Abstract
Importance
Sudden unexpected death in epilepsy (SUDEP) is a common cause of mortality in patients with the disease but it is unknown how neurologists disclose this risk when counseling patients.
Objective
Examine SUDEP discussion practices of neurologists in the U.S. and Canada.
Design
An electronic, web-based survey was sent to 17558 neurologists in the U.S. and Canada. Survey questions included frequency of SUDEP discussion, reasons for discussing/not discussing SUDEP, timing of SUDEP discussions, and perceived patient reactions. We examined factors that influence the frequency of SUDEP discussion and perceived patient response using multivariate logistic regression.
Setting
Survey of U.S. and Canadian neurologists
Participants
Neurologists who completed post-graduate training and devoted >5% of their time to patient care.
Results
There was a response rate of 9.3%; 1200 respondents met eligibility criteria and completed surveys. Only 6.8% of respondents discussed SUDEP with nearly all (>90% of the time) of their patients with epilepsy/caregivers while 11.6% never discussed it. Factors that independently predicted whether SUDEP was discussed nearly all of the time were: number of epilepsy patients seen annually (OR 2.01, 95% CI 1.20-3.37, p < 0.01) and if the respondent had a SUDEP case in the past 24 months (OR 2.27, 95% CI: 1.37-3.66, p < 0.01). A majority of respondents (59.5%) reported that negative reactions were the most common response to a discussion of SUDEP. Having additional epilepsy/neurophysiology training was associated with an increased risk of a perceived negative response (OR 1.36, CI: 1.02-1.82, p = 0.038) while years in practice (OR 0.85, CI: 0.77 - 0.95, p < 0.005) and seeing both adults and children (OR 0.15, CI: 0.032-0.74, p = 0.02) were associated with a decreased likelihood of negative response.
Conclusions
U.S. and Canadian neurologists rarely discuss SUDEP with all patients with epilepsy/caregivers though discussions are more likely among neurologists who frequently see epilepsy patients or had a recent SUDEP in their practice. Perceived negative reactions to SUDEP discussions are common but not universal; more experienced neurologists may be less likely to encounter negative reactions suggesting there may be ways to frame the discussion that minimizes patient/caregiver distress.
Introduction
Sudden unexpected death in epilepsy (SUDEP) is the leading disease-related cause of mortality among people with seizure disorders [1]. Previously called sudden unexplained death, SUDEP is defined as a sudden and unexpected non-traumatic or non-drowning-related death in a person with epilepsy which may or may not associated with a recent seizure [2]. The incidence of SUDEP varies by several orders of magnitude depending on the population studied; it ranges from 0.09-1.2/1000 person-years in the general epilepsy population to 1.1-5.9/1000 person-years, in patients with medically-refractory to 6.3-9.3/1000 person-years in patients who are epilepsy surgery candidates [1, 3]. SUDEP rates are low in children with epilepsy with reported rates of 0.1-0.4 per 1000 person-years [3]. The mechanisms of SUDEP remain uncertain though frequent seizures, especially generalized tonic-clonic seizures (GTCS), are the greatest risk factor [4]. While it appears that seizure control reduces risk of SUDEP, there are no clear additional prevention strategies.
There is controversy whether or not to inform and counsel epilepsy patients and their caregivers about SUDEP, a typically rare outcome. Some, such as the National Institute for Health and Clinical Excellence (NICE) in the United Kingdom [5] and the Scottish Intercollegiate Guidelines Network (SIGN) [6], advocate that all patients with epilepsy be counseled about SUDEP as part of essential education about their disorder. Other authors suggest a more individualized approach such as waiting to discuss SUDEP when patients are ready to receive the information or when discussing anti-epileptic drug (AED) compliance or epilepsy surgery [7, 8] since patients with a low risk for SUDEP (e.g., well-controlled seizures) or low-risk syndromes (e.g. childhood absence epilepsy) may lead to unnecessary distress. Surveys of physicians in the UK[9, 10] and Italy [11] suggest that most physicians do not discuss SUDEP with all of their patients. A survey of 383 UK neurologist found that only 4.7% discussed SUDEP with all of their epilepsy patients, 61.2% discussed SUDEP with few of their patients and 7.5% never discussed SUDEP [9]. One third of the respondents felt that the discussion lead to anxiety though, interestingly, neurologists with a special interest in epilepsy had less negative reactions to the discussion. A more recent survey of 46 pediatric neurologists in the UK found that only 20% provided SUDEP information to all of their patients/caregivers [10]. The same study found that most parents (91%) wanted to know about SUDEP, often at diagnosis.
In the US and Canada, there are no national guidelines regarding SUDEP discussion. A recent statement by the American Epilepsy Society/Epilepsy Foundation joint task force on SUDEP[8] as well as the recent Institute of Medicine report on epilepsy [12] provide some guidance on discussing SUDEP, stating that SUDEP should be discussed in the context of comprehensive education about epilepsy. However, there is no accepted policy or consensus among the general neurology community in the US and Canada regarding this matter. Neurologists provide the majority of epilepsy care and the current practices and understanding of SUDEP is unknown. Furthermore, reasons why neurologists do and do not discuss SUDEP are not understood. Therefore, we undertook a survey of neurologists in the US and Canada to assess knowledge and experience with SUDEP. We examined the frequency of SUDEP discussion, reasons for discussing and not discussing SUDEP as well as understanding SUDEP risk factors.
Methods
We performed an electronic, web-based survey to assess knowledge and experience with SUDEP among US and Canadian neurologists in October 2011. A copy of the survey is included in the supplemental materials (Supplement 1). An invitation to participate in the survey was sent to 17558 unique e-mail addresses of neurologists obtained through the Epilepsy Therapy Project. Subjects were instructed to complete the survey if they were neurologists who devoted >5% of their time to clinical care and had completed post-graduate training. A link to opt out of the survey was also included in the invitation. Two rounds of reminder e-mails were sent 2-3 weeks apart to subjects. The survey was performed using Limequery (limequery.org).
Survey questions included demographic information about the respondent including their practice (adult and/or child neurology; academic versus private practice), additional training in epilepsy or clinical neurophysiology, years in practice (0-5, 5-10, 10-15 or >15) and average number of epilepsy patients followed per year (1-10, 11-20, 21-50, 51-100, and >100). To examine knowledge about SUDEP, respondents were asked to identify known SUDEP risk factors at the time of survey distribution from a list of seven items. A composite knowledge score was determined by subtracting the number of identified incorrect items (sleeping on two or more pillows; EKG showing QTc at the upper limit of normal; nocturnal complex partial seizures) from the number of identified correct items (treatment with 3 or more AEDs, lack of AED therapy and recent GTCS); the possible scores ranged from -3 to 4. This score is not validated but the questions were determined based on the currently available literature.
Subjects who responded that they followed at least one patient per year with epilepsy were asked about their experience with SUDEP and discussing SUDEP with patients and caregivers. They were asked how many of their adult (>18 years old) and pediatric (<18 years old) patients had definite or probable SUDEP (using the definition of Annegers, 1997) in the past 24 months. Respondents were asked how often they discussed SUDEP with patients or caregivers and if they discussed SUDEP, respondents were asked when they discussed it and what clinical factors and lifestyle factors influenced who they discuss SUDEP with. Respondents were also asked whether patient age factored in to their discussion of SUDEP and if so, what patient age groups warranted a discussion of SUDEP (0-8, 9-16, 17-21, 22-54, >55). Respondents who discussed SUDEP were also queried about their three most common reactions from patients and caregivers. Free text responses under the other response category were subsequently categorized into negative (e.g. anger, despair, sadness), neutral (e.g. confusion, concern, denial), and positive (e.g. appreciative, motivated to comply, inquisitive, trust) responses for use in further analysis. Respondents were also asked about reasons for not discussing SUDEP with patients and if they felt knowledge of SUDEP would improve compliance with AEDs. We also inquired about tools that respondents would use to support and educate patients and caregivers around the issue of SUDEP.
In addition to the descriptive statistics of the responses, we examined which practitioner factors were independently associated with discussing SUDEP nearly all the time. Using multivariate logistic regression (SAS, Cary, NC), we examined whether having addition training in epilepsy/clinical neurophysiology, being in academic or private practice, number of years in practice, <100 versus >100 epilepsy patients seen per year, having SUDEP occur in a patient in the past 24 months, or being knowledgeable about SUDEP (defined as a SUDEP knowledge score >2) influenced whether respondents discussed SUDEP with nearly all of the their patients (≥90% of the time). We also examined whether the same factors and the additional factor of discussing SUDEP with most or nearly all of their patients (≥50% of the time) discussion influenced whether the respondents identified the most common response to SUDEP discussion as a “negative” one. Responses classified as “negative” included choices such as anxiety, depression, anger, distress, fear and similar responses. Independent factors which demonstrated a p < 0.2 of an odds ratio different than 1 were included in the multivariate model for further analysis. Additional analyses were performed using Chi-squared test for comparison of categorical data.
The study was approved by the institutional review board at the NYU School of Medicine.
Results
Of the 17558 invitations sent, we received 1645 responses (9.3 % response rate). Response rates among Canadian neurologist (8.6%) did not differ from the overall group. Of those, 425 opted out of the survey, typically because they did not meet one of the inclusion criteria (active clinical practice or still in residency or fellowship training). There were 1200 completed surveys. Because we do not know the number of incorrect email addresses and additional characteristics of all names on our mailing list, the true proportion of eligible subjects responding to the survey is unknown. The characteristics of the respondents are listed in Table 1. The majority (76.4%) identified themselves as adult neurologists and 33.8% of respondents had additional training in epilepsy or clinical neurophysiology. Most respondents (92.8%) were US-based neurologists and 37.1% were in academic practice. A majority (54.1%) were in practice for 10 or more years and 95.8% saw at least one patient with epilepsy annually; 43.0% saw >100 patients with epilepsy per year. Most respondents (82.8%) had incomplete knowledge of published SUDEP risk factors defined as SUDEP knowledge scores of ≤ 2.
Table 1. Characteristics of the survey respondents.
| N (total=1200) | % | |
|---|---|---|
| Adult neurologist only | 917 | 76.4% |
| Child neurologist only | 243 | 20.3% |
| Both adult and child neurologist | 24 | 2.0% |
| Additional training in epilepsy or neurophysiology | 405 | 33.8% |
| Academic practice | 445 | 37.1% |
| Private practice | 233 | 19.4% |
| US-based | 1114 | 92.8% |
| Canada-based | 86 | 7.2% |
| Years in Practice | ||
| 0-5 | 362 | 30.2% |
| 5-10 | 188 | 15.7% |
| 10-15 | 177 | 14.8% |
| > 15 | 472 | 39.3% |
| No response | 1 | 0.1% |
| Patients with epilepsy per year | ||
| None | 47 | 3.9% |
| 1-10 | 92 | 7.7% |
| 11-20 | 110 | 9.2% |
| 21-50 | 208 | 17.3% |
| 51-100 | 224 | 18.7% |
| >100 | 516 | 43.0% |
| SUDEP Risk Factor Knowledge Score | ||
| >2 | 206 | 17.2% |
| ≤2 | 995 | 82.8% |
Of the 1150 responders who saw at least one epilepsy patient annually, 26.1% had at least one SUDEP in the past 24 months. As expected, the number of epilepsy patients seen per year was correlated with the proportion of respondents who had a SUDEP death among their patients. While only 2.2% (N=2/92) of neurologists who see 1-10 epilepsy patients per year had a SUDEP in the past 2 years, 41.7% (N=215/516) of neurologists who see >100 epilepsy patients annually had a SUDEP (p < 0.0001, χ2 = 59, df = 2). The median number of SUDEPs reported was 1 with 90% of neurologists who had a SUDEP reporting between 1 and 4.
There was variability in how often neurologists discussed SUDEP with patients or their caregivers (Figure 1). Only 6.8% (N=78/1150 eligible respondents) discussed SUDEP with nearly all of their epilepsy patients and 14.0% (N = 161/1150) discussed it most of the time (50-90%). The majority of neurologists reported discussing SUDEP sometimes (33.4%, N= 384/1150) or rarely (30.0%, N = 345/1150) while 11.6% (N = 133/1150) reported never discussing SUDEP with patients or their caregivers. Most neurologists (93.1%) discussed SUDEP themselves with patients. In some practices (7.0%), a nurse discussed SUDEP.
Figure 1.
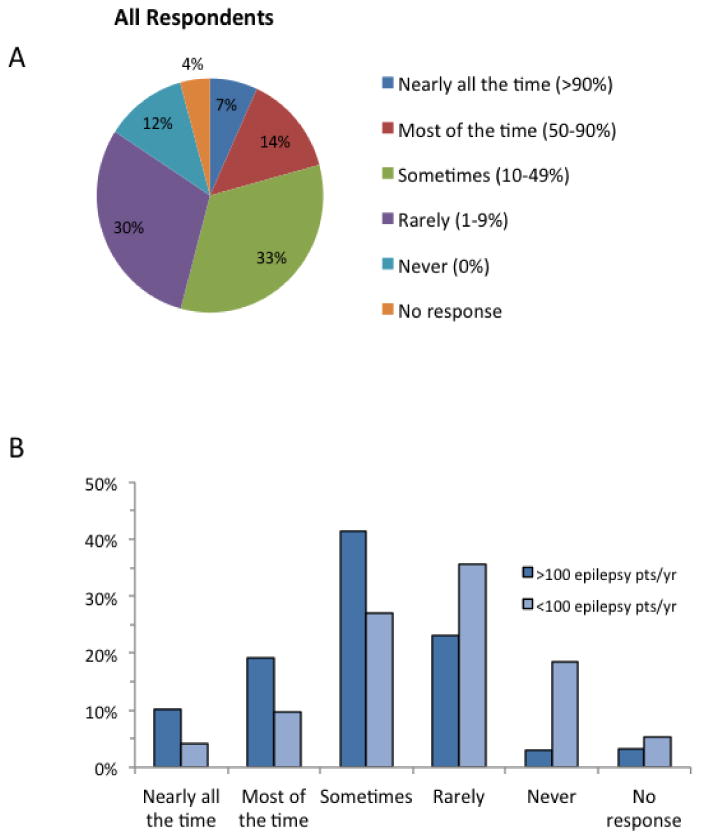
Responses to “How frequently do you discuss SUDEP with patients or their caregivers.” A. Distribution of responses for all neurologists. A majority of neurologists discuss SUDEP only sometimes (10-49% of the time). B. Distribution of responses based on the number of epilepsy patients seen annually by the provider. Neurologists who see > 100 epilepsy discuss SUDEP with more of their patients than neurologists who only less epilepsy patients per year.
Additional epilepsy/neurophysiology training, greater than 100 epilepsy patients seen annually, years in practice, and SUDEP in the past 24 months were all associated with increased likelihood of discussing SUDEP nearly all the time in univariate analysis (p<0.1) and these variables were used in the multivariate logistic regression model. In multivariate analysis, >100 epilepsy patients seen annually (referent is < 100 annual epilepsy patients, OR 2.01, 95% CI 1.20-3.37, p = 0.008) and SUDEP in the past 24 months (OR 2.27, 95% CI: 1.37-3.66, p < 0.01) independently predicted whether SUDEP was discussed nearly all of the time.
The majority of neurologists who discuss SUDEP (N = 1017), do so when they feel a patient is at high risk (62.2%) or when patient asks (57.7%). Other times when SUDEP is discussed include spontaneously during a follow up appointment (27.4%) or at the time of initiating AEDs (19.3%); 9.2% of respondents only discussed SUDEP when a patient/caregiver asks (Figure 2A). Poor compliance with AEDs (80.9%) and intractable epilepsy (79.4%) were the most common patient factors that lead neurologists to discuss SUDEP (Figure 2B).
Figure 2.
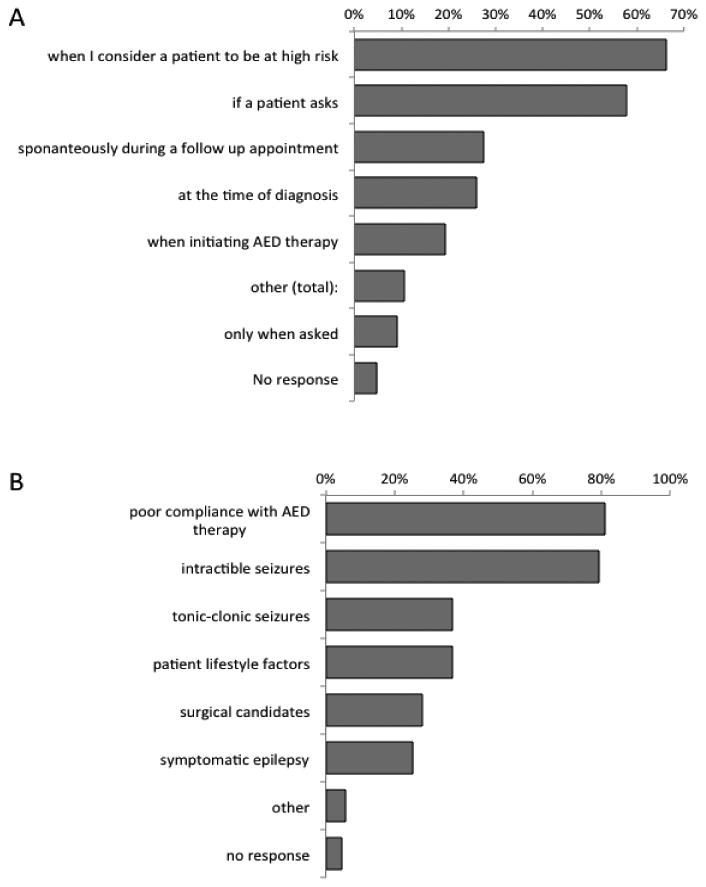
Plot of reasons respondents provided for discussing SUDEP. A, A plot of the most common situations when SUDEP counseling occurs by respondents by the 1017 respondents who discuss it. Respondents could provide more than one response. The majority of times, the neurologist provided counseling on SUDEP when he felt the patient was at high risk. B, A plot of the most common patient factors that influence whether SUDEP counseling is provided (N=1017). Most respondents counseled patients with intractable seizures and poor medication compliance.
Patient reactions, as perceived by the respondents, were variable (Table 2). The most common reported reaction was anxiety; 40.4% of respondents ranked this as the most frequent reaction. Other reactions ranked as most frequent included distress (21.6%), appreciation (18.5%), relief (2.5%), and depression (0.6%). Other reactions (5.1%) included “concern,” “surprise,” “confusion,” “fear,” “acceptance,” “anger” and “disbelief.” Negative responses where the most common patient/caregiver responses for 59.5% of neurologists who discussed SUDEP with at least some of their patients (N = 605/1017). In univariate analysis, scope of neurologic practice (adult, child, both), additional epilepsy/neurophysiology training, > 100 epilepsy patients seen annually, years in practice, and discussing SUDEP ≥ 50% of the time were associated with a perceived negative response (p<0.1) and were used in the multivariate logistic regression model. In the multivariate analysis, having additional epilepsy/neurophysiology training was associated with an increased risk of a perceived “negative” response being most common (OR 1.36, CI: 1.02-1.82, p = 0.038) while years in practice (OR 0.85, CI: 0.77 - 0.95, p = 0.004) and seeing both adults and children (OR 0.15, CI: 0.032-0.74, p = 0.02) were associated with a decreased likelihood of negative reaction. It is possible that some respondent who had addition neurophysiology training focus their practice on electrodiagnostic procedures such EMG and intraoperative monitoring and therefore may not be comfortable with discussions of epilepsy risks. We therefore compared the frequency of perceived “negative” responses to SUDEP discussion among respondents who had additional epilepsy training to those who had additional neurophysiology training and found that, in univariate analysis, additional epilepsy training was associated with an increased likelihood of negative response (OR=1.58, CI:1.20-2.07, p = 0.0014).
Table 2.
Reported perceived reactions to SUDEP discussions among the 1017 respondents who discussed SUDEP with patients/caregivers.
| Response | Most common reaction | 2nd most common reaction | 3rd most common reaction | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| anxiety | 388 | 40.4% | 316 | 33.1% | 127 | 13.3% |
| distress | 208 | 21.6% | 274 | 28.7% | 134 | 14.0% |
| appreciation | 178 | 18.5% | 145 | 15.2% | 196 | 20.5% |
| indifference | 108 | 11.2% | 97 | 10.1% | 205 | 21.4% |
| other | 49 | 5.1% | 38 | 4.0% | 117 | 12.2% |
| relief | 24 | 2.5% | 34 | 3.6% | 45 | 4.7% |
| depression | 6 | 0.6% | 52 | 5.4% | 132 | 13.8% |
The most common reason that neurologists gave for not discussing SUDEP with some or all of their patients/caregivers was that they felt the patient is at low risk (53.6%, N = 575/1019). Respondents were also reluctant to discuss SUDEP because of fear of negatively affecting mood or quality of life (32.8%) or because there is no proven prevention (33.8%). A full list of responses for why SUDEP is not discussed is provided in Table 3.
Table 3.
Reasons respondents do not discuss SUDEP with patients/caregivers. Respondents could report more than one reason.
| Response | N (total=1072) | % |
|---|---|---|
| Patient is at minimal or no risk | 575 | 53.6% |
| There is no proven way to prevent SUDEP | 362 | 33.8% |
| The information could affect my patient's quality of life or mood | 352 | 32.8% |
| I have not yet established a trusting relationship with the patient | 309 | 28.8% |
| SUDEP is so rare and the risks of discussion of outweigh the potential benefits | 275 | 25.7% |
| I do not have sufficient time to discuss SUDEP during an office visit | 198 | 18.5% |
| There is insufficient information about SUDEP | 196 | 18.3% |
| I do not know enough about SUDEP | 191 | 17.8% |
| The patient lacks an adequate support network | 163 | 15.2% |
| other (thematic groups) | 65 | 6.1% |
| No response | 53 | 4.9% |
| Information is available through other sources | 19 | 1.8% |
Discussion
The results of this study represent the largest survey of the experience and attitudes of neurologists with SUDEP available to date. While the study was limited by a relatively low response rate as typical of many internet-based surveys, 1200 neurologists who responded to the survey represent a broad range of practice types including academic and private practice, high and low volume epilepsy case load and variable practice duration suggesting that they are a representative sample of neurologists currently practicing in the US and Canada. However, despite the diversity of respondents, the generalizability of our findings should be interpreted with caution because of the low responder rate. The relatively low rate of SUDEP discussion and accurate identification of SUDEP risk factors suggests that our survey results were not biased by responders with special expertise and interest in SUDEP. Like smaller surveys of neurologists in the UK9 and Italy[11], US and Canadian neurologists do not universally discuss the risks of SUDEP with their epilepsy patients. Few neurologists report discussing SUDEP with a majority of their patients and most discuss it less with half of their patients. One in seven neurologists never discuss SUDEP. Rates of reported SUDEP discussion are higher among neurologists who see a high volume of patients with epilepsy. These neurologists may be more comfortable discussing this sensitive topic, have more time and resources devoted to epilepsy education or have more clinical experience with SUDEP. Indeed, SUDEP cases were not uncommon among neurologists who see >100 patients with epilepsy annually; approximately ¼ of respondents in this category had a SUDEP in the past 2 years and personal experience with this unfortunate outcome appears to influence how often it is discussed.
While SUDEP is not universally discussed, responses suggest that the most common scenario when it is discussed is when neurologists feel patients are at high risk for SUDEP. While many respondents reported intractable epilepsy as a risk factor that spurs SUDEP discussion, modifiable factors such as medication non-compliance and alcohol use were the most frequently reported reasons for discussing SUDEP, suggesting these conversations are often intended to limit risk taking behavior. The most common reasons that neurologists did not discuss SUDEP with individual patients are because they felt that their patients were at low risk and there were no known preventative measures. However, these sentiments may reflect incomplete knowledge of SUDEP risk factors. Though less common, SUDEP can occur in “low-risk” patients such as those without GTCS [13]. Furthermore, pooled analysis of SUDEP rates in randomized controlled trials of add-on AED therapy in patients with intractable partial epilepsy supports the idea that controlling the frequency of seizures may be the most effective way to reduce seizures; patients receiving effective doses of adjunctive AEDs had a 7-fold reduction in SUDEP rates compared to those receiving placebo[14]. This supports extensive evidence from the literature that most SUDEPs follow seizures, usually generalized tonic-clonic seizures. These include epidemiological studies, SUDEPs witnessed in the community or recorded on video-EEG, and neuropathological data.1,3,4 It is possible that educational campaigns targeting knowledge gaps among physicians may make neurologists more comfortable talking about SUDEP with patients and caregivers.
Nearly 60% of respondents felt that the most common reaction following a discussion of SUDEP with patients or their caregivers was negative (e.g. fear, anxiety, depression). It is possible that worry about upsetting the patient or caregiver limits SUDEP discussion. However, it appears that experienced neurologists (years in practice) and those with a diverse age group of patients and caregivers (seeing adults and children) were less likely to perceive negative responses to SUDEP discussion. This suggests that it may be possible to frame the discussion of SUDEP with patients and caregivers in a way to minimize distress. Unlike the survey performed in the UK [9], we found that addition epilepsy training was associated with increased rates of a negative response in our multivariate analysis despite controlling for number of epilepsy patients seen and disclosure rates. This finding requires further exploration but suggests that even epilepsy experts may need guidance on how to best approach the topic of SUDEP.
Our non-validated assessment of SUDEP risk factors revealed that most neurologists (82.8%) have limited knowledge about this subject. This suggests educational needs include neurologists as well as patients and caregivers. Therefore, an accurate understanding about risk factors would assist neurologists in educating their patients. It is possible that more effective education of neurologists and patients could reduce the number of SUDEPs through a greater emphasis on seizure control, especially generalized tonic-clonic seizures, through referral to epilepsy centers, improved compliance and lifestyle modifications. Further studies are needed to examine the effect of SUDEP disclosure on modifiable SUDEP risk factors and seizure-related outcomes. Data supporting the impact of SUDEP counseling on these factors could provide evidence to support a universal, though individually-tailored, approach to disclosure.
In conclusion, like smaller surveys, albeit with higher response rates, performed in the UK and Italy, we found that neurologists do not discuss SUDEP with patients with epilepsy often and when they do, they do not discuss it with all of their epilepsy patients. While recent Epilepsy Foundation/AES guidelines recommend some counseling about SUDEP as part of general epilepsy education, it is not clear how well these recommendations have been disseminated to the neurology community, especially among general neurologists and other non-specialists. Further work is needed to expand education about SUDEP and provide guidance to practioners about how to best counsel their patients because there is mounting evidence that patients and caregivers[10], [15] would like to be told about this rare consequence of their epilepsy.
Supplementary Material
Highlights.
U.S. & Canadian neurologists rarely discuss it with their patients and caregivers
SUDEP discussions are more common among neurologists who treat epilepsy patients
Neurologists commonly perceive negative reactions to SUDEP discussions
Acknowledgments
This study was funded by Epilepsy Therapy Project and FACES (finding a cure for epilepsy and seizures). Dr. Friedman also received support from NYU CTSA grant UL1TR000038 from the National Center for the Advancement of Translational Science (NCATS), NIH. The funding agencies had no role in the design or conduct of this study. Dr. Friedman and Mr. Stephens had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Disclosures: Drs. Friedman and Devinsky have no relevant disclosures. Mr. Stephens has no relevant disclosures.
Dr. Donner is a cofounder of SUDEPAware, a not-for-profit organization dedicated to raising awareness and understanding of Sudden Unexpected Death in Epilepsy (SUDEP).
Ms. Wright is currently the director of the SUDEP Institute, a project lead by the Epilepsy Foundation to promote advocacy and research about SUDEP and other causes of mortality in epilepsy.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Devinsky O. Sudden, unexpected death in epilepsy. The New England journal of medicine. 2011;365:1801–11. doi: 10.1056/NEJMra1010481. [DOI] [PubMed] [Google Scholar]
- 2.Nashef L. Sudden Unexpected Death in Epilepsy: Terminology and Definitions. Epilepsia. 1997;38:S6–S8. doi: 10.1111/j.1528-1157.1997.tb06130.x. [DOI] [PubMed] [Google Scholar]
- 3.Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current knowledge and future directions. Lancet Neurology. 2008;7:1021–31. doi: 10.1016/S1474-4422(08)70202-3. [DOI] [PubMed] [Google Scholar]
- 4.Hesdorffer DC, Tomson T, Benn E, Sander JW, Nilsson L, Langan Y, Walczak TS, Beghi E, Brodie MJ, Hauser A. Combined analysis of risk factors for SUDEP. Epilepsia. 2011;52:1150–9. doi: 10.1111/j.1528-1167.2010.02952.x. [DOI] [PubMed] [Google Scholar]
- 5.National Institute for Health and Clinical Excellence. The diagnosis and management of the epilepsies in adults and children in primary and secondary care. 2007 CG20. [Google Scholar]
- 6.Scottish Intercollegiate Guidelines Network. Diagnosis and management of epilepsy in adults: Guideline 70. 2001 [Google Scholar]
- 7.Brodie MJ, Holmes GL. Should all patients be told about sudden unexpected death in epilepsy (SUDEP)? Pros and Cons. Epilepsia. 2008;49(Suppl 9):99–101. doi: 10.1111/j.1528-1167.2008.01933.x. [DOI] [PubMed] [Google Scholar]
- 8.So EL, Bainbridge J, Buchhalter JR, Donalty J, Donner EJ, Finucane A, Graves NM, Hirsch LJ, Montouris GD, Temkin NR, Wiebe S, Sierzant TL. Report of the American Epilepsy Society and the Epilepsy Foundation Joint Task Force on Sudden Unexplained Death in Epilepsy. Epilepsia. 2009:50. doi: 10.1111/j.1528-1167.2008.01906.x. [DOI] [PubMed] [Google Scholar]
- 9.Morton B, Richardson A, Duncan S. Sudden unexpected death in epilepsy (SUDEP): don't ask, don't tell? Journal of neurology, neurosurgery, and psychiatry. 2006;77:199–202. doi: 10.1136/jnnp.2005.066852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gayatri NA, Morrall MCHJ, Jain V, Kashyape P, Pysden K, Ferrie C. Parental and physician beliefs regarding the provision and content of written sudden unexpected death in epilepsy (SUDEP) information. Epilepsia. 2010;51:777–82. doi: 10.1111/j.1528-1167.2009.02483.x. [DOI] [PubMed] [Google Scholar]
- 11.Vegni E, Leone D, Canevini MP, Tinuper P, Moja EA. Sudden unexpected death in epilepsy (SUDEP): a pilot study on truth telling among Italian epileptologists. Neurol Sci. 2011;32:331–5. doi: 10.1007/s10072-010-0365-7. [DOI] [PubMed] [Google Scholar]
- 12.England MJ, Liverman CT, Schultz AM, Strawbridge LM. Epilepsy across the spectrum: Promoting health and understanding.: A summary of the Institute of Medicine report. Epilepsy & Behavior. 2012;25:266–276. doi: 10.1016/j.yebeh.2012.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Langan Y, Nashef L, Sander JW. Case-control study of SUDEP. Neurology. 2005;64:1131–3. doi: 10.1212/01.WNL.0000156352.61328.CB. [DOI] [PubMed] [Google Scholar]
- 14.Ryvlin P, Cucherat M, Rheims S. Risk of sudden unexpected death in epilepsy in patients given adjunctive antiepileptic treatment for refractory seizures: a meta-analysis of placebo-controlled randomised trials. Lancet Neurol. 2011 doi: 10.1016/S1474-4422(11)70193-4. [DOI] [PubMed] [Google Scholar]
- 15.RamachandranNair R, Jack SM, Meaney BF, Ronen GM. SUDEP: What do parents want to know? Epilepsy & Behavior. 2013;29:560–564. doi: 10.1016/j.yebeh.2013.09.040. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


