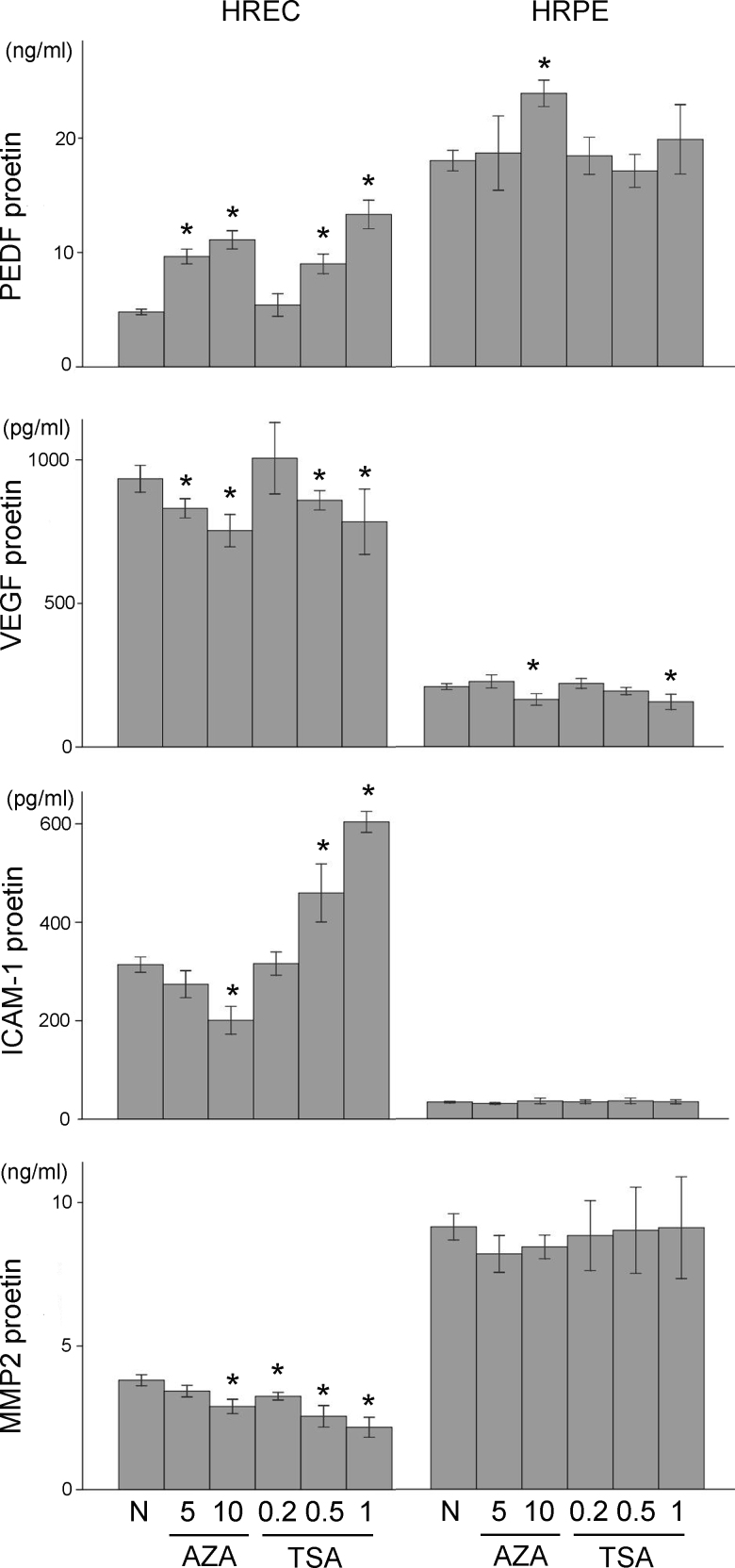
PEDF, VEGF, ICAM-1, IL-1β, and MMP2 were reported to participate in the initiation and progression of DR [7,8]. We first investigated whether 5-aza-dC and TSA regulated these cytokines in the normal physiologic glucose concentration in the HRECs and HRPE cells (Figure 1 and Figure 2).
Figure 1.
Induction of pigment epithelium derived factor (PEDF) and suppression of exacerbating factors at mRNA levels by 5-aza-2’-deoxycytidine (5-aza-dC) in human retinal endothelial cells (HRECs) and human retinal pigment epithelial (HRPE) cells in normal glucose (NG) condition. Similar effects of trichostatin A (TSA) was observed except that intercellular cell adhesion molecule-1 (ICAM-1) mRNA was induced in HRECs by TSA. Cells were cultured for 48 hours in NG with or without 5-aza-dC (5 μM, 10 μM) or TSA (0.2 μM, 0.5 μM, 1 μM). PEDF, vascular endothelial growth factor (VEGF), intercellular cell adhesion molecule-1 (ICAM-1), interleukin (IL)-1β, and matrix metalloproteinase 2 (MMP2) gene expressions was analyzed with real-time PCR. The data are expressed as the mean ± standard deviation (SD; *p<0.05). All experiments were repeated three times with similar results.
Figure 2.
Induction of pigment epithelium derived factor (PEDF) and suppression of exacerbating factors at protein levels by 5-aza-2’-deoxycytidine (5-aza-dC) in human retinal endothelial cells (HRECs) and human retinal pigment epithelial (HRPE) cells in normal glucose (NG) condition. Similar effects of trichostatin A (TSA) was observed except that intercellular cell adhesion molecule-1 (ICAM-1) protein was induced in HRECs by TSA. Cells were cultured for 48 h in NG with or without 5-aza-dC (5 μM, 10 μM) or TSA (0.2 μM, 0.5 μM, 1 μM). PEDF, vascular endothelial growth factor (VEGF), ICAM-1, interleukin (IL)-1β, and matrix metalloproteinase 2 (MMP2) in the supernatants were analyzed with enzyme-linked immunosorbent assay (ELISA). The data are expressed as the mean ± standard deviation (SD; *p<0.05). All experiments were repeated three times with similar results. IL-1β secretion could not be detected due to its low concentration.
5-aza-dC induced PEDF in both cell types in a dose-dependent manner. Dose-dependent down-regulation of VEGF, ICAM-1 (not protein level in HRPE cells), IL-1β, and MMP2 (not protein level in HRPE cells) by 5-aza-dC was observed in both cell types.
TSA induced PEDF in the HRECs but not in the HRPE cells. Only downregulation of VEGF in both cell types, downregulation of MMP2 in HRECs, and IL-1β downregulation in HRPE cells by TSA administration were observed. Notably, adding TSA induced mRNA and secretion of ICAM-1 in the HRECs yet had no effect on ICAM-1 production in the HRPE cells. (The IL-1β protein secretion was too low to be detected with ELISA in the NG and HG groups in our study.)
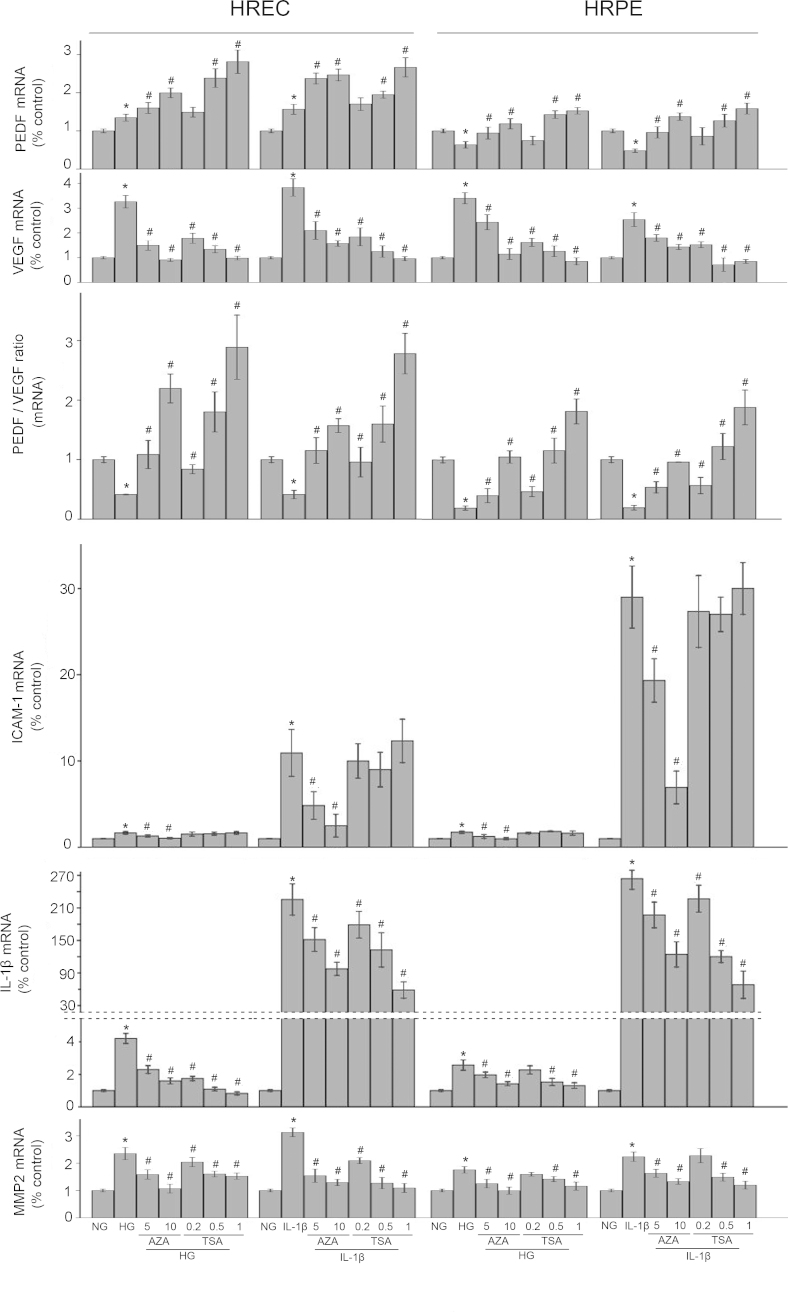
Effect of 5-aza-dC and TSA on VEGF, ICAM-1, IL-1β, and MMP 2 in the HG or IL-1β condition
VEGF, ICAM-1, IL-1β, and MMP2 act as exacerbating factors in DR. Compared with the control conditions, exposure to HG resulted in a significant increase in the levels of VEGF, ICAM-1, IL-1β, and MMP2. Exposure to IL-1β also resulted in a similar increase in the target mediators.
In HRECs, 5-aza-dC mitigated the upregulation of VEGF, ICAM-1, IL-1β, and MMP2 by HG or IL-1β, while TSA had a similar effect on these mediators but not on ICAM-1. In Figure 3, as in the NG condition, TSA did not eliminate the increase in ICAM-1 but further upregulated the ICAM-1 level in the HRECs.
Figure 3.
5-aza-2’-deoxycytidine (5-aza-dC) and trichostatin A (TSA) induced pigment epithelium derived factor (PEDF), reverses PEDF/vascular endothelial growth factor (VEGF) ratio and mitigated the up-regulations of exacerbating factors at mRNA levels in human retinal endothelial cells (HRECs) and human retinal pigment epithelial (HRPE) cells in high glucose (HG) or interleukin (IL)-1β condition while TSA further up-regulated intercellular cell adhesion molecule-1 (ICAM-1) mRNA in HRECs. Cells were cultured for 24 h (IL-1β stimulation) or 48 h (HG stimulation) with or without 5-aza-dC (5 μM, 10 μM) or TSA (0.2 μM, 0.5 μM, 1 μM). PEDF, VEGF, ICAM-1, IL-1β, and matrix metalloproteinase 2 (MMP2) gene expressions and the PEDF/VEGF mRNA ratio were analyzed with real-time PCR. The data are expressed as the mean ± standard deviation (SD). The expression was normalized separately to its control counterpart. *p<0.05 versus the normal physiologic glucose (NG) group, #p<0.05 versus the HG group or the IL-1β group. All experiments were repeated three times with similar results.
In the HRPE cells, 5-aza-dC and TSA mitigated VEGF, ICAM-1 (no change in the TSA-treated HRPE cells), IL-1β, and MMP2 upregulation in the HG or IL-1β condition at varying degrees in a dose-dependent manner (Figure 3 and Figure 4).
Figure 4.
5-aza-2’-deoxycytidine (5-aza-dC) and trichostatin A (TSA) induced pigment epithelium derived factor (PEDF), reverses PEDF/ vascular endothelial growth factor (VEGF) ratio and mitigated the up-regulations of exacerbating factors at protein levels in human retinal endothelial cells (HRECs) and human retinal pigment epithelial (HRPE) cells in high glucose (HG) or interleukin (IL)-1β condition while TSA further up-regulated intercellular cell adhesion molecule-1 (ICAM-1) protein in HRECs. Cells were cultured for 24 h (IL-1β stimulation) or 48 h (HG stimulation) with or without 5-aza-dC (5 μM, 10 μM) or TSA (0.2 μM, 0.5 μM, 1 μM). PEDF, VEGF, ICAM-1, IL-1β, and matrix metalloproteinase 2 (MMP2) secretions and the PEDF/VEGF protein ratio were analyzed with enzyme-linked immunosorbent assay (ELISA). The data are expressed as the mean ± standard deviation (SD). The expression was normalized separately to its control counterpart. *p<0.05 versus the normal physiologic glucose (NG) group, #p<0.05 versus the HG group or the IL-1β group. All experiments were repeated three times with similar results. IL-1β secretion could not be detected in this study. (IL-1β secretion could not be analyzed due to due to its low concentration [the HG group] or the exogenous human recombination IL-1β [the IL-1β stimulation group])”.
5-aza-dC and TSA PEDF and reversed the PEDF/VEGF ratio in the HG or IL-1β condition
In the HRECs, PEDF was upregulated by 30 mM D-glucose or 10 ng/ml IL-1β. Since significant correlations were found between the severity of the vascular damage and the PEDF/VEGF ratio [9] and the PEDF/VEGF ratio was also reported to be correlated with angiogenesis processes [10-12], we further analyzed the PEDF/VEGF ratio in the HRECs. We found that the PEDF/VEGF ratio was significantly decreased by 30 mM D-glucose or 10 ng/ml IL-1β compared with the control cells. After the 5-aza-dC treatment, an additional increase in PEDF production and reversal of the PEDF/VEGF ratio were observed. TSA also further increased PEDF and reversed the PEDF/VEGF ratio in a dose-dependent manner in the HRECs.
In the HRPE cells, in contrast to the HRECs, the PEDF level and the PEDF/VEGF ratio was decreased by the 30 mM D-glucose or 10 ng/ml IL-1β treatments at the mRNA and protein levels. Adding 5-aza-dC and TSA dose-dependently reversed the PEDF level and the PEDF/VEGF ratio in the HRPE cells (Figure 3 and Figure 4).
Discussion
In our study, we sought to determine whether inhibiting DNMTs and HDACs by two DNMT and HDAC inhibitors, 5-aza-dC and TSA, respectively, affect the critical mediators that participate in DR, to evaluate their potential abilities to treat this devastating disease. We showed that in the HG- and IL-1β-induced diabetic environments, 5-aza-dC and TSA increased PEDF and the PEDF/VEGF ratio and downregulated VEGF, ICAM-1(not in HRECs treated with TSA), IL-1β, and MMP2. These results suggest that the HRECs and the HRPE cells are potential therapeutic targets, and 5-aza-dC and TSA may have protective effects in DR.
The inner barrier of the retina, which is formed by the tight junctional complexes between retinal endothelial cells, acts as the first barrier and the first victim in vessel lesions [13]. The retinal pigment epithelium, located in the interface between the neural retina and the choriocapillaris where it forms the outer blood–retinal barrier, helps maintain an appropriate environment for photoreceptor function by its transporting, secretion, and many other functions, whose abnormal cellular states can cause retinal lesions [14]. Therefore, therapeutic strategies that modulate these two cell type impairments are warranted. Hyperglycemia instigates a cascade of events in retinal cells and was one of the independent risks and one of the initiators of DR [1]. More recently, evidence has also arisen supporting a prominent role for inflammation underlying the pathogenesis of DR. IL-1β is a major proinflammatory cytokine secreted by lymphocytes and macrophages and is not only a trigger but also an amplifier of inflammation [7,15]. Therefore, in our study we simulated the hyperglycemia and inflammatory condition of DR in vitro using D-glucose and IL-1β stimulations in HRECs and HRPE cells. We found that all the tested cytokines existed in HRECs and HRPE cells at different abundances, and the stimulation of HG or human recombination IL-1β changed the expression pattern of the mediator production. This suggested that retinal endothelial cells and retinal pigment epithelial cells could react to the diabetic stimuli, taking part in initiating and driving the progress of diabetic lesions.
PEDF is a pluripotent factor with neuroprotective, antiangiogenic, antioxidative, and anti-inflammatory properties and thus acts as a protector for the retina by autocrine and paracrine [16]. Exogenous recombination PEDF exerts protective effects on the retina and retinal cells in the diabetic condition [17]. We found that PEDF was highly expressed and more abundant in the HRPE cells than in the HRECs. HG and IL-1β dramatically downregulated PEDF production in the HRPE cells. In the HRECs, in contrast, PEDF was upregulated by HG or recombination IL-1β. The inconsistent findings of the PEDF changes under diabetic conditions in HRECs and HRPE cells may be due to the different physiologic properties of these two types of cells. In addition, previous studies have shown conflicting results regarding PEDF changes under the diabetic condition. Zheng et al. and Matsuoka et al. have shown PEDF upregulation [9,18,19] while studies by Mohan et al. and Li et al. reported that PEDF was decreased in DR [20,21]. However, despite upregulation of PEDF, a more critical indicator, the PEDF/VEGF ratio, was still significantly decreased as a result of even more upregulation of VEGF, which was also consistent with previous studies [9,18,19]. A significant correlation was found between the severity of vascular damage and the PEDF/VEGF ratio [9]. The PEDF/VEGF ratio was also reported to decrease in the vitreous humor in certain retinal diseases and the time course of the PEDF/VEGF ratio change correlated with angiogenesis processes [10-12]. Therefore, our results indicated that the diabetic stimuli exerted a downregulatory effect on PEDF production or the PEDF/VEGF ratio, and thus weakened the resistance potency of retinal cells under the diabetic condition.
VEGF is a proinflammatory molecule, and the cellular or vitreous level of VEGF is highly correlated with retinal neovascularization and edema. Intraocular delivery of anti-VEGF is a therapy now used widely to treat advanced diabetic retinopathy [22]. ICAM-1 is upregulated in the retinal vasculature in diabetes. Diabetic mice genetically deficient in ICAM-1 or its ligand (CD18) were protected from the expected development of lesions of early diabetic retinopathy (including capillary degeneration, pericyte loss and increased permeability as well as leukostasis) [23]. IL-1β is an upstream cytokine that can trigger a chain of inflammatory responses and have been shown to be involved in retinal diseases including DR. Recent studies have supported a role for IL-1β-driven neuron-inflammation in the pathogenesis of diabetic retinopathy through autostimulation and amplification of inflammation. In addition, the interaction effects between IL-1β and hyperglycemia form a continuous feedback loop, interruption of which could limit the progression of DR [7,24]. MMPs regulate various cellular functions, including apoptosis, proliferation, differentiation, formation of the extracellular matrix (ECM), and angiogenesis, abrogation of which can protect the retina in the diabetic condition [8,25,26]. These cytokines are representative and characteristic mediators in DR and were thus selected to be analyzed in our study. We found that HG and exogenous IL-1β induced these cytokines and thus verified the roles of the target cytokines in cellular damage in the development of DR.
Epigenetic regulation has been shown to play important roles in diabetes and its complications [27,28]. As the main diabetic complication, DR has been reported to be related to epigenetic regulations in vitro and in vivo [29]. Inhibition or activation of involved epigenetic enzymes can intervene in the process of epigenetic activities in cells and organs and thus control the genesis and development of different kinds of diseases [30]. As a nonselective DNMT inhibitor, 5-aza-dC has been reported to be protective in many pathological conditions. 5-aza-dC decreased VEGF121a, VEGF165a angiogenic, and VEGF121b and VEGF165b antiangiogenic variant expression, while significantly increasing expression of the VEGF189b antiangiogenic variant transcript and protein in human lung microvascular endothelial cells [3]. 5-aza-dC may have applications as a novel clinical strategy for increasing the production of Treg cells to modulate the airway inflammation associated with asthma [31]. Xiao et al. demonstrated in vivo that increased DNA methylation and the phenotype of heart hypertrophy and reduced cardiac contractility can be reversed by 5-aza-dC [32]. In our study, 5-aza-dC induced PEDF production and decreased VEGF, ICAM-1 (mRNA only), IL-1β, and MMP2 (mRNA only) in the NG condition. In the HG or IL-1β condition, 5-aza-dC downregulated VEGF and further upregulated PEDF, which subsequently resulted in a decreased VEGF/PEDF ratio and may have relieved cellular damage under diabetic conditions. In addition, 5-aza-dC eliminated the upregulated ICAM-1, IL-1β, and MMP2. These results indicated that 5-aza-dC enhanced the protective factors and removed the harmful factors, thus protecting the retinal cells from diabetic damage.
To date, 18 human HDAC isoforms have been characterized and divided into four major classes: class I HDACs (HDAC1, 2, 3, and 8), class II HDACs (HDAC4, 5, 6, 7, 9, and 10), class III HDACs (SIRT1, 2, 3, 4, 5,6 and 7), and class IV HDAC (HDAC11). Class II HDACs are further subdivided into class IIa (HDAC4, 5, 7, 9) and class IIb (HDAC6 and 10) forms [33]. Different HDAC isoforms may have different functions. For example, silent mating type information regulation 2 homolog (SIRT2) and SIRT6 process anti-inflammation potency [34,35], while HDAC6 inactivation may suppress inflammation [36]. TSA is a class I and II HDAC inhibitor, and initial studies have identified its therapeutic effects in several pathological conditions [37-39]. Tiina Suuronen observed that TSA and azacitidine (AZA) treatments induced prominent increases in the expression levels of clusterin in ARPE-19 cells and might affect the pathogenesis of age-related macular degeneration (AMD) via the inhibition of angiogenesis and inflammation [40]. Yu et al. demonstrated that TSA inhibited IL-1- or interferon (IFN)-γ-induced nitric oxide production [41]. Crosson showed that suppressing HDAC activity by TSA can protect the retina from ischemic injury and the neuroprotective response is associated with the suppression of retinal tumor necrosis factor (TNF)-α expression and signaling, thus providing a novel treatment for ischemic retinal injury [37].
In the present study, similar to 5-aza-dC, TSA effectively modulated the related mediators. However, contrast to 5-aza-dC, TSA had no effects on ICAM-1 in the HRPE cells but induced ICAM-1 production in the HRECs. This suggested that the effect of TSA on certain cytokines may differ depending on the cell type. In addition, a different HDAC inhibitor may affect different HDAC isoforms. Ahmed et al. reported that largazole, a class I histone deacetylase inhibitor, enhanced TNF-α-induced ICAM-1 and vascular cell adhesion molecule 1 (VCAM-1) expression in rheumatoid arthritis synovial fibroblasts and the upregulation was mediated by the induction of HDAC6 after largazole treatment [42]. Similarly, Kyrylenko et al. reported that TSA upregulated SIRT2, 4, 7 while downregulating SIRT1, 5, 6 [43]. Thus, we speculated that ICAM-1 upregulated by TSA in the HRECs may be partly due to the effects of TSA on specific HDAC isoforms. Further studies are needed to investigate the exact mechanisms. The overall effects of non-selective HDAC inhibitors should be fully illustrated when they are considered for use in treating diseases. In addition, selective HDAC inhibitors should also be considered since Vishwakarma et al. demonstrated that tubastatin, a selective histone deacetylase 6 inhibitor, showed anti-inflammatory and antirheumatic effects [42].
In conclusion, we showed that in HG- or IL-1β-induced diabetic environments, 5-aza-dC and TSA increased PEDF and the PEDF/VEGF ratio and downregulated certain mediators with adverse effects. These results suggest that the resistance abilities of the retina cells in pathological conditions in diabetes could be enhanced by the administration of these two drugs and epigenetic inhibitors represent a promising new class of compounds in the treatment of DR. Other affected genes participating in DR, the molecular mechanisms and signaling pathways involved, and the effects of these two epigenetic drugs in vivo remain to be illustrated when they are considered for use in treating DR clinically. Meanwhile, the induction of ICAM-1 by TSA in the HRECs suggested that further and more extensive investigation of the roles of TSA in protecting the retina or a more specific HDAC inhibitor may be needed.
Acknowledgments
This study was supported by the National Natural Science Foundation of China to Shibo Tang (No.81170865) and the Natural Science Foundation of Guangdong province to Andina Hu (No. S2012040006673)
References
- 1.Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376:124–36. doi: 10.1016/S0140-6736(09)62124-3. [DOI] [PubMed] [Google Scholar]
- 2.Dupont C, Armant DR, Brenner CA. Epigenetics: definition, mechanisms and clinical perspective. Semin Reprod Med. 2009;27:351–7. doi: 10.1055/s-0029-1237423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller-Kasprzak E, Jagodzinski PP. 5-Aza-2'-deoxycytidine increases the expression of anti-angiogenic vascular endothelial growth factor 189b variant in human lung microvascular endothelial cells. Biomed Pharmacother. 2008;62:158–63. doi: 10.1016/j.biopha.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 4.Chabane N, Zayed N, Afif H, Mfuna-Endam L, Benderdour M, Boileau C, Martel-Pelletier J, Pelletier JP, Duval N, Fahmi H. Histone deacetylase inhibitors suppress interleukin-1beta-induced nitric oxide and prostaglandin E2 production in human chondrocytes. Osteoarthritis Cartilage. 2008;16:1267–74. doi: 10.1016/j.joca.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 5.Capetandes A, Gerritsen ME. Simplified methods for consistent and selective culture of bovine retinal endothelial cells and pericytes. Invest Ophthalmol Vis Sci. 1990;31:1738–44. [PubMed] [Google Scholar]
- 6.Yue BY, Kawa JE, Chang IL, Sawaguchi S, Fishman GA. Effects of chondroitin sulfate on cultured human retinal pigment epithelial cells. Cell Biol Int Rep. 1991;15:365–76. doi: 10.1016/0309-1651(91)90125-3. [DOI] [PubMed] [Google Scholar]
- 7.Tang J, Kern TS. Inflammation in diabetic retinopathy. Prog Retin Eye Res. 2011;30:343–58. doi: 10.1016/j.preteyeres.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sivak JM, Fini ME. MMPs in the eye: emerging roles for matrix metalloproteinases in ocular physiology. Prog Retin Eye Res. 2002;21:1–14. doi: 10.1016/s1350-9462(01)00015-5. [DOI] [PubMed] [Google Scholar]
- 9.Zheng Z, Chen H, Ke G, Fan Y, Zou H, Sun X, Gu Q, Xu X, Ho PC. Protective effect of perindopril on diabetic retinopathy is associated with decreased vascular endothelial growth factor-to-pigment epithelium-derived factor ratio: involvement of a mitochondria-reactive oxygen species pathway. Diabetes. 2009;58:954–64. doi: 10.2337/db07-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pons M, Marin-Castano ME. Nicotine increases the VEGF/PEDF ratio in retinal pigment epithelium: a possible mechanism for CNV in passive smokers with AMD. Invest Ophthalmol Vis Sci. 2011;52:3842–53. doi: 10.1167/iovs.10-6254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gao G, Li Y, Zhang D, Gee S, Crosson C, Ma J. Unbalanced expression of VEGF and PEDF in ischemia-induced retinal neovascularization. FEBS Lett. 2001;489:270–6. doi: 10.1016/s0014-5793(01)02110-x. [DOI] [PubMed] [Google Scholar]
- 12.Gao G, Li Y, Fant J, Crosson CE, Becerra SP, Ma JX. Difference in ischemic regulation of vascular endothelial growth factor and pigment epithelium-derived factor in brown Norway and Sprague Dawley rats contributing to different susceptibilities to retinal neovascularization. Diabetes. 2002;51:1218–25. doi: 10.2337/diabetes.51.4.1218. [DOI] [PubMed] [Google Scholar]
- 13.Bharadwaj AS, Appukuttan B, Wilmarth PA, Pan Y, Stempel AJ, Chipps TJ, Benedetti EE, Zamora DO, Choi D, David LL, Smith JR. Role of the retinal vascular endothelial cell in ocular disease. Prog Retin Eye Res. 2013;32:102–80. doi: 10.1016/j.preteyeres.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simó R, Villarroel M, Corraliza L, Hernandez C, Garcia-Ramirez M. The retinal pigment epithelium: something more than a constituent of the blood-retinal barrier–implications for the pathogenesis of diabetic retinopathy. J Biomed Biotechnol. 2010;2010:190724. doi: 10.1155/2010/190724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elner VM, Scales W, Elner SG, Danforth J, Kunkel SL, Strieter RM. Interleukin-6 (IL-6) gene expression and secretion by cytokine-stimulated human retinal pigment epithelial cells. Exp Eye Res. 1992;54:361–8. doi: 10.1016/0014-4835(92)90048-w. [DOI] [PubMed] [Google Scholar]
- 16.Broadhead ML, Becerra SP, Choong PF, Dass CR. The applied biochemistry of PEDF and implications for tissue homeostasis. Growth Factors. 2010;28:280–5. doi: 10.3109/08977191003604513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu X, Chen HH, Zhang LW. Potential therapeutic effects of pigment epithelium-derived factor for treatment of diabetic retinopathy. Int J Ophthalmol. 2013;6:221–7. doi: 10.3980/J.ISSN.2222-3959.2013.02.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matsuoka M, Ogata N, Minamino K, Higuchi A, Matsumura M. High levels of pigment epithelium-derived factor in the retina of a rat model of type 2 diabetes. Exp Eye Res. 2006;82:172–8. doi: 10.1016/j.exer.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 19.Matsuoka M, Ogata N, Minamino K, Matsumura M. Leukostasis and pigment epithelium-derived factor in rat models of diabetic retinopathy. Mol Vis. 2007;13:1058–65. [PMC free article] [PubMed] [Google Scholar]
- 20.Mohan N, Monickaraj F, Balasubramanyam M, Rema M, Mohan V. Imbalanced levels of angiogenic and angiostatic factors in vitreous, plasma and postmortem retinal tissue of patients with proliferative diabetic retinopathy. J Diabetes Complications. 2012;26:435–41. doi: 10.1016/j.jdiacomp.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 21.Li C, Chen P, Zhang J, Zhang L, Huang X, Yao Y, Che X, Fan X, Ge S, Wang Z. Enzyme-induced vitreolysis can alleviate the progression of diabetic retinopathy through the HIF-1α pathway. Invest Ophthalmol Vis Sci. 2013;54:4964–70. doi: 10.1167/iovs.12-11443. [DOI] [PubMed] [Google Scholar]
- 22.Stewart MW. The expanding role of vascular endothelial growth factor inhibitors in ophthalmology. Mayo Clin Proc. 2012;87:77–88. doi: 10.1016/j.mayocp.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Joussen AM, Poulaki V, Le ML, Koizumi K, Esser C, Janicki H, Schraermeyer U, Kociok N, Fauser S, Kirchhof B, Kern TS, Adamis AP. A central role for inflammation in the pathogenesis of diabetic retinopathy. FASEB J. 2004;18:1450–2. doi: 10.1096/fj.03-1476fje. [DOI] [PubMed] [Google Scholar]
- 24.Liu Y, Biarnes Costa M, Gerhardinger C. IL-1beta is upregulated in the diabetic retina and retinal vessels: cell-specific effect of high glucose and IL-1beta autostimulation. PLoS ONE. 2012;7:e36949. doi: 10.1371/journal.pone.0036949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kowluru RA, Kanwar M. Oxidative stress and the development of diabetic retinopathy: contributory role of matrix metalloproteinase-2. Free Radic Biol Med. 2009;46:1677–85. doi: 10.1016/j.freeradbiomed.2009.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kowluru RA, Mohammad G, dos Santos JM, Zhong Q. Abrogation of MMP-9 gene protects against the development of retinopathy in diabetic mice by preventing mitochondrial damage. Diabetes. 2011;60:3023–33. doi: 10.2337/db11-0816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miao F, Chen Z, Genuth S, Paterson A, Zhang L, Wu X, Li S, Cleary P, Riggs A, Harlan D, Lorenzi G, Kolterman O, Sun W, Lachin J, Natarajan R. the DCCT/EDIC Research Group. Evaluating the Role of Epigenetic histone modifications in the Metabolic Memory of Type 1 Diabetes. Diabetes. 2014 doi: 10.2337/db13-1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reddy MA, Tak Park J, Natarajan R. Epigenetic modifications in the pathogenesis of diabetic nephropathy. Semin Nephrol. 2013;33:341–53. doi: 10.1016/j.semnephrol.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kowluru RA, Santos JM, Mishra M. Epigenetic modifications and diabetic retinopathy. Biomed Res Int. 2013;2013:635284. doi: 10.1155/2013/635284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Egger G, Liang G, Aparicio A, Jones PA. Epigenetics in human disease and prospects for epigenetic therapy. Nature. 2004;429:457–63. doi: 10.1038/nature02625. [DOI] [PubMed] [Google Scholar]
- 31.Wu CJ, Yang CY, Chen YH, Chen CM, Chen LC, Kuo ML. The DNA Methylation Inhibitor 5-Azacytidine Increases Regulatory T Cells and Alleviates Airway Inflammation in Ovalbumin-Sensitized Mice. Int Arch Allergy Immunol. 2013;160:356–64. doi: 10.1159/000343030. [DOI] [PubMed] [Google Scholar]
- 32.Xiao D, Dasgupta C, Chen M, Zhang K, Buchholz J, Xu Z, Zhang L. Inhibition of DNA methylation reverses norepinephrine-induced cardiac hypertrophy in rats. Cardiovasc Res. 2014;101:373–82. doi: 10.1093/cvr/cvt264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barneda-Zahonero B, Parra M. Histone deacetylases and cancer. Mol Oncol. 2012;6:579–89. doi: 10.1016/j.molonc.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lin J, Sun B, Jiang C, Hong H, Zheng Y. Sirt2 suppresses inflammatory responses in collagen-induced arthritis. Biochem Biophys Res Commun. 2013;441:897–903. doi: 10.1016/j.bbrc.2013.10.153. [DOI] [PubMed] [Google Scholar]
- 35.Lappas M. Anti-inflammatory properties of sirtuin 6 in human umbilical vein endothelial cells. Mediators Inflamm. 2012;2012:597514. doi: 10.1155/2012/597514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ahmed S, Riegsecker S, Beamer M, Rahman A, Bellini JV, Bhansali P, Tillekeratne LM. Largazole, a class I histone deacetylase inhibitor, enhances TNF-α-induced ICAM-1 and VCAM-1 expression in rheumatoid arthritis synovial fibroblasts. Toxicol Appl Pharmacol. 2013;270:87–96. doi: 10.1016/j.taap.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crosson CE, Mani SK, Husain S, Alsarraf O, Menick DR. Inhibition of histone deacetylase protects the retina from ischemic injury. Invest Ophthalmol Vis Sci. 2010;51:3639–45. doi: 10.1167/iovs.09-4538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Diao JS, Xia WS, Yi CG, Wang YM, Li B, Xia W, Liu B, Guo SZ, Sun XD. Trichostatin A inhibits collagen synthesis and induces apoptosis in keloid fibroblasts. Arch Dermatol Res. 2011;303:573–80. doi: 10.1007/s00403-011-1140-1. [DOI] [PubMed] [Google Scholar]
- 39.Agudelo M, Gandhi N, Saiyed Z, Pichili V, Thangavel S, Khatavkar P, Yndart-Arias A, Nair M. Effects of alcohol on histone deacetylase 2 (HDAC2) and the neuroprotective role of trichostatin A (TSA). Alcohol Clin Exp Res. 2011;35:1550–6. doi: 10.1111/j.1530-0277.2011.01492.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suuronen T, Nuutinen T, Ryhanen T, Kaarniranta K, Salminen A. Epigenetic regulation of clusterin/apolipoprotein J expression in retinal pigment epithelial cells. Biochem Biophys Res Commun. 2007;357:397–401. doi: 10.1016/j.bbrc.2007.03.135. [DOI] [PubMed] [Google Scholar]
- 41.Yu Z, Zhang W, Kone BC. Histone deacetylases augment cytokine induction of the iNOS gene. J Am Soc Nephrol. 2002;13:2009–17. doi: 10.1097/01.asn.0000024253.59665.f1. [DOI] [PubMed] [Google Scholar]
- 42.Vishwakarma S, Iyer LR, Muley M, Singh PK, Shastry A, Saxena A, Kulathingal J, Vijaykanth G, Raghul J, Rajesh N, Rathinasamy S, Kachhadia V, Kilambi N, Rajgopal S, Balasubramanian G, Narayanan S. Tubastatin, a selective histone deacetylase 6 inhibitor shows anti-inflammatory and anti-rheumatic effects. Int Immunopharmacol. 2013;16:72–8. doi: 10.1016/j.intimp.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 43.Kyrylenko S, Kyrylenko O, Suuronen T, Salminen A. Differential regulation of the Sir2 histone deacetylase gene family by inhibitors of class I and II histone deacetylases. Cell Mol Life Sci. 2003;60:1990–7. doi: 10.1007/s00018-003-3090-z. [DOI] [PMC free article] [PubMed] [Google Scholar]