Abstract
A purely laparoscopic four-port approach was created for left hepatectomy in pigs. A polyethylene loop was placed on the left two hepatic lobes for traction and lift. Next, penetrating ligation of the lobes using of a double row of silk sutures was performed to control bleeding. A direct hepatic transection was completed using a monopolar hook electrode without meticulous dissection of the left hepatic vein. The raw surface of the liver was coagulated and sealed with fibrin glue. Lobes were retrieved through an enlarged portal. Laparoscopic hepatic lobectomy was completed in all pigs without the use of specialized instruments and with a mean operative time of 179 ± 9 min. No significant perioperative complications were observed. The average weight of each resected lobe was 180 ± 51 g. Complete blood count as well as serum organics and enzyme levels normalized after about 2 weeks. During necropsy, adhesion of the hepatic raw surface to the gastric wall and omentum were observed. No other abnormalities were identified. This minimally invasive left hepatectomy technique in swine could serve as a useful model for investigating liver diseases and regeneration, and offer preclinical information to improve hepatobiliary surgical procedures.
Keywords: hepatectomy, laparoscopy, left, pigs, technique
Introduction
Liver resection is reputed to be one of the most difficult procedures in the era of laparoscopic surgery. Laparoscopic techniques for left hepatectomy have been widely described for humans [1,3,5,12,17,24,29]. Additionally, the ability to perform an anatomically reproducible hepatic resection in a large animal model could promote the investigation of liver surgery [5,18,23,26], transplantation [19,22], and regeneration [2,6,13,15,16,20,26,27] for medical research and experimental studies.
Minimally invasive laparoscopic surgery offers faster recovery times, reduced pain, and a more rapid return to activity compared to conventional surgery [29]. However, there have been only a few previous reports of laparoscopic hepatectomy performed in veterinary surgery, most of which require expensive instruments and vary in the complexity of the procedures [21]. The purpose of this study was to establish a safe and feasible technique for a purely laparoscopic left hepatectomy in pigs and report the outcomes.
Materials and Methods
Animals
Nine healthy Bama miniature pigs (6 male) 3~6 months old and weighing 15.5~25.8 kg were used for this study. They were purchased form the laboratory animal center of Harbin veterinary research institute (number of animal license SYXK 2011-0039). The experimental protocol was approved by the Northeast Agricultural University Ethical Committee (China). Care and handling of the animals were performed in accordance with national animal research guidelines (Approved by the State Council on October 31, 1988 and promulgated by Decree No. 2 of the State Science and Technology Commission on November 14, 1988). The pigs were housed individually, and fed a standard piglet diet (Shenzhen Jinxinnong Feed, China) along with tap water ad libitum.
Surgical technique
After fasting overnight, the pigs were pre-medicated with subcutaneous delivery of 0.04 mg/kg atropine sulfate (Xiantu; Harbin Pharmaceutical Group, China) along with intramuscular injection of 1 mg/kg xylazine (Rompun; Bayer HelthCare, Germany) and 10 mg/kg ketamine hydrochloride (Saituo; Chemfun Medical Technology, China). General anesthesia was induced using 1% to 3% isoflurane gas (Lishi; Jiupai Pharmaceutical, China) after intubation. The operating room temperature was maintained at 22℃. Vital signs were continuously monitored with a Philips monitor (Philips IntelliVue MP30; Philips Medizin Systeme Boeblingen, Germany). Normal saline was infused intravenously at a rate of 3 mL/kg/h through the peripheral ear vein.
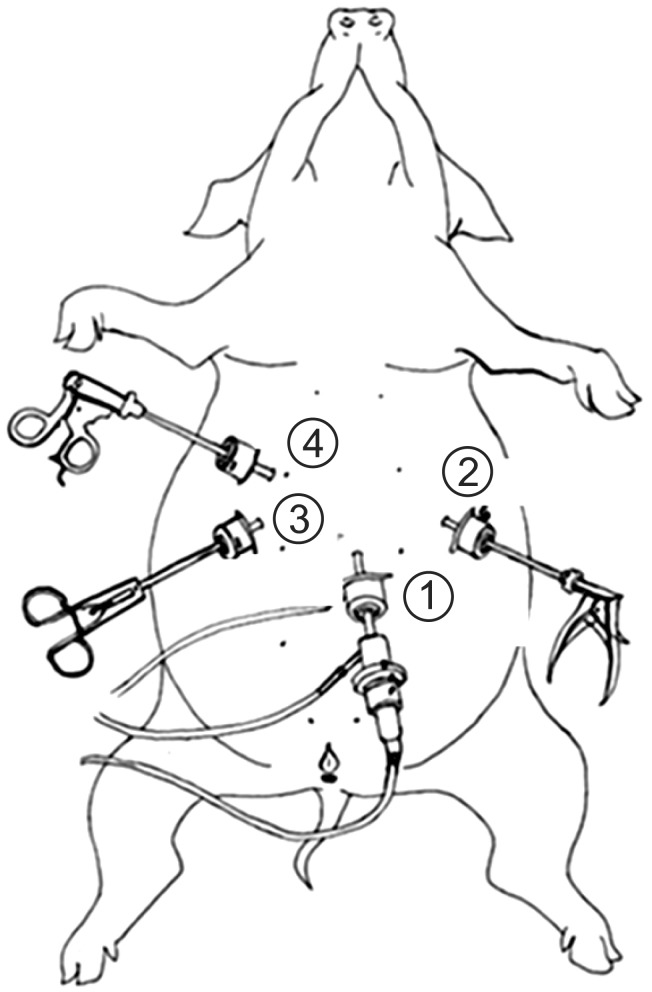
All surgical procedures were performed under aseptic conditions. The animals were positioned in a supine, head-up position with approximately 30° reverse adjustment, and a carbon dioxide pneumoperitoneum of 12 mmHg was established. A four-port, purely laparoscopic technique was adopted for this study. Accordingly, four portals (1, 2, 3, and 4) were created. Portal 1 was located 2~3 cm below the umbilicus along the ventral midline (portal 1 was shifted 2~3 cm to the left in male pigs). Portals 2 and 3 were 3~5 cm cranial to portal 1, and 8~10 cm to the left and right of the ventral midline, respectively. Portal 4 was 3~5 cm cranial to portal 3 and 8~10 cm to the left of the ventral midline (Fig. 1). A trocar-cannula unit (Olympus Corporation, Japan) with a diameter of 10~11 mm was percutaneously inserted at portal 1 and used to introduce the 0° laparoscope (10-mm diameter, Olympus Corporation). Under laparoscopic guidance, one trocar-cannula unit (diameter of 5~5.5 mm; Olympus Corporation) each was advanced through portals 2 and 4, and another trocar-cannula unit (diameter of 10~11 mm, Olympus Corporation) was inserted at portal 3. These units were used to insert laparoscopic instruments such as needle-holding forceps, monopolar hook-electrode, clip applicator, and right angle dissecting forceps (5-mm diameter; Guangdian Medical Instrument, China). The operator stood at the caudal end of the animal, and three assistant surgeons were needed to complete the laparoscopic procedure. After careful inspection with the laparoscope, the hepatectomy was performed.
Fig. 1.
Portal locations. Portal 1 (laparoscope) was located 2~3 cm below the umbilicus along the ventral midline (portal 1 was shifted 2~3 cm to the left in male pigs). Portals 2 and 3 were 3~5 cm cranial to portal 1 and 8~10 cm to the left and right of the ventral midline, respectively. Portal 4 was 3~5 cm cranial to portal 3 and 8~10 cm to the left of the ventral midline. These portals were used to introduce various laparoscopic instruments.
We mobilized the left lobes by sharply dividing the falciform and left triangular ligaments, and then a polyethylene loop (Guangdian Medical Instrument) was placed on the left two lobes for traction and lifting (Figs. 2 and 3). By slowly elevating the lobes, the hepatic hilum was delineated under direct visualization. The left branches of the hepatic artery, portal vein, and bile duct were dissected, and then clipped with medium titanium clips (Ligating clips; Kangsheng Medical Equipment, China) before cutting (Fig. 4). The left hepatic parenchyma was not meticulously dissected in order to reduce the risk of tearing, which could lead to formation of a gas embolism. We controlled bleeding with a double row of silk sutures (2/0 polyglycolic acid; Jinhuan Medical Products, China) that penetrated the parenchyma at the root of the lobes. Three needles threaded with one silk suture were used to penetrate the parenchyma (Fig. 3), and the suture was snipped near the needle shank. A knot was then tied between the ends of the snipped suture with the aid of a second pair of needle-holding forceps inserted from the third trocar (Figs. 5 and 6). A fibrin sealant (Fibrin glue; Puji Medical Technology, China) was then sprayed onto the pinholes.
Fig. 2.
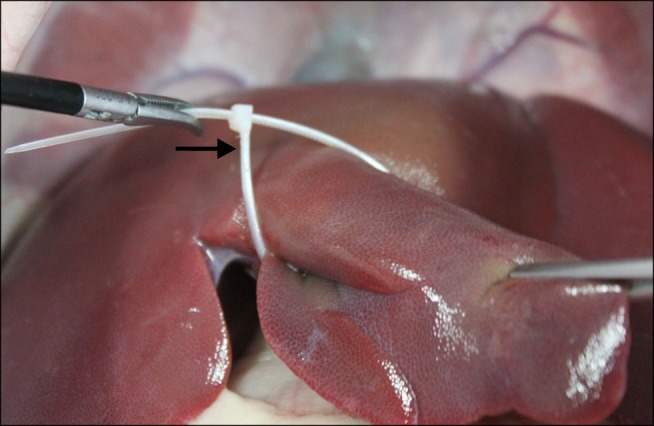
Simulated intraoperative view. A polyethylene loop (arrow) was placed on the left median lobe for traction and lifting.
Fig. 3.
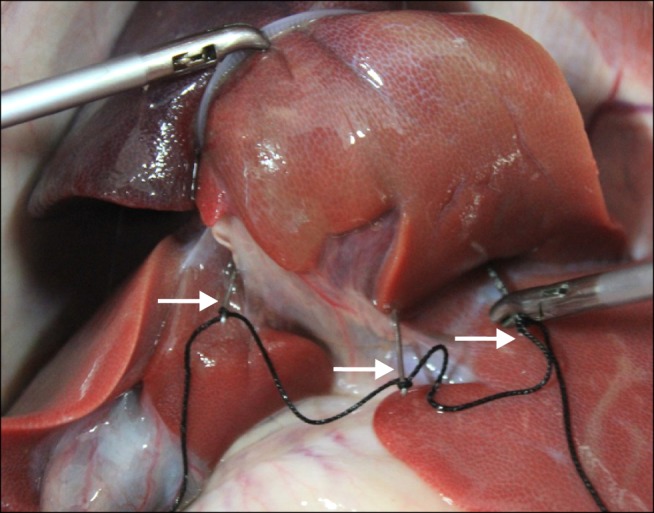
Simulated intraoperative view. Penetrating ligature of the hepatic parenchyma at the root of the lobe using three needles threaded with a silk suture (arrows).
Fig. 4.
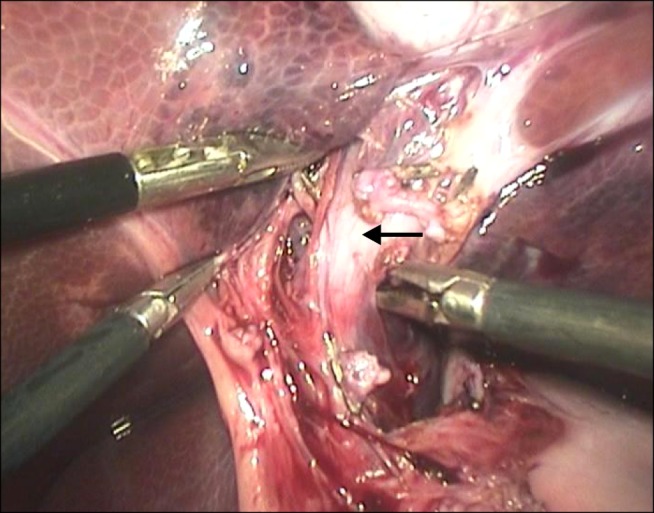
Intraoperative view. The left branches of the portal vein (arrow) were dissected and then clamped with medium titanium clips before cutting.
Fig. 5.
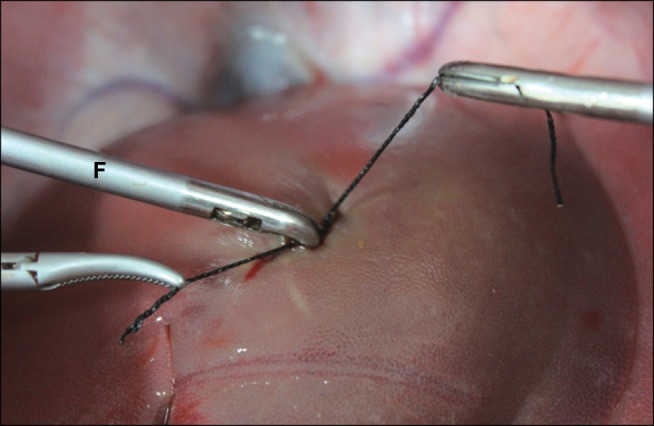
Simulated intraoperative view. A knot was tied between the ends of the snipped sutures with the aid of needle-holding forceps (F).
Fig. 6.

Simulated intraoperative view. A knot was tied with the aid of needle-holding forceps (F) inserted from the third trocar.
Hepatic transection was initiated from the left median lobe (deviating 1 cm from the ligature) using a monopolar hook electrode. Occasionally, intraparenchymal vessels larger than 5 mm were occluded with titanium clips; otherwise, ligation was achieved with sutures. Hepatic transection was performed on the left lateral lobe in the same manner. The raw surface of the liver usually required slight coagulation promoted with a spatula coagulation electrode (5-mm diameter; Tonglu Medical Instruments, China) (Fig. 7) and sealing with fibrin glue (Puji Medical Technology) to ensure hemostasis and biliostasis. A penrose drain (Fr 26; Zhanjiang Star Enterprise, China) was inserted next to the resection site through the second portal. The resected specimen was then placed in a vinyl bag and removed through a mini laparotomy incision that was created by extending the trocar site at the third portal. After ensuring that hemostasis was established, the laparoscopic equipment was removed and the portal were sutured.
Fig. 7.
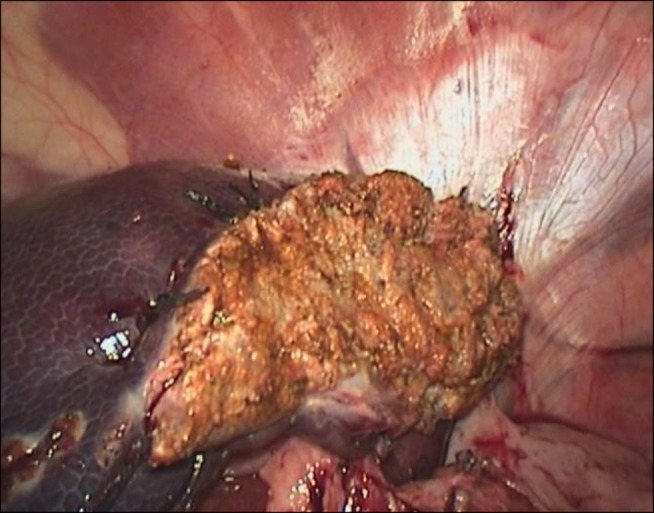
Intraoperative view. The raw area observed immediately after liver resection.
Operative time, estimated blood loss, incision length, resected specimen weight, and early postoperative outcomes were recorded for all cases. CBC results along with serum total bilirubin (T-Bil), aspartate aminotransferase (AST), albumin/globulin (A/G), and γ-glutamyl transferase (γ-GT) levels were obtained 1 day preoperatively and on postoperative days (PODs) 1, 3, 7, 14, and 30 for all pigs.
Postoperative care
After surgery, the animals were given a 5-mg fentanyl patch (5 mg/patch, Duragesic; Janssen Pharmaceutical, China) every 3 days for 6 days. Additionally, ampicillin (20 mg/kg; Shandong Lukang Record Pharmaceutical, China) was administered intramuscularly (IM) every 8 h for 3 days. Once the animals were able to stand on their own, the pigs were transferred to a 25℃ hog house for recovery. Water was given to the pigs at 6 h postoperatively and solid food was provided the following morning. Postoperative monitoring consisted of measuring body temperature as well as a subjective assessment of the pig's disposition and appetite. Drainage tubes were removed from all pigs on POD 3. The animals were evaluated daily until they were euthanized with pentothal (5 mg/kg; Janssen Pharmaceutical) and 10% potassium chloride (10 mL each time; Changle Pharmaceutical, China,) intravenously. A follow-up necropsy was performed 1 month after surgery to reevaluate the entire abdominal cavity and associated viscera.
Statistical analysis
Operating time was defined as the duration from the initial stab incision to the closure of the last portal. Blood loss was estimated by amount of fluid collected in a suction container minus the volume of fluid used for irrigation. Data are expressed as the mean ± standard error of the mean. Pre- and postoperation differences in values were identified by a one-way analysis of variance that was performed using SPSS Statistics 17.0 (SPSS, USA). p values < 0.05 were considered statistically significant.
Results
The laparoscopic procedures were completed in all pigs with a mean operative time of 179 ± 9 min (ranging between 165~192 min). The mean total incision size was 8.3 ± 0.4 cm (ranging from 5 cm to 8.5 cm). Resected liver lobe volumes were determined by the measuring cup immersion method and averaged 127 ± 24 cm3 (with a range of 95~150 cm3). The average lobe mass was 180 ± 51 g (ranging between 124 g and 274 g). Due to our initial inexperience with the surgical procedure, the maximum volume of blood loss was 350 mL. Ultimately, the mean estimated blood loss was 174 ± 96 mL (ranging from 60~350 mL) and no blood transfusions were required. All pigs had relatively satisfactory appetites that were usually observed starting on the second POD.
Three animals had low-grade fevers with leukocytosis on the first POD. Fever was successfully treated with daily intramuscular injections of ampicillin (20 mg/kg; Shandong Lukang Pharmaceutical) and acetaminophen (0.15 g each time; Jiangxi Pharmaceutical, China). Only one pig developed transient biliary leakage and intraperitoneal drainage that persisted until day 5 before dying on postoperative day 10 due to bacterial peritonitis. The necropsy did not produce any evidence of biliary tract dysfunction.
All pigs had CBC results that were within the reference range on POD 7. Vital signs and blood hematocrit values demonstrated that none of the pigs experienced postoperative bleeding. Both serum organics and enzymes levels normalized after 2 weeks (Table 1). None of the pigs showed weight loss by 1 month after surgery. Transection of the left lobes with no gross leakage or abscess formation was observed during necropsy. Close attachment and adherence of the raw hepatic surface to the gastric wall, omentum, or antero-lateral abdominal wall were also discovered. No other abdominal abnormalities were observed.
Table 1.
Main CBC results and assessment of liver function according to serum organics or enzyme analyses
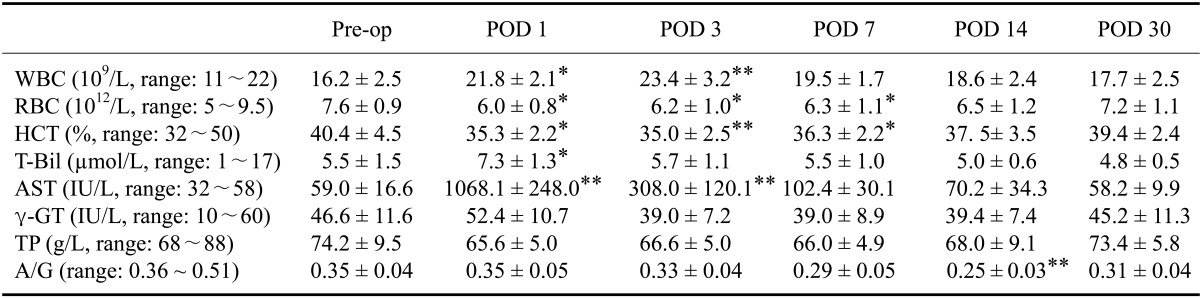
Pre-op: pre-operation, POD: postoperative day. *0.01 < p < 0.05 and **p < 0.01 compared to pre-operation values according to a one-way ANOVA. WBC: white blood cell, RBC: red blood cell, HCT: hematocrit, T-Bil: total bilirubin, AST: aspartate aminotransferase, γ-GT: γ-glutamyl transferase, TP: total protein, A/G: albumin/globulin.
Discussion
Successful laparoscopic left hepatectomy has been reported in a number of small series [6,16,26] that mainly required advanced instruments such as a fan retractor, Endo-GIA Stapler, harmonic scalpel, or argon beam coagulator. In the current study, we developed a laparoscopic left hepatectomy procedure in a large animal model. The four-portal technique we established is relatively simple and does not require specialized instruments (e.g., a Ligasure). Lobe traction can be easily achieved by installing a polyethylene loop. This loop facilitates better exposure of the hepatic portal compared to a fan retractor, thus allowing hepatic hilar dissection and inflow occlusion.
We controlled bleeding with partial clamping of the hepatic hilum, monopolar electrocoagulation, use of titanium clips, and penetrating ligation of the liver parenchyma. Intraoperative blood loss was nearly the same as that reported when using standard laparoscopic staplers (174 ± 96 mL vs. 185 ± 9 mL) for laparoscopic left lateral liver resection [7]. With experience, our operative time decreased by 27 min (from 192 to 165 min) and could improve further with additional practice. Thus, we successfully developed a laparoscopic left hepatectomy protocol without increasing bleeding or operating time, thereby reducing costs compared to previously reported hepatectomy procedures [10,25].
The only pig mortality was caused by bacterial peritonitis. Another pig had a serum T-Bil concentration of 10.2 µmol/L on the first POD. This represents a very acceptable complication rate and is comparable to that of any modern liver resection procedure [4,9,12,28]. In addition, our laparoscopic technique has a greatly simplified surgical protocol compared to purely laparoscopic or hand-assisted techniques previously described in the literature [14,19,22]. Furthermore, our technique is minimally invasive and resulted in less bleeding as well as faster recovery times.
Unlike humans, the hepatic vein and inferior vena cava (IVC) confluence is intraparenchymal in pigs [8,22]. We also found the left hepatic vein to be very friable, short, and prone to damage. We noted that the IVC and intraparenchymal hepatic veins had extremely thin walls, and that the neighboring diaphragm was easily damaged. Resection of the hepatic parenchyma was completed with a direct transection that enabled us to avoid meticulous dissection of the left hepatic vein in order to reduce the risk of tearing, thereby preventing any occurrence of major hemorrhaging, gas embolism formation, or pneumothorax. By partial clamping of the hepatic hilum and penetrating ligation of the parenchyma, specific liver resection complications such as hemorrhage, biliary leaks, and gas embolism development were reduced during surgery. We therefore confirmed that our method may be considered as safe as open resection or the use of Endovascular staplers [9,11]. However, the procedure we developed must be performed by skilled surgeons trained in laparoscopic suturing techniques.
In conclusion, our study demonstrated that laparoscopic left hepatectomy can be performed in healthy pigs. This was accomplished with a four-portal technique using two polyethylene loops for lobe traction, partial blocking of the hepatic hilum with metal clips, penetrating ligation, and monopolar cautery of the liver parenchyma. The resulting postoperative outcomes strongly indicate the promise of our operative procedure.
Footnotes
There is no conflict of interest.
References
- 1.Abu Hilal M, McPhail MJ, Zeidan B, Zeidan S, Hallam MJ, Armstrong T, Primrose JN, Pearce NW. Laparoscopic versus open left lateral hepatic sectionectomy: a comparative study. Eur J Surg Oncol. 2008;34:1285–1288. doi: 10.1016/j.ejso.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 2.Arkadopoulos N, Kostopanagiotou G, Nastos C, Papalois A, Papoutsidakis N, Kalimeris K, Defterevos G, Kanna T, Polyzois K, Kampouroglou G, Kypriotis D, Costopanagiotou C, Pafiti A, Tzanatos H, Smyrniotis V. Reversal of experimental posthepatectomy liver failure in pigs: a new application of hepatocyte bioreactors. Artif Organs. 2011;35:29–36. doi: 10.1111/j.1525-1594.2010.01016.x. [DOI] [PubMed] [Google Scholar]
- 3.Belli G, Fantini C, D'Agostino A, Belli A, Cioffi L, Russolillo N. Laparoscopic left lateral hepatic lobectomy: a safer and faster technique. J Hepatobiliary Pancreat Surg. 2006;13:149–154. doi: 10.1007/s00534-005-1023-y. [DOI] [PubMed] [Google Scholar]
- 4.Buell JF, Koffron AJ, Thomas MJ, Rudich S, Abecassis M, Woodle ES. Laparoscopic liver resection. J Am Coll Surg. 2005;200:472–480. doi: 10.1016/j.jamcollsurg.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 5.Cannon RM, Brock GN, Marvin MR, Buell JF. Laparoscopic liver resection: an examination of our first 300 patients. J Am Coll Surg. 2011;213:501–507. doi: 10.1016/j.jamcollsurg.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 6.Chen YL, Chen WB, Wan YY, Li WG, Huang ZQ, Wu XT, Yang J, Yang L. Effects of partial portal vein arterialization on liver regeneration after hepatectomy in minipigs with obstructive jaundice. Chin Med J (Engl) 2012;125:2302–2305. [PubMed] [Google Scholar]
- 7.Consten EC, Dakin GF, Robertus JL, Bardaro S, Milone L, Gagner M. Perioperative outcome of laparoscopic left lateral liver resection is improved by using a bioabsorbable staple line reinforcement material in a porcine model. Surg Endosc. 2008;22:1188–1193. doi: 10.1007/s00464-007-9718-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Court FG, Wemyss-Holden SA, Morrison CP, Teague BD, Laws PE, Kew J, Dennison AR, Maddern GJ. Segmental nature of the porcine liver and its potential as a model for experimental partial hepatectomy. Br J Surg. 2003;90:440–444. doi: 10.1002/bjs.4053. [DOI] [PubMed] [Google Scholar]
- 9.D'Angelica M. Laparoscopic partial hepatectomy. Surg Pract. 2005;9:90–93. [Google Scholar]
- 10.Eiriksson K, Fors D, Rubertsson S, Arvidsson D. Laparoscopic left lobe liver resection in a porcine model: a study of the efficacy and safety of different surgical techniques. Surg Endosc. 2009;23:1038–1042. doi: 10.1007/s00464-008-0115-6. [DOI] [PubMed] [Google Scholar]
- 11.Frezza EE, Wachtel MS. A proposed canine model of laparoscopic nonanatomic liver resection. J Laparoendosc Adv Surg Tech A. 2006;16:15–20. doi: 10.1089/lap.2006.16.15. [DOI] [PubMed] [Google Scholar]
- 12.Herrero Fonollosa E, Cugat Andorra E, García-Domingo MI, Rivero Deniz J, Camps Lasa J, Rodríguez Campos A, Riveros Caballero M, Marco Molina C. Laparoscopic left lateral sectionectomy. Presentation of our technique. Cir Esp. 2011;89:650–656. doi: 10.1016/j.ciresp.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 13.Hisakura K, Murata S, Fukunaga K, Myronovych A, Tadano S, Kawasaki T, Kohno K, Ikeda O, Pak S, Ikeda N, Nakano Y, Matsuo R, Konno K, Kobayashi E, Saito T, Yasue H, Ohkohchi N. Platelets prevent acute liver damage after extended hepatectomy in pigs. J Hepatobiliary Pancreat Sci. 2010;17:855–864. doi: 10.1007/s00534-010-0276-2. [DOI] [PubMed] [Google Scholar]
- 14.Kurian MS, Gagner M, Murakami Y, Andrei V, Jossart G, Schwartz M. Hand-assisted laparoscopic donor hepatectomy for living related transplantation in the porcine model. Surg Laparosc Endosc Percutan Tech. 2002;12:232–237. doi: 10.1097/00129689-200208000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Kwon YS, Jang KH, Jang IH. The effects of Korean red ginseng (ginseng radix rubra) on liver regeneration after partial hepatectomy in dogs. J Vet Sci. 2003;4:83–92. [PubMed] [Google Scholar]
- 16.Ladurner R, Traub F, Schenk M, Königsrainer A, Glatzle J. Cellular liver regeneration after extended hepatic resection in pigs. HPB Surg. 2009;2009:306740. doi: 10.1155/2009/306740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lai PB, Lee KF, Wong J, Li AK. Techniques for liver resection: a review. Surgeon. 2007;5:166–174. doi: 10.1016/s1479-666x(07)80044-8. [DOI] [PubMed] [Google Scholar]
- 18.Laurence JM, Lam VWT, Langcake ME, Hollands MJ, Crawford MD, Pleass HCC. Laparoscopic hepatectomy, a systematic review. Anz J Surg. 2007;77:948–953. doi: 10.1111/j.1445-2197.2007.04288.x. [DOI] [PubMed] [Google Scholar]
- 19.Lin E, Gonzalez R, Venkatesh KR, Mattar SG, Bowers SP, Fugate KM, Heffron TG, Smith CD. Can current technology be integrated to facilitate laparoscopic living donor hepatectomy? Surg Endosc. 2003;17:750–753. doi: 10.1007/s00464-002-8858-y. [DOI] [PubMed] [Google Scholar]
- 20.Liska V, Treska V, Mirka H, Benes J, Vycital O, Bruha J, Pitule P, Skalicky T, Sutnar A, Chlumska A, Racek J, Trefil L, Finek J, Holubec L. Immediately preoperative use of biological therapy does not influence liver regeneration after large resection-porcine experimental model with monoclonal antibody against epidermal growth factor. In Vivo. 2012;26:683–691. [PubMed] [Google Scholar]
- 21.May LR, Mehler SJ. Complications of hepatic surgery in companion animals. Vet Clin North Am Small Anim Pract. 2011;41:935–948. doi: 10.1016/j.cvsm.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 22.Pinto PA, Montgomery RA, Ryan B, Robert W, Hsu T, Kavoussi P, Klein AS, Kavoussi LR, Molmenti EP. Laparoscopic procurement model for living donor liver transplantation. Clin Transplant. 2003;17(Suppl 9):39–43. doi: 10.1034/j.1399-0012.17.s9.7.x. [DOI] [PubMed] [Google Scholar]
- 23.Rao A, Rao G, Ahmed I. Laparoscopic vs. open liver resection for malignant liver disease. A systematic review. Surgeon. 2012;10:194–201. doi: 10.1016/j.surge.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Robles Campos R, Marín Hernández C, Löpez Conesa A, Abellán B, Pastor Pérez P, Parrilla Paricio P. Laparoscopic resection of the left segments of the liver: the "ideal technique" in experienced centres? Cir Esp. 2009;85:214–221. doi: 10.1016/j.ciresp.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Saidi RF, Ahad A, Escobar R, Nalbantoglu I, Adsay V, Jacobs MJ. Comparison between staple and vessel sealing device for parynchemal transection in laparoscopic liver surgery in a swine model. HPB (Oxford) 2007;9:440–443. doi: 10.1080/13651820701658219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shimoda M, Iwasaki Y, Okada T, Kubota K. Edaravone inhibits apoptosis caused ischemia/reperfusion injury in a porcine hepatectomy model. World J Gastroenterol. 2012;18:3520–3526. doi: 10.3748/wjg.v18.i27.3520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vibert E, Perniceni T, Levard H, Denet C, Shahri NK, Gayet B. Laparoscopic liver resection. Br J Surg. 2006;93:67–72. doi: 10.1002/bjs.5150. [DOI] [PubMed] [Google Scholar]
- 28.Wu JS, Strasberg SM, Luttmann DR, Meininger TA, Talcott MR, Soper NJ. Laparoscopic hepatic lobectomy in the porcine model. Surg Endosc. 1998;12:232–235. doi: 10.1007/s004649900641. [DOI] [PubMed] [Google Scholar]
- 29.Yoon YS, Han HS, Choi YS, Lee SI, Jang JY, Suh KS, Kim SW, Lee KU, Park YH. Total laparoscopic left lateral sectionectomy performed in a child with benign liver mass. J Pediatr Surg. 2006;41:e25–e28. doi: 10.1016/j.jpedsurg.2005.10.068. [DOI] [PubMed] [Google Scholar]