Abstract
Purpose
Little is known about the relationship of worry about hypoglycemia with diabetes-specific and typical-youth behaviors among emerging adults with type 1 diabetes. This study’s purpose was to examine the relationship among worry about hypoglycemia, diabetes management, and glycemic control within the context of alcohol use, hypoglycemia-related weight control behaviors, depressive symptoms, and impulse control among emerging adults with type 1 diabetes.
Research Design and Methods
The sample was 181 emerging adults with type 1 diabetes who were part of a larger study. Path analysis was used to test associations among worry about hypoglycemia, diabetes management, hypoglycemia-related weight control behaviors (WCB), alcohol use, impulse control, depressive symptoms and glycemic control.
Results
Path model fit and modification indices suggested that a feedback loop between worry about hypoglycemia and diabetes management should be incorporated into the original model. Youth with fewer depressive symptoms reported fewer hypoglycemia-related WCB and less worry about hypoglycemia; those with higher impulse control had less alcohol use and better diabetes management; those with lower alcohol use had more worry about hypoglycemia; and better glycemic control was associated with better diabetes management.
Conclusions
Health care professionals need to understand how multiple factors related to worry about hypoglycemia and diabetes management interact in emerging adults. In the context of depressive symptoms, impulse control, alcohol use, and hypoglycemia-related WCB, the path model results suggest several potential avenues for intervening to improve glycemic control in emerging adults.
Keywords: worry about hypoglycemia, diabetes management, alcohol use, weight control behaviors, Emerging Adults, Parents, Type 1 Diabetes
Worry about hypoglycemia associated with hypoglycemic events and blood glucose variability 1 is an issue for all persons with type 1 diabetes, but may be particularly important in youth with type 1 diabetes during their emerging adulthood years, 18 to 25 or more years of age. 2 Hypoglycemia is a significant problem for youth with diabetes; severe hypoglycemic events that is, when assistance is needed or there is a loss of consciousness, have been reported for 44% of youth 5–25 years of age, with older youth reporting more severe events, than younger ones.3 Worry about hypoglycemia may be especially salient during emerging adulthood, when youth rely on themselves for their own diabetes management, 4 in contrast to earlier times when parents are more involved. 5 In addition, alcohol use and weight control behaviors (WCB), also associated with glycemic control, 6,7 are relatively common for this age group, 8,9 and youth with diabetes are also involved in such behaviors.6,10,11 No known published study has examined worry about hypoglycemia and diabetes management within the context of other common health behaviors for emerging adults with diabetes.
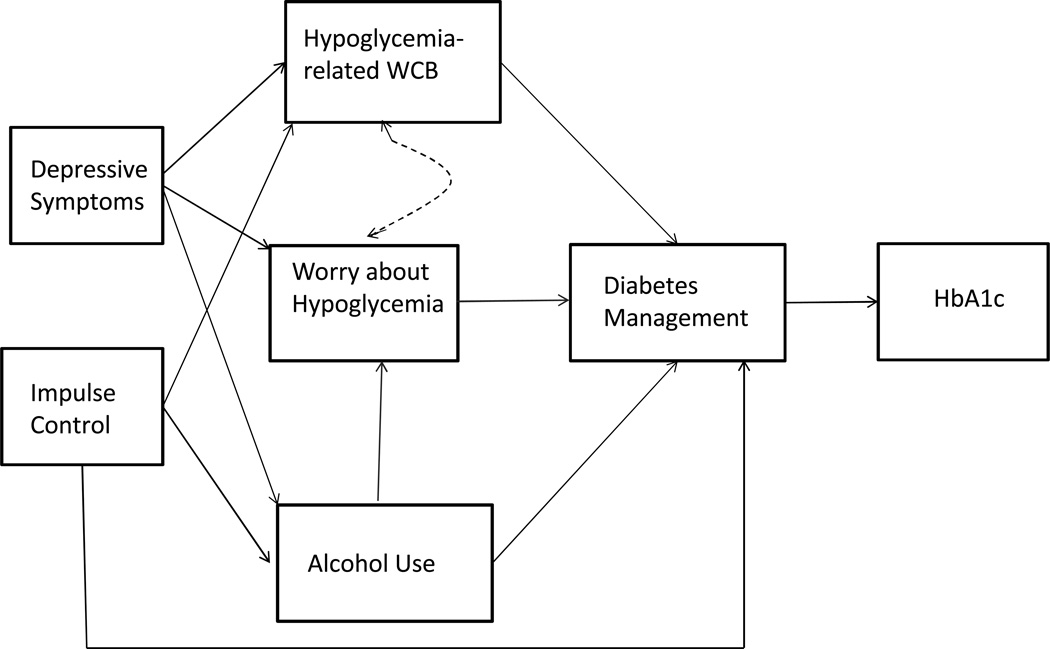
Although diabetes management, worry about hypoglycemia, and glycemic control are associated, the nature of these relationships is not clear.1 Some have hypothesized that high levels of hypoglycemia worry lead to “over-compensating” management behaviors intended to maintain high glucose levels.1 In other words, hypoglycemia avoidance may be given greater priority in diabetes-related decision-making than maintenance of normal blood glucose. However, the over-compensation theory has limited supporting evidence 1 and leaves behaviors unexplained for this age group. An alternative theory would be that worry about hypoglycemia would provide an incentive for these emerging adults to practice good diabetes management. Since emerging adulthood is a time for independence,2 and emerging adults with diabetes are highly autonomous in their diabetes care,4 exercising control over their diabetes management would provide an opportunity for them to deal with their hypoglycemia worries. Thus, it is likely that, among emerging adults with diabetes, more worry about hypoglycemia leads to better diabetes management and, consistent with existing evidence,12 better management in turn will be associated with better glycemic control (See Figure 1).
Figure 1.
The Hypothesized Path Model for the Relationship of Worry about Hypoglycemia, Diabetes Management and Glycemic control within the Context of Emerging Adulthood
Other common health behaviors such as alcohol use and WCB among emerging adults with type 1 diabetes may influence worry about hypoglycemia. Alcohol consumption is associated with hypoglycemic events 13 and reduced hypoglycemia awareness,14 which is also associated with increased risk for hypoglycemia 15 among youth with diabetes. Based on that evidence, we hypothesize that alcohol use directly influences worry about hypoglycemia. Disordered eating is commonly associated with changes in glycemic control in the short term 16 and specifically with hyperglycemia.17 However, some WCB such as skipping meals are associated with severe hypoglycemic events.18 It is likely that engaging in hypoglycemia-related WCB may be associated with worry about hypoglycemia. Given that there is insufficient evidence to hypothesize a path for hypoglycemia-related WCB directly influencing worry about hypoglycemia, but recognizing the potential association between WCB and worry about hypoglycemia, we hypothesize an associational relationship between hypoglycemia-related WCB and worry about hypoglycemia. In addition, diabetes management involves adjustment of diabetes regimen behaviors based upon daily life situations, and thus, it is likely that poor diabetes management occurs when alcohol is consumed or when there are attempts to control weight with hypoglycemia-related behaviors (See Figure 1).
When examining alcohol use and unhealthy WCB, it is important to take into consideration depressive symptoms and impulse control. Depressive symptoms are associated with alcohol use 19 and unhealthy WCB among youth in general.20 Among youth with diabetes, depressive symptoms are linked with disordered eating behaviors.17 Impulse control, the ability to delay immediate gratification to achieve goals,21 is important because it is associated with maturation of the pre-frontal cortex during emerging adulthood 21 and poor impulse control is associated with risk-taking behaviors.21 Among youth with diabetes, important for diabetes management is cognitive functioning 22,23 and impulse control specifically.24 thus, it is likely that depressive symptoms are associated with hypoglycemia-related WCB, alcohol use, and more worry about hypoglycemia, whereas poor impulse control is associated with alcohol use, hypoglycemia-related WCB, and poor diabetes management (See Figure 1).
Little is known about diabetes-specific and typical-youth behaviors in relation to worry about hypoglycemia, diabetes management and glycemic control. Given the roles that these variables play in glycemic control, it is important to understand how they may directly influence each other, and especially the role that worry about hypoglycemia may play as a mediator of those other factors affecting diabetes management. Thus, the purpose of this study was to examine a theoretically derived path model, delineated in Figure 1, of associations among worry about hypoglycemia, diabetes management, and glycemic control within the context of alcohol use, hypoglycemia-related WCB, depressive symptoms, and impulse control in emerging adults with type 1 diabetes. Among emerging adults with type 1 diabetes at the time of HS graduation, it is hypothesized that:
Greater worry about hypoglycemia will be directly associated with better diabetes management and subsequently with better glycemic control.
Greater alcohol use will be directly associated with more worry about hypoglycemia and with poorer diabetes management.
Greater involvement in hypoglycemic-related weight control behaviors will directly be associated with more worry about hypoglycemia and with poorer diabetes management.
More depressive symptoms will be directly associated with greater alcohol use, greater hypoglycemic-related weight control behaviors, and more worry about hypoglycemia.
Less impulse control will be directly associated with greater alcohol use, and greater hypoglycemic-related weight control behaviors, and indirectly with poorer glycemic control, mediated by diabetes management.
Methods
Design
This study had a correlational design, specifically model testing 25 of a priori specified relationships among variables which in this case are worry about hypoglycemic, diabetes management and glycemic control within the context of alcohol use, hypoglycemic-related WCB, impulse control and depressive symptoms. Model testing allows for examination complex relationships among variables, identifying direct and indirect influences. For example, model testing allowed for testing the hypothesis that worry about hypoglycemia directly influences diabetes management as well as testing that worry about hypoglycemia indirectly influences glycemic control through diabetes management, often called a mediating effect. The purpose of this study is consistent with a major aim in the larger study, examining individual characteristics associated with behaviors and health outcomes during the transition to young adulthood among youth with type 1 diabetes. In addition, the sample was high school graduates, a subset of the larger study sample, in attempt to control for a major transitional event 26 and to reflect a relatively non-high-risk group of youth for which WCB would be salient. Reports of other purposes examined in this larger study have been described elsewhere. 4,24,27–30
Participants and Procedure
The larger study consisted of high school seniors with type 1 diabetes who were recruited from outpatient diabetes care clinics of a regional university medical center, a private hospital, and a regional diabetes care center. There was an 83% recruitment rate among the potential pool of participants contacted with lack of interest, being busy, and a wish not to release private health information the reasons for declining. After receiving a brief study summary from their health care provider, participants were enrolled either face to face at a clinic appointment or via the telephone. Eligible participants met the following criteria: 17–19 years of age; in the last six months of high school; diagnosed with type 1 diabetes for at least one year; able to speak and read English; living with their parent(s) or guardian; and without a serious psychiatric disorder or a second chronic illness that would interfere with becoming independent. Then, youth 18 years of age or older provided consent, and those under 18 years of age provided assent and parents provided consent in this IRB-approved study. There was a 91% participation rate after screening and enrollment with 16 not completing baseline questionnaires, 2 requesting to be withdrawn from the study and 2 not being able to be contacted by study staff. A greater number of males than females did not participate (p < .05).
Measures
Web-based entry, with a paper option, was the means for collecting data from participants on most of the measures.
Glycemic Control
was assessed by using HbA1cs obtained from medical records from the health care provider. Because different assays were used by various centers, adjusted HbA1c values were calculated by taking the original HbA1c value and subtracting the assay-specific bias value as determined by the College of American Pathologists (CAP) survey data.31
Diabetes Management
was measured by the 24-item Emerging Adult Diabetes Management Self-Report, developed for this study. This measure was an adaptation of the Diabetes Self-Management Profile (DSMP) interview 32 for self-completion on the Web. Participants were asked to respond to how often in the last three months they had managed their diabetes (performing tasks and making changes in specific situations related to diet, exercise, blood glucose testing, insulin administration, and hypoglycemia). The scores could range from 0–84, with higher scores indicating better management. In accordance with the developers’ suggestion,32 only the summed score for total diabetes management, which had adequate reliability, was used. The Cronbach’s alpha coefficient was .76 in the original study,32 .82 in the recently adapted self-report by the developers,33 and .81 in this study.
Worry about Hypoglycemia
was measured by the worry subscale of the Fear of Hypoglycemia Scale, which has documented reliability and validity.34 The scale was revised from 17 to 18 items for this study. One item was separated into two items because, at least for this age group, being drunk and being stupid could be thought of as different states. Participants were asked to rate how often worries occur from 1 (never) to 5 (very often). The responses were summed for a total score with a potential range of 18–90 and with higher scores reflecting more worry. The scale was developed with adolescents and adults with type 1 diabetes and has a 4th to 5th grade reading level. The Cronbach’s alpha coefficient with this sample was .93.
Alcohol Use
was assessed with a revised item from the Health Behavior Questionnaire.35 Rather than asking within the last six months, participants were asked how often they had used alcohol during the last 3 months; the response options were not at all, once or twice in past 3 months, 2–3 times in past 3 months, about once a month, 2 or 3 days a month, once a week, 2 or 3 days a week, 4 or 5 days a week, and every day. Because alcohol use was minimal in this sample, a categorical variable of either being involved (1) or not (0) in alcohol use was calculated and used in the analysis.
Hypoglycemia-related Weight Control Behaviors
were measured by 6 items from the Project AHEAD Questionnaire.36 A panel of experts in diabetes and youth identified items associated with glycemic changes: fasting, eating little food, skipping meals, exercising, skipping insulin dose, and taking less insulin than prescribed. Participants in this study were asked to respond yes or no to whether they had participated in each of these behaviors in the past 3 months. Those that tend to raise blood glucose levels were reversed scored. A summed score of these six WCB was used in the analysis.
Depressive Symptoms
were measured by the Beck Depression Inventory-Second Edition (BDI-II), demonstrated to have validity and reliability.37 The scale assesses the existence and severity of depressive symptoms as defined by the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV). Participants were asked to rate their experience of the symptoms on a scale from 0 to 3. Summed scores provide a range of 0–63, with scores of 14–19 considered to be mild, 20–28 moderate, and 29–63 severe. Because reported depressive symptoms were low in this sample, a categorical variable of having depressive symptoms (score of 14 or greater) or not (score less than 14) was calculated. The Cronbach’s alpha for this sample was .92.
Impulse Control
was measured by the 11-item Impulse Control subscale of the Self-regulation Questionnaire, developed with emerging adults.38 This scale measures inhibitory control to decisions, plans, and actions. Respondents were asked to indicate the degree to which each statement described them from 1 (strongly disagree) to 5 (strongly agree). Items reflecting lack of control were reverse scored. Then, impulse score responses were summed for a total score with a potential range of 11–55, with higher scores reflecting greater impulse control. The Cronbach’s alpha coefficient was .85 in this study.
Data Analysis
Path analysis was used to test hypothesized relationships among a combination of continuous (glycemic control, diabetes management, worry about hypoglycemia, impulse control, and hypoglycemia-related WCB) and ordered categorical (alcohol use, depressive symptoms) measures. All variables were observed; no latent variables or latent constructs were specified in the path model. Variables in path models can be classified as endogenous or exogenous. If a variable is specified as a dependent variable for any equation in the model, then it is classified as endogenous. If a variable is only used as an independent variable, it is exogenous.39 In this study, the pre-specified relationships tested in the model are delineated in the hypotheses and Figure 1 are tested. Depressive symptoms and impulse control were exogenous (i.e., only used as independent variables), with all others being endogenous. Mplus software 40 was used to detect influential outliers, evaluate model fit, estimate and test path coefficients, and estimate and test indirect and total effects. Since one of the variables (alcohol use) was categorical, endogenous, and mediating, weighted least squares (WLSMV) estimation was used. Direct effects for alcohol use were estimated by MPlus using a probit regression.40 Cook’s distance 41 and log-likelihood influence 42 were used to identify influential observations. The adequacy of how the hypothesized relationships fit the data was evaluated by the following: chi-square p value ≥ .05, comparative fit index (CFI) > .95, root mean square error of approximation (RMSEA) < .06, and weighted root mean square residual (WRMR) ≤ 1.0 according to Hu and Bentler 43 and Yu.44 Due to the exploratory nature of the model, modifications to the model were investigated using modification indices. The covariance matrix used for analysis was based upon all available subjects. There were 182 subjects available for analysis. One subject had missing data on the Beck Depression Inventory, leaving 181 subjects with complete data on all variables ultimately contributing to the analysis.
Results
Sample Characteristics
Characteristics of the 181 high school graduates with complete data on all variables are summarized below and presented in Tables 1 and 2. On average, these emerging adults were 18.2 years of age (SD = 0.4); had been diagnosed with diabetes for 8.6 years (SD = 4.0); had a BMI of 25.4 kg/m2 (SD = 4.0); and had an adjusted HbA1c value of 8.9% (SD = 1.67, range 6.2 - 14.2%). The great majority were White, with a little over half being female. Over half of these youth reported living with both parents in the same household and only a very small minority of their mothers and fathers had less than a high school education. A little over half were administering insulin via injections, the remainder using pumps. Only 12.7% of the sample was considered to have depressive symptoms (scores of 14 or greater), and 23.2% were involved in alcohol use. On average, subjects engaged in slightly more than three hypoglycemic WCB out of six possible (mean=3.13, SD=1.17, range=0–6).
Table 1.
Characteristics of Participants (N=181)
| Characteristics | |
|---|---|
| Gender | |
| Female | 56.9% |
| Male | 43.1% |
| Race | |
| White | 93.4% |
| Black | 5.0% |
| Other | 1.6% |
| Insulin Administration | |
| Injection | 50.3% |
| Pump | 49.7% |
| Mother’s Education | |
| 11 years or less | 3.9% |
| 12 years or high school | 43.7% |
| Associate or vocational degree | 16.6% |
| 4 yr. college degree | 23.2% |
| Master’s degree or higher | 12.2% |
| Refused/don’t know | 0.4% |
| Father’s Education | |
| 11 years or less | 4.4% |
| 12 years or high school | 45.3% |
| Associate or vocational degree | 8.3% |
| 4 yr. college degree | 25.4% |
| Master’s degree or higher | 14.9% |
| Refused/don’t know | 1.7% |
| Living Situation | |
| Only mother or only father | 13.3% |
| Both mother/father in same house | 61.3% |
| Father and step-mother | 3.3% |
| Mother and step-father | 13.3% |
| Other | 8.8% |
Table 2.
Means, standard deviations and correlation coefficients for variables in the path model.
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. |
|---|---|---|---|---|---|---|---|
| 1. HbA1c | 1.00 | −0.23 | −0.05 | 0.10 | 0.05 | 0.11 | −0.13 |
| 2. Diabetes management | 1.00 | 0.14 | −0.08 | −0.27 | −0.18 | 0.47 | |
| 3. Hypoglycemia-related WCB | 1.00 | 0.10 | 0.03 | 0.13 | 0.05 | ||
| 4. Worry about hypoglycemia | 1.00 | −0.06 | 0.36 | −0.31 | |||
| 5. Alcohol use* | 1.00 | 0.07 | −0.22 | ||||
| 6. Depressive symptoms* | 1.00 | −0.47 | |||||
| 7. Impulse control | 1.00 | ||||||
| Mean | 8.87 | 51.44 | 3.13 | 35.28 | 0.23 | 0.13 | 41.41 |
| SD | 1.67 | 11.74 | 1.17 | 11.86 | 0.42 | 0.33 | 7.03 |
Note.
= binary items denoted as having the criterion (1) or not having the criterion (0).
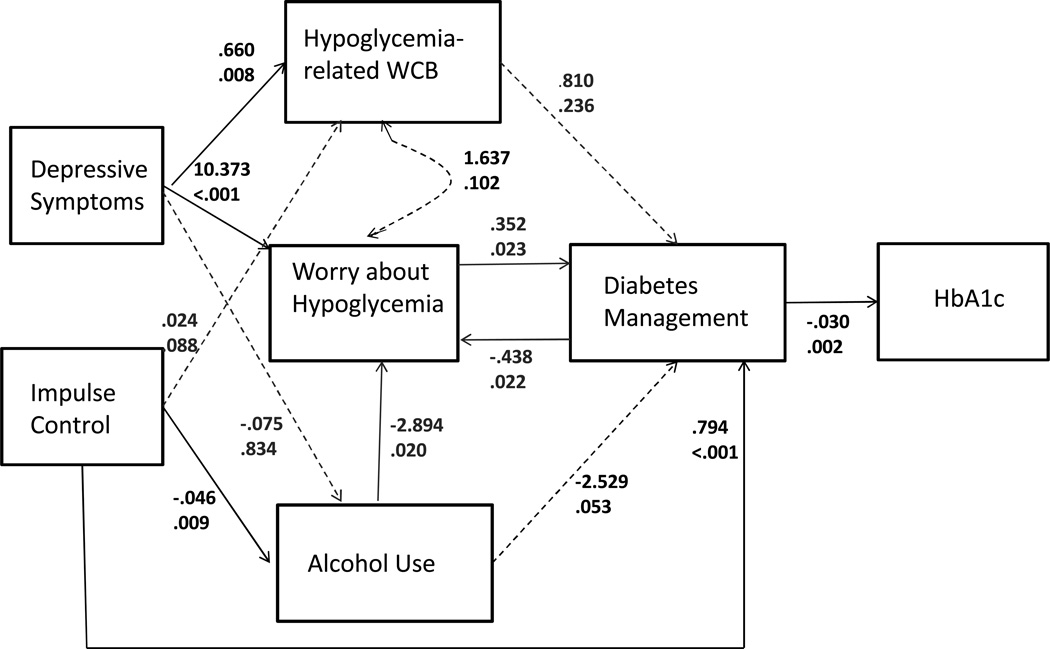
Model
The initial path model was specified to reflect the hypothesized direct effects. However, model fit was inadequate, and modification indices indicated that adding a path from diabetes management to worry about hypoglycemia would significantly improve model fit. Since the resultant feedback loop between fear of hypoglycemia and diabetes management is theoretically plausible (i.e., poor diabetes management may lead to greater worry about hypoglycemia), a path from diabetes management to worry about hypoglycemia was added to the model. Figure 2 shows the unstandardized path coefficients for the revised model. With 22 estimated parameters, model fit was very good according to criteria discussed in the data analysis section above: the chi-square value was 4.09 (df=7, p=0.769), a p value ≥ .05; CFI was 1.0, a value > .95; RMSEA was 0.0 (90% CI = 0 -.063), a value < .06; and WRMR was .353, a value ≤ 1.0, all meeting criteria of a good fit or adequacy of explaining the hypothesized relationships with this sample’s data.
Figure 2.
The Path Model Results for the Relationship of Worry about Hypoglycemia, Diabetes Management and Glycemic control within the Context of Emerging Adulthood
The first hypothesis that greater worry about hypoglycemia will be directly associated with better diabetes management and subsequently with better glycemic control was supported (See Figure 2). Better glycemic control, lower HbA1c values, were directly influenced by higher diabetes management scores (β54 = −0.03, p=.002) which was directly influenced by worry about hypoglycemia (β42 = 0.352, p=.023). However, although more worry lead to better management, there was a feedback loop between worry about hypoglycemia and diabetes management with better management leading to less worry about hypoglycemic (β24= −0.44, p=.022).
The second hypothesis that greater alcohol use will be directly associated with more worry about hypoglycemia and with poorer diabetes management was not supported (See Figure 2). Use of alcohol lead to less worry about hypoglycemia (β23= −2.89, p=.02); although this was significant, this negative relationship was opposite of the hypothesized positive relationship. In addition, use of alcohol was not significantly associated with poorer diabetes management (β43= −2.529, p=.053. However, the direction of the relationship was in the hypothesized direction, i.e., alcohol use would lead to poorer diabetes management.
The third tentative hypothesis that greater involvement in hypoglycemic-related weight control behaviors will directly be associated with more worry about hypoglycemia and with poorer diabetes management was not supported (See Figure 2). Hypoglycemic-related WCB was not significantly associated with diabetes management (β41= .810, p=.236) nor was it in the hypothesized negative direction. In addition, hypoglycemic-related WCB was not significantly associated with worry about hypoglycemia (ψ12= 1.637, p=.102); however, it was in the hypothesized direction.
The fourth hypothesis was partially supported (See Figure 2). Results did not support the hypothesis that more depressive symptoms will be directly associated with greater alcohol use. However the results supported the portion of the hypothesis that having depressive symptoms resulted in higher levels of engagement in hypoglycemia-related WCB (γ11= 0.66, p=.008) and in more worry about hypoglycemia (γ21= 10.37, p<.001).
Portions of the final hypothesis were supported (See Figure 2). Although less impulse control was not associated with greater hypoglycemic-related weight control behaviors (γ12??=0.024, p=.088);, higher levels were associated with a lower likelihood of alcohol use (γ32=−0.05, p=.009) and better diabetes management (γ42=0.79, p<.001). Also, the indirect effect from impulse control through diabetes management to HbA1c (coeff = −0.02, p=.005) was statistically significant, supporting a mediated relationship, that is higher levels of impulse control lead to better management which leads to better HbA1c values.
Discussion
The testing and development of this model expands existing understanding of how worry about hypoglycemia relates to diabetes management among emerging adults with type 1 diabetes. The identification of a negative feedback loop between worry about hypoglycemia and diabetes management in this model does not support the over-compensation theory that more worry about hypoglycemia will lead to poorer management.1 Rather, in this path model, the indication that a negative feedback loop exists between hypoglycemia worry and diabetes management suggests that, although greater worry about hypoglycemia leads to better diabetes management, better diabetes management tends to also allay worry about hypoglycemia. It is likely that an interplay occurs between self-assessment of diabetes management and potential consequences of those management behaviors for these youth in a period of greater freedoms 2 who rely more on themselves for diabetes management.5 In addition, it is likely that better diabetes management, especially frequent blood glucose monitoring, provides information to confirm or assuage hypoglycemia worry. Further longitudinal studies are needed to validate these cross-sectional findings.
Two behaviors typically associated with this age group produced unanticipated findings in relation to worry about hypoglycemia. Use of alcohol, though associated with worry about hypoglycemia, was not in the anticipated direction; alcohol use was associated with less worry about hypoglycemia rather than more worry. It is difficult to speculate why this is the case given that little research has been conducted on alcohol use among youth with type 1 diabetes. It could be that personality characteristics of alcohol users, other than depressive symptoms and impulse control, are associated with less worry for those who use alcohol. Further, some may use alcohol to a degree that decreases hypoglycemia awareness 14 and thus these youth could have less worry about hypoglycemia. Also in contrast to our hypothesis, hypoglycemia-related WCB were not associated with worry about hypoglycemia. It is difficult to speculate about this finding given the paucity of evidence on WCB associated with hypoglycemia; most research has been done more broadly on disordered eating and eating disorders.16,17
The path model provided mixed support for hypothesized relationships among worry about hypoglycemia, typical-youth behaviors, diabetes- specific behaviors, and glycemic control for emerging adults with type 1 diabetes. First, in the model and consistent with existing evidence,12 better glycemic control is associated with better diabetes management. Second, although it is reported that poor glycemic control is associated with alcohol use 7 and unhealthy weight control behaviors,6 these findings suggest that hypoglycemia-related WCB and alcohol use may not be directly and independently associated with diabetes management nor indirectly with glycemic control. The minimal involvement in alcohol use in this sample likely contributed to its lack of association with management and glycemic control. In regard to WCB, the findings are mixed on the association between disordered eating and diabetes control,16 implying that the association is more complex.
These findings also provide insight relative to personal characteristics in association with diabetes management, alcohol use, and hypoglycemia-related WCB among emerging adults with diabetes. Having significant depressive symptoms was associated with a higher level of hypoglycemia-related WCB, but not with alcohol use. These findings are consistent with evidence that depressive symptoms are associated with WCB among youth in general 20 and those with diabetes;17 however, the findings are in conflict with evidence on the relationship of depressive symptoms to alcohol use.19 The low number of participants who used alcohol and the low levels of depressive symptoms in this sample may have contributed to those different findings. In addition, having depressive symptoms was related to greater worry about hypoglycemia; this finding needs to be examined further in research. Higher levels of impulse control were associated with better diabetes management and, in turn, with better glycemic control. The relationship of impulse control to diabetes management is consistent with existing findings for emerging adults with diabetes.24 Further, impulse control was associated with alcohol use, supporting our hypothesis; however, contrary to our other hypothesis, impulse control was not independently associated with hypoglycemia-related WCB. This is not consistent with identified associations between poor impulse control and risk-taking behaviors.21
Limitations of this study need to be considered. First, the findings can only be generalized to similar youth with type 1 diabetes, that is, predominately White, living at home with one or both parents, and generally with less than optimal glycemic control according to American Diabetes Association’s HbA1c goal of ≤ 7.5% for this age range.45 Furthermore, this sample had low involvement in alcohol use and only a small minority reported depressive symptoms, which is at the low end of the 15%–35% of adolescents and emerging adults with diabetes self-reporting depressive symptoms.46–49 The low involvement in alcohol use and reporting of depressive symptoms could be because of one of the study’s sampling criterion to exclude those with serious mental health illnesses that would interfere with independence. In addition, when comparing alcohol use rates, it needs to be kept in mind that these behaviors were asked in relation to the last three months, and thus the reported rates might have been lower than the yearly or ever-used rates reported elsewhere. However, the sample was obtained from different settings and thus reflects some diversity.
Until further research is conducted on diabetes-related and typical youth behaviors in association with worry about hypoglycemia, it is difficult to make suggestions for clinicians. However, clinicians are urged to assess impulse control since it is immature 21 during emerging adulthood and it is directly associated with diabetes management and indirectly glycemic control. Further, when working with emerging adults, clinicians are urged to be open to the possibility that greater worry about hypoglycemia can lead to better diabetes management as well as better management can also allay worry about hypoglycemia. Further, assessment of alcohol use and hypoglycemia-related WCB such as skipping meals is encouraged since they are known to be associated with hypoglycemia.15, 18
Further research is suggested in this area. The findings of this study do not support the over-compensation theory, and longitudinal studies are needed to examine relationships among worry about hypoglycemia, diabetes management, and glycemic control. The findings also suggest that future research should include measures of both depression and impulse control when examining the complex relationships among worry about hypoglycemia, diabetes management, and glycemic control.
Acknowledgements
The project was supported by R01NR009810 (PI KM Hanna) from the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Contributor Information
Kathleen M. Hanna, Indiana University School of Nursing.
Michael T. Weaver, Indiana University School of Nursing.
Timothy E. Stump, Indiana University School of Medicine, Department of Biostatistics.
J. Dennis Fortenberry, Indiana University School of Medicine.
Linda A. DiMeglio, Indiana University School of Medicine.
References
- 1.Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder-Frederick L. A critical review of the literature on fear of hypoglycemia in diabetes: Implications for diabetes management and patient education. Patient Educ Couns. 2007;68(1):10–15. doi: 10.1016/j.pec.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 2.Arnett JJ. Emerging Adulthood: What Is It, and What Is It Good For? Child Dev Perspectives. 2007;1(2):68–73. [Google Scholar]
- 3.Limbert C, Schwingshandl J, Haas J, Roth R, Borkenstein M. Severe hypoglycemia in children and adolescents with IDDM: frequency and associated factors. Journal Diabetes Complicat. 1993;7(4):216–220. [PubMed] [Google Scholar]
- 4.Hanna KM, Weaver MT, Stump TE, et al. Initial findings: primary diabetes care responsibility among emerging adults with type 1 diabetes post high school and move out of parental home. Child: Care Health and Development. 2013;39(1):61–68. doi: 10.1111/j.1365-2214.2011.01320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schilling LS, Knafl KA, Grey M. Changing patterns of self-management in youth with type I diabetes. Journal Pediatr Nurs. 2006;21(6):412–424. doi: 10.1016/j.pedn.2006.01.034. [DOI] [PubMed] [Google Scholar]
- 6.Neumark-Sztainer D, Patterson J, Mellin A, et al. Weight control practices and disordered eating behaviors among adolescent females and males with type 1 diabetes: associations with sociodemographics, weight concerns, familial factors, and metabolic outcomes. Diabetes Care. 2002;25(8):1289–1296. doi: 10.2337/diacare.25.8.1289. [DOI] [PubMed] [Google Scholar]
- 7.Glasgow AM, Tynan D, Schwartz R, et al. Alcohol and drug use in teenagers with diabetes mellitus. J Adolescent Health. 1991;12(1):11–14. doi: 10.1016/0197-0070(91)90033-i. [DOI] [PubMed] [Google Scholar]
- 8.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity. 2008;16(10):2205–2211. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 9.Schulenberg J, O'Malley PM, Bachman JG, Johnston LD. Early adult transitions and their relation to well-being and substance use. In: Settersten RA, Furstenberg FF, Rumbaut RG, editors. On the frontier of adulthood: Theory, research, and public policy. Chicago: The University of Chicago Press; 2005. pp. 417–453. [Google Scholar]
- 10.Barnard K, Sinclair JMA, Lawton J, Young AJ, Holt RIG. Alcohol-associated risks for young adults with Type 1 diabetes: a narrative review. Diabetic Med. 2012;29(4):434–440. doi: 10.1111/j.1464-5491.2012.03579.x. [DOI] [PubMed] [Google Scholar]
- 11.Howe CJ, Jawad AF, Kelly SD, Lipman TH. Weight-related concerns and behaviors in children and adolescents with type 1 diabetes. J Am Psychiatr Nurs Assoc. 2008;13(6):376–385. doi: 10.1177/1078390307310154. [DOI] [PubMed] [Google Scholar]
- 12.Hood KK, Peterson CM, Rohan JM, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics. 2009;124(6):e1171–e1179. doi: 10.1542/peds.2009-0207. [DOI] [PubMed] [Google Scholar]
- 13.Feher MD, Grout P, Kennedy A, Elkeles RS, Touquet R. Hypoglycaemia in an inner-city accident and emergency department: a 12-month survey. Arch Emerg Med. 1989;6(3):183–188. doi: 10.1136/emj.6.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kerr D, Macdonald IA, Heller SR, Tattersall RB. Alcohol causes hypoglycaemic unawareness in healthy volunteers and patients with type 1 (insulin-dependent) diabetes. Diabetologia. 1990;33(4):216–221. doi: 10.1007/BF00404799. [DOI] [PubMed] [Google Scholar]
- 15.Schopman JE, Geddes J, Frier BM. Frequency of symptomatic and asymptomatic hypoglycaemia in Type 1 diabetes: effect of impaired awareness of hypoglycaemia. Diabetic Med. 2011;28(3):352–355. doi: 10.1111/j.1464-5491.2010.03203.x. [DOI] [PubMed] [Google Scholar]
- 16.Young-Hyman DL, Davis CL. Disordered eating behavior in individuals with diabetes: importance of context, evaluation, and classification. Diabetes Care. 2010;33(3):683–689. doi: 10.2337/dc08-1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goebel-Fabbri AE. Disturbed eating behaviors and eating disorders in type 1 diabetes: clinical significance and treatment recommendations. Curr Diabetes Rep. 2009;9(2):133–139. doi: 10.1007/s11892-009-0023-8. [DOI] [PubMed] [Google Scholar]
- 18.The Diabetes Control and Complications Trial (DCCT) Research Group. Epidemiology of Severe Hypoglycemia in the Diabetes Control and Complications Trial. Am J Med. 1991;90(4):450–459. [PubMed] [Google Scholar]
- 19.Testa CR, Steinberg L. Depressive Symptoms and Health-Related Risk-Taking in Adolescence. Suicide Life Threat. 2010;40(3):298–305. doi: 10.1521/suli.2010.40.3.298. [DOI] [PubMed] [Google Scholar]
- 20.Haley CC, Hedberg K, Leman RF. Disordered eating and unhealthy weight loss practices: which adolescents are at highest risk? J Adolescent Health. 2010;47(1):102–105. doi: 10.1016/j.jadohealth.2009.12.023. [DOI] [PubMed] [Google Scholar]
- 21.Casey BJ, Getz S, Galvan A. The adolescent brain. Dev Rev. 2008;28(1):62–77. doi: 10.1016/j.dr.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McNally K, Rohan J, Pendley JS, Delamater A, Drotar D. Executive functioning, treatment adherence, and glycemic control in children with type 1 diabetes. Diabetes Care. 2010;33(6):1159–1162. doi: 10.2337/dc09-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Graziano PA, Geffken GR, Williams LB, et al. Gender differences in the relationship between parental report of self-regulation skills and adolescents' management of type 1 diabetes. Pediatr Diabetes. 2011;12(4 Pt 2):410–418. doi: 10.1111/j.1399-5448.2010.00692.x. [DOI] [PubMed] [Google Scholar]
- 24.Stupiansky NW, Hanna KM, Slaven JE, Weaver MT, Fortenberry JD. Impulse control, diabetes-specific self-efficacy, and diabetes management among emerging adults with type 1 diabetes. J Pediatr Psychol. 2013;38(3):247–254. doi: 10.1093/jpepsy/jss110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grove SK, Burns N, Gray JR. The practice of nursing research: Appraisl, synthesis, and genration of evidence. 7th ed. Elsevier Saunders; 2013. [Google Scholar]
- 26.Furstenberg FF, Jr, Rumbaut RC, Settersten RA., Jr . On the frontier of adulthood: Emerging themes and new directions. In: Settersten RA, Furstenberg FF, Rumbaut RG, editors. On the frontier of adulthood: Theory, research, and public policy. Chicago: The University of Chicago Press; 2005. pp. 3–25. [Google Scholar]
- 27.Hanna KM, Weaver MT, Stump TE, Slaven JE, Fortenberry JD, DiMeglio LA. Readiness for Living Independently Among Emerging Adults With Type 1 Diabetes. Diabetes Educ. 2013;39(1):92–99. doi: 10.1177/0145721712465341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hanna KM, Scott LL, Schmidt KK. Meeting Recruitment and Retention Goals in a Longitudinal Study with Emerging Adults. Clinical Nurse Specialist. 2014;28(1):41–45. doi: 10.1097/NUR.0000000000000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hanna KM, Stupiansky N, Weaver MT, Slaven J, Stump T. Alcohol Use Trajectories after High School Graduation among Emerging Adults with Type 1 Diabetes. Journal Adolescent Health. doi: 10.1016/j.jadohealth.2014.02.002. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hanna KM, Weaver MT, Stump TE, Guthrie D, Oruche UM. Emerging Adults with Type 1 Diabetes during the First Year Post-High School: Perceptions of Parental Behaviors. Emerging Adulthood. doi: 10.1177/2167696813512621. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.College of American Pathologists Survey Data. 2012 http://www.ngsp.org/CAPdata.asp. [Google Scholar]
- 32.Harris MA, Wysocki T, Sadler M, et al. Validation of a structured interview for the assessment of diabetes self-management. Diabetes Care. 2000;23(9):1301–1304. doi: 10.2337/diacare.23.9.1301. [DOI] [PubMed] [Google Scholar]
- 33.Wysocki T, Buckloh LM, Antal H, Lochrie A, Taylor A. Validation of a self-report version of the diabetes self-management profile. Pediatr Diabetes. 2012;13(5):432–437. doi: 10.1111/j.1399-5448.2011.00823.x. [DOI] [PubMed] [Google Scholar]
- 34.Cox DJ, Irvine A, Gonder-Frederick L, Nowacek G, Butterfield J. Fear of hypoglycemia: quantification, validation, and utilization. Diabetes Care. 1987 Sep-Oct;10(5):617–621. doi: 10.2337/diacare.10.5.617. [DOI] [PubMed] [Google Scholar]
- 35.Jessor R, Donovan J, Costa F. Health behavior questionnaire: High school form. 1992 [Google Scholar]
- 36.Project AHEAD. Assessing Health and Eating among Adolescents with Diabetes. U.of. Minnesota; 2000. [Google Scholar]
- 37.Beck AT, Steer RA, Brown GK. BDI-II: Beck Depression Inventory Manual. San Antonio, Texas: Harcourt Assessment, Inc.; 1996. [Google Scholar]
- 38.Neal DJ, Carey KB. A follow-up psychometric analysis of the self-regulation questionnaire. Psychol Addict Behav. 2005;19(4):414–422. doi: 10.1037/0893-164X.19.4.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ullman JB. Structural Equation Modeling. In: Tabachnick BG, Fidell LS, editors. Using multivariate statistics. Fifth ed. Boston: Pearson Education, Inc; 2007. pp. 276–780. [Google Scholar]
- 40.Muthen LK, Muthen BO. Mplus User's Guide. 5th edition. Los Angeles: Muthen & Muthen; 1998-2007. [Google Scholar]
- 41.Cook RD. Detection of influential observations in linear regression. Technometrics. 1997;19:15–18. [Google Scholar]
- 42.Cook RD, Weisberg S. Residuals and influence in regression. New York: Chapman and Hall; 1982. [Google Scholar]
- 43.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equa Modeling. 1999;6(1):1–55. [Google Scholar]
- 44.Yu C. Evaluating cutoff criteria of model fit indices for laten variable models with binary and continuous outcomes. [Accessed 2/17/2014];2002 download/Yudissertaion.pdf. [Google Scholar]
- 45.Silverstein J, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28(1):186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 46.Hood KK, Huestis S, Maher A, Butler D, Volkening L, Laffel LMB. Depressive symptoms in children and adolescents with Type 1 diabetes: Association with diabetesspecific characteristics. Diabetes Care. 2006. 2006;29(6):1389–1391. doi: 10.2337/dc06-0087. [DOI] [PubMed] [Google Scholar]
- 47.Lawrence JM, Standiford DA, Loots B, et al. Prevalence and correlates of depressed mood among youth with diabetes: the SEARCH for Diabetes in Youth study. Pediatrics. 2006;117(4):1348–1358. doi: 10.1542/peds.2005-1398. [DOI] [PubMed] [Google Scholar]
- 48.Stewart SM, Rao U, Emslie GJ, Klein D, White PC. Depressive symptoms predict hospitalization for adolescents with Type 1 diabetes mellitus. Pediatrics. 2005. 2005;115(5):1315–1319. doi: 10.1542/peds.2004-1717. [DOI] [PubMed] [Google Scholar]
- 49.Hislop AL, Fegan PG, Schlaeppi MJ, Duck M, Yeap BB. Prevalence and associations of psychological distress in young adults with Type 1 diabetes. Diabetic Med. 2008;25(1):91–96. doi: 10.1111/j.1464-5491.2007.02310.x. [DOI] [PubMed] [Google Scholar]