Abstract
OBJECTIVE
To compare former pediatric residents’ perceptions of their training in behavioral health care and collaboration from two separate continuity clinic sites within one training program that used either conventional or integrated models of behavioral health care.
METHODS
Residents of a single pediatric residency were assigned to one of two continuity clinic sites at the beginning of training. At one site, psychology fellows and faculty were integrated into the pediatric continuity clinic teams. At the other site, conventional patterns of behavioral health referral (that is, referral to outside specialists) and consultation continued. We surveyed fifteen years of graduates (N=245) from both clinic settings using a mailed 34-item instrument that queried alumni about their experiences during training and their comfort after training with behavioral health care and collaboration.
RESULTS
A total of 174 alumni (71%) returned completed questionnaires. Overall, there were significant differences between graduates in the two groups. Residents who trained and practiced alongside behavioral health fellows and faculty were significantly more likely to have reported consulting with, meeting with, and planning treatment with a behavioral health provider during residency, and more often reported that their continuity clinic experience prepared them for collaborating with behavioral health providers, yet only somewhat more often believed that the overall residency training prepared them for handling behavioral health issues in their current practice.
CONCLUSIONS
These findings suggest that an integrated training milieu can enhance pediatric education in the management of behavioral health problems and collaboration with behavioral health specialists.
Keywords: pediatrics, education, behavioral health, residency, survey
INTRODUCTION
Twenty percent of children and adolescents in the U.S. have diagnosable mental illness that causes impairment--a threefold increase in the past 20 years.1, 2 According to Kelleher, psychosocial problems are “the most common chronic condition for pediatric visits, eclipsing asthma and heart disease.”2 Pediatricians routinely underidentify these children,3-8 and those who are identified often do not get the care they need.9-12 Patient follow-through with referrals is low; as reported in 2002, less than one half of those referred to see a mental health provider did so within 6 months.13
Pediatric education in the care for children with behavior and mental health problems includes anticipatory guidance, problem identification, primary care counseling, referral, and collaborative care with a behavioral health professional.14, 15 The field has taken important steps forward in equipping pediatricians with skills in many of these domains, but opportunities still exist to improve the skill and self-efficacy of pediatricians in identifying and managing developmental and behavioral health problems and the systems of care in which they practice.16, 17 In March of 2009, the American Academy of Child and Adolescent Psychiatry (AACAP) and the American Academy of Pediatrics (AAP), issued a joint position paper highlighting the importance of addressing the mental health needs of children and adolescents in primary care settings and made recommendations for overcoming financial and administrative barriers to mental health care delivery in primary care. The AAP released its own policy statement in the summer of 2009 discussing the need for advances in residency training, continuing education, and clinician commitment for the provision of mental health care within pediatric primary care.
Interdisciplinary collaboration in the care of children with behavioral health problems is one specific area in need of improvement. There is general consensus that children with behavioral health care needs benefit when biomedical and psychosocial health care providers collaborate,18-22 and several excellent examples of interdisciplinary care models exist in the family medicine and pediatric literature.23-28 Developing lasting collaborative relationships with mental health colleagues, making effective referrals, and planning and executing a shared treatment plan across disciplines all require training, skill, and experience.17, 29 Nevertheless, educational systems rarely devote specific attention to equipping pediatric practitioners with the skills needed for productive collaboration.
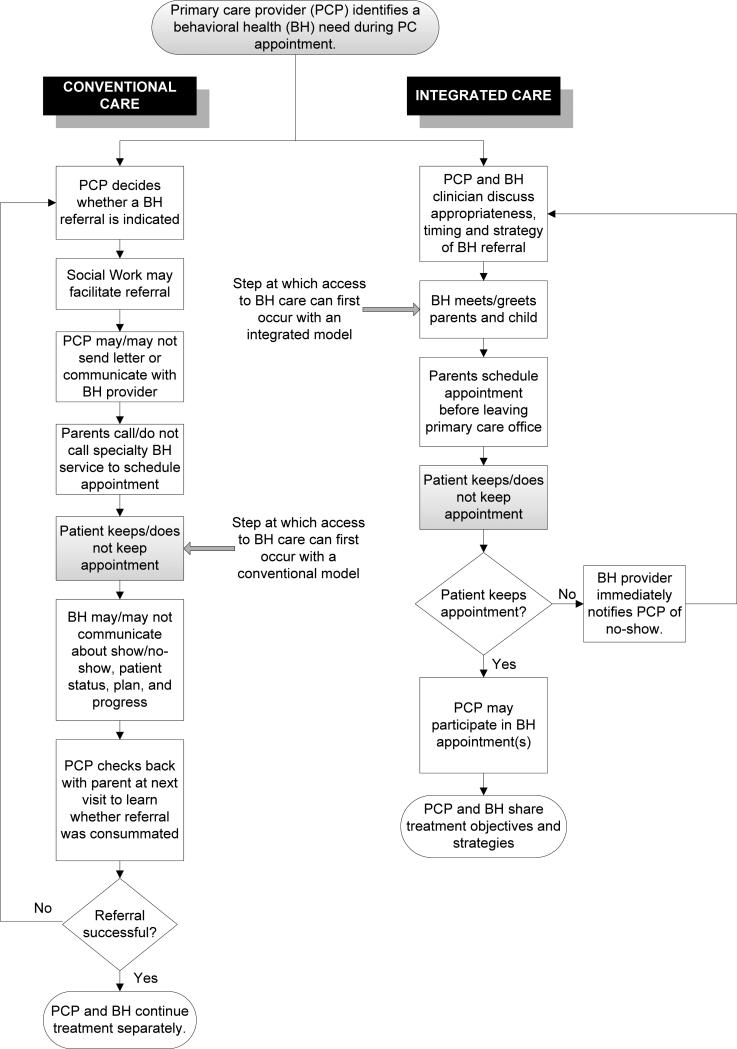
In this article, we examine learner perceptions of a model for enhancing pediatric residency education in behavioral health (BH) care. Our study compares former residents’ views of their training in BH care and collaboration, based on experiences in one of two continuity clinic sites that used different models of BH care and training. At one site, psychology fellows and faculty were integrated into pediatric continuity clinic teams, participating in the pre-clinic conferences and in charting areas, as well as being available for discussion and consultation throughout the clinic session.30 At the other site, BH referral and consultation followed conventional patterns of outside referral to BH specialists. Figure 1 summarizes the key differences between integrated and conventional BH in ambulatory pediatrics. The aim of this study was to examine potential differences in residents’ experiences with interdisciplinary collaboration during residency and their post-residency perceived preparation for and comfort in handling BH problems.
Figure 1. Conventional versus Integrated models of BH referral and care coordination.
This flowchart summarizes integrated and conventional models of BH care in ambulatory pediatrics. The shaded steps indicate the processes shared by the two models, and the non-shaded steps indicate processes that have key differences between the two models. Blocked arrows point to the earliest time at which patient access to BH care can occur in each model. The integrated process of care is not only shorter overall, but provides patients with access to BH care sooner than in the conventional process.
METHODS
This study qualified for expedited review and was approved by the University of Rochester Institutional Review Board Committee on Human Research.
Participants
Investigators mailed questionnaires to all pediatric residency alumni (N=245) who graduated from the University of Rochester residency program between 1989 and 2003. During their residencies, all but 4 of these participants had trained in one of the two hospital-based continuity clinics to which they were generally randomly assigned at the beginning of residency.
Questionnaire
Participants completed and returned by mail a 34-item survey designed to elicit descriptions of their interactions and collaboration with BH professionals, their education in BH care, and their overall BH experiences during residency. Item responses were measured using a 5-point Likert scale (1–Never, 2-Rarely, 3-Occasionally, 4-Sometimes, 5-Often/Always). The items were created by the authors and refined through feedback from colleagues, post-2004 residency graduates who were not eligible for this study, current residents and chief residents, and local consultants with expertise in survey development and instrument design. Study participants had no knowledge that we were comparing differences between continuity sites and time periods.
Continuity clinic settings
The University of Rochester pediatric residency primarily uses two sites for continuity clinic training: one practice is in a large University hospital (UniH) and the other in a large community teaching hospital (ComH). During the years which this survey encompasses, the sites had similar patient volumes (15,000-23,000 annual visits), population attributes (urban, 80% Medicaid), and resident continuity clinic structure. Residents were grouped into four half-day continuity clinics, consisting of 1-3 residents in each year of training, 1-2 advanced practice nurses, and 2-3 faculty preceptors. Although residents were not truly ‘randomly’ assigned (no random number table generation for clinic assignments), the chief residents assigned entering interns to one or the other site in a more or less arbitrary fashion, so it is reasonable to expect that the groups did not differ in any systematic way. Prior to 1994, BH care and training were similar at the two continuity clinics such that pediatricians at both institutions had limited and somewhat unpredictable access to on-site BH professionals (psychologists, family therapists, or social workers), and in most cases BH care followed the conventional model of referral to outside mental health providers (see FIGURE 1).
Changes in behavioral health care and education
In 1994, the Department of Pediatrics at the community hospital initiated a clinical service collaboration with a psychologist (family therapist) from the Department of Psychiatry at the University of Rochester to improve BH care. Between 1994 and 1998, a number of structured clinical and training activities pertaining to behavior and mental health were developed and implemented at the ComH continuity clinic. A defined primary care BH team began in 1994 and by 1998 the process culminated in the integration of postdoctoral psychology fellows and faculty into each of the resident continuity clinics.30
Consequently, BH care and education at the ComH site were carried out in the context of an integrated health team model, while the referral patterns and model of care for children with BH needs at the UniH clinic continued to follow the conventional model. The existence of two subpopulations of residents within a single pediatric training program with two different BH care and education models presented the opportunity for a comparative study.
Quasi-experimental design
We grouped participant responses by continuity clinic site (UniH vs. ComH) and by the training period (Early vs. Recent) of the respondent. “Early” graduates completed their training before 1994 (prior to the presence of integrated BH team at the ComH site), while “Recent” graduates trained from 1994-2003.
These groupings reflect the difference in BH training experiences of residents, depending upon which continuity clinic site they trained in and when. Thus, ComH Recent residents were the only participants who learned and practiced in an integrated continuity clinic alongside psychology fellows and faculty. This group serves as the quasi experimental group in the study: the group in which we would expect to find survey response differences if training in the integrated setting had an impact on their BH experiences, comfort, and preparation. ComH Early graduates and both UniH Early and Recent graduates practiced on continuity clinic teams with conventional BH referral and consultation models. These three groups of alumni served as quasi control groups, both historic (ComH Early vs. UniH Early, and ComH Early vs. ComH Recent and UniH Early vs. UniH Recent) and concurrent (ComH Recent vs. UniH Recent). The historic control groups provided a means of detecting any systematic differences between the two sites at baseline and changes over time at the control site not attributable to the experiment, which might have biased the recent concurrent group comparisons.
Analysis
Likert scale responses to key survey items were dichotomized into Never/Rarely/Occasionally vs. Sometimes/Often-Always and analyzed with Chi-Square tests to detect and quantify differences between the experimental and control groups (ComH Recent vs. UniH Recent and ComH Recent vs. ComH Early), as well as between the experimental group and the control groups combined (ComH Recent vs. ComH Early+UniH Early+UniH Recent). Raw percentages as well as chi-square significance tests are reported.
RESULTS
Response rate
One hundred and seventy four alumni returned surveys, providing an overall response rate of 71%. Table 1 shows that response rates were similar across sites and periods of training. Respondents include 61 residents (76% response rate) who had continuity clinic at ComH, and 111 residents (69% response rate) who had continuity clinic at UniH. Response rates among early graduates (70%) and recent graduates (71%) were also similar. Two alumni who had continuity clinic at a primary care practice in the community also returned surveys and were included with the UniH group, since they also experienced a conventional model of BH care and education.
Table 1.
Response Rate of Graduates by Continuity Clinic Site and Training Period
| Training Period | Continuity Clinic Site | Total # (%) | |
|---|---|---|---|
| Community Hospital n=80 | University Hospital + Other n=163 | ||
| 1989-1993 (Early) | 15/19 | 39/58 | 54/77 (70%) |
| 1994-2003 (Recent) | 46/61 | 74/107 | 120/168 (71%) |
| Total # (%) | 61/80 (76%) | 113/163 (69%) | 174/245 (71%) |
Other = Community (private) pediatric offices without integrated behavioral mental health care
Shaded box is quasi-experimental group.
Integrated v. conventional behavioral health care
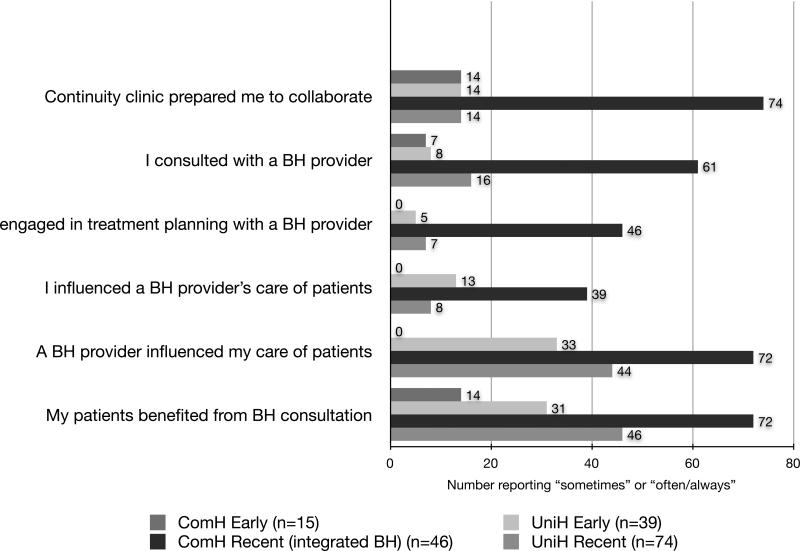
Figure 2 depicts resident responses by site (ComH, UniH) and time period (Early, Recent). There were substantial differences on key items between the experimental group and each of the control groups (p<.01). There were no statistical differences in responses between early and recent graduates at the UniH site, nor were there differences at baseline between early graduates of the ComH and UniH site.
Figure 2. Graduates’ report of experiences with collaboration, by site and period of training.
This graph compares the responses of graduates from the quasi-experimental group (recent period, Community hospital integrated BH model) with those of graduates from each of the three control groups. Responses of graduates from the quasi-experimental group were statistically different from those of graduates from each of the three control groups (p<.001).
Early period: 1989-1993; Recent period: 1994-2003.
ComH = Community teaching hospital
UniH = University hospital
Among recent graduates, 74% at the continuity clinic with integrated BH (ComH Recent) felt that their clinic experience prepared them for BH collaboration, compared with 14% who received conventional BH training (UniH Recent; p<.001). Few graduates (14% from both sites) who trained before 1994 reported that they felt prepared for collaboration with BH professionals.
Recent graduates from the ComH (integrated BH) continuity site reported significantly more experiences with BH consultation during training than did those from the UniH site (61% v. 16%, p<.001) or than those at either site prior to 1994 (7% and 8%, both p<.001). There was no statistical difference between responses of early and recent UniH graduates (16% v. 8%, p=.20). Among recent graduates, ComH graduates were more likely to report having had experiences with joint (that is, involving the pediatrician and the psychologist) meetings and treatment (46% v. 7%, p<.001), compared to 5% of all early graduates.
Recent ComH graduates, compared with recent UniH graduates, were also more likely to report that they felt that their input influenced the care BH professionals provided for their patients (39% v. 8%, p<.001), and they believed that the care they provided was influenced and improved by input from a BH professional (72% v. 44%, p=.003). While there was a trend over time at the UniH site (31% v. 46%, p=.14), only at the ComH site were recent graduates significantly more likely than concurrent peers or early graduates at either site to think that their patients benefited from collaboration with BH professionals (72% v. 46%, 14% and 31%, p=.01).
Overall preparation from residency training
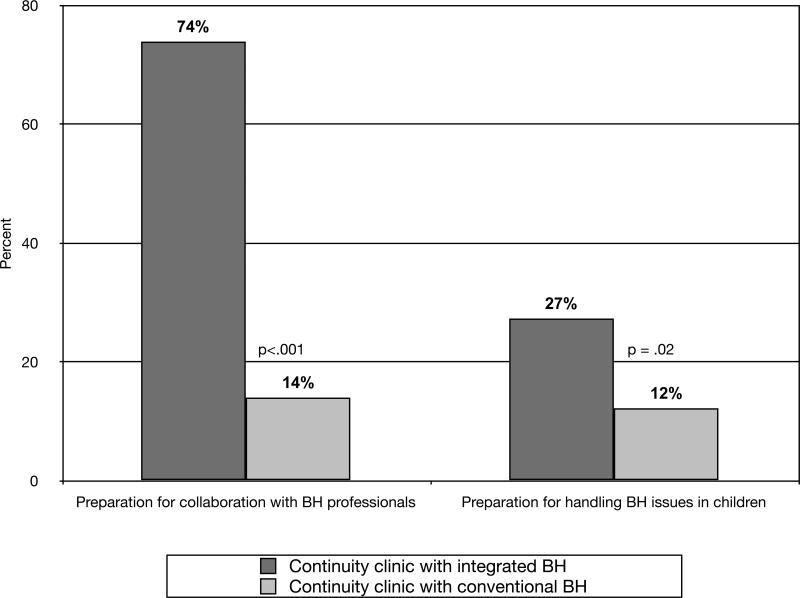
Contrary to expectations, we found only a minimum difference between alumni groups on how well the residency prepared them for managing BH problems in their current practice (see Figure 3). Although the proportion of graduates in the quasi experimental group who were positive about their ability to handle BH issues was significantly greater than the proportion of the quasi control group with the same item responses (27% v. 12%, p=.02), the low percent in both groups shows that, as a whole, neither group felt particularly well prepared. In review of the open-ended questions, graduates mentioned that the majority of BH exposure during residency occurred in the adolescent medicine and behavior/development rotations; however, for those with continuity at the ComH after integration, BH care exposure was reported to occur in their continuity clinic as well.
Figure 3. Graduates’ perceptions of preparation for collaboration compared with their perception of being able to manage children with behavioral issues.
This graph shows the number of graduates responding “sometimes” (4) or “always” (5) to the survey question: “My continuity clinic experience prepared me to collaborate with mental health professionals in the care of children” and the number responding “adequately” (4) or “very well” (5) to the survey question “To what extent did pediatric residency prepare you for handling mental issues?”
Responses of graduates with experience in a continuity clinic with integrated BH are compared with those of graduates with experience in a clinic with a traditional behavioral mental health referral model. Those residents who trained in an integrated practice during continuity clinic believed that they were significantly more prepared for collaboration with BH professionals (p<.001) and for handling BH issues in their current practice (p=.02).
Overall, those residents who trained in an integrated practice during continuity clinic believed that they were significantly more prepared for collaboration with BH professionals (74% v. 14%, p<.001) and somewhat more prepared for handling BH issues in their current practice (27% v. 12%, p=.02).
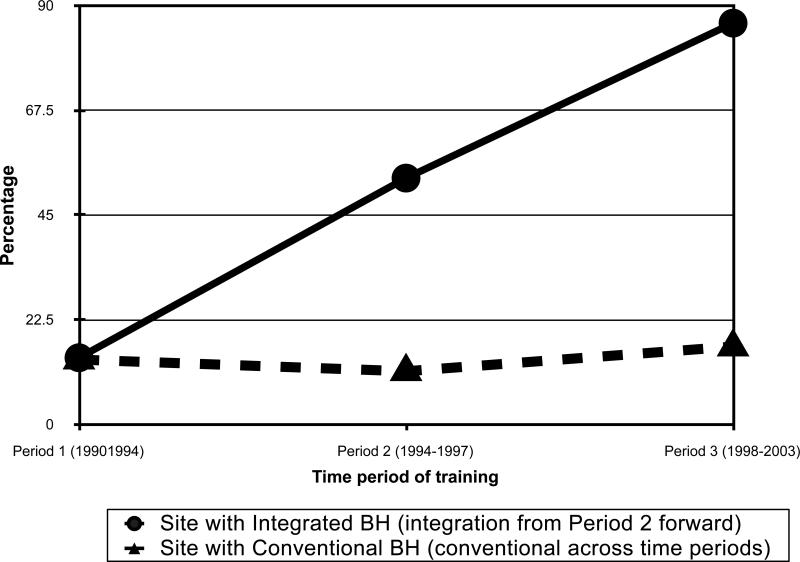
Dosage response
After detecting large differences in resident responses between the experimental and control groups, we sought to examine whether differences were observed based on the amount of exposure residents had to BH integration; that is, can a dose response phenomenon be demonstrated in the data? To examine this question, we plotted residents’ responses to the item, “Continuity clinic prepared me to collaborate with behavioral and mental health professionals,” according to when in the program's development they graduated. Since the integrated model was progressively implemented at the ComH between 1994 and 1998, graduates who had their continuity practice at the ComH during this period had some, but not continuous or complete, exposure to an integrated BH model in their continuity practice. Figure 4 shows that with some exposure to integrated BH (Period 2; graduates between 1994-1998 at the community site), alumni felt less prepared to collaborate with BH providers than those who trained at the ComH after 1998 (Period 3; when the integrated program was fully in place), but more than those with no exposure to an integrated model (Period 1). Furthermore, mere passage of time (without exposure to the integrated model) did not affect responses, as substantiated by the finding that positive responses to this survey item from residents with continuity clinic at UniH remained flat throughout the study.
Figure 4. Percent of graduates reporting that continuity clinic prepared them for collaboration, by clinic site and period of training.
This graph shows the percentage of graduates responding “sometimes” (4) or “always” (5) to the survey question: “My continuity clinic experience prepared me to collaborate with mental health professionals in the care of children.” Responses are compared by training sites across time period of training.
Period 1 (1990-1993): Traditional BH referral at both sites.
Period 2 (1994-1997): Initiation of integrated BH at ComH site, but not yet fully developed. Traditional BH referral at UniH.
Period 3 (1998-2003): Fully developed integrated BH at ComH site. Traditional BH referral at UniH.
DISCUSSION
Graduates who received ambulatory training during residency at the community teaching hospital as part of an integrated BH team were more likely to report feeling prepared for collaborating with mental health professionals. Alumni who trained in this integrated BH setting reported more experience in consultation, joint treatment, and collaborative patient care with BH colleagues, compared to residents who trained at the same site prior to implementation of integrated BH or graduates who trained concurrently at the University site that lacked integrated BH. These differences were consistent across survey items and are consistent with Guevara and colleagues' recent report that pediatricians with co-located mental health providers had a greater chance of consulting with and referring patients to mental health providers.31 Our results suggest that an integrated training milieu can be an effective means of preparing pediatricians to engage in collaborative and coordinated BH care for children facing psychosocial challenges. The differences in alumni reports across sites and time periods are noteworthy because the integrated BH program did not provide extensive didactic training in the skills needed to initiate a collaborative relationship, but rather exposed trainees to a setting and practice culture in which integrated care was the norm.
Our finding that graduates of the integrated BH program, although more comfortable working side-by-side with BH professionals, did not feel particularly comfortable directly managing BH problems in children is not surprising because our program focused on collaboration and integration as being essential to high quality BH care. An alumna who practices in a non-integrated setting might be expected to feel less comfortable without the support to which she had grown accustomed. Based on this finding, our program may need to consider providing more direct teaching about how one might handle a given case in a setting in which BH providers are not available. The failure to transfer training experiences into comfort managing care post-residency could also reflect an insufficient dose of collaborative BH contact. Continuity clinic is only one relatively modest time presence (10-20% of residents' time) in the residency experience. Joint training with BH faculty and trainees across additional rotations (inpatient, intensive care, subspecialty, and emergency department) may be needed to help graduates feel comfortable and competent in providing BH care.
To provide insight into the subjective experiences of the integrated BH experience, we include below an excerpt of a note sent to program faculty by an alumna now in clinical practice who trained in the integrated setting:
“You have ... heard many times how special the clinic at RGH [the ComH] was and I firmly believe that it was one of the most formative parts of my pediatric training... ...I know I would have never been comfortable with that intervention... and collaboration with my psychology colleague if I had not been exposed to that point of reference in training. The collaborative approach with families and external supports is so valuable in what I do everyday...I am a much better pediatrician for having trained with you...”
This study has a number of limitations. The survey was retrospective and included self-report data only. The survey was developed for the purposes of this program evaluation and is not a validated tool. We measured residents' perception of how well the program prepared them, but do not have any direct measure of whether this perception corresponded with actual competence in managing the needs of children with BH problems. Future controlled prospective studies that measure and compare residents' skills and knowledge, in addition to their perceptions of preparedness, would address these limitations.
This study provides evidence that integrated BH training is a promising approach to improve the preparation of pediatric residents to deal with the many complex behavior health problems that they will see in primary care practice. Although our graduates still lack confidence in providing mental health care independently, their increased ability to work in collaboration with BH consultants is an important asset in the primary care setting.
Abbreviations
- BH
behavioral health
- ComH
Community Hospital
- UniH
University hospital
Contributor Information
Lynn C. Garfunkel, Department of Pediatrics University of Rochester/Rochester General Hospital.
Anthony R. Pisani, Departments of Psychiatry and Pediatrics University of Rochester/Rochester General Hospital.
Pieter leRoux, Departments of Psychiatry and Pediatrics University of Rochester/Rochester General Hospital.
David M. Siegel, Departments of Pediatrics and Medicine University of Rochester/Rochester General Hospital.
References
- 1.Substance Abuse and Mental Health Services Administration [4/10/2009];Children and Adolescents with Mental, Emotional, and Behavioral Disorders. 2003 http://mentalhealth.samhsa.gov/publications/allpubs/CA-0006/default.asp.
- 2.Kelleher KJ, McInerny TK, Gardner WP, Childs GE, Wasserman RC. Increasing identification of psychosocial problems: 1979-1996.[see comment]. Pediatrics. 2000 Jun;105(6):1313–1321. doi: 10.1542/peds.105.6.1313. [DOI] [PubMed] [Google Scholar]
- 3.Costello EJ, Edelbrock C, Costello AJ, Dulcan MK, Burns BJ, Brent D. Psychopathology in pediatric primary care: the new hidden morbidity. Pediatrics. 1988 Sep;82(3 Pt 2):415–424. [PubMed] [Google Scholar]
- 4.Costello EJ, Shugart MA. Above and below the threshold: severity of psychiatric symptoms and functional impairment in a pediatric sample. Pediatrics. 1992;90(3):359–368. [PubMed] [Google Scholar]
- 5.Glascoe FP. Increasing identification of psychosocial problems. Pediatrics. 2001;107(6):1496. [PubMed] [Google Scholar]
- 6.Lavigne JV, Binns HJ, Christoffel KK, et al. Behavioral and emotional problems among preschool children in pediatric primary care: prevalence and pediatricians' recognition. Pediatric Practice Research Group. Pediatrics. 1993;91(3):649–655. [PubMed] [Google Scholar]
- 7.Brown JD, Riley AW, Wissow LS, Brown JD, Riley AW, Wissow LS. Identification of youth psychosocial problems during pediatric primary care visits. Adm Policy Ment Health. 2007 May;34(3):269–281. doi: 10.1007/s10488-006-0106-7. [DOI] [PubMed] [Google Scholar]
- 8.Horwitz SM, Kelleher KJ, Stein RE, et al. Barriers to the identification and management of psychosocial issues in children and maternal depression. Pediatrics. 2007 Jan;119(1):e208–218. doi: 10.1542/peds.2005-1997. [DOI] [PubMed] [Google Scholar]
- 9.National Research Council . From Neurons to Neighborhoods: The Science of Early Childhood Development. National Academy Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- 10.Stein REM, Horwitz SM, Penfold RB, et al. Do Pediatricians Think They Should Care for Patients with New Morbidity? Results of the AAP Periodic Survey. PAS meetings. 2005 (PAS 2005:57:1665) [Google Scholar]
- 11.United States Department of Health and Human Services (USDHHS) [November 14, 2008];Report of the Surgeon General's Conference on Children's Mental Health. 2000 http://www.surgeongeneral.gov/topics/cmh/childreport.htm.
- 12.Gardner W, Kelleher KJ, Pajer K, et al. Follow-up care of children identified with ADHD by primary care clinicians: A prospective cohort study. J Pediatr. 2004 Dec;145(6):767–771. doi: 10.1016/j.jpeds.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 13.Rushton J, Bruckman D, Kelleher K. Primary care referral of children with psychosocial problems. Arch Pediatr Adolesc Med. 2002 Jun;156(6):592–598. doi: 10.1001/archpedi.156.6.592. [DOI] [PubMed] [Google Scholar]
- 14.Accreditation Council for Graduate Medical Education [November 12, 2008];Program requirements for residency education in pediatrics. 2007 http://www.acgme.org/acWebsite/downloads/RRC_progReq/320_pediatrics_07012007.pdf.
- 15.Kittredge D, Baldwin CD, Bar-on ME, Beach PS, Trimm RF. [11/12/08];APA Educational Guidelines for Pediatric Residency. 2004 http://www.ambpeds.org/egweb.
- 16.Council on Children With Disabilities Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006 Jul;118(1):405–420. doi: 10.1542/peds.2006-1231. [DOI] [PubMed] [Google Scholar]
- 17.Kelleher KJ, Campo JV, Gardner WP. Management of pediatric mental disorders in primary care: where are we now and where are we going? Curr Opin Pediatr. 2006 Dec;18(6):649–653. doi: 10.1097/MOP.0b013e3280106a76. [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Pediatrics [11/14/2008];Improving Mental Health in Primary Care Through Access, Collaboration, and Training. http://www.aap.org/mentalhealth/docs/IMPACT%20Fact%20Sheet.pdf. 2006.
- 19.American Academy of Pediatrics The future of pediatric education II. Organizing pediatric education to meet the needs of infants, children, adolescents, and young adults in the 21st century. A collaborative project of the pediatric community. Pediatrics. 2000 Jan;105(1 Pt 2):157–212. [PubMed] [Google Scholar]
- 20.American Academy of Pediatrics (Committee on Psychosocial Aspects of Child and Family H. The new morbidity revisited: a renewed commitment to the psychosocial aspects of pediatric care. Pediatrics. 2001 Nov;108(5):1227–1230. doi: 10.1542/peds.108.5.1227. [DOI] [PubMed] [Google Scholar]
- 21.American Academy of Pediatrics (Medical Home Initiatives for Children With Special Needs Project Advisory Committee) The medical home. Pediatrics. 2002 Jul;110(1 Pt 1):184–186. [Google Scholar]
- 22.Pincus HA. Patient-oriented models for linking primary care and mental health care. General Hospital Psychiatry. 1987 Mar;9(2):95–101. doi: 10.1016/0163-8343(87)90020-x. [DOI] [PubMed] [Google Scholar]
- 23.Allmond BW, Tanner JL. The family is the patient. Williams & Wilkens; Baltimore: 1999. [Google Scholar]
- 24.Minkovitz CS, Hughart N, Strobino D, et al. A Practice-Based Intervention to Enhance Quality of Care in the First 3 Years of Life: The Healthy Steps for Young Children Program. JAMA: Journal of the American Medical Association. 2003 Dec;290(23):3081–3091. doi: 10.1001/jama.290.23.3081. [DOI] [PubMed] [Google Scholar]
- 25.Perrin EC. Collaboration in pediatric primary care: A pediatrician's view. Journal of Pediatric Psychology. 1999 Oct;24(5):453–458. doi: 10.1093/jpepsy/24.5.453. [DOI] [PubMed] [Google Scholar]
- 26.Schroeder CS. Psychologists and pediatricians in collaborative practice. In: Resnick RJ, Rozensky RH, editors. Health psychology through the life span: Practice and research opportunities. American Psychological Association; Washington, DC: 1996. pp. 109–131. [Google Scholar]
- 27.Edwards TM, Patterson JE, Grauf-Grounds C, Groban S. Psychiatry, MFT, & family medicine collaboration: The Sharp Behavioral Health Clinic. Families, Systems & Health. 2001;19(1):25–35. [Google Scholar]
- 28.Seaburn D, Gawinski B, Harp J, McDaniel SH, et al. Family systems therapy in a primary care medical setting: The Rochester experience. Journal of Marital & Family Therapy. 1993 Apr;19(2):177–190. [Google Scholar]
- 29.McDaniel SH, Campbell T, Hepworth J, Lorenz A. Family-oriented Primary Care: 2nd Edition. Springer-Verlag; New York: 2004. [Google Scholar]
- 30.Pisani AR, LeRoux P, Siegel D. Joint Training of Pediatric Residents and Psychology Fellows in a Community Hospital Based Teaching Practice. Under Review.
- 31.Guevara JP, Greenbaum PE, Shera D, et al. Survey of mental health consultation and referral among primary care pediatricians. Acad Pediatr. 2009 Mar-Apr;9(2):123–127. doi: 10.1016/j.acap.2008.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]