Abstract
Outpatient opioid addiction treatment with sublingual buprenorphine pharmacotherapy (OBOT) has rapidly expanded in the United States and abroad, and, with this increase in medication availability, there have been increasing concerns about its diversion, misuse and related harms. This narrative review defines the behaviors of diversion and misuse, examines how the pharmacology of buprenorphine alone and in combination with naloxone influence its abuse liability, and describes the epidemiological data on buprenorphine diversion and intravenous misuse, risk factors for its intravenous misuse and the unintended consequences of misuse and diversion. Physician practices to prevent, screen for, and therapeutically respond to these behaviors, which are a form of medication non-adherence, are discussed and gaps in knowledge are identified. OBOT experiences from other countries that have varied health care systems, public policies, and access to addiction treatment are shared in order to make clear that diversion and misuse occur across the world in various contexts, for many different reasons, and are not limited to buprenorphine. Comparisons are made with other opioids with known abuse liability as well as medications with no known abuse. The objective is to facilitate understanding of diversion and misuse so that all factors influencing their expression (patient and provider characteristics and public policy) can be appreciated within a framework that also recognizes the benefits of addiction treatment. With this comprehensive perspective, further careful work can help determine how to minimize these behaviors without eroding the current benefits realized through improved addiction treatment access and expansion.
Keywords: buprenorphine, misuse, diversion, treatment, epidemiology, behavioral pharmacology
Introduction
Outpatient opioid addiction treatment with sublingual buprenorphine formulations (OBOT) has expanded rapidly over the last two decades in many areas of the world. Notably, before its use in addiction treatment, sublingual (e.g., Temgesic®) and injectable buprenorphine (e.g., Buprenex®) formulations were approved for pain treatment, and multiple countries reported problems with their misuse and diversion (Morrison, 1989; Singh, Mattoo, Malhotra, & Varma, 1992). OBOT became available in the United States (U.S.) later, after the passage of the Drug Abuse Treatment Act of 2000; this law allowed schedule IIIV opioids approved by the Food and Drug Administration (FDA) for the treatment of opioid dependence to be prescribed by medical practitioners outside of the confines of federally licensed methadone treatment centers for the first time since the passage of the Harrison Narcotic Act in 1914. Subsequently, the FDA approved both buprenorphine (BUP) and buprenorphine/naloxone combination (BUP/NX) sublingual tablet formulations. However, many European countries, Australia, and some Asian countries had introduced BUP earlier (throughout the 1990's) and BUP/NX followed in some countries (e.g., in 2006 BUP/NX was approved for use in the European Union). Generic tablet formulations have now also entered various markets, and a BUP/NX film product is now available in the U.S. and Australia.
With the growth of OBOT treatment and resulting increased availability of buprenorphine, concerns related to buprenorphine misuse and diversion have arisen (Center for Substance Abuse Research 2011; Johanson et al., 2012), the extent of which has varied widely across countries. This paper will review available published evidence regarding what is known about buprenorphine product misuse, diversion, and the unintended consequences of these behaviors for patients, providers and societies. These behaviors are influenced by an array of variables, including the pharmacological properties of the different medication formulations, patient and health care provider attitudes and behaviors, treatment structures, social and cultural expectations and public policy. It will describe mitigation strategies that can deter misuse and diversion. Understanding the broader international experience, where both access to treatment and the structure of OBOT services differ considerably, along with the current situation in the U.S. may inform strategies for responding to diversion and misuse in the U.S.
Definitions
For the purpose of this review and associated case conference, BUP specifically refers to the monotherapy sublingual tablet, BUP/NX to the combination tablet or film (buprenorphine with naloxone), and buprenorphine refers to both BUP and BUP/NX. Diversion is defined as the unauthorized rerouting or misappropriation of prescription medication to someone other than for whom it was intended. Diversion can occur either voluntarily or involuntarily and either with or without the exchange of money or other services (Larance et al., 2011b). Misuse includes taking medication in a manner, by route or by dose, other than prescribed. For instance, injecting, snorting or smoking medication intended for oral use or double or tripling doses are both examples of misuse. Notably, these definitions do not discuss underlying motives, relatedness to addiction, treatment structure or access, or appropriate clinical responses.
Buprenorphine Formulations and Their Pharmacology
The primary pharmacological activity of buprenorphine in the treatment of opioid dependence arises from its partial agonist activity at the mu opioid receptor; however, it is also an antagonist at the kappa opioid receptor and a partial agonist at the nociceptin or NOP recep (Bloms-Funke et al., 2000; Cowan and Lewis, 1995). As a mu opioid partial agonist, buprenorphine does not exert the same degree of intrinsic activity as a full mu opioid agonist, such as methadone, heroin or oxycodone. This limit on effects at the upper end of the dose response curve is the mechanism underlying the superior safety profile of buprenorphine compared to full mu opioid agonists with respect to respiratory depression and fatal overdose. This partial agonist profile has led some to suggest that buprenorphine would have reduced abuse liability compared to full mu agonists, but it must be recognized that buprenorphine can produce acute effects equivalent to a 60-mg dose of methadone (Walsh et al., 1994) and, thus, in individuals without physical dependence, buprenorphine is appealing for misuse and diversion. However, buprenorphine can also lead to precipitated withdrawal in opioid-dependent individuals because its high affinity/high mu opioid receptor occupancy, coupled with its partial agonist effects, allows it to displace other opioids occupying the receptor, while exerting insufficient activity to replace the displaced opioid's full agonist action (e.g., Walsh et al., 1995). This may occur under some dosing conditions but not others (e.g., Rosado et al., 2007; Strain et al., 1992) and appears to be dependent upon the maintenance opioid, the degree of physical dependence (i.e., maintenance dose), the time since last dose and the dose of buprenorphine. Precipitated withdrawal from buprenorphine can also be largely avoided by dosing only after a patient is experiencing some withdrawal (i.e., when some portion of receptors are already unoccupied and agonist effects are not present).
BUP/NX was developed as an abuse-deterrent formulation. Inclusion of naloxone (which typically has very low or no sublingual bioavailability and, thus, is essentially inert when taken by the proper route) would lead to precipitated withdrawal in an opioid dependent individual when the medication is misused by injection [and naloxone is bioavailable] (Mendelson et al., 1999; Stoller et al., 2001). Moreover, recent data have reported that intranasal administration of the BUP/NX tablets after crushing also delivers clinically relevant concentrations of naloxone (Middleton et al., 2011) that could, under some conditions, lead to precipitated withdrawal. However, more generally, the effects of naloxone are short-lived due its short half-life (~ 60 min), and the naloxone/buprenorphine dose ratio of (1:4) is not high enough to fully block the agonist effects of buprenorphine. Numerous case reports and studies have demonstrated that there are strategies (e.g., administering very small divided doses of BUP/NX), which can be employed to circumvent the precipitation of withdrawal after injection of BUP/NX by opioid dependent individuals (e.g., Larance et al., 2011a; Rosado et al., 2007). Thus, the abuse-deterrent feature of naloxone in the combination product is only relevant (and a deterrent) under a subset of conditions. While the combination formulation is the recommended formulation for providers to prescribe, research volunteers in laboratory and epidemiological studies have generally reported that when both BUP and BUP/NX are available, they prefer BUP over BUP/NX, and when full mu-opioid agonists are available, the full agonists are preferred over both buprenorphine formulations (Alho et al., 2007; Comer et al., 2010; Degenhardt et al., 2009; Strain et al., 2000; Vicknasingam et al., 2010).
Epidemiology of Buprenorphine Diversion and Misuse
Buprenorphine Diversion
Numerous factors contribute to whether a particular drug is diverted for illicit use by individuals without a legitimate prescription, including, for example, drug availability, price, pharmacologic properties, psychosocial and environmental factors (e.g., established distribution systems and social networks) and, in the case of opioids, the degree to which dosing is supervised and the extent to which treatment demand is met (e.g., see review by Bell, 2010). However, it is important to recognize that drug diversion (including sharing or selling a prescribed drug) may be a relatively common behavior; one that is not limited to those with drug dependence disorders. For example, data from the U.S. National Household Survey on Drug Use and Health reported that nearly 17 million persons used a prescription psychotherapeutic drug that had not been prescribed to them in the past year (SAMHSA, 2013). In a smaller national survey, 23% of those queried admitted that they shared their prescription drugs with others, while 27% of the sample reported that they had borrowed prescription medication from another person (Goldsworthy et al., 2008). The most commonly shared drug classes were allergy medications (25%), pain relievers (22%) and antibiotics (21%). Similar to these community dwelling sample surveys (i.e., having a substance use disorder was not required for inclusion), surveys of patients enrolled in outpatient opioid agonist programs (methadone or buprenorphine) across distinct geographical regions with widely varying treatment structures report that 18-28% have sold, given away their medication, removed it while under supervision, or shared other prescribed medication [Germany 23% (Stover, 2011); Australia 28% (Larance et al., 2011a); U.S., 18% (Caviness et al., 2013)]. Thus, sharing and receiving prescribed medications (i.e., diversion) is not unique to those with drug dependence disorders and a variety of medication, not only those with abuse liability, is diverted.
With regard to availability, the rapid growth and penetration of buprenorphine in the addiction medicine marketplace has increased its availability considerably over a relatively short time period. In the U.S., for example, the Automation of Reports and Consolidated Orders System (ARCOS), which monitors the flow of specific controlled substances from manufacture to distribution at the retail level, reports that over 190 million dosage units of buprenorphine were distributed to pharmacies in 2010, which is over four-fold higher than the almost 40 million dosage units distributed just four years prior in 2006 (DHHS, 2012). Notably, only 1.1 million dosage units were distributed to licensed opioid treatment programs during 2010. Almost 800,000 individuals received prescriptions for buprenorphine from physicians with a waiver (also known as an X-license because of the marking on the DEA prescriber's license) to provide OBOT under DATA 2000 in 2010, representing a nearly five-fold increase from the 150,000 individuals estimated in 2006 (DHHS, 2012). Thus, the opportunity to misuse and divert buprenorphine has grown rapidly during this great expansion of OBOT.
There are limited data available that address the specific source of diverted buprenorphine. Larance and colleagues reported on a cohort of out-of-treatment intravenous drug users (IVDU) in Australia who had received diverted buprenorphine. The majority reported receiving it from friends (81% BUP and 63% BUP/NX), while acquaintances (19% BUP and 25% BUP/NX) and dealers (19%) were reported less frequently. In this cohort, half of those receiving diverted BUP believed that it was someone's take-home dose and the majority (71%) had paid for the drug. Interestingly, for BUP/NX, 70% believed that the dose they received was a take-home dose but fewer than half paid for it and 48% stated that they had received the drug for free. Additionally, while 12% and 9% of all BPN and BUP/NX doses dispensed, respectively, were reported as being secretly removed from the mouth during supervised dosing for later use, only a small percentage of these (9% and 13%) were removed for the purpose of selling the drug (Larance et al., 2011a).
Intravenous Misuse By Patients and Out-of-Treatment Opioid Users
Intravenous misuse will be reviewed primarily because of the significant risks associated with IVDU, including spread of infectious diseases (e.g., hepatitis C, HIV), other medical complications (e.g., abscess, endocarditis), and overdose. Intravenous injection of BUP and BUP/NX has been reported around the world by individuals both in and out of treatment. In a survey of individuals presenting for prescription opioid abuse treatment in the U.S. between 2005-2007(n=1000), 6% of participants reported injecting buprenorphine “to get high”, while 37% of participants reported injection of other prescription opioids (e.g., oxycodone) for this reason (Cicero et al., 2007). While that study did not distinguish between BUP and BUP/NX, another surveillance system, RADARS® (Researched Abuse Diversion Addiction Related Surveillance) reported past month prevalence in the U.S. of IV BUP and BUP/NX misuse of 45.5% and 16.3%, respectively, by individuals presenting for opioid abuse treatment (Dart, 2011). Lower prevalence of injection of BUP/NX compared to BUP has also been reported in other countries. In Australia, liquid methadone, BUP, and BUP/NX are all available treatments, and all require a period of initial supervised dosing. Among patients receiving any of these medications as part of OBOT, weekly medication injection was significantly lower for BUP/NX (7%) compared to BUP (13%), but similar to liquid methadone (8%) (Degenhardt et al., 2009).
More recent data from France, where generic formulations have been available since 2006, reported significant differences in prevalence of injection of generic (5% of n=537) versus brand name BUP (10% of n=1159) among surveyed patients who were receiving OBOT through specialty addiction treatment clinics (i.e., not by general practitioners) (Nordmann et al., 2012). The reason for these differences was not evident, but the authors speculated that market penetration, patient preferences, familiarity with brand name, flavorings or other excipients, or even subtle differences in bioavailability could be contributing factors. Only one study to date has compared prevalence of frequent injection (at least weekly) of BUP/NX film to BUP/NX tablets (Larance et al., 2014). This Australian study was conducted in 2012 employing two distinct samples: 1) outof-treatment injection drug users (n=541) and 2) patients in opioid addiction treatment with either buprenorphine or methadone pharmacotherapy (n=544). It showed no significant differences in either sample in the prevalence of frequent injection of BUP/NX films (out-of-treatment: 1%; patients: 3%) compared to BUP/NX tablets (out-of-treatment: 3%; patients: 9%). These percentages were similar to the prevalence of frequent methadone injection (4% among out-of-treatment persons; 3% among patients). Frequent injection of BUP was higher (out-of-treatment: 6%; 11% among patients) than for both BUP/NX formulations.
Reports of buprenorphine injection rates surpassing heroin, methadone or other full mu-opioid agonist analgesics are rare across the world. In the U.S., where there is ready availability of full agonist mu-opioid analgesics (i.e., those formulated for treatment of pain) and heroin, buprenorphine was infrequently described as the primary drug of abuse among individuals seeking prescription drug abuse treatment (<3%) (Cicero et al., 2007). However, this has not been the case in all countries, such as Finland and Malaysia, where far greater problems of regular buprenorphine injection emerged due to unique circumstances in both countries.
Finland developed significant problems with increasing numbers of daily intravenous buprenorphine users in the late 1990's when heroin availability was declining due to decreased supply from Afghanistan (NBI, 2003; Uosukainen et al., 2013c). Finnish authorities reported that the primary source of misused BUP was from outside its borders (Forsell et al., 2010). By 2001, BUP replaced heroin as the most commonly abused opioid among persons seeking addiction treatment (Uosukainen et al., 2013c). Averaged over the 11-year period from 1998-2008, 16% of those surveyed who were seeking any type of substance abuse treatment identified buprenorphine as their primary drug of abuse; 80% were using it intravenously and most also were misusing other prescription-type medications (Uosukainen et al., 2013c). Treatment for people who were abusing buprenorphine was primarily with lofexidine and withdrawal protocols, and mortality rates were high, similar to those with primary abuse of heroin (Uosukainen et al., 2013b). Because of the emergence of widespread IV BUP abuse, BUP was restricted for treatment during pregnancy only, and BUP/NX, introduced in 2006, became the more commonly prescribed formulation. Notably, BUP and BUP/NX treatment have stringent criteria for treatment entry that begins in specialty addiction treatment clinics where dosing is observed (Forsell et al., 2010; Uosukainen et al., 2013a).
To evaluate the impact of the introduction of BUP/NX in Finland on prevalence of injection of BUP, a survey queried out-of-treatment needle exchange participants in 2005 (n=176) and in 2010 (n=276) (Simojoki and Alho, 2013). Daily injection BUP misuse decreased from 81.7% in 2005 to 74.3% in 2010; however, BUP remained the most commonly abused drug by the intravenous route. Daily injection use of BUP/NX was reported to be 14.7% in 2010, over 5-fold lower than daily injection of BUP among these needle exchange participants. The majority (64%) of this sample in 2010 endorsed their desire to enter opioid maintenance treatment. Unfortunately, approximately 50% reported not being accepted for treatment. The study authors concluded, in part, that there was a need for more opioid maintenance treatment options in Finland.
In Malaysia, injection of BUP emerged shortly after its introduction in 2002 during a rapid OBOT expansion provided primarily by general practitioners who received no training or practice guidelines for OBOT (Vicknasingam et al., 2010). Moreover, providers received additional income if they dispensed the medication (rather than prescribed) and received higher payment for more medication dispensed. Reports of frequent prescribing and dispensing of weekly-to-monthly take-home supplies of medication ensued. In 2006, one survey reported that among 276 persons recruited with past weekly IV BUP use, 63% were injecting BUP daily, which was most commonly (i.e., 76% of reports) received from a private general practice clinic (Vicknasingam et al., 2010). BUP was removed from the Malaysian market in 2006 and replaced with BUP/NX in 2007. A mandatory 8-hour training was introduced and a national registry of patients receiving BUP/NX was created. Shortly after BUP/NX became available in 2007, a survey recruited 204 persons with lifetime BUP/NX IV use. Within this sample, 34% were injecting BUP/NX daily. The top reasons for injecting BUP/NX included: to treat addiction (81%); alleviate withdrawal (70%); less expensive than heroin (57%); and for pleasure (36%). The most common source again was private practice general practitioners (77%). The study authors recommended reducing the financial incentives to physicians for dispensing large quantities of BUP/NX (Vicknasingam et al., 2010).
Risk Factors for Intravenous Buprenorphine Misuse
The studies above show that intravenous use of BUP is more frequent than BUP/NX, and IV buprenorphine use can occur in any country - a reminder that no particular type of health care system or addiction treatment system is immune. The Finnish experience demonstrates that medications, just like illicit substances (e.g., heroin), can become available even if the source is not from within one's own country and suggests that having inadequate access and/or stringently controlled access to opioid maintenance treatment is a potential risk factor for continued diversion and misuse of a therapeutic agent with opioid agonist properties. Attempting, but failing, to enter OBOT also has been prospectively identified as a risk factor for use of diverted buprenorphine (route not evaluated) in the United States, specifically Appalachia, Kentucky (Lofwall and Havens, 2012), and many barriers to accessing OBOT have been recently documented by the American Society of Addiction Medicine across the U.S. (ASAM, 2013). The Malaysia experience, on the other hand, suggests that significant IV buprenorphine use can arise within the context of simply providing buprenorphine in substantial supply (i.e., 2 - 4 weeks) to persons with IV opioid addiction in a treatment setting with provider incentives misaligned with patient treatment needs (e.g., payment based upon amount of medication dispensed).
Multiple cross-sectional studies have surveyed BUP/NX injectors to explore the reasons underlying their injecting behavior. Reasons commonly (e.g., >75%) include self-treatment of withdrawal or addiction, but other reasons are offered, including use for euphoric/pleasurable effects (Alho et al., 2007; Bazazi et al., 2011; Moratti et al., 2010; Vicknasingam et al., 2010); notably, these are not mutually exclusive. Much attention has been given to misuse for reasons that mimic the medical reasons for which the medication is prescribed. These latter reasons should not be used to legitimize IV misuse of diverted medication because many persons addicted to illicit substances (e.g., heroin) will similarly report use of heroin to prevent or treat their withdrawal/to feel “normal,” and there is clear morbidity and mortality associated with IVDU. There are no data showing that IV self-medication with buprenorphine is effective treatment. Rather, the high percentages of use of diverted medication for “self-treatment” may be a sentinel public health signal that treatment needs are not being met and that improved access to and/or expansion of treatment are essential.
The evidence base evaluating risk factors for intravenous use of buprenorphine among persons currently receiving buprenorphine treatment is scant with very few prospective studies. One cross-sectional study in France conducted 404 face-to-face confidential interviews with patients receiving treatment with BUP; only those who used BUP for the first time by physician prescription were eligible (Vidal-Trecan et al., 2003). Multivariable logistic regression demonstrated that having a history of IVDU was the most robust risk factor [Odds ratio (OR): 13.2], followed by current cannabis use (OR: 3.4) and having no salary (OR: 1.6). Ongoing heroin use during OBOT was protective (OR: 0.2), likely because injecting buprenorphine may precipitate withdrawal in regular heroin users, but more importantly, this result suggests that the patient could be trading or selling their medication in exchange for their primary opiate of choice, heroin. Another study from France prospectively evaluated patients in BUP treatment by telephone. The first phone survey was conducted after a minimum of three months in OBOT, and the second was conducted six months later (Roux et al., 2008). The response rate was 70% (n=111). Multivariate analysis adjusting for the time since first drug injection (a proxy of drug addiction severity) showed three significant risk factors for IV BUP use over the 6-month period: 1) perception of BUP dose as inadequate (OR: 2.7; median dose was 6 mg); 2) history of suicidal attempt or ideation (OR: 2.6); and 3) the number of years of IVDU (OR: 1.05). Injecting is a behavior that is highly conditioned; it is not surprising that such a behavior chronically repeated over time would continue for some time after treatment entry. However, it is not yet known what interventions may best extinguish injection behavior. This study also highlighted the role of appropriate dosing and comorbid conditions on IV risk and will be discussed in more detail in the recommended practices section.
Consequences of Buprenorphine Misuse and Diversion
Injection of any drug can cause a host of medical problems from local tissue site injury (e.g., tissue necrosis, abscess) to systemic infections such as endocarditis; these are also consequences that have been reported with buprenorphine injection (Gouny et al., 1999; Ho et al., 2009). Additionally, injection of pharmaceuticals intended for oral consumption may contain talc and other excipients that, when injected, can cause additional systemic complications, such as pulmonary granulomas (Waller et al., 1980). Reports of uncommon infections such as ocular candidiasis have occurred after removal of buprenorphine from the mouth (while under “supervision”) for later injection (Aboltins et al., 2005) and after injecting BUP that has been combined with contaminated solutions (Cassoux et al., 2002). There also have been case reports of severe liver pathology after parenteral use, sometimes involving other hepatotoxins and/or co-infection with hepatitis B and/or C (Berson et al., 2001; Herve et al., 2004).
The most worrisome patient and public health outcome to be associated with any medication is death. Deaths involving buprenorphine have been well described from France where BUP treatment rapidly grew from 1,000 patients in 1994 to 55,000 patients in 1998 (Auriacombe et al., 2001). OBOT is provided there primarily by general practitioners (Auriacombe et al., 2004) who can prescribe BUP to an unlimited number of patients and without any required training. A maximum of seven days of take-home doses is now recommended (Auriacombe et al., 2004), and while supervised dosing, urine drug testing and counseling are not required, French pharmacies can and do provide daily supervised dosing if the physician requests this service (Vignau et al., 2001). Surprisingly, buprenorphine maintenance doses were frequently co-prescribed (43%) with benzodiazepines (Thirion et al., 2002). Reports of deaths involving BUP followed; decedents frequently had positive toxicology tests for benzodiazepines and signs of injection drug use, suggesting that the concomitant use of benzodiazepines as well as parenteral administration were risk factors for death (Reynaud et al., 1998; Tracqui et al., 1998). Other countries have also reported buprenorphine-related deaths, most often in the context of concomitant use of benzodiazepines and/or alcohol highlighting the fact that combined use with non-benzodiazepine CNS depressants is also a risk factor for fatal overdose (Hakkinen et al., 2012; Selden et al., 2012). Death rates attributable to BUP were 3-fold less compared to methadone-related deaths in France over 1994-1998 when adjusted for the number of patients receiving each pharmacotherapy (Auriacombe et al., 2001). Importantly, the number of drug overdose deaths decreased by 79% in France from 1995 through 1999 while addiction treatment with BUP and methadone increased by over 95% and syringe exchange programs were developed (Auriacombe et al., 2004).
In the U.S., there are currently approximately 23,000 physicians with a waiver to provide OBOT (28% of those have a 100-patient limit; the remainder have a 30-patient limit; Drug Enforcement Agency National Technical Information Service, 2013). The number of deaths involving sublingual buprenorphine products (including generics) that are specifically approved by the Food and Drug Administration for the indication of opioid dependence treatment from 2002 to October of 2013 totaled 464 [email communication with Reckitt Benckiser Pharmaceuticals (RBP)]. These deaths exclude those involving injectable buprenorphine [i.e., Buprenex®; n=5 and non-specified buprenorphine products (n=53)]. Of the 464 deaths, there were 29 perinatal/neonatal deaths (e.g., miscarriage, stillbirth) whereby the mother was taking buprenorphine during pregnancy (not known if the mother was receiving buprenorphine as part of addiction treatment), six infant deaths, and 3 non-infant pediatric deaths; 423 deaths (91%) involved BUP/NX and 41 (9%) involved BUP. These results should not be interpreted to indicate that BUP/NX is less safe than BUP because BUP/NX has been more widely prescribed than BUP, and, unfortunately, many of these deaths (n=238) were reported to RBP without an assessment of the causality/role of buprenorphine in the death. It also is not known what proportion involved the use of benzodiazepines or other CNS depressants. However, one way to attempt to control for availability in calculation of death rates of BUP/NX versus BUP is to calculate patient treatment years assuming an average dose of 16 mg/day per patient based on amount of product sold (from 2003 for Suboxone® and Subutex® tablets and from September 2010 for Suboxone® film to September 2013; data not available for the generic products). Calculations from RBP show that there have been 1,510,109 patient-treatment years (PTY) for Suboxone® (i.e., 981,056 PTY for Suboxone® tablets and 529,053 PTY for Suboxone® film) and 30,701 PTY for Subutex® tablets. Thus, exposure to Suboxone® products is 49-fold higher than to Subutex® tablets suggesting that the finding of 10-fold higher proportion of deaths involving BUP/NX than BUP is actually lower than expected, although this is not conclusive because the number of deaths included generic product while calculations of PTY excluded generics. It is critical to remember, too, that morbidity and mortality among untreated opioid dependent persons, including fetuses and neonates of pregnant women is higher than the general population without substance abuse (e.g., Alroomi 1988, Hulse 1998, Neumark 2000). For example, among pregnant opioid dependent women, other comorbid substance use, social situations (e.g., domestic violence, problems accessing prenatal care), and medical (e.g., infections) and psychiatric problems can all adversely impact fetal and neonatal outcomes (e.g., Jones and Kaltenbach 2013, Ludlow 2004). For instance, most pregnant opioid dependent women (~90%) smoke cigarettes (e.g., Tuten 2003, Quigley 2013), and cigarette smoking is an independent risk factor for spontaneous abortion, stillbirths and sudden infant death syndrome (Rogers 2008). Recommendations for improvement in substance-involved death data collection systems are listed in Table 3.
TABLE 3.
Ongoing clinical research needs
| Develop sensitive and specific clinical methods for detecting misuse and diversion while in treatment |
| Develop efficacious prevention techniques and therapeutic responses to diversion and misuse that do not adversely affect treatment access or erode treatment benefits |
| Evaluate impact of public policy, including insurer and provider incentives and/or punishments that may inadvertently promote misuse and diversion and prevent therapeutic responses (e.g., limitations on number of provider visits, US Drug Enforcement Agency regulations that do not allow for a OBOT provider to store a patient's prescription medication once dispensed to patient, even if for purpose of supervised dosing at OBOT clinic) |
| Quantify amount of off-label prescribing of buprenorphine for pain and its relationship to diversion and misuse |
| Determine impact of product packaging on diversion and misuse and pediatric exposures |
| Continue drug development and consider alternative pharmaceutical abuse deterrents (e.g., higher naloxone: buprenorphine ratios, alternative abuse deterrent formulations, depot formulations) |
| Improve fatal substance overdose data collection systems to |
| 1. ensure comprehensive assessment of all substances present at the time of death, including both controlled and un-controlled substances [commonly prescribed non-controlled substances may also contribute to fatal outcomes (e.g., anti-hypertensives, antipsychotics)], |
| 2. clarify whether involved substances were prescribed or not prescribed (indicating diversion) to decedents, and |
| 3. include whether there is evidence of new or chronic use of each substance. |
| This information could be used to learn how prescribing practices and patient use patterns of prescribed or diverted substances contribute to overdose mortality and aid in the development of targeted interventions. |
While the number of buprenorphine-related deaths are likely underestimated because coroners are/were not routinely testing for buprenorphine, the number of deaths involving full mu-agonist opioid analgesics is markedly higher. For instance, in the year 2008, the Centers for Disease Control and Prevention (CDC) reported 14,800 deaths due to prescription opioid analgesics, and there is no evidence that deaths involving this class of medication are declining.
There also have been increasing reports of pediatric exposures to buprenorphine (Boyer et al., 2010; Martin & Rocque, 2011; Pedapati & Bateman, 2011). The CDC (www.cdc.gov/mmwr/preview/mmwrhtml/mm6203a5.htm) reports that BUP/NX “caused 9.5% of emergency hospitalizations for drug ingestion by children less than 6 years, a greater proportion than any other single medication, even though in 2009 buprenorphine products amounted to only 2.2% of all retail opioid prescriptions and 0.16% of all retail prescriptions.” While the CDC did not differentiate between BUP/NX tablet and film exposures, a recent study reported significantly lower rates of unintentional exposures to BUP/NX film among children ages 28 days to 6 years old compared to BUP/NX tablet and BUP (Lavonas et al., 2013). It is important for all patients receiving buprenorphine to understand that ingestion of buprenorphine, even without other medications, can be deadly in children; the reported ceiling effects on respiratory depression in adults do not appear to apply to children (Kim et al.,, 2012). Unintentional exposures to children should be preventable. Physicians should discuss the necessity of safe storage with all patients because the source of medication ingested can be from family and friends, who may not have children themselves.
Overall, the safety profile of buprenorphine in the U.S. appears superior to that of methadone with 2- to 3-fold lower rates of drug diversion reports and poison center calls than methadone (Dasgupta et al., 2010). Also, similar to France, recent data reveal a significant relationship between a decline in heroin overdose deaths following the approval and implementation of buprenorphine into the treatment system in Baltimore City, an area of the U.S. with particularly high rates of heroin abuse and heroin-related deaths (Schwartz et al., 2013).
In addition, the finding that benzodiazepines are most commonly associated with deaths related to buprenorphine, similar to their presence also in heroin, methadone, and full mu-opioid agonist prescription analgesic-related deaths, demonstrates that the respiratory depressant effects of buprenorphine are increased in the presence of benzodiazepines and alcohol as supported by mechanistic preclinical studies (e.g., Gueye et al., 2002; Pirnay et al., 2008 and others). Thus, benzodiazepine availability (and co-prescribing), diversion and misuse warrant increased attention from the medical, scientific and public policy makers because this drug class is contributing to public health harms. During the introduction of buprenorphine in France, a significant problem with concomitant benzodiazepine abuse arose with flunitrazepam, specifically. In response, the French Drug Agency modified the regulation of flunitrazepam to limit its prescription and dispensing and its abuse decreased. However, this was followed by a rise in abuse of clonazepam until its regulatory control was tightened in 2010 limiting its prescription to a maximum of 4 weeks as a hypnotic agent and 12 weeks as an anxiolytic (Frauger et al., 2013).
Recommended Practice Behaviors to Deter Misuse and Diversion
There are several published practice guidelines and recommendations for OBOT in the U.S., yet most have a very limited or no discussion about how to evaluate diversion and misuse of buprenorphine clinically nor do they provide strategies for screening, monitoring, or responding to these behaviors specifically within the outpatient setting of OBOT [Fiellin et al., 2004; Kosten and Fiellin, 2004; Kraus et al., 2011, CSAT 2004, CSAT 2005; www.fsmb.org/pdf/2013_model_policy_treatment_opioid_addiction.pdf, and http://pcssmat.org/wp-site/wp-content/uploads/2014/02/PCSSMATGuidanceAdherence-diversion-bup.Martin.pdf). This may be due, in part, to a lack of controlled studies that examine interventions to screen, monitor and reduce medication misuse and diversion. Moreover, there may be concern that, if these behaviors are acknowledged as occurring within U.S. OBOT treatment, it will result in burdensome regulations, such as mandatory supervised dosing for all patients as increased regulation has been a common response to diversion historically (Bell, 2010; Jaffe and O'Keeffe, 2003), or more extreme measures such as revocation of DATA 2000 or the rescheduling of buprenorphine to Schedule II (which would functionally preclude its use in OBOT). The goal here is to remind practitioners why diversion and misuse are deserving of clinical attention and to provide clinical recommendations for detecting, evaluating and responding therapeutically to these behaviors in order to retain patients in treatment and assist them in making positive changes in their recovery. Most of the clinical practices described are informed by basic principles of behavior analysis, addiction medicine and addiction psychiatry.
From the earlier discussion, it is clear that medication misuse and diversion are common behaviors and, when they occur within treatment, they indicate medication non-adherence. Non-adherence decreases treatment effectiveness (for all medical disorders) and is associated with illicit opioid relapse within OBOT (Tkacz et al., 2012). If one is interested in decreasing relapse, one must become interested also in medication adherence. Thus, assessment for misuse and diversion is recommended at each clinical visit with placement of these behaviors on patients’ problem list so they can be addressed therapeutically, rather than punitively.
A punitive “no tolerance” approach with automatic discharge from treatment is highly unlikely to help patients because untreated opioid addiction is characterized by relapse [continued use of illicit (i.e., diverted) opioids is the norm] and increased morbidity and mortality (McLellan et al., 2000). Good treatment benefits both individual and public health even when patients are unable to achieve continuous drug abstinence and cessation from all criminal activity and IVDU (National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction, 1998; Carrieri et al., 2006). For example, a recent study compared three groups of injection drug users receiving needle-exchange services in Norway: 1) persons currently in addiction treatment with methadone or buprenorphine (n=341); 2) persons with no prior treatment with these medications (n=1063); and 3) persons who had prior, but not current, treatment with these medications (n=356). Those currently in treatment, despite continued IVDU, had significantly fewer non-fatal overdoses (O.R.=0.5), committed fewer thefts (O.R.=0.6) and reported dealing drugs (O.R.=0.7) less often in the prior month. They were also less likely to use heroin daily or near daily (O.R.=0.3) compared to the other groups that were not in treatment (Gjersing and Bretteville-Jensen, 2013). This does not imply that physicians must accept and do nothing about medication misuse and diversion or that they should continue to prescribe buprenorphine to patients who are distributing it to others rather than taking it themselves. Rather, the point is that treatment can be beneficial even if the ideal outcome is not attained (e.g., 100% medication adherence and abstinence from all substances of abuse). The goal is to evaluate treatment benefits and harms for each patient, individualizing the treatment plan in order to minimize harms without adversely affecting the benefits provided.
Reasons for buprenorphine diversion and misuse while in OBOT are listed in Table 1. Once providers understand the context and circumstances around these behaviors, practical solutions can be formulated. For instance, for a patient who encounters drug dealers every month at the pharmacy where they fill their prescription and are pressured to sell their medication, a recommendation to change pharmacies and assistance with finding financial help may be welcome if the medication is being sold to pay off old debts. For patients unable to escape from drug-addicted social networks, it may be helpful to discuss the option of maintaining a secretive status regarding having medication (Havnes et al., 2013).
TABLE 1.
Patient reasons for medication diversion and misuse while in OBOT
| Reasons for diversion | Reasons for misuse |
|---|---|
| Peer pressure (e.g., expectation that medication is shared, may be facilitated by excessively high daily doses and large supplies) | Habit (e.g., history of IV or intranasal drug use increases risk of injecting or snorting medication, respectively) |
| Help addicted friend or family member | Perceived under-dosing |
| Make money (e.g., pay off bad debt, pay for living expenses/medical fees, to buy preferred opioid for misuse) | Relieve opioid withdrawal, craving and/or treat addiction |
| Achieve positive effects (e.g., get high, increased energy) | |
| Relieve negative states (e.g., pain, anxiety, depression) |
Patients may not disclose medication misuse and diversion; however, some clinical practice behaviors (see Table 2), such as monitoring urine drug test outcomes, including for buprenorphine, are recommended and may be helpful. Inexpensive CLIA-waived urine tests for buprenorphine are now readily available in the U.S. In a cross-sectional study in India, 14% and 34% of patients receiving BUP/NX and BUP, respectively, tested negative for buprenorphine on random observed urine testing (Balhara and Jain, 2012). A test that is positive for buprenorphine but negative for its primary metabolite, norbuprenorphine, would also be incongruent with daily medication use. Admittedly, urine drug testing has limited practical use in detecting intermittent non-adherence due to the long half-life of buprenorphine, as patients could skip medication for several days and still produce a urine screen positive for buprenorphine. State prescription monitoring reports are useful in detecting multiple buprenorphine prescribers simultaneously (e.g., doctor shopping) as well as receipt of other controlled substances. Random medication counts can also be done at the physician office or at the pharmacy in order to screen for potential diversion and misuse (Lofwall et al., 2010), although there are no data on the sensitivity or specificity of this approach. It is noteworthy that each individually packaged BUP/NX film product in the U.S. contains a unique 10-digit ID number and QR code that could be scanned at any point in the chain of medication distribution. While this tracking technology is not being used currently, it has the potential to trace medication found on the street back to the dispensing pharmacy, physician prescriber and patient recipient. This could be helpful for providers and patients if used therapeutically in treatment, but could be harmful if it became a law enforcement tool used primarily to punish providers and patients.
TABLE 2.
Checklist to help detect diversion and misuse while in OBOT
| Practice behavior | Explanation/Examples |
|---|---|
| Talk | Define diversion and misuse with each patient, ask for patient to give examples of each from their experience with illicit drug use, discuss potential triggers for each patient, develop strategies to combat these behaviors, follow-up at each visit about occurrences or close-calls of medication diversion and misuse just as with use of illicit opioid of choice; discuss openly throughout treatment |
| Examine | Non-healing or fresh track marks or intranasal erythema may indicate buprenorphine injection or intranasal use, respectively, or that other substances are being misused whereby the medication could be sold/traded for the opioid of choice. Lack of objective signs of opioid withdrawal despite ongoing patient report of severe withdrawal. |
| Listen | Repeated requests for early refills due to various reasons [lost, stolen or washed (forgot to take out of clothing) medications] |
| Monitor | Missing appointments, incorrect medication tablet/film counts, urine tests with absence of buprenorphine and/or norbuprenorphine, unexpected medical problems for a patient believed to be in recovery (e.g., abscesses), state prescription monitoring reports showing ongoing receipt of prescription opioids or other controlled substances that the patient denied being prescribed and/or multiple prescriptions from different OBOT providers over the same time period |
| Collaborate | Feedback from pharmacist about unusual behavior from patient, such as appearing intoxicated or being accompanied by someone who appears to be overly interested in the medication, exchange of something in parking lot or in waiting area. Counselor and family members who are not currently addicted and who have patients’ best interest in mind report patient contact with old drug-using friends or non-adherence with medication if they are supervising ingestion. |
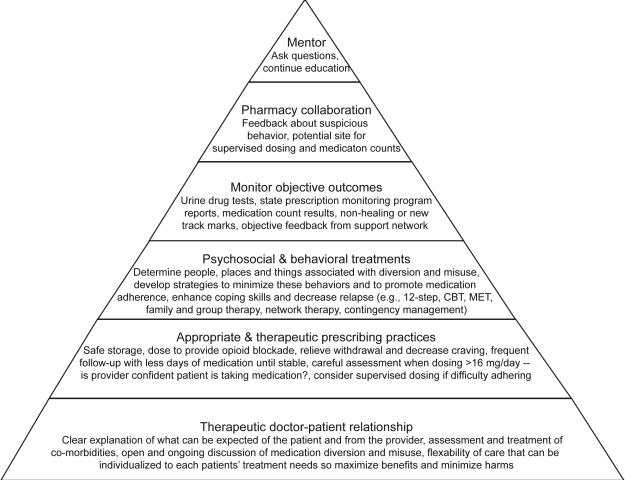
OBOT providers may want to consider how their practice, which should be comprised of numerous components (see Figure 1), can help minimize and respond to misuse and diversion when it occurs. To prevent attracting individuals who are seeking medication to sell on the street, the OBOT provider can make it clear at the time of scheduling the initial appointment that there are multiple aspects of treatment (e.g., assessment, monitoring), and frequent visits until stable. Providers may choose to explain that longer supplies of medication will be provided with increasing objective evidence of stability. This is a practical example of integrating contingency management into clinical practice. Contingency management is a highly effective behavioral therapy that uses positive reinforcers (e.g., longer duration of prescription or less frequent appointments) to encourage and promote desired behavioral changes, such as adherence and drug abstinence (Gerra et al., 2011; Stitzer and Vandrey, 2008). In order to avoid unintentional diversion (and pediatric exposures) from patients’ prescription buprenorphine at home, all OBOT patients could be advised on safe storage practices (e.g., in a lock box and not in kitchens and bathrooms or other common areas where it could be easily “borrowed” or stolen). Use of the combined BUP/NX versus BUP formulation should be preferred for non-pregnant patients given its relative lower abuse liability. However, clinicians may be presented with pleas by patients for prescription of BUP over BUP/NX if generic BUP is significantly less expensive than BUP/NX, particularly for patients without health insurance. Such cases require a careful individual assessment and documentation of the individual risks and benefits of prescribing the formulation without naloxone (e.g., is no treatment the alternative? is this a high risk patient for IV misuse due to history of IVDU?), including a plan for monitoring and switching to product with naloxone should concerns about diversion and misuse arise. Therapeutic dosing and prescribing are also important. The FDA package insert for BUP/NX states that the upper recommended dose is 24 mg/day. Dosing above 24 mg/day is off-label; physicians should document a rationale for surpassing this dosage including showing that lower daily doses were not adequate. There are no studies to date showing that doses higher than 24mg/day produce superior results compared to 24 mg/day. Most patients will stabilize on doses between 8-24 mg/daily. Dosing should be flexible and incremental according to published practice guidelines. Therapeutic dosing must take into account both the evidence base and the individual patient response to medication, in order for dosing and the overall treatment plan to be tailored to each individual patient. Providers should avoid 1) subtherapeutic dosing [e.g., inadequate opioid blockade (i.e., ability to still get high or have good effects from illicit opioid use while taking the prescribed buprenorphine dose) or inadequate withdrawal suppression], 2) supratherapeutic dosing (which may allow patient to maintain stability while sharing or selling a portion of their medication) and 3) providing large drug supplies to unstable patients (e.g., several weeks or more), which can increase risk and provide opportunity for diversion and misuse.
Figure 1.
Components of outpatient opioid dependence treatment. A detailed explanation of the practices detailed in this figure can be viewed on-line @ http://www.cecentral.com/buprecme (Lofwall et al., 2011).
When diversion and misuse are suspected or confirmed, potential responses include practical solutions individualized to the particular patient situation that were discussed earlier (if known), but also include more frequent clinic and/or counseling visits, smaller supplies of unsupervised medication (e.g., one week supply or less), and initiation of or increase in the frequency of supervised medication ingestion. Thrice-weekly dosing of buprenorphine under supervision is an effective treatment strategy that reduces clinic burden without compromising patient treatment outcomes compared to daily dosing under supervision (Amass et al, 2001; Bickel et al., 1999; Marsch et al., 2005). Observed ingestion at the OBOT clinic, pharmacy (more common outside of the U.S.) or by a trusted non-drug-using support that lives with or nearby the patient is another strategy to consider. For example, network therapy encourages patients to enlist non-drug-using supports in their treatment who can monitor medication ingestion. Network therapy has been shown to increase opioid abstinence significantly among heroin dependent adults in OBOT (50%) compared to standard medication management with counseling (23%) (Galanter et al., 2004). However, it is critical to avoid choosing support members with an abusive or exploitative relationship with the patient.
It is important to remember that supervised dosing does not eliminate diversion and misuse as highlighted earlier with the Australian experience. Liquid methadone and buprenorphine tablets can be held in cheeks and taken out of the mouth among patients motivated to misuse and divert if there is a brief lapse in supervision (e.g., supervisor turns around for a moment, lack of mouth check). A recent comparison between the BUP/NX tablet and film product suggests that supervision may be more effective with the film because it dissolves more quickly and is more mucoadhesive (i.e., stickier) than the tablet, making it difficult to remove from the mouth (Lintzeris et al., 2013). However, a recent study showed that under “supervision,” doses of medication for opioid addiction treatment were removed among patients dispensed BUP/NX tablet (19%) and BUP/NX film (20%) (Larance et al., 2014). It is not clear if patients were able to slip medication from hand to pocket due to medication not being placed directly into the patient's mouth, or if there were other strategies (e.g., dry mouth and overlapping films that may decrease effective mucoadhesion). Notably, in this study, among patients receiving supervised BUP/NX film dosing, 43% reported that more than three films were placed in their mouth at once suggesting that overlap of films may have played a role.
Daily supervised dosing as a regulatory requirement for all patients may pose a barrier to treatment entry for patients, limit further treatment expansion (e.g., increased costs and requirements for storing and dispensing controlled drug from a clinic), and exacerbate the problems of untreated addiction. It is possible, however, that supervised dosing may be helpful in circumstances where patients do not have safe storage options (e.g., homeless) or would benefit from the increased structure and clinic contact that supervised dosing can provide. While limited data exist on the frequency of supervised dosing and treatment outcomes, one randomized controlled study showed that thrice-weekly versus once-weekly supervised buprenorphine dosing in OBOT produced only modest decreases in patient treatment satisfaction and no differences in treatment retention, opioid use, or medication adherence (Barry et al., 2007; Fiellin et al., 2006). Some patients may require an alternative treatment setting or pharmacotherapy, such as methadone (Kakko et al., 2007). Improving linkages between practices and providers which vary in their intensity and setting are necessary for flexible and uninterrupted quality care.
Conclusions
Overall, buprenorphine diversion and misuse appear to be common behaviors of opioid addicted individuals, whereby the frequency of use of diverted medication, route of misuse, and subsequent harms are influenced by a variety of factors. These factors include the pharmacologic profile of the particular buprenorphine formulations, physical dependence status of the individual, individual experience with route of drug use, availability of buprenorphine or alternative opioids in the environment, and public policies within and surrounding geographic areas regarding opioid addiction treatment services. Table 3 suggests areas for future clinical research where current gaps in knowledge exist. Unfortunately, deaths involving buprenorphine have occurred around the globe, most commonly in combination with CNS depressants, and in the U.S., deaths involving buprenorphine are far fewer in number compared to deaths involving methadone and other full-mu opioid agonist prescription analgesics. Importantly, epidemiologic data from France and the U.S. showed that with OBOT expansion, there was an overall decrease in drug overdose deaths. Thus, any steps taken to minimize buprenorphine diversion and misuse must be careful not to undermine the positive patient and public health benefits gained from expanded treatment access.
Acknowledgements
The authors thank Vickie Seeger and Rolley E. Johnson PharmD from Reckitt Benckiser Pharmaceuticals for their sharing of U.S. death reports involving buprenorphine products and Dr. Kaarlo Simojoki for providing information about the opioid addiction treatment system and heroin supply in Finland.
Conflicts of interest and source of funding. The source of funding for this review is, in part, derived from NIDA grant R01DA016718 and R01DA033932 (SLW). Drs. Lofwall and Walsh are on the steering committee for the European Quality Patient Care Network that is part of PCM Scientific (a British educational company) and have received payment from PCM Scientific for developing educational materials and giving educational talks. In addition, Dr. Walsh has received payment for Chairing and organizing a three-day conference supported by PCM Scientific through an unrestricted grant from Reckitt Benckiser. Dr. Lofwall has been a consultant for Orexo Pharmaceuticals and has had research contract funding from CRS Associates in the past (contract funding goes to her institution). Dr. Walsh has received payment for service on a Safety Advisory Board for MEDA Pharmaceuticals and for service on the American Society of Addiction Medicine Board Exam Committee. She has served as a consultant for DemeRx, Eli Lilly and Co., KSI Consulting, MedSignals and Cephalon. She has received honoraria and travel reimbursement for participating in educational meetings for physicians through Real Science Communications and the University of Kentucky.
References
- Aboltins CA, Allen P, Daffy JR. Fungal endophthalmitis in intravenous drug users injecting buprenorphine contaminated with oral Candida species. Med J Aust. 2005;182:427. doi: 10.5694/j.1326-5377.2005.tb06764.x. [DOI] [PubMed] [Google Scholar]
- Amass L, Kamien JB, Mikulich SK. Thrice-weekly supervised dosing with the combination buprenorphine-naloxone tablet is preferred to daily supervised dosing by opioid-dependent humans. Drug Alcohol Depend. 2001;61:173–181. doi: 10.1016/s0376-8716(00)00141-1. [DOI] [PubMed] [Google Scholar]
- National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction Effective Medical Treatment of Opiate Addiction. JAMA. 1998;280:1936–1943. [PubMed] [Google Scholar]
- Alho H, Sinclair D, Vuori E, et al. Abuse liability of buprenorphine-naloxone tablets in untreated IV drug users. Drug Alcohol Depend. 2007;88:75–78. doi: 10.1016/j.drugalcdep.2006.09.012. [DOI] [PubMed] [Google Scholar]
- Alroomi LG, Davidson J, Evans TJ, et al. Maternal narcotic abuse and the newborn. Arch Dis Child. 1988;63:81–3. doi: 10.1136/adc.63.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Society of Addiction Medicine (ASAM) Advancing Access to Addiction Medications: Implications for Opioid Addiction Treatment. A Project of the ASAM. 2013 Available on-line http://www.asam.org/docs/advocacy/Implications-for-Opioid-Addiction-Treatment.
- Auriacombe M, Fatseas M, Dubernet J, et al. French field experience with buprenorphine. Am J Addict. 2004;13:S17–28. doi: 10.1080/10550490490440780. [DOI] [PubMed] [Google Scholar]
- Auriacombe M, Franques P, Tignol J. Deaths attributable to methadone vs buprenorphine in France. JAMA. 2001;285:45. doi: 10.1001/jama.285.1.45. [DOI] [PubMed] [Google Scholar]
- Balhara Y, Jain R. A Urinanalysis-based comparative study of treatment adherence on buprenorphine and buprenorphine/naloxone combination used as opioid substitution treatment. Innov Clin Neurosci. 2012;9:24–29. [PMC free article] [PubMed] [Google Scholar]
- Barry DT, Moore BA, Pantalon MV, et al. Patient satisfaction with primary care office-based buprenorphine/naloxone treatment. J Gen Intern Med. 2007;22:242–245. doi: 10.1007/s11606-006-0050-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazazi AR, Yokell M, Fu JJ, et al. Illicit use of buprenorphine/naloxone among injecting and noninjecting opioid users. J Addict Med. 2011;5:175–180. doi: 10.1097/ADM.0b013e3182034e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell J. The global diversion of pharmaceutical drugs: opiate treatment and the diversion of pharmaceutical opiates: a clinician's perspective. Addiction. 2010;105:1531–1537. doi: 10.1111/j.1360-0443.2010.03014.x. [DOI] [PubMed] [Google Scholar]
- Berson A, Gervais A, Cazals D, et al. Hepatitis after intravenous buprenorphine misuse in heroin addicts. J Hepatol. 2001;34:346–350. doi: 10.1016/s0168-8278(00)00049-0. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Amass L, Crean JP, Badger GJ. Buprenorphine dosing every 1, 2, or 3 days in opioid-dependent patients. Psychopharmacology (Berl) 1999;46:111–118. doi: 10.1007/s002130051096. [DOI] [PubMed] [Google Scholar]
- Bloms-Funke P, Gillen C, Schuettler AJ, et al. Agonistic effects of the opioid buprenorphine on the nociceptin/OFQ receptor. Peptides. 2000;21:1141–1146. doi: 10.1016/s0196-9781(00)00252-7. [DOI] [PubMed] [Google Scholar]
- Boyer EW, McCance-Katz EF, Marcus S. Methadone and buprenorphine toxicity in children. Am J Addict. 2010;19:89–95. doi: 10.1111/j.1521-0391.2009.00002.x. [DOI] [PubMed] [Google Scholar]
- Carrieri MP, Amass L, Lucas GM, et al. Buprenorphine use: the international experience. Clin Infect Dis. 2006;43:S197–215. doi: 10.1086/508184. [DOI] [PubMed] [Google Scholar]
- Cassoux N, Bodaghi B, Lehoang P, et al. Presumed ocular candidiasis in drug misusers after intravenous use of oral high dose buprenorphine (Subutex). Br J Ophthalmol. 2002;86:940–941. doi: 10.1136/bjo.86.8.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caviness CM, Anderson BJ, de Dios MA, et al. Prescription medication exchange patterns among methadone maintenance patients. Drug Alcohol Depend. 2013;127:232–238. doi: 10.1016/j.drugalcdep.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Substance Abuse Research (CESAR) Buprenorphine availability, diversion, misuse: A summary of the CESAR FAX Series. 2011;20(34) [Google Scholar]
- Center for Substance Abuse Treatment (CSAT) Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2004. Treatment Improvement Protocol (TIP) Series 40. DHHS Publication No. (SMA) 04-3939. [PubMed] [Google Scholar]
- CSAT . Medication-assisted treatment for opioid addiction in opioid treatment programs. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2005. Treatment Improvement Protocol (TIP) Series 43. DHHS Publication No. (SMA) 06-4214. [PubMed] [Google Scholar]
- Cicero TJ, Surratt HL, Inciardi J. Use and misuse of buprenorphine in the management of opioid addiction. J Opioid Manag. 2007;3:302–308. doi: 10.5055/jom.2007.0018. [DOI] [PubMed] [Google Scholar]
- Comer SD, Sullivan MA, Vosburg SK, et al. Abuse liability of intravenous buprenorphine/naloxone and buprenorphine alone in buprenorphine-maintained intravenous heroin abusers. Addiction. 2010;105:709–718. doi: 10.1111/j.1360-0443.2009.02843.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowan A, Lewis J. Buprenorphine: Combatting Drug Abuse with a Unique Opioid. Wiley Liss; New York: 1995. [Google Scholar]
- Dart RC. 5th Annual Scientifica Meeting Presentation. Evaluation of ADFs using RADARS system data. 2011 Slides available at http://www.radars.org/Home2/AnnualMeeting/RADARSSystem2011AnnualMeeting.aspx.
- Dasgupta N, Bailey EJ, Cicero T, et al. Post-marketing surveillance of methadone and buprenorphine in the United States. Pain Med. 2010;11:1078–1091. doi: 10.1111/j.1526-4637.2010.00877.x. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Larance BK, Bell JR, et al. Injection of medications used in opioid substitution treatment in Australia after the introduction of a mixed partial agonist-antagonist formulation. Med J Aust. 2009;191:161–165. doi: 10.5694/j.1326-5377.2009.tb02729.x. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services (DHHS) Department of Health and Human Services 42 CFR Part 8 RIN 0930 AA14. 2012 available @ http://www.gpo.gov/fdsys/pkg/FR-2012-12-06/html/2012-29417.htm.
- Fiellin DA, Kleber H, Trumble-Hejduk JG, et al. Consensus statement on office-based treatment of opioid dependence using buprenorphine. J Subst Abuse Treat. 2004;27:153–159. doi: 10.1016/j.jsat.2004.06.005. [DOI] [PubMed] [Google Scholar]
- Fiellin DA, Pantalon MV, Chawarski MC, et al. Counseling plus buprenorphine-naloxone maintenance therapy for opioid dependence. N Engl J Med. 2006;355:365–374. doi: 10.1056/NEJMoa055255. [DOI] [PubMed] [Google Scholar]
- Forsell M, Virtanen A, Jaaskelainen M, et al. Drug Situation in Finland 2010. National report to the EMCDDA by the Finnish National Focal Point. National Institue for Helath and Welfare (THL). Report 39/2010. Available on-line@ http://www.thl.fi/thl-client/pdfs/7445c896-5bc1-4bbc-b9e3-f41be4fa94e5.
- Frauger E, Moracchini C, Le Boisselier R, et al. OPPIDUM surveillance program: 20 years of information on drug abuse in France. Fundam Clin Pharmacol. 2013:1–11. doi: 10.1111/fcp.12024. [DOI] [PubMed] [Google Scholar]
- Galanter M, Dermatis H, Glickman L, et al. Network therapy: decreased secondary opioid use during buprenorphine maintenance. J Subst Abuse Treat. 2004;26:313–318. doi: 10.1016/j.jsat.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Gerra G, Saenz E, Busse A, et al. Supervised daily consumption, contingent take-home incentive and non-contingent take-home in methadone maintenance. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:483–489. doi: 10.1016/j.pnpbp.2010.12.002. [DOI] [PubMed] [Google Scholar]
- Gjersing L, Bretteville-Jensen AL. Is opioid substitution treatment beneficial if injecting behaviour continues? Drug Alcohol Depend. 2013;133:121–126. doi: 10.1016/j.drugalcdep.2013.05.022. [DOI] [PubMed] [Google Scholar]
- Goldsworthy RC, Schwartz NC, Mayhorn CB. Beyond abuse and exposure: framing the impact of prescription-medication sharing. Am J Public Health. 2008;98:1115–1121. doi: 10.2105/AJPH.2007.123257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gouny P, Gaitz JP, Vayssairat M. Acute hand ischemia secondary to intraarterial buprenorphine injection: treatment with iloprost and dextran-40--a case report. Angiology. 1999;50:605–606. doi: 10.1177/000331979905000711. [DOI] [PubMed] [Google Scholar]
- Gueye PN, Borron SW, Risede P, et al. Buprenorphine and midazolam act in combination to depress respiration in rats. Toxicol Sci. 2002;65:107–114. doi: 10.1093/toxsci/65.1.107. [DOI] [PubMed] [Google Scholar]
- Hakkinen M, Launiainen T, Vuori E, et al. Benzodiazepines and alcohol are associated with cases of fatal buprenorphine poisoning. Eur J Clin Pharmacol. 2012;68:301–309. doi: 10.1007/s00228-011-1122-4. [DOI] [PubMed] [Google Scholar]
- Havnes IA, Clausen T, Middelthon AL. ‘Diversion’ of methadone or buprenorphine: ‘harm’ versus ‘helping’. Harm Reduct J. 2013;10:24. doi: 10.1186/1477-7517-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herve S, Riachi G, Noblet C, et al. Acute hepatitis due to buprenorphine administration. Eur J Gastroenterol Hepatol. 2004;16:1033–1037. doi: 10.1097/00042737-200410000-00013. [DOI] [PubMed] [Google Scholar]
- Ho RC, Ho EC, Tan CH, et al. Pulmonary hypertension in first episode infective endocarditis among intravenous buprenorphine users: case report. Am J Drug Alcohol Abuse. 2009;35:199–202. doi: 10.1080/00952990902939719. [DOI] [PubMed] [Google Scholar]
- Hulse GK, Milne E, English, et al. Assessing the relationship between maternal opiate use and antepartum haemorrhage. Addiction. 1998;93:1553–8. doi: 10.1046/j.1360-0443.1998.9310155312.x. [DOI] [PubMed] [Google Scholar]
- Jaffe JH, O'Keeffe C. From morphine clinics to buprenorphine: regulating opioid agonist treatment of addiction in the United States. Drug Alcohol Depend. 2003;70:S3–11. doi: 10.1016/s0376-8716(03)00055-3. [DOI] [PubMed] [Google Scholar]
- Johanson CE, Arfken CL, di Menza S, et al. Diversion and abuse of buprenorphine: findings from national surveys of treatment patients and physicians. Drug Alcohol Depend. 2012;120:190–195. doi: 10.1016/j.drugalcdep.2011.07.019. [DOI] [PubMed] [Google Scholar]
- Jones HE, Kaltenbach K. Treating women with substance use disorders during pregnancy: a comprehensive approach to caring for mother and child. Oxford University Press; 2013. [Google Scholar]
- Kakko J, Gronbladh L, Svanborg KD, et al. A stepped care strategy using buprenorphine and methadone versus conventional methadone maintenance in heroin dependence: a randomized controlled trial. Am J Psychiatry. 2007;164:797–803. doi: 10.1176/ajp.2007.164.5.797. [DOI] [PubMed] [Google Scholar]
- Kim HK, Smiddy M, Hoffman RS, Nelson LS. Buprenorphine may not be as safe as you think: a pediatric fatality from unintentional exposure. Pediatrics. 2012;130(6):e1700–1703. doi: 10.1542/peds.2012-1342. [DOI] [PubMed] [Google Scholar]
- Kosten TR, Fiellin DA, et al. Buprenorphine for office-based practice: consensus conference overview. Am J Addict. 2004;13:S1–7. doi: 10.1080/10550490490440744. [DOI] [PubMed] [Google Scholar]
- Kraus ML, Alford DP, Kotz MM, et al. Statement of the American Society Of Addiction Medicine Consensus Panel on the use of buprenorphine in office-based treatment of opioid addiction. J Addict Med. 2011;5:254–263. doi: 10.1097/ADM.0b013e3182312983. [DOI] [PubMed] [Google Scholar]
- Larance B, Degenhardt L, Lintzeris N, et al. Post-marketing surveillance of buprenorphine-naloxone in Australia: diversion, injection and adherence with supervised dosing. Drug Alcohol Depend. 2011a;118:265–273. doi: 10.1016/j.drugalcdep.2011.04.002. [DOI] [PubMed] [Google Scholar]
- Larance B, Degenhardt L, Lintzeris N, et al. Definitions related to the use of pharmaceutical opioids: extramedical use, diversion, non-adherence and aberrant medication-related behaviours. Drug Alcohol Rev. 2011b;30:236–245. doi: 10.1111/j.1465-3362.2010.00283.x. [DOI] [PubMed] [Google Scholar]
- Larance B, Lintzeris N, Ali R, Dietze, et al. The diversion and injection of a buprenorphine-naloxone soluble film formulation. Drug Alcohol Depend. 2014;136:21–27. doi: 10.1016/j.drugalcdep.2013.12.005. [DOI] [PubMed] [Google Scholar]
- Lavonas EJ, Banner W, Bradt P, et al. Root causes, clinical effects, and outcomes of unintentional exposures to buprenorphine by young children. J Pediatr. 2013;163:1377–1383. e1371–1373. doi: 10.1016/j.jpeds.2013.06.058. [DOI] [PubMed] [Google Scholar]
- Lintzeris N, Leung SY, Dunlop AJ, et al. A randomised controlled trial of sublingual buprenorphine-naloxone film versus tablets in the management of opioid dependence. Drug Alcohol Depend. 2013;131:119–126. doi: 10.1016/j.drugalcdep.2012.12.009. [DOI] [PubMed] [Google Scholar]
- Lofwall MR, Havens JR. Inability to access buprenorphine treatment as a risk factor for using diverted buprenorphine. Drug Alcohol Depend. 2012;126:379–383. doi: 10.1016/j.drugalcdep.2012.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lofwall MR, Wunsch MJ, Nuzzo PA, Walsh SL. Efficacy of continuing medical education to reduce the risk of buprenorphine diversion. J Subst Abuse Treat. 2011;41:321–9. doi: 10.1016/j.jsat.2011.04.008. [DOI] [PubMed] [Google Scholar]
- Lofwall MR, Wunsch MJ, Walsh SL. Pharmacy willingness to partner with office-based opioid dependence treatment providers in conducting random buprenorphine pill counts. Am J Addict. 2010;19:195–196. doi: 10.1111/j.1521-0391.2009.00026.x. [DOI] [PubMed] [Google Scholar]
- Ludlow JP, Evans SF, Hulse G. Obstetric and perinatal outcomes in pregnancies associated with illicit substance abuse. Aust N Z J Obstet Gynaecol. 2004;44:302–6. doi: 10.1111/j.1479-828X.2004.00221.x. [DOI] [PubMed] [Google Scholar]
- Marsch LA, Bickel WK, Badger GJ, et al. Buprenorphine treatment for opioid dependence: the relative efficacy of daily, twice and thrice weekly dosing. Drug Alcohol Depend. 2005;77:195–204. doi: 10.1016/j.drugalcdep.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Martin TC, Rocque MA. Accidental and non-accidental ingestion of methadone and buprenorphine in childhood: a single center experience, 1999-2009. Curr Drug Saf. 2011;6:12–16. doi: 10.2174/157488611794480034. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O'Brien CP, et al. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Mendelson J, Jones RT, Welm S, et al. Buprenorphine and naloxone combinations: the effects of three dose ratios in morphine-stabilized, opiate-dependent volunteers. Psychopharmacology (Berl) 1999;141:37–46. doi: 10.1007/s002130050804. [DOI] [PubMed] [Google Scholar]
- Middleton LS, Nuzzo PA, Lofwall MR, et al. The pharmacodynamic and pharmacokinetic profile of intranasal crushed buprenorphine and buprenorphine/naloxone tablets in opioid abusers. Addiction. 2011;106:1460–1473. doi: 10.1111/j.1360-0443.2011.03424.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moratti E, Kashanpour H, Lombardelli T, et al. Intravenous misuse of buprenorphine: characteristics and extent among patients undergoing drug maintenance therapy. Clin Drug Investig. 2010;30:S3–11. doi: 10.2165/11536020-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Morrison V. Psychoactive substance use and related behaviours of 135 regular illicit drug users in Scotland. Drug Alcohol Depend. 1989;23:95–101. doi: 10.1016/0376-8716(89)90013-6. [DOI] [PubMed] [Google Scholar]
- National Bureau of Investigation (NBI) NBI of Finland. Archive IDKRP/RTP 7433/213/2003. 2003.
- Neumark YD, Van Etten ML, Anthony JC. “Drug dependence” and death: survival analysis of the Baltimore ECA sample from 1981-1995. Subst Use Misuse. 2000;35:313–27. doi: 10.3109/10826080009147699. [DOI] [PubMed] [Google Scholar]
- Nordmann S, Frauger E, Pauly V, et al. Misuse of buprenorphine maintenance treatment since introduction of its generic forms: OPPIDUM survey. Pharmacoepidemiol Drug Saf. 2012;21:184–190. doi: 10.1002/pds.2263. [DOI] [PubMed] [Google Scholar]
- Pedapati EV, Bateman ST. Toddlers requiring pediatric intensive care unit admission following at-home exposure to buprenorphine/naloxone. Pediatr Crit Care Med. 2011;12:e102–107. doi: 10.1097/PCC.0b013e3181f3a118. [DOI] [PubMed] [Google Scholar]
- Pirnay SO, Megarbane B, Borron SW, et al. Effects of various combinations of benzodiazepines with buprenorphine on arterial blood gases in rats. Basic Clin Pharmacol Toxicol. 2008;103:228–239. doi: 10.1111/j.1742-7843.2008.00273.x. [DOI] [PubMed] [Google Scholar]
- Quigley J, Knudsen HK, Nuzzo PA, et al. Substance Use Characteristics and Treatment Perceptions Among Opioid Dependent Pregnant Women Initiating Methadone Treatment. Journal of Kentucky Medical Association. 2013;111:261–5. [Google Scholar]
- Reynaud M, Petit G, Potard D, et al. Six deaths linked to concomitant use of buprenorphine and benzodiazepines. Addiction. 1998;93:1385–1392. doi: 10.1046/j.1360-0443.1998.93913859.x. [DOI] [PubMed] [Google Scholar]
- Rogers JM. Tobacco and pregnancy: overview of exposures and effects. Birth Defects Res C Embryo Today. 2008;84:1–15. doi: 10.1002/bdrc.20119. [DOI] [PubMed] [Google Scholar]
- Rosado J, Walsh SL, Bigelow GE, et al. Sublingual buprenorphine/naloxone precipitated withdrawal in subjects maintained on 100mg of daily methadone. Drug Alcohol Depend. 2007;90:261–269. doi: 10.1016/j.drugalcdep.2007.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux P, Villes V, Blanche J, et al. Buprenorphine in primary care: risk factors for treatment injection and implications for clinical management. Drug Alcohol Depend. 2008;97:105–113. doi: 10.1016/j.drugalcdep.2008.03.025. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) National Survey on Drug Use and Health Detailed Tables. 2012 accessed online @ http://www.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/DetTabs/NSDUH-DetTabsSect1peTabs1to46-2012.htm - Tab1.17A. [PubMed]
- Schwartz RP, Gryczynski J, O'Grady KE, et al. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995-2009. Am J Public Health. 2013;103:917–922. doi: 10.2105/AJPH.2012.301049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selden T, Ahlner J, Druid H. Toxicological and pathological findings in a series of buprenorphine related deaths. Possible risk factors for fatal outcome. Forensic Sci Int. 2012;220:284–290. doi: 10.1016/j.forsciint.2012.03.016. et ak. [DOI] [PubMed] [Google Scholar]
- Simojoki K, Alho H. A Five-year follow-up of buprenorphine abuse potential. J Alcohol Drug Depend. 2013;1:1–6. 2013. [Google Scholar]
- Singh RA, Mattoo SK, Malhotra A, Varma VK. Cases of buprenorphine abuse in India. Acta Psychiatr Scand. 1992;86:46–48. doi: 10.1111/j.1600-0447.1992.tb03224.x. [DOI] [PubMed] [Google Scholar]
- Stitzer ML, Vandrey R. Contingency management: utility in the treatment of drug abuse disorders. Clin Pharmacol Ther. 2008;83:644–647. doi: 10.1038/sj.clpt.6100508. [DOI] [PubMed] [Google Scholar]
- Stoller KB, Bigelow GE, Walsh SL, et al. Effects of buprenorphine/naloxone in opioid-dependent humans. Psychopharmacology (Berl) 2001;154:230–242. doi: 10.1007/s002130000637. [DOI] [PubMed] [Google Scholar]
- Stover H. Barriers to opioid substitution treatment access, entry and retention: a survey of opioid users, patients in treatment, and treating and non-treating physicians. Eur Addict Res. 2011;17:44–54. doi: 10.1159/000320576. [DOI] [PubMed] [Google Scholar]
- Strain EC, Preston KL, Liebson IA, Bigelow GE. Acute effects of buprenorphine, hydromorphone and naloxone in methadone-maintained volunteers. J Pharmacol Exp Ther. 1992;261:985–993. [PubMed] [Google Scholar]
- Strain EC, Stoller K, Walsh SL, et al. Effects of buprenorphine versus buprenorphine/naloxone tablets in non-dependent opioid abusers. Psychopharmacology (Berl) 2000;148:374–383. doi: 10.1007/s002130050066. [DOI] [PubMed] [Google Scholar]
- Thirion X, Lapierre V, Micallef J, et al. Buprenorphine prescription by general practitioners in a French region. Drug Alcohol Depend. 2002;65:197–204. doi: 10.1016/s0376-8716(01)00161-2. [DOI] [PubMed] [Google Scholar]
- Tkacz J, Severt J, Cacciola J, et al. Compliance with buprenorphine medication-assisted treatment and relapse to opioid use. Am J Addict. 2012;21:55–62. doi: 10.1111/j.1521-0391.2011.00186.x. [DOI] [PubMed] [Google Scholar]
- Tracqui A, Kintz P, Ludes B. Buprenorphine-Related Deaths Among Drug Addicts in France: A Report on 20 Fatalities. J Anal Toxicol. 1998;22:430–434. doi: 10.1093/jat/22.6.430. 1998. [DOI] [PubMed] [Google Scholar]
- Tuten M, Jones HE, Svikis DS. Comparing homeless and domiciled pregnant substance dependent women on psychosocial characteristics and treatment outocomes. Drug Alcohol Depend. 2003;69:95–9. doi: 10.1016/s0376-8716(02)00229-6. [DOI] [PubMed] [Google Scholar]
- Uosukainen H, Bell JS, Laitinen K, et al. First insights into community pharmacy based buprenorphine-naloxone dispensing in Finland. Int J Drug Policy. 2013a;24:492–497. doi: 10.1016/j.drugpo.2013.02.004. [DOI] [PubMed] [Google Scholar]
- Uosukainen H, Kauhanen J, Bell JS, et al. Mortality among clients seeking treatment for buprenorphine abuse in Finland. Drug Alcohol Depend. 2013b;133:391–397. doi: 10.1016/j.drugalcdep.2013.06.022. [DOI] [PubMed] [Google Scholar]
- Uosukainen H, Kauhanen J, Voutilainen S, et al. Twelve-year trend in treatment seeking for buprenorphine abuse in Finland. Drug Alcohol Depend. 2013c;127:207–214. doi: 10.1016/j.drugalcdep.2012.07.002. [DOI] [PubMed] [Google Scholar]
- Vicknasingam B, Mazlan M, Schottenfeld RS, et al. Injection of buprenorphine and buprenorphine/naloxone tablets in Malaysia. Drug Alcohol Depend. 2010;111:44–49. doi: 10.1016/j.drugalcdep.2010.03.014. [DOI] [PubMed] [Google Scholar]
- Vidal-Trecan G, Varescon I, Nabet N, et al. Intravenous use of prescribed sublingual buprenorphine tablets by drug users receiving maintenance therapy in France. Drug Alcohol Depend. 2003;69:175–181. doi: 10.1016/s0376-8716(02)00312-5. [DOI] [PubMed] [Google Scholar]
- Vignau J, Duhamel A, Catteau J, et al. Practice-based buprenorphine maintenance treatment (BMT): how do French healthcare providers manage the opiate-addicted patients? J Subst Abuse Treat. 2001;21:135–144. doi: 10.1016/s0740-5472(01)00189-1. [DOI] [PubMed] [Google Scholar]
- Waller BF, Brownlee WJ, Roberts WC. Self-induced pulmonary granulomatosis. A consequence of intravenous injection of drugs intended for oral use. Chest. 1980;78:90–94. doi: 10.1378/chest.78.1.90. [DOI] [PubMed] [Google Scholar]
- Walsh SL, June HL, Schuh KJ, et al. Effects of buprenorphine and methadone in methadone-maintained subjects. Psychopharmacology (Berl) 1995;119:268–276. doi: 10.1007/BF02246290. [DOI] [PubMed] [Google Scholar]
- Walsh SL, Preston KL, Stitzer ML, et al. Clinical pharmacology of buprenorphine: ceiling effects at high doses. Clin Pharmacol Ther. 1994;55:569–580. doi: 10.1038/clpt.1994.71. [DOI] [PubMed] [Google Scholar]