Abstract
Background:
Honey is one of the oldest known medicines. Its use has been rediscovered in later times by the medical profession, especially for dressing wounds. It has been reported from various clinical studies on the usages of honey as a dressing for infected wounds that the wound become sterile in 3-6 days, others have al so reported that the honey is effective in cleaning up infected wound.
Materials and Methods:
The 54 patients of dry socket were selected from the from the outpatient department of oral and maxillofacial surgery. A diagnosis of dry socket was made clinically. This study was under taken to evaluate the effect of honey dressing in management of dry socket.
Results:
In this study there was significant reduction if inflammation, hyperemia, edema and exudation after honey dressing that results in soothing effect and reduction in pain and discomfort. There was al so significant reduction in CRP level post operative days .There was side effect of honey was observed in our study, so it can be used as alternative for the management of dry socket.
Discussion:
It has al so been reported that the honey dressing halt advancing necrosis. It has al so been found to act as barrier preventing wounds from becoming infected, preventing cross infection, and allowing burn wound to heal rapidly.
Conclusions:
There are no side effects of honey. Excess use of euginol, can lead to necrosis of bone. The honey can be used as medicament for the management of dry socket.
Keywords: Dry socket, euginol, honey
INTRODUCTION
Honey is one of the oldest known medicines and its use has been rediscovered in later times by the medical profession, especially for dressing wounds. It has been reported from various clinical studies on the usages of honey as a dressing for infected wounds that the wound become sterile in 3-6 days, others have also reported that the honey is effective in cleaning up infected wound. It has also been reported that honey dressing halt advancing necrosis. Hence the honey can be used for the management of dry socket. In Ayurveda, - honey is considered to positively affect all three primitive imbalance of the body. Charak and Sushruta applied honey dressing for sores. In the third century, Greek philosopher Celsus used mixes honey and bran to treat burn.
Dry socket or alveolar osteitis is one of the most common post-operative complications following the extraction of permanent teeth. It is a condition in which there is a loss of clot from the socket clinically post-operative discomfort can range from simple local inflammation to classic alveolar osteitis including halitosis regional trismus dull thrombing pain irradiating from empty socket, normally to ipsilateral ear, temporal region or eye. Occasionally regional lymphadenopathy is al so noted. It is believed to be multi factorial in origin and these are some commonly etiological aggravating and precipitating factors.
Oral microorganism, trauma during surgery, roots and bone fragments remaining in the cavity, excessive curettage and irrigation, dislodgement of blood clot, oral contraceptives and smoking are the some of the important factors.
There are various treatment modalities used for management of dry socket like bland obtundant dressing, pain reducing dressing such as zinc oxide euginol dressing, anti-infective agents, systemic or local, antifibrinolytic agent, surgical intervention to remove necrotic clot and encourage the formation of blood clot.
METHODOLOGY
A total of 54 patients of dry socket were selected from the out-patient Department of Oral and Maxillofacial Surgery. The informed consent was taken prior to treatment. Patients with systemic illness like diabetes, pregnant and lactating female were not included in the study. Sterile gouge soaked with honey was used as a dressing. A diagnosis of dry socket was made clinically. This packing is changed until the post-operative pain symptoms subsided. This study was under taken to evaluate the effect of honey dressing in management of dry socket [Tables 1–6].
Table 1.
Gender
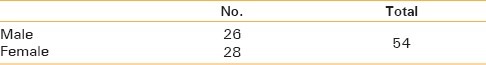
Table 6.
C-reactive protein
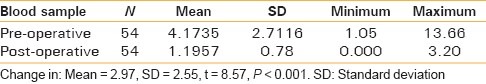
Table 2.
Clinical symptoms
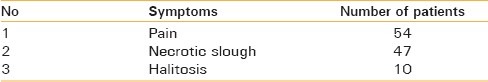
Table 3.
Associated clinical symptoms
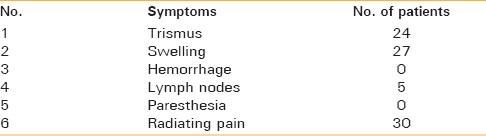
Table 4.
Days of onset of symptoms
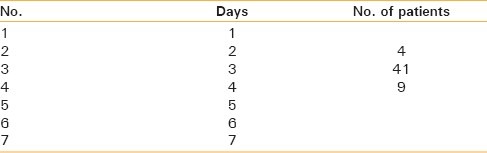
Table 5.
Resolution of symptoms
All the 54 patients had pain and necrotic slough and 18 patients had halitosis.
In 41 patients symptoms developed at 3rd day and 9 patients reported at 4th day after extraction.
Symptoms-resolutions of symptoms in 30 patients all the symptoms subsided at 5th day in other 16, patient on 6th day and in 3 patients on 8th day after extraction [Figures 1–3].
Figure 1.

Pre-treatment
Figure 3.

Clinical image after 2nd dressing
Figure 2.

Clinical image of dry socket after 1st dressing
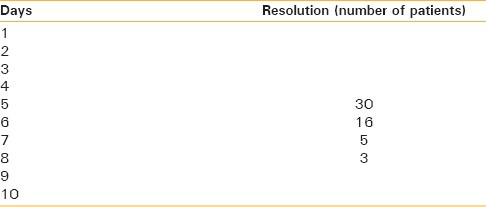
C-reactive protein (CRP) reduced significantly at post-operative.
The CRP levels are often elevated in patients with odontogenic infection and post-operative complications.[1] Rapid reductions in serum CRP level indicate successful treatment. It is a cytokine induced acute phase protein that increases in concentration as a result of inflammation. In our study, CRP reduced significantly at post-operative.
No adverse effect have been reported in the present study, honey has been used topically on wound over thousands of years without any adverse effect.
Allergy to honey is rare but there could be an allergic reaction to either the pollen or the bee protein in the honey. Honey gives a fast rate of tissue regeneration and suppression of inflammation, edema exudation and malodor in the wounds.
Honey can be expected to have a direct nutrient effect on regenerating tissues because it contains a wide range of amino acids, vitamins and trace elements in addition to large quantities of readily assimilable sugars.
DISCUSSION
Natural products have been used for several years in folk medicine. Honey has an effective antibacterial potential to combat oral pathogens and hold promises for the treatment of periodontal diseases and mouth ulcers. Honey was used to treat infected wounds as long ago as 2000 years before bacteria was discovered to be cause of infection. 50 AD Dioscorides described honey as being good for all rotten and hollow ulcers. Honey has been reported to have an inhibitory effect to around 60 species of bacteria including aerobes and anaerobes. Gram-positive and Gram negative microorganisms.[2]
The antibacterial property of honey was first recognized in 1892 by van Ketel. The minimum inhibitory concentration was found to a range from 1.8% to 10. 8% (v/v) indicating that the honey has sufficient antibacterial potency to stop bacterial growth if diluted at least 9 times due to its hygroscopic properties, its acidic pH and hydrogen peroxide.[2]
Glucose + H2 O + O2 → Gluconic acid + H2 O2. It serve to preserve the honey. The major antibacterial activity in honey has been found to be due to hydrogen peroxide produced enzymatically in the honey. Phytochemical factors it has enzyme and tissue nutrition material and vitamins that help repair tissue directly. The proliferation of peripheral blood B lymphocytes and T lymphocytes in cell culture is stimulated by honey at concentration as low as 0.1%. It all so stimulates monocytes in cell culture to release cytokines tumor necrosis factors-α, interleukin-1 (IL-1) and IL-6 which activate the immune response to infection.[2]
There are some other explanations of the antibacterial activity of the honey like.
Osmotic effect
The honey is saturated or supersaturated solution of the sugar 84% being the mixture of fructose or sucrose the water content is usually 15-21% by weight. The strong interaction of these molecules with water molecules leaves very few of the water molecules available for microorganisms. This free water is what is measured as water activity (aw) : m0 ean value for the honey have been reported from 0.562 to 0.62. Many species of bacteria have their growth completely inhibited if (aw) is in the range of 0>94-0.99.
Acidity - it is quite acidic its pH is from 3.2 to 4.5, low enough to be inhibitory for many pathogens.
Hydrogen peroxide
The major antibacterial activity in honey has been found to be due to hydrogen peroxide enzymatically in the honey. The glucose oxide enzyme is secreted from the hypo pharyngeal gland of the bee in to the nectar to assist in the formation of honey from the nectar.
Glucose + H2 O2 + O2 → Gluconic acid + H2 O2. This serves to preserve the honey. The hydrogen peroxide produced would be the effect as a sterilizing agent only during ripening of the honey. Full strength honey has a negligible level of hydrogen peroxide because this substance is short lived in the presence of transition metal ions and ascorbic acid in the honey which catalyzes its decomposition to water and oxygen. On dilution of honey the activity increases by a factor of 2500-50,000 thus giving a slow release antiseptic at a level which is antibacterial but not tissue damaging.[2,3]
Phytochemical factors
All the antibacterial activity does not account for peroxide generating system it shows that there must be an additional antibacterial factor involved. several chemicals with antibacterial activity has been identified in the honey by various researches, pinocembrin, terpenes, benzyol alcohol, 3,5-dimethoxy-4-hrdroxy benzoic acid, methyl 3,5-dimothoxy 4-hydroxy benzoiate, 3,45 trimethoxy benzoic acid, 2 hydroxy, 3 phenyl propoinic acid, 2 hydrobenzioc acid and 1,4 dihrdroxy benzene.
It appears that the honey from certain plants has better antibacterial properties than from others but there are no sufficient evidence.[3]
It has been reported from various clinical studies on the uses of honey as dressing for the infected wounds that the wounds become sterile in 3-6 days and other reported that honey is effective in cleaning up infective wounds. It has also been reported that the honey dressing halt advancing necrosis. It has also been found to act as a barrier preventing wounds from becoming infected, preventing cross infection and allowing burn wound to heal rapidly. Honey has been reported to promote the formation of clean healthy granulation tissues. It all so reduces inflammation, reduced hyperemia, edema, exudation and soothing effect when applied to wounds.[2,3] Hence its physical properties provide a protective barrier, by osmosis, create moist healing environment, in the form of the solution, not to stick underlying tissue. The antibacterial properties of honey prevents bacterial colonization, of the moist environment and no impairment of the healing process through adverse effect on wound tissue to the contrary it appears to have a stimulatory effect on tissue regeneration.[4,5,6] There are clean indication of anti-inflammatory action, so this can be used as a therapeutic agent for the dry socket.
CONCLUSIONS
There are no side-effects of honey. Excess use of euginol, can lead to necrosis of bone. The honey can be used as a medicament for the management of dry socket.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.C-reactive protein. [Last accessed on 2014 Jul 9]. Available from: http://www.nlm.nih.gov/medlineplus/ency/article/003356 .
- 2.Molan PC. The antibacterial activity of honey. [Last accessed on 2011 Apr 10];The nature of antibacterial activity. Bee World. 1992 73:5–28. Available from: http://www.worldwidewounds.com/2001/november/Molan/honey-as-topical-agent.html . [Google Scholar]
- 3.Namias N. Honey in the management of infections. Surg Infect (Larchmt) 2003;4:219–26. doi: 10.1089/109629603766957022. [DOI] [PubMed] [Google Scholar]
- 4.Cooper RA, Molan PC. Honey in wound care. J Wound Care. 1999;8:340. doi: 10.12968/jowc.1999.8.7.26179. [DOI] [PubMed] [Google Scholar]
- 5.Molan PC. Potential of honey in the treatment of wounds and burns. Am J Clin Dermatol. 2001;2:13–9. doi: 10.2165/00128071-200102010-00003. [DOI] [PubMed] [Google Scholar]
- 6.Green AE. Wound healing properties of honey. Br J Surg. 1988;75:1278. doi: 10.1002/bjs.1800750718. [DOI] [PubMed] [Google Scholar]


