Patients with anti-N-methyl-D-aspartate-glutamic-receptors (NMDAR) encephalitis often develop complex abnormal movements that may manifest early in the course of illness.1 Exceptionally, movement disorders are the prominent manifestation in patients with NMDAR encephalitis who do not develop the full spectrum of symptoms.2 Here, we report a patient who developed paroxysmal exercise-induced foot weakness early in the course of anti-NMDAR encephalitis.
Case Report
A 17-year-old boy developed paroxysmal exercise-induced right foot weakness that occurred many times per day, without behavioral change. He had no medical or psychiatric history and functioned very well socially and academically. Two weeks later, he developed hyperthermia and convulsive status epilepticus. The patient was admitted to another hospital, intravenous valproate resolved the status, brain MRI and extensive blood tests including glucose were normal. The CSF revealed 6 white blood cells/μl with normal glucose and slightly increased protein concentrations without oligoclonal bands. The diagnosis was viral encephalitis with epileptic status, for which oral valproate (1.0 gr/day) was prescribed.
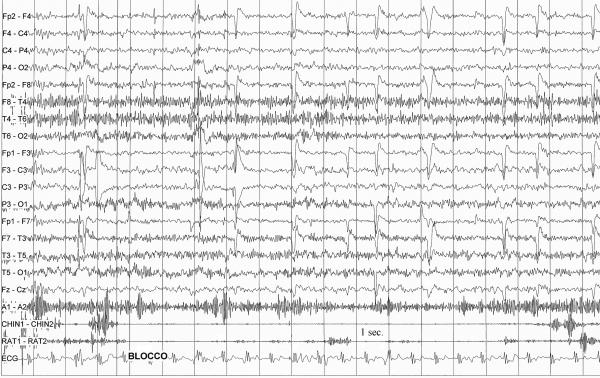
After two weeks, he came to us because the paroxysmal episodes of right foot weakness persisted. They started suddenly after 2-3 minutes of running, lasted up to 1-2 minutes and disappeared completely after rest. They recurred any time he began to running without any refractory period or other triggering factors. They were not carbohydrate-induced and no findings occurred in the left foot. Neurological examination between attacks was normal. EEG was normal, as also electromyography and cortical somatosensory evoked potentials. During attacks, neurological examination revealed weakness of tibialis anterior (grade 1/5) and gastrocnemius (grade 3/5) muscles, and video-polygraphy (see VIDEO) showed transient loss of lower limb muscle activity without any EEG changes (Figure). There was no aura, concomitant autonomic involvement, pain or sensory signs. NMDAR antibodies were present in CSF (1:4) and serum (1:100). No tumor was found. He was treated with intravenous methylprednisolone (1 gr/daily for 5 days) plus immunoglobulins (0.4 gr/kg for 5 days) with rapid resolution of his symptoms. Eight months later he is asymptomatic, despite the tapering of valproate.
Figure.
EEG-polygraphic recording of an episode of paroxysmal right foot weakness triggered by repetitive right foot flex-extensions that resembled walking. Note the transitory (11 sec.) loss of muscular activity in the right tibialis (Chin1-2) and gastrocnemious (RAT1-2) muscles, without any EEG changes. During the episodes, muscle activity was maintained in the right quadriceps muscle (A1-A2).
Discussion
Our case enlarges the spectrum of abnormal movements as presentation of oligosymptomatic anti-NMDAR encephalitis.1,2 Recognition of these peculiar episodes and their association with NMDAR antibodies should prompt consideration of immunotherapies, and might prevent the onset and long-term consequences of full-blown encephalitis. The present case gives further evidence of young patients with NMDAR antibodies encephalitis who are less likely to have a tumor, and may have a milder course.3
Regarding the nature of these episodes, we believe that the overall evidences argue in favor of a movement disorder rather than an epileptic phenomenon. Indeed, EEG was unchanged during attacks; moreover the patient had no other epileptic phenomena or impaired consciousness during attacks. They may be considered the negative motor counterpart of exercise-induced dyskinesia,4 and are close to the complex movement disorders with a variable distribution and response to sensory stimulation, including unilateral symptoms, which often occur in patients with anti-NMDAR encephalitis.1-3,5-6 Conversely, they differ from episodic paralysis syndromes in which weakness typically develops over minutes to hours and involves the proximal musculature.7
Supplementary Material
Panel shows (A) immunoreactivity of CSF of the patient (diluted 1:2) with a section of rat hippocampus giving the typical neuropil hippocampal reactivity seen with NMDAR antibodies, and (B) the reactivity with cultures of dissociated rat hippocampal neurons, demonstrating cell surface reactivity. In addition, the serum and CSF of the patient reacted with NR1 subunit of the NMDAR in a cell based assay (not shown here).
Video-polygraphic recording of three consecutive episodes of paroxysmal right foot weakness triggered by repetitive right foot flex-extensions that resembled walking. During the third attack, neurological examination revealed weakness of tibialis anterior (grade 1/5) and gastrocnemius (grade 3/5) muscles.
Acknowledgments
Work supported in part by the National Institutes of Health RO1NS077851, RO1MH094741, the National Cancer Institute RO1CA089054, Fondo de Investigaciones Sanitarias (FIS, 11/01780), and Fundació la Marató de TV3 (Josep Dalmau). Dr. Dalmau has a research grant from Euroimmun, and receives royalties from patents for the use of Ma2 and NMDAR as autoantibody tests.
Footnotes
Disclosure: AL, AQ, and AG report no conflicts of interest.
Roles: AG and AL contributed to design, conceptualization of the study, interpretation of the data, drafting and revising the manuscript. AQ and JD contributed to the interpretation of the data, and revising the manuscript.
References
- 1.Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011;10:63–74. doi: 10.1016/S1474-4422(10)70253-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rubio-Agustí I, Dalmau J, Sevilla T, Burgal M, Beltran E, Bataller L. Isolated hemidystonia associated with NMDA receptor antibodies. Mov Disord. 2011;26:351–352. doi: 10.1002/mds.23315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Florance NR, Davis RL, Lam C, et al. Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol. 2009;66:11–18. doi: 10.1002/ana.21756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bruno MK, Hallett M, Gwinn-Hardy K, et al. Clinical evaluation of idiopathic paroxysmal kinesigenic dyskinesia: new diagnostic criteria. Neurology. 2004;63:2280–22877. doi: 10.1212/01.wnl.0000147298.05983.50. [DOI] [PubMed] [Google Scholar]
- 5.Kleinig TJ, Thompson PD, Matar W, et al. The distinctive movement disorder of ovarian teratoma-associated encephalitis. Mov Dis. 2008;23:1256–1261. doi: 10.1002/mds.22073. [DOI] [PubMed] [Google Scholar]
- 6.Labate A, Irani SR, Vincent A, Gambardella A, Piane EL, Cianci V, Aguglia U. Anti-NMDA receptor encephalitis: a video case report. Epileptic Disord. 2009;11:267–269. doi: 10.1684/epd.2009.0268. [DOI] [PubMed] [Google Scholar]
- 7.Venance SL, Cannon SC, Fialho D, et al. The primary periodic paralyses: diagnosis, pathogenesis and treatment. Brain. 2006;129:8–17. doi: 10.1093/brain/awh639. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Panel shows (A) immunoreactivity of CSF of the patient (diluted 1:2) with a section of rat hippocampus giving the typical neuropil hippocampal reactivity seen with NMDAR antibodies, and (B) the reactivity with cultures of dissociated rat hippocampal neurons, demonstrating cell surface reactivity. In addition, the serum and CSF of the patient reacted with NR1 subunit of the NMDAR in a cell based assay (not shown here).
Video-polygraphic recording of three consecutive episodes of paroxysmal right foot weakness triggered by repetitive right foot flex-extensions that resembled walking. During the third attack, neurological examination revealed weakness of tibialis anterior (grade 1/5) and gastrocnemius (grade 3/5) muscles.