Abstract
Background/Objectives
It has been hypothesized that assuming most of the caloric intake later in the day leads to metabolic disadvantages, but few studies are available on this topic. Aim of our study was to prospectively examine whether eating more of the daily caloric intake at dinner leads to an increased risk of obesity, hyperglycemia, metabolic syndrome, and non-alcoholic fatty liver disease (NAFLD).
Subjects/Methods
1245 non-obese, non-diabetic middle-aged adults from a population-based cohort underwent a 3-day food record questionnaire at enrollment. Anthropometric values, blood pressure, blood metabolic variables, and estimated liver fat were measured at baseline and at 6-year follow-up.
Design
Prospective cohort study.
Results
Subjects were divided according to tertiles of percent daily caloric intake at dinner. A significant increase in the incidence rate of obesity (from 4.7 to 11.4%), metabolic syndrome (from 11.1 to 16.1%), and estimated NAFLD (from 16.5 to 23.8%) was observed from the lower to higher tertile. In a multiple logistic regression model adjusted for multiple covariates, subjects in the highest tertile showed an increased risk of developing obesity (OR = 2.33; 95% CI 1.17–4.65; p = 0.02), metabolic syndrome (OR = 1.52; 95% CI 1.01–2.30; p = 0.04), and NAFLD (OR = 1.56; 95% CI 1.10–2.22; p = 0.01).
Conclusions
Consuming more of the daily energy intake at dinner is associated with an increased risk of obesity, metabolic syndrome, and NAFLD.
Introduction
A novel, intriguing hypothesis suggests it is not what you eat, but when you eat that plays a role in weight balance. Breakfast skipping has been associated with weight gain and obesity, dyslipidemia, diabetes and cardiovascular diseases in adults [1]–[4]. Breakfast skippers usually make less healthy food choices compared to breakfast consumers and overcompensate the intake of energy during the day [5]. However, a recent study did not confirm these findings [6]. The current trend for adults is to eat very little in the morning and shift most of the caloric intake later in the day [7]. Emerging evidence shows a relationship between the timing of food intake during the day and weight regulation in animals [8]–[10]. In humans, shifting food ingestion toward the night has been shown to disrupt metabolic homeostasis and raise postprandial triglycerides [11]. Furthermore, two cross-sectional studies in adults found an increased risk of overweight and obesity when more of the daily caloric intake was eaten in the evening [12]–[13], but a prospective cohort study found no association between evening eating and weight change [14]. Yet, late-night eaters showed an increased coronary heart disease risk in a prospective US cohort [4]. No human studies have investigated the relationship between the time of eating and non-alcoholic fatty liver disease (NAFLD), the excessive liver fat accumulation closely associated with obesity and insulin resistance, that can be predicted by noninvasive tools [15].
Our aim was to prospectively assess whether assuming more of the daily caloric intake at dinner predisposes to obesity, hyperglycemia, metabolic syndrome, and estimated liver fat content in a population-based cohort of middle-aged adults.
Subjects and Methods
Participants and setting
All the 45–64 years old Caucasian patients (n = 1877) of six general practitioners were invited to participate in a metabolic screening in 2001–2003. These subjects were representative of the age-corresponding population living in the province of Asti (Northwest Italy) [16]. Of these, 1658 (88.3%) subjects provided written informed consent to participate while 219 declined. Both the participants and non-participants were similar to the resident population of the corresponding age range in terms of male prevalence, education, prevalence of known diabetes, and residence in a rural area [16]. Patients with obesity (n = 315) or type 2 diabetes (n = 94) at baseline, and those who died during the follow-up (n = 61) were excluded. Since these conditions often coexisted in the same individuals, 413 patients were excluded, and data from 1245 subjects were finally analyzed.
The study was approved by the local ethics committee (“Comitato Etico Interaziendale A.S.O. SS.Antonio e Biagio e C.Arrigo” of Alessandria). All the procedures conformed to the principles of the Helsinki Declaration.
Measurements
In the morning, after at least 12 h of fasting, weight, height, waist circumference, and blood pressure were measured. Waist circumference was measured by a plastic tape meter at the level of the umbilicus. Two blood pressure measurements were performed using mercury sphygmomanometers and appropriate cuff sizes after a 10-minute rest in the sitting position; reported values are the means of the two measurements. A blood sample was drawn for the determination of glucose, insulin, total cholesterol, HDL-cholesterol, triglycerides, alanine aminotransferase (ALT), γ-glutamyl transferase (GGT) and high-sensitivity C-reactive protein (CRP) values. If serum glucose was ≥110 mg/dl, a second fasting glucose determination was performed.
All patients were submitted to a health screening questionnaire at baseline, from July 2001 to September 2003. Data on smoking habits, alcohol consumption, educational level, health conditions, current medications (in particular drugs influencing glucose control and/or body weight, such as hypoglycemic drugs, insulin, antidepressant/antipsychotic, and estrogen/steroid use), mean weekly number of meals consumed in restaurants (including fast-food restaurants and pizzerias), and hours of sleep were collected for each subject. Sleep duration was defined as self-reported time in bed (calculated from bedtime to get up time) minus sleep latency. At baseline, patients completed the Minnesota Leisure Time Physical Activity questionnaire [17], previously validated in an European cohort [18], and the semi-quantitative food-frequency questionnaire used in the EPIC (European Prospective Investigation into Cancer and Nutrition) study [19]. The EPIC questionnaire assessed the average frequency and portion intake of 148 foods consumed in the 12 months prior to examination, but it did not evaluate the food distribution during the day. The frequency of food intake was assessed using ten categories, ranging from “never” to “five times per day or more”, whereas quantity was determined comparatively using photographs of standard portion sizes. Contemporarily, at baseline, all subjects were submitted to a 3-day food record, which consisted of a detailed written food diary. Subjects were instructed to record everything they ate or drank during 2 consecutive week days and 1 week-end day [20]. The 53 food photos and measuring guides (cups, spoons, glasses, etc) of the EPIC questionnaire aided respondents in estimating the amount of foods or beverages consumed during the compilation of the 3-day food record. The temporal pattern of food consumption was also recorded, as participants were asked to list foods eaten at breakfast, lunch, dinner, and during mid-morning, mid-afternoon, and after dinner. An instruction sheet defining each meal was given together with the food record: breakfast was defined as the meal consumed after waking up; the mid-morning meal as the food consumed after breakfast and before lunch in the morning (until 12 am), lunch as the meal consumed from 12 am to 3 pm, mid-afternoon meal as the food consumed after lunch before dinner, until 7 pm; dinner as the meal consumed from 7 pm to 10 pm; after-dinner meal as the food consumed after dinner until going to sleep. This was in line with the Italian habits.
We considered as dinner the eating occasion self-reported as dinner; skipping breakfast was defined when no consumption of any food for breakfast was reported.
When evaluating the frequency of eating occasions, we considered as eating occasion every episode with a caloric intake corresponding at least to the 15% of the total daily caloric intake [21].
A dietician, blinded to the study details, checked all questionnaires for completeness, internal coherence, and plausibility. In case of uncertain answers, the patients were interviewed by the dietician. Overall, patient compliance was high, because of the collaboration with general practitioners, who supported the patients during the recall and collection of data.
The 3-day food record data were loaded on the Win Food Pro 3 software (Medimatica, Colonnella, Teramo, Italy), and the mean nutritional values for the 3 days were reported. The reliability of the reported energy intake was assessed by calculating the ratio of estimated energy intake to predicted basal metabolic rate using age- and sex-specific formulas derived by Schofield [22]. Subjects with a ratio <0.88 were classified as under-reporters [23].
The entire sample (n = 1658) was then divided into three tertiles, according to percentage of daily caloric intake at dinner (the first tertile had the lowest dinner caloric intake, <33% of daily kcal; the third tertile the highest, ≥48% of daily kcal). These cutoffs divided the 1245 subjects evaluated in the final analysis into three groups of 423, 418, and 404 individuals, respectively.
The physical activity level was calculated as the product of the duration and frequency of each activity (in hours/week), weighted by an estimate of the metabolic equivalent of the activity (METS) and summed for the activities performed.
The laboratory methods have been described previously [16], [24]. Glycated hemoglobin (HbA1c) values were evaluated by High Performance Liquid Cromatography (Tosoh, Turin, Italy). This is a standardized method, as certified by the International Federation of Clinical Chemistry and Laboratory Medicine. The correlation coefficient and coefficient of variation were, respectively, 0.9998 and 0.21%.
All samples were run blindly.
Follow-up
From January to November 2008, patients were contacted for follow-up visits. Weight, waist circumference and blood pressure were measured, and a blood sample was drawn for the determination of the same fasting metabolic parameters evaluated at baseline (see above). Since the visits were performed in collaboration with the general practitioners of the patients, we were able to contact all the patients.
Definitions
The homeostasis model assessment of insulin resistance (HOMA-IR) [25] was employed to estimate insulin resistance. Diabetes and impaired fasting glucose (IFG) were defined according to published recommendations [26]. In particular, a diagnosis of diabetes was made in the presence of fasting plasma glucose ≥126 mg/dl; only 3 patients presented the classic symptoms of hyperglycemia and a random plasma values ≥200 mg/dl. In line with the Harmonization definition, metabolic syndrome was defined by the presence of three of the following five components: waist circumference ≥94 cm (men) or ≥80 cm (women), triglycerides ≥150 mg/dl, HDL cholesterol <40.0 mg/dl (men) or <50.0 mg/dl (women), systolic blood pressure ≥130 mmHg and/or diastolic blood pressure ≥85 mmHg and/or antihypertensive drug therapy and fasting glucose ≥100 mg/dl or hypoglycemic therapy [27]. NAFLD was estimated with the NAFLD liver fat score, according to the following formula [15]:
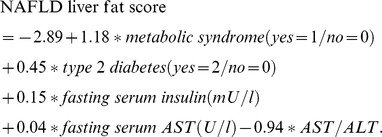 |
The estimated liver fat percentage was calculated with the liver fat [15]:
 |
NAFLD was defined as >5% estimated liver fat percentage [15].
Statistical analyses
Because the distributions of alcohol intake, triglyceride, fasting insulin, HOMA-IR, ALT, GGT, CRP values, and NAFLD score were highly skewed, their values were log-transformed to obtain a normal distribution. In all analyses, the log-transformed values were then used. For ease of data interpretation, the untransformed values are reported in the tables.
The Friedman test was used to detect differences within individuals in the caloric intake at dinner across the 3 days of the food records.
The ANOVA and the χ2-test were performed to assess the differences among tertiles of dinner caloric intake in the continuous and categorical variables, respectively.
A multiple logistic regression analysis was used to estimate the odds of incident obesity and diabetes, IFG, the metabolic syndrome, and estimated NAFLD, each used as a dependent variable, with tertiles of dinner caloric intakes, used as a dummy variable. Both unadjusted (crude ORs) and adjusted models were carried out for each outcome variable. In the model 1, the following variables were introduced into the model: age (as a continuous variable), sex (males = 1/females = 0), BMI at baseline (as a continuous variable), METS h/week (as a continuous variable), living in a rural area (yes = 1/no = 0); in the model 2, all the above described variables plus intake of total energy and SFA (both as continuous variables), and skipping breakfast (yes = 1/no = 0) were introduced. Since the outcome incidence was evaluated in the living participants at the end of the follow-up during 2008, we were not able to obtain the date of the outcome incidence, and to perform a survival analysis.
The lower tertile of dinner caloric intake (the first tertile) was considered as the reference group, and the other two groups were introduced as dummy variables (STATISTICA software 5.1, Statsoft Italia).
Results
The mean caloric intake at dinner during the 3 days was 905.4±485.4 kcal; the mean caloric intake from dinner was not significantly different during day 1, 2, and 3 (the latter was the week-end day): 901.1, 896.9, and 918.4 kcal, respectively. Out of 1245 subjects, 103 (8.3%) resulted under-reporters. Among the tertiles of caloric intake at dinner, the percentage of under-reporters did not differ (8.5%, 8.1%, and 8.2% in the first, second, and third tertile, respectively).
Baseline lifestyle and dietary characteristics according to the tertile of percentage of daily caloric intake at dinner are summarized in Table 1; clinical and laboratory values of the participants are reported in Table 2. Subjects in the first tertile were less likely to skip breakfast and consumed lower total energy and SFA, while percentage of calories from carbohydrates, protein, total fat and polyunsaturated fatty acids (PUFA), and fiber and alcohol intake did not differ from the other tertiles (Table 1). The dinner dietary composition, with the exception of total caloric intakes, did not differ among groups (Table 1). At baseline, no significant difference was found among tertiles for age, sex, educational level, drugs used, blood pressure and anthropometric values, laboratory variables, and prevalence of NAFLD, IFG, and the metabolic syndrome (Tables 1–2).
Table 1. Baseline lifestyle and dietary characteristics by the percentage of total daily caloric intake from dinner.
| Lower tertile | Middle tertile | Higher tertile | |
| Number | 423 | 418 | 404 |
| % total kcal from dinner | <33 | 33–48 | ≥48 |
| Physical activity (METS h/week)1 | 22.4±9.6 | 21.2±8.9 | 21.3±9.1 |
| Actual smoking (%) | 24.6 | 24.2 | 23.3 |
| Hours sleep/day1 | 7.2±1.1 | 7.1±1.2 | 7.1±1.2 |
| Antidepressant use (%) | 4.0 | 2.6 | 3.5 |
| Restaurant foods >3/week | 2.4 | 2.9 | 3.9 |
| Skipping breakfast (%) | 7.8 | 28.7a | 22.3a |
| After-dinner eating (%) | 13.2 | 12.9 | 13.4 |
| Kcal from after-dinner eating1 | 100.3±15.7 | 104.0±36.9 | 105.6±37.9 |
| Frequency of eating occasions2 | |||
| 1 | 2.4 | 2.9 | 2.5 |
| 2 | 14.9 | 13.9 | 12.6 |
| 3 | 47.5 | 48.8 | 47.3 |
| 4 | 12.3 | 12.7 | 13.9 |
| ≥5 | 22.9 | 21.8 | 23.8 |
| Total intakes | |||
| Total kcal1 | 2053.9±657.3 | 2165.5±631.5b | 2132.7±677.7 |
| Carbohydrates (% kcal)1 | 48.9±7.3 | 48.8±6.6 | 48.4±7.4 |
| Protein (% kcal)1 | 16.3±2.9 | 16.1±2.3 | 16.2±2.5 |
| Fat (% kcal)1 | 34.7±6.0 | 34.8±5.6 | 35.4±6.0 |
| SFA (% kcal)1 | 11.8±3.0 | 11.9±2.9 | 12.3±3.7b |
| PUFA (% kcal)1 | 4.3±1.6 | 4.2±1.5 | 4.3±1.4 |
| Fiber (g/day)1 | 21.7±10.5 | 21.0±8.1 | 21.0±9.8 |
| Alcohol (g/day)3 | 10.0 (30.0) | 5.0 (30.0) | 10.0 (20.0) |
| Dinner intakes | |||
| Kcal1 | 522.4±236.3 | 860.1±284.1a | 1353.4±477.5a |
| Variance of kcal from dinner | 55849.7 | 80718.3 | 227985.4 |
| Protein (% kcal)1 | 18.7±3.0 | 18.6±2.3 | 18.6±2.6 |
| Fat (% kcal)1 | 35.5±6.0 | 35.6±5.6 | 36.2±6.0 |
| Fiber (g/1000 kcal)1 | 4.6±1.8 | 4.5±1.6 | 4.6±1.7 |
| Therapy | |||
| Estrogen/steroid drugs (%) | 5.9 | 6.2 | 6.2 |
| Antidepressant/antipsychotic drugs (%) | 4.0 | 2.6 | 3.5 |
| Oral hypoglycemic drugs/insulin (%) | 0 | 0 | 0 |
mean±SD.
eating occasion = every episode with ≥15% of the total daily caloric intake.
median (inter-quartile range).
p<0.01 vs tertile 1;
p<0.05 vs tertile 1; p-values were evaluated by ANOVA or chi-square-test.
Metabolic equivalent of the activity (MET); saturated fatty acids (SFA); polyunsaturated fatty acids (PUFA).
Table 2. Baseline clinical and laboratory characteristics by the percentage of total daily caloric intake from dinner.
| Lower tertile | Middle tertile | Higher tertile | |
| Number | 423 | 418 | 404 |
| Age (years)1 | 54.4±5.7 | 54.5±5.7 | 54.1±5.6 |
| Males (%) | 47.5 | 45.0 | 45.3 |
| Education (%) | |||
| Secondary school | 19.4 | 17.5 | 19.3 |
| Graduated | 9.0 | 8.4 | 9.2 |
| Living in a rural area (%) | 40.9 | 40.0 | 36.9 |
| Systolic blood pressure (mmHg)1 | 131.6±15.4 | 132.3±15.9 | 131.0±14.9 |
| Diastolic blood pressure (mmHg)1 | 81.7±8.2 | 82.6±9.7 | 81.9±8.8 |
| BMI (kg/m2)1 | 24.6±2.9 | 24.9±2.7 | 24.9±2.9 |
| Waist circumference (cm)1 | 86.8±10.9 | 87.6±9.9 | 87.5±10.6 |
| Fasting glucose (mg/dl)1 | 99.4±20.1 | 99.5±18.2 | 101.0±23.8 |
| HbA1c (%) | 5.04±0.45 | 5.07±0.44 | 5.09±0.47 |
| Triglycerides (mg/dl)2 | 113.0 (63.0) | 107.0 (69.0) | 113.0 (67.0) |
| Total cholesterol (mg/dl)1 | 219.4±40.1 | 213.7±42.0 | 218.0±40.3 |
| HDL cholesterol (mg/dl)1 | 62.4±14.1 | 61.2±13.0 | 61.4±13.5 |
| Fasting insulin (µU/ml)2 | 6.7 (1.8) | 6.6 (1.7) | 6.7 (2.3) |
| HOMA-IR score (mmol/l×µU/ml)2 | 1.6 (0.6) | 1.6 (0.6) | 1.6 (0.7) |
| ALT (UI/l)2 | 17.0 (12.0) | 18.0 (13.0) | 17.5 (11.0) |
| GGT (UI/l)2 | 17.0 (17.0) | 17.0 (13.0) | 17.0 (16.0) |
| NAFLD score2 | −3.0 (1.4) | −2.9 (1.3) | −2.9 (1.4) |
| Prevalent NAFLD3 (%) | 10.7 | 7.5 | 9.3 |
| CRP (mg/l)2 | 1.1 (1.6) | 1.0 (1.6) | 1.2 (1.7) |
| IFG (%) | 10.4 | 13.9 | 14.9 |
| Metabolic syndrome (%) | 27.9 | 30.9 | 29.7 |
mean±SD.
median (inter-quartile range).
NAFLD was defined as >5% estimated liver fat percent [15].
p<0.01 vs tertile 1;
p<0.05 vs tertile 1; p-values were evaluated by ANOVA or chi-square-test.
Homeostasis model assessment of insulin resistance (HOMA-IR); alanine aminotransferase (ALT); γ-glutamyl transferase (GGT); non-alcoholic fatty liver disease (NAFLD); C-reactive protein (CRP); impaired fasting glucose (IFG).
Mean follow-up period was 6.1±0.34 years (median 5.8 years). Subjects in the first tertile showed a significantly lower BMI and NAFLD prevalence, and a more favourable NAFLD score (Table 3). The incidence of obesity, diabetes, IFG, NAFLD, and metabolic syndrome were respectively: 101/1245 (8.1%), 30/1245 (2.4%), 286/1245 (23.0%), 229/1245 (18.4%), and 172/1245 (13.8%). The incidence of obesity significantly increased from the first to third tertile; the incidence of metabolic syndrome and estimated NAFLD were significantly higher in the upper tertile (Table 3). Individuals who consumed almost half of their daily caloric intake at dinner were 2-fold more likely to become obese in a multiple logistic regression model, after adjusting for age, sex, BMI at baseline, physical activity, living in a rural area, intake of total energy and SFA, and skipping breakfast (Table 4). In the same model, other variables were significantly associated with the incidence of obesity: the physical activity level expressed as METS h/week (OR = 0.94; 95% CI 0.91–0.97; p<0.001); percentage of SFA intake (OR = 1.10; 95% CI 1.03–1.18; p = 0.006); total energy (OR = 1.06; 95% CI 1.01–1.10; p = 0.005 for each 100 kcal increase); skipping breakfast (OR = 2.13; 95% CI 1.20–3.81; p = 0.01).
Table 3. Characteristics at follow-up by the percentage of total daily caloric intake from dinner.
| Lower tertile | Middle tertile | Higher tertile | |
| Number | 423 | 418 | 404 |
| Systolic blood pressure (mmHg)1 | 132.9±16.1 | 132.8±17.8 | 132.4±15.7 |
| Diastolic blood pressure (mmHg)1 | 81.8±8.8 | 82.5±9.2 | 81.4±9.2 |
| BMI (kg/m2)1 | 24.8±3.1 | 25.2±3.0a | 25.5±3.2b |
| Waist circumference (cm)1 | 88.6±10.9 | 89.2±10.4 | 89.4±10.5 |
| Fasting glucose (mg/dl)1 | 97.7±21.1 | 97.4±13.7 | 99.9±20.3 |
| HbA1c (%) | 5.03±0.72 | 5.03±0.50 | 5.11±0.71 |
| Triglycerides (mg/dl)2 | 109.0 (66.0) | 106.0 (73.0) | 113.0 (68.0) |
| Total cholesterol (mg/dl)1 | 220.7±39.7 | 217.7±39.3 | 224.4±41.5 |
| HDL cholesterol (mg/dl)1 | 58.7±15.2 | 56.6±14.6 | 58.0±14.7 |
| Fasting insulin (µU/ml)2 | 6.5 (5.3) | 7.3 (4.9) | 6.8 (5.2) |
| HOMA-IR score (mmol/l×µU/ml)2 | 1.5 (1.2) | 1.7 (1.2) | 1.6 (1.2) |
| ALT (UI/l)2 | 20.0 (11.0) | 22.0 (13.0) | 22.0 (14.0) |
| GGT (UI/l)2 | 21.0 (19.0) | 21.0 (15.0) | 22.0 (21.0) |
| NAFLD score2 | −1.7 (1.9) | −1.3 (1.8) | −1.2 (2.0)a |
| Prevalent NAFLD3 (%) | 20.4 | 17.8 | 28.2b |
| CRP (mg/l)2 | 1.0 (1.0) | 1.0 (1.7) | 1.0 (1.5) |
| Incident obesity (%) | 4.7 | 8.4a | 11.4b |
| Incident diabetes (%) | 1.7 | 1.9 | 3.7 |
| Incident IFG (%) | 22.2 | 22.5 | 24.3 |
| Incident NAFLD4 (%) | 16.5 | 15.0 | 23.8a |
| Incident metabolic syndrome (%) | 11.1 | 14.4 | 16.1a |
| Therapy | |||
| Estrogen/steroid drugs (%) | 6.1 | 6.0 | 6.2 |
| Antidepressant/antipsychotic drugs (%) | 4.3 | 2.9 | 3.9 |
| Oral hypoglycemic drugs/insulin (%) | 1.2 | 1.4 | 2.5 |
mean±SD.
median (inter-quartile range).
NAFLD was defined as >5% estimated liver fat percent [15].
incident NAFLD was not equal to the difference between prevalent NAFLD at follow-up minus prevalent NAFLD at baseline, since some individuals whose estimated liver fat percent at baseline was >5%, showed a <5% liver fat percent at follow-up, i.e. their metabolic pattern ameliorated during follow-up.
p<0.05 vs tertile 1;
p<0.01 vs tertile 1; p-values were evaluated by ANOVA or chi-square-test.
Homeostasis model assessment of insulin resistance (HOMA-IR); alanine aminotransferase (ALT); γ-glutamyl transferase (GGT); non-alcoholic fatty liver disease (NAFLD); C-reactive protein (CRP); impaired fasting glucose (IFG).
Table 4. Association between outcomes at follow-up (dependent variables) and the percentage of total daily caloric intake from dinner in multiple logistic regression models.
| Lower tertile | Middle tertile | Higher tertile | |
| OR; 95% CI; p | OR; 95% CI; p | ||
| Incident obesity (%) | |||
| Crude | 1 | 1.84; 1.04–3.25; 0.03 | 2.59; 1.50–4.46; <0.001 |
| Model 11 | 1 | 1.88; 0.97–3.66; 0.06 | 2.75; 1.45–5.20; 0.002 |
| Model 22 | 1 | 1.79; 0.89–3.62; 0.10 | 2.33; 1.17–4.65; 0.02 |
| Incident diabetes (%) | |||
| Crude | 1 | 1.16; 0.42–3.23; 0.78 | 2.29; 0.92–5.69; 0.07 |
| Model 11 | 1 | 1.13; 0.40–3.15; 0.82 | 2.36; 0.94–5.90; 0.07 |
| Model 22 | 1 | 0.97; 0.34–2.78; 0.96 | 2.26; 0.89–5.75; 0.09 |
| Incident IFG (%) | |||
| Crude | 1 | 1.00; 0.98–1.01; 0.76 | 1.00; 0.99–1.02; 0.55 |
| Model 11 | 1 | 1.00; 0.98–1.01; 0.66 | 1.00; 0.99–1.02; 0.64 |
| Model 22 | 1 | 1.00; 0.97–1.01; 0.61 | 0.99; 0.97–1.01; 0.49 |
| Incident metabolic syndrome (%) | |||
| Crude | 1 | 1.34; 0.89–2.02; 0.16 | 1.53; 1.02–2.30, 0.04 |
| Model 11 | 1 | 1.32; 0.88–2.00; 0.18 | 1.54; 1.03–2.32; 0.04 |
| Model 22 | 1 | 1.32; 0.87–2.01; 0.19 | 1.52; 1.01–2.30; 0.04 |
| Incident NAFLD (%) | |||
| Crude | 1 | 0.89; 0.61–1.30; 0.56 | 1.58; 1.12–2.24; 0.01 |
| Model 11 | 1 | 0.86; 0.59–1.25; 0.43 | 1.54; 1.09–2.18; 0.01 |
| Model 22 | 1 | 0.88; 0.60–1.30; 0.53 | 1.56; 1.10–2.22; 0.01 |
Model 1: multiple logistic regression model, after adjustment for age, sex, BMI at baseline, METS h/week, living in a rural area.
Model 2: multiple logistic regression model, after adjustment for age, sex, BMI at baseline, METS h/week, living in a rural area, intake of total energy and saturated fat, and skipping breakfast.
Impaired fasting glucose (IFG); non-alcoholic fatty liver disease (NAFLD); metabolic equivalent of the activity (MET).
The incidence of the metabolic syndrome (OR = 1.52; 95% CI 1.01–2.30; p = 0.04) and the estimated NAFLD (OR = 1.56; 95% CI 1.10–2.22; p = 0.01) were significantly higher in the third tertile of daily caloric intake at dinner (Table 4).
The incidence of diabetes was calculated also taking into account the HbA1c criteria (values ≥6.5%) and was 1.2%, 1.9% and 3.2% in the 423, 418 and 404 individuals, respectively. The association between incident diabetes, diagnosed according to the HbA1c criteria, and the second and third tertiles were respectively: OR = 1.44 (95% CI 0.45–4.56; p = 0.54) and OR = 2.78 (95% CI 0.96–8.10; p = 0.06) in the adjusted model (model 2).
The results did not significantly change after excluding the 103 under-reporters or the 164 individuals who consumed foods after-dinner, and after adjusting for total fiber and alcohol intake, dinner nutrient intakes, restaurant food consumption, sleep duration, number of eating occasions, the follow-up period and use of hypoglycemic drugs, insulin, antidepressant/antipsychotic, and estrogen/steroid at follow-up.
Discussion
In our population-based prospective cohort of middle-aged individuals, energy intake at dinner was significantly associated with the incidence of obesity, metabolic syndrome, and estimated NAFLD. Subjects consuming the largest amount of calories at dinner (“big dinner”) were almost one third of our sample, in line with the literature [12], [14]. After a 6-year follow-up, those individuals were 2-fold more likely to be obese. This association remained significant after adjusting for the intake of energy, SFA and fiber, exercise, skipping breakfast, and other covariates.
Timing of meals and obesity
A few cross-sectional studies have shown that assuming more of the daily energy intake in the evening is associated with an increased risk of overweight and obesity [12]–[13], [28]–[29] while consuming more of the daily calories at lunch or breakfast [12], [28], [30] are inversely associated. A large prospective cohort study found that both skipping breakfast and eating late at night are related to an increased risk of coronary heart disease. This was intriguing since 76% of late-eaters had breakfast [4]. It has been hypothesized that the timing of the meal may be a proxy for healthy lifestyle habits and/or for consuming specific foods, like high-fat foods at dinner or high-fiber foods at breakfast [4], [31]. Eating in the late evening seems to have a lower satiety value than eating in the morning [31]. Nevertheless, in our cohort, there were no differences among groups for dietary pattern at dinner, as well as exercise, smoking, sleep duration and alcohol intake.
Timing of food intake seem to play a role also in weight loss strategies: late lunch eaters lost less weight than early eaters [32]; overweight/obese women with metabolic syndrome lost significantly more weight after a low-calorie dinner weight-loss program than after an isocaloric high-calorie dinner program [33].
Not all studies confirmed the direct association between weight and food intake at dinner [14], [34]. Yet, a positive association between percentage of evening energy intake and long-term weight change was evident in specific subgroups (smoking men, physically active men, inactive women) in a prospective US cohort [14].
Many hypotheses have been suggested to explain the association between the timing of meals and obesity risk. Insulin sensitivity has been reported to decrease later in the day [35]. Increased levels of free fatty acids, fluctuation in cortisol concentrations, increased urinary epinephrine levels, higher morning ACTH plasma values, and/or a delayed peak in the counteracting activity of glucagon after evening meals may be possible contributors to the circadian modulation of insulin secretion or action [11], [34], [35]–[39]. Diet-induced thermogenesis is significantly higher after the consumption of a snack in the morning than after the consumption of the same snack at night [40], and a reduced evening thermic response may be due to the nocturnal insulin resistance [41]. Habitual nighttime eating or snacking have been associated with reduced fat oxidation, potentially promoting weight gain [42]–[43]. Additionally, morning gastric emptying may be more rapid than evening gastric emptying [44], and an increased efficacy of absorption of dietary carbohydrates has been demonstrated under late suppertime conditions [45]. Circadian variations in satiety hormones, energy expenditure, and genetic mutations of the circadian clock genes have been associated with weight gain and metabolic abnormalities in mice [8]–[10], [46], as well as humans [32], [47].
Timing of meals and the metabolic syndrome
Eating habits have been associated with the development of insulin resistance and the metabolic syndrome [2]–[3], [48]–[49]. In a small randomized crossover trial, healthy adults showed significantly higher blood values of glucose, insulin, and triglycerides after night meals compared to the ingestion of the same meals during the day [11], thus supporting the well known association between shift work and increased cardiovascular disease and metabolic risk [50]–[51]. These associations seem to be related to the disruption of circadian rhythms leading to worsen the physiological nocturnal decrease of glucose tolerance and adverse metabolic and cardiovascular consequences [35], [52]. Accordingly, in our cohort, individuals consuming a big dinner showed a 1.5-fold higher incidence of metabolic syndrome and a 2-fold higher incidence of diabetes at follow-up; the low number of incident cases of diabetes (30/1245) probably did not allow us to observe a significant associations.
The relationships between caloric intake from dinner and obesity or metabolic syndrome were attenuated after adjusting for breakfast skipping, a condition associated with an increased prevalence of obesity and metabolic diseases [1]–[4], [53]. In our cohort, breakfast skippers more frequently consumed a big dinner and showed a 2-fold higher risk of incident obesity.
Even though eating behaviors are highly inter-related, consuming a big dinner and skipping breakfast were both independently associated with incident obesity and metabolic syndrome in a multiple logistic regression analysis, without reciprocal interference in our cohort.
Timing of meals and NAFLD
We found that the timing of food intake during the day affected liver fat accumulation and the risk of developing NAFLD, the most common chronic liver disease and an emerging cardio-metabolic risk factor. The exact molecular mechanisms underlying this association are still to be elucidated. A recent metabolomic study discloses extensive and coordinate clock-controlled oscillations of many metabolites, including those within the amino-acid, carbohydrate and lipid metabolic pathways [54]. Other studies are warranted to investigate molecular basis of the interaction between different nutrients and the endogenous metabolic clock in the liver.
Limitations and strengths
The limitations of a follow-up study are due to competitive risks existing during the follow-up time. We have not evaluated the presence of night eating syndrome; however, we have reduced the possibility of introducing this bias by excluding obese individuals at baseline. Furthermore, the hours of sleep and the percentage of post-dinner eating individuals did not differ among the groups. Our results may be culture-specific and might not be applicable to cultures with different temporal distribution of food intake over the day. Measurement errors are known to be associated with all dietary questionnaires, and underestimation of energy intake seems to be greater in obese individuals [13], [28]. We have excluded obese individuals at baseline, and therefore our prevalence of underreporting was lower than in literature [55]. A 3-day food record may be inadequate to evaluate the individual usual eating patterns. However, it is usually employed to characterize dietary habits of groups of individuals [55]. Furthermore, the comparability of our data with other Italian data [55] is reassuring, although it is not sufficient to establish the validity of the data. The possibility of residual confounding factors cannot be excluded, due to the observational study design. Finally, our results cannot be extended to obese individuals.
This was a prospective study providing extensive and complete clinical measures as well as data on different lifestyle conditions with which to explore confounders and mediators of the associations under investigation.
Conclusions
A better understanding of the mechanisms of weight gain could have important implications for developing new strategy to counteract the obesity epidemic. The timing of energy intake is a modifiable lifestyle habit that might impact on the incidence of obesity, metabolic syndrome, and NAFLD. Intervention trials are needed to evaluate the opportunity to include in dietary recommendations advice on the time-of-day for food consumption, besides advice on food quality and quantity.
Funding Statement
This study was supported by a grant from: Regione Piemonte, 2009. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Timlin MT, Pereira MA (2007) Breakfast frequency and quality in the etiology of adult obesity and chronic diseases. Nutr Rev 65: 268–281. [DOI] [PubMed] [Google Scholar]
- 2. Farshchi HR, Taylor MA, Macdonald IA (2005) Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr 81: 388–396. [DOI] [PubMed] [Google Scholar]
- 3. Mekary RA, Giovannucci E, Willett WC, van Dam RM, Hu FB (2012) Eating pattern and type 2 diabetes risk in men: breakfast omission, eating frequency, and snacking. Am J Clin Nutr 95: 1182–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cahill LE, Chiuve SE, Mekary RA, Jensen MK, Flint AJ, et al. (2013) Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation 128: 337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Castro JM (2009) When, how much and what foods are eaten are related to total daily food intake. Br J Nutr 102: 1228–1237. [DOI] [PubMed] [Google Scholar]
- 6. Levitsky DA, Pacanowski CR (2013) Effect of skipping breakfast on subsequent energy intake. Physiol Bev 119: 9–16. [DOI] [PubMed] [Google Scholar]
- 7. Almoosawi S, Winter J, Prynne CJ, Hardy R, Stephen AM (2012) Daily profiles of energy and nutrient intakes: are eating profiles changing over time? Eur J Clin Nutr 66: 678–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW (2009) Circadian timing of food intake contributes to weight gain. Obesity 17: 2100–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fonken LK, Workman JL, Walton JC, Weil ZM, Morris JS, et al. (2010) Light at night increases body mass by shifting the time of food intake. Proc Natl Acad Sci 107: 18664–18669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bray MS, Tsai JY, Villegas-Montoya C, Boland BB, Blasier Z, et al. (2010) Time-of-day-dependent dietary fat consumption influences multiple cardiometabolic syndrome parameters in mice. Int J Obes 34: 1589–1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Al-Naimi S, Hampton SM, Richard P, Tzung C, Morgan LM (2004) Postprandial metabolic profiles following meals and snacks eaten during simulated night and day shift work. Chronobiol Intern 21: 937–947. [DOI] [PubMed] [Google Scholar]
- 12. Wang JB, Patterson RE, Ang A, Edmond JA, Shetty N, et al. (2014) Timing of energy intake during the day is associated with the risk of obesity in adults. J Hum Nutr Diet 27 Suppl 2255–262. [DOI] [PubMed] [Google Scholar]
- 13. Bertéus Forslund H, Lidroos AK, Sjöström L, Lissner L (2002) Meal patterns and obesity in Swedish women –a simple instrument describing usual meal types, frequency and temporal distribution. Eur J Clin Nutr 56: 740–747. [DOI] [PubMed] [Google Scholar]
- 14. Kant AK, Schatzkin A, Ballard-Barbash R (1997) Evening eating and subsequent long-term weight change in a national cohort. Int J Obes 21: 407–412. [DOI] [PubMed] [Google Scholar]
- 15. Kotronen A, Peltonen M, Hakkarainen A, Sevastianova K, Bergholm R, et al. (2009) Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology 137: 865–872. [DOI] [PubMed] [Google Scholar]
- 16. Bo S, Gentile L, Ciccone G, Baldi C, Benini L, et al. (2005) The metabolic syndrome and high C-reactive protein: prevalence and difference by sex in a southern-European population-based cohort. Diabetes Metab Research Rev 21: 515–524. [DOI] [PubMed] [Google Scholar]
- 17. Taylor HL, Jacobs DR Jr, Schucker B, Knudsen J, Leon AS, et al. (1978) Questionnaire for the assessment of leisure time physical activities. J Chronic Diseases 31: 741–755. [DOI] [PubMed] [Google Scholar]
- 18. Elosua R, Marrugat J, Molina L, Pons S, Pujol E (1994) Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish men. The MARATHOM Investigators. Am J Epidemiol 139: 1197–1209. [DOI] [PubMed] [Google Scholar]
- 19. Kroke A, Klipstein-Grobusch K, Voss S, Moseneder J, Thielecke F, et al. (1999) Validation of a self-administered food-frequency questionnaire administered in the European Prospective Investigation into Cancer and Nutrition (EPIC) study: comparison of energy, protein, and macronutrient intakes estimated with the doubly labeled water, urinary nitrogen, and repeated 24-h dietary recall methods. Am J Clin Nutr 70: 439–447. [DOI] [PubMed] [Google Scholar]
- 20. Bo S, Ciccone G, Durazzo M, Gambino R, Massarenti P, et al. (2007) Efficacy of antioxidant treatment in reducing resistin serum levels: A randomized study. PLoS Clin Trials 2: e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gregori D, Foltran F, Ghidina M, Zobec F, Ballali S, et al. (2011) The “snacking child” and its social network: some insights from an italian survey. Nutr J 10: 132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schofield WN (1985) Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 39 (Suppl 1)5–41. [PubMed] [Google Scholar]
- 23. Goldberg GR, Black AE, Jebb SA, Cole TJ, Murgatroyd PR, et al. (1991) Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr 45: 569–581. [PubMed] [Google Scholar]
- 24. Bo S, Durazzo M, Guidi S, Carello M, Sacerdote C, et al. (2006) Dietary magnesium and fiber intake, inflammatory and metabolic parameters in middle-aged subjects from a population-based cohort. Am J Clin Nutr 84: 1062–1069. [DOI] [PubMed] [Google Scholar]
- 25. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, et al. (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28: 412–419. [DOI] [PubMed] [Google Scholar]
- 26. American Diabetes Association (2012) Diagnosis and classification of diabetes mellitus. Diabetes Care 35: S64–S71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, et al. (2009) Harmonizing the metabolic syndrome. Circulation 120: 1640–1645. [DOI] [PubMed] [Google Scholar]
- 28. Berg C, Lappas G, Wolk A, Strandhagen E, Torén K, et al. (2009) Eating patterns and portion size associated with obesity in a Swedish population. Appetite 52: 21–26. [DOI] [PubMed] [Google Scholar]
- 29. Baron KG, Reid KJ, Kern AS, Zee PC (2011) Role of sleep timing in caloric intake and BMI. Obesity 19: 1374–1381. [DOI] [PubMed] [Google Scholar]
- 30. Summerbell CD, Moody RC, Shanks J, Stock MJ, Geissler C (1996) Relationship between feeding pattern and body mass index in 220 free-living people in four age groups. Eur J Clin Nutr 50: 513–519. [PubMed] [Google Scholar]
- 31. de Castro JM (2004) The time of food intake influences overall intake in humans. J Nutr 134: 104–111. [DOI] [PubMed] [Google Scholar]
- 32. Garaulet M, Gómez-Abellán P, Alburquerque-Bèjar JJ, Lee YC, Ordovás JM, et al. (2013) Timing of food intake predicts weight loss effectiveness. Int J Obes 37: 604–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jakubowicz D, Barnea M, Wainstein J, Froy O (2013) High caloric intake at breakfast vs dinner differentially influences weight loss of overweight and obese women. Obesity 21: 2504–2512. [DOI] [PubMed] [Google Scholar]
- 34. Keim NL, Van Loan MD, Horn WF, Barbieri TF, Mayclin PL (1997) Weight loss is greater with consumption of large morning meal and fat-free mass is preserved with large evening meals in women on a controlled weight reduction regimen. J Nutr 127: 75–82. [DOI] [PubMed] [Google Scholar]
- 35. Van Cauter E, Desir D, Decoster C, Fery F, Balasse EG (1989) Nocturnal decrease of glucose tolerance during constant glucose infusion. J Clin Endocrinol Metab 69: 604–611. [DOI] [PubMed] [Google Scholar]
- 36. Van Cauter E, Shapiro ET, Tillil H, Polonsky KS (1992) Circadian modulation of glucose and insulin responses to meals: relationship to cortisol rhythm. Am J Physiol 262: E467–E475. [DOI] [PubMed] [Google Scholar]
- 37. Van Cauter E, Refetoff S (1985) Multifactorial control of the 24-hour secretion profiles of pituitary hormones. J Endocrinol Invest 8: 381–391. [DOI] [PubMed] [Google Scholar]
- 38. Goetz F, Bishop J, Halberg F, Sothern RB, Brunning R, et al. (1976) Timing of single daily meal influences relations among human circadian rhythms in urinary cycle AMP and hemic glucagon, insulin and iron. Experientia 32: 1081–1084. [DOI] [PubMed] [Google Scholar]
- 39. Lucassen EA, Zhao X, Rother KI, Mattingly MS, Courville AB, et al. (2013) Evening chronotype is associated with changes in eating behaviour, more sleep apnea, and increased stress hormones in short sleeping obese individuals. PLoS One 8: e56519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Romon M, Edme JL, Boulenguez C, Lescroart JL, Fritmat P (1993) Circadian variation of diet-induced thermogenesis. Am J Clin Nutr 57: 476–480. [DOI] [PubMed] [Google Scholar]
- 41. Ravussin E, Acheson KJ, Vernet O, Danforth E, Jéquier E (1985) Evidence that insulin resistance is responsible for the decreased thermic effect of glucose in human obesity. J Clin Invest 76: 1268–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gluck ME, Venti CA, Salbe AD, Votruba SB, Krakoff J (2011) Higher 24-h respiratory quotient and higher spontaneous physical activity in nighttime eaters. Obesity 19: 319–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hibi M, Masumoto A, Naito Y, Kiuchi K, Yoshimoto Y, et al. (2013) Nighttime snacking reduces whole body fat oxidation and increases LDL cholesterol in healthy young women. Am J Physiol Regul Integr Comp Physiol 304: R94–R101. [DOI] [PubMed] [Google Scholar]
- 44. Goo RH, Moore JG, Greenberg E, Alazraki HP (1987) Circadian variation in gastric emptying of meals in humans. Gastroenterology 93: 515–518. [DOI] [PubMed] [Google Scholar]
- 45. Tsuchida Y, Hata S, Sone Y (2013) Effects of a late supper on digestion and the absorption of dietary carbohydrates in the following morning. J Physiol Anthropol 32: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Turek FW, Joshu C, Kohsaka A, Lin E, Ivanova G, et al. (2005) Obesity and metabolic syndrome in circadian Clock mutant mice. Science 308: 1043–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Garaulet M, Lee YC, Shen J, Parnell LD, Arnett DK, et al. (2009) CLOCK genetic variation and metabolic syndrome risk: modulation by monounsaturated fatty acids. Am J Clin Nutr 90: 1466–1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jenkins DJ, Wolever TM, Vuksan V, Brighenti F, Cunnane SC, et al. (1989) Nibbling versus gorging: metabolic advantages of increased meal frequency. N Engl J Med 321: 929–934. [DOI] [PubMed] [Google Scholar]
- 49. Almoosawi S, Prynne CJ, Hardy R, Stephen AM (2013) Time-of-day and nutrient composition of eating occasions: prospective association with the metabolic syndrome in the 1946 British birth cohort. Int J Obes 37: 725–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Knuttson A, Åkerstedt T, Jonsson BG, Orth-Gomer K (1986) Increased risk of ischaemic heart disease in shift workers. Lancet i: 89–91. [DOI] [PubMed] [Google Scholar]
- 51. Esquinol Y, Bongard V, Mabile L, Jonnier B, Soulat JM, et al. (2009) Shift wok and metabolic syndrome: respective impact of job strain, physical activity, and dietary rhythms. Chronobiol Int 26: 544–559. [DOI] [PubMed] [Google Scholar]
- 52. Scheer FAJL, Hilton MF, Mantzoros CS, Shea SA (2009) Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci 106: 4453–4458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Leidy HJ, Ortinau LC, Douglas SM, Hoertel HA (2013) Beneficial effects of a higher-protein breakfast on the appetitive, hormonal, and neural signals controlling energy intake regulation in overweight/obese, “breakfast-skipping”. late adolescents girls. Am J Clin Nutr 97: 677–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Eckel-Mahan KL, Patel VR, Mohney RP, Vignola KS, Baldi P, et al. (2012) Coordination of the transcriptome and metabolome by the circadian clock. Proc Natl Acad Sci USA 109: 5541–5546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ferrari P, Slimani N, Ciampi A, Trichopoulou A, Naska A, et al. (2002) Evaluation of under- and overreporting of energy intake in the 24-hour diet recalls in the European Prospective Investigation into Cancer and Nutrition (EPIC). Publ Health Nutr 5: 1329–1345. [DOI] [PubMed] [Google Scholar]


