Abstract
AIM: To study the morbidity and complications associated to ileostomy reversal in colorectal surgery patients, and if these are related to the time of closure.
METHODS: A retrospective analysis of 93 patients, who had undergone elective ileostomy closure between 2009 and 2013 was performed. Demographic, clinical and surgical variables were reviewed for analysis. All complications were recorded, and classified according to the Clavien-Dindo Classification. Statistical univariate and multivariate analysis was performed, setting a P value of 0.05 for significance.
RESULTS: The patients had a mean age of 60.3 years, 58% male. The main procedure for ileostomy creation was rectal cancer (56%), and 37% had received preoperative chemo-radiotherapy. The average delay from creation to closure of the ileostomy was 10.3 mo. Postoperative complications occurred in 40% of the patients, with 1% mortality. The most frequent were ileus (13%) and wound infection (13%). Pseudomembranous colitis appeared in 4%. Increased postoperative complications were associated with delay in ileostomy closure (P = 0.041). Male patients had more complications (P = 0.042), mainly wound infections (P = 0.007). Pseudomembranous colitis was also associated with the delay in ileostomy closure (P = 0.003). End-to-end intestinal anastomosis without resection was significantly associated with postoperative ileus (P = 0.037).
CONCLUSION: Although closure of a protective ileostomy is a fairly common surgical procedure, it has a high rate of complications, and this must be taken into account when the indication is made. The delay in stoma closure can increase the rate of complications in general, and specifically wound infections and colitis.
Keywords: Protective ileostomy, Stomas, Stoma-related complications, Surgical infections, Colorectal surgery
Core tip: Protective ileostomies are widely used by surgeons for the protection of anastomoses, but they imply a second intervention for reversal. Despite being considered a minor intervention, ileostomy reversal does not lack complications. Adjuvant treatment, complications from the first intervention, or low-priority consideration can delay the closure of the stoma. In our study, we reviewed all complications following ileostomy reversal and found they were considerably high (40%), and increased as did the time (in months) until closure (P = 0.041). In multivariate analysis, male patients had more complications (P = 0.042), mainly wound infections (P = 0.007). Pseudomembranous colitis was also associated with the delay in ileostomy closure (P = 0.003).
INTRODUCTION
Diverting loop ileostomies are widely used by colorectal surgeons for the protection of low rectal anastomoses, as they can reduce the morbidity and rate of reintervention if an anastomotic leak occurs[1]. The use of a protective ileostomy is specially indicated in very low rectal resections, coloanal anastomosis and pouches[2,3].
However, there can be an important morbidity associated to the stoma itself, deriving in a bad quality of life for the patient. Some common problems associated to the ileostomy can be electrolytic alterations, dehydration, renal failure, infection, obstruction, prolapse, and hernias[4]. Postoperative complications of variable severity (and even mortality) have been reported in different series reviewing protective ileostomy closure, ranging from 3% to over 40%[5,6]. Surgical infection of the wound is always a relevant one. A recent systematic review on ileostomy reversal reported an overall mortality of 0.4%[7], with values ranging from 0% to 4% in different studies. The aim of our study was to review our institutional series of ileostomy reversals and identify possible risk factors for postoperative complications.
MATERIALS AND METHODS
A retrospective analysis of patients who underwent elective ileostomy reversal in our institution between 2009 and 2013 (first semester) was performed. La Paz University Hospital (Madrid, Spain) is a tertiary care university hospital, with a high-volume Colorectal Surgery Unit. Ninety-three patients were included in the study. All data from the patients were retrieved from medical records and included in a database. Analyzed variables were: demographics, comorbidities, the American Society of Anesthesiologists classification for operative risk (ASA) index, body mass index (BMI), initial surgery (when the ileostomy was created), adjuvant chemo-radiotherapy before stoma closure, time interval from stoma creation to reversal, surgical technique employed, hospital stay, surgical complications, readmissions and mortality. All patients were assessed preoperatively by a member of the Colorectal Surgery Unit, who indicated the closure of the stoma, and by an Anesthesiologist for preoperative assessment. Regarding reversal, an oval incision was performed around the stoma to release the ileal loop. The anastomotic technique employed was either a handsewn end-to-end anastomosis without resection, a handsewn end-to-end with resection, a handsewn side-to-side with resection or a stapled anastomosis. Closure of the abdominal wall was performed with absorbable sutures (PDS or Vicryl©), and skin was closed with either staples, subcuticular or interrupted sutures, at surgeon’s will. All these technical data were retrieved from the surgical charts and reports in the patients’ records. Thirty-day morbidity and mortality were reviewed using medical records, outpatient clinic notes and the hospital’s database.
Statistical analysis was performed using SPSS 16 Software for Windows, setting statistical significance at P < 0.05. χ2 or Mann-Whitney tests were used for univariate analysis (when appropriate), and a multivariate analysis of all variables was performed.
RESULTS
The patients had a mean age of 60.3 years (range 22-88 years), 58% male. Demographic and clinical data, including the initial indication for ileostomy, are shown in Table 1. Data related to the interval from stoma creation to reversal, and the surgical technique employed for ileostomy and skin closure are shown in Table 2. A total of 26 patients (28%) presented at least one associated major comorbidity, including liver metastases (19%), diabetes and heart disease (11.5% each), pulmonary disease, thrombotic disease, hematologic disorders, lung metastases (7.7% each), and finally arrhythmias, other malignancies and tuberculosis (1% each). Average time for reversal was 10.3 mo, ranging from 1 to 36 mo. There was an 8.6% readmission rate due to dehydration before ileostomy closure. Postoperative complications globally occurred in 38 (40%) of the patients, and some patients presented more than one complication; these are detailed in Table 3. There was a 1% mortality. The mean hospital stay was 11.5 d, ranging from 3 d to 3 mo.
Table 1.
Characteristics of the 93 patients who underwent loop ileostomy reversal
| Clinical characteristics | n (%) |
| Patients included, total | 93 (100) |
| Gender | |
| Male | 54 (58) |
| Female | 39 (42) |
| BMI | |
| Underweight | 3 (3.1) |
| Normal weight | 44 (47) |
| Overweight | 31 (33.3) |
| Obese | 15 (15.8) |
| ASA Index | |
| I | 5 (5.5) |
| II | 59 (63) |
| III | 29 (31) |
| Indication for ileostomy | |
| Colorectal cancer | 52 (56) |
| Anastomotic leak | 16 (17.2) |
| IBD | 6 (6.4) |
| Colectomy for polyposis | 5 (5.3) |
| Endometriosis | 5 (5.3) |
| Diverticular disease | 3 (3.2) |
| Intestinal necrosis | 1 (1.07) |
| Pelvi-peritonectomy | 1 (1.07) |
| Post-endoscopy perforation | 1 (1.07) |
| Trauma | 1 (1.07) |
| Adjuvant therapy (in oncological patients) | |
| Chemotherapy | 16 (17.2) |
| Chemo-radiotherapy | 35 (37) |
Demographic data, BMI, ASA Index, indications for ileostomy creation and adjuvant therapy. BMI: Body mass index; ASA: The American Society of Anesthesiologists classification for operative risk; IBD: Inflammatory bowel disease.
Table 2.
Characteristics of the ileostomy reversal procedure, including surgical technique and skin closure
| Surgical variable | n (%) |
| Ileostomy closure technique | 93 (100) |
| Stapled anastomosis | 9 (9.7) |
| Handsewn anastomosis | 84 (90.3) |
| Side-to-side with resection | 28 (33.3) |
| End-to-end with resection | 8 (9.5) |
| End-to-end without resection | 48 (57.1) |
| Skin closure technique | 70 (100) |
| Staples | 17 (24) |
| Subcuticular | 29 (41) |
| Interrupted suture | 24 (34) |
Table 3.
Postoperative complications after loop ileostomy reversal in our study
| Complications | n (%) |
| Total patients | 38 (40.8) |
| Ileus | 12 (12.9) |
| Wound infection | 12 (12.9) |
| Rectal bleeding | 5 (5.8) |
| Pseudomembranous colitis | 4 (4.3) |
| Anemia/bleeding | 3 (3.2) |
| Intestinal obstruction | 3 (3.2) |
| Anastomotic leak | 2 (2.15) |
| Urinary tract infection | 2 (2.15) |
| Acute renal failure | 2 (2.15) |
| Abdominal abscess | 2 (2.15) |
| Pneumonia | 1 (1) |
| Intestinal necrosis | 1 (1) |
| Multiple organ failure | 1 (1) |
| Thromboembolism | 1 (1) |
| Sepsis | 1 (1) |
| Evisceration | 1 (1) |
| Clavien-Dindo classification | |
| Grade I | 21 (55) |
| Grade II | 9 (24) |
| Grade III | 7 (18) |
| Grade IV | 0 (0) |
| Grade V | 1 (3) |
Total number of patients and detailed complications classified by the Clavien-Dindo classification.
Multivariate analysis was performed to identify risk factors for complications. Male patients had complications in 50% of cases (27/54) while females did in 28% (11/39). This result reached statistical significance (P = 0.042), so in our study male sex was a risk factor for postoperative complications. When analyzing specific complications, there was a strong association between male sex and wound infection (P = 0.007). Age was associated to rectal bleeding (P = 0.006). There was no statistically significant association between complications and ASA, BMI, or previous chemo-radiotherapy.
In our series, the increased number of postoperative complications was associated with the delay in ileostomy closure (P = 0.041); a graphic representation of these data is shown in Figure 1. Occurrence of pseudomembranous colitis was also associated with the delay in ileostomy closure, with statistical significance (P = 0.003). The four cases of pseudomembranous colitis occurred in patients with ileostomy closure ranging from 9 to 15 mo.
Figure 1.
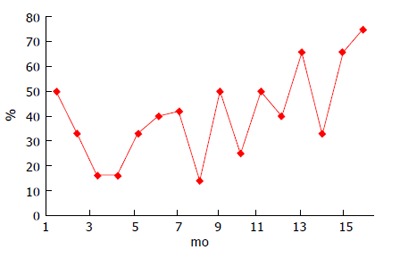
Percentage of postoperative complications related to ileostomy closure and time (in months) from creation to reversal.
According to the surgical technique for ileostomy reversal, only end-to-end intestinal anastomosis without resection was significantly associated with a specific complication, which was postoperative paralytic ileus (P = 0.037). There was no significant association between the surgical technique employed and postoperative hospitalization.
Regarding skin closure, the rate of surgical wound infection was studied in each group, when data on wound closure were available. In the staples group, infection was 5.8% (1/17 patients), in the subcuticular suture group 13% (4/29 patients) and in the interrupted suture group 20% (5/24 patients). Despite the rate of infection was highest in the interrupted suture group and lowest in the staples group these results did not reach statistical significance. All statistically significant results of the multivariate analysis are shown in Table 4.
Table 4.
Statistically significant conditions/complications in the multivariate analysis and their specific P values
| Condition/complication | Statistical significance |
| Gender (male) and overall complications | P = 0.042 |
| Gender (male) and wound infection | P = 0.007 |
| Age and rectal bleeding | P = 0.006 |
| Complications and time to closure (months) | P = 0.041 |
| Closure > 6 mo and pseudomembranous colitis | P = 0.003 |
| End-to-end intestinal anastomosis (without resection) and postoperative ileus | P = 0.037 |
DISCUSSION
Diverting loop ileostomies have become a common procedure when very low or high-risk rectal anastomoses are performed. Despite they can reduce morbidity and avoid reintervention if a leak occurs, their creation binds the patient to a second surgical procedure. This reversal procedure, as many published series have proven, can be associated to a high rate of morbidity, and even mortality[8]. In a recent systematic review[7], the high morbidity associated to ileostomy reversal raised concerns over the real indication of diverting stomas related to clinical outcomes, and if a better selection of patients should be made. Luglio et al[9], consider that if there is a > 5% risk of anastomotic leak in the primary operation, a protective stoma must be created.
In our study, the rate of postoperative morbidity was high (40%), but still among published data. The most common complications in our study were postoperative ileus and wound infections. Complications were mostly minor, classified as Clavien-Dindo I-II, and only 18% were considered major complications needing reoperation or invasive interventions (Clavien-Dindo III). In a national study by Mengual-Ballester et al[6] data were similar to our own, with complications up to 45.9%, being ileus/obstruction the most frequent, followed by diarrhea and wound infection.
Ileus and bowel obstruction are still a concern after stoma reversal, and different studies have tried to elucidate if technical issues can reduce these complications. The surgical technique employed for the ileal anastomosis has been widely studied, and various published randomized controlled trials (RCTs) compare handsewn vs stapled anastomoses[10,11]. In our study, when analyzing the surgical technique and related complications, we only found statistical significance between end-to-end anastomosis without resection and postoperative paralytic ileus. This coincides with published meta-analysis[12-14] which mention a significant reduction in surgical time and a lower incidence of bowel obstruction when stapled anastomoses are performed compared to handsewn. Other complications (including infections, leak, readmission and reoperation rates) are similar.
Surgical infections after stoma reversal have been a subject of debate. Although both ileostomies and colostomies can be safe, the latter present a higher rate of infection after reversal. Therefore many authors recommend protective ileostomies for fecal diversion, if dehydration is not to be expected[15]. The rate of wound infection in our study (12.9%) was similar to other published data[16]. Wound infection is usually underestimated due to different definitions or considerations, and can be influenced by patient’s characteristics and comorbidities. In some series of ileostomy closure for pouch-anal anastomoses such as that from van Westreenen et al[3], only a 1.4% rate of infection is reported. When analyzing patient’s characteristics we realize mean age is only 49 years, most patients are ASA I-II, and indications for ileostomy are polyposis or inflammatory bowel disease rather than cancer. Data are therefore not comparable if the population of study is older or weaker. In our series, mean age was 60 years and patients mainly ASA II-III, with the main indication for ileostomy creation being colorectal cancer (56%).
Another important factor is if the 30-d infection rate is reported, or just the rate of infection during hospitalization. This can underestimate infections, as many of them occur after discharge and are managed in the outpatient clinic or by General Practitioners. This has been taken into consideration, and some recent publications already study standardized 30-d complications[17], and use classifications such as Clavien-Dindo to report results[9].
Different efforts have been made to reduce the infection rate of stoma-closure wounds. The technique employed has shown statistically significant results in various RCTs, such as that from Camacho-Mauries et al[18], favoring purse-string closure vs conventional sutures. In our study, a limitation regarding the retrospective analysis of skin closure was that data were incomplete and some surgical reports did not state the specific closure technique. From those available, interrupted, non absorbable sutures were the most frequently used, followed by subcuticular and staples. The staples group had a lower infection rate, but these data were not significant. Studies on the subject show contradictory results. In the retrospective study by Kobayashi et al[19], wound infection rate was as high as 23.5%, and subcuticular sutures apparently showed a protective effect. However, very recent studies and RCTs on wound closure, report purse-string sutures to achieve a 0% infection rate compared to other methods, thus not recommending linear closure of stoma wounds[20,21]. Other attempts, such as subcutaneous antibiotic implants (Gentamycin) in the wound, have not shown a relevant reduction in surgical site infections[22].
Another controversy around the subject is the best timing for stoma reversal. Some groups defend very early closure, even during the first admission, such as Alves et al[23], who perform reversal on the 8th postoperative day if no complications of the first intervention have occurred. Nevertheless, it is widely accepted to delay closure, and different studies report mean times of 3-6 mo, with a low medical priority given to this procedure[24].
In our study, we demonstrate that the delay in ileostomy closure (> 6 mo) is a risk factor for increased complications, and is associated with a higher incidence of pseudomembranous colitis, which was 4.3%. As can be seen in Figure 1, the incidence of complications increased with time (in months); there was an apparently ‘safer’ period around 3-6 mo, which could be considered optimal. From 9 mo onwards the rate of complications was > 30%.
Pseudomembranous colitis (PMC) is secondary to Clostridium difficile (C.diff) infection, and associated with substantial morbidity and mortality, increased duration of hospitalization, and a marked economic impact[25]. C.diff is a toxin-producing anaerobic bacterium responsible for antibiotic-associated colitis, and it is now the most common infectious cause of nosocomial diarrhea. Risk factors for PMC include advanced age, systemic antibiotic therapy, hospitalization, nursing homes or long-term care facilities, contact with active carriers, and presence of comorbidities[26]. It has been speculated that stoma closure can be another risk factor for PMC, which associates all the previous to an excluded and defunctioned bowel with altered flora, that could be more susceptible to C.diff infection[27]. In a large series of 13245 United States patients undergoing ileostomy closure, Wilson et al[28], report a 1.6% incidence of pseudomembranous colitis. This is an important factor to be considered, especially if an earlier closure can in fact reduce the risk.
This study was a retrospective analysis of institutional patients in order to identify risk factors for postoperative complications after ileostomy reversal and improve quality of care in our Colorectal Surgery Unit. Therefore, limitations are all those of an observational retrospective study, and in some cases (as in skin closure technique) data were missing from medical records. Due to the small number of patients some data may not reach statistical significance.
Although closure of a protective ileostomy is a fairly common surgical procedure, it has a high rate of complications, and this must be taken into account when the indication is made. The delay in stoma closure can increase the rate of complications in general, and specifically wound infections and colitis.
COMMENTS
Background
The creation of a defunctioning stoma after some colorectal procedures has demonstrated to highly reduce morbidity and mortality rates if a leak occurs, and is usually widely recommended. However, a stoma can be an issue for many patients both psychologically and due of stoma-related complications. As these stomas are supposed to be temporary, a planned second operation for reversal must be performed. In some cases, due to cancer-related complications or comorbidities stomas are never reversed. In patients considered fit for surgery, the reversal of the stoma should be performed at the “safest” time possible, to reduce complications. This timing is sometimes difficult to determine, as it depends on clinical factors, oncological follow-up and treatment, surgeon’s decision and institutional issues, such as “low-priority” consideration in surgical waiting lists.
Research frontiers
In the field of Colorectal Surgery, the optimization of anastomoses and methods to reinforce or protect them to avoid leaks is a matter of active research. Eventually, the creation of stomas would become obsolete if this could be achieved, improving surgical outcomes and reducing complications.
Innovations and breakthroughs
When revising the literature for the optimal timing for stoma reversal, recommendations usually suggest a 3 to 6 mo interval after the first intervention, always tailored to the specific risk factors and situation of the patient. When revising the real timing in our general practice, the authors realize there is a significant delay, and these recommendations are not followed. Complications related to prolonged bowel defunctioning (such as ileus, bleeding, diarrhea or Clostridium difficile colitis) and wound infections could be reduced if the time for closure is optimal. The best practice would be to guarantee an adequate healing from the first operation and close the stoma early enough to avoid the consequences of a prolonged defunctioning.
Applications
The study suggests that there is an optimal time frame to be considered when planning the ileostomy reversal that could reduce postoperative complications.
Terminology
A protective ileostomy is an opening of a loop of small bowel (usually the terminal ileum) in the abdominal wall, so that a distal anastomosis performed in the colon or rectum is protected from fecal matter and can heal properly. The ileostomy reversal is the surgical intervention performed to close the loop of small bowel and restore normal intestinal transit.
Peer review
Abstract is concise, topic is interesting, methods are appropriate, a well-structured discussion.
Footnotes
P- Reviewer: Gorseta K, O’Dwyer P S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
References
- 1.Bax TW, McNevin MS. The value of diverting loop ileostomy on the high-risk colon and rectal anastomosis. Am J Surg. 2007;193:585–587; discussion 587-588. doi: 10.1016/j.amjsurg.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Tan WS, Tang CL, Shi L, Eu KW. Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg. 2009;96:462–472. doi: 10.1002/bjs.6594. [DOI] [PubMed] [Google Scholar]
- 3.van Westreenen HL, Visser A, Tanis PJ, Bemelman WA. Morbidity related to defunctioning ileostomy closure after ileal pouch-anal anastomosis and low colonic anastomosis. Int J Colorectal Dis. 2012;27:49–54. doi: 10.1007/s00384-011-1276-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cottam J, Richards K, Hasted A, Blackman A. Results of a nationwide prospective audit of stoma complications within 3 weeks of surgery. Colorectal Dis. 2007;9:834–838. doi: 10.1111/j.1463-1318.2007.01213.x. [DOI] [PubMed] [Google Scholar]
- 5.D’Haeninck A, Wolthuis AM, Penninckx F, D’Hondt M, D’Hoore A. Morbidity after closure of a defunctioning loop ileostomy. Acta Chir Belg. 2011;111:136–141. doi: 10.1080/00015458.2011.11680724. [DOI] [PubMed] [Google Scholar]
- 6.Mengual-Ballester M, García-Marín JA, Pellicer-Franco E, Guillén-Paredes MP, García-García ML, Cases-Baldó MJ, Aguayo-Albasini JL. Protective ileostomy: complications and mortality associated with its closure. Rev Esp Enferm Dig. 2012;104:350–354. doi: 10.4321/s1130-01082012000700003. [DOI] [PubMed] [Google Scholar]
- 7.Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S. The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis. 2009;24:711–723. doi: 10.1007/s00384-009-0660-z. [DOI] [PubMed] [Google Scholar]
- 8.Thalheimer A, Bueter M, Kortuem M, Thiede A, Meyer D. Morbidity of temporary loop ileostomy in patients with colorectal cancer. Dis Colon Rectum. 2006;49:1011–1017. doi: 10.1007/s10350-006-0541-2. [DOI] [PubMed] [Google Scholar]
- 9.Luglio G, Pendlimari R, Holubar SD, Cima RR, Nelson H. Loop ileostomy reversal after colon and rectal surgery: a single institutional 5-year experience in 944 patients. Arch Surg. 2011;146:1191–1196. doi: 10.1001/archsurg.2011.234. [DOI] [PubMed] [Google Scholar]
- 10.Löffler T, Rossion I, Bruckner T, Diener MK, Koch M, von Frankenberg M, Pochhammer J, Thomusch O, Kijak T, Simon T, et al. HAnd Suture Versus STApling for Closure of Loop Ileostomy (HASTA Trial): results of a multicenter randomized trial (DRKS00000040) Ann Surg. 2012;256:828–835; discussion 835-836. doi: 10.1097/SLA.0b013e318272df97. [DOI] [PubMed] [Google Scholar]
- 11.Hasegawa H, Radley S, Morton DG, Keighley MR. Stapled versus sutured closure of loop ileostomy: a randomized controlled trial. Ann Surg. 2000;231:202–204. doi: 10.1097/00000658-200002000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sajid MS, Craciunas L, Baig MK, Sains P. Systematic review and meta-analysis of published, randomized, controlled trials comparing suture anastomosis to stapled anastomosis for ileostomy closure. Tech Coloproctol. 2013;17:631–639 [DOI 10.1007/s10151-013-1027-6]. doi: 10.1007/s10151-013-1027-6. [DOI] [PubMed] [Google Scholar]
- 13.Gong J, Guo Z, Li Y, Gu L, Zhu W, Li J, Li N. Stapled vs hand suture closure of loop ileostomy: a meta-analysis. Colorectal Dis. 2013;15:e561–e568. doi: 10.1111/codi.12388. [DOI] [PubMed] [Google Scholar]
- 14.Leung TT, MacLean AR, Buie WD, Dixon E. Comparison of stapled versus handsewn loop ileostomy closure: a meta-analysis. J Gastrointest Surg. 2008;12:939–944. doi: 10.1007/s11605-007-0435-1. [DOI] [PubMed] [Google Scholar]
- 15.Klink CD, Lioupis K, Binnebösel M, Kaemmer D, Kozubek I, Grommes J, Neumann UP, Jansen M, Willis S. Diversion stoma after colorectal surgery: loop colostomy or ileostomy? Int J Colorectal Dis. 2011;26:431–436. doi: 10.1007/s00384-010-1123-2. [DOI] [PubMed] [Google Scholar]
- 16.Mirbagheri N, Dark J, Skinner S. Factors predicting stomal wound closure infection rates. Tech Coloproctol. 2013;17:215–220. doi: 10.1007/s10151-012-0908-4. [DOI] [PubMed] [Google Scholar]
- 17.Sharma A, Deeb AP, Rickles AS, Iannuzzi JC, Monson JR, Fleming FJ. Closure of defunctioning loop ileostomy is associated with considerable morbidity. Colorectal Dis. 2013;15:458–462. doi: 10.1111/codi.12029. [DOI] [PubMed] [Google Scholar]
- 18.Camacho-Mauries D, Rodriguez-Díaz JL, Salgado-Nesme N, González QH, Vergara-Fernández O. Randomized clinical trial of intestinal ostomy takedown comparing pursestring wound closure vs conventional closure to eliminate the risk of wound infection. Dis Colon Rectum. 2013;56:205–211. doi: 10.1097/DCR.0b013e31827888f6. [DOI] [PubMed] [Google Scholar]
- 19.Kobayashi S, Ito M, Sugito M, Kobayashi A, Nishizawa Y, Saito N. Association between incisional surgical site infection and the type of skin closure after stoma closure. Surg Today. 2011;41:941–945. doi: 10.1007/s00595-010-4405-y. [DOI] [PubMed] [Google Scholar]
- 20.Klink CD, Wünschmann M, Binnebösel M, Alizai HP, Lambertz A, Boehm G, Neumann UP, Krones CJ. Influence of skin closure technique on surgical site infection after loop ileostomy reversal: retrospective cohort study. Int J Surg. 2013;11:1123–1125. doi: 10.1016/j.ijsu.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Habbe N, Hannes S, Liese J, Woeste G, Bechstein WO, Strey C. The use of purse-string skin closure in loop ileostomy reversals leads to lower wound infection rates--a single high-volume centre experience. Int J Colorectal Dis. 2014;29:709–714. doi: 10.1007/s00384-013-1822-6. [DOI] [PubMed] [Google Scholar]
- 22.Haase O, Raue W, Böhm B, Neuss H, Scharfenberg M, Schwenk W. Subcutaneous gentamycin implant to reduce wound infections after loop-ileostomy closure: a randomized, double-blind, placebo-controlled trial. Dis Colon Rectum. 2005;48:2025–2031. doi: 10.1007/s10350-005-0164-z. [DOI] [PubMed] [Google Scholar]
- 23.Alves A, Panis Y, Lelong B, Dousset B, Benoist S, Vicaut E. Randomized clinical trial of early versus delayed temporary stoma closure after proctectomy. Br J Surg. 2008;95:693–698. doi: 10.1002/bjs.6212. [DOI] [PubMed] [Google Scholar]
- 24.Floodeen H, Lindgren R, Matthiessen P. When are defunctioning stomas in rectal cancer surgery really reversed? Results from a population-based single center experience. Scand J Surg. 2013;102:246–250. doi: 10.1177/1457496913489086. [DOI] [PubMed] [Google Scholar]
- 25.Voelker R. Study: Vast majority of C. difficile infections occur in medical settings. JAMA. 2012;307:1356. doi: 10.1001/jama.2012.380. [DOI] [PubMed] [Google Scholar]
- 26.Khanna S, Pardi DS. Clostridium difficile infection: new insights into management. Mayo Clin Proc. 2012;87:1106–1117. doi: 10.1016/j.mayocp.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Randall JK, Young BC, Patel G, Fitzgerald A, George BD. Is Clostridium difficile infection a particular problem after reversal of ileostomy? Colorectal Dis. 2011;13:308–311. doi: 10.1111/j.1463-1318.2009.02139.x. [DOI] [PubMed] [Google Scholar]
- 28.Wilson MZ, Hollenbeak CS, Stewart DB. Impact of Clostridium difficile colitis following closure of a diverting loop ileostomy: results of a matched cohort study. Colorectal Dis. 2013;15:974–981. doi: 10.1111/codi.12128. [DOI] [PubMed] [Google Scholar]


