Abstract
Purpose
The Tisseel/Tissucol for mesh fixation in Lichtenstein hernia repair (TIMELI) study showed that mesh fixation with human fibrin sealant during inguinal hernia repair significantly reduced moderate–severe complications of pain 12 months post-operatively compared with sutures. Further analyses may assist surgeons by investigating predictors of post-surgical complications and identifying patients that may benefit from Tisseel/Tissucol intervention.
Methods
Univariate and multivariate analyses identified risk factors for combined pain, numbness and groin discomfort (PND) visual analogue scale (VAS) score 12 months post-operatively. Variables tested were: fixation method, age, employment status, physical activity, nerve handling, PND VAS score at pre-operative visit and 1 week post-operatively. The effect of fixation technique on separate PND outcomes 12 months post-surgery was also assessed. Analyses included the intention-to-treat (ITT) population and a subpopulation with pre-operative PND VAS > 30 mm.
Results
316 patients were included in the ITT, with 130 patients in the subpopulation with pre-operative PND VAS > 30. Multivariate analysis identified mesh fixation with sutures, worsening pre-operative PND and worsening PND 1 week post-surgery as significant predictors of 12-month PND in the ITT population; mesh fixation with sutures was a significant predictor of 12-month PND in the pre-operative PND VAS > 30 subpopulation (p < 0.05). Mesh fixation with Tisseel/Tissucol resulted in significantly less numbness and a lower intensity of groin discomfort compared with sutures at 12 months; there was no difference in pain between the treatment groups.
Conclusions
Pre-operative discomfort may be an important predictor of post-operative pain, numbness and discomfort. Tisseel/Tissucol may improve long-term morbidity over conventional sutures in these patients.
Keywords: Inguinal hernia repair, Mesh fixation, Lichtenstein technique, Chronic pain, Chronic numbness, Chronic groin discomfort
Introduction
In general surgery, inguinal hernia repair is one of the most commonly performed procedures. It is estimated that over 20 million groin hernia repairs are performed each year [1], with over 800,000 inguinal hernia repair procedures performed in the United States alone [2]. This places a significant burden on global healthcare costs and patient quality of life. Over the past decade, developments in modern surgical techniques have greatly reduced the rate of recurrence following inguinal hernia repair. As such, the reduction of acute and chronic post-operative pain has become increasingly important as a key clinical target [3].
Post-operative pain is known to vary depending on the type of surgical procedure or technique employed, with current research focused on open versus laparoscopic hernia repair. The Lichtenstein technique is an open, tension-free mesh-onlay procedure that has been shown to result in low recurrence and complication rates [4]. As such, it is currently recommended by the European Hernia Society for the open treatment of uncomplicated primary unilateral hernias [5], and was the chosen method for the recent Tisseel/Tissucol for mesh fixation in Lichtenstein hernia repair (TIMELI) study [6]. The aim of the TIMELI study was to determine whether mesh fixation using standard sutures, or using a human fibrin sealant (Tisseel®/Tissucol®, Baxter Healthcare, Deerfield, IL, USA), impacted on chronic moderate–severe complications of pain [a composite of pain, numbness and groin discomfort (PND)] [6]. Tisseel/Tissucol is a biodegradable and biocompatible combination of highly concentrated human-derived fibrinogen and thrombin, which is activated by calcium chloride to polymerize into a fibrin fibre matrix. Primary results from this study have been published, and showed Tisseel/Tissucol to significantly reduce the risk of chronic moderate–severe PND 12 months post-operatively [7].
Here we describe the results of post hoc secondary analyses from the TIMELI study. The main objectives of these analyses were to investigate factors that could potentially influence 12-month PND using univariate and multivariate analyses and to identify subsets of patients that may benefit specifically from Tisseel/Tissucol use compared with conventional sutures. These data may assist surgeons in predicting which patients may experience post-surgical complications, provide information on how best to treat them, and aid management of patient expectations.
Methods
Study design
The TIMELI study was a randomised, blinded, controlled, multicentre European study (NCT00306839), whose rationale and methodology have been described in detail previously [6]. Briefly, males aged 18–80 years diagnosed with an uncomplicated unilateral primary inguinal hernia or an uncomplicated bilateral hernia, who were eligible for surgical repair using the Lichtenstein technique, were enrolled into the study. Full exclusion criteria have been previously reported, which included among others a body mass index ≥35 kg/m2, a large hernia (L3/M3 EHS Groin Hernia Classification) [8], and concomitant abdominal surgery [6].
Surgical procedure
On enrolment, patients were randomised to suture or Tisseel/Tissucol mesh fixation 24 h prior to surgery. Inguinal hernia repair was performed using the Lichtenstein technique [9] by a surgeon experienced in the procedure. Precise details of the surgical methodology have been previously reported [6]. In summary, local/regional/general anaesthesia was used depending on the study centre and nerves preserved. If nerve resection did occur, where possible it was subsequently cut, ligated and/or implanted into the muscles according to Lichtenstein and at the discretion of the attending surgeon [9, 10]. The heavyweight polypropylene flat mesh was tailored for the patient and then fixed by sutures as described by classical Lichtenstein technique, [9] or by application of 2 ml of fibrin sealant (where 2 ml of thrombin are added making 4 ml of the final volume) with 0.5 ml used dropwise on the pubic tubercle and pressing the mesh onto this for 2 min, after which the remainder of the sealant (1.5 ml) was sprayed over the entire surface of the mesh as a thin layer. The skin and external fascia were then closed according to standard surgical procedure [6]. Patients received standard analgesia treatment in the immediate post-operative period.
Outcome measures
Assessments for pain, numbness and groin discomfort were performed <14 days prior to the procedure (Visit 1) and post-operatively at hospital discharge (Visit 2), and at 1 week, 1, 6 and 12 months post-operatively (Visits 3–6). Measures of each PND were quantified on a 100-mm visual analogue scale (VAS), where 0 mm reflects no experience of outcome and 100 mm the worst conceivable experience (combined PND thus ranged from 0 to 300 mm as the addition of the three outcome). VAS scores for study Visits 1 and 3–6 were evaluated by patient’s self-assessment and ascertained by a blinded evaluator, who first explained the scale to the patients verbally. Patients were asked to record the worst pain experienced since the last study visit [6]. VAS scores were categorised as none = 0, mild = 1–30, moderate = 31–60, severe = 61–100 mm.
Secondary analyses
The post hoc analyses presented here were undertaken to identify factors that affect combined PND VAS scores at 12 months after surgery, through univariate and multivariate analysis. In addition, comparisons of separate PND VAS scores between the two mesh fixation groups (Tisseel/Tissucol versus sutures) were also undertaken. Secondary analyses were performed on the intention-to-treat (ITT) population, defined as all randomised subjects who underwent the surgical procedure. As high levels of pain prior to surgery have been found to significantly predict chronic post-operative pain [11, 12], it was decided to also perform the analyses in this clinically important subpopulation, defined as those patients in the ITT experiencing moderate/severe pre-operative PND (at least one VAS >30 mm, e.g., patients with VAS pain >30 or VAS numbness >30 or VAS groin discomfort >30 at pre-operative visit).
Statistical analyses
All statistical analyses were performed using SAS software (Statistical Analysis System, version 8.02) on Pentium (compatible IBM).
VAS scores are presented as mean values ± standard deviation (SD) and severity categories (none = 0, mild = 1–30, moderate = 31–60, severe = 61–100 mm) as percentages of each individual subpopulation. To identify predictors of combined PND at 12 months (continuous variable), Pearson correlations (for continuous variables), Mann–Whitney–Wilcoxon tests and Kruskal–Wallis tests (for categorical variables) were used in the univariate analyses, and non-parametric mixed covariance analyses with centre as random factor were used for the multivariate analyses. To assess the effect of mesh fixation on separate PND outcomes at 12 months, non-parametric mixed covariance analysis (when PND was considered as continuous variable) and mixed logistic models (when PND was considered as binary variable; VAS = 0 versus VAS > 0) with centre as random factor were used.
Variables included in the univariate analyses were chosen based on their potential to influence the course of post-operative PND. These were: fixation method (Tisseel/Tissucol versus sutures); age (≤50 versus >50 years); employment status [blue and white collar, self-employed, other (unemployed/student/retired)]; physical activity (sportive versus non-sportive); combined VAS score at pre-operative visit (continuous variable); combined VAS score 1 week post-operatively (continuous variable); and nerve handling (3 nerves, 2 nerves, 1 nerve, or 0 nerves seen and preserved). Age has been considered in two classes instead of a continuous variable. For employment status, this variable has been considered as reflecting the psychological state of mind of the patient. Consequently, it has been categorised in three categories: blue and white collar, where blue collar refers to tradesmen (plumbers, electricians etc.) and white collar refers to office workers, business people etc.; self-employed and others. Physical activity was considered in two classes based on engagement in professional or leisure sporting activities (sportive) or not (non-sportive) For nerve handling, patients were grouped according to the number of nerves seen and preserved during surgery; it was assumed that if nerves were not seen, they were not damaged.
Based on the univariate analyses, variables were selected for the multivariate analysis model if p < 0.2. As patients from the same centre are not independent, multivariate analyses were performed using mixed models with centre integrated as random factor. In this way, centre effect was taken into consideration in the model and estimations of fixed factors are more reliable. Variables found to be significant at the 0.05 level (p < 0.05) in initial multivariate models were subsequently retained in the final multivariate model using a backward selection procedure. In order to maintain the statistical validity of the multivariate analyses, any variables found to be correlated to another variable being investigated were not included in the same model.
Results
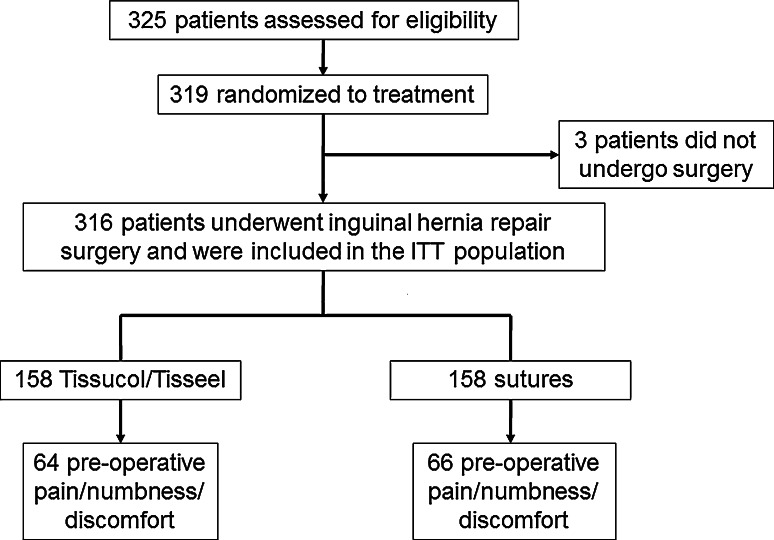
The patient disposition for the TIMELI study ITT population and the subgroup of patients experiencing pre-operative PND are summarised in Fig. 1. Overall, 316 patients were randomised to treatment and included in the ITT population (158 in each treatment group), and 130 patients experienced pre-operative PND (at least one VAS >30 mm; 64 in the Tisseel/Tissucol group, 66 in the sutures group).
Fig. 1.
Patient disposition for the TIMELI trial: ITT population and the subgroup of patients experiencing pre-operative PND
Baseline characteristics for both the ITT population and the pre-operative PND subgroup are summarised in Table 1; no significant differences between Tisseel/Tissucol and sutures groups were identified.
Table 1.
Baseline characteristics (n, % unless otherwise stated): ITT population and patients experiencing pre-operative PND
| ITT population | Patients experiencing pre-operative PND (at least one VAS >30 mm) | |||
|---|---|---|---|---|
| Tisseel/Tissucol N = 158 | Sutures N = 158 | Tisseel/Tissucol N = 64 | Sutures N = 66 | |
| Age, median (range), years | 58 (19–84) | 59 (21–80) | 58 (19–84) | 55 (21–77) |
| Employment status | ||||
| Blue collar | 37 (23.7) | 39 (25.0) | 18 (28.6) | 23 (34.8) |
| White collar | 49 (31.4) | 45 (28.8) | 17 (27.0) | 16 (24.2) |
| Self-employed | 14 (9.0) | 14 (9.0) | 4 (6.3) | 3 (4.5) |
| Not employed | 3 (1.9) | 3 (1.9) | 3 (4.8) | 0 (0.0) |
| Retired | 51 (32.7) | 55 (35.3) | 21 (33.3) | 24 (36.4) |
| If employed | ||||
| Full time | 96 (96.0) | 95 (96.9 | 36 (92.3) | 40 (95.2) |
| Part time | 4 (4.0) | 3 (3.1) | 3 (7.7) | 2 (4.8) |
| BMI, mean (SD) | 25.5 (2.9) | 25.5 (2.6) | 25.3 (3.0) | 25.5 (2.6) |
| General health | ||||
| ASA I/II n (%) | 148 (94.2) | 153 (96.9) | 59 (92.2) | 62 (93.9) |
| ASA III n (%) | 9 (5.7) | 5 (3.2) | 5 (7.8) | 4 (6.1) |
| Paina | ||||
| None (0) | 56 (35.4) | 59 (37.3) | 12 (18.8) | 11 (16.7) |
| Mild (1–30) | 65 (41.1) | 59 (37.3) | 15 (23.4) | 15 (22.7) |
| Moderate (31–60) | 28 (17.7) | 29 (18.4) | 28 (43.8) | 29 (43.9) |
| Severe (61–100) | 9 (5.7) | 11 (7.0) | 9 (14.4) | 11 (16.7) |
| Numbnessa | ||||
| None (0) | 113 (71.5) | 110 (69.6) | 46 (71.9) | 45 (68.2) |
| Mild (1–30) | 33 (20.9) | 31 (19.6) | 6 (9.4) | 4 (6.1) |
| Moderate (31–60) | 6 (3.8) | 14 (8.9) | 6 (9.4) | 14 (21.2) |
| Severe (61–100) | 6 (3.8) | 3 (1.9) | 6 (9.4) | 3 (4.5) |
| Groin discomforta | ||||
| None (0) | 51 (32.3) | 47 (29.7) | 7 (10.9) | 6 (9.1) |
| Mild (1–30) | 60 (38.0) | 63 (40.0) | 10 (15.6) | 12 (18.2) |
| Moderate (31–60) | 38 (24.1) | 38 (24.1) | 38 (59.4) | 38 (57.6) |
| Severe (61–100) | 9 (5.7) | 10 (6.3) | 9 (14.1) | 10 (15.2) |
ASA American Society of Anesthesiology categorisation, BMI body mass index, ITT intention-to-treat, PND pain, numbness and groin discomfort, SD standard deviation
aAs assessed by the visual analogue scale (VAS), ranging from 0 mm (none) to 100 mm (worst conceivable)
Predictors of combined PND at 12 months in the ITT population
Univariate correlation analyses showed that fixation with sutures (compared with Tisseel/Tissucol), worsening pre-operative PND and worsening PND at 1 week post-operatively were significant predictors of PND at 12 months (n = 299; p = 0.008; r = 0.23, p < 0.0001; r = 0.31, p < 0.0001, respectively). In addition, the following factors were significant at the 0.2 level and were selected for the multivariate analysis: decreasing age (≤50 versus >50 years) and employment status [stratified by three classes: blue- and white-collar employment, self-employed, other (unemployed, student, retired)] (Table 2).
Table 2.
Univariate analyses assessing the impact of demographic, clinical and surgical variables on PND (combined VAS) at 12 months post-operatively: ITT population and patients experiencing pre-operative PND (at least one VAS >30 mm)
| n | ITT population | p value | n | Pre-operative PND (at least one VAS >30 mm) | p value | |
|---|---|---|---|---|---|---|
| Fixation methoda | ||||||
| Tisseel/Tissucol | ||||||
| Mean ± SD | 149 | 15.0 ± 27.2 | 60 | 19.0 ± 29.4 | ||
| Median (range) | 0.0 (0–155) | 10.0 (0–150) | ||||
| Interquartile range | 0–20 | 0.008* | 0–25 | 0.003* | ||
| Sutures | ||||||
| Mean ± SD | 150 | 23.5 ± 34.1 | 62 | 38.9 ± 44.3 | ||
| Median (range) | 10.0 (0–230) | 25.0 (0–230) | ||||
| Interquartile range | 0–35 | 0–50 | ||||
| Agea | ||||||
| ≤50 years | ||||||
| Mean ± SD | 92 | 24.8 ± 38.5 | 44 | 34.0 ± 44.6 | ||
| Median (range) | 10.0 (0–230) | 25.0 (0–230) | ||||
| Interquartile range | 0–32 | 0.053* | 0–50 | 0.313 | ||
| >50 years | ||||||
| Mean ± SD | 207 | 16.8 ± 26.8 | 78 | 26.3 ± 35.3 | ||
| Median (range) | 0 (0–150) | 11.0 (0–150) | ||||
| Interquartile range | 0–25 | 0–40 | ||||
| Employment statusb | ||||||
| Blue and white collar | ||||||
| Mean ± SD | 161 | 19.4 ± 30.3 | 70 | 26.9 ± 35.3 | ||
| Median (range) | 10 (0–155) | 10.0 (0–140) | ||||
| Interquartile range | 0–25 | 0.091* | 0–40 | 0.697 | ||
| Self-employed | ||||||
| Mean ± SD | 28 | 14.9 ± 44.1 | 7 | 48.1 ± 82.8 | ||
| Median (range) | 0.0 (0–230) | 12.0 (0–230) | ||||
| Interquartile range | 0–11 | 0–60 | ||||
| Other (unemployed/student/retired) | ||||||
| Mean ± SD | 107 | 20.8 ± 28.5 | 44 | 30.2 ± 34.7 | ||
| Median (range) | 10.0 (0–150) | 20.0 (0–150) | ||||
| Interquartile range | 0–25 | 0–50 | ||||
| Physical activitya | ||||||
| Sportive | ||||||
| Mean ± SD | 149 | 20.2 ± 31.8 | 67 | 25.7 ± 36.4 | ||
| Median (range) | 10.0 (0–230) | 19.0 (0–230) | ||||
| Interquartile range | 0–25 | 0.229 | 0–35 | 0.522 | ||
| Non-sportive | ||||||
| Mean ± SD | 150 | 18.3 ± 30.4 | 55 | 33.2 ± 41.7 | ||
| Median (range) | 0.0 (0–150) | 15.0 (0–150) | ||||
| Interquartile range | 0–25 | 0–50 | ||||
| Combined VAS score at pre-operative visit**c | 299 | – | <0.0001* | 122 | – | 0.593 |
| Combined VAS score 1 week post-operatively**c | 299 | – | <0.0001* | 122 | – | 0.007* |
| Nerve handling (seen and preserved)b | ||||||
| 3 nerves | ||||||
| Mean ± SD | 147 | 18.9 ± 26.7 | 69 | 24.8 ± 32.2 | ||
| Median (range) | 10.0 (0–150) | 15.0 (0–150) | ||||
| Interquartile range | 0–25 | 0–34 | ||||
| 2 nerves | ||||||
| Mean ± SD | 64 | 20.9 ± 33.8 | 24 | 32.0 ± 37.1 | ||
| Median (range) | 0.0 (0–155) | 17.5 (0–121) | ||||
| Interquartile range | 0–30 | 0.248 | 0–45 | 0.238 | ||
| 1 nerve | ||||||
| Mean ± SD | 54 | 21.4 ± 40.8 | 17 | 44.4 ± 60.9 | ||
| Median (range) | 5.0 (0–230) | 19.0 (0–230) | ||||
| Interquartile range | 0–20 | 10–60 | ||||
| 0 nerves | ||||||
| Mean ± SD | 27 | 9.3 ± 16.3 | 12.9 ± 22.2 | |||
| Median (range) | 0.0 (0–55) | 7 | 0.0 (0–50) | |||
| Interquartile range | 0–15 | 0–40 | ||||
ITT intention-to-treat, PND pain, numbness and groin discomfort, SD standard deviation, VAS visual analogue scale
p values were calculated using a Mann–Whitney–Wilcoxon tests, b Kruskal–Wallis tests, and c Pearson correlations. * Significant at the 0.20 level, ** Continuous variable (0–300 mm)
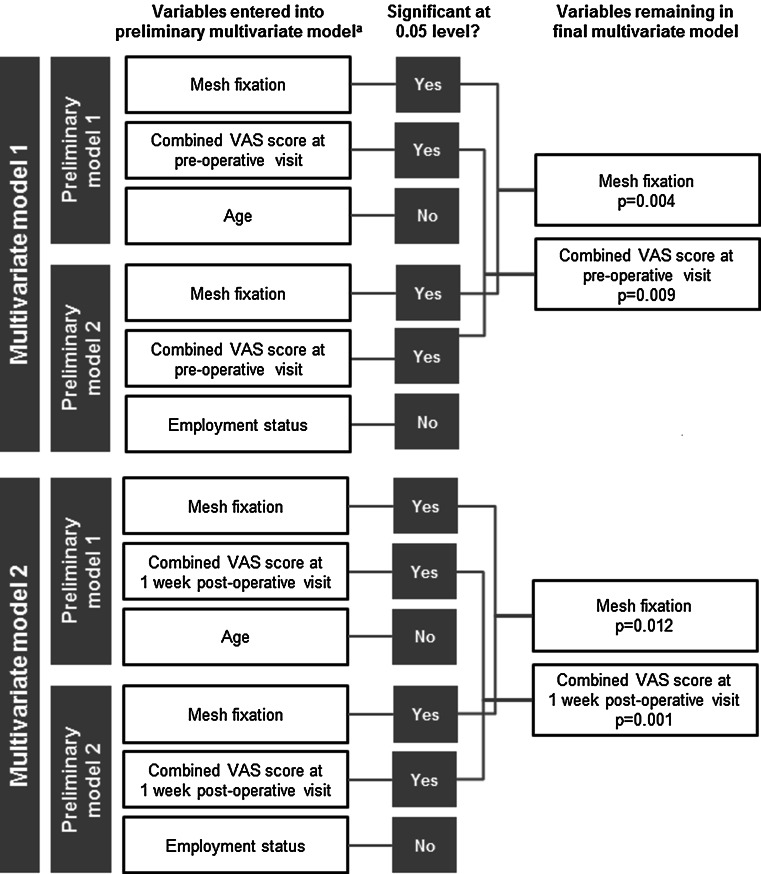
Results of the multivariate analyses using non-parametric covariance modelling are summarised in Fig. 2. Five variables were found to be significant at the 0.2 level in the univariate analyses (mesh fixation, worsening pre-operative PND, worsening PND 1 week post-operatively, age and employment status). Among them, several were correlated to each other, precluding their use in the same multivariate model; i.e., age and employment status are not independent variables, and combined VAS score at the pre-operative visit and combined VAS score at the 1-week post-operative visit are also not independent of each other. Therefore, two models of multivariate analysis were tested in order to separate these related factors.
Fig. 2.
Variables significantly associated with 12-month PND score as determined by multivariate analysis: ITT population p values calculated using mixed non-parametric covariance analysis performed on rank data with study centre as random factor. aVariables identified as significant (p < 0.2) in the univariate analyses were included in the multivariate analyses. These were: mesh fixation (Tisseel/Tissucol versus sutures), age, employment status, pre-operative PND score, and 1-week post-operative PND score. Two multivariate models were tested to separate correlated variables. For Models 1 and 2, two preliminary models with three uncorrelated variables were tested. After the backward selection procedure, only mesh fixation, Combined VAS score at pre-operative visit and Combined VAS score at 1-week post-operative visit remained significant at the 0.05 level
For Model 1, two preliminary models were tested, each with three variables: mesh fixation, combined VAS score at pre-operative visit and either age or employment status. For Model 2 the two preliminary models included the variables: mesh fixation, combined VAS score at 1-week post-operative visit and either age or employment status. After a backward selection procedure, final modelling analyses showed that the factors significantly associated with 12-month PND were mesh fixation with sutures (compared with Tisseel/Tissucol), worsening pre-operative PND and worsening PND at 1 week after surgery (Fig. 2).
Effect of mesh fixation on separate PND outcomes at 12 months in the ITT population
Comparisons of separate PND mean VAS scores at 12 months showed that the intensity of numbness and groin discomfort was lower in the Tisseel/Tissucol mesh fixation group compared with sutures (p = 0.019 and 0.049, respectively, Table 3). No significant difference was found in pain as measured by VAS score (p = 0.113). The median VAS score was 0 for each separate outcome in both treatment groups.
Table 3.
Visual analogue scale assessments (mm) of pain, numbness and groin discomfort at the 12-month post-operative visit: ITT population and patients with pre-operative PND (at least one VAS >30 mm)
| ITT population | Patients experiencing pre-operative PND (at least one VAS >30 mm) | |||||
|---|---|---|---|---|---|---|
| Tisseel/Tissucol N = 149 | Sutures N = 150 | p value | Tisseel/Tissucol N = 60 | Sutures N = 62 | p value | |
| Pain | ||||||
| Mean ± SD | 3.9 ± 11.5 | 5.9 ± 14.8 | 0.113 | 6.6 ± 14.6 | 10.7 ± 19.3 | 0.195 |
| Median (range) | 0 (0–76) | 0 (0–90) | 0 (0–76) | 0 (0–90) | ||
| Interquartile range | 0–0 | 0–0 | 0–5 | 0–15 | ||
| Numbness | ||||||
| Mean ± SD | 4.1 ± 10.6 | 7.4 ± 14.6 | 0.019* | 3.4 ± 8.6 | 11.0 ± 19.7 | 0.008* |
| Median (range) | 0 (0–91) | 0 (0–100) | 0 (0–50) | 0 (0–100) | ||
| Interquartile range | 0–0 | 0–10 | 0–0 | 0–19 | ||
| Groin discomfort | ||||||
| Mean ± SD | 7.1 ± 14.6 | 10.2 ± 16.8 | 0.049* | 9.0 ± 14.6 | 17.3 ± 21.5 | 0.018* |
| Median (range) | 0 (0–75) | 0 (0–80) | 0 (0–50) | 7.5 (0–80) | ||
| Interquartile range | 0–10 | 0–20 | 0–18 | 0–25 | ||
ITT intention-to-treat, PND pain, numbness and pain discomfort, SD standard deviation, VAS visual analogue scale
* p < 0.05 for Tisseel versus suture subgroup, non-parametric mixed covariance analysis
The effect of mesh fixation on the presence (VAS > 0) or absence (VAS = 0) of separate PND outcomes at 12 months post-operatively was also analysed. Mixed logistic model analysis showed that fixation with sutures led to a higher incidence of numbness at 12 months post-operatively (p = 0.033), but not of pain or groin discomfort (p = 0.110 and 0.108) (Table 4).
Table 4.
Presence of pain, numbness and groin discomfort at the 12-month post-operative visit: ITT population and patients with pre-operative PND (at least one VAS >30 mm)
| ITT population | Patients experiencing pre-operative PND (at least one VAS >30 mm) | |||||
|---|---|---|---|---|---|---|
| Tisseel/Tissucol N = 149 | Sutures N = 150 | p value | Tisseel/Tissucol N = 60 | Sutures N = 62 | p value | |
| Pain, n (%) | ||||||
| VAS = 0 (no pain) | 125 (83.9) | 115 (76.7) | 0.110 | 45 (75.0) | 40 (64.5) | 0.220 |
| VAS > 0 (some pain) | 24 (16.1) | 35 (23.3) | 15 (25.0) | 22 (35.5) | ||
| Numbness, n (%) | ||||||
| VAS = 0 (no numbness) | 115 (77.2) | 99 (66.0) | 0.033* | 48 (80.0) | 37 (59.7) | 0.021* |
| VAS > 0 (some numbness) | 34 (22.8) | 51 (34.0) | 12 (20.0) | 25 (40.3) | ||
| Groin discomfort, n (%) | ||||||
| VAS = 0 (no discomfort) | 106 (71.1) | 95 (63.3) | 0.108 | 38 (63.3) | 31 (50.0) | 0.101 |
| VAS > 0 (some discomfort) | 43 (28.9) | 55 (36.7) | 22 (36.7) | 31 (50.0) | ||
ITT intention-to-treat, PND pain, numbness and pain discomfort, VAS visual analogue scale
* p < 0.05 for Tisseel versus suture subgroup, mixed logistic model analysis
Predictors of combined PND at 12 months in patients experiencing pre-operative PND (at least one VAS >30 mm)
In this subgroup, univariate analyses identified mesh fixation with sutures (compared with Tisseel/Tissucol; n = 122, p = 0.003) and worsening PND 1 week post-operatively (n = 122, r = 0.24, p = 0.007) as significantly associated with a worsening 12-month PND (Table 2). When these factors were included in the multivariate model, only mesh fixation (p = 0.0014) remained significant at 0.05 level.
Effect of mesh fixation on separate PND outcomes at 12 months in patients experiencing pre-operative PND (at least one VAS >30 mm)
When directly comparing separate PND mean VAS scores at 12 months, mesh fixation with Tisseel/Tissucol resulted in a lower intensity of numbness or groin discomfort compared with sutures (p = 0.008 and 0.018, respectively, Table 3), but no difference in pain was found (p = 0.195). The median VAS score for pain and numbness, respectively, was 0 in both treatment groups; for groin discomfort the median VAS score was 0 in the Tisseel/Tissucol group and 7.5 in the sutures group.
The presence (VAS > 0) or absence (VAS = 0) of separate PND outcomes at 2 months was also compared between the two mesh fixation groups. Mixed logistic model analysis showed fixation with sutures to be a significant predictor of numbness at 12 months post-operatively (p = 0.021), but was not associated with an increased incidence of pain or groin discomfort when compared with mesh fixation with Tisseel/Tissucol at this time point (p = 0.220 and 0.101) (Table 4).
Discussion
This was a comprehensive secondary analysis of data from the TIMELI study to investigate factors that could influence the combined outcome of pain, numbness and groin discomfort 12 months after surgery, and to identify any subsets of patients that could gain particular benefit from Tisseel/Tissucol use during Lichtenstein inguinal hernia repair.
Through multivariate modelling, our study identified three factors that increased the risk of experiencing chronic PND in the overall population; these were receiving sutures rather than Tisseel/Tissucol during surgery, experiencing worsening pre-operative PND and experiencing worsening PND 1 week after surgery. Univariate analyses also identified younger age (≤50 years) and employment status as significant at the 0.2 level. Nerve handling during surgery and physical activity were not found to have a significant effect on the outcome of PND 12 months post-surgery.
Several risk factors for persistent post-operative pain/discomfort have been identified in the literature, including both surgery-related factors such as surgical technique and post-operative complications and patient-specific factors such as pre-operative pain and psychological vulnerability [12]. The risk factors identified in our secondary analyses are generally in agreement with other reports predicting risk factors for post-surgical chronic pain, although direct comparisons cannot be made due to our use of the novel PND outcome [7]. A retrospective, questionnaire-based study including 2,456 patients from the Swedish Hernia Registry investigated factors associated with residual pain 2–3 years after primary inguinal and femoral hernia repair [11]. They found that age below median (59 years), a high level of pain before the operation, and post-operative complications significantly and independently predicted long-term pain in multivariate logistic analysis when “worst pain last week” was used as outcome variable. Notably, and unlike our current analyses, this study did not find any specific surgical technique to be associated with risk of residual pain. Furthermore, a small retrospective study of patients who were referred to a chronic pain clinic following inguinal hernia repair demonstrated a link between pre-operative pain and the development of severe chronic pain after hernia repair; 14/24 patients presented pre-operatively with severe pain compared with 3/24 sex- and age-matched pain-free controls (p < 0.005) [13].
Psychological risk factors such as lower pre-operative optimism and lower perceived control over pain have been associated with higher pain after inguinal hernia repair surgery [14]. Although psychological factors were not directly assessed in our study, employment status may be interpreted as an indirect marker of the psychological condition of a patient. As the primary TIMELI analysis reported that the incidence of moderate/severe PND 1 year after surgery was higher in retired patients than active patients [7], it is somewhat surprising that employment status was not found to significantly predict post-operative PND at 12 months in the current analysis (although it was identified in the univariate analysis).
The identification and preservation of inguinal nerves have been implicated as an important factor in persistent post-surgical pain, but there are conflicting views as to which nerve handling procedure best reduces this outcome. The general consensus seems to be that identification of all nerves during open inguinal hernia repairs can avoid iatrogenic injury. Alfieri et al. [15] showed that lack of identification of nerves and the division of nerves was significantly correlated with the presence of chronic pain in univariate analysis, and that lack of identification remained significant in the multivariate model. Furthermore, a study by Smeds et al. [16] also found that non-identification of nerves led to worse pain rates at 3 months post-surgery. Conversely, a recent paper by Bischoff et al. [17] found no differences in the risk of substantial pain-related functional impairment between patients where the iliohypogastric nerve, ilioinguinal nerve, genitofemoral nerve or all nerves were seen. Our analyses are more consistent with this observation and suggest that other factors may contribute to the risk of nerve damage and persistent pain [18].
In the subgroup of patients experiencing pre-operative PND, mesh fixation with sutures was found to significantly predict chronic PND; worsening PND 1 week after surgery was also identified as significant at the 0.2 level in the univariate analysis. These findings, together with the analyses conducted in the overall study population, suggest that patients experiencing pre-operative PND (at least one VAS >30 mm) appear more likely to benefit from mesh fixation using Tisseel/Tissucol.
The main endpoint in the TIMELI study was the composite outcome of pain, numbness and groin discomfort. This combined endpoint was chosen to allow a robust overall quantitative assessment of three overlapping, moderate–severe complications that occur at relatively low frequency, as discussed previously [7]. Although pain is generally regarded as the most disabling element of the composite endpoint, the outcomes of groin discomfort and numbness can also negatively affect quality of life, especially if these complications persist over long periods after hernia repair. When comparing the three complications separately in patients treated with Tisseel/Tissucol and those treated with sutures, differences in the presentation of these separate outcomes were observed 1 year after surgery. Fibrin sealant resulted in significantly less numbness 12 months after surgery in both analysis populations. Interestingly, the intensity of groin discomfort was higher in patients treated with sutures than with fibrin sealant, but the incidence of discomfort was similar between treatment groups in both the ITT population and in patients experiencing pre-operative PND. The higher mean intensity of groin discomfort in the sutures group could be explained by outliers skewing the data. However, in the subgroup of patients experiencing pre-operative PND, a higher median VAS score was observed that may indicate a true difference. Finally, no difference in pain was found between the groups both in the overall study population and the subpopulation experiencing pre-operative pain. These observations may warrant further investigation to explore the mechanisms behind these chronic complications of pain, and the possible benefits of mesh fixation with Tisseel/Tissucol and how they relate to quality of life.
These results provide strong evidence that mesh fixation using Tisseel/Tissucol should be the preferred technique, especially in patients experiencing pre-operative PND. Because of the large number of inguinal hernia repairs performed annually, and the substantial percentage of patients experiencing pre-operative PND (41.1 % in this study), using Tisseel/Tissucol instead of sutures in these patients could potentially reduce the global healthcare burden and improve patient quality of life.
Limitations of the TIMELI trial design and primary efficacy and safety analyses have been previously reported [7]. One of the main limitations of the secondary analyses presented here is the relatively small sample size of the subpopulation. Despite this limitation, significant differences were observed for many of the comparisons between treatment groups in the subpopulation of patients experiencing pre-operative PND. Finally, as the study population only included patients undergoing surgery for small/medium-sized hernias, the use of fibrin sealant for mesh fixation to repair larger L3 or M3 hernias requires investigation in further clinical studies.
Conclusion
The TIMELI study demonstrated that Tisseel/Tissucol is a well-tolerated and effective means of mesh fixation during the repair of small/medium inguinal hernias using the Lichtenstein technique. These secondary analyses show that pre-operative PND has a significant impact on predicting chronic moderate–severe PND. As such, the patients experiencing pre-operative PND may especially benefit from an atraumatic and non-tissue-penetrating mesh fixation technique using Tisseel/Tissucol, which may improve long-term morbidity over conventional suture fixation.
Acknowledgments
This investigator-driven study was sponsored and coordinated by Professor Giampiero Campanelli with funding from Baxter Healthcare. Assistance from MAPI Clinical Research Organization, for data management, analysis and development of the clinical study report, and Fishawack Communications with the production of the manuscript draft, was funded by Baxter Healthcare. All authors made critical revisions to the manuscript and approved the final version for publication.
Conflict of interest
AH declares grant support for this study, consultancy outside submitted work, fees for participation in review activities and no other conflict of interest. AK declares grant support for this study and no other conflict of interest. GC declares expert testimony and grants/grants pending outside submitted work, grant support for this study and no other conflict of interest. GCh declares grant support for this study and no other conflict of interest. MP declares grant support for this study and no other conflict of interest. JR declares expert testimony and grants/grants pending outside submitted work, payment for lectures including service on speakers’ bureaus, grant support for this study and no other conflict of interest. MBd declares conflict of interest directly related to the submitted work and outside the submitted work as a Baxter employee, holds stock/stock options with Baxter Healthcare and no other conflict of interest. MM declares board membership, consultancy, grants/grants pending payment for lectures including service on speakers’ bureaus and payment for development of educational presentations outside the submitted work, grant support for this study and no other conflict of interest.
References
- 1.Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet. 2003;362(9395):1561–1571. doi: 10.1016/S0140-6736(03)14746-0. [DOI] [PubMed] [Google Scholar]
- 2.Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83(5):1045–1051. doi: 10.1016/S0039-6109(03)00132-4. [DOI] [PubMed] [Google Scholar]
- 3.Aasvang E, Kehlet H. Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth. 2005;95(1):69–76. doi: 10.1093/bja/aei019. [DOI] [PubMed] [Google Scholar]
- 4.Amid PK, Lichtenstein IL. Long-term results and current status of the Lichtenstein open tension-free hernioplasty. Hernia. 1998;2:89–94. doi: 10.1007/BF01207492. [DOI] [Google Scholar]
- 5.Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13(4):343–403. doi: 10.1007/s10029-009-0529-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campanelli G, Champault G, Hidalgo Pascual M, Hoeferlin A, Kingsnorth A, Rosenberg J, Miserez M. Randomized, controlled, blinded trial of Tissucol/Tisseel for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: rationale and study design of the TIMELI trial. Hernia. 2008;12:159–165. doi: 10.1007/s10029-007-0315-3. [DOI] [PubMed] [Google Scholar]
- 7.Campanelli G, Pascual MH, Hoeferlin A, Rosenberg J, Champault G, Kingsnorth A, Miserez M. Randomized, controlled, blinded trial of Tisseel/Tissucol for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: results of the TIMELI trial. Ann Surg. 2012;255(4):650–657. doi: 10.1097/SLA.0b013e31824b32bf. [DOI] [PubMed] [Google Scholar]
- 8.Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, Hoeferlin A, Kingsnorth AN, Mandala V, Palot JP, Schumpelick V, Simmermacher RK, Stoppa R, Flament JB. The European hernia society groin hernia classification: simple and easy to remember. Hernia. 2007;11(2):113–116. doi: 10.1007/s10029-007-0198-3. [DOI] [PubMed] [Google Scholar]
- 9.Amid PK. Lichtenstein tension-free hernioplasty: its inception, evolution, and principles. Hernia. 2004;8(1):1–7. doi: 10.1007/s10029-003-0160-y. [DOI] [PubMed] [Google Scholar]
- 10.Amid PK. Causes, prevention, and surgical treatment of postherniorrhaphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia. 2004;8(4):343–349. doi: 10.1007/s10029-004-0247-0. [DOI] [PubMed] [Google Scholar]
- 11.Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U. Risk factors for long-term pain after hernia surgery. Ann Surg. 2006;244(2):212–219. doi: 10.1097/01.sla.0000218081.53940.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Association for the Study of Pain (IASP) (2011) Chronic pain after surgery or injury, vol XIX, iss no 1. Pain Clinical Updates
- 13.Dennis R, O’Riordan D. Risk factors for chronic pain after inguinal hernia repair. Ann R Coll Surg Engl. 2007;89(3):218–220. doi: 10.1308/003588407X178991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Powell R, Johnston M, Smith WC, King PM, Chambers WA, Krukowski Z, McKee L, Bruce J. Psychological risk factors for chronic post-surgical pain after inguinal hernia repair surgery: a prospective cohort study. Eur J Pain. 2012;16(4):600–610. doi: 10.1016/j.ejpain.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Alfieri S, Rotondi F, Di Giorgio A, Fumagalli U, Salzano A, Di Miceli D, Ridolfini MP, Sgagari A, Doglietto G. Influence of preservation versus division of ilioinguinal, iliohypogastric, and genital nerves during open mesh herniorrhaphy: prospective multicentric study of chronic pain. Ann Surg. 2006;243(4):553–558. doi: 10.1097/01.sla.0000208435.40970.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smeds S, Lofstrom L, Eriksson O. Influence of nerve identification and the resection of nerves ‘at risk’ on postoperative pain in open inguinal hernia repair. Hernia. 2010;14(3):265–270. doi: 10.1007/s10029-010-0632-9. [DOI] [PubMed] [Google Scholar]
- 17.Bischoff JM, Aasvang EK, Kehlet H, Werner MU. Does nerve identification during open inguinal herniorrhaphy reduce the risk of nerve damage and persistent pain? Hernia. 2012;16(5):573–577. doi: 10.1007/s10029-012-0946-x. [DOI] [PubMed] [Google Scholar]
- 18.Kehlet H, Bischoff JM, Aasvang EK, Werner MU. Intraoperative nerve identification and chronic postherniorrhaphy pain. Hernia. 2012;16(5):583. doi: 10.1007/s10029-012-0991-5. [DOI] [PubMed] [Google Scholar]