Abstract
Purpose
The purpose of the study was to determine the effects of gender on participation in a community-based, culturally tailored diabetes lifestyle intervention, led by trained community health workers (CHW), and conducted with African Americans and Latinos with type 2 diabetes.
Methods
This study utilized data collected from 180 participants. Multivariable binary and cumulative logistic regression models were used to analyze associations between gender and race/ethnicity with study completion and participation in three aspects of the intervention: group classes, CHW home visits, and CHW-accompanied doctor visits.
Results
Among Latinos, men were less likely than women to complete the study, attend >x classes, and complete # CHW home visits. There were no gender differences in participation seen among African-Americans.
Conclusions
Diabetes management interventions may need to adapt their designs to optimize retention and participation of Latino men. Among African American men, the CHW model may be promising. Reasons for low participation among Latino men should receive more study. Future studies should assess whether similar findings apply in other communities and populations.
Keywords: Diabetes, Men, Intervention, Health Care Utilization
Diabetes is one of the leading causes of death in the United States1, increases the risk for other health conditions such as heart disease and stroke, and is the leading cause of kidney failure, non-traumatic lower-limb amputation and new cases of blindness in adults in the U.S.1 According to the Center for Disease Control (CDC) (2011), diabetes affects 25.8 million people, or 8.3% of the U.S. population,1 and is significantly more prevalent among African-American and Hispanic men than non-Hispanic white men.2,3 From 1997–2010, rates of diabetes increased 52% for Mexican American men and 143% for African American men.2,3 Access to health care and culturally appropriate lifestyle interventions can play an important role in preventing diabetes and diabetes related complications.4–10 However, disparities in access to diabetes care and the quality of diabetes care have been reported for low-income African Americans and Latinos, specifically if they utilize public health insurance or are uninsured.1
An extensive body of research indicates that minority men, in particular, have health seeking behaviors that may lower their participation in diabetes interventions, general health care and self-management.11–14 During their lifetime men have fewer visits with physicians and go longer periods in between seeing physicians in comparison to women.13,14 Latino men who are non-English speaking and/or do not have US citizenship face additional barriers to treatment due to potential fear of deportation and language barriers. Factors documented to impact help-seeking and health care utilization in African American and Latino men include medical mistrust, lack of access to health insurance and health care facilities, lack of usual source of care, and traditional male norms about disclosing vulnerability.18–21
Many studies have examined the effectiveness of interventions in addressing racial and ethnic disparities in diabetes.4–10 However, to the authors’ knowledge there are no studies that examine whether minority men participate less in diabetes interventions than minority women. Considering the growing evidence of the importance of community-based diabetes treatment programs in effective diabetes self-management and control,5,7,8,11 it is important to examine whether gender influences diabetes intervention participation. The primary aims of this study were to examine the impact of gender on participation in a community-based, culturally tailored, community health worker (CHW)-led diabetes intervention, conducted with African Americans and Latinos with type 2 diabetes. The study hypothesized that adult African American and Latino men with diabetes would have lower levels of study completion and intervention participation than African American and Latino women.
Methods
Research Design
Socio-demographic variables were cross-tabulated by gender for Latinos, African Americans, and for both groups combined. To compare socio-demographics by gender, a t-test was used for continuous variables, Fisher’s exact test for categorical variables with expected count under 5 in any cell, and Pearson’s chi-square test for all other categorical variables.
Logistic regression models were used to examine the association between gender and participation, and between gender and study completion. Separate models examined the participation outcomes of completion, intervention class attendance, doctor visits with CHWs, and home visits with CHWs—first including gender as an independent predictor, then including a race/ethnicity by gender interaction (race/ethnicity × gender). For the models with interaction terms, linear combinations of parameters produced estimates for the association of gender with participation, and gender with completion, for each racial/ethnic subgroup. When obtaining the estimates all covariates were set to their average values, except for healthcare site, which was set to its average values in the dataset. Because healthcare site was strongly correlated with race/ethnicity, the study used the actual distribution for African Americans or Latino/as in the model-based estimates odds of participation. For the rest of the covariates, the mean was used in the estimations. While completion was a binary variable, class attendance, doctor visits with CHWs, and home visits by CHWs were multi-category. Cumulative logistic models were used for the multiple-category outcomes. Cumulative logit models were selected because the Akaike Information criteria (AIC) indicated that they fit the data better than Poisson and Normal models.23 Number of one-to-one CHW visits was included in the models for completion and doctor visits, but omitted from the models for class attendance and home visits because a one-to-one visit had been counted as a class make-up session and as a home visit. Based on the magnitude of differences in completion rates by gender and sample size, the study had over 75% power to detect a 35 point difference in completion between Latino men and women (n =71).24 The observed difference in completion rates between African-American men and women was less than the difference the study had power to detect, based on the N of participants. Analyses were conducted with SAS Version 9.3 software.25
Sample and Setting
The present study utilized data collected during the Racial and Ethnic Approaches to Community Health (REACH) Detroit Partnership’s community-based, culturally tailored diabetes lifestyle and self-management intervention.8,9 The intervention’s primary goals were to improve diabetes-related lifestyle and self-management behaviors, and clinical outcomes, among African American and Latino adults in two Detroit, Michigan low-income communities. Participants were recruited from 3 health care systems in Detroit, one of which was a Federally Qualified Community Health Center. The intervention was conducted in a nonrandomized, 1-group design. The intervention was 6 months long, with surveys and interviews at baseline, 6 months and 12 months. The African American-centered Journey to Health and Latino-centered El Camino a la Salud curricula were culturally and linguistically tailored to each population using a community-based participatory approach, and delivered during 11 group meetings by trained CHWs.9 Curriculum content involved key diabetes management behaviors, such as physical exercise, health eating, and medication adherence.9 CHWs offered one-to-one intervention class make-up sessions with participants who missed group class sessions. CHWs also attempted to complete at least 6 home visits, and offered to attend doctor visits with participants during the intervention.8,9 At post-intervention follow up, participants on average had improved knowledge of the relationship between health eating, exercise, and blood sugar control, along with significant healthy eating changes and improvement in HbA1c values.9 Intervention participants had a significantly larger drop in HbA1c than matched non- participants at the same healthcare sites.9
Study variables
Outcome Variables
Dependent variables included study completion rate, intervention class attendance, home visits by CHWs, and doctor visits with CHWs. Completion was categorized as withdrew (0), and completed (1). A completer was defined as someone who completed either the survey or the interview at the 12 month data collection point, whether or not they attended any intervention sessions. Intervention class attendance was coded as no classes (0), 1–5 classes (1), 6–10 classes (2), and 11 classes (3), so that the distribution in each category was even. Doctor visits with CHW’s was coded as no doctor visits (0), 1 doctor visit (1), 2 doctor visits (2), 3 doctor visits (3) and 4 or more doctor visits (4). Lastly, home visits were categorized as 0–14 home visits (coded as 0–14) and 15 or more visits (15).
Independent Variables
Independent variables added to models as covariates included socio-demographic characteristics (education, age, race/ethnicity, and marital status). Education was categorized as less than high school education (0), and high school education or greater (1). Age was recorded in years at the time of the baseline interview. Marital status was categorized as single (1), and married or partnered (2).
Other independent variables added to models because they are documented to be related to diabetes management were self-rated health, diabetes emotional distress, doctor satisfaction, and doctor support. Self-rated health was measured by a standard 5-point scale. Diabetes-specific emotional distress was measured by the Problem Areas in Diabetes (PAID) scale.22 PAID scores were calculated using the mean score among 20 items using a five point Likert-scale, and then scaling to a 0–100 range. Doctor support scores were calculated using the mean of a five-item scale that measured how participants perceived level of doctor support. Respondents rated questions as strongly disagree (1), disagree (2), neutral (3), agree (4), and strongly agree (5). The five-item scale included the following questions: (1) you feel understood by your doctor; (2) you feel trust in your doctor; (3) your doctor answers your questions fully and carefully; (4) your doctor tried to understand how you see things before suggesting a new way to do things; and (5) you get all the support that you need from your doctor. Doctor satisfaction scores were calculated using the mean of a 5-item scale. Respondents rated their satisfaction as: not at all satisfied (1), not very satisfied (2), somewhat satisfied (3), very satisfied (4), and completely satisfied (5). The five-item scale documented satisfaction for time spent with doctor, accessibility of doctor, communication with doctor and support provided by other health professionals in the doctor’s office, including nurses and educators.
Attending a one-to-one intervention class make-up session was also included in models as an additional predictor of intervention participation. Whether or not a participant had a one-to-one intervention class make-up session with a CHW was coded as (1) for yes and (0) for no.
RESULTS
Participant characteristics
Table 1 describes demographic differences for Latino/a and African American men and women who participated in the intervention. Within ethnic groups, there were no significant gender differences in age and educational level. Latino/a men and women averaged 54 and 49 years of age and African American men and women averaged 59 and 60 years of age, respectively. Almost 77% of Latina women and almost 89% of Latino men had less than a high school education, compared to 27% and 32% of African American women and men, respectively. Overall, Latino and African American men were much more likely to be married compared to women in their race/ethnic group. Only 45% of Latina women and 25% of African American women reporting being married or partnered, compared to 72% and 68% of their male counterparts, respectively. Among Latino/as, men were more likely to be employed than women (39% of men and 14% of women). Among African Americans, similar percentages were employed (28% of men and 26% of women).
Table 1.
Selected Baseline Characteristics of Study Participants (n=180)
| Variable of Interest | Latinos (N = 71) |
African Americans (N = 109) |
Everyone (N = 180) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Women (N=53) |
Men (N=18) |
P valuea | Women (N=81) |
Men (N=28) |
P value | Women (N=134) |
Men (N=46) |
P value | |
| Age, mean (SD)b | 53.7 (13.7) | 48.6 (17.0) | 0.20 | 59.5 (12.8) | 59.0 (12.6) | 0.84 | 57.2 (13.4) | 54.9 (15.2) | 0.33 |
| Education, n(%) | 0.49 | 0.61 | 0.39 | ||||||
| <HS | 41 (77.4) | 16 (88.9) | 22 (27.2) | 9 (32.1) | 63 (47.0) | 25 (54.3) | |||
| HS | 12 (22.6) | 2 (11.1) | 59 (72.8) | 19 (67.9) | 71 (53.0) | 21 (45.7) | |||
| Marital Status, n(%) | 0.05 | <0.01 | <0.01 | ||||||
| Single | 29 (54.7) | 5 (27.8) | 61 (75.3) | 9 (32.1) | 90 (67.2) | 14 (30.4) | |||
| Married/Partnered | 24 (45.3) | 13 (72.2) | 20 (24.7) | 19 (67.9) | 44 (32.8) | 32 (69.6) | |||
| Employment*, n(%) | 0.02 | 0.84 | 0.13 | ||||||
| Unemployed | 44 (86.3) | 11 (61.1) | 57 (74.0) | 18 (72.0) | 101 (78.9) | 29 (67.4) | |||
| Full/Part-time | 7 (13.7) | 7 (38.9) | 20 (26.0) | 7 (28.0) | 27 (21.1) | 14 (32.6) | |||
Omitted missing responses (N=2 Latinos, N=10 African Americans).
p-values were obtained using the t-test for continuous variables, Fisher’s exact test for categorical variables with expected count < 5 in any cell, and Pearson’s chi-square test for all other categorical variables.
SD=Standard Deviation
Study Participation
Only 39% of Latino men completed the study compared to 74% of Latinas (Table 2). Among African Americans, the completion rate did not differ significantly by gender: 79% and 68% of African American women and men, respectively. Latino men also had the lowest class attendance of all groups, attending an average of 3 classes compared to 6 by Latina women. African American men and women attended an average of 8 and 7 intervention classes, respectively. In general, all four groups participated in the same number of home visits, with an average of two over the span of the intervention. Latinos/as, were accompanied by a CHW to more doctor visits than African Americans, regardless of gender.
Table 2.
Outcome Variable Distribution (n=180)
| Variable of Interest | Latinos (N = 71) |
African Americans (N = 109) |
Everyone (N = 180) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Women (N=53) |
Men (N=18) |
P valuea | Women (N=81) |
Men (N=28) |
P value | Women (N=134) |
Men (N=46) |
P value | |
| Withdrawal, n(%) | 0.01 | 0.23 | 0.01 | ||||||
| Active | 39 (73.6) | 7 (38.9) | 64 (79.0) | 19 (67.9) | 103 (76.9) | 26 (56.5) | |||
| Withdrew | 14 (26.4) | 11 (61.1) | 17 (21.0) | 9 (32.1) | 31 (23.1) | 20 (43.5) | |||
| Total Classes, mean(SD)b | 6.4 (4.0) | 3.2 (3.8) | <0.01 | 7.4 (4.4) | 8.1 (4.3) | 0.49 | 7.0 (4.2) | 6.2 (4.7) | 0.27 |
| CHW Home visits, mean(SD) | 2.3 (2.9) | 1.9 (3.5) | 0.60 | 2.0 (2.6) | 1.9 (2.7) | 0.87 | 2.1 (2.7) | 1.9 (3.0) | 0.63 |
| CHW Dr visits, mean(SD) | 1.7 (2.3) | 1.2 (1.8) | 0.42 | 0.4 (0.6) | 0.3 (0.6) | 0.59 | 0.9 (1.7) | 0.7 (1.3) | 0.30 |
p-values were obtained using the t-test for continuous variables, Fisher’s exact test for categorical variables with expected count < 5 in any cell, and Pearson’s chi-square test for all other categorical variables.
SD=Standard Deviation
Association Between Gender and Participation
Adjusted Analysis with No Interaction Term Between Gender and Race/Ethnicity
Table 3 reports results for models with and without the interaction term, adjusting for covariates. The first set of adjusted regression models did not include an interaction term between gender and race/ethnicity. Men, overall, were less likely to complete the study than women (OR=0.38 [0.15, 0.96]); p<.05. Gender was not significantly associated with doctor’s visits with CHWs, intervention class attendance or home visits with CHWs.
Table 3.
Adjusted Odds Ratios* for the Influence of Gender on Participation, With and Without Race/Ethnicity by Gender Interaction
| Logistic Regression Models for Participation Measures | ||||
|---|---|---|---|---|
| Intervention Retention2,4 | CHW Dr. Visits3,4 | Intervention Classes3 | CHW Home Visits3 | |
| Gender | AOR5 [95% CI] |
AOR5 [95% CI] |
AOR5 [95% CI] |
AOR5 [95% CI] |
| Model 1 without Interaction Term | ||||
| Men1 | 0.38* (0.15, 0.96) | 0.57 (0.24, 1.37) | 0.84 (0.40, 1.74) | 0.65 (0.32, 1.30) |
| Model 2 with Interaction Term | ||||
| African American Men1 | 0.54 (0.17, 1.78) | 0.59 (0.19, 1.84) | 2.42 (0.90, 6.49) | 0.96 (0.41, 2.26) |
| Latino Men1 | 0.24* (0.06, 0.92) | 0.55 (0.17, 1.82) | 0.24** (0.09, 0.70) | 0.34* (0.11, 0.99) |
Adjusted odds ratios derived from multiple logistic regression models. Covariates were held at their mean for estimations: Age, Education, Marital Status, Treatment Site, Self-rated Health, PAID, MD Satisfaction, MD Support, One-to-One visits3
p<.05;
p < .01;
p < .001
Reference category=Women, 2 Reference category=African-American women, 3 Reference category=Latina women
Binary outcome, logistic regression
Ordered categories, cumulative logit regression
One-to-One Visits were included in models for Withdrawal & Dr. Visits only
Adjusted Odds Ratio
Adjusted Analysis with Interaction Between Gender and Race/Ethnicity
Next, the study added interaction terms between gender and race/ethnicity to all of the study models. Among Latinos, men were less likely to complete the study than women (OR=0.24 [0.06, 0.92]); p<.05, had lower intervention class attendance than Latino women (OR= 0.24 [0.09, 0.70]); p<.01 and had fewer CHW home visits (OR=0.34 [0.11, 0.99]); p<.05. Significant racial/ethnic and gender differences were not found for doctor visits accompanied by CHWs. Among African Americans, completion and intervention class attendance and CHW home visits did not differ significantly by gender.
Receiving one-to-one intervention class make-up sessions with CHWs increased odds for study completion (OR=5.99 [2.57, 14.00]); p<.001 and increased CHW accompanied doctor visits for each racial/ethnic group (OR=3.06 [1.56, 6.01]); p<.01 (data not shown in Table 3).
African American women and men, and Latina women, had statistically similar odds of attending all classes versus less than all classes (Figure 1). Latino males had lower odds (OR= 0.14 [0.05, 0.37]) than African American males (OR=1.67 [0.70, 3.99]) of attending all 11 intervention classes. Latina (OR=0.55 [0.30, 1.01]) and African American women (OR=0.69 [0.41, 1.16]) had statistically similar class attendance. Latina women (OR=3.10 [1.37, 7.04]), African American women (OR=6.16 [2.89, 13.15]), and African American men (OR=3.35 [1.18, 9.50]) had higher odds of study completion versus withdrawal. Latino men (OR=0.75 [0.23, 2.47]) had statistically similar odds of completing or withdrawing.
Figure 1.
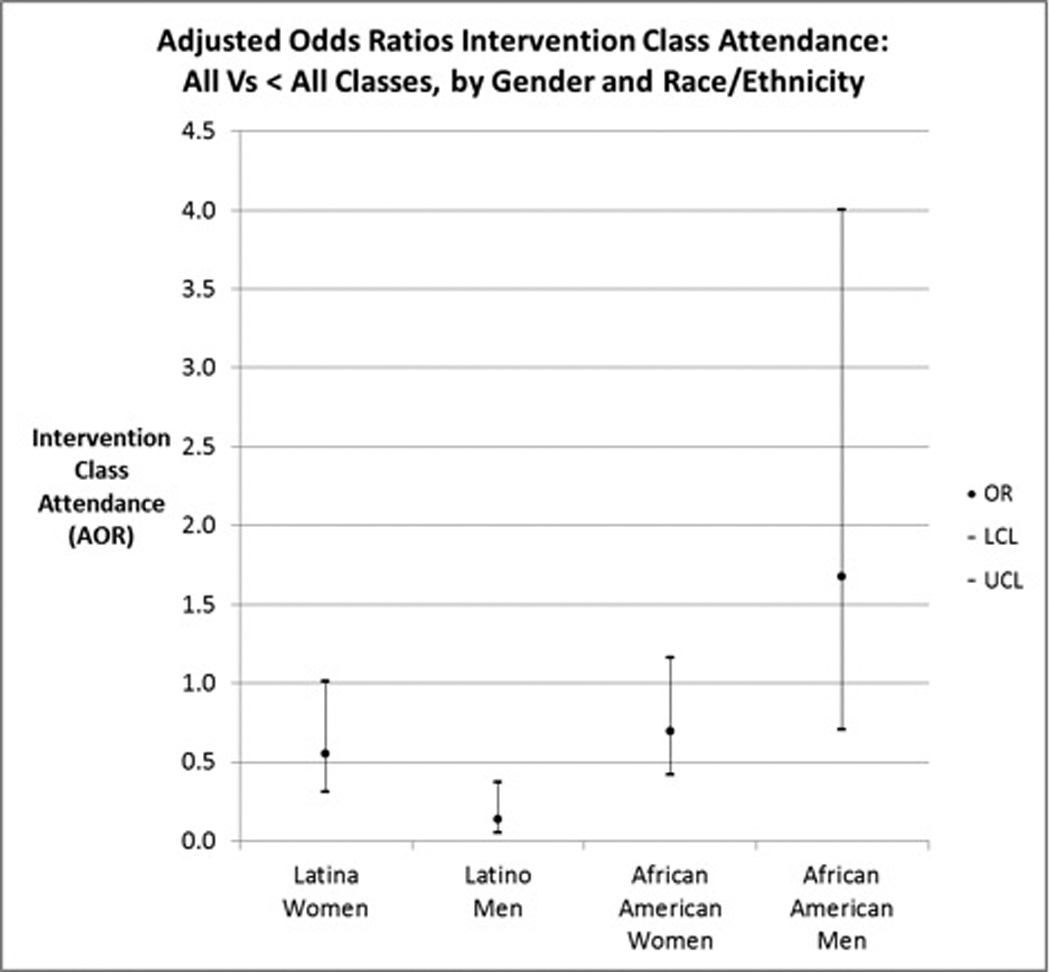
Adjusted Odds Ratios Intervention Class Attendance: All Vs < All Classes, by Gender and Race/Ethnicity
DISCUSSION
In this study of African American and Latinos, gender had an inconsistent impact on participation in a culturally tailored CHW-led diabetes lifestyle intervention. Although, overall, men had lower study completion rates than women, this finding was driven by the very low study completion rate of Latino men. When analyzing men separately by race/ethnicity, African-American men were similar to African-American women in all measures of participation, while Latino men had significantly lower participation than Latino women by most measures.
A prior study in this population found that the present CHW-led intervention was effective for improving several diabetes-related outcomes.8–10 Other studies have demonstrated the effectiveness of CHW’s with ethnic minority women;26 however, none have specifically examined their effectiveness with men. A systematic review of CHW literature and semi-structured interviews with CHW staff of programs that worked primarily with minority populations,27 found that some programs had problems with recruitment, retention, and communication with men. Two of the CHW programs examined found that gender was a factor in recruitment into programs and revealed that some programs had difficulty matching male CHW’s with male clients, which led to problems communicating about sensitive topics, such as sexual dysfunction as a result of diabetes complications.27 In the REACH Detroit CHW intervention, CHW’s were predominately women, which may have led to reluctance to discuss particular issues, or to communicate in general. One CHW was male and also African American, which could have led to greater participation and less completion in African American men than for Latino men. Further studies should compare male participation in CHW-led versus non-CHW-led community diabetes interventions and assess whether staffing by male CHW’s and more attention to gender-specific issues may contribute to increased male participation.
The fact that African American men had higher intervention class attendance than Latino men may be evidence that aspects of this intervention were more successful with African American men despite the potential barrier gender may play in CHW models and men’s health more generally. For both groups, women tend to be more involved in family networks and men in ethnic minority groups may rely on wives or other female family members as ‘health managers’.28 However, African American men who are older tend to have smaller support networks and live alone at higher rates, while Latino men may be more likely to depend on wives for self-care, especially in relation to diet, making self-care largely dependent on another individual.28 Given the differences in study completion and participation rates between the two groups, and what is already known about the role of women as gatekeepers in health, more research should be conducted that closely examines the nature of successful and unsuccessful relationships between female CHWs and male clients. More research regarding the incorporation of family participation in the CHW model, particularly in relation to significant others, should also be considered.
One-to-one CHW sessions also significantly increased the odds of intervention participation among men in the study. These one-to-one sessions helped to maintain participation in the study by serving as make-up sessions for missed intervention classes and home visits by CHWs. This finding demonstrates that flexibility and individualized services might improve overall intervention participation. Contrary to the present study, a study of a diabetes self-management education program for African American men with type 2 diabetes tested whether monthly or 3-month one-to-one follow up with intervention clinicians influenced patient performance, diabetes-related quality of life and diabetes-related health outcomes.28 The study found that the intervention was effective on a variety of diabetes outcome measures. However, men who received monthly follow-up versus 3-month follow-up had no significant differences in outcomes.28 More research should be conducted to determine which specific aspects of the CHW one-to-one sessions may have assisted participants in participating successfully in the intervention.
Limitations
This study has limitations. The small sample size of Latino and African American may have limited the ability to detect significant differences and to generalize those findings to other patient populations. Further studies with larger sample sizes are needed to examine the influence of gender and race/ethnic group interactions on participation in interventions for diabetes and other chronic disease management interventions is recommended. Despite these limitations, this is the first study to examine participation in several components of a CHW-led diabetes lifestyle intervention by Latino and African American men compared to women.
In summary, this study provides unique insights on the influence of gender on participation in a community-based CHW-led intervention in two racial/ethnic minority groups. Interventions may need to vary their approach to men, generally, and for African American and Latino men, specifically. Use of male CHWs who are matched by race/ethnicity and the use of flexibility and individualized services may be important features of community-based diabetes interventions. Future studies should tailor interventions by gender and examine their effects on decreasing disparities in participation and diabetes outcomes among both men and women of color.
Acknowledgements
This research was supported by the National Institute of Diabetes and Digestive and Kidney Disease (NIDDK, R18DK0785501A1), Centers for Disease Control and Prevention Cooperative Agreement No. U50/CCU417409, the Michigan Diabetes Research and Training Center Behavioral, Clinical and Health Systems Core (NIH Grant 5P60-DK20572), and the Robert Wood Johnson Foundation Clinical Scholars Program. We thank the CHASS/REACH Detroit Partnership staff, the REACH Detroit Partnership Steering Committee (www.reachdetroit.org), and the REACH Detroit Family Intervention participants for their involvement in this study. The REACH Detroit Partnership is affiliated with the Detroit Community-Academic Urban Research Center (www.sph.umich.edu/URC/).
Contributor Information
Jaclynn Hawkins, University of Michigan School of Social Work; REACH Detroit Partnership, Detroit, Michigan.
Edith Kieffer, University of Michigan School of Social Work; REACH Detroit Partnership, Detroit, Michigan.
Brandy Sinco, University of Michigan School of Social Work; REACH Detroit Partnership, Detroit, Michigan.
Michael Spencer, University of Michigan School of Social Work; REACH Detroit Partnership, Detroit, Michigan.
Michael Anderson, REACH Detroit Partnership, Detroit, Michigan; Community Health and Social Services Center, Detroit.
Ann-Marie Rosland, REACH Detroit Partnership, Detroit, Michigan; University of Michigan Medical School Department of Internal Medicine; VA Ann Arbor Center for Clinical Management Research.
References
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Fact sheet: Number of Americans with diabetes continues to increase, 2008. [Accessed January 1 2011]; Available at http://www.cdc.gov/diabetes/statistics/prev/national/figraceethsex.htm.
- 3.Centers for Disease Control and Prevention. Fact sheet: Number of Americans with diabetes continues to increase, 2008. [Accessed January 1 2011]; Available at http://www.cdc.gov/diabetes/statistics/prev/national/fighispanicthsex.htm.
- 4.Mauldon M, Melkus GD, Cagganello M. Tornado control: A culturally appropriate diabetes education program for Spanish-speaking individuals with type 2 diabetes mellitus—Evaluation of a pilot project. Diabetes Educ. 2006;32(5):751–760. doi: 10.1177/0145721706291999. [DOI] [PubMed] [Google Scholar]
- 5.Samuel-Hodge CD, Keyserling SP, Johnston LF, Gizlice Z, Bandgdiwala SI. A randomized trial of a church-based diabetes self-management program for African Americans with type 2 diabetes. Diabetes Educ. 2009;35(3):439–453. doi: 10.1177/0145721709333270. [DOI] [PubMed] [Google Scholar]
- 6.Hill-Briggs F, Renosky R, Lazo M, et al. Development and pilot evaluation of literacy-evaluation of literacy-adapted diabetes and CVD education in urban, diabetic African Americans. J Gen Intern Med. 2008;23(9):1491–1504. doi: 10.1007/s11606-008-0679-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Botri JM, Davis-Smith YM, Seale JP, Shellenberger S, Okosun IS, Cornelius ME. Diabetes prevention in a faith-based setting: results of translational research. J Public Health Manag Pract. 2008;14(1):29–32. doi: 10.1097/01.PHH.0000303410.66485.91. [DOI] [PubMed] [Google Scholar]
- 8.Two Feathers. Kieffer EC, Palmisano G, et al. Racial and ethnic approaches to community health (reach) Detroit partnership: improving diabetes-related outcomes among African American and Latino adults. Am J Public Health. 2005;95(9):1552–1560. doi: 10.2105/AJPH.2005.066134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Two Feathers J. Kieffer EC, Palmisano G, et al. The development, implementation, and process evaluation of the reach Detroit partnership’s diabetes lifestyle intervention. Diabetes Educ. 2007;33:509–520. doi: 10.1177/0145721707301371. [DOI] [PubMed] [Google Scholar]
- 10.Spencer MS, Rosland AM, Kieffer EC, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health. 2011;101(12):2253–2260. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McDonough P, Walters V. Gender Differences in Health: Reassessing Patterns and Explanations. Soc Sci Med. 2001;52:547–559. doi: 10.1016/s0277-9536(00)00159-3. [DOI] [PubMed] [Google Scholar]
- 12.Courtaney WH. Key determinants of the health and well-being of men and boys. Int J Mens Health. 2003;2(1):1–30. (2003). [Google Scholar]
- 13.O’Brien R, Hunt K, Hart G. ‘It's caveman stuff, but that is to a certain extent how guys still operate’: Men's accounts of masculinity and help-seeking. Soc Sci Med. 2005;61(3):503–516. doi: 10.1016/j.socscimed.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 14.Pinkhasov RM, Wong J, Kashanian M, et al. Are men shortchanged on health? Perspective on health care utilization and health risk behavior in men and women in the United States. Int J Clin Pract. 2010;64(4):475–487. doi: 10.1111/j.1742-1241.2009.02290.x. [DOI] [PubMed] [Google Scholar]
- 15.Jani JS, Ortiz L, Aranda MP. Latino outcome studies in social work: a review of the literature. Res Soc Work Pract. 2009;19(2):179–194. [Google Scholar]
- 16.Spencer MS, Gunter KE, Palmisano G. Community health workers and their value to social work. Social Work. 2010;55(2):169–180. doi: 10.1093/sw/55.2.169. [DOI] [PubMed] [Google Scholar]
- 17.Courtaney WH. Key determinants of the health and well-being of men and boys. Int J Mens Health. 2003;2(1):1–30. (2003). [Google Scholar]
- 18.Clark L, Vincent D, Zimmer L, Sanchez J. Cultural values and political economic contexts of diabetes among low-income Mexican americans. J of Transcult Nur. 2009;20(4):382–394. doi: 10.1177/1043659609334851. (2009). [DOI] [PubMed] [Google Scholar]
- 19.Early KB, Shultz JA, Corbett C. Assessing diabetes goals and self-management based on in-depth interviews with Latino and Caucasian clients with type 2 diabetes. J Transcult Nur. 2009;20(4):371–381. doi: 10.1177/1043659609334928. [DOI] [PubMed] [Google Scholar]
- 20.Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 21.Cheatham CT, Barksdale DJ, Rodgers SG. Barriers to health care and health-seeking behaviors faced by Black men. J Am Acad Nurse Pract. 2008 Nov;20(11):555–562. doi: 10.1111/j.1745-7599.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- 22.Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, Schwartz CE. Assessment of diabetes-related distress. Diabetes Care. 1995;18:754–60. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]; Agresti A. Categorical Data Analysis. 2nd ed. New Jersey: John Wiley & Sons, Inc; 2003. [Google Scholar]
- 23.Burnham KP, Anderson DR. Model Selection and Inference: A Practical Information-Theoretic Approach. New York: Springer-Verlag; 1998. [Google Scholar]
- 24.Agresti A. Categorical Data Analysis. Hoboken, NJ: John Wiley & Sons; 2002. pp. 240–244. [Google Scholar]
- 25.SAS Institute. SAS(R): Statistical Analysis Software, Release 9.3. Cary, NC: SAS Institute; 2011. [Computer Software]. [Google Scholar]
- 26.Andrews JO, Felton G, Wewers ME, Heath J. Use of community health workers in research with ethnic minority women. J Nurs Scholarship. 2004;36:358–365. doi: 10.1111/j.1547-5069.2004.04064.x. [DOI] [PubMed] [Google Scholar]
- 27.Cherrington A, Ayala GX, Amick H, et al. Implementing the community health worker model within diabetes management: Lessons learned from across the United States. Diabetes Educ. 2008;34(5):824–833. doi: 10.1177/0145721708323643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Devlin H, Roberts M, Okaya A, Xiong YM. Our lives were healthier before: Focus groups with African American, American Indian, Hispanic/Latino, and Hmong people with diabetes. Health Promot Proct. 2006;7:47–55. doi: 10.1177/1524839905275395. [DOI] [PubMed] [Google Scholar]


