Abstract
In this study, in vitro and in vivo experiments were carried out with the high-affinity multifunctional D2/D3 agonist D-512 in order to explore its potential neuroprotective effects in models of Parkinson’s disease (PD) and the potential mechanism(s) underlying such properties. Pretreatment with D-512 in vitro was found to rescue rat adrenal phaeochromocytoma PC12 cells from toxicity induced by 6-hydroxydopamine (6-OHDA) administration in a dose-dependent manner. Neuroprotection was found to coincide with reductions in intracellular reactive oxygen species, lipid peroxidation, and DNA damage. In vivo, pretreatment with 0.5 mg/kg D-512 was protective against neurodegenerative phenotypes associated with systemic administration of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), including losses in striatal dopamine (DA), reductions in numbers of DAergic neurons in the substantia nigra (SN), and locomotor dysfunction. These observations strongly suggest that the multifunctional drug D-512 may constitute a novel viable therapy for PD.
Keywords: neuroprotection, Parkinson’s disease, MPTP, substantia nigra, 6-hydroxydopamine, dopamine agonist, oxidative stress, multifunctional drug
Introduction
Parkinson’s disease (PD) is the 2nd most common progressive neurodegenerative disorder after Alzheimer’s disease, mostly affecting the elderly population. The primary clinical hallmark of the disease is severe motor dysfunction. PD is clinically characterized by tremors, bradykinesia, rigidity and postural instability, all representative features of motor dysfunction characteristic of the disorder (Carlsson 1959, Parkinson 2002). Cardinal motor symptoms associated with the disease are due to the selective loss of dopaminergic neurons within the substantia nigra pars compacta (SNpc) (Barbeau 1962, Bertler & Rosengren 1959, Hornykiewicz & Kish 1987). Loss of these cells is associated with significant changes in oxidative stress markers (Hornykiewicz & Kish 1987, Sofic et al. 1992), increased iron accumulation (Jellinger et al. 1992, Jellinger et al. 1990), and accumulation of intracytoplasmic protein-rich inclusions called “Lewy bodies” (Braak et al. 2003, Forno 1996).
The etiology of PD has not been fully elucidated. Aging (Hornykiewicz 1989), environmental toxins (Langston et al. 1983, Tanner et al. 2011), mitochondrial dysfunction (Schapira 1993), and genetic mutations (Chartier-Harlin et al. 2004, Polymeropoulos et al. 1997, Singleton et al. 2003) have all been shown to increase the risk for PD. Genetic mutations, however, only account for 5–10% of PD cases (Lesage & Brice 2009). Excessive formation and/or lack of detoxification of destructive oxygen radicals and hydrogen peroxide (collectively referred as reactive oxygen species, “ROS”) in critical areas of the brain are associated with neuropathology in the more common sporadic form of the disorder, likely occurring as a consequence of aging and/or environmental exposures over a lifespan (Hornykiewicz & Kish 1987). Amongst the various organelles and enzymes that can generate ROS within the cell, mitochondria are responsible for more than 90% of ROS generation. Various environmental toxins associated with PD including rotenone, MPTP, and paraquat, all result in inhibition of mitochondrial complex I, leading to formation of defects in the electron transport system. Mitochondrial dysfunction caused by environmental toxins and/or aging itself may result in leakage of electrons and cellular energy deficiency. Leaked electrons contribute to the generation of ROS. Energy deficiency and ROS together likely contribute to PD cell death (Chinta & Andersen 2008, Jenner 2003). The selective vulnerability of dopaminergic neurons in PD implicates dopamine (DA) itself as another major contributing factor in disease initiation and progression. DA auto-oxidation as well as its metabolism by monoamine oxidase B (MAO-B) can yield 6-hydroxydopamine (6-OHDA) and dopamine quinones which can increase ROS generation (Linert & Jameson 2000). The iron content in the SNpc of PD patients has also been shown to be elevated (Jellinger et al. 1992, Jellinger et al. 1990). Iron can act to generate highly reactive hydroxyl radical via the Fenton reaction. ROS generated by these various factors are highly unstable and can instantaneously oxidize biomolecules in their vicinity. Post-mortem analyses of the SNpc from PD patients versus controls indicate significant elevations in lipid peroxides, DNA oxidation, and protein carbonyls, indirect markers of oxidative burden (Zecca et al. 2004). Loss of antioxidant capacity within the PD SNpc may also contribute to increased ROS and subsequent damage; for example, levels of total as well as reduced glutathione (a thiol tripeptide) have been shown to be significantly depleted in the SNpc of brains of PD patients (Sofic et al. 1992).
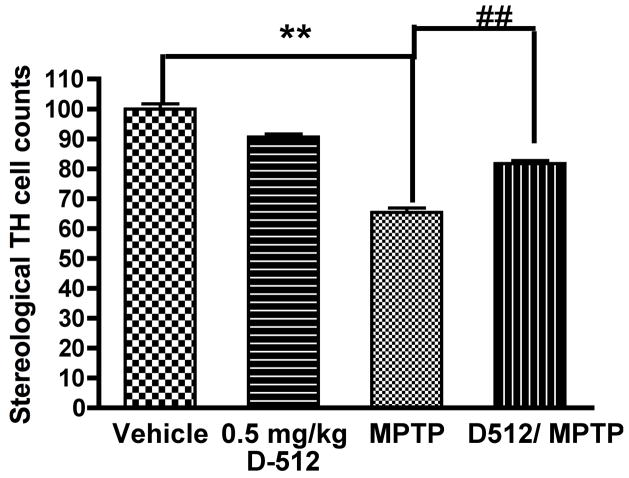
Currently available clinical therapy for PD targets restoration of DA levels within the nigrostriatal tract, preventing symptomatic effects associated with the disorder without addressing the underlying neuropathology. L-DOPA, the first FDA-approved drug treatment for PD which is still widely-utilized in patients with the disorder, is a precursor of DA that is converted in the brain by the enzyme dopa-decarboxylase (Cotzias et al. 1967). L-DOPA usage is unfortunately associated with side-effects including dyskinesia and its long-term use can produce sudden “on-off” effects (Marsden & Parkes 1976). L-DOPA has also been reported to increase levels of oxidative stress and to enhance disease progression (Basma et al. 1995, Fahn 1996). DA agonists including pramipexole and ropinirole are also widely used for treatment of the disease. They too provide only symptomatic relief and may only be helpful during the early phases of PD. The development of clinically viable drugs that act as disease-modifying agents rather than providing only symptomatic relief is therefore crucial for the treatment of this devastating disorder. PD is a complex disease with multiple pathogenic factors and thus it would be of great value to develop novel therapeutics that can act on various mechanisms associated with the overall disease process (Van der Schyf et al. 2007, Youdim 2010, Youdim 2013). In our continued efforts to discover multi-pronged therapeutics targeting multiple complex factors involved in PD neuropathology, we have developed a series of dopamine D2/D3 agonist compounds that possess potential antioxidant, iron-chelator, and neuroprotective properties (Li et al. 2010, Gogoi et al. 2011, Johnson et al. 2012). Here, we describe the evaluation of one of our lead compounds, D-512 (Figure 1), a novel highly potent D2/D3 receptor agonist, as a novel symptomatic and neuroprotective treatment agent for PD (Johnson et al. 2012). Recently, we have shown that D-512 significantly attenuates 6-OHDA- and MPP+-induced neurotoxicity in dopaminergic MN9D cells in a dose-dependent manner. Inhibition of caspase 3/7 activity and reductions in lipid peroxidation along with restoration of tyrosine hydroxylase levels in 6-OHDA-treated cells may partially explain D-512’s mechanism of action (Santra et al. 2013). In this current study, we further explore the neuroprotective effect of D-512 in an alternative cellular model, rat adrenal phaeochromocytoma PC12 cells (a rat pheochromocytoma line), against 6-OHDA-induced cytotoxicity, as well as possible mechanisms involved. 6-OHDA is a widely used toxin that mimics the generation of oxidative stress observed in PD. 6-OHDA induces neurotoxicity via its auto-oxidation and subsequent hydrogen peroxide generation (Blum et al. 2000, Soto-Otero et al. 2000). We have additionally carried out studies assessing the effects of pre-treatment with D-512 in an in vivo MPTP model of PD in terms of its ability to abrogate reductions in striatal DA levels, loss of DAergic SNpc neurons, and motor dysfunction associated with this model (Langston & Ballard 1983, Przedborski et al. 2000, Jackson-Lewis & Przedborski 2007).
Figure 1.
Molecular structure of D-512
Materials and Methods
Materials
PC12 Adh (ATCC® CRL1721.1™) cells, a rat adrenal pheochromocytoma cell line, were purchased from ATCC. RPMI 1640, heat-inactivated horse serum, fetal bovine serum, penicillin-streptomycin and trypsin were purchased from GIBCO. 6-hydroxydopamine hydrochloride, dimethyl sulfoxide, methyl thiazolyl blue tetrazolium bromide (MTT), thiobarbituric acid, 2′,7′-dichloro-fluorescein diacetate (DCF-DA), Dulbecco’s phosphate-buffered saline, Triton-x-100, ribonuclease A, and proteinase K were purchased from Sigma-Aldrich. Sodium nitroprusside (SNP) and isopropanol were purchased from Acros Organics. Ethanol and ethidium bromide were purchased from Fisher Scientific. Agarose was purchased from Invitrogen. Ammonium acetate was purchased from Lancaster Chemicals. BCA protein assay reagents and Hoechst 33342 dye were purchased from Thermo Fisher Scientific Inc. (Rockford, IL, USA).
Cell culture and treatments
Cells were cultured in T-75 flasks (Greiner Bio One, Frickenhausen, Germany) and maintained in RPMI 1640 medium supplemented with 10% heat-inactivated horse serum, 5% fetal bovine serum, 100U/mL penicillin, and 100ug/mL streptomycin at 37°C in 95% air/5% CO2. Stock solutions of D-512 and 6-hydroxydopamine were prepared in DMSO and aliquots were stored at −20°C and −80°C, respectively. A stock solution of sodium nitroprusside was prepared fresh in DI water before treatment. 10 mM stock solution of DCF-DA was prepared in methanol and stored at −20°C. For all experiments assessing neuroprotective effects of D-512, PC12 cells were pre-treated with indicated concentrations of D-512 for 24 hours and then co-treated with D-512 and 75 μM 6-OHDA for another 24 hours unless stated otherwise. Controls were treated with media containing 0.01% DMSO.
Measurement of cell viability
To determine the neuroprotective effect of D-512 on 6-OHDA-mediated cell death, a quantitative colorimetric MTT assay was performed. PC12 cells were plated at 17,000 cells/well density in 100 μL media in 96 well plates for 24 hours. Cells were treated with varying concentrations of either 6-OHDA or D-512 to determine their direct effect on cell viability and to determine the optimum concentration of 6-OHDA in subsequent neuroprotection experiments. Neuroprotection experiments were conducted by treating cells for 24 hours with varying concentrations of D-512, followed by their treatment with either 75 μM 6-OHDA alone (pre-treatment only) or with 75 μM 6-OHDA and varying concentrations of D-512 for another 24 hours (pre-treatment and co-treatment). After incubation, 5 mg/mL MTT solution (prepared in 1X PBS) was added to the cells (to a final concentration of 0.5 mg/mL) and the plates further incubated at 37°C in 95% air/5% CO2 atmosphere for 3–4 hours to produce dark blue formazan crystals. Afterwards, the plate was centrifuged at 1500 rpm (450 g) for 10 minutes and the supernatants carefully removed. Formazan crystals were dissolved by adding 100 μL of methanol:DMSO (1:1) mixture to each well and shaking at room temperature for 30 min. Absorbance values were measured on a microplate reader (Biotek Epoch, USA) at 570 nm with background correction performed at 690 nm. Data from at least 3 experiments were analyzed using Graphpad software (Version 4, San Diego, USA). Cell viability was defined as percentage reduction in absorbance compared to untreated controls.
Determination of intracellular ROS levels
The effect of D-512 on ROS levels was measured by 2′,7′-dichlorofluorescein diacetate (DCF-DA) assay, a fluorescence-based quantitative assay. Briefly, PC12 cells were seeded at 5X105 cells/well density in 2 mL media in 6 well plates for 24 hours to allow cell attachment. Adhered cells were treated with varying concentrations of D-512 for 24 hours followed by co-treatment with 100 μM of 6-OHDA for another 24 hours. For drug alone controls, cells were treated with varying concentrations of D-512 for 24 hours. After incubation, cells were scraped with a cell scraper, centrifuged and washed with 1X PBS. Cells were incubated with 1 mL of 10 μM DCF-DA prepared in serum free RPMI medium for 30 min. Cells were centrifuged and washed with 1X PBS (2 times) and re-suspended in 50 μL of 1X PBS. Cells were subjected to 2 freeze-thaw cycles then lysed via 3–10 sec pulses using an ultrasonicator (Branson Inc, Danbury, CT) at 50% amplitude. Whole cell lysates were centrifuged at 4°C for 10 min at 14,000 rpm (16,800 g) and supernatant collected. Protein concentration for each treatment group was determined by BCA protein assay and equal amount of protein was loaded into black 96-well plates and fluorescence of the loaded samples measured at 485 nm (excitation) and 520 (emission) using a microplate reader (Biotek Synergy, USA). Fluorescence units were expressed as percentage of untreated control cells.
Lipid peroxidation assay
Levels of lipid peroxidation were measured using the sodium nitroprusside (SNP) assay. For all experiments, PC12 cells were plated at 2X105 cells/well density in 2 mL media in 12 well plates for 24 hours. Adhered cells were pre-treated with different concentrations of D-512 for 24 hours followed by their co-treatment with 200 μM SNP and D-512 for 8 hours. Controls consisted of SNP (200 μM), drug (1 μM D-512) or DMSO (0.01%) alone in fresh media. Cells were harvested using a cell scraper, centrifuged, and washed with 1X PBS. Cells were resuspended in 120 μL 1X PBS. Suspended cells were sonicated via 3–5 sec pulses using an ultrasonicator (Branson Inc, Danbury, CT) at 30% amplitude. Whole cell lysates were used to determine thiobarbituric acid reactive species (TBARS). 100 μL 1% SDS and 100 μL whole cell lysate were mixed with 4 mL color reagent (prepared by mixing 320 mg thiobarbituric acid dissolved in 30 mL of 0.1M NaOH and 30 mL of 3.5 M diluted acetic acid. The mixture was boiled for 1 hour at 100°C in the dark and fluorescence read at 520 nm excitation and 550 nm emission wavelengths using a BioTek Synergy H-1 fluorescence plate reader. Fluorescence was plotted after subtracting the blank (prepared using 100 μL 1X PBS, 100 μL 1% SDS, and 4mL color reagent) and considering the control (consisting of 100 μL cell lysate without any treatment, 100 μL 1% SDS, and 4 mL color reagent) as 100%.
Hoechst staining
In order to assess levels of nuclear condensation, Hoechst 33342 staining was performed. PC12 cells were seeded in 48-well plates at a density of 3.5X104 cells/well. After incubation for 24 hours, medium was removed and 0.5 ml of fresh medium containing 10 μM D-512 added to 6-OHDA and drug-only groups. DMSO (0.01%) in fresh media was added to 6-OHDA only and untreated controls. Following 24 hours of pretreatment with the drug, 75 μM of 6-OHDA was added into the 6-OHDA-treated plates +/− drug and incubation continued for an additional 12 hours. Media was removed and cells washed twice with 1X PBS. Cells were fixed with 0.5 ml 4% paraformaldehyde solution (EM Sciences) for 15 min at room temperature, followed by washing twice with 1X PBS. The cells were stained with 0.5 μM Hoechst 33342 in 0.15% Triton-X-100 (0.5 ml) for 20 min at room temperature, followed by washing twice with 1X PBS. Cells were observed under fluorescence microscope at 40X magnification (EVOS FL digital inverted microscope, AMG) at 357 nm excitation and 447 nm emission wavelengths, respectively.
DNA fragmentation assay
To evaluate nuclear apoptotic damage, a DNA laddering assay was performed using the agarose gel electrophoresis method modified from Kotamraju et. al. 2000 (Kotamraju et al. 2000). 4X106 cells were plated in 100 mm petri-dishes in 10 mL media and allowed to adhere for 24 h. Adhered cells were then pre-treated with various concentrations of D-512 for 24 hours. Pre-treated cells were co-treated with 75 μM 6-OHDA and various concentrations of D-512 for an additional 24 hours. Cells were then trypsinized (1 mL trypsin), centrifuged at 2000 rpm (800 g) 5 min, and washed with 1X PBS at 2000 rpm (800 g) 5 min. Cell pellets were lysed using 100 μL lysis buffer (0.1% Triton-X-100 in 20 mM EDTA, 50 mM Tris-HCl, pH 7.5) for 5 minutes with intermittent pipetting. Cell debris was removed by centrifugation (3,000 rpm, 1800 g, 5 min) and supernatants treated with 10 μL of 10% SDS solution. Lysates were treated with 10 μL of 50 mg/mL RNase A for 2 h at 56°C followed by 12.5 μL of 20 mg/ml proteinase K for 2 h at 37°C. Resulting lysates were treated with 65 μL of 10 M ammonium acetate and 250 μL ice-cold isopropanol. After vigorous shaking, isopropanol precipitation was performed by incubating the lysates at −20°C for 3 days. Precipitated DNA was collected by centrifugation at 12000 rpm (12, 400 g) for 20 min. DNA was washed with 200 μL 80% ice-cold ethanol and air-dried for 10 min at room temperature. DNA was dissolved in 50 μL Tris-EDTA buffer. 4 μg (determined by UV absorbance) of DNA from each sample was separated on 1.2% agarose gels containing 0.5 μg/mL ethidium bromide at 5V/cm for 4 hours. Agarose gel images were taken using a Biorad Gel Doc XR+ imaging system.
In vivo MPTP and D512 administration
12-week-old male C57BL/6 mice (Jackson Labs, Bar Harbor, ME) used in this study were housed according to standard animal care protocols, kept on a 12 h light/dark cycle, and maintained in a pathogen-free environment in the Buck Institute vivarium. All experiments were approved by local IACUC review and conducted according to current NIH policies on the use of animals in research. For D512 studies, D-512 was diluted to a final dose of 0.5 mg/kg dissolved in saline and administered intraperitoneally (i.p.) to mice once daily for 5 days; control animals received saline vehicle. On day 4, mice were co i.p.-injected with either saline vehicle or 20 mg/kg MPTP, administered 12 h apart. D512 or vehicle were administered 30 min before each MPTP injection (Joyce et al. 2003).
Pole test
7 days post the final MPTP injection, locomoter behavior was monitored via the pole test. Briefly, animals were placed on top of a rough-surfaced wooden pole (50 cm in length and 1 cm in diameter) and allowed to descend to the base of the pole. Mice were initially habituated and trained the day prior to testing. On testing day, animals are placed head-up on the top of the pole. The time it takes for the animal to turn its head downwards and descend the entire length of the pole was taken. The best performance for each animal over five consecutive trials was subsequently recorded (Lieu et al., PLOS One 2013). The test was performed in at least triplicate for each individual animal, n=4 per condition.
HPLC assay of striatal dopamine levels
A subset of mice (n=4 per condition) were used for analysis of levels of striatal DA. Dissected striata (harvested 24 hours after the final MPTP injection) were sonicated and centrifuged in chilled 0.1 M perchloric acid (PCA, 100 μl/mg tissue). Supernatants were taken for measurements of dopamine by HPLC as described previously (Beal et al. 1990, Beal et al. 1992) Briefly, 15 μl supernatant was isocratically eluated through an 80 x 4.6 mm C18 column (ESA, Inc Chelmsford, MA) with a mobile phase containing 0.1 M LiH2PO4, 0.85 mM 1-octanesulfonic acid and 10% (v/v) methanol. DA was detected via a 2-channel Coulochem II electrochemical detector (ESA, Inc. Chelmsford, MA). Concentrations of DA are expressed as nanograms per milligram protein. Protein concentrations of tissue homogenates were measured according to the Bio-Rad protein analyze protocol (Bio-Rad Laboratories, Hercules, CA) using a Perkin Elmer Bio Assay Reader (Norwalk, CT) and used to normalize striatal DA levels.
HPLC assay of striatal MPP+ levels
MPP+ levels (nanograms per milligram of protein) were quantified by HPLC via UV detection using a Waters 2475 multifluorescence detector at excitation/emission wavelengths 295/375 nm, respectively. Striatal tissue was harvested from drug treated versus untreated animals 90 minutes following the last injection of 20 mg/kg MPTP intraperitoneally, immediately immersed in ice cold 0.1 M perchloric acid and sonicated. An aliquot was injected onto an analytical column (ESA Meta 250 x 4.6 cm, partial size 5 um, and pore size 100A) equipped with a SecurityGuard Phenomenex pre-column housed in a Waters column temperature controller TMC. Samples were eluted isocratically using a mobile phase consisting of 20 mM boric acid-sodium borate buffer containing 3 mM tetrabutylammonium hydrogen sulfate, 0.25 mM 1-heptanesulfonic acid, and 10% isopropanol, pH 8.0. The mobile phase was pumped isocratically using a Waters 1525 binary HPLC pump with the flow rate 0.8 ml/min. All instruments were controlled by Breeze2 software. Concentrations of MPP+ are expressed as nanograms per milligram of wet tissue.
Stereological assessment of DAergic SNpc cell numbers
A subset of mice (n=8 per condition) were subjected to cardiac perfusion with phosphate-buffered saline (PBS) followed by 4% paraformaldehyde at day 7 following the final MPTP injection. Brains were removed, dehydrated in 30% sucrose, and sectioned at 20 μm. Immunohistochemistry was performed using antibody against tyrosine hydroxylase (1:1000 TH, Chemicon, Temecula, CA) followed by biotin-labeled secondary antibody and development using DAB (Vector Labs, Burlingame, CA) to immunostain dopaminergic neurons. TH-positive cells in the SNpc were counted stereologically using the optical fractionator method (Kaur et al. 2003). Sections were cut at a 40 μm thickness, and every 4th section was counted using a grid of 100×100 μm. TH staining was verified by Nissl staining (Pilati et al. 2008).
Statistical analysis
Data are expressed as mean value ± standard error mean (SEM). For multiple groups, statistical significance was determined using one way analysis of variance (ANOVA) following Tukey’s Multiple Comparison post hoc test. In all cases P< 0.05 was considered as statistically significant.
Results
Effect of D-512 on in vitro 6-OHDA-induced neurotoxicity
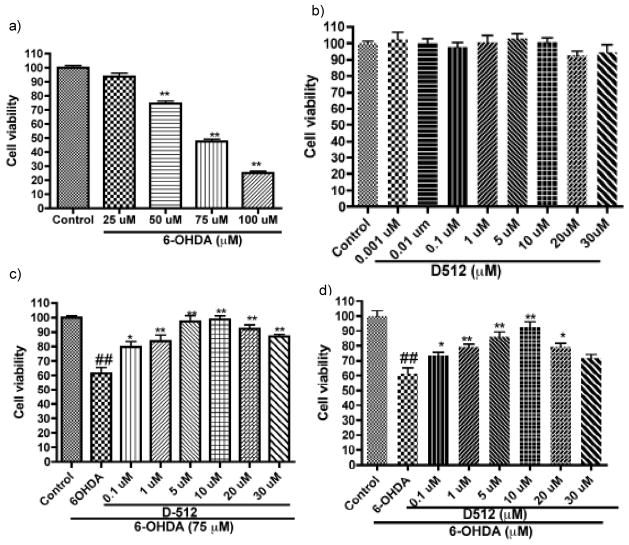
Treatment of PC12 cells with 6-OHDA for 24 h results in a significant dose-dependent neurotoxicity. Cell viability was significantly decreased ~50% in cells exposed to 75 μM 6-OHDA (Figure 2a); this concentration was used for all subsequent in vitro experiments. In contrast, cells treated with increasing concentrations of D-512 alone (0.001–30 μM) showed no significant cell loss compared to untreated control (Figure 2b). The potential neuroprotective effect of D-512 on 6-OHDA-induced toxicity was evaluated following either pre- or co-treatment. Following pre-treatment, cells exposed to D-512 for 24 h followed by exposure to 6-OHDA for 24 hours displayed significant prevention of PC12 cell loss at all concentrations (Figure 2c). Pre-treatment of cells with D-512 for 24 hours followed by co-treatment in the presence of 6-OHDA for an additional 24 hours also showed significant protection against 6-OHDA neurotoxicity (Figure 2d), although not significantly greater than pre-treatment alone. These data suggests that pre-treatment of cells with D-512 has a neuroprotective effect on PC12 cell loss induced by 6-OHDA.
Figure 2.
Dose-dependent effect of pretreatment as well as pretreatment followed by co-treatment of D-512 on cell viability of PC12 cells from toxicity induced by 75 μM 6-OHDA. (a) PC12 cells were treated with different concentrations of 6-OHDA (25 μM to 100 μM). (b) Dose-dependent effect of D-512 on cell viability. (c) PC12 cells were pretreated with different dosages of D-512 for 24 h followed by treatment with 75 μM 6-OHDA for 24 h. (d) PC12 cells were pretreated with different doses of D-512 for 24 h followed by co-treatment with 75 μM 6-OHDA for 24 h. Values shown are means ± SDs of three independent experiments performed in 4–6 replicates. One way ANOVA analysis (F (4,30) = 313.6, p < 0.0001 for 2a; F (8, 49) = 16.04, p < 0.0001) for 2c; F (8, 63) = 22.19, p < 0.0001 for 2d), followed by Tukey’s Multiple Comparison post hoc test were performed. **p<0.001 compared to the 6-OHDA or control groups; ##p<0.001 compared to the control group.
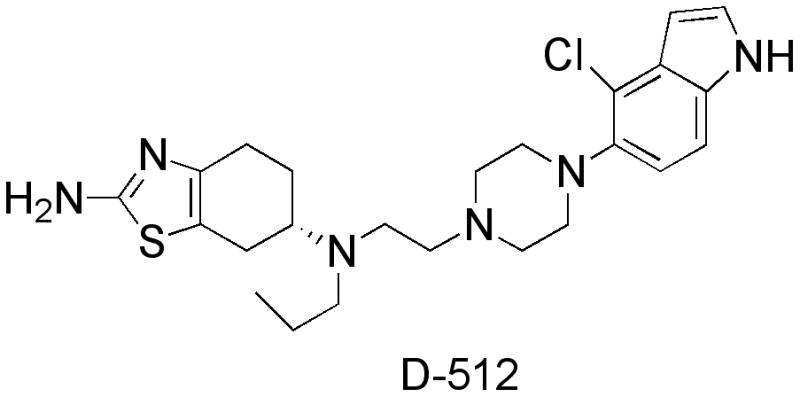
Effect of D-512 on in vitro 6-OHDA-induced intracellular ROS production
The oxidative conversion of cell permeable DCF-DA to fluorescent 2,7-dichlorodihydrofluorescein (DCFH) by 100 μM 6-OHDA was quantified as a measurement of increased ROS generation. As indicated in Figure 3b, treatment with 100 μM 6-OHDA produced a significant increase in fluorescence in these cells, almost two-fold relative to untreated controls. Cells pretreated with D-512 displayed a dose-dependent reduction of intracellular oxidative stress. Such reduction was significant (p< 0.001) at concentrations of 10 and 5 μM. In contrast, cells treated with increasing concentrations of D-512 alone for 24 h did not display significant ROS generation (Figure 3a).
Figure 3.
Effect of pretreatment with different concentrations of D-512 on ROS generation following treatment with 100 μM 6-OHDA in PC12 cells. (a) Dose-dependent effects of D-512 alone. (b) Cells were pretreated with D-512 for 24 h followed by co-treatment with 6-OHDA for another 24 h. Cells were then treated with 10 μM DCF-DA for 30 min and fluorescence intensity measured. Control data represents cells not treated with 6-OHDA and is represented as 100% with respect to the other groups. The values shown are means ± SDs of three independent experiments performed in triplicate or quadruple. One way ANOVA analysis (F (4,10) = 25.50, p < 0.0001) followed by Bonferroni’s Multiple Comparison post hoc test were performed. ##p<0.001 compared to the control group; **p<0.001 compared to the 6-OHDA + drug group.
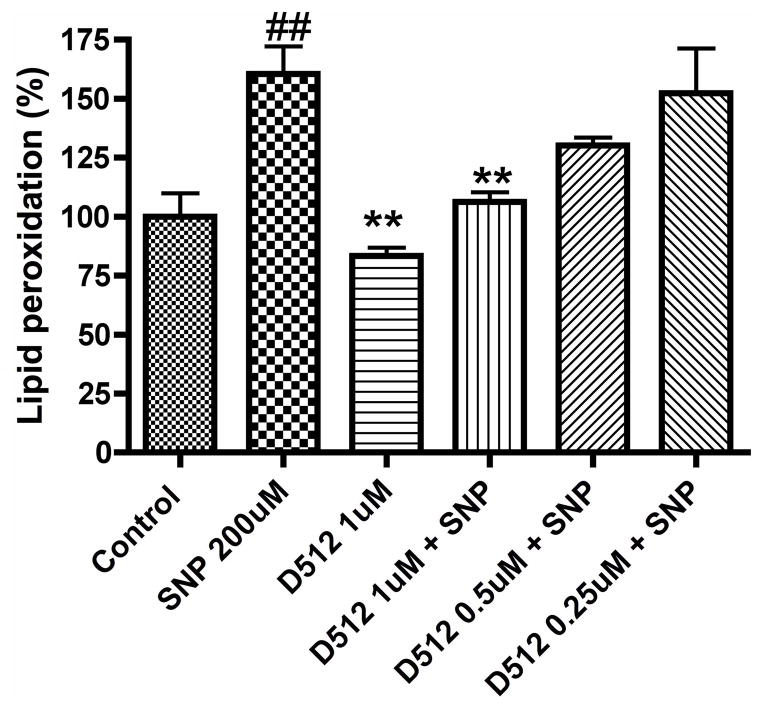
Effect of D-512 on in vitro sodium nitroprusside-induced lipid peroxidation by TBARs assay
We utilized SNP to generate lipid peroxidation as 6-OHDA does not induce lipid peroxidation in PC12 cells on its own (data not shown). We observed that 200 μM SNP was able to induce a 60% increase in lipid peroxidation compared to untreated control cells. Treatment with D-512 showed dose-dependent effect in preventing the lipid peroxidation induced by SNP in a dose-dependent manner; treatment with 1 μM of the drug prevented ~90% of the induced lipid peroxidation whereas 0.5 μM D-512 and 0.25 μM D-512 showed 60% and approximately 40% prevention against SNP-induced lipid peroxidation, respectively (although the latter is not statistically significant, Figure 4).
Figure 4.
Effect of pretreatment with different concentrations of D-512 on production of thiobarbituric acid reactive substances production induced by SNP (200 μM). Control data represents cells not treated with SNP and is represented as 100% with respect to the other groups. The values shown are means ± SDs of three independent experiments performed in triplicate or quadruple. One way ANOVA analysis (F (5, 10) = 7.984, p < 0.0029) followed by Bonferroni’s Multiple Comparison post hoc test were performed. ##p<0.01 compared to the control group; **p<0.05 compared to the SNP + drug group.
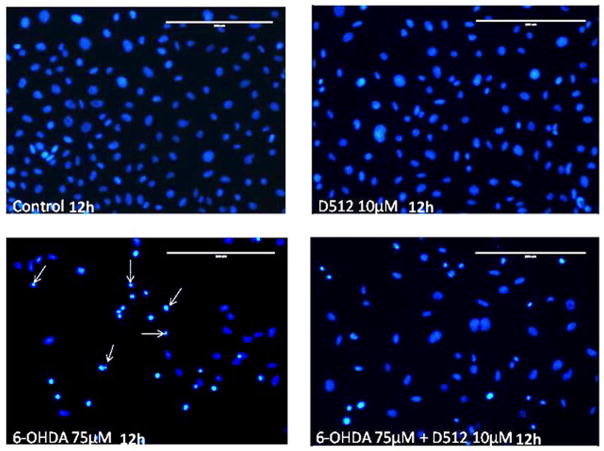
Effect of D-512 on in vitro 6-OHDA induced nuclear morphology
Nuclear morphology is one of the characteristic features of cell integrity. 6-OHDA-mediated changes in the nuclear morphology of PC12 cells pre-treated with D-512 versus untreated controls was assessed by Hoechst 33342 staining. Control cells showed homogeneous staining of their nuclei without any abnormalities, whereas cells treated with 6-OHDA alone showed signs of nuclear condensation; while 10 μM D-512 alone does not alter nuclear morphology compared to control cells, this dosage was found to reduce the nuclear condensation of 6-OHDA treated cells (Figure 5a).
Figure 5.
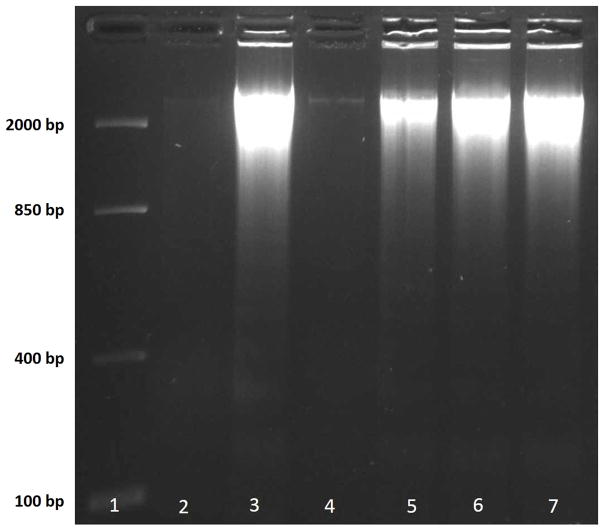
(a) Effect of D-512 on 6-OHDA-induced nucleic condensation. Apoptotic nuclei were visualized via fluorescence dye 33342 staining. Apoptotic cells with high fluorescence intensity are indicated by arrows. Scale bar: 200 μm. (b) Effect of pretreatment with varying concentration of D-512 followed by co-treatment with 75 μM 6-OHDA on DNA fragmentation in PC12 cells. Lanes 1–4: marker, DNA laddering of control cells, DNA laddering in response to 75 μM 6-OHDA alone, or 10 μM D-512 alone. Lanes 5–7: DNA laddering in response to pretreatment with varying concentrations of D-512 (10 μM, 5 μM and 1 μM) along with co-treatment with 75 μM 6-OHDA + 10 μM D-512, 75 μM 6-OHDA + 5 μM D-512, or 75 μM 6-OHDA + 1 μM D-512.
Effect of D-512 on in vitro 6-OHDA induced DNA fragmentation
DNA fragmentation is a hallmark feature of apoptosis. We assessed the effect of D-512 treatment on 6-OHDA-induced DNA fragmentation. In contrast to PC12 cells treated with 6-OHDA, control cells and cells treated with D-512 alone did not display fragmented DNA. D-512 was found to prevent fragmentation of DNA in 6-OHDA treated PC12 in a dose-dependent manner (Figure 5b and supplementary material).
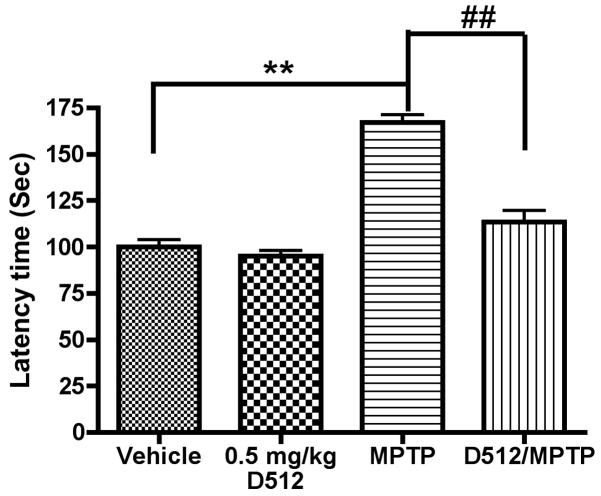
D-512 treatment improves behavioral performance in MPTP-treated mice
To test the impact of D-512 on motor coordination, mice were assessed 7 days following final MPTP administration in the absence and presence of D-512 treatment as described using the pole test. Latency for mice to reach the bottom of the pole was increased by more than 170% in the MPTP-treated mice (p < 0.001) compared to control animals. Pretreatment with D-512 at a dosage of 0.5 mg/kg for three days followed by 2 days of co-treatment with MPTP was found to significantly attenuate motor function impairment (p < 0.001) (Figure 6). Effect of D-512 alone was indistinguishable from control animals.
Figure 6.
Effect of D512 on motor coordination and balance in the pole test. One way ANOVA analysis (F (3, 12) = 58.22, p < 0.0001) indicates *p<0.001 between vehicle/sal and veh/MPTP; # p<0.001 between veh/MPTP and D512/MPTP (n=4).
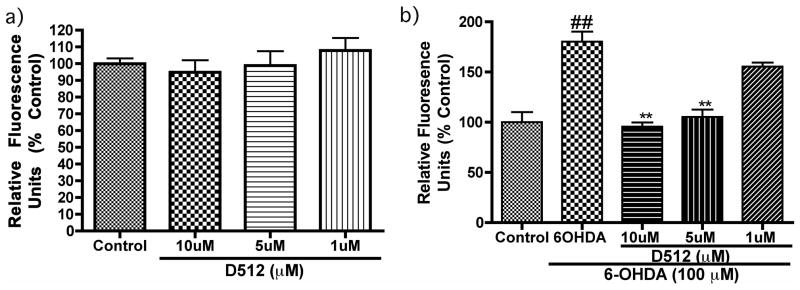
D-512 protects against MPTP-induced depletion of striatal DA content
As previously shown by ourselves (Kaur et al. 2003, Lee et al. 2009), treatment with MPTP using this dosage regime was found to result in 60% depletion in striatal DA levels compared to controls. Treatment with 0.5 mg/kg D-512 however was effective in significantly abrogating striatal DA depletion compared to the MPTP-treated group (~24% reduction in loss of DA in the drug treated group, p<0.01, Figure 7a).
Figure 7.
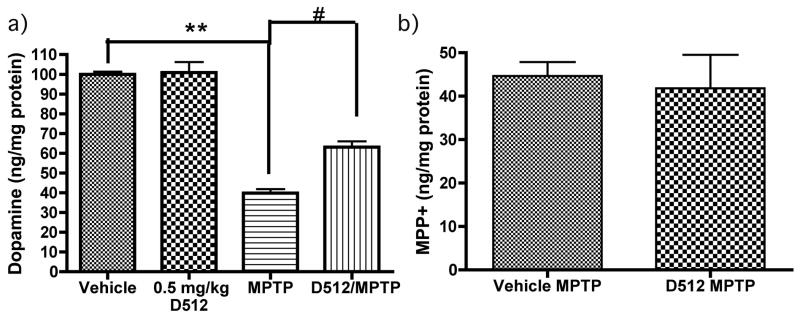
a.) Effect of pretreatment of 0.5 mg/kg D512 for three days followed by two days co-treatment with MPTP (20 mg/kg, 12 h apart) on striatal DA levels. One way ANOVA analysis (F (3, 9) = 74.59, p < 0.0001) ** p < 0.001 between vehicle/Sal and Vehicle/MPTP; # p<0.01 between D512/MPTP and Vehicle/MPTP (n=4). (b) MPP+ levels were measured in striatal tissues collected from C57BL 6 mice treated with vehicle MPTP or D512 MPTP. Tissue was harvested 90 min post-MPTP injection (20 mg/kg) and analyzed via HPLC with electrochemical detection. Values are presented as ng MPP+/mg protein, n = 4 per treatment condition.
D-512 does not alter metabolism of MPTP
Our HPLC data demonstrates that the levels of striatal MPP+ is not altered in D-512 treated mice compared to MPTP treated mice alone (Figure 7b), indicating an absence of effect of D-512 on MPTP metabolism.
D-512 protects against MPTP- induced SNpc DAergic cell loss
As previously demonstrated by ourselves (Lee et al. 2009, Kaur et al. 2003), treatment with MPTP using this dosage regime conferred a significant (~35%) loss of DAergic SNpc neurons compared to saline-treated controls (p<0.001, Figure 8a). Treatment with D-512 followed by exposure to MPTP resulted in a significant effect on DAergic cell loss in this brain region (~19% loss of DAergic SN neurons in the drug treated group, p<0.001).
Figure 8.
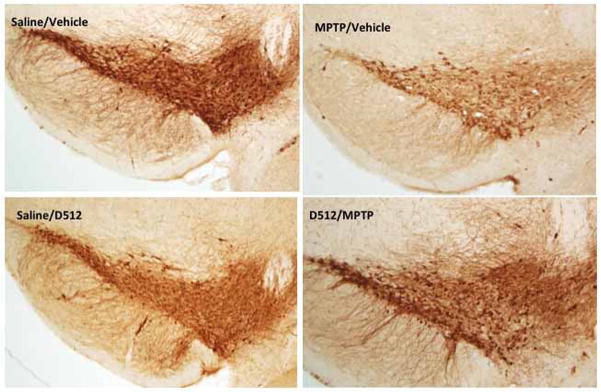
(a) Stereological quantification of TH-positive DAergic cell counts within the SNpc. One way ANOVA analysis (F (3, 24) = 117.2, p <0.0001) indicates ** p < 0.001 between Vehicle/Sal and Vehicle/MPTP; ## p < 0.001 between D512/MPTP and Vehicle/MPTP D512 at 0.5mg/Kg concentration (n=8). (b) Representative photomicrographs of the SN with TH immunohistochemistry (10X).
Discussion
In our recent publications, we have shown that newly developed D2/D3 agonists may act as both symptomatic and neuroprotective agents for the treatment of PD (Biswas et al. 2008, Li et al. 2010, Gogoi et al. 2011). In this regard, we have recently characterized the neuroprotective effects of two lead compounds, D-512 and D-440, via assessment of their effects on neurotoxicity associated with 6-OHDA and MPP+ administration in DAergic MN9D cells (Santra et al. 2013). We have now begun to further explore the possible mechanisms underlying D-512’s neuroprotective effects in several additional studies. We have reported that D-512 inhibits the activity of apoptotic enzymes caspase 3/7 and restores the loss of tyrosine hydroxylase levels induced by the treatment with 6-OHDA in vitro. In order to better understand the scope of neuroprotection induced by D-512, we have carried out additional in vitro and in vivo experiments.
Oxidative stress has been strongly implicated in neurodegeneration associated with PD. 6-OHDA is a neurotoxin that produces oxidative stress in both in vitro and in vivo experimental PD models (Soto-Otero et al. 2000). 6-OHDA has been demonstrated to induce apoptosis in PC12 cells via release of cytochrome c and activation of caspase-3 (Ochu et al. 1998). In order to further validate our results on the neuroprotective effects of D-512 in MN9D cells, we carried out additional experiments using PC12 cells. 6-OHDA produces dose-dependent toxicity in PC12 cells, with 75 μM producing ~50% cell loss (Figure 2a). D-512 alone was found to have no effect on cell viability (Figure 2b). Interestingly, this lack of effect of different doses of D-512 on cell proliferation is different from the drugs effect in MN9D cells where a significant cell proliferation occurred at higher concentrations of the drug (Santra et al. 2013). Compounds with trophic factor properties have been shown to induce cell proliferation in MN9D cells (Signore et al. 2006). The fact that we do not observe any D-512-induced cell proliferation in PC12 cells underscores an important difference between the two cell types. D512 was found to be neuroprotective against 6-OHDA toxicity following both pre-treatment and co-treatment or pre-treatment alone (Figures 2c, 2d) in PC12 cells. Thus, our current data establish the neuroprotective property of D-512 beyond a single specific DAergic cell line.
In our earlier study, we demonstrated that D-512 has potent in vitro antioxidant activity using the 2,2-diphenyl-1-picrylhydrazyl (DPPH) assay (Johnson et al. 2012). In our current study, the capacity for D-512 to reduce intracellular ROS levels was assessed via the DCF-DA assay. As described in Figure 3b, as assessed by DCFH fluorescence, dose-dependent pretreatment with D-512 reduced the production of ROS generated by 6-OHDA. Treatment with drug alone however did not alter the levels of ROS compared to untreated controls (Figure 3a). These results suggest that D-512 is able to inhibit ROS produced by 6-OHDA. This may be due to its ability to either scavenge free radical species, or by enhancing the endogenous cellular antioxidant defense system, or a combination of both processes. In our efforts to further ascertain the anti-oxidant activity of D-512, a cell-based lipid peroxidation assay was carried out using sodium nitroprusside (SNP), a strong oxidizing agent. As shown in Figure 4, D-512 reduced lipid peroxidation induced by 200 μM SNP in a dose-dependent manner. These results further strengthened the suggestion that D-512 is capable of neutralizing cellular ROS, thereby decreasing oxidative stress.
Oxidative stress can lead to DNA damage including fragmentation. Treatment with 6-OHDA has been previously shown to cause nuclear chromatin condensation and DNA fragmentation (Kim et al. 2011). In our hands, treatment of PC12 cells with 6-OHDA for 24 hours produced significant nuclear condensation compared to controls as assessed by Hoechst 33342 staining (Figure 5a). Pretreatment with D-512 reduced this significantly. Treatment with drug alone produced a similar profile as control, indicating no effects on DNA. Further DNA laddering experiments validated these findings. As shown in Figure 5b, 6-OHDA caused a significant fragmentation of DNA, while untreated control cells displayed no DNA fragmentation (Lane 2 and 3). Pretreatment with D-512 produced a dose-dependent reduction of DNA fragmentation with the highest dose (10 μM) producing the greatest effect (Lane 5, 6 and 7). Pretreatment with D-512 alone did not produce any DNA fragmentation (Lane 4).
To further validate the neuroprotective effects of D-512 noted in our in vitro studies, we carried out additional in vivo neuroprotection studies using the well-characterized MPTP mouse model. Systemic administration of MPTP results in selective destruction of DAergic SNpc neurons in both primates and rodents resulting in an acute Parkinsonism phenotype (Lee et al. 2009, Przedborski et al. 2004). MPTP has been demonstrated to exert its neurotoxic effect via selective inhibition of mitochondrial complex I activity resulting in both a reduction in ATP synthesis and accumulation of reactive oxygen species. MPTP reproduces many hallmark symptoms of the disease, including inhibition of mitochondrial complex I activity, decreased GSH and increased oxidative stress levels in the SN, preferential neurodegeneration of the DAergic nigrostriatal system, striatal DA depletion, and motor control deficits. The MPTP mouse model is currently widely used to study the disease (Kaur et al. 2003).
As shown in Figures 6, pretreatment with D-512 improved MPTP-mediated effects on locomotor behavior as assessed by the pole test. Results from the pole test indicate that pretreatment with D-512 improves motor coordination as measured by a greater than 50% decrease in latency time compared to MPTP-only treated controls. This result clearly demonstrates that D-512 provides potent protection of motor function against the neurotoxic effects of MPTP. As shown in Figure 7A, neurochemical analysis of the striatum revealed significant protection (>24%) against MPTP-mediated losses in striatal DA content in the group pretreated with D-512 followed by MPTP compared to the MPTP-alone treated group. Protection against striatal DAergic loss correlated well with immunohistochemical analysis of numbers of DAergic SN cells in the D-512 pre-treatment group compared to the MPTP-only group (Figure 8a–b). In order to assess whether D-512 had any effect on metabolism of MPTP to its neurotoxic metabolite MPP+, we evaluated the level of MPP+ in both drug treated/MPTP and control MPTP groups. The results indicate that D-512 did not influence the metabolic conversion of MPTP to MPP+ demonstrating that neuroprotection conferred by D-512 is not due to alterations in production of MPP+. It is important to note that the anti-parkinsonian effect of D-512 was exhibited at a dosage comparable to that used in the current MPTP study (Santra et al. 2013). This is highly relevant in the context of our multifunctional drug development approach to address both symptomatic (relieving motor dysfunction) and development of disease-modifying neuroprotective effects to slow or stop the progression of the disease.
Conclusion
We have shown that D-512 is neuroprotective in an in vitro model of DAergic neurons (PC12 cells) treated with the neurotoxin 6-OHDA. In our effort to understand the mechanisms underlying this protection, we carried out further in vitro studies with the drug. In both DCF-DA and lipid peroxidation assays, D-512 was found to be an inhibitor of ROS production, confirming its potent antioxidant activity. This may be mediated by the ability of the compound to scavenge ROS or by enhancing endogenous cellular antioxidant defense systems. Pretreatment with D-512 was also found to prevent nuclear condensation and DNA fragmentation, consistent with its ability to inhibit apoptotic mechanisms. Further in vivo studies using the mouse MPTP administration model demonstrated that D-512 conferred significant protection in terms of both loss of DAergic SNpc neurons and locomotor behavior associated with MPTP. These results validate the multifunctional symptomatic and potential disease-modifying properties of D-512.
Supplementary Material
Acknowledgments
This work is supported by National Institute of Neurological Disorders and Stroke/National Institute of Health (NS047198, AKD).
This work was funded by NIH/NINDS (grant number NS047198):
Footnotes
The authors have no conflicts of interest to declare.
References
- Barbeau A. The pathogenesis of Parkinson’s disease: a new hypothesis. Can Med Assoc J. 1962;87:802–807. [PMC free article] [PubMed] [Google Scholar]
- Basma AN, Morris EJ, Nicklas WJ, Geller HM. L-dopa cytotoxicity to PC12 cells in culture is via its autoxidation. J Neurochem. 1995;64:825–832. doi: 10.1046/j.1471-4159.1995.64020825.x. [DOI] [PubMed] [Google Scholar]
- Beal MF, Matson WR, Storey E, Milbury P, Ryan EA, Ogawa T, Bird ED. Kynurenic acid concentrations are reduced in Huntington’s disease cerebral cortex. Journal of the neurological sciences. 1992;108:80–87. doi: 10.1016/0022-510x(92)90191-m. [DOI] [PubMed] [Google Scholar]
- Beal MF, Matson WR, Swartz KJ, Gamache PH, Bird ED. Kynurenine pathway measurements in Huntington’s disease striatum: evidence for reduced formation of kynurenic acid. J Neurochem. 1990;55:1327–1339. doi: 10.1111/j.1471-4159.1990.tb03143.x. [DOI] [PubMed] [Google Scholar]
- Bertler A, Rosengren E. Occurrence and distribution of dopamine in brain and other tissues. Experientia. 1959;15:10–11. doi: 10.1007/BF02157069. [DOI] [PubMed] [Google Scholar]
- Biswas S, Hazeldine S, Ghosh B, Parrington I, Kuzhikandathil E, Reith ME, Dutta AK. Bioisosteric heterocyclic versions of 7-{[2-(4-phenyl-piperazin-1-yl)ethyl]propylamino}-5,6,7,8-tetrahydronaphthalen-2- ol: identification of highly potent and selective agonists for dopamine D3 receptor with potent in vivo activity. J Med Chem. 2008;51:3005–3019. doi: 10.1021/jm701524h. [DOI] [PubMed] [Google Scholar]
- Blum D, Torch S, Nissou MF, Benabid AL, Verna JM. Extracellular toxicity of 6-hydroxydopamine on PC12 cells. Neurosci Lett. 2000;283:193–196. doi: 10.1016/s0304-3940(00)00948-4. [DOI] [PubMed] [Google Scholar]
- Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24:197–211. doi: 10.1016/s0197-4580(02)00065-9. [DOI] [PubMed] [Google Scholar]
- Carlsson A. The occurrence, distribution and physiological role of catecholamines in the nervous system. Pharmacol Rev. 1959;11:490–493. [PubMed] [Google Scholar]
- Chartier-Harlin MC, Kachergus J, Roumier C, et al. Alpha-synuclein locus duplication as a cause of familial Parkinson’s disease. Lancet. 2004;364:1167–1169. doi: 10.1016/S0140-6736(04)17103-1. [DOI] [PubMed] [Google Scholar]
- Chinta SJ, Andersen JK. Redox imbalance in Parkinson’s disease. Biochim Biophys Acta. 2008;1780:1362–1367. doi: 10.1016/j.bbagen.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotzias GC, Van Woert MH, Schiffer LM. Aromatic amino acids and modification of parkinsonism. N Engl J Med. 1967;276:374–379. doi: 10.1056/NEJM196702162760703. [DOI] [PubMed] [Google Scholar]
- Fahn S. Is levodopa toxic? Neurology. 1996;47:S184–195. doi: 10.1212/wnl.47.6_suppl_3.184s. [DOI] [PubMed] [Google Scholar]
- Forno LS. Neuropathology of Parkinson’s disease. J Neuropathol Exp Neurol. 1996;55:259–272. doi: 10.1097/00005072-199603000-00001. [DOI] [PubMed] [Google Scholar]
- Gogoi S, Antonio T, Rajagopalan S, Reith M, Andersen J, Dutta AK. Dopamine D(2)/D(3) agonists with potent iron chelation, antioxidant and neuroprotective properties: potential implication in symptomatic and neuroprotective treatment of Parkinson’s disease. ChemMedChem. 2011;6:991–995. doi: 10.1002/cmdc.201100140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornykiewicz O. Ageing and neurotoxins as causative factors in idiopathic Parkinson’s disease--a critical analysis of the neurochemical evidence. Prog Neuropsychopharmacol Biol Psychiatry. 1989;13:319–328. doi: 10.1016/0278-5846(89)90121-8. [DOI] [PubMed] [Google Scholar]
- Hornykiewicz O, Kish SJ. Biochemical pathophysiology of Parkinson’s disease. Adv Neurol. 1987;45:19–34. [PubMed] [Google Scholar]
- Jackson-Lewis V, Przedborski S. Protocol for the MPTP mouse model of Parkinson’s disease. Nat Protoc. 2007;2:141–151. doi: 10.1038/nprot.2006.342. [DOI] [PubMed] [Google Scholar]
- Jellinger K, Kienzl E, Rumpelmair G, Riederer P, Stachelberger H, Ben-Shachar D, Youdim MB. Iron-melanin complex in substantia nigra of parkinsonian brains: an x-ray microanalysis. J Neurochem. 1992;59:1168–1171. doi: 10.1111/j.1471-4159.1992.tb08362.x. [DOI] [PubMed] [Google Scholar]
- Jellinger K, Paulus W, Grundke-Iqbal I, Riederer P, Youdim MB. Brain iron and ferritin in Parkinson’s and Alzheimer’s diseases. J Neural Transm Park Dis Dement Sect. 1990;2:327–340. doi: 10.1007/BF02252926. [DOI] [PubMed] [Google Scholar]
- Jenner P. Oxidative stress in Parkinson’s disease. Ann Neurol. 2003;53(Suppl 3):S26–36. doi: 10.1002/ana.10483. discussion S36-28. [DOI] [PubMed] [Google Scholar]
- Johnson M, Antonio T, Reith ME, Dutta AK. Structure-activity relationship study of N(6)-(2-(4-(1H-Indol-5-yl)piperazin-1-yl)ethyl)-N(6)-propyl-4,5,6,7-tetrahydroben zo[d]thiazole-2,6-diamine analogues: development of highly selective D3 dopamine receptor agonists along with a highly potent D2/D3 agonist and their pharmacological characterization. J Med Chem. 2012;55:5826–5840. doi: 10.1021/jm300268s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce JN, Presgraves S, Renish L, Borwege S, Osredkar T, Hagner D, Replogle M, PazSoldan M, Millan MJ. Neuroprotective effects of the novel D3/D2 receptor agonist and antiparkinson agent, S32504, in vitro against 1-methyl-4-phenylpyridinium (MPP+) and in vivo against 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP): a comparison to ropinirole. Exp Neurol. 2003;184:393–407. doi: 10.1016/s0014-4886(03)00353-4. [DOI] [PubMed] [Google Scholar]
- Kaur D, Yantiri F, Rajagopalan S, et al. Genetic or pharmacological iron chelation prevents MPTP-induced neurotoxicity in vivo: a novel therapy for Parkinson’s disease. Neuron. 2003;37:899–909. doi: 10.1016/s0896-6273(03)00126-0. [DOI] [PubMed] [Google Scholar]
- Kim MK, Kim SC, Kang JI, et al. 6-Hydroxydopamine-induced PC12 cell death is mediated by MEF2D down-regulation. Neurochemical research. 2011;36:223–231. doi: 10.1007/s11064-010-0309-x. [DOI] [PubMed] [Google Scholar]
- Kotamraju S, Konorev EA, Joseph J, Kalyanaraman B. Doxorubicin-induced apoptosis in endothelial cells and cardiomyocytes is ameliorated by nitrone spin traps and ebselen. Role of reactive oxygen and nitrogen species. J Biol Chem. 2000;275:33585–33592. doi: 10.1074/jbc.M003890200. [DOI] [PubMed] [Google Scholar]
- Langston JW, Ballard P, Tetrud JW, Irwin I. Chronic Parkinsonism in humans due to a product of meperidine-analog synthesis. Science. 1983;219:979–980. doi: 10.1126/science.6823561. [DOI] [PubMed] [Google Scholar]
- Langston JW, Ballard PA., Jr Parkinson’s disease in a chemist working with 1-methyl-4-phenyl-1,2,5,6-tetrahydropyridine. N Engl J Med. 1983;309:310. doi: 10.1056/nejm198308043090511. [DOI] [PubMed] [Google Scholar]
- Lee DW, Rajagopalan S, Siddiq A, Gwiazda R, Yang L, Beal MF, Ratan RR, Andersen JK. Inhibition of prolyl hydroxylase protects against 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced neurotoxicity: model for the potential involvement of the hypoxia-inducible factor pathway in Parkinson disease. J Biol Chem. 2009;284:29065–29076. doi: 10.1074/jbc.M109.000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesage S, Brice A. Parkinson’s disease: from monogenic forms to genetic susceptibility factors. Hum Mol Genet. 2009;18:R48–59. doi: 10.1093/hmg/ddp012. [DOI] [PubMed] [Google Scholar]
- Li C, Biswas S, Li X, Dutta AK, Le W. Novel D3 dopamine receptor-preferring agonist D-264: Evidence of neuroprotective property in Parkinson’s disease animal models induced by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine and lactacystin. J Neurosci Res. 2010;88:2513–2523. doi: 10.1002/jnr.22405. [DOI] [PubMed] [Google Scholar]
- Linert W, Jameson GN. Redox reactions of neurotransmitters possibly involved in the progression of Parkinson’s Disease. J Inorg Biochem. 2000;79:319–326. doi: 10.1016/s0162-0134(99)00238-x. [DOI] [PubMed] [Google Scholar]
- Marsden CD, Parkes JD. “On-off” effects in patients with Parkinson’s disease on chronic levodopa therapy. Lancet. 1976;1:292–296. doi: 10.1016/s0140-6736(76)91416-1. [DOI] [PubMed] [Google Scholar]
- Ochu EE, Rothwell NJ, Waters CM. Caspases mediate 6-hydroxydopamine-induced apoptosis but not necrosis in PC12 cells. J Neurochem. 1998;70:2637–2640. doi: 10.1046/j.1471-4159.1998.70062637.x. [DOI] [PubMed] [Google Scholar]
- Parkinson J. An essay on the shaking palsy. 1817. J Neuropsychiatry Clin Neurosci. 2002;14:223–236. doi: 10.1176/jnp.14.2.223. discussion 222. [DOI] [PubMed] [Google Scholar]
- Pilati N, Barker M, Panteleimonitis S, Donga R, Hamann M. A rapid method combining Golgi and Nissl staining to study neuronal morphology and cytoarchitecture. J Histochem Cytochem. 2008;56:539–550. doi: 10.1369/jhc.2008.950246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polymeropoulos MH, Lavedan C, Leroy E, et al. Mutation in the alpha-synuclein gene identified in families with Parkinson’s disease. Science. 1997;276:2045–2047. doi: 10.1126/science.276.5321.2045. [DOI] [PubMed] [Google Scholar]
- Przedborski S, Jackson-Lewis V, Djaldetti R, Liberatore G, Vila M, Vukosavic S, Almer G. The parkinsonian toxin MPTP: action and mechanism. Restor Neurol Neurosci. 2000;16:135–142. [PubMed] [Google Scholar]
- Przedborski S, Tieu K, Perier C, Vila M. MPTP as a mitochondrial neurotoxic model of Parkinson’s disease. J Bioenerg Biomembr. 2004;36:375–379. doi: 10.1023/B:JOBB.0000041771.66775.d5. [DOI] [PubMed] [Google Scholar]
- Santra S, Xu L, Shah M, Johnson M, Dutta A. D-512 and D-440 as Novel Multifunctional Dopamine Agonists: Characterization of Neuroprotection Properties and Evaluation of In Vivo Efficacy in a Parkinson’s Disease Animal Model. ACS Chem Neurosci. 2013 doi: 10.1021/cn400106n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schapira AH. Mitochondrial complex I deficiency in Parkinson’s disease. Adv Neurol. 1993;60:288–291. [PubMed] [Google Scholar]
- Signore AP, Weng Z, Hastings T, Van Laar AD, Liang Q, Lee YJ, Chen J. Erythropoietin protects against 6-hydroxydopamine-induced dopaminergic cell death. J Neurochem. 2006;96:428–443. doi: 10.1111/j.1471-4159.2005.03587.x. [DOI] [PubMed] [Google Scholar]
- Singleton AB, Farrer M, Johnson J, et al. alpha-Synuclein locus triplication causes Parkinson’s disease. Science. 2003;302:841. doi: 10.1126/science.1090278. [DOI] [PubMed] [Google Scholar]
- Sofic E, Lange KW, Jellinger K, Riederer P. Reduced and oxidized glutathione in the substantia nigra of patients with Parkinson’s disease. Neurosci Lett. 1992;142:128–130. doi: 10.1016/0304-3940(92)90355-b. [DOI] [PubMed] [Google Scholar]
- Soto-Otero R, Mendez-Alvarez E, Hermida-Ameijeiras A, Munoz-Patino AM, Labandeira-Garcia JL. Autoxidation and neurotoxicity of 6-hydroxydopamine in the presence of some antioxidants: potential implication in relation to the pathogenesis of Parkinson’s disease. J Neurochem. 2000;74:1605–1612. doi: 10.1046/j.1471-4159.2000.0741605.x. [DOI] [PubMed] [Google Scholar]
- Tanner CM, Kamel F, Ross GW, et al. Rotenone, paraquat, and Parkinson’s disease. Environ Health Perspect. 2011;119:866–872. doi: 10.1289/ehp.1002839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Schyf CJ, Mandel S, Geldenhuys WJ, et al. Novel multifunctional anti-Alzheimer drugs with various CNS neurotransmitter targets and neuroprotective moieties. Curr Alzheimer Res. 2007;4:522–536. doi: 10.2174/156720507783018226. [DOI] [PubMed] [Google Scholar]
- Youdim MB. Why do we need multifunctional neuroprotective and neurorestorative drugs for Parkinson’s and Alzheimer’s disorders? Rambam Maimonides Med J. 2010;1:e0011. doi: 10.5041/RMMJ.10011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youdim MB. Multi target neuroprotective and neurorestorative anti-Parkinson and anti-Alzheimer drugs ladostigil and m30 derived from rasagiline. Exp Neurobiol. 2013;22:1–10. doi: 10.5607/en.2013.22.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zecca L, Youdim MB, Riederer P, Connor JR, Crichton RR. Iron, brain ageing and neurodegenerative disorders. Nat Rev Neurosci. 2004;5:863–873. doi: 10.1038/nrn1537. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.