Abstract
Over the last 20 years, laparoscopic colorectal surgery has shown equal efficacy for benign and malignant colorectal diseases when compared to open surgery. However, a laparoscopic approach reduces postoperative morbidity and shortens hospital stay. In the quest to optimize outcomes after laparoscopic colorectal surgery, reduction of access trauma could be a way to improve recovery. To date, one method to reduce access trauma is natural orifice specimen extraction (NOSE). NOSE aims to reduce access trauma in laparoscopic colorectal surgery. The specimen is delivered via a natural orifice and the anastomosis is created intracorporeally. Different methods are used to extract the specimen and to create a bowel anastomosis. Currently, specimens are delivered transcolonically, transrectally, transanally, or transvaginally. Each of these NOSE-procedures raises specific issues with regard to operative technique and application. The presumed benefits of NOSE-procedures are less pain, lower analgesia requirements, faster recovery, shorter hospital stay, better cosmetic results, and lower incisional hernia rates. Avoidance of extraction site laparotomy is the most important characteristic of NOSE. Concerns associated with the NOSE-technique include bacterial contamination of the peritoneal cavity, inflammatory response, and postoperative outcomes, including postoperative pain and the functional and oncologic outcomes. These issues need to be studied in prospective randomized controlled trials. The aim of this systematic review is to describe the role of NOSE in minimally invasive colorectal surgery.
Keywords: Laparoscopy, Colorectal surgery, Natural orifice specimen extraction, Natural orifice specimen extraction-colectomy, Transcolonic, Transrectal, Transanal, Transvaginal, Transanal minimally invasive surgery, Gastrointestinal endoscopy
Core tip: Natural orifice specimen extraction (NOSE) will be the way forward to avoid abdominal wall incisions and reduce access trauma during laparoscopic colorectal resection. This systematic review addresses all aspects of NOSE in laparoscopic colorectal surgery and discusses the advantages and disadvantages of this technique. Moreover, a detailed discussion of all available studies concerning NOSE-procedures is given. Although different surgical techniques are being used, it is clear that worldwide experience with this minimally invasive procedure is increasing and that the barriers to the use of natural orifice transluminal endoscopic surgery procedures are decreasing.
INTRODUCTION
Laparoscopic colectomy and total mesorectal excision (TME) require a utility incision for specimen delivery and bowel anastomosis. Therefore, natural orifice specimen extraction (NOSE) could be the key to reducing access trauma in laparoscopic colorectal surgery (laparoscopic NOSE-colectomy), with the subsequent reduction of postoperative pain, improvement of patient recovery and a positive long-term outcome in matters such as cosmesis and incisional hernia rates. Because the length of the abdominal incision is directly related to the incisional hernia rate[1], avoiding laparotomy might influence the rate of postoperative wound complications. In NOSE, the specimen is delivered via a natural orifice and the anastomosis is created intracorporeally. Although this procedure appears to be an attractive option to improve postoperative outcome, the literature regarding NOSE-colectomy has not been extensively investigated to date. The aims of this systematic review were to describe the role of NOSE in minimally invasive colorectal surgery, to examine the differences in the reported surgical techniques and the impact on postoperative outcome and to discuss the future of NOSE.
TERMS AND DEFINITIONS
The terminology regarding NOSE should be uniform. In defining NOSE-colectomy, differentiation between transcolonic, transrectal, transanal and transvaginal specimen extraction is necessary. The authors propose that the site where the hollow viscus is opened should define the specimen extraction site: (1) Transcolonic NOSE-colectomy: the specimen is extracted via the colon through the rectum and anal canal; (2) Transrectal NOSE-colectomy: the specimen is extracted through the intact rectum and anal canal (e.g., this could be performed during a sigmoid or high anterior resection); (3) Transanal NOSE-colectomy: the specimen is extracted through the anal canal (e.g., this could be performed during a TME); and (4) Transvaginal NOSE-colectomy: the specimen is extracted via the vagina by a posterior colpotomy.
LITERATURE SEARCH
Medline (PubMed) was systematically searched until the 1st of September 2013 using the following search criteria: laparoscopy and (transcolonic or transrectal or transanal or transvaginal extraction) or colectomy and (transcolonic or transrectal or transanal or transvaginal extraction) or (natural orifice specimen extraction) or (full laparoscopic) or (totally laparoscopic) or (“natural orifice specimen extraction” or “transcolonic” or “transrectal” or “transanal” or “transvaginal” and “laparoscopy” and “colorectal”). Randomized and controlled clinical trials or cohort observational studies (excluding case reports) were considered for inclusion. Studies reporting on pediatric surgery were excluded. To be included, studies had to describe a NOSE-technique applied in laparoscopic colorectal surgery. First, the titles were screened and appropriate studies were selected. Of these studies, the full text was acquired. The language was restricted to English. Relevant data from the studies included were extracted with a standard fill-out form of predefined parameters regarding indications, operative approach (number of ports), anastomotic technique, duration of surgery, postoperative complications and length of hospital stay, and entered into an Excel database.
RESULTS
This literature search resulted in 12134 hits (flow diagram Figure 1). Reading the full text of 139 studies led to the exclusion of an additional 65 studies for a variety of reasons. After the exclusion of 33 case reports[2-34], a total of 41 studies were included in this review[35-75]. One study reported on transcolonic NOSE, 12 studies on transrectal NOSE, 18 on transanal NOSE, and 10 on transvaginal NOSE. Three authors each described the results of two extraction sites in one article. Choi et al[43] and Wang et al[71] reported both transanal and transvaginal NOSE-colectomy, but only a minority of patients had undergone transvaginal specimen extraction, and the results were not reported separately. Franklin et al[49] reported the outcome of both transrectal and transvaginal specimen extraction in one paper, and the results are included in both tables. During the past 10 years, the literature regarding NOSE techniques has evolved, focusing more predominantly on transrectal and transanal NOSE surgery (Figure 2).
Figure 1.
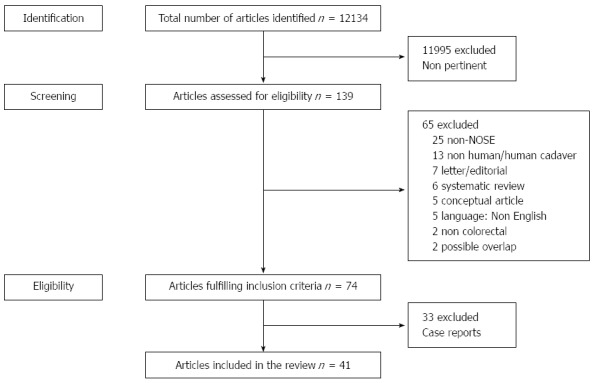
Study flow chart: Search strategy. NOSE: Natural orifice specimen extraction.
Figure 2.
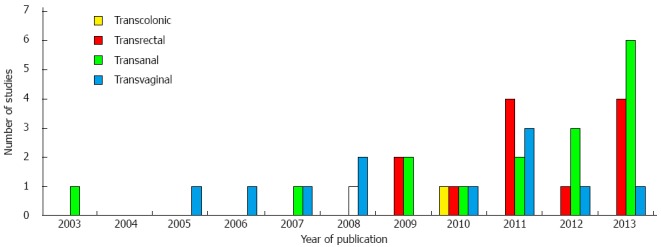
Evolution of publications on natural orifice specimen extraction-colectomy.
TRANSCOLONIC NOSE
The literature search yielded only two reports regarding transcolonic specimen extraction after a laparoscopic ileocolic or segmental colonic resection[25,48]. Both reports described a technique using a colonoscope for specimen extraction. Since the introduction of natural orifice transluminal endoscopic surgery (NOTES), the use of flexible instruments and scopes inserted via natural orifices has gained popularity in the surgical world and in the literature[76,77]. As such, this area of research can be observed as a bridge toward the application of NOTES procedures. Saad et al[25] reported on a case of a laparoscopic transverse colectomy with colonoscopic retrieval of the specimen via the descending colon, sigmoid, rectum and anus. A double-stapled anastomosis was made and the postoperative course was uneventful. In a feasibility study, Eshuis et al[48] prospectively studied 10 young patients (median age 31 years) with Crohn’s disease in whom ileocecal resection was indicated. In this cohort, the specimen was extracted transcolonically with a colonoscope. In 2 patients, it was impossible to extract the specimen because the inflammatory mass was too bulky. In comparison with a conventional laparoscopic ileocecal resection, the operating time was significantly longer, which might have been due to the learning curve. Surgical site-related complications were higher. Nevertheless, two theoretical advantages of this technique are the possibility to extract specimens throughout the colon and its applicability to both male and female patients. However, issues could be raised with regard to mechanical bowel preparation, sterility, size of the lesion/mass, and bowel protection. A major drawback is the need for mechanical bowel preparation to clean the colon and enable colonoscopy. Avoidance of bowel preparation is an important element of enhanced recovery programs and for right-sided colonic resections, it has been shown that mechanical bowel preparation can be omitted[78]. Another concern is the use of a non-sterile colonoscope and the perioperative opening of the bowel. This might cause leakage of bowel contents intra-peritoneally, which can lead to contamination and subsequent abscess formation. However, data from transrectal specimen extractions have not shown any impact on the inflammatory response or infectious morbidity[45,58]. With regard to specimen size and patient characteristics (e.g., BMI), there are no data showing cut-off values above which colonoscopic extraction is contra-indicated and double-stapled anastomosis is difficult to perform. Moreover, there are no studies on patients with a colorectal tumor, and oncological data for colonoscopic specimen extraction are still awaited. An ileocolic specimen is extracted through an unprotected colon, and this might be problematic when large T3 or T4 tumors require extraction. Furthermore, the best method for proceeding if a specimen becomes lodged in the colon during extraction remains to be determined. A final remark concerns the need for a joint effort by the surgical and gastroenterological team in many centers to make this hybrid procedure possible. Colonoscopy should be performed with CO2 to coincide with laparoscopic insufflation. Issues relating to procedural costs and time still need to be investigated.
TRANSRECTAL NOSE
The technique and concept of a transrectal NOSE-colectomy was developed in the early 1990s[79,80], and Franklin et al[80] were the first to publish results on a group of patients who underwent sigmoid resection with transrectal specimen extraction. In 2012, we reported a systematic review referring to 6 studies on transrectal NOSE[81]. To date, a total of 12 reports including a total of 462 patients have been published describing variations of the transrectal technique in different centers (Table 1). There is heterogeneity amongst studies with regard to operating ports (3 ports-25%, 4 ports-50%, 5 ports-25%), rectal protection (none-25%, rigid rectoscope-33%, camera sleeve or retrieval bag-42%), and anastomotic technique (double stapled-17% and tripled stapled-83%). Therefore, postoperative outcome regarding morbidity and length of hospital stay cannot be compared between these studies. However, it is important to investigate and report surgery-related complications when the safety and feasibility of new techniques are evaluated (Table 2). Overall, anastomotic leakage was reported in 13 of 462 patients (2.8%), but this percentage is biased due to differences in anastomotic techniques and small uncontrolled case studies reporting a learning curve phenomenon. There were no randomized trials comparing transrectal NOSE to conventional laparoscopic resection, but 3 case-matched studies were identified. One study failed to show any benefit from transrectal NOSE[44], while there was a significantly lower analgesic requirement in the transrectal NOSE-colectomy groups in the other 2 papers[45,73]. Moreover, a significantly shorter operative time was observed when comparing transrectal NOSE-colectomy with conventional laparoscopic colectomy[73]. Transrectal NOSE appears to be a valid option for specimen extraction and the creation of a colorectal anastomosis because of its applicability in both sexes and its frequent indications in left-sided colonic disease such as diverticulitis, endometriosis, adenoma and carcinoma. Moreover, the straightness of the rectum and relatively easy access to the peritoneal cavity further contribute to the feasibility of the procedure. Additionally, it can be easily standardized and taught. Even so, all studies reporting on transrectal NOSE-colectomy have described different surgical approaches and methods of rectal protection and anastomosis, leading to a considerable bias when the results from these studies are interpreted. Moreover, patient selection appears to be of paramount importance, and the limiting factors include a BMI > 30 kg/m2, a bulky mesocolon, large tumors, the presence of a rectal stricture and proximal diverticular disease[81]. In addition to the above-mentioned technical difficulties and differences, the bacteriological impact on the peritoneal cavity secondary to intraoperative colo- and rectotomy might be a concern. Although some studies did not report intraperitoneal abscesses[45,58], this complication has not yet been studied in a large prospective controlled study.
Table 1.
Studies reporting on natural orifice specimen extraction-colectomy
| Author | Type of study | Patients (n) | Type of surgery | Type of NOSE | Indication |
| Akamatsu et al[36], 2009 | Case series | 16 | Sigmoid resection | Transrectal | Malignant |
| Cheung et al[42], 2009 | Case series | 10 | Sigmoid resection | Transrectal | Malignant |
| Christoforidis et al[44], 2013 | Case-matched | 11 | Sigmoid resection | Transrectal | Benign |
| Costantino et al[45], 2012 | Case-matched | 17 | Sigmoid resection | Transrectal | Benign |
| Franklin et al[49], 2013 | Case series | 277 | Sigmoid and anterior resection | Transrectal | Benign and malignant |
| Fuchs et al[50], 2013 | Case series | 15 | Sigmoid resection | Transrectal | Benign |
| Han et al[53], 2013 | Case series | 34 | Sigmoid and anterior resection | Transrectal | Malignant |
| Leroy et al[58], 2011 | Case series | 16 | Sigmoid resection | Transrectal | Diverticulitis |
| Nishimura et al[61], 2011 | Case series | 16 | Sigmoid resection | Transrectal | Malignant |
| Saad et al[66], 2010 | Case series | 8 | Sigmoid resection | Transrectal | Benign and malignant |
| Wolthuis et al[73], 2011 | Case-matched | 21 | Sigmoid resection | Transrectal | Endometriosis |
| Wolthuis et al[74], 2011 | Case series | 21 | Sigmoid resection | Transrectal | Benign and malignant |
| Akamatsu et al[37], 2009 | Case series | 7 | TME | Transanal | Malignant |
| Bie et al[39], 2013 | Case series | 131 | TME | Transanal | Malignant |
| Choi et al[43], 2009 | Case series | 13 | TME | Transanal(11 patients) | Malignant |
| de Lacy et al[46], 2013 | Case series | 20 | TME | Transanal | Malignant |
| Dumont et al[47], 2012 | Case series | 4 | TME | Transanal | Malignant |
| Gaujoux et al[51], 2011 | Case series | 2 | TME | Transanal | Malignant |
| Hara et al[54], 2011 | Case series | 9 | Sigmoid resection | Transanal | Malignant |
| Kang et al[55], 2012 | Comparative | 53 | TME | Transanal | Malignant |
| Lacy et al[56], 2013 | Case series | 3 | TME | Transanal | Malignant |
| Lamadé et al[57], 2010 | Case series | 3 | RPC | Transanal | IBD (UC) |
| Marks et al[59], 2010 | Case series | 79 | TME | Transanal (36 TATA) | Malignant |
| Prete et al[64], 2007 | Case series | 10 | TME | Transanal | Malignant |
| Rullier et al[65], 2003 | Case series | 32 | TME | Transanal | Malignant |
| Sylla et al[67], 2013 | Case series | 5 | TME | Transanal | Malignant |
| Velthuis et al[70], 2013 | Case series | 5 | TME | Transanal | Malignant |
| Wang et al[71], 2013 | Case series | 21 | TME | Transanal (16 patients) | Malignant |
| Watanabe et al[72], 2000 | Case series | 7 | TME | Transanal | Malignant |
| Zorron et al[75], 2012 | Case series | 2 | TME | Transanal | Malignant |
| Abrao et al[35], 2005 | Case series | 8 | Sigmoid resection | Transvaginal | Endometriosis |
| Awad et al[38], 2011 | Case series | 14 | Right hemicolectomy | Transvaginal | Benign and malignant |
| Boni et al[40], 2007 | Case series | 11 | Sigmoid resection | Transvaginal | Endometriosis |
| Breitenstein et al[41], 2006 | Case series | 2 | Sigmoid resection (+ hysterectomy) | Transvaginal | Diverticulitis |
| Franklin et al[49], 2013 | Case series | 26 | Right hemicolectomy | Transvaginal | Benign and malignant |
| Ghezzi et al[52], 2008 | Case series | 33 | Sigmoid resection | Transvaginal | Endometriosis |
| McKenzie et al[60], 2010 | Case series | 4 | Right hemicolectomy | Transvaginal | Benign and malignant |
| Palanivelu et al[62], 2008 | Case series | 7 | Restorative proctocolectomy | Transvaginal | Fap |
| Park et al[63], 2011 | Case-matched | 34 | Right hemicolectomy | Transvaginal | Malignant |
| Tarantino et al[68], 2011 | Case series | 34 | Sigmoid resection | Transvaginal | Diverticulitis |
| Torres et al[69], 2012 | Case series | 21 | Sigmoid and high anterior resection | Transvaginal | Benign and malignant |
FAP: Familial adenomatous polyposis; IBD: Inflammatory bowel disease; UC: Ulcerative colitis; TATA: Transanal transabdominal; TME: Total mesorectal excision; RPC: Restorative proctocolectomy.
Table 2.
Operative details and outcome of natural orifice specimen extraction-colectomy
| Author | Ports | Protection | Anastomosis | Duration of surgery (min) | Morbidity (n, Dindo-score) | LOS (d) |
| Transrectal NOSE | ||||||
| Akamatsu et al[36], 2009 | 4 | None | TS | Mean 180 (137-257) | Wound infection (1, 1) | Mean 11 (8-14) |
| Cheung et al[42], 2009 | 5 | TEO | TS | Median 127.5 (105-170) | None | Median 7 (4-18) |
| Christoforidis et al[44], 2013 | 4 | Camera sleeve | TS | Median 200 (120-360) | Abscess (1, 3a), leakage (3b) and trocar hernia (3b) | Median 6 (4-33) |
| Costantino et al[45], 2012 | 3 | None | TS | 122 ± 36.5 | Bleeding (1, 1), fever (2, 2), abscess (1, 2), leakage (1, 3b) | 7.2 ± 4.9 |
| Franklin et al[49], 2013 | 4 | Retrieval bag | TS | 164.7 ± 47.5 | Leakage (3, 3b) | 6.9 ± 2.8 |
| Fuchs et al[50], 2013 | 3 | TEA | TS | Mean 131 (55-184) | Bleeding (1, 1), ileus (1, 2) | NA |
| Han et al[53], 2013 | 5 | TEM and bag | DS | Mean 151.6 (125-185) | Leakage (6, 3b) | Median 9 (7-66) |
| Leroy et al[58], 2011 | 3 | None | TS | Mean 120.9 (std 41.9) | Epigastric pain (1, 1) and transient fever (3, 2) | 6.1 ± 2.4 |
| Nishimura et al[61], 2011 | 5 | Wound retractor | DS | Mean 241 (188-309) | Leakage (1, 2) | Median 6 (4-16) |
| Saad et al[66], 2010 | 4 | McCarteny Tube | TS | 95-180 | None | 4-8 d |
| Wolthuis et al[73], 2011 | 4 | Retrieval bag | TS | Median 90 (85-105) | UTI (1, 2) | Median 6 (5-7) |
| Wolthuis et al[74], 2011 | 4 | Retrieval bag | TS | Median 105 (90-110) | Leakage (1, 3b) | Median 6 (5-7) |
| Transanal NOSE | ||||||
| Akamatsu et al[37], 2009 | 5 | None | DS | Median 299 (255-343) | None | Mean 25 (14-49) |
| Bie et al[39], 2013 | NA | None | SS | Median 166 (120-280) | None | Median 10 (8-17) |
| Choi et al[43], 2009 | 5 | Retrieval bag | SS | 260.8 ± 62.9 | Bleeding (1, 3a), leakage and bleeding (1, 3b/3b) | Median 7 (6-14) |
| de Lacy et al[46], 2013 | 3 | None | DS | 235 ± 56 | Retention (2, 1), ileus (1, 2), dehydration (1, 2) | 6.5 ± 3.1 |
| Dumont et al[47], 2012 | 1 | None | Hand-sewn | Median 360 (270-460) | Leakage (1, 3b) | Median 13 (10-21) |
| Gaujoux et al[51], 2011 | 1 | None | Hand-sewn | 195 and 210 | None | 5 and 6 |
| Hara et al[54], 2011 | 4 | None | DS | Median 293 (220-342) | None | NA |
| Kang et al[55], 2012 | 5 (6) | Retrieval bag | SS | Mean 357 std 66.8 | Leakage (4), abscess (2) | 9 ± 4.8 |
| Lacy et al[56], 2013 | 3 | None | SS | 125, 150, and 155 | Dehydration (1, 2) | 4, 5, and 5 |
| Lamadé et al[57], 2010 | 1 + TV assistance | None | DS | NA | None | 11, 12, and 14 |
| Marks et al[59], 2010 | 3-6 | None | Hand-sewn | NA | 19% minor, 11% major | Median 5 (3-24) |
| Prete et al[64], 2007 | NA | None | Hand-sewn | NA | Leakage (1, 3b), hemorrhagic gastropathy (1, 2) | Mean 8.5 (6-10) |
| Rullier et al[65], 2003 | NA | None | Hand-sewn | Median 420 (300-600) | 22% major | Median 9 (7-29) |
| Sylla et al[67], 2013 | 4 (5) | None | Hand-sewn | 274.6 ± 85.4 | Urinary dysfunction (2, 2), ileus (1, 2) | 4, 4, 4, 4, and 10 |
| Velthuis et al[70], 2013 | 1 | Wound retractor | Hand-sewn and SS | Median 175 (160-194) | Ileus and pneumonia (1, 2), abscess (1, 3b) | NA |
| Wang et al[71], 2013 | 3 | Retrieval bag | DS | 187 ± 35 | Ileus (1, 2) | Mean 7.5 (2-11) |
| Watanabe et al[72], 2000 | 5 | None | Hand-sewn | 280-450 | Leakage (1, 3b) | NA |
| Zorron et al[75], 2012 | 3 | None | Hand-sewn | 350 and 360 | None | 6 |
| Transvaginal NOSE | ||||||
| Abrao et al[35], 2005 | 4 | None | DS | Mean 177.5 (119-251) | None | Mean 4.13 (2-5) |
| Awad et al[38], 2011 | 5 | Retrieval bag | DS | Mean 229 (172-360) | Bleeding (1, 3b), ileus (3, 2) | Mean 9.6 (2-30) |
| Boni et al[40], 2007 | 4 | Retrieval bag | DS | 240 ± 63 | None | 5 ± 2 |
| Breitenstein et al[41], 2006 | 4 | None | DS | NA | C. difficile-colitis (1, 2), UTI (1, 2) | 15 and 9 |
| Franklin et al[49], 2013 | 4 | Retrieval bag | DS | 159 ± 27.1 | None | 5.5 ± 2.5 |
| Ghezzi et al[52], 2008 | 4 | None | DS | Median 290 (200-390) | Seroma (1, 3b), retention (3, 2) | 6.7 ± 1.8 |
| McKenzie et al[60], 2010 | 4 | Retrieval bag | DS | Mean 212.3 | Internal hernia (1, 3b) | 3, 4, 5 and 34 |
| Palanivelu et al[62], 2008 | 5 | Retrieval bag | DS | Mean 222.5 (165-280) | Leakage (1, 2) | Mean 25.5 (11-40) |
| Park et al[63], 2011 | 5 | Retrieval bag | DS | Mean 170.8 (std 46.4) | Ileus (1, 2), retention (1, 1), bleeding (2, 2) | 7.9 ± 0.8 |
| Tarantino et al[68], 2011 | 4 | Wound retractor | DS | Median 172.5 (107-312) | Leakage (1, 3b) | Median 6 (3-23) |
| Torres et al[69], 2012 | 4 | Wound retractor | DS | NA | NA | 3-6 |
C. difficile: Clostridium difficile; DS: Double stapled; LOS: Length of stay; NA: Not available; SS: Single stapled; TEA: Transanal endoscopic applicator; TEM: Transanal endoscopic microsurgery; TEO: Transanal endoscopic operation; TS: Triple stapled; TV: Transvaginal; UTI: Urinary tract infection.
TRANSANAL NOSE
TME optimizes outcome in patients with rectal cancer[82] and most patients now have the prospect of a restorative procedure to avoid a permanent colostomy[83]. Recent meta-analyses have shown that laparoscopic TME is feasible and safe, with an outcome comparable to open TME but with short-term benefits regarding postoperative recovery[84,85]. However, laparoscopic TME is a demanding procedure involving a significant learning curve[86]. One of the most difficult steps of laparoscopic TME is the mobilization and transection of the most distal part of the rectum. Specimen retrieval and the construction of a colonic J-pouch require an abdominal wall incision. The length of the incision will be adapted to the size of the specimen and the tumor. This extraction site is not without risk of morbidity. Wound infections rates of 9% have been documented albeit usually only local septic complications[87]. Additionally, acceptance of a shorter distal resection margin (1 cm)[88], neo-adjuvant chemoradiation with an increased interval to surgery (> 7 wk)[89] and the surgical technique of intersphincteric dissection have all increased the rates of “sphincter-preserving” surgery in patients with distal rectal cancer[83]. If intersphincteric dissection is required, the mobilized rectum can be extracted via the muscular anal canal avoiding any further abdominal incision. During this perineal or transanal phase, a neorectum (e.g., rectoplasty[65,90], terminolateral anastomosis[91] or colonic J-pouch[92,93]) or a straight coloanal anastomosis can be created. In both cases, mobilization of the splenic flexure is most often necessary. In 1997, Teramoto et al[94] described a new technique of laparoscopic TME with intersphincteric dissection and “per anum” specimen retrieval. From that same group data from a small cohort of patients were reported by Watanabe et al[72] and Teramoto et al[94]. In 2003, Rullier et al[65] added coloplasty to this technique, and Person et al[23] described the original technique for totally laparoscopic low anterior resection with transperineal handsewn colonic J-pouch anastomosis for low rectal cancer. A similar technique of pouch reconstruction during perineal rectosigmoidectomy for total full-thickness rectal prolapse was described in 1998. These authors advised the creation of a colonic pouch to improve functional results. In 2007, Prete et al[64] published results using the same technique in a small series of 10 patients. Since then, the number of publications regarding transanal NOSE techniques has gradually increased (Table 1, Figure 2). Although almost all studies have reported cases concerning colorectal malignant disease with the performance of a TME, specimens were extracted via an unprotected anus in 14 of 17 studies (82%). In laparoscopic resections for malignancies, port-site metastases were an issue almost 20 years ago and a temporary moratorium was called[95,96]. Thus, a word of caution may be of value when specimens containing a tumor are extracted through an unprotected orifice (Figure 3). Whether this new approach has similar oncologic outcomes regarding local recurrence, disease-free survival and cancer-specific survival have yet to be studied in prospective trials comparing transanal TME with conventional TME. Operative techniques differ amongst studies with a different number of ports used and different ways of creating a coloanal anastomosis: hand-sewn in 50% of studies, single-stapled in 22%, and double-stapled in 28% (Table 2). Due to these differences in technique, it is impossible to perform inter-study comparisons of data concerning operative details; such as duration of surgery and postoperative outcome, e.g., complications and length of hospital stay. The ongoing evolution of minimally invasive laparoscopic surgery has led to the introduction of robotic surgery to perform TME[97,98]. The use of robotic platforms has influenced the treatment of complex pelvic disorders and for a TME the learning curve involves 21-23 cases[99-101]. The high-definition 3D system, ergonomic positioning of the surgeon, instrument articulation with greater precision and absence of tremor might lead to a higher accuracy, a more precise dissection and, possibly, fewer postoperative complications. However, a major limitation for the use of a robotic platform is its high cost. Only 1 study reported on the use of robotics in transanal NOSE[55], describing a cohort of 53 patients who underwent robotic-assisted laparoscopic TME with transanal specimen extraction. The short-term postoperative outcome was comparable to that of a group of 66 patients, but robotic assistance in transanal NOSE-TME was associated with less pain and faster recovery. In reviewing the literature regarding transanal NOSE, the differences must be highlighted between techniques describing laparoscopic TME with the anus as the extraction site and techniques describing transanal TME. Both procedures are transanal NOSE techniques, but in the latter, TME is performed in a reversed way. A laparoscopic low anterior resection with transanal pull-through and hand-sewn anastomosis could be indicated in patients requiring TME with coloanal anastomosis for distal rectal tumors. Transanal rectal excision by transanal minimally invasive surgery is an option to improve the difficult visualization of the distal rectum, particularly in obese male patients with a narrow pelvis. Recent publications concerning transanal rectal excision, or so-called “down-to-up” or reversed TME, show the feasibility and safety of this new technique, reporting intact TME specimens and adequate lymph node harvest. In the future, large prospective studies should focus on the functional and oncological outcomes. If laparoscopy can be omitted in this setting, true NOTES might become possible in a consecutive series of patients.
Figure 3.
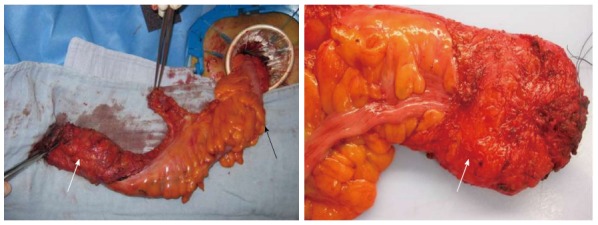
Transanal natural orifice specimen extraction. A laparoscopic transanal transabdominal-total mesorectal excision (TME) was performed. The TME-specimen with the vascular pedicle (black arrow) and colon used for the reconstruction and the hand-sewn anastomosis (white arrow) can be observed.
TRANSVAGINAL NOSE
Transvaginal NOSE using a posterior colpotomy has extensively been reported during gynecologic laparoscopic procedures[102-104]. Although the peritoneal cavity is entered by deliberately opening the vagina, it appears that a vaginotomy or so-called colpotomy will not increase postoperative morbidity. A colpotomy is safe and does not lead to surgical site infections or dyspareunia[105,106]. Moreover, a randomized trial showed less postoperative pain when comparing transvaginal and transumbilical specimen extraction for adnexal masses[107]. In 1996, Redwine et al[108] first described a segmental colectomy with transvaginal extraction and hand-sewn anastomosis for bowel endometriosis. A combined laparoscopic-transvaginal approach, with transvaginal specimen extraction, has been published for the treatment of colorectal diseases. Moreover, several authors have reported short-term results (Table 1). A total of 11 studies including 194 patients were found regarding transvaginal specimen extraction in laparoscopic colorectal surgery. The main advantage of transvaginal NOSE is the possibility to extract large specimens from both right-sided and left-sided colonic resections, but this approach is only applicable in female patients with a non-intact hymen who give informed consent. No randomized controlled trials could be found and apart from 1 case-matched study, only small case series were included. Multiple variants of transvaginal NOSE-colectomy have been described, making the evidence poor. Four studies have reported right-sided disease and 6 studies left-sided disease (Table 2). Palanivelu et al[62] described the results of 7 female patients with familial adenomatous polyposis, who underwent restorative proctocolectomy with ileoanal pouch anastomosis. All specimens were extracted through the vagina in a retrieval bag. A 15 cm ileoanal pouch was created completely laparoscopically with endostaplers, and the anvil of the circular stapler was inserted and secured by a purse string. The double-stapled anastomosis was performed in a standardized manner. One patient developed an anastomotic leakage, requiring drainage and antibiotics. The mean length of hospital stay was 25.5 d in this series. For a right hemicolectomy, a double-stapled anastomosis was performed in all cases and the specimen was extracted in a retrieval bag to protect the vagina. The difficulty concerning laparoscopic right hemicolectomy is the creation of an intracorporeal anastomosis[109]. Both the ileum and colon should be cleaned of mesentery and omental fat to allow adequate and safe stapling and this can sometimes be difficult in obese patients. Moreover, the remaining enterocolostomy should be closed with an intracorporeal suture. However, specimen extraction and extracorporeal anastomosis can also pose a problem in obese patients, risking bleeding and twisting of the terminal ileum[110,111]. The mean BMIs were 31.7, 24.5, and 23.9 kg/m2 in the studies of Awad et al[38], McKenzie et al[60], and Park et al[63], respectively, indicating that intracorporeal anastomosis is feasible in this group of patients. These authors reported small case series concerning laparoscopic right hemicolectomy with transvaginal NOSE and intracorporeal anastomosis for benign and malignant right-sided colorectal disease. The mean operative times were 229 min and 212 min for Awad et al[38] and McKenzie et al[60], respectively, but only 171 min for Park and colleagues. Park et al[112] had already published their experience with transvaginal NOSE in 2010. Therefore, the shorter operative times included in this review could reflect the learning curve. Franklin et al[49] had a mean operative time of 159 min in their cohort of 26 patients. Postoperative ileus, internal hernia and bleeding for which reintervention was necessary in 2 patients contributed to the observed postoperative morbidity. This led to a mean length of hospital stay of more than 1 wk in 3 studies and to a mean of 5.5 d in the study published by Franklin et al[49]. Six authors reported transvaginal NOSE for sigmoid and high anterior resection in a total of 109 patients. The indications were endometriosis, diverticular disease and cancer. In all studies, 4 ports were used and intracorporeal anastomoses were performed with the double-stapling technique (Figure 4). In 3 studies, the vagina was protected using either a retrieval bag or a wound retractor[40,68,69]. One anastomotic leak was reported requiring reintervention. The length of hospital stay was approximately 6 d in the largest series. In conclusion, transvaginal NOSE-colectomy could have a place in laparoscopic colorectal surgery to treat both right-sided and left-sided disease. It might pave the way for transvaginal NOTES and scarless surgery in selected patients.
Figure 4.
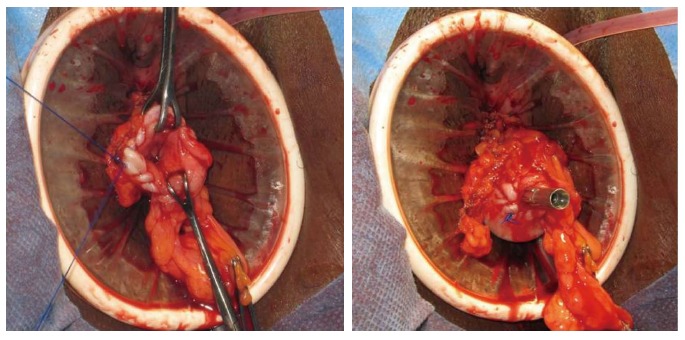
Transvaginal natural orifice specimen extraction. The sigmoid colon has been resected, and the anvil from a 29 mm circular stapler has been sutured into the proximal colon with a purse string. Note the wound retractor protecting the vagina.
CONCLUSION
A state-of-the-art review was presented concerning laparoscopic NOSE-colectomy. The reduction of incision-related morbidity is one of the goals of modern minimally invasive laparoscopic colorectal surgery. Abdominal wall incisions can still cause postoperative morbidity, such as infection, pain and trocar-site incisional hernia. In addition to reports on operative and oncological outcome, surgical technique and novel methods to reduce access trauma have become important issues in current practice. This narrative review described the technical possibilities and shortcomings in laparoscopic NOSE-colectomy. A new era has dawned to further minimize access trauma and to explore new surgical strategies in bridging conventional laparoscopic surgery to pure human NOTES procedures. NOSE could be the next step in minimizing minimally invasive surgery. Although NOSE theoretically has the potential to improve outcome in laparoscopic colorectal surgery, its implementation in daily practice and its assumed benefits have yet to be studied in prospective controlled trials.
Footnotes
P- Reviewer: Mures T, Wong GLH S- Editor: Gou SX L- Editor: A E- Editor: Ma S
References
- 1.Laurent C, Leblanc F, Bretagnol F, Capdepont M, Rullier E. Long-term wound advantages of the laparoscopic approach in rectal cancer. Br J Surg. 2008;95:903–908. doi: 10.1002/bjs.6134. [DOI] [PubMed] [Google Scholar]
- 2.Alba Mesa F, Amaya Cortijo A, Romero Fernandez JM, Komorowski AL, Sanchez Hurtado MA, Fernandez Ortega E, Sanchez Margallo FM. Transvaginal sigmoid cancer resection: first case with 12 months of follow-up--technique description. J Laparoendosc Adv Surg Tech A. 2012;22:587–590. doi: 10.1089/lap.2011.0469. [DOI] [PubMed] [Google Scholar]
- 3.Allam M, Piskun G, Fogler R. Laparoscopic-assisted abdominoperineal proctosigmoidectomy for rectal prolapse. A new technique. Surg Endosc. 1997;11:150–151. doi: 10.1007/s004649900319. [DOI] [PubMed] [Google Scholar]
- 4.Atallah S, Nassif G, Polavarapu H, deBeche-Adams T, Ouyang J, Albert M, Larach S. Robotic-assisted transanal surgery for total mesorectal excision (RATS-TME): a description of a novel surgical approach with video demonstration. Tech Coloproctol. 2013;17:441–447. doi: 10.1007/s10151-013-1039-2. [DOI] [PubMed] [Google Scholar]
- 5.Awad ZT. Laparoscopic subtotal colectomy with transrectal extraction of the colon and ileorectal anastomosis. Surg Endosc. 2012;26:869–871. doi: 10.1007/s00464-011-1926-4. [DOI] [PubMed] [Google Scholar]
- 6.Cheung TP, Cheung HY, Ng LW, Chung CC, Li MK. Hybrid NOTES colectomy for right-sided colonic tumors. Asian J Endosc Surg. 2012;5:46–49. doi: 10.1111/j.1758-5910.2011.00106.x. [DOI] [PubMed] [Google Scholar]
- 7.Co CS, Cheung HY, Yau KK, Chung CC, Li M. Combined single-port and endoluminal technique for laparoscopic anterior resection. Surg Laparosc Endosc Percutan Tech. 2010;20:253–256. doi: 10.1097/SLE.0b013e3181e21b33. [DOI] [PubMed] [Google Scholar]
- 8.Dozois EJ, Larson DW, Dowdy SC, Poola VP, Holubar SD, Cima RR. Transvaginal colonic extraction following combined hysterectomy and laparoscopic total colectomy: a natural orifice approach. Tech Coloproctol. 2008;12:251–254. doi: 10.1007/s10151-008-0428-4. [DOI] [PubMed] [Google Scholar]
- 9.Ebert AD, Burkhardt T, Parlayan S, Riediger H, Papadopoulos T. Transvaginal-laparoscopic anterior rectum resection in a hysterectomized woman with deep-infiltrating endometriosis: Description of a gynecologic natural orifice transendoluminal surgery approach. J Minim Invasive Gynecol. 2009;16:231–235. doi: 10.1016/j.jmig.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Facy O, De Magistris L, Poulain V, Goergen M, Orlando G, Azagra JS. Right colectomy: value of the totally laparoscopic approach. J Visc Surg. 2013;150:207–212. doi: 10.1016/j.jviscsurg.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 11.Franklin ME, Kelley H, Kelley M, Brestan L, Portillo G, Torres J. Transvaginal extraction of the specimen after total laparoscopic right hemicolectomy with intracorporeal anastomosis. Surg Laparosc Endosc Percutan Tech. 2008;18:294–298. doi: 10.1097/SLE.0b013e3181772d8b. [DOI] [PubMed] [Google Scholar]
- 12.García Flórez LJ, Argüelles J, Quijada B, Alvarez V, Galarraga MA, Graña JL. Transvaginal specimen extraction in a laparoscopic anterior resection of a sigmoid colon neoplasia with en bloc right salpingo-oophorectomy. Tech Coloproctol. 2010;14:161–163. doi: 10.1007/s10151-009-0561-8. [DOI] [PubMed] [Google Scholar]
- 13.Knol J, D’Hondt M, Dozois EJ, Vanden Boer J, Malisse P. Laparoscopic-assisted sigmoidectomy with transanal specimen extraction: a bridge to NOTES? Tech Coloproctol. 2009;13:65–68. doi: 10.1007/s10151-009-0461-y. [DOI] [PubMed] [Google Scholar]
- 14.Lacy AM, Adelsdorfer C. Totally transrectal endoscopic total mesorectal excision (TME) Colorectal Dis. 2011;13 Suppl 7:43–46. doi: 10.1111/j.1463-1318.2011.02781.x. [DOI] [PubMed] [Google Scholar]
- 15.Lacy AM, Saavedra-Perez D, Bravo R, Adelsdorfer C, Aceituno M, Balust J. Minilaparoscopy-assisted natural orifice total colectomy: technical report of a minilaparoscopy-assisted transrectal resection. Surg Endosc. 2012;26:2080–2085. doi: 10.1007/s00464-011-2117-z. [DOI] [PubMed] [Google Scholar]
- 16.Leroy J, Barry BD, Melani A, Mutter D, Marescaux J. No-scar transanal total mesorectal excision: the last step to pure NOTES for colorectal surgery. JAMA Surg. 2013;148:226–30; discussion 231. doi: 10.1001/jamasurg.2013.685. [DOI] [PubMed] [Google Scholar]
- 17.Leroy J, Diana M, Wall J, Costantino F, D’Agostino J, Marescaux J. Laparo-endoscopic single-site (LESS) with transanal natural orifice specimen extraction (NOSE) sigmoidectomy: a new step before pure colorectal natural orifices transluminal endoscopic surgery (NOTES®) J Gastrointest Surg. 2011;15:1488–1492. doi: 10.1007/s11605-011-1557-z. [DOI] [PubMed] [Google Scholar]
- 18.Leroy J, Perretta S, Diana M, Wall J, Lindner V, Harrison M, Marescaux J. An original endoluminal magnetic anastomotic device allowing pure NOTES transgastric and transrectal sigmoidectomy in a porcine model: proof of concept. Surg Innov. 2012;19:109–116. doi: 10.1177/1553350611429029. [DOI] [PubMed] [Google Scholar]
- 19.Makris KI, Rieder E, Kastenmeier AS, Swanström LL. Video. Transanal specimen retrieval using the transanal endoscopic microsurgery (TEM) system in minimally invasive colon resection. Surg Endosc. 2012;26:1161–1162. doi: 10.1007/s00464-011-2021-6. [DOI] [PubMed] [Google Scholar]
- 20.Messori P, Faller E, Albornoz J, Leroy J, Wattiez A. Laparoscopic sigmoidectomy for endometriosis with transanal specimen extraction. J Minim Invasive Gynecol. 2013;20:412. doi: 10.1016/j.jmig.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 21.Msika S, Iannelli A, Flamant Y, Hay JM. Laparoscopic sigmoid colectomy with intracorporeal hand-sewn anastomosis. Surg Endosc. 2000;14:866. doi: 10.1007/s004640040002. [DOI] [PubMed] [Google Scholar]
- 22.Ooi BS, Quah HM, Fu CW, Eu KW. Laparoscopic high anterior resection with natural orifice specimen extraction (NOSE) for early rectal cancer. Tech Coloproctol. 2009;13:61–64. doi: 10.1007/s10151-009-0460-z. [DOI] [PubMed] [Google Scholar]
- 23.Person B, Vivas DA, Wexner SD. Totally laparoscopic low anterior resection with transperineal handsewn colonic J-pouch anal anastomosis for low rectal cancer. Surg Endosc. 2006;20:700–702. doi: 10.1007/s00464-005-0581-z. [DOI] [PubMed] [Google Scholar]
- 24.Reissman P, Weiss E, Teoh TA, Cohen SM, Wexner SD. Laparoscopic-assisted perineal rectosigmoidectomy for rectal prolapse. Surg Laparosc Endosc. 1995;5:217–218. [PubMed] [Google Scholar]
- 25.Saad S, Schmischke D, Martin C, Schieren T. Hybrid laparoscopic colectomy with transluminal colonoscopic specimen extraction--a step toward natural orifice surgery. Endoscopy. 2010;42 Suppl 2:E346–E347. doi: 10.1055/s-0030-1255978. [DOI] [PubMed] [Google Scholar]
- 26.Sanchez JE, Rasheid SH, Krieger BR, Frattini JC, Marcet JE. Laparoscopic-assisted transvaginal approach for sigmoidectomy and rectocolpopexy. JSLS. 2009;13:217–220. [PMC free article] [PubMed] [Google Scholar]
- 27.Shelygin YA, Frolov SA, Achkasov SI, Sushkov OI, Shakhmatov DG. Transvaginal laparo-endoscopic single-site sigmoidectomy. Tech Coloproctol. 2012;16:251–253. doi: 10.1007/s10151-012-0809-6. [DOI] [PubMed] [Google Scholar]
- 28.Stipa F, Giaccaglia V, Santini E, Tammaro L. Totally double laparoscopic colon resection with intracorporeal anastomosis and transvaginal specimens extraction. Int J Colorectal Dis. 2011;26:815–816. doi: 10.1007/s00384-010-1068-5. [DOI] [PubMed] [Google Scholar]
- 29.Sylla P. Current experience and future directions of completely NOTES colorectal resection. World J Gastrointest Surg. 2010;2:193–198. doi: 10.4240/wjgs.v2.i6.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Takayama S, Takahashi H, Takeyama H. Pure laparoscopic sigmoidectomy. Surg Laparosc Endosc Percutan Tech. 2011;21:e104–e106. doi: 10.1097/SLE.0b013e31820df955. [DOI] [PubMed] [Google Scholar]
- 31.Tuech JJ, Bridoux V, Kianifard B, Schwarz L, Tsilividis B, Huet E, Michot F. Natural orifice total mesorectal excision using transanal port and laparoscopic assistance. Eur J Surg Oncol. 2011;37:334–335. doi: 10.1016/j.ejso.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 32.Wilson JI, Dogiparthi KK, Hebblethwaite N, Clarke MD. Laparoscopic right hemicolectomy with posterior colpotomy for transvaginal specimen retrieval. Colorectal Dis. 2007;9:662. doi: 10.1111/j.1463-1318.2007.01313.x. [DOI] [PubMed] [Google Scholar]
- 33.Wolthuis AM, Cini C, Penninckx F, D’Hoore A. Transanal single port access to facilitate distal rectal mobilization in laparoscopic rectal sleeve resection with hand-sewn coloanal anastomosis. Tech Coloproctol. 2012;16:161–165. doi: 10.1007/s10151-011-0795-0. [DOI] [PubMed] [Google Scholar]
- 34.Zhang H, Zhang YS, Jin XW, Li MZ, Fan JS, Yang ZH. Transanal single-port laparoscopic total mesorectal excision in the treatment of rectal cancer. Tech Coloproctol. 2013;17:117–123. doi: 10.1007/s10151-012-0882-x. [DOI] [PubMed] [Google Scholar]
- 35.Abrao MS, Sagae UE, Gonzales M, Podgaec S, Dias JA. Treatment of rectosigmoid endometriosis by laparoscopically assisted vaginal rectosigmoidectomy. Int J Gynaecol Obstet. 2005;91:27–31. doi: 10.1016/j.ijgo.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 36.Akamatsu H, Omori T, Oyama T, Tori M, Ueshima S, Nakahara M, Abe T, Nishida T. Totally laparoscopic sigmoid colectomy: a simple and safe technique for intracorporeal anastomosis. Surg Endosc. 2009;23:2605–2609. doi: 10.1007/s00464-009-0406-6. [DOI] [PubMed] [Google Scholar]
- 37.Akamatsu H, Omori T, Oyama T, Tori M, Ueshima S, Nishida T, Nakahara M, Abe T. Totally laparoscopic low anterior resection for lower rectal cancer: combination of a new technique for intracorporeal anastomosis with prolapsing technique. Dig Surg. 2009;26:446–450. doi: 10.1159/000239761. [DOI] [PubMed] [Google Scholar]
- 38.Awad ZT, Qureshi I, Seibel B, Sharma S, Dobbertien MA. Laparoscopic right hemicolectomy with transvaginal colon extraction using a laparoscopic posterior colpotomy: a 2-year series from a single institution. Surg Laparosc Endosc Percutan Tech. 2011;21:403–408. doi: 10.1097/SLE.0b013e31823945ac. [DOI] [PubMed] [Google Scholar]
- 39.Bie M, Wei ZQ. A new colorectal/coloanal anastomotic technique in sphincter-preserving operation for lower rectal carcinoma using transanal pull-through combined with single stapling technique. Int J Colorectal Dis. 2013;28:1517–1522. doi: 10.1007/s00384-013-1723-8. [DOI] [PubMed] [Google Scholar]
- 40.Boni L, Tenconi S, Beretta P, Cromi A, Dionigi G, Rovera F, Dionigi R, Ghezzi F. Laparoscopic colorectal resections with transvaginal specimen extraction for severe endometriosis. Surg Oncol. 2007;16 Suppl 1:S157–S160. doi: 10.1016/j.suronc.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 41.Breitenstein S, Dedes KJ, Bramkamp M, Hess T, Decurtins M, Clavien PA. Synchronous laparoscopic sigmoid resection and hysterectomy with transvaginal specimen removal. J Laparoendosc Adv Surg Tech A. 2006;16:286–289. doi: 10.1089/lap.2006.16.286. [DOI] [PubMed] [Google Scholar]
- 42.Cheung HY, Leung AL, Chung CC, Ng DC, Li MK. Endo-laparoscopic colectomy without mini-laparotomy for left-sided colonic tumors. World J Surg. 2009;33:1287–1291. doi: 10.1007/s00268-009-0006-6. [DOI] [PubMed] [Google Scholar]
- 43.Choi GS, Park IJ, Kang BM, Lim KH, Jun SH. A novel approach of robotic-assisted anterior resection with transanal or transvaginal retrieval of the specimen for colorectal cancer. Surg Endosc. 2009;23:2831–2835. doi: 10.1007/s00464-009-0484-5. [DOI] [PubMed] [Google Scholar]
- 44.Christoforidis D, Clerc D, Demartines N. Transrectal specimen extraction after laparoscopic left colectomy: a case-matched study. Colorectal Dis. 2013;15:347–353. doi: 10.1111/codi.12006. [DOI] [PubMed] [Google Scholar]
- 45.Costantino FA, Diana M, Wall J, Leroy J, Mutter D, Marescaux J. Prospective evaluation of peritoneal fluid contamination following transabdominal vs. transanal specimen extraction in laparoscopic left-sided colorectal resections. Surg Endosc. 2012;26:1495–1500. doi: 10.1007/s00464-011-2066-6. [DOI] [PubMed] [Google Scholar]
- 46.de Lacy AM, Rattner DW, Adelsdorfer C, Tasende MM, Fernández M, Delgado S, Sylla P, Martínez-Palli G. Transanal natural orifice transluminal endoscopic surgery (NOTES) rectal resection: “down-to-up” total mesorectal excision (TME)--short-term outcomes in the first 20 cases. Surg Endosc. 2013;27:3165–3172. doi: 10.1007/s00464-013-2872-0. [DOI] [PubMed] [Google Scholar]
- 47.Dumont F, Goéré D, Honoré C, Elias D. Transanal endoscopic total mesorectal excision combined with single-port laparoscopy. Dis Colon Rectum. 2012;55:996–1001. doi: 10.1097/DCR.0b013e318260d3a0. [DOI] [PubMed] [Google Scholar]
- 48.Eshuis EJ, Voermans RP, Stokkers PC, van Berge Henegouwen MI, Fockens P, Bemelman WA. Laparoscopic resection with transcolonic specimen extraction for ileocaecal Crohn’s disease. Br J Surg. 2010;97:569–574. doi: 10.1002/bjs.6932. [DOI] [PubMed] [Google Scholar]
- 49.Franklin ME, Liang S, Russek K. Natural orifice specimen extraction in laparoscopic colorectal surgery: transanal and transvaginal approaches. Tech Coloproctol. 2013;17 Suppl 1:S63–S67. doi: 10.1007/s10151-012-0938-y. [DOI] [PubMed] [Google Scholar]
- 50.Fuchs KH, Breithaupt W, Varga G, Schulz T, Reinisch A, Josipovic N. Transanal hybrid colon resection: from laparoscopy to NOTES. Surg Endosc. 2013;27:746–752. doi: 10.1007/s00464-012-2534-7. [DOI] [PubMed] [Google Scholar]
- 51.Gaujoux S, Bretagnol F, Au J, Ferron M, Panis Y. Single port access proctectomy with total mesorectal excision and intersphincteric resection with a primary transanal approach. Colorectal Dis. 2011;13:e305–e307. doi: 10.1111/j.1463-1318.2011.02676.x. [DOI] [PubMed] [Google Scholar]
- 52.Ghezzi F, Cromi A, Ciravolo G, Rampinelli F, Braga M, Boni L. A new laparoscopic-transvaginal technique for rectosigmoid resection in patients with endometriosis. Fertil Steril. 2008;90:1964–1968. doi: 10.1016/j.fertnstert.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 53.Han Y, He YG, Zhang HB, Lv KZ, Zhang YJ, Lin MB, Yin L. Total laparoscopic sigmoid and rectal surgery in combination with transanal endoscopic microsurgery: a preliminary evaluation in China. Surg Endosc. 2013;27:518–524. doi: 10.1007/s00464-012-2471-5. [DOI] [PubMed] [Google Scholar]
- 54.Hara M, Takayama S, Sato M, Imafuji H, Takahashi H, Takeyama H. Laparoscopic anterior resection for colorectal cancer without minilaparotomy using transanal bowel reversing retrieval. Surg Laparosc Endosc Percutan Tech. 2011;21:e235–e238. doi: 10.1097/SLE.0b013e3182297667. [DOI] [PubMed] [Google Scholar]
- 55.Kang J, Min BS, Hur H, Kim NK, Lee KY. Transanal specimen extraction in robotic rectal cancer surgery. Br J Surg. 2012;99:133–136. doi: 10.1002/bjs.7719. [DOI] [PubMed] [Google Scholar]
- 56.Lacy AM, Adelsdorfer C, Delgado S, Sylla P, Rattner DW. Minilaparoscopy-assisted transrectal low anterior resection (LAR): a preliminary study. Surg Endosc. 2013;27:339–346. doi: 10.1007/s00464-012-2443-9. [DOI] [PubMed] [Google Scholar]
- 57.Lamadé W, Ulmer C, Hochberger J, Matthes K, Friedrich C, Thon KP. Trilumenal hybrid-NOS proctocolectomy. Surg Innov. 2010;17:164–169. doi: 10.1177/1553350610365702. [DOI] [PubMed] [Google Scholar]
- 58.Leroy J, Costantino F, Cahill RA, D’Agostino J, Morales A, Mutter D, Marescaux J. Laparoscopic resection with transanal specimen extraction for sigmoid diverticulitis. Br J Surg. 2011;98:1327–1334. doi: 10.1002/bjs.7517. [DOI] [PubMed] [Google Scholar]
- 59.Marks J, Mizrahi B, Dalane S, Nweze I, Marks G. Laparoscopic transanal abdominal transanal resection with sphincter preservation for rectal cancer in the distal 3 cm of the rectum after neoadjuvant therapy. Surg Endosc. 2010;24:2700–2707. doi: 10.1007/s00464-010-1028-8. [DOI] [PubMed] [Google Scholar]
- 60.McKenzie S, Baek JH, Wakabayashi M, Garcia-Aguilar J, Pigazzi A. Totally laparoscopic right colectomy with transvaginal specimen extraction: the authors’ initial institutional experience. Surg Endosc. 2010;24:2048–2052. doi: 10.1007/s00464-009-0870-z. [DOI] [PubMed] [Google Scholar]
- 61.Nishimura A, Kawahara M, Suda K, Makino S, Kawachi Y, Nikkuni K. Totally laparoscopic sigmoid colectomy with transanal specimen extraction. Surg Endosc. 2011;25:3459–3463. doi: 10.1007/s00464-011-1716-z. [DOI] [PubMed] [Google Scholar]
- 62.Palanivelu C, Rangarajan M, Jategaonkar PA, Anand NV. An innovative technique for colorectal specimen retrieval: a new era of „natural orifice specimen extraction“ (N.O.S.E) Dis Colon Rectum. 2008;51:1120–1124. doi: 10.1007/s10350-008-9316-2. [DOI] [PubMed] [Google Scholar]
- 63.Park JS, Choi GS, Kim HJ, Park SY, Jun SH. Natural orifice specimen extraction versus conventional laparoscopically assisted right hemicolectomy. Br J Surg. 2011;98:710–715. doi: 10.1002/bjs.7419. [DOI] [PubMed] [Google Scholar]
- 64.Prete F, Prete FP, De Luca R, Nitti P, Sammarco D, Preziosa G. Restorative proctectomy with colon pouch-anal anastomosis by laparoscopic transanal pull-through: an available option for low rectal cancer? Surg Endosc. 2007;21:91–96. doi: 10.1007/s00464-004-9263-5. [DOI] [PubMed] [Google Scholar]
- 65.Rullier E, Sa Cunha A, Couderc P, Rullier A, Gontier R, Saric J. Laparoscopic intersphincteric resection with coloplasty and coloanal anastomosis for mid and low rectal cancer. Br J Surg. 2003;90:445–451. doi: 10.1002/bjs.4052. [DOI] [PubMed] [Google Scholar]
- 66.Saad S, Hosogi H. Natural orifice specimen extraction for avoiding laparotomy in laparoscopic left colon resections: a new approach using the McCartney tube and the tilt top anvil technique. J Laparoendosc Adv Surg Tech A. 2010;20:689–692. doi: 10.1089/lap.2010.0303. [DOI] [PubMed] [Google Scholar]
- 67.Sylla P, Bordeianou LG, Berger D, Han KS, Lauwers GY, Sahani DV, Sbeih MA, Lacy AM, Rattner DW. A pilot study of natural orifice transanal endoscopic total mesorectal excision with laparoscopic assistance for rectal cancer. Surg Endosc. 2013;27:3396–3405. doi: 10.1007/s00464-013-2922-7. [DOI] [PubMed] [Google Scholar]
- 68.Tarantino I, Linke GR, Lange J, Siercks I, Warschkow R, Zerz A. Transvaginal rigid-hybrid natural orifice transluminal endoscopic surgery technique for anterior resection treatment of diverticulitis: a feasibility study. Surg Endosc. 2011;25:3034–3042. doi: 10.1007/s00464-011-1666-5. [DOI] [PubMed] [Google Scholar]
- 69.Torres RA, Orban RD, Tocaimaza L, Vallejos Pereira G, Arévalo JR. Transvaginal specimen extraction after laparoscopic colectomy. World J Surg. 2012;36:1699–1702. doi: 10.1007/s00268-012-1528-x. [DOI] [PubMed] [Google Scholar]
- 70.Velthuis S, van den Boezem PB, van der Peet DL, Cuesta MA, Sietses C. Feasibility study of transanal total mesorectal excision. Br J Surg. 2013;100:828–31; discussion 831. doi: 10.1002/bjs.9069. [DOI] [PubMed] [Google Scholar]
- 71.Wang Q, Wang C, Sun DH, Kharbuja P, Cao XY. Laparoscopic total mesorectal excision with natural orifice specimen extraction. World J Gastroenterol. 2013;19:750–754. doi: 10.3748/wjg.v19.i5.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Watanabe M, Teramoto T, Hasegawa H, Kitajima M. Laparoscopic ultralow anterior resection combined with per anum intersphincteric rectal dissection for lower rectal cancer. Dis Colon Rectum. 2000;43:S94–S97. doi: 10.1007/BF02237232. [DOI] [PubMed] [Google Scholar]
- 73.Wolthuis AM, Meuleman C, Tomassetti C, D’Hooghe T, Fieuws S, Penninckx F, D’Hoore A. Laparoscopic sigmoid resection with transrectal specimen extraction: a novel technique for the treatment of bowel endometriosis. Hum Reprod. 2011;26:1348–1355. doi: 10.1093/humrep/der072. [DOI] [PubMed] [Google Scholar]
- 74.Wolthuis AM, Penninckx F, D’Hoore A. Laparoscopic sigmoid resection with transrectal specimen extraction has a good short-term outcome. Surg Endosc. 2011;25:2034–2038. doi: 10.1007/s00464-010-1472-5. [DOI] [PubMed] [Google Scholar]
- 75.Zorron R, Phillips HN, Coelho D, Flach L, Lemos FB, Vassallo RC. Perirectal NOTES access: “down-to-up” total mesorectal excision for rectal cancer. Surg Innov. 2012;19:11–19. doi: 10.1177/1553350611409956. [DOI] [PubMed] [Google Scholar]
- 76.Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114–117. doi: 10.1016/s0016-5107(04)01309-4. [DOI] [PubMed] [Google Scholar]
- 77.Rattner D, Kalloo A. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc. 2006;20:329–333. doi: 10.1007/s00464-005-3006-0. [DOI] [PubMed] [Google Scholar]
- 78.Guenaga KK, Matos D, Wille-Jørgensen P. Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev. 2009;(1):CD001544. doi: 10.1002/14651858.CD001544.pub3. [DOI] [PubMed] [Google Scholar]
- 79.Darzi A, Super P, Guillou PJ, Monson JR. Laparoscopic sigmoid colectomy: total laparoscopic approach. Dis Colon Rectum. 1994;37:268–271. doi: 10.1007/BF02048165. [DOI] [PubMed] [Google Scholar]
- 80.Franklin ME, Ramos R, Rosenthal D, Schuessler W. Laparoscopic colonic procedures. World J Surg. 1993;17:51–56. doi: 10.1007/BF01655705. [DOI] [PubMed] [Google Scholar]
- 81.Wolthuis AM, Van Geluwe B, Fieuws S, Penninckx F, D’Hoore A. Laparoscopic sigmoid resection with transrectal specimen extraction: a systematic review. Colorectal Dis. 2012;14:1183–1188. doi: 10.1111/j.1463-1318.2011.02869.x. [DOI] [PubMed] [Google Scholar]
- 82.Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet. 1986;1:1479–1482. doi: 10.1016/s0140-6736(86)91510-2. [DOI] [PubMed] [Google Scholar]
- 83.Rullier E, Denost Q, Vendrely V, Rullier A, Laurent C. Low rectal cancer: classification and standardization of surgery. Dis Colon Rectum. 2013;56:560–567. doi: 10.1097/DCR.0b013e31827c4a8c. [DOI] [PubMed] [Google Scholar]
- 84.Breukink S, Pierie J, Wiggers T. Laparoscopic versus open total mesorectal excision for rectal cancer. Cochrane Database Syst Rev. 2006;(4):CD005200. doi: 10.1002/14651858.CD005200.pub2. [DOI] [PubMed] [Google Scholar]
- 85.Xiong B, Ma L, Zhang C. Laparoscopic versus open total mesorectal excision for middle and low rectal cancer: a meta-analysis of results of randomized controlled trials. J Laparoendosc Adv Surg Tech A. 2012;22:674–684. doi: 10.1089/lap.2012.0143. [DOI] [PubMed] [Google Scholar]
- 86.Ito M, Sugito M, Kobayashi A, Nishizawa Y, Tsunoda Y, Saito N. Influence of learning curve on short-term results after laparoscopic resection for rectal cancer. Surg Endosc. 2009;23:403–408. doi: 10.1007/s00464-008-9912-1. [DOI] [PubMed] [Google Scholar]
- 87.Hackert T, Uhl W, Büchler MW. Specimen retrieval in laparoscopic colon surgery. Dig Surg. 2002;19:502–506. doi: 10.1159/000067605. [DOI] [PubMed] [Google Scholar]
- 88.Bujko K, Rutkowski A, Chang GJ, Michalski W, Chmielik E, Kusnierz J. Is the 1-cm rule of distal bowel resection margin in rectal cancer based on clinical evidence? A systematic review. Ann Surg Oncol. 2012;19:801–808. doi: 10.1245/s10434-011-2035-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wolthuis AM, Penninckx F, Haustermans K, De Hertogh G, Fieuws S, Van Cutsem E, D’Hoore A. Impact of interval between neoadjuvant chemoradiotherapy and TME for locally advanced rectal cancer on pathologic response and oncologic outcome. Ann Surg Oncol. 2012;19:2833–2841. doi: 10.1245/s10434-012-2327-1. [DOI] [PubMed] [Google Scholar]
- 90.Z’graggen K, Maurer CA, Birrer S, Giachino D, Kern B, Büchler MW. A new surgical concept for rectal replacement after low anterior resection: the transverse coloplasty pouch. Ann Surg. 2001;234:780–785; discussion 785-787. doi: 10.1097/00000658-200112000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Baker JW. Low end to side rectosigmoidal anastomosis; description of technic. Arch Surg. 1950;61:143–157. doi: 10.1001/archsurg.1950.01250020146016. [DOI] [PubMed] [Google Scholar]
- 92.Lazorthes F, Fages P, Chiotasso P, Lemozy J, Bloom E. Resection of the rectum with construction of a colonic reservoir and colo-anal anastomosis for carcinoma of the rectum. Br J Surg. 1986;73:136–138. doi: 10.1002/bjs.1800730222. [DOI] [PubMed] [Google Scholar]
- 93.Parc R, Berger A, Tiret E, Frileux P, Nordlinger B, Hannoun L. [Colo-anal anastomosis with reservoir in the treatment of rectal cancer] Ann Gastroenterol Hepatol (Paris) 1987;23:329–331. [PubMed] [Google Scholar]
- 94.Teramoto T, Watanabe M, Kitajima M. Per anum intersphincteric rectal dissection with direct coloanal anastomosis for lower rectal cancer: the ultimate sphincter-preserving operation. Dis Colon Rectum. 1997;40:S43–S47. doi: 10.1007/BF02062019. [DOI] [PubMed] [Google Scholar]
- 95.Wexner SD, Cohen SM. Port site metastases after laparoscopic colorectal surgery for cure of malignancy. Br J Surg. 1995;82:295–298. doi: 10.1002/bjs.1800820305. [DOI] [PubMed] [Google Scholar]
- 96.Zanghì A, Cavallaro A, Piccolo G, Fisichella R, Di Vita M, Spartà D, Zanghì G, Berretta S, Palermo F, Cappellani A. Dissemination metastasis after laparoscopic colorectal surgery versus conventional open surgery for colorectal cancer: a metanalysis. Eur Rev Med Pharmacol Sci. 2013;17:1174–1184. [PubMed] [Google Scholar]
- 97.Baek JH, McKenzie S, Garcia-Aguilar J, Pigazzi A. Oncologic outcomes of robotic-assisted total mesorectal excision for the treatment of rectal cancer. Ann Surg. 2010;251:882–886. doi: 10.1097/SLA.0b013e3181c79114. [DOI] [PubMed] [Google Scholar]
- 98.Pigazzi A, Luca F, Patriti A, Valvo M, Ceccarelli G, Casciola L, Biffi R, Garcia-Aguilar J, Baek JH. Multicentric study on robotic tumor-specific mesorectal excision for the treatment of rectal cancer. Ann Surg Oncol. 2010;17:1614–1620. doi: 10.1245/s10434-010-0909-3. [DOI] [PubMed] [Google Scholar]
- 99.Akmal Y, Baek JH, McKenzie S, Garcia-Aguilar J, Pigazzi A. Robot-assisted total mesorectal excision: is there a learning curve? Surg Endosc. 2012;26:2471–2476. doi: 10.1007/s00464-012-2216-5. [DOI] [PubMed] [Google Scholar]
- 100.Jiménez-Rodríguez RM, Díaz-Pavón JM, de la Portilla de Juan F, Prendes-Sillero E, Dussort HC, Padillo J. Learning curve for robotic-assisted laparoscopic rectal cancer surgery. Int J Colorectal Dis. 2013;28:815–821. doi: 10.1007/s00384-012-1620-6. [DOI] [PubMed] [Google Scholar]
- 101.Sng KK, Hara M, Shin JW, Yoo BE, Yang KS, Kim SH. The multiphasic learning curve for robot-assisted rectal surgery. Surg Endosc. 2013;27:3297–3307. doi: 10.1007/s00464-013-2909-4. [DOI] [PubMed] [Google Scholar]
- 102.Diana M, Perretta S, Wall J, Costantino FA, Leroy J, Demartines N, Marescaux J. Transvaginal specimen extraction in colorectal surgery: current state of the art. Colorectal Dis. 2011;13:e104–e111. doi: 10.1111/j.1463-1318.2011.02599.x. [DOI] [PubMed] [Google Scholar]
- 103.Ghezzi F, Raio L, Mueller MD, Gyr T, Buttarelli M, Franchi M. Vaginal extraction of pelvic masses following operative laparoscopy. Surg Endosc. 2002;16:1691–1696. doi: 10.1007/s00464-002-9043-z. [DOI] [PubMed] [Google Scholar]
- 104.Tsin DA, Colombero LT, Mahmood D, Padouvas J, Manolas P. Operative culdolaparoscopy: a new approach combining operative culdoscopy and minilaparoscopy. J Am Assoc Gynecol Laparosc. 2001;8:438–441. doi: 10.1016/s1074-3804(05)60346-5. [DOI] [PubMed] [Google Scholar]
- 105.Lomanto D, Chua HC, Myat MM, So J, Shabbir A, Ho L. Microbiological contamination during transgastric and transvaginal endoscopic techniques. J Laparoendosc Adv Surg Tech A. 2009;19:465–469. doi: 10.1089/lap.2009.0007. [DOI] [PubMed] [Google Scholar]
- 106.Wood SG, Panait L, Duffy AJ, Bell RL, Roberts KE. Complications of transvaginal natural orifice transluminal endoscopic surgery: a series of 102 patients. Ann Surg. 2014;259:744–749. doi: 10.1097/SLA.0b013e3182916138. [DOI] [PubMed] [Google Scholar]
- 107.Ghezzi F, Cromi A, Uccella S, Bogani G, Serati M, Bolis P. Transumbilical versus transvaginal retrieval of surgical specimens at laparoscopy: a randomized trial. Am J Obstet Gynecol. 2012;207:112.e1–112.e6. doi: 10.1016/j.ajog.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 108.Redwine DB, Koning M, Sharpe DR. Laparoscopically assisted transvaginal segmental resection of the rectosigmoid colon for endometriosis. Fertil Steril. 1996;65:193–197. doi: 10.1016/s0015-0282(16)58051-0. [DOI] [PubMed] [Google Scholar]
- 109.Carnuccio P, Jimeno J, Parés D. Laparoscopic right colectomy: a systematic review and meta-analysis of observational studies comparing two types of anastomosis. Tech Coloproctol. 2014;18:5–12. doi: 10.1007/s10151-013-1029-4. [DOI] [PubMed] [Google Scholar]
- 110.Blumberg D. Laparoscopic colectomy performed using a completely intracorporeal technique is associated with similar outcome in obese and thin patients. Surg Laparosc Endosc Percutan Tech. 2009;19:57–61. doi: 10.1097/SLE.0b013e318193c780. [DOI] [PubMed] [Google Scholar]
- 111.Tarta C, Bishawi M, Bergamaschi R. Intracorporeal ileocolic anastomosis: a review. Tech Coloproctol. 2013;17:479–485. doi: 10.1007/s10151-013-0998-7. [DOI] [PubMed] [Google Scholar]
- 112.Park JS, Choi GS, Lim KH, Jang YS, Kim HJ, Park SY, Jun SH. Clinical outcome of laparoscopic right hemicolectomy with transvaginal resection, anastomosis, and retrieval of specimen. Dis Colon Rectum. 2010;53:1473–1479. doi: 10.1007/DCR.0b013e3181f1cc17. [DOI] [PubMed] [Google Scholar]


