Abstract
Low-income, urban African American (AA) girls are at heightened risk for sexually transmitted infections (STIs), and violence exposure may be an important risk factor. AA girls (N= 177) from low-income communities in Chicago completed a 2-year longitudinal study of HIV-risk behavior involving five waves of data collection (ages 12–16 at baseline) and a sixth wave (ages 14–22) assessing lifetime trauma and victimization history. Childhood exposure to violence (CEV) represented reports of physical, sexual, or witnessed violence before age 12. Latent growth curve analysis examined CEV as a covariate of sexual experience, number of sexual partners, and inconsistent condom use trajectories. CEV was associated with greater sexual risk, although the pattern differed across the three outcomes. Overall, findings emphasize the need for early interventions to reduce sexual risk among low-income urban girls who have experienced violence. Efforts to address or prevent violence exposure may also reduce rates of STIs in this population.
Keywords: sexual risk, violence exposure, African American girls
Introduction
Young African American (AA) women are among demographic groups bearing the greatest burden of sexually transmitted infections (STIs), including HIV/AIDS, in the United States (US). AA women account for the largest proportion of HIV/AIDS cases among US women (Centers for Disease Control and Prevention, 2008), with the rate of HIV/AIDS among young Black women estimated to be 11 times that for young white women (Centers for Disease Control and Prevention, 2010). Most new HIV/AIDS cases among women are diagnosed between the ages of 15–39, and AA women ages 15–24 currently suffer from the highest rates of both Chlamydia and Gonorrhea reported in the US (Centers for Disease Control and Prevention, 2009). A Centers for Disease Control and Prevention (CDC) study found that 44% of AA girls, compared to 20% of White and Mexican American girls, were infected with a STI (Forhan et al., 2009). Moreover, in the most recent CDC Youth Risk Behavior Survey, AA girls were more likely than their White and Hispanic peers to report having sex, having had four or more partners, and sexual debut before age 13 (Centers for Disease Control and Prevention, 2012). Most HIV-positive women are infected through heterosexual contact and at young ages (Centers for Disease Control and Prevention, 2008), and physiological development makes adolescent girls and young women particularly vulnerable to STIs (Center for AIDS Prevention Studies, 2002; Centers for Disease Control and Prevention, 2008; Quinn & Overbaugh, 2005). Like other health disparities that affect minority women, these disproportionate rates of STIs are likely rooted in the effects of poverty and social disadvantage (Pearlin, Schieman, Fazio, & Meersman, 2005). And this high risk profile is elevated for AA girls in psychiatric treatment, since teens in mental health treatment tend to engage in higher rates of sexual risk behaviors (Donenberg & Pao, 2004).
Violence exposure is prevalent among youth in mental health treatment (Jennings, 2004) and may be an important risk factor contributing to high rates of STIs among AA girls growing up in low-income, urban neighborhoods. Youth from inner-city communities are at disproportionate risk for violence exposure (Foster et al., 2007; Voisin, 2007; Wilson, Woods, Emerson, & Donenberg, 2012) because these communities have the highest rates of crime and violence (Berman, Silverman, & Kurtines, 2002; Osofsky, 1999). Adverse childhood experiences have been linked to negative health consequences including sexual risk behavior, STIs, and substance use (Dube, Felitti, Dong, Giles, & Anda, 2003; Repetti, Taylor, & Seeman, 2002; Rodgers et al., 2004). Likewise, stress is implicated as a root cause of health disparities, such as heightened rates of HIV/AIDS, impacting ethnic minority groups in the US (Ickovics et al., 2002; Pearlin et al., 2005).
Exposure to violence can have broad effects across multiple, interacting domains of development, with sexual risk representing one possible outcome. From a biological perspective, development of neurological structure and function can be disrupted by repetitive activation of the physiological stress response system (De Bellis, 2001; Ulrich-Lai & Herman, 2009). In particular, processes related to stress response and coping, emotion regulation, and executive function appear to be affected by childhood trauma (De Bellis, 2001; Ulrich-Lai & Herman, 2009), and alterations of these systems can put youth at a disadvantage in negotiating emotionally charged, often stressful sexual situations. Moreover, violence exposure can interfere with key aspects of psychosocial development (Margolin & Gordis, 2000), including attachment and family relationships (Osofsky, 1999; Voisin, Jenkins, & Takahashi, 2011), academics and peer relationships (Voisin et al., 2011), emotion regulation (Ehrensaft et al., 2003; Kim, Pears, Capaldi, & Owen, 2009), and behavioral control (Wolfe, Jaffe, & Crooks, 2006). Romantic relationships may be a particularly potent context linking violence exposure to sexual risk in both adolescents and adults (Wilson & Widom, 2011; Wilson et al., 2012). AA girls typically have less power than their male partners, who tend to be older, in terms of physical strength, social status, financial resources, and control over sexual decisions such as condom use or even whether to have sex (Wingood & DiClemente, 1998, 2000). History of violence exposure may magnify this power differential as it diminishes sense of control and self-efficacy (Margolin & Gordis, 2000). In addition, childhood exposure to violence increases risk of dating violence (Ehrensaft et al., 2003; Wolfe & Wekerle, 2004), which is associated with unwanted and unprotected sex (Wingood & DiClemente, 1998). Thus, different forms of violence may have similar developmental effects.
A growing body of research now links various forms of violence exposure, including sexual victimization, physical victimization, and witnessed community violence, to sexual risk behaviors (e.g., Brady & Donenberg, 2006; Senn, Carey, & Vanable, 2008; Voisin & Neilands, 2010; Wilson & Widom, 2008; Wyatt et al., 2002). In a sample of AA girls from low-income urban neighborhoods, more extensive exposure to physical victimization, sexual victimization, or witnessed violence was associated with more sexual partners and less consistent condom use (Wilson et al., 2012). In this study, findings were stronger for physical victimization than for sexual victimization or witnessed violence. However, most research in this area has focused on sexual victimization, limiting our understanding of the broader effects of violence on sexual risk. The current study defines violence broadly as exposure to a range of violent experiences in childhood, including physical and sexual victimization and witnessed violence occurring at home, at school, or in the neighborhood.
Finally, the relationship between violence exposure and sexual risk behavior may be more complex than can be captured in studies that only examine sexual behavior at a single point in time. Maladaptive and adaptive behaviors emerge in complex, dynamic patterns that can best be understood through observation of behaviors as they unfold over time (Sroufe & Rutter, 1984). However, existing studies linking violence exposure to sexual risk have generally relied on cross-sectional analyses (Malow, Devieux, & Lucenko, 2006; Senn et al., 2008), and none have assessed the development of sexual risk across multiple points in time. One longitudinal study found that court-substantiated childhood physical abuse, sexual abuse, and neglect predicted sexual risk in individuals followed into adulthood (Wilson & Widom, 2008, 2009). Another longitudinal study (Noll, Trickett, & Putnam, 2003) supported links from childhood sexual abuse to sexual risk behavior in adolescence. A recent longitudinal study found that allegations of sexual abuse documented by child welfare agencies from birth to age 12 years predicted sexual intercourse and alcohol use by age 14 years, but did not separate sexual activity from alcohol use (Jones et al., 2010).
The current study expanded upon existing research to examine relationships between childhood exposure to violence (CEV) and developmental patterns of sexual risk-taking among low-income, urban AA adolescent girls with histories of seeking mental health treatment. This sample represented a population at high risk of CEV since violence exposure is associated with mental health problems ranging from internalizing symptoms such as depression and anxiety to externalizing problems such as delinquency (Berman et al., 2002; Margolin & Gordis, 2000; Osofsky, 1999). Moreover, knowledge about links between CEV and sexual risk in treatment-seeking girls can be used to design interventions for reducing risk among girls presenting to mental health clinics. This study improved upon existing research by: (1) assessing multiple types of violence exposure; (2) focusing on low-income AA girls, a high-risk but underserved population, and thereby limiting confounds associated with race/ethnicity, gender, or socioeconomic status (SES); (3) examining longitudinal patterns of sexual behavior over six time points from early to late adolescence; and (4) considering multiple types of sexual behavior, including sexual experience, number of partners, and inconsistent condom use. We hypothesized that self-reported CEV would be associated with greater likelihood of sexual experience, more sexual partners, and more inconsistent condom use over the six time points. We also hypothesized that self-reported CEV would be associated with a sharper increase in these risk behaviors over time.
Methods
Design and Participants
Participants were 177 adolescent girls who participated in a longitudinal study of HIV-risk behavior involving five waves of data collected over two years, and a sixth follow-up to assess trauma history. AA girls ages 12–16 years old were originally recruited from eight outpatient mental health clinics, serving urban, mostly low-SES communities in Chicago. Clinic staff asked eligible families for permission to provide their contact information to research staff. Girls identified by clinic staff as cognitively delayed (n = 6) or wards of the Illinois Department of Child and Family Services (n = 3) were excluded from the study. Eighty-two percent of invited families participated in the study. A total of 266 participants completed the baseline interview, and between 75% and 82% of the baseline sample was retained at each of the original five waves of data collection. On the Computerized NIMH Diagnostic Interview Schedule for children (CDISC 4.0) (Shaffer, Fisher, Lucas, Dulcan, & Schwabstone, 2000) completed at baseline, 5% of girls reported past-year symptoms meeting DSM-IV criteria for PTSD, 4% for major depressive disorder (MDD), and 11% for conduct disorder (CD). Caregiver report on the CDISC 4.0 indicated that 3% met criteria for PTSD, 8% for MDD, 13% for CD, and 10% for ADHD. Using the methods of Brown et al. (2010), 66% of the girls met sub-threshold or threshold criteria for a psychiatric diagnosis based on self or parent report on the CDISC. At baseline, 38% of the girls were actively receiving mental health services based on caregiver report, 53% indicated that they had recently sought counseling, 7% reported being on a waitlist, and 2% reported a scheduled appointment. The majority of those receiving mental health services reported more than one treatment modality including individual, family, or group therapy, medication management, and day treatment (Emerson, Donenberg, & Wilson, 2012).
During 2009–2010, participants who completed the baseline and at least one follow-up wave were asked to return for a new study (Wave 6). Of eligible participants, 178 (74%) were enrolled; 3% refused, and 23% were lost because they could not be located, did not respond to contact attempts, or had moved out of the state. One enrolled case was dropped due to lack of comprehension and inconsistent responding. Girls were a mean of 17.72 years (SD = 1.65; range = 14.25 – 22.67), and on average completed Wave 6 3.27 years after baseline and 1.14 years after Wave 5. Average socio-economic status (SES) rating was 2.38 on the Hollingshead (1975) Index, reflecting semi-skilled work. The majority of female caregivers were biological mothers (76%), 71% described themselves as single parents, and 57% reported post high school education. Girls who completed Wave 6 did not differ significantly from those lost to attrition on baseline measurements of age (14.43 vs 14.52; t = −.63, df = 209.25, p > .10), SES rating (2.38 vs 2.22; t = 1.05, df = 253, p > .10), internalizing (15.83 vs 16.04; t = −.18, df = 264, p > .10) or externalizing (15.24 vs 15.54, t = −.24, df = 264, p > .10) mental health symptoms on the Youth Self Report, past six month number of sexual partners (.51 vs .79; t = −.89, df = 264, p > .10), consistency of condom use (.48 vs .62; t = −.97, df = 264, p > .10), or proportion reporting sexual experience (31.6% vs 37.1%, χ2 = .79, df = 1, p > .10).
CEV was assessed during the Wave 6 interviews with the adolescent girls, and sexual risk behavior was assessed at all six waves. All procedures were approved by the Institutional Review Boards at the universities involved in the study. Written, informed parental consent and adolescent assent or consent (ages 18 or over) was obtained for all participants.
Measures
Lifetime Victimization and Trauma History (LTVH)
Adolescent girls completed the LTVH (Widom, Dutton, Czaja, & Dumont, 2005), a 30-item gated instrument that assessed lifetime trauma and victimization history through a structured in-person interview. Questions referred to “scary and upsetting things” that happen to people “at home, in their neighborhood, or someplace else” and covered seven categories of trauma (general traumas, physical assault/abuse, sexual assault/abuse, family/friend murdered or suicide, witnessed trauma to someone else, crime victimization, and kidnapped or stalked). For each item, participants were first asked if they ever had the experience (e.g., “Has anyone ever shot at you, stabbed you, hit you, kicked you, beaten you, punched you, slapped you around, or hurt your body in some other way?”). For positively endorsed items, follow-up questions included the ages at which the event first and last occurred, the number of times it happened, and relationship of the perpetrator or victim. Participants could report up to four events corresponding to each item, and each event could reflect ongoing experiences. The interview took approximately 30–45 minutes depending on how many items and events were endorsed. The LTVH was originally developed with a diverse sample of adults (49% female; 35% Black) who tended toward lower income and education levels, and the measure demonstrated validity related to other self-reports and documented cases of child abuse (Widom et al., 2005). The youth version was modified through pilot testing and language modifications by the author of the measure. The current analysis focused on CEV, which was coded as a binary variable reflecting any report of physical victimization, sexual victimization, or witnessed violence that occurred before age 12 according to girls’ reports (“1” = any CEV; “0” = no CEV). This study utilized an aggregate-level variable given our conceptualization of violence as a broad construct encompassing multiple kinds of exposures (physical, sexual, witnessed).
AIDS-Risk Behavior Assessment (ARBA)
Sexual risk was assessed with the ARBA, a computer-assisted structured interview designed specifically for use with teens to assess sexual behavior, drug use, and needle use (Donenberg, Emerson, Bryant, Wilson, & Weber-Shifrin, 2001). The ARBA was derived from several well-established measures (see Donenberg et al., 2001) and assesses alcohol and drug use (e.g., lifetime use, method of use, frequency), needle use (e.g., sharing, tattooing, piercing), and sexual behavior (e.g., lifetime sexual intercourse, frequency, contraceptive use, high-risk sexual behavior). Separate sets of questions were asked about oral, anal, and vaginal sex with clear definitions of these behaviors (e.g., “by vaginal sex, we mean has anyone put his penis into your vagina/private part?”). The ARBA took 10–20 minutes to complete and assessed behavior over the past 6 months.
Information from the ARBA was used to create three separate variables reflecting sexual risk. Sexual experience reflected cumulative reports (i.e., a report of sexual experience at one time point indicated sexual experience at the following points) of vaginal, anal, or oral sexual experience. Number of partners was calculated from two items asking about male and female partners in the past 6 months (“How many male/female sex partners have you had in the past 6 months?”) considering vaginal, oral, and anal sex. Condom use inconsistency reflected use of condoms during vaginal sex in the past 6 months (0 = no vaginal sex; 1 = always used condoms; 2 = more than half the time; 3 = half the time; 4 = some of the time; 5 = never used condoms) based on response to the question, “Of the times you had vaginal sex in the past 6 months, how often did you or your partner use condoms/latex protection?” Only condom use during vaginal sex was included since vaginal sex was most commonly reported, and separate items asked about condom use during oral or anal sex. ARBA data from all six waves of the study were included in the current analyses.
Analyses
Relationships between childhood violence exposure and sexual risk were examined with latent curve modeling (LCM) using MPlus 7. LCM employs a structural equation modeling (SEM) framework to test models with latent growth factors (i.e., intercept and slope) reflecting the level of and change in an outcome across multiple points in time (Bollen & Curran, 2006). This approach incorporates both developmental change and within-subjects variation. LCM proceeded in two stages. The first stage involved testing separate unconditional growth models representing patterns of change in sexual risk (sexual experience, number of partners, inconsistent condom use) from T1 to T6. In unconditional models, the intercept factor indicated the level of sexual risk at T1, and the slope factor indicated increase or decrease in sexual risk over time. Both linear and quadratic models were examined, with quadratic terms indicating change in the slope. Models with sexual experience as the growth process were probit models, which reflect cumulative normal probability of the dependent variable. Mean and variance estimates for growth factors and their standard errors (se) were examined, except that the mean of the intercept was not evaluated in probit models since it is not meaningful.
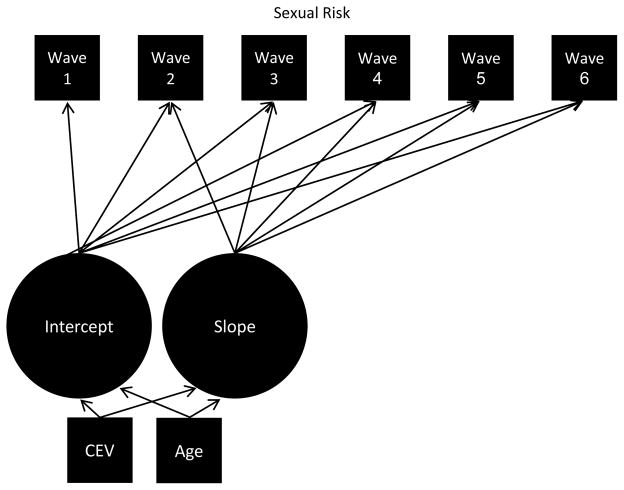
The second stage (Figure 1) examined conditional models with CEV as a time-invariant covariate predicting variation in the slope and intercept factors. Baseline age was also included as a time-invariant covariate to account for age-related differences in sexual risk. In conditional models, the relationship between CEV and the intercept represented the difference in the level of sexual risk between girls who reported CEV and those who did not. Multiple iterations of the models were run with the intercept set at each time point to determine differences between the CEV and comparison group at each respective point. The relationship between CEV and the slope indicated between group differences in the pattern of change across time. Both magnitude (i.e., effect size) and statistical significance of standardized coefficients (β) were evaluated.
Figure 1.
Latent curve model
Missing data was handled with full information maximum likelihood (FIML) estimation, which utilizes all data available for each case and thus avoids biases and loss of power associated with traditional approaches to missing data (Allison, 2003; Schlomer, Bauman, & Card, 2010). Thus, cases were included even when data were not available for all six time points. We used a maximum likelihood estimator that is robust to non-normality and non-independence of observation (MLR), equivalent to the Yuan-Bentler T2* test, for the continuous sexual risk variables and a weighted least square parameter estimator using a diagonal weight matrix with standard errors and mean- and variance-adjusted chi-square test statistic (χ2) using a full weight matrix (WLSMV) for the binary sexual experience models. We evaluated multiple indices of overall model fit (Barrett, 2007; Bollen & Curran, 2006). A non-significant (p > .05) chi-square (χ2) indicates a good fit; Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI) of greater than .90 indicate a good fit; Root Mean Square Error of Approximation (RMSEA) of less than or equal to .05 is considered a very close fit and .05 – .10 a moderate fit; Weighted Root-Mean-Square Residual (WRMR) of less than or equal to .9 is considered a good fit for binary outcomes; Standardized Root-Mean-Square Residual (SRMR) of less than or equal to .08 is considered a good fit for continuous outcomes.
Results
Descriptive Information
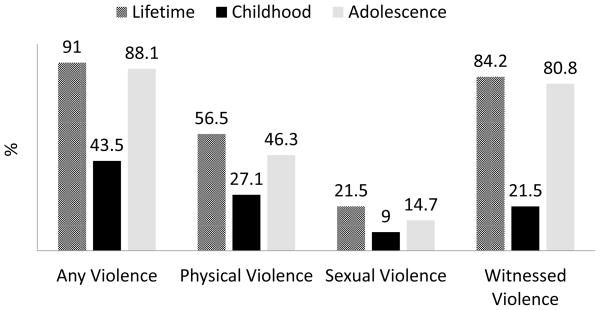
Prevalence of violence exposure reported by the sample is provided in Figure 2. The majority of girls (91%) reported some form of violence exposure in either childhood or adolescence, and nearly half (43.5%) reported exposure to violence during childhood. Physical violence was most commonly reported in childhood (27.1%), compared to sexual violence (9%) or witnessed violence (21.5%). In subsequent analyses, the binary independent variable for CEV reflected 43.5% in the CEV group, and 56.5% were in the comparison group.
Figure 2.
Percentage of sample reporting violence exposure
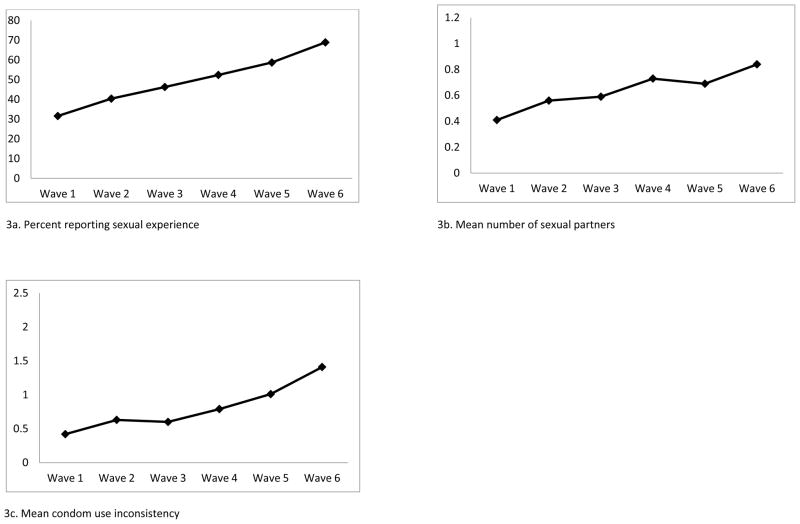
Sexual experience in the sample increased over time (Figure 3a), with 31.6% at Wave 1 to 68.9% at Wave 6. Average number of sexual partners (Figure 3b) also increased over time, with a mean of .41 at Wave 1 to .84 at Wave 6. Means of less than 1 reflected the sizeable portion of the sample reporting no sexual partners at each wave. The pattern of condom use changed from consistent (or no sexual activity) at Wave 3 (mean = .60), around age 15, to use less than always by Wave 6 (mean = 1.41).
Figure 3.
Sexual risk across Waves 1–6
Unconditional Growth Models
The unconditional probit model for sexual experience provided a strong fit with observed data (see Table 1). Variance around the intercept was moderate, but there was almost no estimated variability in the slope. Consistent with Figure 3a, the positive mean slope indicated an increase in the likelihood of sexual experience over time.
Table 1.
Unconditional Growth Curve Models
| Model | Model Fit Statistics | Intercept Factor | Slope Factor | Covariance | Quadratic Factor | |||
|---|---|---|---|---|---|---|---|---|
| M | Var (S.E.) | M | Var (S.E.) | β | M | Var (S.E.) | ||
| Sexual Experience (probit) | χ2 = 5.78, df = 11; p = .89 | |||||||
| CFI = 1.00; TLI = 1.00; RMSEA = .00; WRMR = .19 | NA | .98 (.08)*** | 1.82* | .01 (.01) | −.51 | |||
| Number of Partners (linear) | χ2 = 28.77, df = 16, p = .03 | |||||||
| CFI = .90; TLI = .91; RMSEA = .07; SRMR = .11 | .51*** | .67 (.18)*** | .40*** | .04 (.01)** | −.49*** | |||
| Number of Partners (quadratic) | χ2 = 7.38, df = 12, p = .83 | |||||||
| CFI = 1.00; TLI = 1.05; RMSEA = .00; SRMR = .06 | .54*** | .59 (.21)** | .17 | .25 (.10)* | .02 | −.002 | .01 (.004)* | |
| Inconsistent Condom Use (linear) | χ2 = 54.39, df = 17, p = .00 | |||||||
| CFI = .78; TLI = .80; RMSEA = .11; SRMR = .09 | .43*** | .98 (.25)*** | .56 | .08 (.02)*** | −.38*** | |||
| Inconsistent Condom Use (quadratic) | χ2 = 16.43, df=13, p = .23 | |||||||
| CFI = .98; TLI = .98; RMSEA = .04; SRMR = .05 | .53*** | .93 (.22)*** | .08 | .54 (.15)*** | −.32* | .19 | .02 (.01)*** | |
NOTE: M = mean; Var = variance; S.E. =standard error; β = standardized coefficient; NA = mean intercept is not estimated for binary outcomes. Covariance refers to the covariance of the intercept and slope. χ2 = chi-square statistic reflecting overall model fit (p > .05 indicates a good fit); df = degrees of freedom; CFI = Comparative Fit Index (≥ .90 indicates a good fit); TFI = Tucker-Lewis Index (≥ .90 indicates a good fit); RMSEA = Root Mean Square Error of Approximation (≤ .05 is considered a very close fit; .05 – .10 is considered a moderate fit); WRMR = Weighted Root-Mean-Square Residual (used for binary outcomes, ≤ .9 is considered a good fit); SRMR = Standardized Root-Mean-Square Residual (used for continuous outcomes, ≤ .08 is considered a good fit).
p ≤ .05
p ≤ .01
p ≤ .001
As shown in Table 1, fit indices for the unconditional linear model for number of partners were slightly outside the desired range, with a significant χ2 and SRMR greater than .08. The intercept was significantly different than zero, and the slope indicated an increase in number of partners over time, consistent with Figure 3b. Although improvement in model fit with addition of the quadratic term did not quite reach statistical significance (χ2 difference = 8.30, df = 4, p = .08), all fit indices were within the desired range for the quadratic model, and therefore this model was used in subsequent analyses. The intercept was significantly different than zero. In a quadratic model, the slope changes over time. The increase in number of partners was statistically significant at Wave 2 (mean = .25, p < .05; variance = .11, se = .04, p < .05), Wave 3 (mean = .36, p < .001; variance = .05, se = .02, p < .001), and Wave 4 (mean = .31, p < .01; variance = .07, se = .02, p < .01), but not at Wave 1 (mean = .17, p = .09; variance = .25, se = .10, p < .05), Wave 5 (mean = .20, p = .07; variance = .16, se = .06, p < .05), or Wave 6 (mean = .14, p = .21; variance = .33, se = .13, p < .05). The quadratic term was non-significant.
The quadratic model for inconsistent condom use (see Table 1) provided an improved fit over the linear model (χ2 difference = 33.96, df = 4, p < .001) and therefore was used in subsequent analyses. The residual variance of condom use at Wave 1 was fixed at zero due to a negative estimated variance (i.e., very little heterogeneity within the sample). The intercept differed significantly from zero. The slope was non-significant at Wave 1 (mean = .08, p = .40; variance = .54, se = .15, p < .001) but was positive and significant at Wave 2 (mean = .23, p < .05; variance = .23, se = .06, p < .001), Wave 3 (mean = .57, p < .001; variance = .08, se = .02, p < .001), Wave 4 (mean = .66, p < .001; variance = .11, se = .03, p < .01), Wave 5 (mean = .50, p < .001; variance = .30, se = .08, p < .001), and Wave 6 (mean = .40, p < .001; variance = .66, se = .17, p < .001). Although it did not quite reach statistical significance (p = .06), the quadratic term indicated acceleration in inconsistent condom use, as depicted at Wave 3 in Figure 3c.
Conditional Growth Models
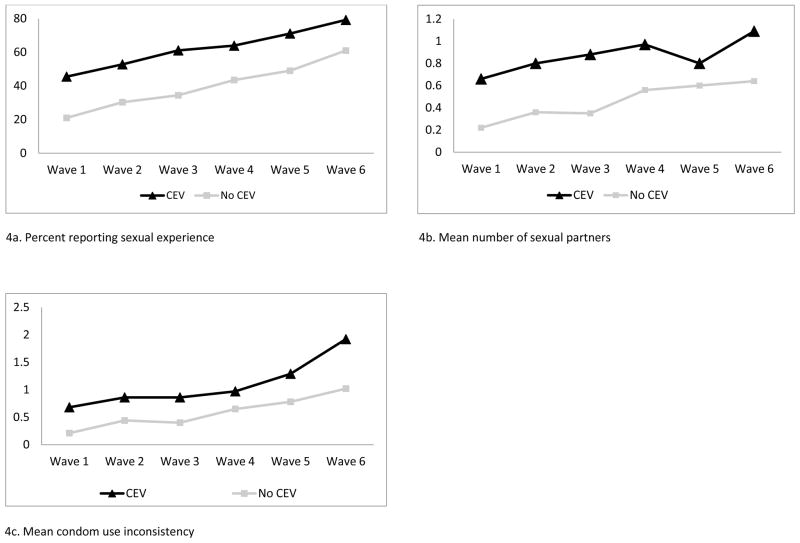
Sexual experience
Between group differences in patterns of sexual risk are depicted in Figure 4, and the results of conditional growth models are presented in Table 2. The conditional sexual experience model with CEV and age as covariates provided a strong fit. CEV was significantly associated with the intercept at Waves 1 through 4, indicating increased likelihood of sexual experience in the CEV group, but not at Waves 5 or 6. CEV was not significantly related to the slope, indicating a similar rate of increase in both groups. Age was negatively associated with the slope, indicating less increase over time with increased age, and increased likelihood of sexual experience at Waves 1 to 5 but not at Wave 6.
Figure 4.
Sexual risk across Waves 1–6 in girls reporting CEV and girls not reporting CEV
Table 2.
Conditional Growth Curve Models
| Model | Sexual Experience | Number of Partners | Inconsistent Condom Use |
|---|---|---|---|
| Model Fit Statistics | |||
| χ2 (df) | 10.70 (19) | 14.30 (18) | 14.30 (19) |
| p-value | .93 | .71 | .27 |
| CFI | 1.00 | 1.00 | .99 |
| TLI | 1.00 | 1.03 | .98 |
| RMSEA | .00 | .00 | .03 |
| WRMR | .20 | .05 | .04 |
| Path coefficients | β (p-value) | β (p-value) | β (p-value) |
| Intercept (T1) on CEV | .23 (.009) | .26 (.000) | .20 (.001) |
| Intercept (T2) on CEV | .23 (.007) | .22 (.002) | .16 (.039) |
| Intercept (T3) on CEV | .23 (.008) | .19 (.015) | .14 (.104) |
| Intercept (T4) on CEV | .23 (.020) | .18 (.020) | .16 (.057) |
| Intercept (T5) on CEV | .23 (.065) | .19 (.012) | .22 (.010) |
| Intercept (T6) on CEV | .21 (.183) | .19 (.025) | .27 (.003) |
| Slope (T1) on CEV | −.19 (.256) | −.03 (.803) | −.09 (.322) |
| Slope (T2) on CEV | −.19 (.256) | −.03 (.772) | −.05 (.559) |
| Slope (T3) on CEV | −.19 (.256) | −.03 (.752) | .06 (.509) |
| Slope (T4) on CEV | −.19 (.256) | −.01 (.887) | .18 (.081) |
| Slope (T5) on CEV | −.19 (.256) | −.001 (.994) | .18 (.071) |
| Slope (T6) on CEV | −.19 (.256) | .01 (.961) | .18 (.080) |
| Quadratic on CEV | NA | .02 (.878) | .15 (.135) |
| Intercept (T1) on Age | .47 (.000) | .21 (.027) | .31 (.000) |
| Intercept (T2) on Age | .45 (.000) | .21 (.027) | .36 (.000) |
| Intercept (T3) on Age | .42 (.000) | .19 (.049) | .32 (.000) |
| Intercept (T4) on Age | .38 (.003) | .18 (.062) | .27 (.001) |
| Intercept (T5) on Age | .32 (.019) | .16 (.070) | .19 (.026) |
| Intercept (T6) on Age | .23 (.196) | .11 (.208) | .07 (.395) |
| Slope (T1) on Age | −.54 (.003) | −.04 (.730) | .09 (.374) |
| Slope (T2) on Age | −.54 (.003) | −.02 (.846) | .05 (.605) |
| Slope (T3) on Age | −.54 (.003) | −.02 (.783) | −.06 (.507) |
| Slope (T4) on Age | −.54 (.003) | −.07 (.429) | −.18 (.019) |
| Slope (T5) on Age | −.54 (.003) | −.08 (.451) | −.19 (.037) |
| Slope (T6) on Age | −.54 (.003) | −.07 (.483) | −.18 (.062) |
| Quadratic on Age | NA | −.06 (.577) | −.15 (.154) |
NOTE: χ2 = chi-square statistic reflecting overall model fit (p > .05 indicates a good fit); df = degrees of freedom; CFI = Comparative Fit Index (≥ .90 indicates a good fit); TFI = Tucker-Lewis Index (≥ .90 indicates a good fit); RMSEA = Root Mean Square Error of Approximation (≤ .05 is considered a very close fit; .05 – .10 is considered a moderate fit); WRMR = Weighted Root-Mean-Square Residual (used for binary outcomes, ≤ .9 is considered a good fit); SRMR = Standardized Root-Mean-Square Residual (used for continuous outcomes, ≤ .08 is considered a good fit). β = standardized regression coefficient; T = Wave 1; T2 = Wave 2; T3 = Wave 3; T4 = Wave 4; T5 = Wave 5; T6 = Wave 6; CEV = childhood exposure to violence. Models are tested with the intercept set at each time point. Note that in quadratic models, the slope also changes over time, whereas the slope is constant in the probit model.
Number of partners
The conditional quadratic model for number of partners provided a strong fit (see Table 2). CEV was associated with a higher intercept (i.e., greater number of partners) at all waves of the study, but not with the slope at any wave (note that the slope changes in a quadratic model). Age was positively associated with the intercept at Waves 1 to 3, but this relationship reduced to non-significance at Waves 4 to 6. Age was not associated with the slope at any wave.
Inconsistent condom use
The conditional quadratic model for inconsistent condom use yielded a strong fit (see Table 2). CEV was associated with more inconsistent condom use at Waves 1 and 2 and at Waves 5 and 6, but not Waves 3 or 4. CEV was not significantly associated with the slope at any time point or with the quadratic term. Age was associated with inconsistent condom use at Waves 1 through 5 but not at Wave 6. Age was negatively and significantly associated with the slope at Waves 4 and 5, suggesting less increase in risk for older girls, but was not associated with the quadratic term.
Discussion
In a sample of low-income, mental health treatment-seeking AA girls, childhood violence exposure (CEV) was associated with increased sexual risk, and this relationship generally persisted over time. Notably, the link between CEV and sexual risk was evident even though violence exposure after age 12 was prevalent in the sample and is strongly associated with sexual risk (Wilson et al., 2012). This relationship existed above and beyond the effects of age on sexual behavior. For all girls in the sample, sexual risk increased over time, and the pattern of increase was parallel for girls exposed to violence and those who did not report violence exposure. Although girls reporting CEV endorsed higher levels of sexual risk, in both groups, risk behavior increased over time and at a similar rate.
The pattern of findings differed somewhat for sexual experience, number of partners, and inconsistent condom use. Although CEV was associated with earlier onset of sexual experience and greater likelihood of sexual experience through the fourth wave of the study, when girls averaged 15 years old, this relationship was no longer as clear by the final assessment when the majority of girls in the sample were sexually active. By contrast, the relationship between CEV and number of sexual partners was significant at all waves of the study. Inconsistent condom use, on the other hand, was associated with CEV at all points except for Waves 3 and 4, at which point the sample in general showed an acceleration in this risk behavior and a shift from consistent to inconsistent use of protection. Other studies have reported that condom use decreases with age and that teens are less likely to use condoms with serious partners than with casual partners (Centers for Disease Control and Prevention, 2012; Lescano et al., 2006). Our findings suggest that risk associated with CEV in low-income girls may be influenced by developmental changes in sexual behavior across adolescence. As sexual activity becomes more normative by late adolescence, the relationship with CEV may manifest in predicting less safe sex. Likewise, CEV may be a less salient predictor of condom use during periods of normative decrease due to age and other developmental factors.
Exposure to violence may be one important mechanism leading to sexual risk in low-income, urban African American girls with mental health concerns. Findings from this study suggest that girls presenting to mental health clinics with histories of violence exposure would likely benefit from interventions to reduce sexual risk-taking. Early interventions, before initiation of sexual activity, might prevent a persistent pattern of health-compromising sexual behaviors. Outpatient mental health services offer a valuable setting to implement interventions to address sexual risk in girls exposed violence, given high rates of CEV in clinic populations and the availability of resources for behavioral interventions. Screening for CEV during clinic evaluations may reveal girls at particular risk for negative sexual health outcomes and who need interventions to promote healthy sexual relationships and decision-making. Integrating empirically supported interventions to reduce sexual health risk in AA girls (DiClemente et al., 2004) with evidence based treatments for trauma (Cohen and Mannarino, 2008) may prove beneficial in reducing rates of STIs and other negative sexual health consequences in this highly vulnerable population of girls.
Further research is needed to understand the specific biological and psychosocial mechanisms that may link CEV to sexual risk. Previous research has supported maladaptive romantic relationships as an important mediator of the pathway from childhood maltreatment to sexual risk in middle adulthood (Wilson & Widom, 2011). Another study similarly found that involvement with risky partners explained increased risk for STIs among women with histories of sexual abuse (Testa, VanZile-Tamsen, & Livingston, 2005). Unhealthy or risky romantic relationships might help to explain sexual risk in adolescent girls with histories of CEV. Previous findings with the current sample suggested that violence in the context of dating relationships (either victimization or witnessed experiences) was a stronger predictor of sexual risk than violence involving family, peers, or other community members (Wilson et al., 2012). As discussed in the introduction of this article, CEV may amplify the power differential between girls and their partners (Wingood & DiClemente, 1998, 2000), making it difficult for them to refuse sex or ensure safe sex. Consistent with this hypothesis, one study found that low sexual assertiveness mediated the relationship between sexual abuse and sexual risk in adult women (Morokoff et al., 2009). Other developmental mechanisms may also explain this relationship. Importantly, physiological processes related to stress response and coping, emotion regulation, and executive function (De Bellis, 2001; Ulrich-Lai & Herman, 2009) likely play a role in the pathway from CEV to sexual risk in adolescent girls.
Although a causal relationship cannot be concluded from this study, reports of violence exposure before age 12, and thus before girls entered the study and completed Wave 1 reports of sexual behavior, provide an approximation of temporal precedence. Similarly, the pattern persisted over time, providing support for a plausible causal mechanism. In addition, controls for age and demographic characteristics help to rule out these potential confounding variables. However, a number of alternate explanations are plausible. For example, the connection between CEV and sexual risk could reflect an overall pattern of risky behaviors and circumstances. Nonetheless, CEV appears to be a marker for increased sexual risk in this population of adolescent girls.
A number of other important limitations should be considered in interpreting the results of this study. First, self-report of childhood trauma is subject to a number of recall errors and biases (Widom & Czaja, 2012). Girls may not have remembered very early experiences or may have chosen not to talk about certain experiences. Second, it is possible that some reports of sexual behavior in this study reflected abusive or coercive experiences. However, nearly 70% of the sample reported sexual experience by the end of the study, whereas only 22% reported experiences of sexual victimization. In teens, it is difficult to tease apart sexual experiences that are truly mutually consensual from those that involve some level of coercion. Nonetheless, both consensual and non-consensual experiences place girls at risk for HIV and other STIs. Third, this study focused on a broad conceptualization of childhood violence exposure, and power considerations precluded splitting the sample into small groups reflecting more specific forms of violence, which could be associated with different patterns of sexual risk. Finally, the sample of low-income AA girls in this study may not generalize to other adolescent girls, and moreover, families who were willing and able to participate in this six-wave longitudinal study may differ in meaningful ways from typical individuals in their community.
In conclusion, findings from this study highlight the connection between CEV and sexual risk in low-income, urban girls seeking mental health treatment. Consideration of developmental changes in sexual behavior from early to late adolescence provided a robust test of this relationship and revealed a complex pattern that differed over time and with developmental change. These findings emphasize the need for developmentally targeted interventions to reduce sexual risk among low-income urban girls who have experienced violence. Early interventions with this population are needed to delay sexual activity, whereas later interventions must emphasize use of safe sex practices such as consistent condom use. Finally, efforts to address or prevent violence exposure may also reduce rates of STIs in AA girls growing up in impoverished urban communities.
Acknowledgments
This research was supported by funding from the National Institute of Mental Health (R03MH086361; R01MH065155) and National Institute of Child Health and Human Development (R01HD067511-01). We thank the mothers and daughters who participated in the study, and gratefully acknowledge the administrators and clinical staff at the outpatient mental health clinics who worked with us to identify eligible families. These data reflect self-reported behaviors that place girls at risk for sexually transmitted infections, including HIV/AIDS, and may not represent girls’ willingness to engage the behavior. We also thank Gloria Coleman, Bola Animashaun, Tiffany Brakefield, Neha Darji, Laura Pettineo, Paige Saltzberg, and Mary Beth Tull for their invaluable assistance in recruiting families, conducting interviews, and entering data.
Contributor Information
Helen W. Wilson, Stanford University School of Medicine
Geri R. Donenberg, University of Illinois at Chicago
Erin Emerson, University of Illinois at Chicago.
References
- Allison Paul D. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;117:545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- Barrett P. Structural equation modelling: Adjudging model fit. Personality and Individual Differences. 2007;42:815–824. [Google Scholar]
- Berman SL, Silverman WK, Kurtines WM. The effects of community violence on children and adolescents: Intervention and social policy. In: Bottoms BL, Kovera MB, McAuliff BD, editors. Children, social science, and the law. Cambridge, UK: Cambridge University Press; 2002. pp. 301–321. [Google Scholar]
- Bollen KA, Curran PJ. Latent growth curve models: A structural equation perspective. Hoboken, NJ: Wiley & Sons; 2006. [Google Scholar]
- Brady SS, Donenberg GR. Mechanisms linking violence exposure to health risk behavior in adolescence: Motivation to cope and sensation seeking. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:673–680. doi: 10.1097/01.chi.0000215328.35928.a9. [DOI] [PubMed] [Google Scholar]
- Brown LK, Hadley W, Stewart A, Lescano C, Whiteley L, Donenberg G Project STYLE Study Group. Psychiatric disorders and sexual risk among adolescents in mental health treatment. Journal of Consulting and Clinical Psychology. 2010;78:590–597. doi: 10.1037/a0019632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for AIDS Prevention Studies. What are young women’s HIV prevention needs? Center for AIDS Prevention Studies (CAPS) and the AIDS Research Institute, University of California; San Fransciso: 2002. [Google Scholar]
- Centers for Disease Control and Prevention. CDC HIV/AIDS Fact Sheet. 2008. HIV/AIDS among women. [Google Scholar]
- Centers for Disease Control and Prevention. Sexually transmitted diseases in the United States, 2008: National surveillance data for chlamydia, gonorrhea, and syphilis. 2009. [Google Scholar]
- Centers for Disease Control and Prevention. HIV and AIDS among African American youth. 2010. [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance -- United States, 2011. MMWR. 2012;61(4) [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Trauma-focused cognitive behavioural therapy for children and parents. Child and Adolescent Mental Health. 2008;13(4):158–162. doi: 10.1111/j.1475-3588.2008.00502.x. [DOI] [PubMed] [Google Scholar]
- De Bellis MD. Developmental traumatology: The psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology. 2001;13:539–564. doi: 10.1017/s0954579401003078. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Hook EW, Robillard A. Efficacy of an HIV prevention intervention for African American adolescent girls: a randomized controlled trial. Journal of the American Medical Association. 2004;292(2):171–179. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- Donenberg GR, Emerson E, Bryant B, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donenberg GR, Pao M. HIV/AIDS prevention and intervention: Youths and psychiatric illness. Contemporary Psychiatry. 2004;2:1–8. [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: Evidence from four birth cohorts dating back to 1900. Preventive Medicine. 2003;37:268–277. doi: 10.1016/s0091-7435(03)00123-3. [DOI] [PubMed] [Google Scholar]
- Ehrensaft MK, Cohen P, Brown J, Smailes E, Chen H, Johnson JG. Intergenerational transmission of partner violence: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2003;71:741–753. doi: 10.1037/0022-006x.71.4.741. [DOI] [PubMed] [Google Scholar]
- Emerson E, Donenberg GR, Wilson HW. Health-protective effects of attachment among African American girls in psychiatric care. Journal of Family Psychology. 2012;26(1):124–132. doi: 10.1037/a0026352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forhan SE, Gottlieb SL, Sternberg MR, Xu F, Datta SD, McQuillan GM, Markowitz LE. Prevalence of sexually transmitted infections among female adolescents aged 14 to 19 in the United States. Pediatrics. 2009;124:1505–1512. doi: 10.1542/peds.2009-0674. [DOI] [PubMed] [Google Scholar]
- Foster H, Brooks-Gunn J, Martin A, Flannery DJ, Vazsonyi AT, Waldman ID. The Cambridge handbook of violent behavior and aggression. New York, NY, US: Cambridge University Press; 2007. Poverty/socioeconomic status and exposure to violence in the lives of children and adolescents; pp. 664–687. [Google Scholar]
- Hollingshead AB. Four-factor index of social status. New Haven, CT: Yale University; 1975. [Google Scholar]
- Ickovics JR, Beren SE, Grigorenko EL, Morrill AC, Druley JA, Rodin J. Pathways of risk: Race, social class, stress, and coping as factors predicting heterosexual risk behaviors for HIV among women. AIDS and Behavior. 2002;6:339–350. [Google Scholar]
- Jennings A. The damaging consequences of violence and trauma: Facts, discussion points, and recommendations for the behavioral health system. National Technical Assistance Center for State Mental Health Planning (NTAC); 2004. [Google Scholar]
- Jones DJ, Runyan DK, Lewis T, Litrownik AJ, Black MM, Wiley T, Nagin DS. Trajectories of childhood sexual abuse and early adolescent HIV/AIDS risk behaviors: The role of other maltreatment, witnessed violence, and child gender. Journal of Clinical Child and Adolescent Psychology. 2010;39:667–680. doi: 10.1080/15374416.2010.501286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HK, Pears KC, Capaldi DM, Owen LD. Emotional dysregulation in the intergenerational transmission of romantic relationship conflict. Journal of Family Psychology. 2009;23:585–595. doi: 10.1037/a0015935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lescano CM, Vazquez EA, Brown LK, Litvin EB, Pugatch DM Project SHIELD Study Group. Condom use with “casual” and “main” partners: What’s in a name? Journal of Adolescent Health. 2006;39:443e441–443.e447. doi: 10.1016/j.jadohealth.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Malow R, Devieux J, Lucenko BA. History of childhood sexual abuse as a risk factor for HIV risk behavior. Journal of Trauma Practice. 2006;5:13–32. [Google Scholar]
- Margolin G, Gordis EB. The effects of family and community violence on children. Annual Review of Psychology. 2000;51:445–479. doi: 10.1146/annurev.psych.51.1.445. [DOI] [PubMed] [Google Scholar]
- Morokoff PJ, Redding CA, Harlow LL, Cho S, Rossi JS, Meier KS, Brown-Peterside P. Associations of sexual victimization, depression, and sexual assertiveness with unprotected sex: A test of the multifaceted model of HIV risk across gender. Journal of Applied Biobehavioral Research. 2009;14:30–54. doi: 10.1111/j.1751-9861.2009.00039.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noll JG, Trickett PK, Putnam FW. A prospective investigation of the impact of childhood sexual abuse on the development of sexuality. Journal of Consulting and Clinical Psychology. 2003;71:575–586. doi: 10.1037/0022-006x.71.3.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osofsky JD. The impact of violence on children. Domestic Violence and Children. 1999;9(3):33–49. [PubMed] [Google Scholar]
- Pearlin L, Schieman S, Fazio EM, Meersman SC. Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior. 2005;46:205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Quinn TC, Overbaugh J. HIV/AIDS in women: An expanding epidemic. Science. 2005;308:1582–1583. doi: 10.1126/science.1112489. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. [PubMed] [Google Scholar]
- Rodgers CS, Lang AJ, Laffate C, Satz LE, Dresselhaus TR, Stein MB. The impact of individual forms of childhood maltreatment on health behavior. Child Abuse and Neglect. 2004;28:575–586. doi: 10.1016/j.chiabu.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, Card NA. Best practices for missing data management in counseling psychology. Journal of Counseling Psychology. 2010;57:1–10. doi: 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- Senn TE, Carey MP, Vanable PA. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: Evidence from controlled studies, methodological critique, and suggestions for research. Clinical Psychology Review. 2008;28:711–735. doi: 10.1016/j.cpr.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwabstone ME. NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, difference from previous versions and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sroufe LA, Rutter M. The domain of developmental psychopathology. Child Development. 1984;55:17–29. [PubMed] [Google Scholar]
- Testa M, VanZile-Tamsen C, Livingston JA. Childhood sexual abuse, relationship satisfaction, and sexual risk taking in a community sample of women. Journal of Consulting and Clinical Psychology. 2005;73:1116–1124. doi: 10.1037/0022-006X.73.6.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulrich-Lai YM, Herman J. Neural regulation of endocrine and autonomic stress responses. Nature Reviews Neuroscience. 2009;10:397–409. doi: 10.1038/nrn2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voisin DR. The effects of family and community violence exposure among youth: Recommendations for practice and policy. Journal of Social Work Education. 2007;43:51–66. [Google Scholar]
- Voisin DR, Jenkins EJ, Takahashi L. Toward a conceptual model linking community violence exposure to HIV-related risk behaviors among adolescents: Directions for research. Journal of Adolescent Health. 2011;49:230–236. doi: 10.1016/j.jadohealth.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voisin DR, Neilands TB. Community violence and health risk factors among adolescents among adolescents on Chicago’s Southside: Does gender matter? Journal of Adolescent Health. 2010;46:600–602. doi: 10.1016/j.jadohealth.2009.11.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom CS, Czaja SJ. Childhood trauma, psychopathology, and violence: Disentangling causes, consequences, and correlates. In: Widom CS, editor. Trauma, psychopathology, and violence: Causes, correlates, or consequences? New York: Oxford University Press; 2012. [Google Scholar]
- Widom CS, Dutton MA, Czaja SJ, Dumont KA. Development and validation of a new instrument to assess lifetime trauma and victimization history. Journal of Traumatic Stress. 2005;18(5):519–531. doi: 10.1002/jts.20060. [DOI] [PubMed] [Google Scholar]
- Wilson HW, Widom CS. An examination of risky sexual behavior and HIV among victims of child abuse and neglect: A thirty-year follow-up. Health Psychology. 2008;27:49–158. doi: 10.1037/0278-6133.27.2.149. [DOI] [PubMed] [Google Scholar]
- Wilson HW, Widom CS. Sexually transmitted diseases among adults who had been abused and neglected as children: A 30-year prospective study. American Journal of Public Health. 2009;99:S197–S203. doi: 10.2105/AJPH.2007.131599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson HW, Widom CS. Pathways from childhood abuse and neglect to HIV-risk sexual behavior in middle adulthood. Journal of Consulting and Clinical Psychology. 2011;79:236–246. doi: 10.1037/a0022915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson HW, Woods BA, Emerson Erin, Donenberg Geri R. Patterns of violence exposure and sexual risk in low-income, urban African American girls. Psychology of Violence. 2012;2:194–207. doi: 10.1037/a0027265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. Partner influences and gender-related factors associated with noncondom use among young adult African American women. American Journal of Community Psychology. 1998;26:29–51. doi: 10.1023/a:1021830023545. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Education and Behavior. 2000;27:539–565. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]
- Wolfe DA, Jaffe PG, Crooks CV. Adolescent Risk Behaviors: Why Teens Experiment and Strategies to Keep Them Safe. New Haven, CT: Yale University Press; 2006. [Google Scholar]
- Wolfe DA, Wekerle C. Predicting abuse in adolescent dating relationships over 1 year: The role of child maltreatment and trauma. Journal of Abnormal Psychiatry. 2004;113:406–415. doi: 10.1037/0021-843X.113.3.406. [DOI] [PubMed] [Google Scholar]
- Wyatt GE, Myers HF, Williams JK, Kitchen CR, Loeb T, Carmona JV, Presley N. Does a history of trauma contribute to HIV risk for women of color? Implications for prevention and policy. American Journal of Public Health. 2002;92:660–665. doi: 10.2105/ajph.92.4.660. [DOI] [PMC free article] [PubMed] [Google Scholar]