Abstract
Background:
The study assessed whether low maternal serum cholesterol during early pregnancy is associated with preterm delivery.
Patients and Methods:
It was a prospective observational cohort study involving pregnant women at gestational age of 14-20 weeks over a period of 12 months. Blood samples were obtained to measure total serum cholesterol concentrations and the sera were then analysed enzymatically by the cholesterol oxidase: p-aminophenazone (CHOD PAP) method.
Results:
The study showed an incidence of 5.0% for preterm delivery in the low risk study patients. Preterm birth was 4.83-times more common with low total maternal cholesterol than with midrange total cholesterol (11.8% versus 2.2%, P = 0.024).
Conclusion:
Low maternal serum cholesterol (hypocholesterolaemia) is associated with preterm delivery. Optimal maternal serum cholesterol during pregnancy may have merit, therefore pregnant women should be encouraged to follow a healthy, balanced diet.
Keywords: Hypocholesterolaemia, preterm birth, preterm delivery, perinatal mortality
INTRODUCTION
Preterm birth is a major challenge in perinatal health care, with preterm babies accounting for 5-25% of all deliveries1,2 and up to 75% of all perinatal mortality in some series.1 In Nigeria, preterm babies account for 40-60% of all perinatal deaths.3,4,5 Preterm birth is also an important risk factor for neurological impairment and disability. The social and emotional cost of perinatal morbidity and mortality associated with prematurity is certainly enormous.6 Preterm birth not only affects infants and their families — providing care for preterm infants, who may spend several months in hospital, has increasing cost implications for health services.
Preterm delivery is defined as birth occurring prior to 37 completed weeks of gestation.7 The majority is preceded by spontaneous preterm labour, which is defined as labour that occurs with regular, and frequent uterine contractions causing progressive cervical changes before 37 completed weeks of gestation.8
Preterm infants are at increased risk of death,9 short- and long-term pulmonary,10 ophthalmologic11 and neurologic morbidity; and delayed psychomotor development.12,13 A large proportion of these morbidity and mortality occur in the developing countries.14 The exact cause of preterm labour and delivery remains elusive and is likely to be multifactorial. In 50% cases, it is spontaneous and idiopathic although several potential risk factors have been identified. The most notable is premature rupture of membrane (PROM), and others are multiple pregnancy, polyhydramnios, hypertensive disorder of pregnancy, infections, cervical incompetence, antepartum haemorrhage, fetal and uterine anomalies, anaemia, heavy work, smoking, etc. It is also related to socioeconomic status and geographic location.15,16
Prevention of viable spontaneous preterm birth through screening is one of the key aims of antenatal care as these have implications for child, mother and society. If women can be identified to be at high risk from early pregnancy, they can be targeted for more intensive antenatal surveillance and prophylactic interventions (primary prevention). However, the disease mechanisms behind preterm delivery are not well understood. Consequently, tests for its prediction and treatments for its prevention are not well developed. The predictors may be used in the management of women at high risk for preterm labour, such as women with previous preterm labour and also can be used as a part of a management protocol to individualise patient care. This therefore supports the need to investigate the association between preterm labour and basic biochemical functions of the body of which cholesterol biosynthesis is among.
Maternal cholesterol is essential for both the hormonal and physical changes of early pregnancy.17 Circulating low-density lipoprotein cholesterol is the chief substrate for placental progesterone biosynthesis.18,19 Subclasses of high-density lipoprotein cholesterol also participate in placental cholesterol balance.20 Cholesterol is a bulk constituent of decidual tissue critical to implantation and uteroplacental vascularisation.21 Alterations in placental cholesterol concentrations have been associated with changes in placental transport functions during gestation.22 The physiologic hypercholesterolaemia of later pregnancy.23,24 therefore suggests an adaptive function for pregnancy maintenance.25 It is thus hypothesised specifically that low maternal serum cholesterol may increase the risk for preterm delivery.
It is not known whether optimal levels of maternal serum cholesterol during pregnancy can be defined. There is presently very few data addressing any potential risk to the pregnancy when maternal serum cholesterol falls below a lower bound.
This study will therefore aim to investigate whether low maternal serum cholesterol level during early gestation may be associated with preterm delivery in the Nigerian setting.
PATIENTS AND METHODS
The study was conducted at the Antenatal clinic and Labour ward complex of a Lagos tertiary hospital. It was a prospective observational cohort study of pregnancy outcome in young, generally healthy pregnant women attending the antenatal clinic of the hospital.
The sample size (N) for the study was determined using the statistical formula by Schlesselman.26 While making provision for attrition rate of 10%, a total of 320 participants were enrolled at gestational ages of 14 and 20.
Eligible participants were pregnant women aged 18 to 35 years and have a singleton gestation. Exclusion criteria included pregnant women with multiple gestations, history of diabetes or hypertension, human immunodeficiency virus (HIV), current or previous history of smoking, other described substance use, and reports of previous abnormal pregnancy history. Additional patients were excluded at delivery when records indicated significant intercurrent infections or other illness, preeclampsia or other gestational disorders. th
Participants for the study were selected by consecutive sampling method over a period of 12 months. A structured interviewer administered questionnaire was used to collect data after obtaining informed written consent from each participant upon explanation of the nature and purpose of the study. Social classes were determined using the Oyedeji socioeconomic classification scheme.27
Venous blood samples were obtained from fasting patient in the morning to measure total serum cholesterol concentrations between 14 and 20 weeks’ gestation. Samples were collected in lithium heparin specimen bottles. Total cholesterol in serum was then analysed enzymatically by the cholesterol oxidase: P-aminophenazone (CHOD-PAP) method using reagents from the manufacturer (BIOLABO SA, 02160, Maizy, France).
The reference value for normal serum cholesterol is 200-239 mg/dl.28 Thus, low maternal serum cholesterol pregnancies were defined as those in which maternal serum cholesterol level fall below 200 mg/dL. Gestational duration was based upon gestation from participants’ last normal menstrual period confirmed or modified by ultrasound. Preterm delivery was used as confirmatory outcome variable in the analysis.
All quantitative data were entered in computer and analysed using Statistical Package for the Social Sciences (SPSS) version 17 for windows.29 Descriptive statistics were computed for all relevant data. Association between low maternal serum cholesterol and preterm delivery was tested using chi-square. All significances are reported at P < 0.05.
Ethical approval for the study was obtained from the hospital's Health Research and Ethics committee prior to the commencement of the study and written consent obtained from each participant before involvement in the study.
RESULTS
The study is a prospective observational cohort study in which 320 pregnant women with singleton gestation between the gestational age of 14-20 weeks were enrolled at the point of sample collections. However, on review of clinical data at delivery, 33 (10.3%) of the ascertained cohort subjects were excluded.
The final cohort available for analysis was therefore 287 (representing 89.7% of the study patients) which included 76 (26.5%) women with total cholesterol levels below the reference range (200-239 mg/dL) and 211 (73.5%) women with higher total cholesterol with the breakdown showing 185 women with mid-range and 26 with high total cholesterol levels respectively [Figure 1]. The 26 subjects with high total cholesterol levels were also excluded prior to the final analysis.
Figure 1.
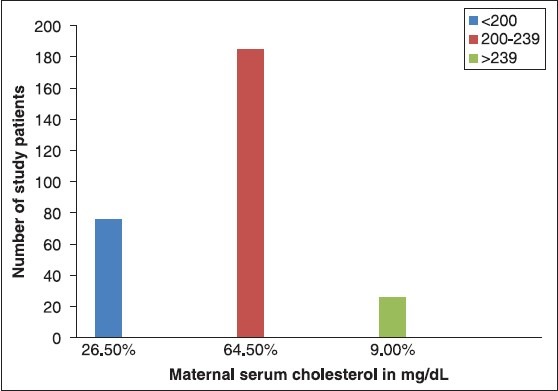
The final cohort available for analysis was therefore 287 (representing 89.7% of the study patients) which included 76 (26.5%) women with total cholesterol levels below the reference range (200-239 mg/dL) and 211 (73.5%) women with higher total cholesterol with the breakdown showing 185 women with mid-range and 26 with high total cholesterol levels respectively
When maternal characteristics were examined according to the serum cholesterol levels [Tables 1 and 2], there were no significant differences found between the mothers with low total cholesterol and control subjects with mid-range total cholesterol with respect to the gestational age at enrolment or samples collection (P = 0.111), gestation at delivery (P = 0.857), parity (P = 0.534), marital status (P = 0.064), tribe (P = 0.830), religion (P = 0.106) and mode of delivery (P = 0.139). However, there were positive linear relationships between serum cholesterol levels with maternal age (P = 0.007) and body mass index (BMI; P = 0.032). A weak but statistically significant relationship was found between low total cholesterol and the lower socioeconomic class (P = 0.044) when compared to women with mid-range total cholesterol.
Table 1.
Maternal serum cholesterol levels and socio-demographic characteristics of study patients

Table 2.
Maternal serum cholesterol levels and socio-demographic characteristics of study patients

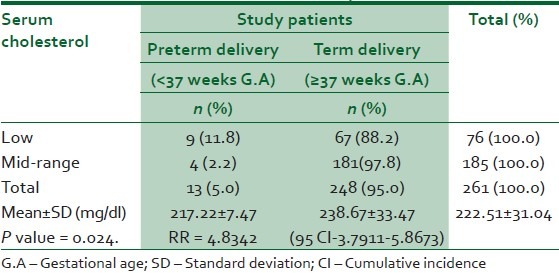
Table 3 showed that even among this low-risk cohort of patients used in the study, the incidence of preterm delivery was found to be 5.0%. Preterm birth was 4.83-times more common with low total maternal cholesterol than with midrange cholesterol (11.8% versus 2.2%, P = 0.024).
Table 3.
Relationship between low maternal serum cholesterol and preterm delivery
DISCUSSIONS
This observational cohort study examined how a substantially low value of maternal serum cholesterol levels in early pregnancy which represents a relatively normal peri-conceptional cholesterol level that failed to rise as expected in the second trimester, would affect later events, such as week of delivery.
There was a weak but statistically significant relationship between low total cholesterol and the lower socioeconomic class when compared to women with mid-range total cholesterol. This indicates that, micronutrient deficiencies may be more common among the low-total cholesterol risk group studied here and could account for the observed outcome. Many such nutritional deficiencies have been studied as predictors of preterm delivery.30
The incidence of preterm delivery in this highly selected study cohort (5.0%) was only slightly lower than that quoted in the study by Edison et al., (6.6%)31 but it is still within the range quoted by Kierse at 5-10%2 and from a study done in a regional tertiary hospital in Nigeria by Ezechukwu et al., (5-25%)1 This was probably due to the similarities in the patients populations used in all these studies.
The almost fivefold statistical elevation in the risk of preterm labour among mothers with low-total cholesterol compared to those with mid-range total cholesterol is similar to the finding by Edison et al., who also reported a 2.93 folds increase risk.31 Although, this association was observed only among the white mothers by Edison et al., our study showed that the association also exists among the black Nigerian mothers. The possible explanation may lie in the control study population which included both women with mid-range and high total cholesterol levels in the Edison's study while only women with mid-range total cholesterol were used in this present study thus increasing the likelihood of having more women in the low total cholesterol group compared to the control group.
LIMITATIONS TO THE STUDY
Since the study is hospital based, there was selection-bias in the enrolment of participants thus limiting the generalizability of the study to the whole population. The incessant strike action by the hospital staff also resulted in a higher than expected fall-out rate of the recruited participants in the study.
CONCLUSION
Based on this study, low maternal serum cholesterol (hypocholesterolaemia) is associated with preterm delivery. It is therefore recommended that pregnant women should be encouraged to follow a healthy balanced diet intake in order to maintain an optimal range of maternal serum cholesterol during pregnancy to avoid preterm delivery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ezechukwu CC, Ugochukwu EF, Egbuonu I, Chukwuka JO. Risk factors for neonatal mortality in a regional tertiary hospital in Nigeria. Nig J Clin Pract. 2004;7:50–2. [Google Scholar]
- 2.Kierse MJ. New perspectives for the effective treatment of preterm labour. Am J Obstet Gynecol. 1995;173:618–28. doi: 10.1016/0002-9378(95)90292-9. [DOI] [PubMed] [Google Scholar]
- 3.Chike-Obi U. Preterm delivery in Ilorin: Multiple and teenage pregnancies major aetiologic factors. West Afr J Med. 1993;12:228–30. [PubMed] [Google Scholar]
- 4.Njokanma OF, Olanrewaju DM. A study of neonatal deaths at the Ogun State University Teaching Hospital, Sagamu, Nigeria. J Trop Med Hyg. 1995;98:155–60. [PubMed] [Google Scholar]
- 5.Njokanma OF, Sule-Odu OA, Akesode FA. Perinatal mortality at the Ogun State University Teaching Hospital, Sagamu, Nigeria. J Trop Paediatr. 1994;40:78–81. doi: 10.1093/tropej/40.2.78. [DOI] [PubMed] [Google Scholar]
- 6.Azikeh ME. Preterm labour and delivery. In: Okpere E, editor. Clinical Obstetrics. Benin City: University of Benin Press; 2003. pp. 203–9. [Google Scholar]
- 7.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arius F. Practical Guide to High Risk Pregnancy and Delivery. 2nd ed. USA; 1993. Preterm Labour; pp. 71–99. [Google Scholar]
- 9.Kramer MS, Demissie K, Yang H, Platt RW, Sauvé R, Liston R. The contribution of mild and moderate preterm birth to infant mortality. Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. JAMA. 1990;284:843–9. doi: 10.1001/jama.284.7.843. [DOI] [PubMed] [Google Scholar]
- 10.McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;312:82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- 11.Page JM, Schneeweiss S, Whyte HE, Harvey P. Ocular sequelae in premature infants. Pediatrics. 1993;92:787–90. [PubMed] [Google Scholar]
- 12.Stewart AL, Rifkin L, Amess PN, Kirkbride V, Townsend JP, Miller DH, et al. Brain structure and neurocognitive and behavioural function in adolescents who were born very preterm. Lancet. 1999;353:1653–7. doi: 10.1016/s0140-6736(98)07130-x. [DOI] [PubMed] [Google Scholar]
- 13.Hack M, Wilson-Costello D, Friedman H, Taylor GH, Schluchter M, Fanaroff AA. Neurodevelopment and predictors of outcomes of children with birth weights of less than 1000 g: 1992-1995. Arch Pediatr Adolesc Med. 2000;154:725–31. doi: 10.1001/archpedi.154.7.725. [DOI] [PubMed] [Google Scholar]
- 14.Brian-D Adinma JI, Agbai AO. Pattern of twin births in Nigerian Igbo woman. West Afr J Med. 1994;13:234–6. [PubMed] [Google Scholar]
- 15.Worldwide Atosiban versus Beta-agonists Study Group. Effectiveness and safety of the oxytocin antagonist atosiban versus beta-adrenergic agonists in the treatment of preterm labour. The Worldwide Atosiban versus Beta-agonists Study Group. BJOG. 2001;108:133–42. [PubMed] [Google Scholar]
- 16.Lumley J. Defining the problem: The epidemiology of preterm birth. BJOG. 2003;110:3–7. [PubMed] [Google Scholar]
- 17.Woollett LA. The origins and roles of cholesterol and fatty acids in the fetus. Curr Opin Lipidol. 2001;12:305–12. doi: 10.1097/00041433-200106000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Tuckey RC. Progesterone synthesis by the human placenta. Placenta. 2005;26:273–81. doi: 10.1016/j.placenta.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 19.Henson MC, Shi W, Greene SJ, Reggio BC. Effects of pregnant human, non-pregnant human and fetal bovine sera on human chorionic gonadotropin, estradiol, and progesterone release by cultured human trophoblast cells. Endocrinology. 1996;13:2067–74. doi: 10.1210/endo.137.5.8612549. [DOI] [PubMed] [Google Scholar]
- 20.Knopp RH, Warth MR, Charles D, Childs M, Li JR, Mabuchi H, et al. Lipoprotein metabolism in pregnancy, fat transport to the fetus, and the effects of diabetes. Biol Neonate. 1986;50:297–317. doi: 10.1159/000242614. [DOI] [PubMed] [Google Scholar]
- 21.Woollett LA. Maternal cholesterol in fetal development: Transport of cholesterol from the maternal to the fetal circulation. Am J Clin Nutr. 2005;82:1155–61. doi: 10.1093/ajcn/82.6.1155. [DOI] [PubMed] [Google Scholar]
- 22.Sen A, Ghosh PK, Mukherjea M. Changes in lipid composition and fluidity of human placental basal membrane and modulation of bilayer protein functions with progress of gestation. Mol Cell Biochem. 1998;187:183–90. doi: 10.1023/a:1006839711587. [DOI] [PubMed] [Google Scholar]
- 23.Winkler K, Wetzka B, Hoffmann MM, Friedrich I, Kinner M, Baumstark MW, et al. Low density lipoprotein (LDL) subfractions during pregnancy: Accumulation of buoyant LDL with advancing gestation. J Clin Endocrinol Metab. 2000;85:4543–50. doi: 10.1210/jcem.85.12.7027. [DOI] [PubMed] [Google Scholar]
- 24.Brizzi P, Tonolo G, Esposito F, Puddu L, Dessole S, Maioli M, et al. Lipoprotein metabolism during normal pregnancy. Am J Obstet Gynecol. 1999;181:430–4. doi: 10.1016/s0002-9378(99)70574-0. [DOI] [PubMed] [Google Scholar]
- 25.Tranquilli AL, Cester N, Giannubilo SR, Corradetti A, Nanetti L, Mazzanti L. Plasma lipids and physicochemical properties of the erythrocyte plasma membrane throughout pregnancy. Acta Obstet Gynecol Scand. 2004;83:443–8. doi: 10.1111/j.0001-6349.2004.00341.x. [DOI] [PubMed] [Google Scholar]
- 26.Schlesselman JJ. Sample size requirements in cohort and case control studies of disease. Am J Epidemiol. 1974;99:381–4. doi: 10.1093/oxfordjournals.aje.a121625. [DOI] [PubMed] [Google Scholar]
- 27.Oyedeji GA. Socioeconomic status and cultural background of hospitalized children in Ilesa. Nig J Paediatr. 1985;12:111–7. [Google Scholar]
- 28.Clinical Guide to laboratory test. 4th ed. NW Tietz; 2006. pp. 244–9. [Google Scholar]
- 29.The SPSS System for Windows [computer program]. Version 17. Cary, NC: SPSS Institute Inc; 2008. [Google Scholar]
- 30.Scholl TO. Iron status during pregnancy: Setting the stage for mother and infant. Am J Clin Nutr. 2005;81:1218–22S. doi: 10.1093/ajcn/81.5.1218. [DOI] [PubMed] [Google Scholar]
- 31.Edison RJ, Berg K, Remaley A, Kelley R, Rotimi C, Stevenson RE, et al. Adverse birth outcome among mothers with low serum cholesterol. Paediatrics. 2007;120:723–33. doi: 10.1542/peds.2006-1939. [DOI] [PubMed] [Google Scholar]


