Abstract
Objectives
To 1) characterize complementary and alternative medicine (CAM) studies for posttraumatic stress disorder symptoms (PTSD), 2) evaluate the quality of these studies, and 3) systematically grade the scientific evidence for individual CAM modalities for PTSD.
Design
Systematic Review. Eight data sources were searched. Selection criteria included any study design assessing PTSD outcomes and any CAM intervention. The body of evidence for each modality was assessed with the Natural Standard evidence-based, validated grading rationale.™
Results and Conclusions
Thirty-three studies (n=1329) were reviewed. Scientific evidence of benefit for PTSD was Strong for repetitive transcranial magnetic stimulation and Good for acupuncture, hypnotherapy, meditation, and visualization. Evidence was Unclear or Conflicting for biofeedback, relaxation, Emotional Freedom and Thought Field therapies, yoga, and natural products. Considerations for clinical applications and future research recommendations are discussed.
Keywords: posttraumatic stress disorder, complementary, alternative medicine
INTRODUCTION
Posttraumatic stress disorder (PTSD) is a serious and growing health issue. Approximately 7.7 million American adults (3.5%) have PTSD in a given year.1 Not only do people with PTSD experience debilitating symptoms of PTSD, but they also have a higher prevalence of other psychiatric and physical co-morbid conditions such as depression. The annual economic burden of anxiety disorders in the United States is estimated at $42.3–$46.6 billion.2 The personal and societal costs of PTSD are high due to chronic symptoms, increased co-morbidities, and marked functional impairment.3–5
PTSD may occur when a person has been exposed to a traumatic event that involves actual or threatened death, serious injury, or threat to the physical integrity of self or others. People who acquire PTSD after a traumatic event experience a constellation of symptoms that were not present before the trauma. Symptoms fall into four diagnostic criteria: intrusion, avoidance, negative alterations in cognitions and mood, and alterations in arousal and reactivity. People with PTSD persistently re-experience the trauma through recurrent and intrusive distressing recollections of the event, and may experience severe distress when exposed to cues that symbolize or resemble aspects of the trauma. They also avoid thoughts, feelings, conversations, people, places, or activities that are reminiscent of the initial event. People with PTSD can have negative alterations in cognition or mood criteria such as the inability to recall key features of the traumatic event, persistent negative beliefs and expectations about oneself or the world, and markedly diminished interest in significant activities. They also have altered arousal and reactivity symptoms such as hypervigilance, difficulty concentrating, difficulty falling or staying asleep, irritability or outbursts of anger, or exaggerated startle response.6
The complex psychopathology and frequency of co-morbid conditions often makes PTSD difficult to treat. Trauma-focused psychotherapy has the strongest evidence for PTSD treatment.7 Yet, a high percentage of individuals do not engage in or drop-out prematurely from these treatments because of chronic patterns of avoidance and an inability to tolerate the intense emotions often experienced with these approaches.8 Avoidance behaviors may maintain PTSD symptoms by interfering with the processing of traumatic memories and preventing habituation or relearning to conditioned stimuli.9 Selective serotonin and serotonin-norepinephrine reuptake inhibitors also have strong evidence for PTSD treatment; however, medication refusal and non-compliance are quite high in this population.10 Thus, the evaluation of PTSD treatments that could be used in conjunction with or as an alternative to existing therapies is warranted.
Complementary and alternative medicines (CAM) may be beneficial for people with PTSD. The National Institutes of Health, National Center for Complementary and Alternative Medicine (NCCAM) defines CAM as a group of diverse medical and health care systems, practices, and products that are not generally considered part of conventional medicine.11 CAM therapies are attractive because they use an integrative approach to healing and usually do not report side-effects. Most CAM modalities engage the healing process without trauma recall, and are thus, not trauma-focused.
Many people with PTSD currently use CAM for their symptoms despite a lack of definitive evidence for their benefit. Thirty-eight percent of the 23,393 U.S. adults polled in a 2007 National Health Interview Survey used CAM. Of these CAM users, 2.8% reported using CAM for anxiety symptoms or anxiety related conditions including PTSD.12 The most commonly used modalities were natural products, deep breathing, meditation, chiropractic, massage, yoga, diet-based therapies, progressive relaxation, guided imagery, and homeopathic treatment. Another survey of 1004 adults reported that 43% of respondents used CAM for Generalized Anxiety Disorder, Panic Disorder, Social Anxiety Disorder, or Post-Traumatic Stress Disorder. Acupuncture, meditation/relaxation, biofeedback, chiropractic, massage, prayer, or spiritual practices were the most commonly used modalities, followed by dietary supplement and/or herbal medicine use.13 Additionally, nearly 40% people with PTSD surveyed within the Veterans Administration used CAM to address emotional and mental problems.14
PTSD is a serious and growing health concern without treatment that is acceptable to all people. CAM therapies may offer complementary and alternative therapies to existing treatments and people with PTSD are already using them for their symptoms. However, the evidence of efficacy of CAM for PTSD is limited. To date, two systematic reviews have assessed the efficacy of CAM for anxiety-related disorders including PTSD. One meta-analysis found that meditative therapies provided significant improvements in anxiety symptoms compared to controls.15 This study only included one CAM modality and was not specific for PTSD. Another systematic review found very few CAM randomized controlled trials for PTSD using stringent inclusion/exclusion criteria and the authors were unable to make any conclusions about efficacy.16
Building upon this previous work, the purpose of this systematic review was to assess the state of the science of CAM for PTSD. The objectives of this systematic review were to: 1) characterize CAM studies where PTSD outcomes were assessed, 2) evaluate the quality of these studies, and 3) systematically evaluate the evidence of CAM for PTSD symptoms. This study adds to the CAM and PTSD field by evaluating the efficacy of CAM modalities for PTSD with broader inclusion/exclusion criteria and therefore, describing a wider view of the research literature than previously done.
METHODS
Literature search methods
Comprehensive searches were conducted by a research librarian using MEDLINE (1950-3/12/2013), PsycINFO (1967-3/12/2013), CINAHL (1982-3/12/2013), Alt HealthWatch (1984-3/12/2012), AMED (1980 - 3/12/2013), Cochrane Library: CENTRAL (3/12/2013), Cochrane Database of Systematic Reviews (3/12/13), Database of Abstracts of Reviews of Effects (3/12/2013), and Health Technology Assessment Database (3/12/13). Search terms included CAM modalities and PTSD terms dependent on the search strategy required for each database (the search strategy for MEDLINE is included as Supplemental Data). All peer-reviewed studies in any language were included.
Study eligibility
Two reviewers independently screened titles and abstracts of all publications retrieved by the search strategies. Studies meeting the following inclusion criteria, and those with insufficient information to determine eligibility from the abstract, were selected for further review:
Study design
Randomized controlled trials (RCTs), non-randomized controlled trials (CTs), cross-over trials, prospective and retrospective observational studies with controls, case-control studies, and uncontrolled pre-post studies where the sample size was greater or equal to five. Studies with intention-to-treat or completer analyses were included.
Types of participants
Adults diagnosed with PTSD and/or adult participants who were administered a measure assessing PTSD symptoms.
Interventions
Any CAM modality as described on the NIH NCCAM website at the time this review was planned (3/1/12)11 including: Natural Products (herbal medicines, botanical medicine, botanicals, vitamins, minerals, other "natural products", dietary supplements, probiotics, fish oil); Mind-Body Medicine (meditation, yoga, deep-breathing exercises, guided imagery, hypnotherapy, progressive relaxation, qi gong, tai chi, biofeedback); Whole Medical Systems (acupuncture or traditional Chinese medicine, homeopathy, naturopathy, ayurvedic medicine); Manipulative and Body-Based Practices (spinal manipulation, chiropractic, osteopathy, massage); Movement Therapies (Feldenkrais method, Alexander technique, pilates, Rolfing Structural Integration, Trager psychophysical integration); Traditional/Spiritual Healing (shamanic healing, curandero); and Energy medicine (magnet therapy, light therapy, biofields, applied qi gong, Reiki, healing touch, therapeutic touch). The interventions included were based solely on the NCCAM website at the time of study design rather than on the presence of a rationale or mechanism for each included CAM modality and why it may or may not be appropriate for PTSD. Cognitive Behavioral Therapy, Prolonged Exposure Therapy, Eye Movement Desensitization (EMDR) and Reprocessing, Imagery Rehearsal and Restructuring, journaling or expressive writing studies were not included because they are used as evidenced-based standard-care for PTSD treatment. If one of these therapies was compared to a CAM therapy directly, such as EMDR versus Relaxation Therapy, the study was included. If the therapy was multimodal, where it included Cognitive Behavioral Therapy or Prolonged Exposure Therapy in addition to some CAM modalities such as relaxation or creative arts, it was excluded. Repetitive transcranial magnetic stimulation was included as a magnet therapy, and hypnotherapy and biofeedback were included as mind-body medicine therapies.
Outcome measures
Each study had to include at least one measure assessing PTSD symptoms such as intrusion, avoidance, negative alterations in cognitions and mood, and alterations in arousal and reactivity. Outcomes from any version of the Diagnostic and Statistical Manual of Mental Disorders were allowed.
Data extraction and management
The following data were collected: study design, number of treatment arms, setting, participant description, inclusion and exclusion criteria, number of subjects, mean age, intervention type and description, attrition rate, home practice details (if any), group or individual practice, outcome, time points at which outcomes were measured, p-values for each measure, and adverse events. A single reviewer extracted data and another independent reviewer verified the accuracy and completeness of the data extraction. Any discrepancies were resolved by consensus. All study data were managed with Microsoft Excel and an Access relational database (Microsoft Corporation, Redmond, Washington).
Assessment of methodological quality
Each study was evaluated for risk of bias and methodological quality. RCTs were evaluated with the Cochrane Risk of Bias Tool17 and the Quality Assessment Tool.18,17 Non-RCT studies were assessed for quality with the Quality Assessment Tool only since the Cochrane Risk of Bias Tool is specifically designed for RCTs. Two reviewers assessed the methodological quality of studies independently. A third reviewer resolved any disagreements through consensus.
Instruments used to assess Risk of Bias and Methodological Quality
The Cochrane Risk of Bias Tool evaluates selection, performance, detection, attrition, reporting and other biases and is the current gold standard for assessing bias in RCTs. Each criterion are categorized as High risk of bias, Unclear risk of bias, or Low risk of bias and consider whether the risk of bias is sufficient enough to have a notable impact on the results or conclusions of the trial. A treatment fidelity criterion, which evaluated whether or not the intervention was delivered as designed or that potential intervention deviations were assessed, was added as an “Other Bias.”
The Quality Assessment Tool (QAT) used in this study is modeled after the “Aid to the Evaluation of Therapeutic Studies” developed by Reisch et al18 and was modified as recommended by Deeks.17,19 It grades study quality on important constructs such as blinding, randomization, adequate reporting, attrition, sample size determination, and control group usage. A quantitative score is calculated that is adjusted for study design by removing questions about randomization, comparisons between groups, and blinding for non-RCT and uncontrolled trials. The result is an adjusted score on a scale of 0–100, 100 being a higher quality study.
Data synthesis and evidence grading
A meta-analysis for this study was not possible because of substantial variation in participant type, interventions, implementation, and outcomes across studies. Therefore, we sought to provide a general understanding of the available evidence for each modality. First, each study was rated as a positive, mixed, negative or neutral study (positive = most PTSD outcomes are positive; mixed = only 1–2 PTSD subscales are positive; negative = no PTSD outcomes are positive; neutral = no difference between intervention and active control)(Table 2). Studies were then grouped by modalities. The level of evidence was then graded for each modality according to the Natural Standard evidence-based grading rationale.™20 Letter grades of A-F reflect the level of scientific evidence in support of a given therapy for PTSD (A=strong scientific evidence; B=good scientific evidence; C=unclear or conflicting scientific evidence; D = fair negative scientific evidence; F = strong negative scientific evidence; L = lack of evidence). The criteria to designate each grade are described in more detail in Table 1. Grades reflect the level of available scientific data for or against the use of each therapy for a specific medical condition. For example, to receive an A level of evidence a modality had to have statistically significant evidence of benefit from >2 properly conducted RCT’s, OR evidence from one properly conducted RCT AND one properly conducted meta-analysis, OR evidence from multiple RCTs with a clear majority of the properly conducted trials showing statistically significant evidence of benefit AND with supporting evidence in basic science, animal studies, or theory. Natural Standard was founded by healthcare providers and researchers to provide high-quality, evidence-based information about CAM therapies.
Table 2.
Characteristics of included studies.
| Study/ Design |
n | % Drop out or missing data |
Gender F: M |
Mean age yrs ± SD (Range) |
Intervention
vs. Comparator |
PTSD dx required |
Participant characteristics |
Duration of intervention |
PTSD outcomes |
Results | Overall Study Outcome* |
Quality Assessment Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ENERGY MEDICINE | ||||||||||||
| Boggio, 2010 RCT | 30 | 13% | 21:9 | 44.5 ± 4.4 | rTMS 20Hz to right or left dlPFC vs.Sham rTMS | Yes, SCID criteria | Mixed trauma types | 5 sessions (1600 pulses per session)/ wk for 2 wks | PCL, TOPS | Right and left rTMS sig dec PTSD outcomes vs sham (PCL p<.001; TOPS p<.001). | Positivea | 92 |
| Cohen, 2004 RCT | 29 | 17% | 7:17* | 41.7 ± 11.4 (22–68) | rTMS 10Hz or rTMS 1Hz to right dlPFC vs.Sham rTMS | Yes, SCID criteria | Mixed trauma types | Five 20-min sessions/wk for 2 wks | PCL, TOPS, CAPS-Hebrew version | For PCL and TOPS: 10Hz rTMS sig better than sham and 1Hz (p<.002). No diff 1Hz rTMS vs. sham. | Positivea | 85 |
| Grisaru, 1998 Pre-post | 10 | 0% | 3:7 | 47 (21–53) | rTMS 0.3Hz | Yes, DSM-IV criteria | Mixed trauma types | Single session of 30 pulses at 1 min intervals | IES | No sig change in total IES or IES-I; Sig dec IES-A at 7 day follow up (p=0.033); no sig diff 28 day follow up. | Mixedc | 71 |
| Osuch, 2009 Cross-over | 9 | 0% | 8:1 | 41.4 ± 12.3 (24–56) | Imaginal exposure therapy plus rTMS 1Hz to right dlPFC vs. Imaginal exposure therapy plus sham rTMS | Yes, no criteria specified | Mixed trauma types | Three to five 30-min sessions/wk for a total of 20 sessions | CAPS, IES | No sig diff between exposure + active rTMS vs. exposure + sham rTMS except for moderate dec CAPS hyperarousal subscale (p=0.08). | Mixeda | 70 |
| Watts, 2012 RCT | 20 | 0% | 2:18 | Tx: 54 ± 12.3; Ctrl: 57.8 ± 11.8 | rTMS 1Hz to right dlPFC vs. Sham rTMS | Yes, SCID criteria | Veterans with mostly combat trauma | Five 20-min sessions/wk for 2 wks | CAPS, PCL | rTMS sig reduced CAPS (p=.009) and PCL (p=.0002) vs sham rTMS. | Positivea | 80 |
| CHINESE MEDICINE | ||||||||||||
| Hollifield, 2007 RCT | 84 | 27% | 57:27 | Acu: 42.3 ± 12.1; CBT: 40.9 ± 13.4; Ctrl: 43.4 ± 13.5 | Acupuncture vs. 1) CBT; 2) 12-wk waitlist control | Yes, SCID criteria | Mixed trauma types | Acupuncture: two 1-hr sessions/wk for 12 wks; CBT: one 2-hr session/wk for 12 wks | PSS-SR | Both acupuncture and CBT dec PTSD outcomes vs waitlist controls (p<.01). No diff between acup and CBT as both groups improved (p=0.29). | Neutrala; Positiveb | 88 |
| Zhang, 2011 RCT | 91 | 1% | 55:36 | 35.0 ± 19.3 (4–89) | Acupoint stimulation (50Hz) + CBT vs.CBT | Yes, WHO criteria | Acute PTSD from China's 2008 Zhejiang Province earthquake | Acupoint and CBT: 30 min session every other day over one wk | IES-R Chinese version | Acupoint +CBT more effective reducing IES-R than CBT alone (p<0.01). | Positivea | 77 |
| MIND-BODY: BIOFEEDBACK | ||||||||||||
| Lande, 2010 CT | 49 | 20% | 6:33* | mean/range not reported | HRV Biofeedback vs. TAU | No | Active duty combat soldiers with self-report PTSD | Two 20-mintue sessions/wk for 3 wks | PCL-M | Both biofeedback and control groups experienced sig dec in PTSD symptoms over time, no sig diff between groups. | Negativeb | 62 |
| Muller, 2009 Pre-post | 13 | 15% | 8:3* | 35.7 ± 6.1 | Pain-focused cognitive behavioral biofeedback | Yes, MINI criteria | Refugees with PTSD, chronic pain, and experience of torture or war | One 90-min session/wk for 10 wks | Post-traumatic Diagnostic Scale | No sig changes in PTSD symptoms over time. | Negativec | 76 |
| Tan, 2011 RCT | 20 | 5% | 0:20 | 36.0 ± 13.1 (24–62) | HRV Biofeedback vs. TAU | Yes, no criteria specified | Veterans with combat-related PTSD | One 30-min session/wk for 8 wks | CAPS, PCL | Biofeedback sig dec CAPS (p<.001) and PCL (p=.035) pre-post; Only CAPS-AN better in biofeedback group vs TAU; no other between group diff but moderate effect sizes for change in overall sx (Cohen’s d = 0.52–0.70 for CAPS and PCL respectively). | Mixedb | 80 |
| Zucker, 2009 RCT | 50 | 24% | 17:21* | (18–60) | RSA Biofeedbackvs.Progressive muscle relaxation recording | No | Substance use disorder and elevated PTSD sx; mixed trauma types | Personal instruction for portable biofeedback device or PMR recording: 20-mins/day for 4 wks. | PCL, PTS-T | Both groups decreased PTSD scores over time (both groups p<.01). Biofeedback did not improve PCL scores (p=0.32) or PTS-T scores (p=0.73) over control. | Neutrala | 81 |
| MIND-BODY: THOUGHT FIELD THERAPIES | ||||||||||||
| Folkes, 2002 Pre-post | 61 | 49% | not reported | 27.7 (5–48) | TFT | No | Adult and child refugees from five language groups | One 60 to 90-min session | PCL (adult or child version) | 50% dropout rate, analysis completed on 31 individuals with complete data sets. PCL-C scores dropped 40% from pre- to post-intervention (p=0.05). | Positivec | 62 |
| Karatzias, 2011 RCT | 46 | 43% | 26:20 | EFT: 39.7 ± 10.9; EMDR: 41.5 ± 10.8 | EFT vs.EMDR | Yes, DSM-IV criteria | Mixed trauma types | Up to eight 1-hour sessions. EMDR group received 3.7 ± 2.3 hrs, EFT group received 3.8 ± 2.6 hrs. | CAPS, PCL | 43.5% dropped out from the EMDR group, and 39.1% dropped out from the EFT group. Both EFT and EMDR improved all outcomes (p<.001). Effect size Cohen's d= 0.80 for both modalities. | Neutrala | 85 |
| MIND-BODY: HYPNOSIS | ||||||||||||
| Abramowitz, 2008 RCT | 32 | 0% | 0:32 | 31.7 (21–40) | Hypnosisvs.Zolpidem 10mg | Yes, DSM-IV criteria | Chronic combat-related PTSD with insomnia | Hypnosis: Two 1.5-hour sessions/wk for 2 wks; Zolpidem: 10mg nightly for 2 wks | IES-R, PDS | Hypnosis group had sig reductions in PDS (p<.034) and IES scores (p<.0005) compared to Zolpidem over the course of the study. | Positivea | 77 |
| Abramowitz, 2010 Pre-post | 37 | 3% | 0:37 | 41.2 ± 12.2 (24–64) | Hypnosis paired with olfactory based exposure | Yes, semi-structured interview with DSM-IV criteria | Combat trauma | One 90-min session/wk for 6 wks | IES-R | Hypnosis technique decreased stress reaction after 6 wks (p<.0001). | Positivec | 81 |
| Bryant, 2006 RCT | 87 | 46% | 53:34 | (17–60) | Hypnosis + CBTvs.1) CBT; 2) Supportive counseling | No | Acute stress disorder from motor vehicle accident or sexual assault | CBT and CBT plus hypnosis-Both groups five 90-min sessions | CAPS, IES | No diff in IES scores among groups. CAPS scores for CBT and CBT Hypnosis groups were 43% lower than counseling group at 3 year follow-up (p=0.05). | Neutrala | 77 |
| MIND-BODY: MEDITATION | ||||||||||||
| Bormann, 2005 Pre-post | 101 | 39% | 6:56* | 61.8 ± 13.2 (33–84) | Mantram Meditation | No | Veterans with combat-related trauma | One 90-min instructional session/wk for 5 wks plus home practice | PCL | PTSD scores (only available for n=30) decreased 13.7% from pre- to post-intervention (p=0.02). | Positivec | 90 |
| Bormann, 2008 RCT | 33 | 14% | 0:33 | 56 ± 6.6 (40–76) | Mantram Meditationvs. Waitlist control | Yes, no criteria specified | Veterans with combat-related PTSD | One 90-min session/wk for 6 wks | PCL, CAPS | Intervention improved CAPS score (effect size −0.33) and PCL score (effect size −0.72), no p values provided. | Positiveb | 85 |
| Brooks, 1985 CT | 25 | 28% | 0:18* | 33.3 | Transcendental Meditation vs.Psychotherapy | No | Vietnam veterans with chronic PTSD | Meditation: One 60-min session/wk for 12 wks; Therapy: One 60-min session/wk for 12 wks | Non-standard PTSD Scale (no reference provided in paper) | Meditation showed positive effect compared to psychotherapy for PTSD and related subscales of emotional numbness, anxiety, depression, alcohol use, insomnia, and family problems (all p<.05). | Positivea | 54 |
| Harris, 2011 RCT | 54 | 6% | 6:48 | 45.5 ± 13.5 | Spiritual prayer and/or meditation vs.Waitlist control | No | Veterans with trauma exposure, mixed trauma types | One 2-hour session/wk for 8 wks | PCL | Spiritual prayer/mediation group dec PCL vs waitlist control (p<.02) | Positiveb | 73 |
| Kearney, 2012 Pre-post | 92 | 20% | 22:70 | 51.0 ± 10.6 | Mindfulness Based Stress Reduction (MBSR) | No | Veterans, 74% screened positive for PTSD at baseline | One 2.5-hour session/wk for 8 wks | PCL | MBSR decreased PCL total and all subscores (p<.001). | Positivec | 86 |
| Kimbrough, 2010 Pre-post | 27 | 22% | 24:3 | 45 (23–68) | Mindfulness Based Stress Reduction | No | Adults with history of childhood sexual abuse | One 3-hour session/wk for 8 wks, followed by 3 refresher courses | PCL | MBSR decreased PCL total and all subscores at 8 and 24-wks post-enrollment (p<.0001). | Positivec | 95 |
| Price, 2005 RCT | 25 | 4% | 25:0 | 41 (median) (26–56) | Mindful Awareness in Body Oriented Therapyvs.Massage | No | Adult women currently in therapy for childhood sexual abuse | Two 60-min sessions/wk for 4 wks | Crime-related PTSD Scale | Both body-oriented therapy and regular massage improved PTSD symptoms, no sig diff between the groups (p>.05). | Neutrala | 81 |
| Price, 2006 RCT | 8 | 0% | 8:0 | (28–52) | Mindful Awareness in Body Oriented Therapyvs.Waitlist control | No | Adult women currently in therapy for childhood sexual abuse | One 60-min session/wk for 8 wks | Crime-related PTSD Scale | Body-oriented therapy group had sig pre-post improvement in PTSD scale (p<0.01), control group did not experience sig improvements. | Positiveb | 72 |
| Rosenthal, 2011 Pre-post | 6 | 17% | 0:6 | (25–40) | Transcendental meditation | PTSD as judged by investigator | OEF/OIF vets with combat-related | 3–5 hrs of instruction followed by home practice: 20 mins twice a day for 12 wks | CAPS, PCL-M | Participants showed sig improved CAPS (p=0.02) and PCL-M (p=0.02) scores. | Positivec | 86 |
| MIND-BODY: RELAXATION | ||||||||||||
| Colosetti, 2000 Cross-over | 5 | 0% | 5:0 | 38.8 (25–50) | Relaxation (control condition)vs.EMDR | Yes, CAPS criteria | Incarcerated women with history of abuse in an intimate relationship | One session relaxation training/wk for 3 to 6 wks followed by one session of EMDR/wk for 3 wks | IES | Neither relaxation training or EMDR exhibited sig changes in PTSD outcomes, no statistics provided due to small sample size. | Negativea | 65 |
| Echeburua, 1997 CT | 20 | 0% | 20:0 | 20 ± 7.1 | PMR (control condition)vs.Gradual self-exposure with cognitive restructuring | Yes, ADIS-R DSM-III criteria | Women with history of sexual abuse | 1x/wk for 6 wks; home practice 2x/day. | Scale of Severity of Posttraumatic Stress Disorder Symptoms | Cognitive restructuring lead to the reversal of DSM-III PTSD diagnosis in 100% of participants while relaxation was only 40% by 12 months. PTSD scale score was 4×lower in the cognitive restructuring group. | Negativea | 60 |
| Mitani, 2006 Pre-post | 22 | 0% | 0:22 | 42.2 ± 9.7 | Relaxation | No | Japanese fire fighters in a select fire station | One 60-min instructional session followed by home practice: 2–3 x/wk for 2 months. | IES-R (Japanese version) | Total IES-R scores dec 60% from pre- to post in PTSD stress-related group (p=0.04). Intrusion subscale dec sig in the PTSD stress-related group (p=.038); hyperarousal and avoidance did not change sig. No sig changes in the non-PTSD stress-related group IES scores noted (p=.76 – 1.0). | Mixedc | 68 |
| Taylor, 2003 RCT | 60 | 25% | 45:15 | 37 ± 10 | Relaxation (control condition)vs. 1) Exposure therapy; 2) EMDR | Yes, DSM-IV criteria | Mixed trauma types | Eight 90-min individualized session of relaxation, exposure, or EMDR therapy. | CAPS, PTSD Symptom Severity Scale, PTSD dx | Exposure superior to relaxation in reducing # who met PTSD dx (p<.02); no sig diff between EMDR and exposure or EMDR and relaxation for this outcome. CAPS and Symptom Severity Scale dec sig in all groups with no difference between groups. | Neutrala | 85 |
| MIND-BODY: GUIDED IMAGERY | ||||||||||||
| Jain, 2012 RCT | 123 | 17% | 11:112 | Tx: 27.1 (20–42); Ctrl: 27.9 (20–48) | Healing touch plus guided imagery vs.TAU | No | Returning combat-exposed active duty military with sig PTSD sx | Two 60-min sessions/wk for 3 wks | PCL-M | Healing touch/guided imagery group had sig dec in PCL score compared to controls (p<0.0005). | Positiveb | 92 |
| MIND-BODY: YOGIC BREATH WORK | ||||||||||||
| Descilo, 2010 CT | 183 | 3% | 160:23 | Tx 1: 30.8; Tx 2: 35.1; Ctrl: 34.7 | Yogic breath workvs. 1) Yoga breath work with exposure therapy; 2) 6-wk waitlist control | No | 2004 South East Asian tsunami survivors living in refugee camps who scored > 50 on the PCL | Breath work: one 2-hr session/day×4 days. Exposure therapy: as above + 3–5 exposure sessions | PCL | Both treatment groups showed improvement in PCL scores over waitlist control (p<.0001), no diff between active treatments. | Neutrala; Positiveb | 83 |
| NUTRACEUTICAL | ||||||||||||
| Kaplan, 1996 Cross-over | 17 | 24% | 5:8* | 39.7 (25–56) | Inositol powder 12g/day vs. Placebo (glucose powder) 12g/day | Yes, DSM-III-R criteria | Trauma type not reported | Inositol or placebo daily for 4 wks, 2 wk washout between cross-over | IES-Hebrew version | No sig diff between inositol and placebo for total IES scores or avoidance and intrusion subscales, no p values reported. | Negativea | 73 |
| Shams,2007 RCT | 40 | 0% | 34:6 | Tx: 38.2 ± 11.2; Ctrl: 38.5 ± 13.7 | Gingko Biloba 200mg vs. Placebo | Yes, DSM-IV | Earthquake survivors | 12 wks | Watson’s PTSD Scale | Sig improvement in gingko group over control (p<.01) | Positivea | 73 |
Acu: acupuncture; ADIS-R: Anxiety Disorders Interview schedule Revised; CAPS: Clinician-Administered PTSD Scale; CAPS-AN: Clinician-Administered PTSD Scale Avoidance/Numbing Subscale; CBT: cognitive behavioral therapy; CGI-I: Clinical Global Impression-Improvement; CGI-S: Clinical Global Impression-Severity; Ctrl: Control group; Dec: decreased; Diff: difference; dlPFC: dorsolateral prefrontal cortex; DSM: Diagnostic and Statistical Manual of Mental Disorders; EFT: Emotional Freedom Technique; EMDR: Eye Movement Desensitization and Reprocessing; Hr: Hour; IES: Impact of Event Scale; IES-R: Impact of Event Scale-Revised; IES-I: Impact of Event Scale Intrusion Subscale; IES-A: Impact of Event Scale Avoidance Subscale; MBSR: Mindfulness Based Stress Reduction; Min: Minute; MINI: Mini International Neuropsychiatric Interview with DSM-IV criteria; OEF: Operation Enduring Freedom; OIF: Operation Iraqi Freedom; PCL: PTSD Checklist Civilian Version; PCLM: PTSD Checklist Military Version; PDS: Posttraumatic Diagnostic Scale; PMR: Progressive muscle relaxation; PSS-SR: Posttraumatic Stress Disorder Symptom Scale Self Report; PTS-T: Posttraumatic Stress-Total scale of the Detailed Assessment of Posttraumatic States; RSA: Respiratory sinus arrhythmia; rTMS: repetitive transcranial stimulation; SCID: Structured Clinical Interview DSM-IV; Sig: Significant; Sx: Symptom; TAU: Treatment as usual; TFT: Thought field therapy; TOPS: Treatment Outcomes for PTSD Scale; Tx: Treatment; WHO: World Health Organization; Wk: Week
These studies only provided gender characteristics for those who completed the trial.
Criteria for determining overall study outcome: Positive = most PTSD outcomes showed statistically significant improvements, Mixed = only 1–2 PTSD subscales are significantly improved, Negative = no PTSD outcomes significantly improved, Neutral = both intervention and active control showed significant improvements, no difference between the groups, Two studies have two grades to account for comparisons between the active control and non-active control groups. For example, Hollifield had a positive results compared to the waitlist (Positiveb) but a Neutral results compared to the active control because both active control groups had improvements from before to after the intervention.
= active control comparison
= non-active control comparison
= no control
Table 1.
Natural Standard evidence-based validated grading rationale.
| Level of evidence grade | Criteria |
|---|---|
| A (Strong scientific evidence) | Statistically significant evidence of benefit from >2 properly randomized trials (RCTs), OR evidence from one properly conducted RCT AND one properly conducted meta-analysis, OR evidence from multiple RCTs with a clear majority of the properly conducted trials showing statistically significant evidence of benefit AND with supporting evidence in basic science, animal studies, or theory. |
| B (Good scientific evidence) | Statistically significant evidence of benefit from 1–2 properly randomized trials, OR evidence of benefit from >1 properly conducted meta-analysis OR evidence of benefit from >1 cohort/case-control/non-randomized trials AND with supporting evidence in basic science, animal studies, or theory. |
| C (Unclear or conflicting scientific evidence) | Evidence of benefit from >1 small RCT(s) without adequate size, power, statistical significance, or quality of design by objective criteria, OR conflicting evidence from multiple RCTs without a clear majority of the properly conducted trials showing evidence of benefit or ineffectiveness, OR evidence of benefit from >1 cohort/case-control/non-randomized trials AND without supporting evidence in basic science, animal studies, or theory, OR evidence of efficacy only from basic science, animal studies, or theory. |
| D (Fair negative scientific evidence) | Statistically significant negative evidence (i.e., lack of evidence of benefit) from cohort/case-control/non-randomized trials, AND evidence in basic science, animal studies, or theory suggesting a lack of benefit. |
| F (Strong negative scientific evidence) | Statistically significant negative evidence (i.e., lack of evidence of benefit) from >1 properly randomized adequately powered trial(s) of high-quality design by objective criteria. |
| Lack of evidence | Unable to evaluate efficacy due to lack of adequate available human data. |
RESULTS
Search results
A total of 1596 studies were identified (Figure 1). After removing duplicates, 1337 titles and abstracts were screened for inclusion criteria. Ninety full text articles were assessed for eligibility, and of these, 33 were included in the final review (Table 2).
Figure 1.
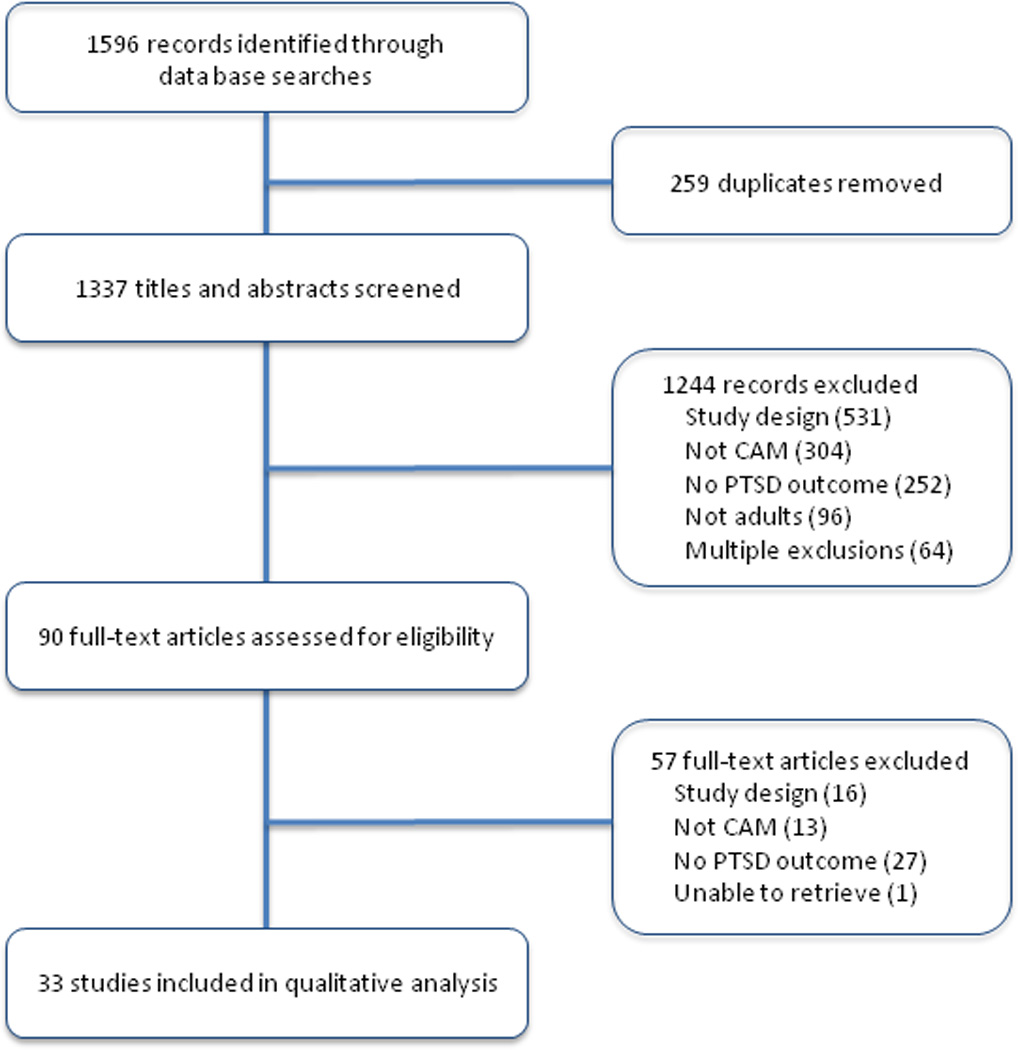
Study flow diagram.
Description of included studies
All manuscripts were published between 1985 and 2012. Eighteen of the studies were conducted within the last 5 years (2008–2012). There were 17 RCTs, four non-RCTs, nine pre-post designs, and three crossover interventions. The mean sample size was 40 ± 38 (range 5–183). In total, 1329 participants were included. Of the controlled trials, 13 used active control groups (either another intervention or placebo intervention), six used non-active controls (waitlist or treatment as usual), and two used active and non-active controls. Eighteen studies confirmed PTSD diagnosis of participants and 15 did not. PTSD diagnosis was confirmed using clinician assessed diagnostic criteria and/or through structured clinical interviews (DSM-III (2); DSM-IV (6), CAPS (1), M.I.N.I. (1), WHO criteria (1), SCID (4)) for most but not all studies. Three studies did not note criteria for confirming PTSD diagnosis. Participants experienced diverse traumatic events: combat exposure (10 studies), natural disaster (3), sexual assault (3), abuse (2), war (2), fire-fighting (1), mixed traumatic events (11), and one study did not report the trauma type. Seven studies had all male participants and four studies had all female participants. The remaining studies had an average of 45% females ± 38% (range 9–89%). One study did not report gender data. Most studies used mind-body therapies, including biofeedback (4 studies), hypnosis (3), meditation (9), relaxation (4), Emotional Freedom and Thought Field therapies (2), visualization (1), and yogic breath work (1). Other modalities represented were repetitive transcranial magnetic stimulation (rTMS) (5), acupuncture (2), and natural products (inositol and ginkgo biloba) (2). PTSD outcomes varied and included one or more of the following: the PTSD Checklist (PCL, civilian and military versions), Clinician-Administered PTSD Scale (CAPS), Impact of Events Scale (IES), Crime-related PTSD Scale, Posttraumatic Diagnostic Scale, Severity of Symptoms Scale for PTSD (Spanish adaptation of PTSD Symptom Scale by Foa 1993), Treatment Outcome PTSD Scale, and the Clinical Global Impressions (CGI).
Methodological quality of included studies
Methodological quality for all studies as determined by the QAT is presented in Table 2. The mean score was mean 78 ± 9 (median 80, range 54–95). Several criteria were met by the majority of studies (at least 31 out of 33): the purpose of the study was stated, outcomes were validated and adequately described, the intervention was reasonable and appropriate to answer questions posed by researchers, intervention protocols were adequately described, participant demographic information was reported, and descriptive measures were identified for all important variables. Five studies reported a power calculation to determine adequate sample size. Blinding of participants or outcome assessors was discussed in 11 of the 24 controlled and cross-over design studies. Thirteen studies reported adverse events.
Table 3 summarizes the risk of bias for the 17 RCTs included in this review. Several of the studies failed to provide enough detail for adequate assessment; methods of random sequence generation and allocation concealment were particularly poorly reported. The rTMS studies and the nutraceutical studies used a sham or placebo control group that allowed for participant blinding. One study21 assessed treatment credibility as it was perceived by the participants (i.e. expectation). Nine of the studies explicitly stated that outcomes assessors were blinded to treatment group. In general, RCT sample sizes were small (7 of the 17 RCTs had n < 33). Three studies performed intention-to-treat analyses.22–24
Table 3.
Summary of risk of bias for randomized controlled CAM trials for PTSD.
| Study | Intervention | Random sequence generation |
Allocation concealment |
Blinding of participants/ personnel |
Blinding of outcome assessment |
Incomplete outcome data |
Selective reporting |
Fidelity of intervention assessed |
|---|---|---|---|---|---|---|---|---|
| Energy modalities | ||||||||
| Boggio, 2010 | rTMS | + | ? | + | + | + | + | N/A |
| Cohen, 2004 | rTMS | ? | ? | + | + | ? | + | N/A |
| Watts, 2012 | rTMS | ? | ? | + | + | + | + | N/A |
| Chinese medicine | ||||||||
| Hollifield, 2007 | Acupuncture | + | + | - | + | + | + | + |
| Zhang, 2011 | Acupoint stimulation | ? | ? | - | - | + | + | - |
| Nutraceutical | ||||||||
| Shams, 2007 | Ginkgo Biloba | ? | ? | + | ? | + | + | ? |
| Mind-body modalities | ||||||||
| Tan, 2011 | Biofeedback | ? | ? | - | ? | + | + | + |
| Zucker, 2009 | Biofeedback | + | ? | - | ? | + | + | ? |
| Karatzias, 2011 | EFT | + | ? | - | + | + | + | ? |
| Abramowitz, 2008 | Hypnosis | ? | ? | - | ? | + | + | ? |
| Bryant, 2006 | Hypnosis | + | - | - | + | - | + | + |
| Bormann, 2008 | Meditation | + | ? | - | + | + | + | + |
| Harris, 2011 | Meditation | + | ? | - | ? | + | + | + |
| Price, 2005 | Meditation | ? | ? | - | ? | + | + | + |
| Price, 2006 | Meditation | ? | ? | - | ? | + | + | + |
| Taylor, 2003 | Relaxation | ? | ? | + | + | - | + | + |
| Jain, 2012 | Guided imagery | + | + | - | + | ? | + | ? |
EFT: emotional freedom technique; rTMS: repetitive transcranial magnetic stimulation
( ) Low risk of bias
) Low risk of bias
( ) High risk of bias
) High risk of bias
( ) Unclear risk of bias
) Unclear risk of bias
Quality of the body of evidence for each modality
The body of evidence for each modality for PTSD was reviewed. Letter grades were derived for each modality using the Natural Standard evidence-based grading rationale.™ Table 1 describes the criterion for each grade. The individual study outcomes that determined the grades are listed in Table 2.
rTMS
Five trials (3 RCTs, 1 pre-post, and 1 cross-over) were included. The RCTs were of generally high quality (QAT scores ranging from 71 – 88) and all had positive results. Both the pre-post and cross-over trials had lower quality ratings and showed mixed result. GRADE A.
Acupuncture
Two RCTs, both of which demonstrated significantly improved symptoms over control conditions were included. Hollifield found that acupuncture was as effective as CBT when compared to a waitlist control,23 and Zhang found that acupoint stimulation combined with CBT was more effective than CBT alone.25 Because these are slightly different modalities, further research is warranted. GRADE B.
Biofeedback
Four trials (1 RCTs, 1 CT, and 2 pre-post studies) were included. The controlled trials had high QAT quality scores, with either mixed results or no difference from the control group. The other studies had small sample sizes and methodological concerns. GRADE C.
Emotional Freedom Technique/Thought Field Therapy
The body of evidence for these mind-body techniques includes one RCT showing no difference between Emotional Freedom Technique and EMDR, and 1 pre-post trial with positive results. While the non-inferiority of Emotional Freedom Technique to EMDR is an intriguing finding, both trials had significant drop out rates (43% and 49%, respectively), bringing into question the validity of results. GRADE C.
Hypnotherapy
Three studies (2 RCTs and 1 pre-post) were included. Both RCTs had active control groups. In one study, the hypnotherapy group did just as well as the CBT group at a three-year follow-up.22 In the other study, the hypnotherapy group had significantly greater improved outcomes than Zolpidem.26 The Zolpidem study was targeted at improving insomnia for people with PTSD rather than PTSD symptoms directly and Zopidem as a hypnotic pharmaceutical would not be expected to improve PTSD symptoms. The grade remains the same if this study is excluded. GRADE B.
Meditation
Nine studies were included, five RCTs and four pre-posts. Meditation represents the largest number of CAM studies for any modality included in this review. All the pre-post studies showed positive outcomes and high QAT scores (all > 86). While the RCTs were of variable quality and sample size, the majority favored meditation over waitlist controls. Several different types of meditation were assessed and heterogeneity complicated the grading of this modality. GRADE B.
Relaxation
Four studies (2 RCTs, 1 pre-post, and 1 cross-over) were included, three of which had significant methodological issues and showed mixed or negative results. GRADE C.
Visualization
One large, high quality RCT was included. This study combined healing touch with guided imagery and demonstrated significant improvements in PTSD symptoms compared to treatment as usual. GRADE B.
Yoga breath work
One large non-randomized CT was included demonstrating that yoga breath work alone and in combination with exposure therapy is better than wait list for acute trauma survivors. GRADE C.
Natural products
Two RCTs were included. One small RCT showed no effect of inositol compared to placebo. Another small RCT showed a positive effect of ginkgo biloba on PTSD outcomes compared to placebo. GRADE C.
Grades were reassessed for two sub-groups: 1) studies where PTSD was required and 2) RCTs. These subgroup analyses are important because they reflect more stringent inclusion criteria and lend credibility to the application of these modalities under more specific circumstances. When evaluating only those studies where a PTSD diagnosis was required, all grades remained the same except for three modalities. Meditation was reduced from a B to a C because only one out of the nine meditation studies required a PTSD diagnosis. Guided Imagery and yoga breath work were downgraded to Lack of Evidence because neither of these studies required a PTSD diagnosis. When evaluating only the RCTs, all grades remained the same except, again, yoga breath work was downgraded to Lack of Evidence because it did not include an RCT.
Discussion
The objectives of this review were to systematically characterize and evaluate CAM studies for PTSD. We believe that at this relatively young stage of CAM research it is important to evaluate all the available evidence for a particular modality, and inclusion criteria were deliberately kept broad to capture as many studies as possible. We found 33 CAM studies that used 10 different modalities to assess PTSD outcomes. Scientific evidence of benefit for PTSD was Strong for rTMS, and Good for acupuncture, hypnotherapy, meditation, and visualization. Evidence was Unclear or Conflicting for biofeedback, relaxation, Emotional Freedom and Thought Field therapies, yoga breath work, and natural products.
Implications for research
Studies included in this review were of variable quality. Important aspects of rigorous research design were often not conducted or not reported. In order to improve the quality of the CAM research field and accurately determine efficacy of CAM modalities, investigators are encouraged to consider the following when designing studies: 1) Choose an appropriate control (i.e. active, non-active or both) depending on the research question;27 2) Assess for expectancy and placebo effects because they play a pivotal role in mind-body studies;28,29 3) Blind research staff and participants if possible; 4) Randomize participants; 5) Clearly define the population being studied; 6) Determine an appropriate sample size; and 7) Follow standard rigorous clinical design and reporting guidelines.30,31 This will help improve the quality of CAM studies and thus the quality of evidence.
Overall completeness and applicability of evidence
Studies in this review recruited from a variety of settings (e.g. Veteran’s Administration facilities, outpatient clinics, prison) and countries (North America, Asia, Iran, and Israel). Participants were from the general population, combat veterans, firefighters, and sexual abuse survivors. About one-third of the studies were specific for combat-related trauma and another third enrolled participants with a diverse mix of trauma exposure. Studies varied widely with respect to participant gender. Some studies enrolled only men, other studies only women, and several had a diverse mix of male and female participants. All-male studies most frequently targeted combat-related trauma whereas all-female studies more often addressed sexual abuse, thus reflecting gender differences associated with these trauma exposures. While the grades did not distinguish by trauma type or gender, the results lend preliminary support to the acceptability of CAM for people with a variety of trauma exposures and genders. Additional research and synthesis of evidence is needed to address the efficacy of each modality by trauma exposure and gender.
Implications for clinical practice
There is positive evidence of effectiveness for rTMS, acupuncture, hypnotherapy, meditation, and visualization for the treatment of PTSD symptoms. rTMS had the strongest scientific evidence followed by acupuncture, hypnotherapy, meditation, and visualization. Practitioners may take this evidence into account when considering these CAM modalities for treating patients with PTSD symptoms.
rTMS is a noninvasive and painless technique that directly stimulates cortical neurons and is approved by the Food and Drug administration for the treatment of depression.32 TMS induces significant changes on monoamine neurotransmitters and cortisol, neuroendocrine factors also affected in PTSD. Future TMS research would clarify dosing relationships to efficacy (i.e. frequency used (low or high), area of brain treated, and timing and duration of sessions). Acupuncture is a Chinese medicine energy modality that uses needles inserted into specific points along the body’s energetic meridians. Acupuncture may help PTSD through its effects on the autonomic nervous system and prefrontal and limbic brain structures, systems that are intrinsically involved in PTSD pathophysiology.23,33
Meditation also appears to be helpful for PTSD. While there are various meditation styles, all types incorporate self-observation of mental activity, attention training, and cultivating an attitude that highlights process rather than content.34 Meditation studies show positive benefit for a variety of symptoms related to PTSD such as depressive symptoms or relapse,35–41 anxiety,40,42–45 suicidal behavior,46 and sleep disturbances.47,48 Meditation may affect PTSD symptoms through attention training, improving prefrontal cortex activity and autonomic nervous system function, changing thought patterns, increasing emotional acceptance and reducing avoidance, and regulating the hypothalamic-pituitary-adrenal axis.49
Hypnotherapy, another mind-body medicine, is a psychotherapeutic technique based on the hypnotist providing suggestions for changes in sensation, perception, cognition, affect, mood, or behavior.50 Hypnotherapy may allow people with PTSD to down-regulate their autonomic nervous system and thus become more receptive to changes in cognition, mood or behavior.
Similarly, visualization is designed specifically for the patient’s imagination (mind) to have an effect on a physiological system (body). Visualization is a lived experience that is a dynamic, quasi-real, psychophysiological process.51 Guided imagery is a variation on visualization where another person leads an individual through experiences in the mind to access the physical, emotional and spiritual dimensions that effect physiological change, modulating the individual’s response.52 Both hypnotherapy and visualization/guided imagery could be modified to specifically address the symptoms the person with PTSD is experiencing.
At this point, the evidence is Unclear or Conflicting for biofeedback, Emotional Freedom and Thought Field Therapies, yoga breath work, relaxation, and natural products. Future studies are warranted to clarify results before practitioners should recommend them specifically for PTSD symptoms.
Agreement and disagreements with other studies or reviews
Our work builds on a previous review conducted by Strauss et al. that found inconclusive evidence for all the CAM modalities they assessed using very stringent inclusion and exclusion criteria.16 Similarly, we found inconclusive evidence for some modalities. However, because we included study designs other than RCTs, participants with PTSD symptoms (and not just a PTSD diagnosis), and used a different grading schema, we were able to present a broader view of the state of CAM research. Our study was also different in that we included rTMS as a CAM modality, evaluated Natural Products, and included non-English papers in our search criteria. While our overall search strategy was not as comprehensive, both reviews highlight the importance of improved CAM clinical trial methods, more rigorous reporting, and the need for more RCTs in CAM research.
Limitations
Various limitations must be considered when reviewing these results. Some modalities included in this review may not be considered CAM modalities (e.g. rTMS because of its psychiatry heritage; biofeedback because of its common use in mainstream academic medicine and clinical psychology; and hypnotherapy as a psychosocial treatment). For this study, we used the CAM definition a priori as explained on the NCCAM website11 at the time of designing the study. Those definitions included magnet therapy under the Energy Medicine category and hypnotherapy under the Mind-Body Medicine category. rTMS, biofeedback, and hypnotherapy could also be included as complementary because they are not evidence-based standard care treatments for PTSD, even though they may be considered conventional for other conditions.
Although we included all languages in our search strategy we only found English papers. We searched only published papers; grey literature resources were not included and hand-searches of relevant bibliographies were not conducted. Publication bias is present when positive trials are more frequently published over negative studies. It is possible that this impacted our review as we found 17 positive trials and five negative trials (7 neutral and four mixed). Another limitation is that we did not take into account outcome measure timing in our grading schema. For example, we were not able to distinguish if each modality had more or less evidence for PTSD symptoms immediately after the treatment versus at a longer-term follow-up. Additional studies with less heterogeneity in methods, participants and outcomes need to be conducted before rigorous meta-analyses can be done. Because of this, the results from this study must be viewed as qualitative trends rather than conclusions.
Conclusions
Several CAM modalities may be helpful for improving PTSD symptoms. rTMS has the strongest evidence for benefit followed by acupuncture, hypnotherapy, meditation, and visualization. There is insufficient evidence to recommend biofeedback, Emotional Freedom and Thought Field Therapies, relaxation, yoga breath work, and natural products at this time. Future research should include larger, properly randomized, controlled trials with appropriately selected control groups and rigorous methodology.
Supplementary Material
Acknowledgment
The authors would like to thank Hannah Moshontz for her help with this project. This work was supported by the National Center for Complementary and Alternative Medicine of the National Institutes of Health [Grant numbers T32AT002688, K01AT004951, K24AT005121]; and the Agency for Healthcare Research Quality [Grant number 5T32HS017582-05]. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest statement No competing financial interests exist for all authors.
References
- 1.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 15939839. 2005 Jun;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marciniak MD, Lage MJ, Dunayevich E, et al. The cost of treating anxiety: the medical and demographic correlates that impact total medical costs. Depress Anxiety 16075454. 2005;21(4):178–184. doi: 10.1002/da.20074. [DOI] [PubMed] [Google Scholar]
- 3.Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Psychoneuroimmunology and psychosomatic medicine: back to the future. Psychosom Med 11818582. 2002 Jan-Feb;64(1):15–28. doi: 10.1097/00006842-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Solomon SD, Davidson JR. Trauma: prevalence, impairment, service use, cost. J Clin Psychiatry 9329445. 1997;58(Suppl 9):5–11. [PubMed] [Google Scholar]
- 5.Brunello N, Davidson JR, Deahl M, et al. Posttraumatic stress disorder: diagnosis and epidemiology, comorbidity and social consequences, biology and treatment. Neuropsychobiology 11287794. 2001;43(3):150–162. doi: 10.1159/000054884. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Publishing Inc.; 2013. [Google Scholar]
- 7.Berg AO, Breslau N, Goodman SN, et al. Treatment of PTSD: An Assessment of the Evidence. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 8.Grunert BK, Weis JM, Smucker MR, Christianson HF. Imagery rescripting and reprocessing therapy after failed prolonged exposure for post-traumatic stress disorder following industrial injury. J Behav Ther Exp Psychiatry 18037391. 2007 Dec;38(4):317–328. doi: 10.1016/j.jbtep.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Foa EB, Hembree EA, Rothbaum B. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences. New York: Oxford University Press; 2007. [Google Scholar]
- 10.Rakofsky JJ, Levy ST, Dunlop BW. Conceptualizing Treatment Nonadherence in Patients with Bipolar Disorder and PTSD. CNS Spectr 21406162. 2011 Jan 15; doi: 10.1017/S1092852912000119. [DOI] [PubMed] [Google Scholar]
- 11.NCCAM. What Is Complementary and Alternative Medicine? 2008 http://webarchiveorg/web/20130216005936/http://nccamnihgov/health/whatiscam.
- 12.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report 19361005. 2008 Dec 10;(12):1–23. [PubMed] [Google Scholar]
- 13.Bystritsky A, Hovav S, Sherbourne C, et al. Use of complementary and alternative medicine in a large sample of anxiety patients. Psychosomatics 22304968. 2012 May;53(3):266–272. doi: 10.1016/j.psym.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Libby DJ, Pilver CE, Desai R. Complementary and alternative medicine in VA specialized PTSD treatment programs. Psychiatric Services 23117511. 2012 Nov;63(11):1134–1136. doi: 10.1176/appi.ps.201100456. [DOI] [PubMed] [Google Scholar]
- 15.Chen KW, Berger CC, Manheimer E, et al. Meditative therapies for reducing anxiety: a systematic review and meta-analysis of randomized controlled trials. Depression and Anxiety 22700446. 2012 Jul;29(7):545–562. doi: 10.1002/da.21964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Strauss JL, Coeytaux R, McDuffie J, Nagi A, Williams JW. Efficacy of Complementary and Alternative Medicine Therapies for Posttraumatic Stress Disorder. Washington (DC): Department of Veterans Affairs; 2011. [2011/12/31 ed]. [PubMed] [Google Scholar]
- 17.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ (Clinical Research Ed) 22008217. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reisch JS, Tyson JE, Mize SG. Aid to the evaluation of therapeutic studies. Pediatrics 2797977. 1989 Nov;84(5):815–827. [PubMed] [Google Scholar]
- 19.Deeks JJ, Dinnes J, D'Amico R, et al. Evaluating non-randomised intervention studies. Health Technol Assess. 2003;7(27):iii–x. 1–173. doi: 10.3310/hta7270. [DOI] [PubMed] [Google Scholar]
- 20.Natural Standard. Natural Standard evidence-based validated grading rationale. [Accessed 10/10/13];2010 http://wwwnaturalstandardcom/gradingasp. [Google Scholar]
- 21.Taylor S, Thordarson DS, Maxfield L, Fedoroff IC, Lovell K, Ogrodniczuk J. Comparative efficacy, speed, and adverse effects of three PTSD treatments: exposure therapy, EMDR, and relaxation training. J Consult Clin Psychol. 2003;71(2):330–338. doi: 10.1037/0022-006x.71.2.330. [DOI] [PubMed] [Google Scholar]
- 22.Bryant RA, Moulds ML, Nixon RDV, Mastrodomenico J, Felmingham K, Hopwood S. Hypnotherapy and cognitive behaviour therapy of acute stress disorder: a 3-year follow-up. Behaviour Research & Therapy. 2006 Sep;44(9):1331–1335. doi: 10.1016/j.brat.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 23.Hollifield M, Sinclair-Lian N, Warner TD, Hammerschlag R. Acupuncture for posttraumatic stress disorder: a randomized controlled pilot trial. J Nerv Ment Dis. 2007 Jun;195(6):504–513. doi: 10.1097/NMD.0b013e31803044f8. [DOI] [PubMed] [Google Scholar]
- 24.Karatzias T, Power K, Brown K, et al. A controlled comparison of the effectiveness and efficiency of two psychological therapies for posttraumatic stress disorder: eye movement desensitization and reprocessing vs. emotional freedom techniques. J Nerv Ment Dis. 2011 Jun;199(6):372–378. doi: 10.1097/NMD.0b013e31821cd262. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, Feng B, Xie J-P, Xu F-Z, Chen J. Clinical study on treatment of the earthquake-caused post-traumatic stress disorder by cognitive-behavior therapy and acupoint stimulation. J Tradit Chin Med. 2011 Mar;31(1):60–63. doi: 10.1016/s0254-6272(11)60014-9. [DOI] [PubMed] [Google Scholar]
- 26.Abramowitz EG, Barak Y, Ben-Avi I, Knobler HY. Hypnotherapy in the treatment of chronic combat-related PTSD patients suffering from insomnia: a randomized, zolpidem-controlled clinical trial. The International journal of clinical and experimental hypnosis. 2008 Jul;56(3):270–280. doi: 10.1080/00207140802039672. [DOI] [PubMed] [Google Scholar]
- 27.Caspi O, Burleson KO. Methodological challenges in meditation research. Adv Mind Body Med 15973854. 2005 Spring;21(1):4–11. [PubMed] [Google Scholar]
- 28.Oken BS, Zajdel D, Kishiyama S, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern Ther Health Med 16454146. 2006 Jan-Feb;12(1):40–47. [PMC free article] [PubMed] [Google Scholar]
- 29.Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H. The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review. Health Technol Assess 10448203. 1999;3(3):1–96. [PubMed] [Google Scholar]
- 30.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med 20352064. 2010;7(3):e1000251. doi: 10.1371/journal.pmed.1000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 18283207. 2008 Feb 19;148(4):295–309. doi: 10.7326/0003-4819-148-4-200802190-00008. [DOI] [PubMed] [Google Scholar]
- 32.Berlim MT, Van den Eynde F, Jeff Daskalakis Z. Clinically meaningful efficacy and acceptability of low-frequency repetitive transcranial magnetic stimulation (rTMS) for treating primary major depression: a meta-analysis of randomized, double-blind and sham-controlled trials. Neuropsychopharmacology. 2013 Mar;38(4):543–551. doi: 10.1038/npp.2012.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hollifield M. Acupuncture for posttraumatic stress disorder: conceptual, clinical, and biological data support further research. CNS Neurosci Ther. 2011 Dec;17(6):769–779. doi: 10.1111/j.1755-5949.2011.00241.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ospina MB, Bond K, Karkhaneh M, et al. Meditation practices for health: state of the research. Evid Rep Technol Assess (Full Rep) 17764203. 2007 Jun;(155):1–263. [PMC free article] [PubMed] [Google Scholar]
- 35.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res 15256293. 2004 Jul;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 36.Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. J Consult Clin Psychol 14756612. 2004 Feb;72(1):31–40. doi: 10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- 37.Mason O, Hargreaves I. A qualitative study of mindfulness-based cognitive therapy for depression. Br J Med Psychol 11802836. 2001 Jun;74(Part 2):197–212. [PubMed] [Google Scholar]
- 38.Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol 10965637. 2000 Aug;68(4):615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 39.Kenny MA, Williams JM. Treatment-resistant depressed patients show a good response to Mindfulness-based Cognitive Therapy. Behav Res Ther 16797486. 2007 Mar;45(3):617–625. doi: 10.1016/j.brat.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Finucane A, Mercer SW. An exploratory mixed methods study of the acceptability and effectiveness of Mindfulness-Based Cognitive Therapy for patients with active depression and anxiety in primary care. BMC Psychiatry 16603060. 2006;6:14. doi: 10.1186/1471-244X-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sephton SE, Salmon P, Weissbecker I, et al. Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: results of a randomized clinical trial. Arthritis Rheum. 2007 Feb 15;57(1):77–85. doi: 10.1002/art.22478. [DOI] [PubMed] [Google Scholar]
- 42.Tacon AM, McComb J, Caldera Y, Randolph P. Mindfulness meditation, anxiety reduction, and heart disease: a pilot study. Fam Community Health 12802125. 2003 Jan-Mar;26(1):25–33. doi: 10.1097/00003727-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Miller JJ, Fletcher K, Kabat-Zinn J. Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. Gen Hosp Psychiatry 7649463. 1995 May;17(3):192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- 44.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry 1609875. 1992 Jul;149(7):936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- 45.McKee L, Zvolensky MJ, Solomon SE, Bernstein A, Leen-Feldner E. Emotional-vulnerability and mindfulness: a preliminary test of associations among negative affectivity, anxiety sensitivity, and mindfulness skills. Cogn Behav Ther 17530495. 2007;36(2):91–101. doi: 10.1080/16506070601119314. [DOI] [PubMed] [Google Scholar]
- 46.Williams JM, Duggan DS, Crane C, Fennell MJ. Mindfulness-Based cognitive therapy for prevention of recurrence of suicidal behavior. J Clin Psychol 16342287. 2006 Feb;62(2):201–210. doi: 10.1002/jclp.20223. [DOI] [PubMed] [Google Scholar]
- 47.Shapiro SL, Bootzin RR, Figueredo AJ, Lopez AM, Schwartz GE. The efficacy of mindfulness-based stress reduction in the treatment of sleep disturbance in women with breast cancer: an exploratory study. J Psychosom Res 12505559. 2003 Jan;54(1):85–91. doi: 10.1016/s0022-3999(02)00546-9. [DOI] [PubMed] [Google Scholar]
- 48.Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med 16262547. 2005;12(4):278–285. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- 49.Wahbeh H. Mindfulness meditation for posttraumatic stress disorder. In: Ie A, Ngnoumen CT, Langer E, editors. The Wiley Blackwell Handbook of Mindfulness. First ed. Chichester, UK: John Wiley & Sons, Ltd; 2014. pp. 776–793. [Google Scholar]
- 50.Montgomery GH, Schnur JB, Kravits K. Hypnosis for cancer care: over 200 years young. CA. Cancer J. Clin. 2013 Jan;63(1):31–44. doi: 10.3322/caac.21165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Menzies V, Taylor AG, Bourguignon C. Effects of guided imagery on outcomes of pain, functional status, and self-efficacy in persons diagnosed with fibromyalgia. J Altern Complement Med 16494565. 2006 Jan-Feb;12(1):23–30. doi: 10.1089/acm.2006.12.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Achterberg J. Imagery in Healing Shamanism and Modern Medicine. Boston: Massachusetts: Shambhala Publications, Inc; 1985. [Google Scholar]
Included Studies
- Abramowitz EG, Barak Y, Ben-Avi I, Knobler HY. Hypnotherapy in the treatment of chronic combat-related PTSD patients suffering from insomnia: a randomized, zolpidem-controlled clinical trial. International Journal of Clinical & Experimental Hypnosis. 2008;56(3):270–280. doi: 10.1080/00207140802039672. [DOI] [PubMed] [Google Scholar]
- Abramowitz EG, Lichtenberg P. A new hypnotic technique for treating combat-related posttraumatic stress disorder: a prospective open study. International Journal of Clinical & Experimental Hypnosis. 2010;58(3):316–328. doi: 10.1080/00207141003760926. [DOI] [PubMed] [Google Scholar]
- Boggio PS, Rocha M, Oliveira MO, Fecteau S, Cohen RB, Campanha C, Fregni F. Noninvasive brain stimulation with high-frequency and low-intensity repetitive transcranial magnetic stimulation treatment for posttraumatic stress disorder. The Journal of Clinical Psychiatry. 2010;71(8):992–999. doi: 10.4088/JCP.08m04638blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bormann JE, Smith TL, Becker S, Gershwin M, Pada L, Grudzinski AH, Nurmi EA. Efficacy of frequent mantram repetition on stress, quality of life, and spiritual well-being in veterans: a pilot study. Journal of Holistic Nursing. 2005;23(4):395–414. doi: 10.1177/0898010105278929. [DOI] [PubMed] [Google Scholar]
- Bormann JE, Thorp S, Wetherell JL, Golshan S. A spiritually based group intervention for combat veterans with posttraumatic stress disorder: feasibility study. Journal of Holistic Nursing. 2008;26(2):109–116. doi: 10.1177/0898010107311276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks JS, Scarano T. Transcendental Meditation in the treatment of post-Vietnam adjustment. Journal of Counseling & Development. 1985;64(3):212–215. [Google Scholar]
- Bryant RA, Moulds ML, Nixon RD, Mastrodomenico J, Felmingham K, Hopwood S. Hypnotherapy and cognitive behaviour therapy of acute stress disorder: a 3-year follow-up. Behaviour Research and Therapy. 2006;44(9):1331–1335. doi: 10.1016/j.brat.2005.04.007. [DOI] [PubMed] [Google Scholar]
- Cohen H, Kaplan Z, Kotler M, Kouperman I, Moisa R, Grisaru N. Repetitive Transcranial Magnetic Stimulation of the Right Dorsolateral Prefrontal Cortex in Posttraumatic Stress Disorder: A Double-Blind, Placebo-Controlled Study. The American Journal of Psychiatry. 2004;161(3):515–524. doi: 10.1176/appi.ajp.161.3.515. [DOI] [PubMed] [Google Scholar]
- Colosetti SD, Thyer BA. The relative effectiveness of EMDR versus relaxation training with battered women prisoners. Behavior Modification. 2000;24(5):719–739. doi: 10.1177/0145445500245006. [DOI] [PubMed] [Google Scholar]
- Descilo T, Vedamurtachar A, Gerbarg PL, Nagaraja D, Gangadhar BN, Damodaran B, Brown RP. Effects of a yoga breath intervention alone and in combination with an exposure therapy for post-traumatic stress disorder and depression in survivors of the 2004 South-East Asia tsunami. Acta Psychiatrica Scandinavica. 2010;121(4):289–300. doi: 10.1111/j.1600-0447.2009.01466.x. [DOI] [PubMed] [Google Scholar]
- Echeburua E, de Corral P, Zubizarreta I, Sarasua B. Psychological treatment of chronic posttraumatic stress disorder in victims of sexual aggression. Behavior Modification. 1997;21(4):433–456. doi: 10.1177/01454455970214003. [DOI] [PubMed] [Google Scholar]
- Folkes CE. Thought field therapy and trauma recovery. International Journal of Emergency Mental Health. 2002;4(2):99–103. [PubMed] [Google Scholar]
- Grisaru N, Amir M, Cohen H, Kaplan Z. Effect of transcranial magnetic stimulation in posttraumatic stress disorder: A preliminary study. Biological Psychiatry. 1998;44(1):52–55. doi: 10.1016/s0006-3223(98)00016-x. [DOI] [PubMed] [Google Scholar]
- Harris J, Erbes CR, Engdahl BE, Thuras P, Murray-Swank N, Grace D, Le T. The effectiveness of a trauma-focused spiritually integrated intervention for veterans exposed to trauma. Journal of Clinical Psychology. 2011;67(4):425–438. doi: 10.1002/jclp.20777. [DOI] [PubMed] [Google Scholar]
- Hollifield M, Sinclair-Lian N, Warner TD, Hammerschlag R. Acupuncture for posttraumatic stress disorder: a randomized controlled pilot trial. Journal of Nervous & Mental Disease. 2007;195(6):504–513. doi: 10.1097/NMD.0b013e31803044f8. [DOI] [PubMed] [Google Scholar]
- Jain S, McMahon GF, Hasen P, Kozub MP, Porter V, King R, Guarneri EM. Healing touch with guided imagery for PTSD in returning active duty military: A randomized controlled trial. Military Medicine. 2012;177(9):1015–1021. doi: 10.7205/milmed-d-11-00290. [DOI] [PubMed] [Google Scholar]
- Kaplan Z, Amir M, Swartz M, Levine J. Inositol treatment of post-traumatic stress disorder. Anxiety. 1996;2(1):51–52. doi: 10.1002/(SICI)1522-7154(1996)2:1<51::AID-ANXI8>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Karatzias T, Power K, Brown K, McGoldrick T, Begum M, Young J, Adams S. A controlled comparison of the effectiveness and efficiency of two psychological therapies for posttraumatic stress disorder: eye movement desensitization and reprocessing vs. emotional freedom techniques. Journal of Nervous & Mental Disease. 2011;199(6):372–378. doi: 10.1097/NMD.0b013e31821cd262. [DOI] [PubMed] [Google Scholar]
- Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Association of participation in a mindfulness program with measures of PTSD, depression and quality of life in a veteran sample. Journal of Clinical Psychology. 2012;68(1):101–116. doi: 10.1002/jclp.20853. [DOI] [PubMed] [Google Scholar]
- Kimbrough E, Magyari T, Langenberg P, Chesney M, Berman B. Mindfulness intervention for child abuse survivors. Journal of Clinical Psychology. 2010;66(1):17–33. doi: 10.1002/jclp.20624. [DOI] [PubMed] [Google Scholar]
- Lande RG, Williams LB, Francis JL, Gragnani C, Morin ML. Efficacy of biofeedback for post-traumatic stress disorder. Complementary Therapies in Medicine. 2010;18(6):256–259. doi: 10.1016/j.ctim.2010.08.004. [DOI] [PubMed] [Google Scholar]
- Mitani S, Fujita M, Sakamoto S, Shirakawa T. Effect of autogenic training on cardiac autonomic nervous activity in high-risk fire service workers for posttraumatic stress disorder. Journal of Psychosomatic Research. 2006;60(5):439–444. doi: 10.1016/j.jpsychores.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Muller J, Karl A, Denke C, Mathier F, Dittmann J, Rohleder N, Knaevelsrud C. Biofeedback for pain management in traumatised refugees. [Research Support, Non-U.S. Gov't] Cognitive Behaviour Therapy. 2009;38(3):184–190. doi: 10.1080/16506070902815024. [DOI] [PubMed] [Google Scholar]
- Osuch EA, Benson BE, Luckenbaugh DA, Geraci M, Post RM, McCann U. Repetitive TMS combined with exposure therapy for PTSD: A preliminary study. Journal of Anxiety Disorders. 2009;23(1):54–59. doi: 10.1016/j.janxdis.2008.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price C. Body-oriented therapy in recovery from child sexual abuse: an efficacy study. Alternative Therapies in Health & Medicine. 2005;11(5):46–57. [PMC free article] [PubMed] [Google Scholar]
- Price C. Body-oriented therapy in sexual abuse recovery: A pilot-test comparison. Journal of Bodywork and Movement Therapies. 2006;10:58–64. [Google Scholar]
- Rosenthal JZ, Grosswald S, Ross R, Rosenthal N. Effects of transcendental meditation in veterans of Operation Enduring Freedom and Operation Iraqi Freedom with posttraumatic stress disorder: a pilot study. Military Medicine. 2011;176(6):626–630. doi: 10.7205/milmed-d-10-00254. [DOI] [PubMed] [Google Scholar]
- Tan G, Dao TK, Farmer L, Sutherland RJ, Gevirtz R. Heart rate variability (HRV) and posttraumatic stress disorder (PTSD): a pilot study. Applied Psychophysiology & Biofeedback. 2011;36(1):27–35. doi: 10.1007/s10484-010-9141-y. [DOI] [PubMed] [Google Scholar]
- Taylor S, Thordarson DS, Maxfield L, Fedoroff IC, Lovell K, Ogrodniczuk J. Comparative efficacy, speed, and adverse effects of three PTSD treatments: exposure therapy, EMDR, and relaxation training. Journal of Consulting & Clinical Psychology. 2003;71(2):330–338. doi: 10.1037/0022-006x.71.2.330. [DOI] [PubMed] [Google Scholar]
- Watts BV, Landon B, Groft A, Young-Xu Y. A sham controlled study of repetitive transcranial magnetic stimulation for posttraumatic stress disorder. Brain Stimulation. 2012;5(1):38–43. doi: 10.1016/j.brs.2011.02.002. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Feng B, Xie JP, Xu FZ, Chen J. Clinical study on treatment of the earthquake-caused post-traumatic stress disorder by cognitive-behavior therapy and acupoint stimulation. Journal of Traditional Chinese Medicine. 2011;31(1):60–63. doi: 10.1016/s0254-6272(11)60014-9. [DOI] [PubMed] [Google Scholar]
- Zucker TL, Samuelson KW, Muench F, Greenberg MA, Gevirtz RN. The effects of respiratory sinus arrhythmia biofeedback on heart rate variability and posttraumatic stress disorder symptoms: a pilot study. Applied Psychophysiology & Biofeedback. 2009;34(2):135–143. doi: 10.1007/s10484-009-9085-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


