Abstract
Purpose
Children's physical activity (PA) levels are commonly assessed in pediatric clinical research, but rigorous self-report assessment tools for children are scarce, and computer adaptive test implementations are rare. Our objective was to improve pediatric self-report measures of activity using semi-structured interviews with experts and children for conceptualization of a child-informed framework.
Methods
Semi-structured interviews were conducted to conceptualize physical activity, sedentary behaviors, and strengthening activities. We performed systematic literature reviews to identify item-level concepts used to assess these 3 domains.
Results
We developed conceptual frameworks for each domain using words and phrases identified by children as relevant.
Conclusions
Semi-structured interview methods provide valuable information of children's perspectives and the ways children recall previous activities. Conceptualized domains of physical activity are based on the literature and expert views that also reflect children's experiences and understanding providing a basis for pediatric self-report instruments.
Keywords: adolescent; child; female; health status; humans; information systems; male; outcome assessment (health care)/methods; parents; pediatrics/methods; physical activities; sedentary lifestyle; strengthening, quality of life
Introduction
Physical activity (PA) and sedentary behaviors (SB) are health behaviors often assessed in clinical research.1–3 Activity level is associated with musculoskeletal coordination, sensorimotor integration, and neuromotor skills in children, each an essential factor for physical and cognitive development.1 Further, children’s social competencies and wellbeing are enhanced through participation in active sports and play.3 The detrimental effects of a sedentary lifestyle on development, current and future health have gained increasing attention in the past decade with numerous interventions directed at promoting a healthy level of PA in combination with minimization of SB.
Commonly measurement of PA and SB include direct measures of metabolism or energy expenditure(e.g. doubly labeled water technique),physiological measures (e.g. heart rate) or objective monitoring of motion (e.g. pedometers, step activity monitors, or accelerometers). Objective monitoring devices are commonly used to assess absolute motion performed by the individual during specified time periods by detecting bodily acceleration signals. These tools provide reliable assessments of motion related to energy expenditure, but are limited by inconsistencies in methods used to score and analyze resultant data, a lack of standardized cut-points that reflect meaningful differences in motion among children, and by the cost, burden and compliance issues associated with their use.2,6 Further, such motion detection devices do not adequately measure physical activities performed with restricted motion such as during force production (e.g., weight lifting) or activities that promote flexibility (e.g., stretching).
Though objective monitoring of PA is quite common, PA behavior assessment is typically done using self-reports as the main or only method of data collection.5 Self-report measures (e.g. PA recalls, logs or diaries), of PA and SB remain necessary elements of assessments performed by clinicians, including physical therapists, in clinical practice and for clinical effectiveness research. Both PA and SB are complex and multi-dimensional concepts consisting of varied activity types, contexts and intensities that have different effects on clinical health.4 Haskell4 recently noted that PA self-report has been and will continue to be a highly valuable research methodology to support development and evaluation of health guidelines for PA, SB and strengthening activities. While recent technological advances have made direct measurement of motion related to PA more common, health and behavioral research examining PA as an exposure or outcome often relies on self-report as the principal method of data collection.5 Hence, the development of valid and reliable self-report measures based on theoretically based definitions of PA and SB continues to be a high priority within the clinical research community.
Self-reports measures of PA and SB are necessary to support development and evaluation of health guidelines for population level assessments of activity.4 A variety of self-report PA measures for young people are available in the literature but few integrate input from children directly in their development.7 In addition, most were developed to be administered as traditional fixed length instruments, surveys in which every respondent answers the same questions regardless of their relevance to their condition or level of PA.
Computer adaptive tests (CATs) for self-report have become more common in both clinical research and practice, and provide a more efficient and often more precise way to measure certain health concepts than do traditional fixed length surveys.8 The foundation of CATs are large sets of calibrated items, referred to as an item bank. All items in an item bank consistently scale along a dimension of low to high values of the trait of interest (e.g. PA or SB in our case) modeled statistically using item response theory methods. In addition to the item bank, CATS rely on software that includes algorithms for determining subsequent item selection, starting and stopping the CAT, along with scoring procedures. CATs support outcome measures that balance the need for breadth of coverage, precision of measurement, and ease of administration.8
The value of CATs within the field of pediatric rehabilitation has been well supported within the recent literature.8,9,10 Pediatric self-report instruments, both traditional and CATs, are available to measure activity, defined as “the execution of speci?c tasks or actions by an individual” by The World Health Organization’s International Classi?cation of Functioning, Disability and Health (ICF).11 Common examples of activity, performance and participation in pediatric physical therapy practice include the Children’s Assessment of Participation and Enjoyment (CAPE) and Preferences for Activities of Children (PAC),12 and the Activities Scale for Kids – performance version (ASK-p).13 Though the CAPE and ASK-p can be used to capture aspects of activity behaviors, they were not specifically developed to provide measures of health-related PA behaviors or serve as a basis for CATs. Similarly, our focus on PA related self-report measures are not meant to serve as condition specific measures of participation in populations with disabilities as, for example, the Life-H is intended to measure.14 We are unaware of any publically available PA, SED, Strength items banks or CATs which are designed to measure the related health concept of physical activity reflecting a more narrowly defined concept than “activity”.
Improving the reliability and validity of self-report measures for activity behaviors is a high priority within the clinical research community. Several issues regarding self-report (e.g. administration burden, recall error, subjectivity bias and lack of standardization) have been identified in guideline documents for improving the quality of activity self-report in general and children in particular.4,5 Recall error or bias may be reduced in self-report instruments by ensuring the content of the item is easily understood and relevant to the respondent, and by considering the cognitive strategies respondents use for recall.15 Inclusion of PA characteristics in self-report items may be useful for enhancing the precision of recall. Physical activity behaviors of adults are often characterized by their frequency, duration and intensity; organized by the contexts of leisure, occupation, household, or transport; and, described contextually by dimensions of time, place, position or person.16 Inclusion of any, or all, of these should be addressed in the self-report items. For example, adults tend to best recall moderate-to-high intensity activities, or periods of structured exercise, rather than activities that are primarily for socialization or routine tasks of daily living.5,16 In pediatric activity assessment, the specific activity characteristics that improve recall are less defined, and may differ substantially across stages of development and population subgroups. Hence, fewer guidelines exist on how best to enhance recall in pediatric self-report.
In adults, cognitive heuristics are used to aid recall effort by examining fewer cues, reducing the effort of memory retrieval of cue values, simplifying the weighting of cues to form a response, examining fewer alternatives, and/or integrating less information.17 In adults we know that recall strategies, or cognitive heuristics, generally ignore some information to enable faster, more efficient decision making that may also be more accurate than complex recall strategies.15 Such strategies also include the reliance on recognition or familiarity of response concepts rather than specific recollection, the speed of recognition of the response meaning (the one recognized faster is more often chosen), the perceived value of response (pick the one you think is “better”). Interestingly, little is known about how these heuristic tools change across the lifespan, or if the same heuristics are used in children and adults.
Developing an improved understanding of how children conceptualize and recall activity, as well as their cognitive heuristics in responding could enhance accuracy of pediatric self-reports. The need to probe children’s cognitive heuristics for recall of activities, and the underlying logic and approach to cognitively organizing and reasoning about daily PA was a priority for semi-structured child interviews we conducted.
This work was conducted as part of the National Institute of Health’s Patient Reported Outcome Measurement Information System (PROMIS®) initiative.18,19 The application of PROMIS standard methods for definition of relevant concepts and identification of item pools as described in this manuscript, is the first step in the development of item banks and related person reported outcomes. The purpose of this study was to explore how children between 8 and 18 years of age conceptualize and recall their PA, SB and strength to support the development of item pools that measure these concepts. Our long-term goal is to develop CATs from item banks based on our conceptual domains of PA, SB and strength.
Methods
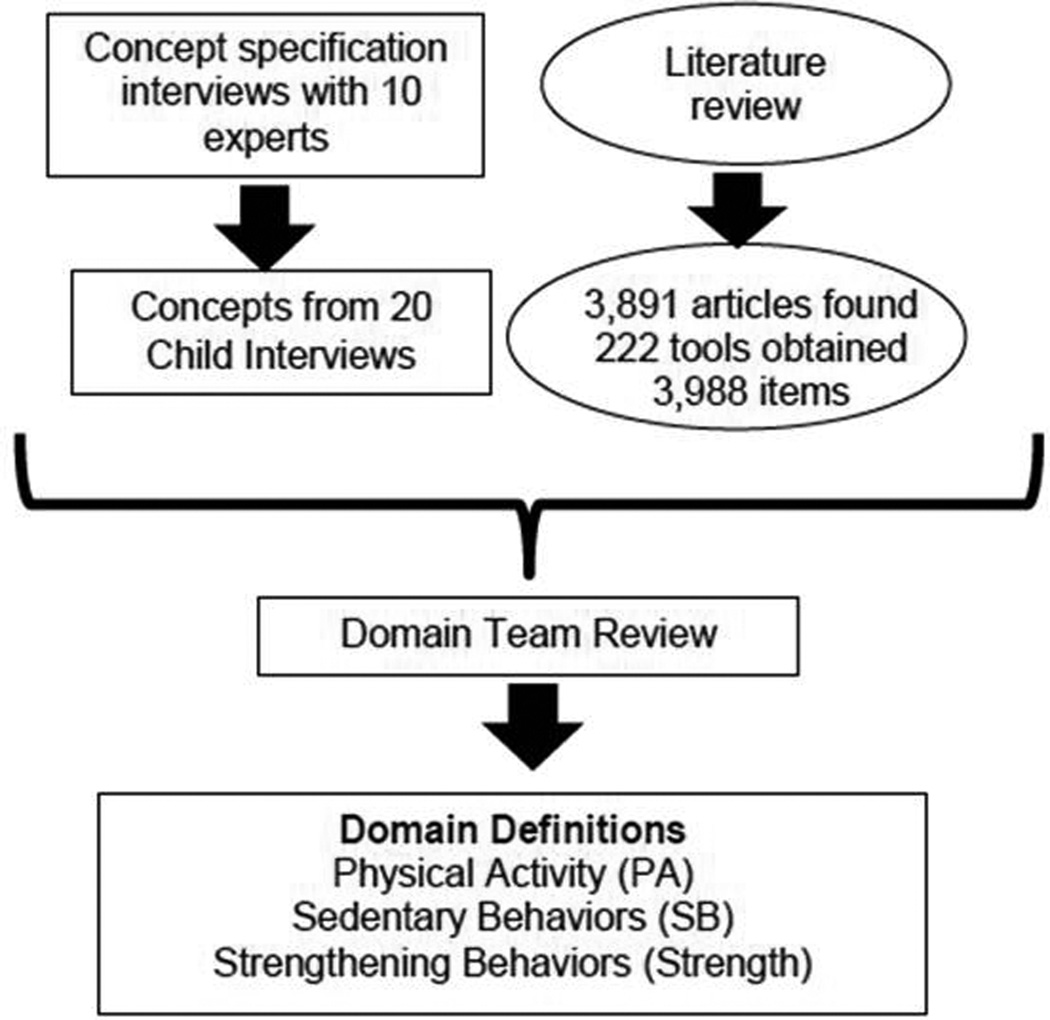
The following activities were performed: expert and child semi-structured interviews for conceptualization, literature review to identify existing self-report activity concepts, and item concept generation (Figure 1). These activities adhered to the existing PROMIS standards for domain conceptualization and item pool development that rely on well-defined qualitative research methods. Full details of the PROMIS Standards that include the methodological guidelines can be found at www.nihpromis.org. Parental informed consent and child assent were obtained in accordance with protocols approved by the institutional review boards of Temple University and The Children’s Hospital of Philadelphia.
Figure 1.
Overview of the Development of the Conceptual Framework of PROMIS Pediatric Physical Activity, Sedentary Behavior and Strength Impact Domains Item.
Initial Domain Conceptualization of Activity Behaviors
The theoretical constructs underlying activity behaviors were based on a review of the literature, expert interviews, and child interviews. The domains that emerged from the theoretical literature review, consistent with adult domains were 1) PA, 2) sedentary behaviors, and 3) strengthening activities.
Physical activity has been defined as “any bodily movement produced by skeletal muscle resulting in energy expenditure – above resting levels”.20 This definition underlies direct measures that assess the amount of body motion. Other concepts of activity place greater emphasis on the integration of complex movement patterns that culminate in the performance of specific behaviors in the context of people’s daily lives. For example, Pettee-Gabriel and colleagues define (physical) activity as “the behavior that involves human movement, resulting in physiological attributes including increased energy expenditure and physical fitness”.16 Pettee-Gabriel’sactivity behavior model served as a starting point for our discussions with experts and children.
In addition to movement-related aspects of activity, an individual’s muscle strength, the capability of the muscle tissue to generate force, is also a core element of activity and supports physical independence.21 Current guidelines recommend that children perform activities that maintain or increase muscular strength and endurance for a minimum of 3 days each week. Muscle-strengthening activities include weight-training programs, weight-bearing calisthenics, climbing (in play or stair climbing), gymnastics, and resistance exercises that use the major muscle groups. The frequency, duration and intensity of strength activities, both as structured exercise and those performed during daily activities provide a basis for self-report measurement. Despite the physiological and functional importance of strength, relatively little has been accomplished in the development of self-report measures of strengthening activities, particularly for children.
Another emerging area of interest is the effect and measurement of sedentary behaviors, such as sitting, reclining, sleeping and watching TV.3,22 Sedentary behaviors appear to be distinct from the low end of the PA domain and have different determinants. Sedentary behavior refers to behaviors that expend 1.5 or less Metabolic Equivalents of Task (METs).22 Typically SBs include activities of rest, or those performed while lying down, sitting or quietly standing. Measures of SB should be used in complement with measures of activity, yet conceptualization of and self-report measures of SBs are just emerging within the literature. Recent systematic reviews of methods used to assess SB in adults, 23 in children24 the use of self or proxy report fixed length measures as well as objective monitors. Literature supports the use of self-report together with objective monitors to optimally assess the amount, type and context of SB. The use of item banks and CATs has not been reported for assessment of SB.
Within each of these 3 domains (PA, SB, and strengthening activities), we defined facets, distinct sub-components that provide a hierarchical or ordered representation of the conceptual domain. Facets in the PS and SB domains were defined based on levels of movement and related energy expenditure for various behaviors (duration of reclining, sitting, standing, walking, running behaviors etc).25 We used the 2011 compendium of PA25 to identify activity behaviors across ranges of metabolic costs. For the strength domain, the frequency of strengthening behaviors and the relative difference in strength requirements needed for functioning (e.g., lift a glass of liquid, heavy books) were represented in the facets.
Expert Interviews to Refine Domain Conceptualization
Ten experts in pediatric PA (7 from the United States and 3 from outside the US) participated in semi-structured interviews to evaluate and refine the domain and facet conceptualizations. Experts were identified by scientific contributions through publications and professional recognition in the field of pediatric physical functioning and activity. Their specific areas of expertise included measurement, adolescent and childhood physical functioning, and health outcomes related to physical function. Experts were asked to respond to the domain-facet frameworks and provide suggestions for improving children’s recall of their activity behaviors. Interviews were audio recorded, transcribed, and subjected to thematic analysis.26 Thematic analyses refer to the process of identifying common themes and patterns of living and/or behaviors from interviews based on the presence of common words, phrases or examples. In our work, we developed themes for each possible PA related behavior the experts noted as important health outcomes. We noted theme frequencies and theme co-occurrence between experts, and the framework was iteratively revised such that new versions were produced after each interview. We continued interviews until no additional common themes were identified and our framework required no revisions. The final framework was shared with all participating experts at the end of the interview process.
Child Semi-Structured Interviews to Identify Child Conceptualization of Activity
Child interviews were conducted to ensure that the domain-facet framework comprehensively and meaningfully covered children’s activity behaviors. Semi-structured interviews were conducted with 20 children aged 8–17 years with 50% female, 15% White, 65% African American, 10% Asian, 10% unknown race, and 30% with a chronic health condition. An important goal of these interviews was to elicit children’s cognitive heuristics’ for recalling activity behaviors. We probed for contextual cues that children used to recall the timing and duration of their activities and for cues or phrases that improved the saliency of the questions, and consistency of responses. Our interview process was terminated when we no new concepts were identified regarding physical activity, sedentary and strength concepts.
During the interview, each child was presented with a sheet of paper with blank timelines. They were asked to indicate times and their daily activities from “waking to bedtime” for the prior weekday and a typical weekend day (Figure 2). Children were prompted to add details for missing periods of time, and asked how they recalled the specific activities. In particular, they were encouraged to identify events that marked temporal transitions (e.g. change of class, bus arrival times, alarm clock set, timing of favorite TV shows etc.), environmental contexts (e.g. at school, home, outside), and social interactions (with friends, classmates, family members) to elucidate cues that may enhance the accuracy of their self-reports.
Figure 2.
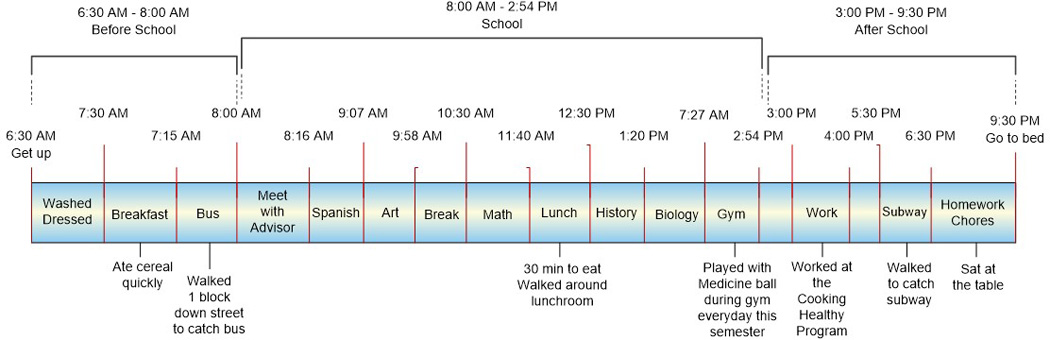
Example of Semi-structured Interview Child-Derived Activity Timeline
To better understand how children experience activity, we also inquired about body signs and sensations that children associate with exertion (e.g., sweating, breathing hard, general and muscle fatigue), strengthening (e.g. muscles burning or muscle fatigue) and inactivity (e.g., tired, low energy). Throughout the discussion, interviewers recorded on index cards the specific activities that children mentioned. In the final phase of the interview, children were asked to sort the cards “however they wanted” into groups meaningful to them. The card sort was used to elucidate conceptual categories of activity behaviors.
Identification of Relevant Item Concepts from Existing Self-Report Measures
A comprehensive, systematic literature review was conducted using the search methodology of Klem and colleagues, who previously applied their procedure to the development of PROMIS item banks.27 Working collaboratively with a team of biomedical librarians at the University of Pennsylvania, we implemented a protocol to identify existing questionnaires, monitoring forms, and interview based surveys measuring one’s engagement in physical, strength, flexibility, and leisure activities.
The literature search was conducted using MEDLINE, CINHAL, PsychINFO, and HaPI (health and psychosocial instruments) that were selected because they catalogue an extensive literature on health outcome measurement instruments. Investigators worked closely with the librarians to develop search terms specific to each search engine database through an iterative process to assure terms would capture a wide range of physical activity measurement tools. Vocabulary lists were constructed to capture 3 distinct aspects of the desired literature: constructs of PA (e.g., exercise, physical activity, leisure activity, physical strength), self-report (e.g., self report, self evaluation), and measurement (e.g. survey, outcome measurement, questionnaires). The search vocabulary was refined using the thesaurus for each database and by combining terms according to standard search conventions such as restrictions regarding sample (e.g., youth <18 years of age) and type of article (e.g., English only). The final list of search terms are included in Appendix A (online Supplemental file 1).
Two study investigators (CAT and RT) reviewed all article titles and abstracts to identify those focused on the development or application of child-report activity instruments. Articles that included instruments that measured mediators or moderators of activity (but not activity as a primary outcome) were considered out-of-scope (e.g., measures of self-efficacy or well-being associated with PA). The identified, in-scope measurement tools were obtained from the instrument authors or from published works in the public domain are listed in Appendix B available online (Supplemental file 2). Each instrument was catalogued into an item library database containing the context, item stems and response categories with linkages to source instruments. For all instruments, we extracted item concepts and assigned them to a domain (PA, SB, or strength). The domain assignment of each item was based on comparison of the meaningful words and phrases in each item (lexical) with additional consideration of the stated intent of the instrument.
Item classification, selection, and generation
Item concepts (i.e., the primary focus of the item) were classified independently by 2 subject matter experts (CAT and RT) into the domains and component facets identified through the expert and child interviews. When reviewers disagreed about an item concept’s facet categorization, consensus was achieved with input from a third reviewer (CBF).If an item concept did not fit into an existing facet category, it was marked as “other.” Subsequently, conceptually similar items categorized as “other” were then reviewed and re-grouped to create novel facets. When item concept classification was complete, we evaluated each facet to determine the extent to which its constituent item-level concepts evaluated the full range (floor to ceiling) of the domain (PA, SB, or strength) with minimal gaps or item redundancies.
Results
Development of Domain-Facet Concept Maps
The content experts suggested that separate item banks were needed for the domains of PA, SB, and strengthening activities. Item concepts that captured the hierarchical aspects of activity behaviors (e.g., levels of energy expenditure) were considered a priority for inclusion. Additional item concepts that included the activity’s behavioral context, purpose, physical environment and social groupings were also considered. The experts supported the objective to advance self-report of PA. Our initial conceptualization of activity was generally consistent with the experts, but the inclusion of SB and strengthening activities was more highly prioritized after the expert interviews. Domain definitions were iteratively revised based on input from the experts during the interview process.
Child Semi-Structured Interviews
Children defined PA in terms of participation in sports and structured exercises (e.g., playing soccer, doing jumping jacks or push-ups). Selected comments from the semi-structured interviews for concept elicitation are provided in Table 1. Many younger children felt that PA and exercise were “the same thing.” However, a conceptual differentiation between activity behaviors that youth “do for fun” (play) and “to stay fit” (exercise) emerged among adolescents. Interviews confirmed the frequent occurrence of SB in children’s daily lives, especially engagement in computer-based social networks among adolescents. Unlike adults, children did not consider physical exertion during the fulfillment of daily tasks (e.g., transportation, completion of household chores) in their definitions of PA.
Table 1.
Selected Exemplar Comments fromChild Interviews by Age
| Question | Example Responses |
|---|---|
| What does being physically active mean to you? [Word Association] |
Responses from 14 – 17 year olds: Sports, running, all kinds of different sports like track, soccer, football, lacrosse Physical activity is something that you do that's physical, something that helps you move around, get your body strong. I'd say 'you play basketball, that's one form of physical activity. Physical activity is exercising and eating healthy. I can feel that my arms and legs are getting stronger, 'cause that's what you use the most. And after I know that my muscles are really tightened up. |
| Responses from 8 – 11 year olds: You get to do kinds of activities, games; sometimes I do physical activities in school. [probe: when do you use that word?] like for writing and for talking to my teacher. [probe: do other people talk to you about Physical Activity?] Yes, my gym teacher Exercise; Being out of the house more, playing basketball, football, lets go play some sports, ride some bikes | |
| What are some ways that you are active or could try to be more active? | Responses from 14 – 17 year olds: Go out, go on vacations, play games, have fun with family, have cook-outs, do good things, get attention, do things with friends, go to school, listen to parents, likes what he/she likes doing, enjoys her activities, make their friends laugh |
| Responses from 8 – 11 year olds: Chase each other, play tag, go outside, play tag Go outside more, run around more. Chasing my dog or my brother. [probe: what about something that's physically active at home but outside?] running around. [probe: what about parks and fields?] I do monkey bars. [probe: is there another place that's not home or school that you spend a lot of time in?] Yes, my cousin's house. | |
| Describe a time when you were extremely physically active and moving around. What were you doing? Why did you stop? | Responses from a 17 year old: When we hiked up the mountain, we went to Hawk mountain. I didn't make it all the way up, but I made it far. [probe: did you like it?] Yeah, it was ok; I just wish I didn't get as tired as fast as I did. [probe: do you know why you think you got so tired?] Because I'm overweight. [probe: can you think of anything that would make it easier?] I think if I was smaller. [probe: did it seem like that activity flew by or was it dragging on forever?] It was flying by and once I got tired it was going slow. [probe: how did your body feel?] My heart was beating real fast and my legs weren't really tired but it was an incline so I could feel the burning, I was breathing heavy. [probe: is that why you stopped?] Yes. [probe: how did you feel after you did that hike?] Exhausted, my feet were hurting, I guess I wasn't wearing the right sneakers, I just felt tired. [probe: how long did it take for you to feel back to normal?] The next day. |
| Responses from an 8 year old: I was at my cousin's house and we're playing kickball in their basement. [probe: how long were you playing for?] An hour. [probe: was it hard to keep track of time? Did it seem like time was passing quickly?] No. [probe: were there other people there with you besides your cousins?] My aunt, my uncle and my mom. [probe: when's the last time you played kickball like this?] Not that long ago, we were there in September or something. [probe: what do you notice about your body?] My feet move, sometimes I had to catch the ball. [probe: did your body feel different than normal?] Yes, it felt tingly then funny a little. [probe: when do you get the tingly feeling?] When I run. [probe: how long did it take for your body to get back to normal?] A couple days. [probe: what happened to your energy after you were really physically active?] It got a little stronger | |
| Describe being physically inactive | Responses from a 14 – 17 year olds: [probe: how describe inactive feeling to someone?] felt like going to sleep, feel tired [probe: how often do you do that?] maybe every two months; [probe: other words to describe how this feels?] no, not really. [p: what are some things you like to do that are inactive?] watching tv, getting on facebook, go on youtube, watch videos and stuff [probe: how much time did you spend being inactive yesterday?] maybe about 4 hours watching tv and an hour on the computer, andi did read my book watch TV, coloring w/ my nephew, [probe: how does your body feel when you're sitting around watching TV?] its like nothing. knitting, I started that 2 years ago. My mom knits and I was always interested so I asked her to teach me. [p: how long do you knit for?] A long time, if I have the time. This past summer. [p: do you think you have more or less energy after you're knitting?] I get tired so I think I get less energy [p: how do you feel when you're sitting around?] I was feeling tired, lazy and fat |
| Response from 8- 12 year old on a Saturday, when it was raining, we just sat in the house and watched TV. I played some of my video games, some board games. [probe: how did you feel?] I'm used to going outside a lot but now the school year started and its cut. So now I usually just come home from school, go home, do my homework, sit down and relax. [probe: if I was to ask another kid, what would be a better word than you felt like a big blob?] Lazy. [probe: what does that do to your energy?] It went down. [p: how would you fix it?] Moving around, getting up, stretching. [probe: How does somebody look when they have a lot of energy?] Not tired, not looking lazy. [probe: what part of the body do you look at when you're deciding if they have a lot of energy?] Mostly their legs. [probe: how do tired legs look?] Just dragging. |
|
| Describe a time you worked out getting your muscles stronger | Responses from 14 – 17 year olds: I can feel that my arms and legs are getting stronger, 'cos that's what you use the most. And after I know that my muscles are really tightened up Lifting weights, push-ups, sit-ups, jumping jacks, bench pressing, and I ran around my house a couple times too. [probe: what were the things that let you know you were exercising hard?] Sweat, my muscles were getting bigger, and I was feeling a little bit tired. |
| Responses from 8 – 11 year olds: When my uncle took me to the gym for the first time about a year ago. We were there from 6:00 to 8:00. We jumped rope, push-ups, sit-ups, treadmill. [probe” how'd you feel, how'd you know you were working really hard?] well I can't really do push-ups, that was really difficult for me. Something hurt, my arms and legs. You're sweating, your body is sore. [probe: why did you stop? did you have enough?] I had enough. [probe: how'd you feel the next day?] Sore. [probe: would you do it again?] Not really, because it hurt |
To explore how children recalled and mentally organized their activities, we employed 2 techniques: an open-ended response timeline activity and a card sort. The child-derived timelines of activity showed that specific times were easily recalled for events when linked with external schedules (e.g., “bus comes at 8:17 AM”, “was 43 minutes because that’s how long class is”, “curfew is 11 and it’s a 7 minute walk home”) (Figure 2). Though start and end times could often be very specifically recalled, children less clearly defined differences in activity levels during those specific blocks of times.
We found that when children think and talk about their physiologic reactions to activity they used colloquial phrases like “muscles burning” or “body gave out” in addition to the more typically expected expressions of “heart racing” or “breathing hard.” The use of “sweating” was more varied with many children reporting they either “do not sweat” or that they viewed “sweating” negatively. Sensations associated with strengthening activities were either muscle or body part specific (e.g. muscles got tight, arms gave out) or more general (e.g. felt pumped up). Children associated SB with more general expressions of “feeling lazy,” “felt like a blob,” or “low energy” with few specific body-focused sensations emerging.
The card sort exercise also revealed that many children did not typically group activities based on the physical nature (e.g., aerobic, sedentary, and strengthening) of the task. Two common sort criteria emerged: 1) discretionary versus non-discretionary activities - in one child’s words, “there are things I have to do (shower, homework, make pizzas) and things I don’t have to do (read, jump rope, sit and talk);” and 2) who they were active with (peers, family, alone) - some children had cards solely grouped for activities they did alone, with family, or with friends.
Domain Frameworks & Definitions
The domain definitions derived from our expert interviews were then modified to reflect the children’s views of PA, SB and strength were refined (Table 2 and used a basis to guide development of items (context, item stems and responses), described in our companion manuscript. These definitions provide item concepts as well as the organization of the underlying hierarchical construct for each domain and the related concepts children used to recall and structure their thinking of prior day activities.
Table 2.
Domain concepts and descriptions developed from expert, child and parent input integrated with systematic literature review.
| Domain | Description |
|---|---|
| Physical Activity | Physical Activity refers to one's level of bodily movement and performance of activities that require physical actions, ranging from simple static behaviors with minimal muscle activity to more complex activities that require dynamic or sustained muscle activity and greater movement of the body. The Physical Activity item pool should consist of a range of items that estimate the amount of complex physical movements and behaviors and the contexts in which they occur. The underlying hierarchical factor is relative energy expenditure. Thenon-hierarchical context characteristics reflect the purpose of the activity (e.g. self-care, sports, school, and recreation), physical environment (e.g. school home, community) and social situations (e.g. alone, family, peers). |
| Sedentary Behaviors | Sedentary Behaviors are behaviors that require minimal effort and reflect a high level of inactivity that can be characterized by duration, temporal (time of day) and contextual coverage of purpose (screen time, transportation, socializing, work/school (non-discretionary), environment and social situations. |
| Strength Behaviors | Strength Behaviorsreflect the capacity of individuals to perform functional activities of daily living that require significant amount of muscle force generation. Items may includea phrase (e.g. “were you strong enough to…”) providing attribution of the functional capacity to one’s strength. |
Discussion
The semi-structured interviews with experts and children in this study generated conceptualizations and domain definitions that integrated the children’s perspectives of the concepts of PA, SB, and strength. Our methods reflect current best practices in item bank development previously reported in the pediatric literature by Coster28 and Haley29 among others. More specifically, our final domain framework and definitions are based on existing literature, supported by the expert interviews, and are developmentally appropriate for children, both in terms of definition as well as a breadth of concepts to engage different aspects of possible child cognitive heuristics. This framework serves as the basis for the development of items that reflect the children’s recall of their previous activities as well as insights into the wording of concepts from the children’s perspective. For example, children, recall prior activity with more apparent ease when asked to think of specific periods of the day (e.g. evening, after school) or their social setting (e.g. with family or friends). When asked how many times in the past week they exercised for 30 minutes, the children took longer to respond, apparently needing time for that mental calculation. Children also easily recalled times when they experienced symptoms of activity and were able to describe the corresponding activity.
A limitation of this work is that our semi-structured child interviews were drawn primarily from an urban region of the mid-Atlantic US that may limit generalizability. This limitation will be offset in the subsequent phases of instrument development process with the cultural harmonization review, which his described in our companion manuscript, as well as with the data collection associated with calibration and norming which includes larger numbers of national and international respondents.
Conclusion
This phase of item bank development has resulted in a child-informed conceptual framework of pediatric PA, SB and strength. Our work provides strong support for the development and content validity of item banks and related instruments of physical activity, sedentary behavior and strength impact that will provide valid and standardized endpoints for application and comparison across clinical studies assessing the relative effectiveness of interventions directed towards changing PA and SB patterns.
Acknowledgments
Grant Support: This work was funded by NIH/NIAMS as U01 AR057956 (PI – Forrest, CB): Pediatric PROMIS: Advancing the Measurement and Conceptualization of Child Health. PROMIS® was funded with cooperative agreements from the National Institutes of Health (NIH) Common Fund Initiative (Northwestern University, PI: David Cella, PhD, U54AR057951, U01AR052177; Northwestern University, PI: Richard C. Gershon, PhD, U54AR057943; American Institutes for Research, PI: Susan (San) D. Keller, PhD, U54AR057926; State University of New York, Stony Brook, PIs: Joan E. Broderick, PhD and Arthur A. Stone, PhD, U01AR057948, U01AR052170; University of Washington, Seattle, PIs: Heidi M. Crane, MD, MPH, Paul K. Crane, MD, MPH, and Donald L. Patrick, PhD, U01AR057954; University of Washington, Seattle, PI: Dagmar Amtmann, PhD, U01AR052171; University of North Carolina, Chapel Hill, PI: Harry A. Guess, MD, PhD (deceased), Darren A. DeWalt, MD, MPH, U01AR052181; Children’s Hospital of Philadelphia, PI: Christopher B. Forrest, MD, PhD, U01AR057956; Stanford University, PI: James F. Fries, MD, U01AR052158; Boston University, PIs: Alan Jette, PT, PhD, Stephen M. Haley, PhD (deceased), and David Scott Tulsky, PhD (University of Michigan, Ann Arbor), U01AR057929; University of California, Los Angeles, PIs: Dinesh Khanna, MD (University of Michigan, Ann Arbor) and Brennan Spiegel, MD, MSHS, U01AR057936; University of Pittsburgh, PI: Paul A. Pilkonis, PhD, U01AR052155; Georgetown University, PIs: Carol. M. Moinpour, PhD (Fred Hutchinson Cancer Research Center, Seattle) and Arnold L. Potosky, PhD, U01AR057971; Children’s Hospital Medical Center, Cincinnati, PI: Esi M. Morgan DeWitt, MD, MSCE, U01AR057940; University of Maryland, Baltimore, PI: Lisa M. Shulman, MD, U01AR057967; and Duke University, PI: Kevin P. Weinfurt, PhD, U01AR052186). NIH Science Officers on this project have included Deborah Ader, PhD, Vanessa Ameen, MD (deceased), Susan Czajkowski, PhD, Basil Eldadah, MD, PhD, Lawrence Fine, MD, DrPH, Lawrence Fox, MD, PhD, Lynne Haverkos, MD, MPH, Thomas Hilton, PhD, Laura Lee Johnson, PhD, Michael Kozak, PhD, Peter Lyster, PhD, Donald Mattison, MD, Claudia Moy, PhD, Louis Quatrano, PhD, Bryce Reeve, PhD, William Riley, PhD, Peter Scheidt, MD, Ashley Wilder Smith, PhD, MPH, Susana Serrate-Sztein, MD, William Phillip Tonkins, DrPH, Ellen Werner, PhD, Tisha Wiley, PhD, and James Witter, MD, PhD. The contents of this article uses data developed under PROMIS. These contents do not necessarily represent an endorsement by the US Federal Government or PROMIS. See www.nihpromis.org for additional information on the PROMIS® initiative.
Footnotes
Conflicts of Interest The author’s declare no conflicts of interest.
References
- 1.Weiss MR, editor. Developmental Sport & Exercise Psychology: A Lifespan Perspective. Morgantown, WV: Fitness Information Technology; 2004. [Google Scholar]
- 2.Welk GJ, editor. Physical Activity Assessments for Health-Related Research. Champaign, IL: Human Kinetics Publishers, Inc; 2002. [Google Scholar]
- 3.Smith AL, Biddle SJH. Youth Physical Activity and Sedentary Behavior: Challenges and Solutions. Human Kinetics; Champaign, IL: 2008. [Google Scholar]
- 4.Haskell WL. Physical activity by self-report: A brief history and future issues. Journal of Physical Activity and Health. 2012;9(Suppl 1):S5–S10. doi: 10.1123/jpah.9.s1.s5. [DOI] [PubMed] [Google Scholar]
- 5.Bowles HR. Measurement of active and sedentary behaviors: Closing the gaps in self-report methods. JPAH. 2012;9(suppl1):S1–S4. doi: 10.1123/jpah.9.s1.s1. [DOI] [PubMed] [Google Scholar]
- 6.Cain KL, Sallis JF, Conway TL, Van Dyck D, Calhoon L. Using accelerometers in youth physical activity studies: a review of methods. J Phys Act Health. 2013 Mar;10(3):437–450. doi: 10.1123/jpah.10.3.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Biddle SJH, Gorely T, Pearson N, Bull FC. An assessment of self-reported physical activity instruments in young people for population surveillance: Project ALPHA. IJBNPA. 2011;8:1. doi: 10.1186/1479-5868-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tucker CA, Haley SM, Dumas HM, et al. Physical function for children and youth with cerebral palsy: Item bank development for computer adaptive testing. Journal of Pediatric Rehabilitation Medicine: An Interdisciplinary Approach. 1(2008):245–253. [PubMed] [Google Scholar]
- 9.Haley SM, Fragala-Pinkham MA, Dumas HM, Ni P, Gorton GE, Watson K, Montpetit K, Bilodeau N, Hambleton RK, Tucker CA. Evaluation of an item bank for a computerized adaptive test of activity in children with cerebral palsy. Phys Ther. 2009 Jun;89(6):589–600. doi: 10.2522/ptj.20090007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dumas HM, Fragala-Pinkham MA, Haley SM, Ni P, Coster W, Kramer JM, Kao YC, Moed R, Ludlow LH. Computer adaptive test performance in children with and without disabilities: prospective field study of the PEDI-CAT. Disabil Rehabil. 2012;34(5):393–401. doi: 10.3109/09638288.2011.607217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.International Classi?cation of Functioning, Disability and Health (ICF) Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 12.King GA, Law M, King S, Hurley P, Hanna S, Kertoy M, Rosenbaum P. Measuring children’s participation in recreation and leisure activities: construct validation of the CAPE and PAC. Child care, Health and Development. 2006;33(1):28–39. doi: 10.1111/j.1365-2214.2006.00613.x. [DOI] [PubMed] [Google Scholar]
- 13.Young NL, Williams JI, Yoshida KK, Wright JG. Measurement properties of the Activites Scale for Kids. J Clin Epidemiol. 2000;53:125–137. doi: 10.1016/s0895-4356(99)00113-4. [DOI] [PubMed] [Google Scholar]
- 14.Noreau L, LePage C, Boissiere L, Picard R, Fougeyrollas P, Mathieu J. Desmarais, Measuring participation in children with disabilities using the Assessment of Life Habits. Developmental Medicine & Child Neurology. 2007;49(9):666–671. doi: 10.1111/j.1469-8749.2007.00666.x. [DOI] [PubMed] [Google Scholar]
- 15.Gigerenzer G, Gaissmaier W. Heuristic Decision Making. Annu Rev Psych. 2011;62:451–482. doi: 10.1146/annurev-psych-120709-145346. [DOI] [PubMed] [Google Scholar]
- 16.Pettee-Gabriel KK, Morrow JR, Woolsey AT. Framework for physical activity as a complex and multidimensional behavior. JPAH. 2012;9(suppl1):S11–S18. doi: 10.1123/jpah.9.s1.s11. [DOI] [PubMed] [Google Scholar]
- 17.Kahneman D, Shane Frederick S. Representativeness Revisited: Attribute Substitution in Intuitive Judgment. In: Gilovich Thomas, Griffin Dale, Kahneman Daniel., editors. Heuristics and Biases: The Psychology of Intuitive Judgment. Cambridge: Cambridge University Press; 2002. pp. 49–81. [Google Scholar]
- 18.Forrest CB, Bevans KB, Tucker C, et al. The Patient reported outcome measurement information system (PROMIS) for children and youth: Application to pediatric psychology. J Pediatr Psychol. 2012 Jul;37(6):614–621. doi: 10.1093/jpepsy/jss038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Medical Care. 2007;45:S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Casperson CJ, Powell KE, Christenson GM. Physical activity, exercise and physical fitness: Definitions and distinctions for health-related research. Public Health Reports. 1985;100:126–131. [PMC free article] [PubMed] [Google Scholar]
- 21.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. American College of Sports Medicine, American Heart Association. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007 Aug 28;116(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 22.Pate RR, O’Neill JR, Lobelo F. The evolving definition of"sedentary”. Exerc Sport Sci Rev. 2008;36(4):173–178. doi: 10.1097/JES.0b013e3181877d1a. [DOI] [PubMed] [Google Scholar]
- 23.Proper KI, Singh AS, van Mechelen W, Chinapaw MJ. Sedentary behaviors and health outcomes among adults: a systematic review of prospective studies. Am J Prev Med. 2011;40(2):174–182. doi: 10.1016/j.amepre.2010.10.015. [DOI] [PubMed] [Google Scholar]
- 24.Lubans DR, Hesketh K, Cliff DP, et al. A systematic review of the validity and reliability of sedentary behaviour measures used with children and adolescents. Obesity Reviews. 2011;12:781–799. doi: 10.1111/j.1467-789X.2011.00896.x. [DOI] [PubMed] [Google Scholar]
- 25.Ainsworth B, Haskell W, Hermann S, Meckes N, Bassett D, Tudor-Locke C, et al. 2011 Compendium of physical activities: A second update of codes and MET values. Medicine and Science in Sports and Exercise. 2011 doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 26.Boyatzis R. Transforming Qualitative Information: Thematic Analysis and Code Development. Sage Publications; Thousand Oaks, CA: 1998. [Google Scholar]
- 27.Klem ML, Saghafi E, Abromiti R, Stover A, Dew MA, Pilkonis PA. Building PROMIS item banks: Librarians as co-investigators. Quality of Life Research. 2009;18(7):881–888. doi: 10.1007/s11136-009-9498-7. (PMCID: PMC2744389) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bedell GM, Khetani MA, Cousins MA, Coster WJ, Law MC. Parent perspectives to inform development of measures of children's participation and environment. Arch Phys Med Rehabil. 2011 May;92(5):765–773. doi: 10.1016/j.apmr.2010.12.029. PubMed PMID: 21530724. [DOI] [PubMed] [Google Scholar]
- 29.Mulcahey MJ, DiGiovanni N, Calhoun C, Homko E, Riley A, Haley SM. Children'sand parents' perspectives about activity performance and participation afterspinal cord injury: initial development of a patient-reported outcome measure. Am J Occup Ther. 2010 Jul-Aug;64(4):605–613. doi: 10.5014/ajot.2010.08148. PubMed PMID: 20825132. [DOI] [PubMed] [Google Scholar]