Abstract
Myelolipoma in posterior mediastinum is indeed rare. As a benign tumor, it consists of mature fat with scattered foci of haematopoietic elements resembling bone marrow. The computed tomography (CT) and magnetic resonance imaging (MRI) are effective methods to detect them, while the definite diagnosis still depends on pathological diagnosis. Up to now, there is no standard treatment for this disease. Surgery is thought to be the best choice in some literatures reports. In this paper, two patients with primary posterior mediastinal tumor are reported, both of whom were underwent Video-assisted thoracoscopic surgery (VATS). Postoperative pathological diagnosis was myelolipoma.
Keywords: Mediastinum, myelolipoma, extra-adrenal, video-assisted thoracic surgery (VATS)
Introduction
Myelolipoma was first described in 1905, and named ‘myelolipoma’ in 1929 (1). It is an unusual benign neoplasm composed of mature adipocytes and hematopoietic tissue (2). It is commonly found in adrenal gland. Myelolipomas can also occur in extra-adrenal location. The occurrence in extra-adrenal site is quite rare with an incidence of 0.08-0.2% at autopsy (3). Atypical sites of origin include the presacral region, retroperitoneum, liver, spleen, stomach, greater omentum, leptomeninges, and mediastinum, where myelolipoma is discovered accidentally (4-10). Until now only 28 cases of mediastinal myelolipoma (1-3) including our cases have been reported (11-32). Some of the patients were asymptomatic, while others suffered from a wide variety of symptoms, such as endocrine disorder, anemia, hypertension, splenomegaly, etc(20-32). Here we represent two cases of posterior mediastinal myelolipoma, whose clinical features and treatments after using minimally invasive thoracic surgery are discussed.
Case report
Case one
A 60-year-old woman presented to our department with a right lower posterior mediastinal mass which was incidentally revealed by chest computed tomography (CT) scan. Repeated coughing and expectoration for one month made her seek medical assistance. Her past medical history was significant for thalassemia and splenomegaly for 10 years. Enhanced CT scan revealed a partial enhanced mass located in the right lower posterior mediastinum. It was 3.7 cm in diameter beside the vertebral column (Figure 1). There was no evidence of bony erosion in nearby rib or vertebra, pleural effusion or surrounding tissue infiltration. Magnetic resonance imaging (MRI) demonstrated that the mass extended from the paravertebral region and moderately intensified signal showed in T1-weighted images (Figure 1). Complete blood cell count revealed her red blood cells of 3.65×1012/L, hemoglobin of 65 g/L, white blood cells of 3.54×109/L and platelets of 75×109/L. It was considered as a neurogenic tumor initially and video-assisted thoracic surgery (VATS) was performed for tumor resection. Grossly, the surgical specimen was approximately 3.7 cm × 3.5 cm × 3 cm as a round-shaped, well-encapsued, soft and purple mass (Figure 2). A microscopic examination revealed a predominant mature adipose and hematopoietic tissue with intermingled. Immunohistochemical stains showed positivity for CD3, CD15, CD20, CD68, CD138 and MPO antibodies (Figure 2). Cytokeratin, neuron specific enolase (NSE) and S100 antibodies were negative. Based on these findings, the myelolipoma was confirmed. The patient discharged in the third postoperative day and has remained disease free at 6-month follow-up.
Figure 1.
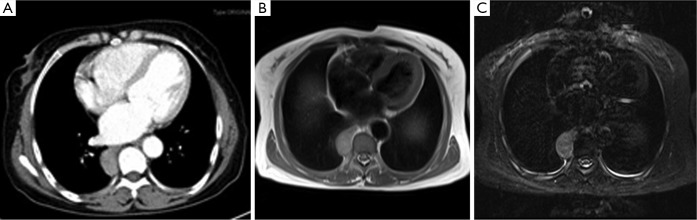
(A) An enhanced chest CT scan revealed a posterior mediastinal mass, which could be partially enhanced; (B,C) MRI demonstrated that the mass extended from the paravertebral region and was moderately intensified in T1-weighted image. CT, computed tomography; MRI, magnetic resonance imaging.
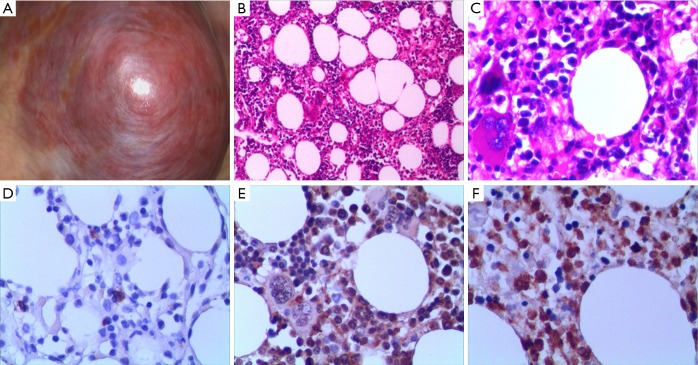
Figure 2.
Macro and microscopical findings of this myelolipoma: (A) a round-shaped, well-encapsued, soft and purple mass was identified in the posterior mediastinum; (B,C) a microscopic examination revealed predominant mature adipose tissue with hematopoietic tissue. There was a variable blend of adipocytes, myeloid, erythroid precursors and mature cells and even megakaryocytes and lymphoid cells resembling all together bone marrow. (Hematoxylin and eosin, B: ×200, C: ×400); (D-F) immunohistochemical stains showed positivity for CD20, CD68 and MPO antibodies (×400).
Case two
A 68-year-old man was admitted to our hospital and underwent chest CT scan because of palpitation, chest tightness, and shortness of breath. He was diagnosed with a right lower posterior mediastinal tumor. He had been through paroxysmal hypertension (the highest value was 200/100 mmHg) for 1 year and it hard to be controlled by medicine. The patient also had a history of type 2 diabetes for 15 years. Noradrenaline and epinephrine of blood and urine were relatively normal. We suspected that it was pheochromocytoma initially. CT revealed there was a mass shadow, which was 2.1 cm in diameter and located in the right lower posterior mediastinum. Its boundary was clear. Enhanced chest CT revealed the mass was partially enhanced (Figure 3). We considered it as a pheochromocytoma and VATS was performed for tumor resection. During the operation, a round-shaped, well-encapsuled purple mass was identified in posterior mediastinum in diameter of 1.5 cm. A pathological examination was the same as above-mentioned in the case one postoperatively (Figure 3). Thus mediastinal myelolipoma was confirmed, and no signs of malignancy were observed. Paroxysmal increased blood pressure was disappeared and the blood pressure was easy to control by medicine after surgery. After more than 6-month follow-up, he remained clinically well and a CT scan showed no residual tumor.
Figure 3.
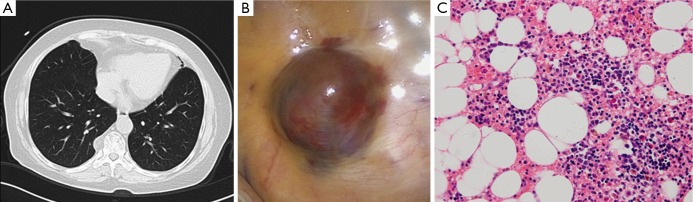
(A) Chest CT scan revealed one posterior mediastinal mass; (B) grossly, a round-shaped, well-encapsued purple mass was identified in the posterior mediastinum; (C) the pathology demonstrated predominant adipose tissue interspersed with mature bone marrow elements (Hematoxylin and eosin, ×200). CT, computed tomography.
Discussion
Myelolipoma is a familiar adrenal tumor with an incidence of 3-5%. However, extra-adrenal myelolipoma is rare with the morbidity of 0.08-0.2% (3). Since the first mediastinum myelolipoma reported in 1925, only 28 cases including our cases have been reported so far in English literatures (Table 1). Based on the literature reviews (Table 2), most of them arose from the posterior mediastinum (93%). There were 12 females and 16 males, at a mean age of 64 years. The mass diameter ranged from 1.5 to 25 cm with mean diameter of 5.9 cm. About 25% patients were asymptomatic, while 75% of them were symptomatic. Mainly complaints were cough, chest pain and dyspnea. Almost all the tumors were benign and non-invasive, so did our cases. The prognosis was well after tumor resection.
Table 1. Reported cases of mediastinal myelolipoma*.
| Main author | Age/sex | Tumor location | Size (cm) | Clinical feature | Treatment or management | Outcome |
|---|---|---|---|---|---|---|
| Saleeby, 1925 (1) | 81/F | Posterior mediastinum | 2.5 | / | Autopsy | Death |
| Foster, 1958 (11) | 80/M | Posterior mediastinum | 4 | / | Autopsy | Death |
| Litwer, 1960 (12) | 63/M | Posterior mediastinum | 9 | Chronic anemia | Autopsy | Death |
| 62/M | Posterior mediastinum | 7 | Chronic anemia | Thoracotomy | Not stated | |
| Krag, 1972 (13) | 71/F | Anterior mediastinum | 5 | / | Autopsy | Death |
| Schön, 1984 (14) | 50/M | Posterior mediastinum | Not stated | Anemia | Not stated | Not stated |
| Kim, 1984 (2) | 55/M | Posterior mediastinum | 7 | Coronary heart disease, hypertension | Thoracotomy | Not stated |
| Bastion, 1990 (15) | 72/F | Posterior mediastinum. | 10 | Hereditary spherocytosis | Thoracotomy | Not stated |
| Pulsoni, 1992 (16) | 60/M | Bilateral paravertebral area | Right: 4.0; | Hereditary spherocytosis | Thoracotomy | Not stated |
| left: 4.4 | ||||||
| De Montpréville, 1993 (17) | 65/M | Posterior mediastinum | 8 | Anemia | Thoracotomy | Not stated |
| Strimlan, 1993 (18) | 65/F | Posterior mediastinum | 5 | Chronic obstructive lung disease, chronic respiratory failure | Thoracotomy | No recurrence |
| Wyttenbach, 1994 (19) | 53/M | Anterior mediastinum | 8 | / | Thoracotomy | Not stated |
| Minamiya, 1997 (20) | 59/M | Posterior mediastinum | 6.5 | / | Thoracotomy | No recurrence |
| Koizumi, 1999 (21) | 55/M | Posterior mediastinum | 4 | Chest pain | VATS | No recurrence at 8 months |
| Fonte, 1999 (3) | 74/F | Posterior mediastinum | 2 | Back pain | Not stated | Not stated |
| Kawanami, 2000 (22) | 72/M | Bilateral paravertebral area | Not stated | Diabetes mellitus | CT-guided needle biopsy | Not stated |
| Gao, 2002 (23) | 59/ M | Posterior mediastinum | 2.5 | Hypertension, bronchitis | Thoracotomy | Not stated |
| Franiel, 2004 (24) | 65/ F | Bilateral posterior mediastinum | Left: 4.5; | Hypertension, chronic obstructive bronchitis | Thoracotomy | No recurrence at 12 months |
| right: 6.5 | ||||||
| Mohan, 2006 (25) | 46/M | Paratracheal mediastinum | 4.5 | Chest pain | Not stated | Not stated |
| Rossi, 2007 (26) | 73/F | Posterior mediastinum | 7 | / | Fine−needle aspiration, thoracotomy | Not stated |
| Vaziri, 2008 (27) | 56/M | Posterior mediastinum | 25 | Cough, dyspnea | Thoracotomy | No recurrence |
| Geng, 2013 (28) | 68/F | Bilateral posterior mediastinum | Right: 10.0; left: 9.0 | Back pain, cough, anemia, type 2 diabetes | Thoracotomy | No recurrence at 3 years |
| Ema, 2013 (29) | 68/M | Posterior mediastinum | 3 | / | VATS | No recurrence at 10 months |
| Fonda, 2013 (30) | 64/F | Posterior mediastinum | 3 | Type 2 diabetes, leukocytosis | VATS | No recurrence |
| Migliore, 2014 (31) | 56/F | Posterior mediastinum | 3.5 | Obese, chest pain | VATS | No recurrence at 11 months |
| Nakagawa, 2014 (32) | 79/M | Bilateral paravertebral area | Th-8:1.9; | Hypertension, nephrosclerosis, alcoholic liver hepatitis | VATS | No recurrence at |
| Th-10:4; | 4 years | |||||
| Th-9~10:7.5 | ||||||
| Our case | 60/F | Posterior mediastinum | 3.7 | Cough, thalassemia, splenomegaly | VATS | No recurrence |
| 68/F | Posterior mediastinum | 2.1 | palpitation, chest tightness, Hypertension, type 2 diabetes | VATS | No recurrence |
Table 2. The summary characteristics of reported patients with mediastinal myelolipoma*.
| Characteristics | Number |
|---|---|
| Age [mean] (year) | 46-81 [64] |
| Male:female | 16:12 |
| Symptoms [%]† | |
| Endocrine disorder | 6.0 [21] |
| Hematopoietic systemic abnormality | 9.0 [32] |
| CVD | 5.0 [18] |
| Symptoms of respiratory system | 10.0 [36] |
| Another | 6 |
| Tumor size [mean] (cm) | 1.5-25 [5.9] |
| Tumor location [%] | |
| Posterior mediastinum | 26.0 [93] |
| Anterior mediastinum | 2.0 [7] |
| Treatment | |
| VATS | 7 |
| Thoracotomy | 13 |
| Another | 8 |
*, values are number of patients unless specified otherwise; †, some patients had multiple symptoms; symptoms (%), number of patients with this symptom/total number of patients (%); tumor location (%), number of patients in this location/total number of patients (%); VATS, video-assisted thoracoscopic surgery; CVD, cardiovascular disease. Data from references (1-3) and (11-32).
The etiology of myelolipoma is unclear at present. About four hypotheses were proposed to explain the pathogenesis: (I) most theories indicated that the development and differentiation of either ectopic adrenal or hematopoietic stem cell received triggering stimulus by obesity, hypertension, chronic inflammation, carcinoma, previous trauma or endocrinic disorders, which had been studied in some reported cases. Maybe our second case supports this opinion (23,29,30); (II) some studies suggested that myelolipoma evolved from metaplastic change of embryonic primitive mesenchymal cells or embolism of bone marrow cells via the blood stream (14,17,29); (III) Chang et al. reported chromosomal translocations (3,21) (q25;P11) in one case of adrenal myelolipoma without other adrenal lesions (33). This clonal chromosome abnormality was commonly reported to be found in acute myelogenous leukemia and myelodysplastic syndrome. Therefore, this finding suggested that the myelolipoma might be a neoplastic phenomenon as the result of a particular chromosomal mutation. Some cases which were related to anemic condition such as hereditary spherocytosis and thalassemia, might support this hypothesis, so did our first case; (IV) another theory raised the hypothesis that majority of tumors were attached to vertebral bodies, haematopoietic tissue might project from vertebral microfractures to paravertebral space. Ectopic haematopoietic tissue may include stem cells that would be the origin of myelolipoma formation (30).
The mediastinum myelolipoma does not have any pathognomonic signs or symptoms. Thus it is difficult to definitively diagnose without histopathologic evaluations. Ultrasonography, CT scan and MRI have become more common as useful diagnostic tools and given some clues to the correct diagnosis (19,22,26). Although CT and MRI were effective in diagnosing myelolipoma, a confident conclusion was made difficultly before surgery. Some authors reported that Fine-needle aspiration under the guidance of CT scan or ultrasonography—combined with pathological examination—could be used to confirm the diagnosis (22,23,26). However, due to myelolipoma mostly occurring in posterior mediastinum (93%), especially for small mass, it is too difficult to biopsy accurately by Fine-needle aspiration from anterior chest wall, which can be associated with a risk simultaneously, such as hemorrhage, pneumothorax etc. The spine blocks the Fine-needle aspiration if entering from posterior chest wall. Therefore, Fine-needle aspiration with posterior mediastinum is not be advocated in our opinion.
At present, there is no standard treatment for mediastinal myelolipoma. According to treatment with mediastinal tumor (34), once a neoplasm is discovered in the mediastinum, especially unconfirmed behavior of the tumor, surgical resection may be an optimal treatment for patient. Particularly, VATS is a satisfactory choice (30-32). As we can see in Table 1, the tumor size ranges from 1.5 to 25 cm, which reveals that the myelolipoma has potential of continuous growth. With the tumor growing constantly, the patients have to receive thoracotomy eventually, which would cause more trauma and risks, particularly to seniors. Therefore, once the mediastinal myelolipoma is found, surgery is a preferred treatment for patient in our opinion, especially with VATS.
Conclusions
Myelolipoma in posterior mediastinum is a rare tumor, without exact etiology. It primarily occurs in seniors with concealed onset. The patients usually resort to medical attention for symptoms by chest discomfort, anemia, hypertension, endocrinic disorders. In our reports, they might be closely related to ectopic hematopoiesis and endocrine disorder. Maybe we should spend more time and energy on investigating the cause of myelolipoma. Radiological investigations are the diagnostic modality of choice. Surgery is an optimal treatment for patient, especially VATS. The long-term prognosis is very good.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Saleeby ER. Heterotopia of the Bone Marrow without Apparent Cause. Am J Pathol 1925;1:69-76.3. [PMC free article] [PubMed]
- 2.Kim K, Koo BC, Davis JT, et al. Primary myelolipoma of mediastinum. J Comput Tomogr 1984;8:119-23 [DOI] [PubMed] [Google Scholar]
- 3.Fonte JM, Varma JD, Kuligowska E, et al. Thoracic case of the day. Kartagener's syndrome. AJR Am J Roentgenol 1999;173:822, 826-7 [DOI] [PubMed] [Google Scholar]
- 4.Fowler MR, Williams RB, Alba JM, et al. Extra-adrenal myelolipomas compared with extramedullary hematopoietic tumors: a case of presacral myelolipoma. Am J Surg Pathol 1982;6:363-74 [DOI] [PubMed] [Google Scholar]
- 5.Vaziri M, Sadeghipour A, Pazooki A, et al. Primary mediastinal myelolipoma. Ann Thorac Surg 2008;85:1805-6 [DOI] [PubMed] [Google Scholar]
- 6.Prahlow JA, Loggie BW, Cappellari JO, et al. Extra-adrenal myelolipoma: report of two cases. South Med J 1995;88:639-43 [DOI] [PubMed] [Google Scholar]
- 7.Radhi J.Hepatic myelolipoma. J Gastrointestin Liver Dis 2010;19:106-7 [PubMed] [Google Scholar]
- 8.Cina SJ, Gordon BM, Curry NS. Ectopic adrenal myelolipoma presenting as a splenic mass. Arch Pathol Lab Med 1995;119:561-3 [PubMed] [Google Scholar]
- 9.Le Bodic MF, Mussini-Montpellier J, Magois JY, et al. Myelolipoma of the stomach. Arch Anat Pathol (Paris) 1974;22:119-22 [PubMed] [Google Scholar]
- 10.Karam AR, Nugent W, Falardeau J, et al. Multifocal extra-adrenal myelolipoma arising in the greater omentum. J Radiol Case Rep 2009;3:20-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Foster JB. Primary thoracic myelolipoma: case report. AMA Arch Pathol 1958;65:295-7 [PubMed] [Google Scholar]
- 12.Litwer H.Myelolipoma of the mediastinum. Radiology 1960;74:471-3 [DOI] [PubMed] [Google Scholar]
- 13.Krag D, Reich SB. Heterotopic bone marrow (myelolipoma) of the mediastinum. Chest 1972;61:514-5 [DOI] [PubMed] [Google Scholar]
- 14.Schön HR, Emmerich B, Arnold H, et al. Hemolytic anemia with pyruvate kinase deficiency presenting as paravertebral myelolipoma. Klin Wochenschr 1984;62:133-7 [DOI] [PubMed] [Google Scholar]
- 15.Bastion Y, Coiffier B, Felman P, et al. Massive mediastinal extramedullary hematopoiesis in hereditary spherocytosis: a case report. Am J Hematol 1990;35:263-5 [DOI] [PubMed] [Google Scholar]
- 16.Pulsoni A, Ferrazza G, Malagnino F, et al. Mediastinal extramedullary hematopoiesis as first manifestation of hereditary spherocytosis. Ann Hematol 1992;65:196-8 [DOI] [PubMed] [Google Scholar]
- 17.De Montpréville VT, Dulmet EM, Chapelier AR, et al. Extramedullary hematopoietic tumors of the posterior mediastinum related to asymptomatic refractory anemia. Chest 1993;104:1623-4 [DOI] [PubMed] [Google Scholar]
- 18.Strimlan CV, Khasnabis S. Primary mediastinal myelolipoma. Cleve Clin J Med 1993;60:69-71 [DOI] [PubMed] [Google Scholar]
- 19.Wyttenbach R, Fankhauser G, Mazzucchelli L, et al. Primary mediastinal myelolipoma: a case report. European Radiology. 1994;4:492-5 [Google Scholar]
- 20.Minamiya Y, Abo S, Kitamura M, et al. Mediastinal extraadrenal myelolipoma: report of a case. Surg Today 1997;27:971-2 [DOI] [PubMed] [Google Scholar]
- 21.Koizumi J, Harada H, Yamamoto N, et al. A case of mediastinal myelolipoma. Kyobu Geka 1999;52:869-71 [PubMed] [Google Scholar]
- 22.Kawanami S, Watanabe H, Aoki T, et al. Mediastinal myelolipoma: CT and MRI appearances. Eur Radiol 2000;10:691-3 [DOI] [PubMed] [Google Scholar]
- 23.Gao B, Sugimura H, Sugimura S, et al. Mediastinal myelolipoma. Asian Cardiovasc Thorac Ann 2002;10:189-90 [DOI] [PubMed] [Google Scholar]
- 24.Franiel T, Fleischer B, Raab BW, et al. Bilateral thoracic extraadrenal myelolipoma. Eur J Cardiothorac Surg 2004;26:1220-2 [DOI] [PubMed] [Google Scholar]
- 25.Mohan K, Gosney JR, Holemans JA. Symptomatic mediastinal myelolipoma. Respiration 2006;73:552. [DOI] [PubMed] [Google Scholar]
- 26.Rossi M, Ravizza D, Fiori G, et al. Thoracic myelolipoma diagnosed by endoscopic ultrasonography and fine-needle aspiration cytology. Endoscopy 2007;39Suppl 1:E114-5 [DOI] [PubMed] [Google Scholar]
- 27.Vaziri M, Sadeghipour A, Pazooki A, et al. Primary mediastinal myelolipoma. Ann Thorac Surg 2008;85:1805-6 [DOI] [PubMed] [Google Scholar]
- 28.Geng C, Liu N, Yang G, et al. Primary mediastinal myelolipoma: A case report and review of the literature. Oncol Lett 2013;5:862-864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ema T, Kawano R. Myelolipoma of the posterior mediastinum: report of a case. Gen Thorac Cardiovasc Surg. 2013 doi: 10.1007/s11748-013-0230-8. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fonda P, de Santiago E, Guijarro M, et al. Mediastinal myelolipoma with leukocytosis. BMJ Case Rep 2013;2013. pii: bcr2013010349. [DOI] [PMC free article] [PubMed]
- 31.Migliore M, Calvo D, Criscione A, et al. An unsual symptomatic case of mediastinal myelolipoma treated by VATS approach. Ann Ital Chir 2014;85:85-7 [PubMed] [Google Scholar]
- 32.Nakagawa M, Kohno T, Mun M, et al. Bilateral video-assisted thoracoscopic surgery resection for multiple mediastinal myelolipoma: report of a case. Korean J Thorac Cardiovasc Surg 2014;47:189-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chang KC, Chen PI, Huang ZH, et al. Adrenal myelolipoma with translocation (3;21)(q25;p11). Cancer Genet Cytogenet 2002;134:77-80 [DOI] [PubMed] [Google Scholar]
- 34.Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005;128:2893-909 [DOI] [PubMed] [Google Scholar]