Abstract
Ameloblastoma or adamantinoma is the rarest of the three forms of tumor of the odontogenic type. They are benign, locally aggressive neoplasms arising from ameloblasts, which typically occur at the angle of the mandible, and are often associated with an un-erupted tooth and must, therefore, be differentiated from a dentigerous cyst which will be centered on the crown. When in the maxilla (less common), they are located in the premolar region, and can extend up in the maxillary sinus. Ameloblastoma is reported to constitute about 1-3% of tumors and cysts of the jaws. The tumor is by far more common in the mandible than in the maxilla and shows predilection for various parts of the mandible in different racial groups. The relative frequency of the mandible to maxilla is reported as varying from 80-20% to 99-1%. Here, we are representing a case of ameloblastoma of anterior mandible which was considered as a rare site of occurrence.
Keywords: Ameloblastoma, anterior mandible, rare
INTRODUCTION
Ameloblastoma is a benign, slow growing, locally invasive odontogenic tumor.[1] It is the second most common odontogenic neoplasm. It accounts for 11% of all odontogenic tumors. It occurs in all age groups but the lesion is most commonly diagnosed in the third and fourth decades.[2] Exact etiology of ameloblastoma is not known. Ameloblastoma may arise from: Cell rest of enamel organ either remnant of dental lamina or remnant of Hertwigs sheath; epithelium of odontogenic cyst; and disturbances of developing enamel organ.[3] The tumor frequently develops in the mandible (80%), maxilla (16%) while peripheral adamantinoma located in the soft tissue account for remaining 4%.[4] In the mandible, it frequently involves molar and mandibular angle (70%), premolar (20%), and rarely anterior region (10%).[4] The tumor is usually asymptomatic, painless, and present with bony deformity. Wide surgical excision with adequate safe margins is the treatment of choice. We present a rare case ameloblastoma of anterior mandible arising from symphysis. Segmental resection of mandible was done and stabilized with reconstruction plates.
CASE REPORT
A 60-year-old lady reported to the Department of Oral and Maxillofacial Surgery (OMFS) with chief complaint of swelling at anterior region of mandible since 6 months. Patient gave history of trauma at chin region due to Road Traffic Accident (RTA) 3 years back. At that time, patient was conservatively managed by some private clinician. After 6 months of trauma, patient noticed an extra oral swelling over anterior mandible with pus discharge intraorally. After 1 year of time, patient noticed loosening of mandibular anterior teeth. Patient again went to a private clinician where she was again conservatively managed with medication. Since past 2 years pus used to appear intermittently from same place, which used to stop on use of antibiotics. But since last 6 months, there is gradual increase in swelling of anterior mandible for which patient reported to OMFS department where patient was examined, evaluated and incisional biopsy of lesion was done which was suggestive of ameloblastoma. Then patient was admitted to OMFS ward for further management.
Extra-oral inspection showed a large swelling in anterior region of mandible over chin area crossing midline, measuring approximately 8 × 7 cm in size. Face was asymmetrical, deviated towards left. Scar mark was present over right side of chin. Color of the overlying skin was normal. On palpation, the swelling was bony hard. It was non-compressible, non-fluctuant, and slightly tender. Temperature of overlying skin was normal. Swelling extends to involve bilateral body of mandible [Figure 1].
Figure 1.

Extraoral photograph of patient
Intra-oral inspection showed a large swelling seen involving buccal vestibule, floor of the mouth, and lower alveolus region. Mouth opening was adequate. On palpation, intraoral swelling was hard and mild tender. Sinus opening with respect to lower right and left canine (may be socket of teeth). There was bleeding from lower left canine region on palpation [Figure 2].
Figure 2.

Intraoral photograph of patient
Incisional biopsy revealed epithelial islands admixed with fibrocollagenous tissue. Outermost layer of epithelial island was composed of tall columnar cells with polarization of the nuclei away from the basement membrane. The central portion of the island was composed of loose network of cells showing squamous metaplasia [Figure 3].
Figure 3.
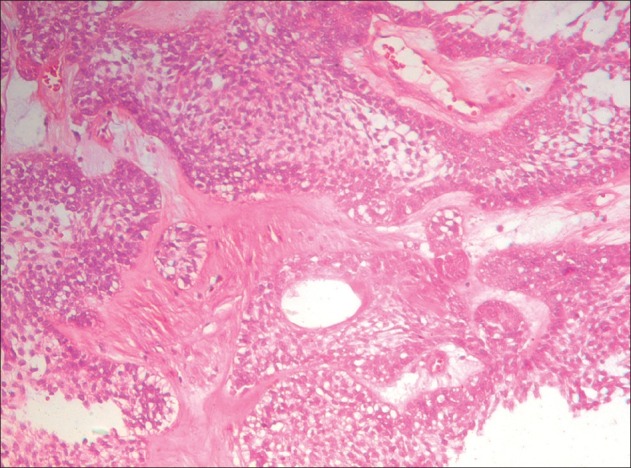
Histopathological picture
Orthopantomogram (OPG) of mandible showed multilocular expansile lytic lesion involving the symphysis and bilateral body of mandible. All mandibular teeth were lost except one molar tooth on either side [Figure 4].
Figure 4.

Orthopantogram of patient
Computed tomography (CT) scan revealed: Plain and contrast axial and coronal CT scans of face region revealed large multiloculated cystic expansile lesions arising from symphysis menti and bilateral body of mandible, and extending up to bilateral angle of mandible. Margins of the lesions were sclerotic and scalloped. Overlying all mandibular teeth was lost except one molar tooth on either side. Bilateral masseter muscles and tongue was normal in CT attenuation and dimensions. No obvious cervical lymphadenopathy [Figures 5 and 6].
Figure 5.
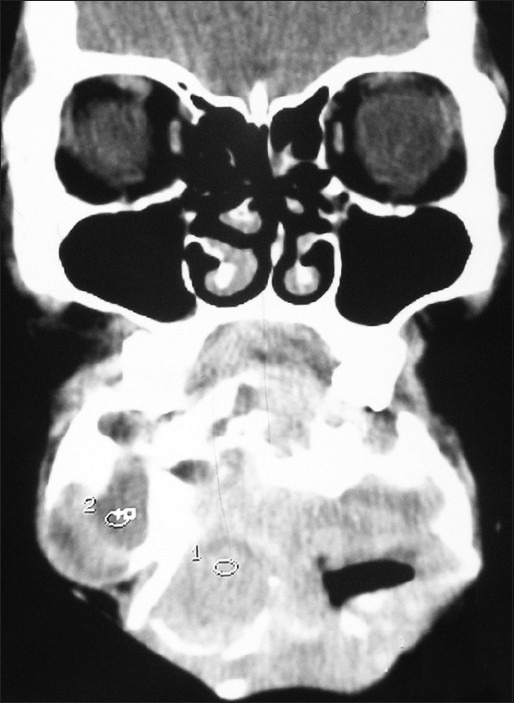
CT scan-coronal view
Figure 6.
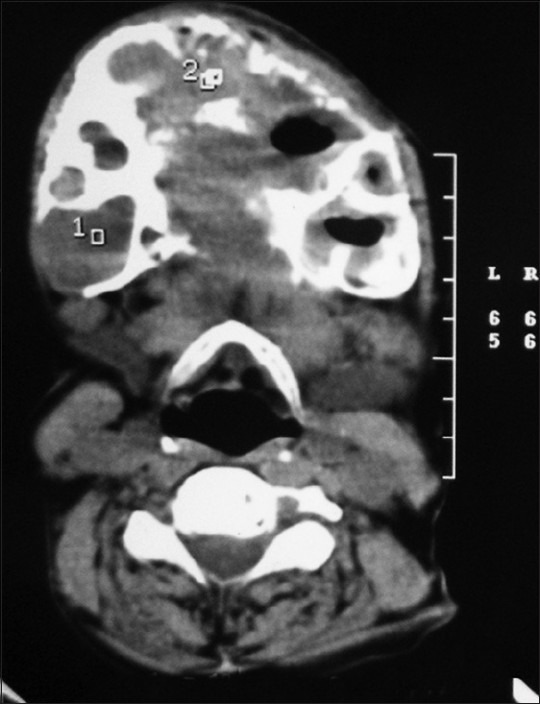
CT scan-axial view
On the basis of above findings, resection of mandible and reconstruction with reconstruction plate was planned, under general anesthesia. The mandible was resected bilaterally at the body. The specimen was taken out and the defect was reconstructed using reconstruction plate. The genioglosus and the geniohyoid muscles were tied to the reconstruction plate and the incision was closed [Figures 7–9].
Figure 7.
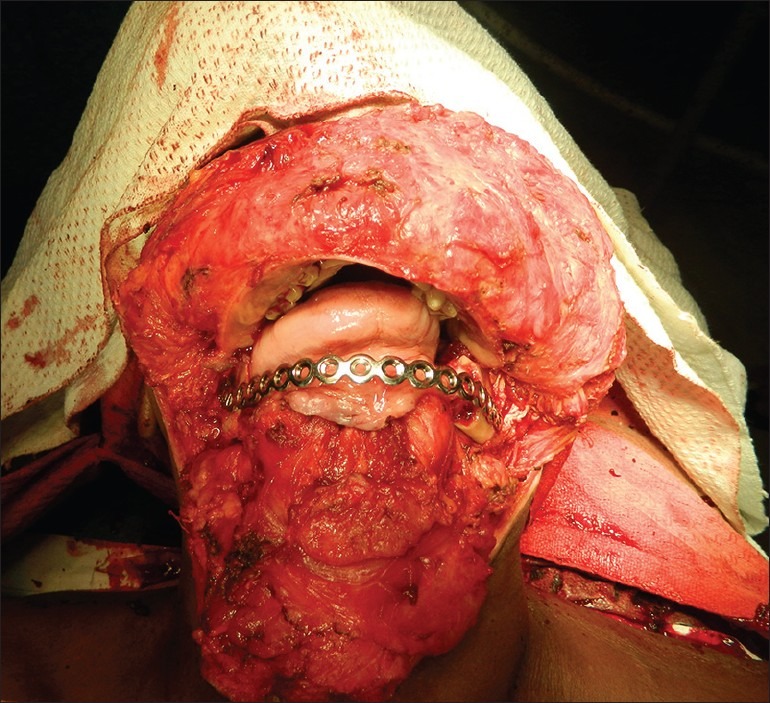
Intraoperative photograph of patient
Figure 9.

Postoperative photograph of patient
Figure 8.

Postoperative orthopantogram of patient
Histopathological findings of excised specimen confirmed the diagnosis of ameloblastoma.
DISCUSSION
Ameloblastoma or admantinoma is a benign odontogenic tumor of epithelial origin. It was described in 1827 by Cusack and designated as an adamantinoma in 1885 by the French physician Louis-Charles Malassez and renamed as ameloblastoma in 1930 by Ivey and Churchill.[5]
Ameloblastoma are seen in wide range of age but are usually diagnosed between the 4th and 5th decades of life except in unicystic variety (20-30 years). No gender predominance is noted.[6] However, some workers have seen involvements of females frequently.
Etiology of ameloblastoma is unknown. In most cases, ameloblastoma are usually asymptomatic and found on routine x-rays; when they attain considerable size then they present with jaw expansion. They may cause displacement of tooth or root resorption. In our case, patient had lower jaw swelling with bony deformity and gradual spontaneous fall of lower central incisor and canine teeth, difficulty in chewing of food.
Radiologically, ameloblastoma are osteolytic, being usually lucent and frequently multilocular with well-defined sclerotic margins which may appear scalloped or expand the cortical plate, tooth roots may move or be resorbed.[7] Approximately, 80% of the tumors are found in the mandible.[8,9] The maxilla is infrequently affected. It occurs in the posterior maxilla in 98% of cases and anterior in 2%. The molar/ramus area is the most frequently involved in Japanese[10,11] and Whites[12] more than 70% of the ameloblastomas involve this region. In blacks, ameloblastomas occur more frequently in the anterior region of the jaws.[12]
These are histologically classified into follicular, granular, plexiform, desmoplastic, basal cell, and acanthomatous variety.[13] Diagnosis is usually made by fine needle aspiration, which reveals palisaded basal cell layer with stellate reticulum like epithelium. Differential diagnosis of ameloblastomas includes calcifying epithelial odontogenic tumor (CEOT), odontogenic myxoma, central giant cell granuloma, or ameloblastic fibroma.
Different treatment modalities are surgical excision, enucleation, curettage, cryotherapy, radiotherapy, and chemotherapy. Wide surgical excision with safe margins is the preferred treatment method. Surgical excision is treatment of choice and involves complete removal of tumor with negative margin of 15-20 mm.[4]
Ameloblastomas are well-known for its recurrence. Lau et al., reported that recurrence rates were 3.6% for wide resection, 30.5% for enucleation, and 16% for enucleation followed by use of Carnoy's solution.[14] Several factors influences in rate of recurrence which includes clinicopathological variant of tumor, anatomic site, safe margins during surgery, and histological variant. There are three variant of ameloblastoma designated as solid or multicystic or conventional, unicystic, and peripheral. The solid variety has the greatest propensity for local infiltration and recurrence.[2] The dense cortical bone of the mandible prevents the tumor from spread than maxilla.[15] Inadequate surgical margins are frequent cause of recurrence. Treatment of ameloblastoma by curettage leave small tumor island in bone, which may later cause recurrence.[16]
Role of radiotherapy, as a useful treatment modality in case ameloblastoma, is not established.[17] Role of chemotherapy is not yet well-defined, however, few reports showed little response with Cisplatin and Paclitaxel.[18]
Malignant transformations of ameloblastoma are rarely seen, accounting for less than 1% of cases. Malignant ameloblastoma may arise de novo or transformation of pre-existing ameloblastoma. Most common site of spread are lung, cervical lymph nodes, and rarely brain.[19]
Due to high rate of recurrence of ameloblastoma, long-term follow up is recommended for more than 10 years. Regular follow up of the patient should be done, irrespective of the treatment done.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Torres-Lagares D, Infante-Cossío P, Hernández-Guisado JM, Gutiérrez-Pérez JL. Mandibular ameloblastoma. A review of the literature and presentation of six cases. Med Oral Patol Oral Cir Bucal. 2005;10:231–8. [PubMed] [Google Scholar]
- 2.Adekeye EO, Lavery KM. Recurrent ameloblastoma of the maxillo-facial region. Clinical features and treatment. J Maxillofac Surg. 1986;14:153–7. doi: 10.1016/s0301-0503(86)80282-x. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. WHO classification of tumours: Textbook of Oral Pathology. In: Levy SH, editor. Cyst and Tumour of Odontogenic Origin. 4th ed. Geneva: WHO; 2010. p. 277. [Google Scholar]
- 4.Niedzielska I, Pajak J, Langowska-Adamczyk H. Szkliwiak Szczeki-opisdwoch przypadkow I przeglad pismiennictwa. Czas Stomatol. 2004;57:255–60. [Google Scholar]
- 5.Malassez L. Sur le role des debris epitheliaux papdentaires. Arch Physiol Norm Pathol. 1885;6:379–449. [Google Scholar]
- 6.Stanley HR, Diehl DL. Ameloblastoma potential of follicular cysts. Oral Surg Oral Med Oral Pathol. 1965;20:260–8. doi: 10.1016/0030-4220(65)90200-8. [DOI] [PubMed] [Google Scholar]
- 7.Ueda M, Kaneda T. Combined chemotherapy and radiotherapy for advanced maxillary ameloblastoma. A case report. J Craniomaxillofac Surg. 1991;19:272–4. doi: 10.1016/s1010-5182(05)80069-1. [DOI] [PubMed] [Google Scholar]
- 8.Robinson HB. Ameloblastoma: A survey of the 379 cases of the literatures. Arch Pathol. 1937;23:831–43. [Google Scholar]
- 9.Olaitan AA, Adekeye EO. Unicystic ameloblastoma of the mandible: A long-term follow-up. J Oral Maxillofac Surg. 1997;55:345–8. doi: 10.1016/s0278-2391(97)90122-1. [DOI] [PubMed] [Google Scholar]
- 10.Ueno S, Nakamura S, Mushimoto K, Shirasu R. A clinicopathologic study of ameloblastoma. J Oral Maxillofac Surg. 1986;44:361–5. doi: 10.1016/s0278-2391(86)80031-3. [DOI] [PubMed] [Google Scholar]
- 11.Kameyama Y, Takehana S, Mizohata M, Nonobe K, Hara M, Kawai T, Fukaya M. A clinicopathological study of ameloblastomas. Int J Oral Maxillofac Surg. 1987;16:706–12. doi: 10.1016/s0901-5027(87)80057-7. [DOI] [PubMed] [Google Scholar]
- 12.Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: Biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31:86–99. doi: 10.1016/0964-1955(94)00037-5. [DOI] [PubMed] [Google Scholar]
- 13.Grucia B, Stauffer E, Buser D, Bornstein M. Ameloblastoma of the follicular, plexiform and acanthomatous type in the maxillary sinus: A case report. Quintessence Int. 2003;34:311–4. [PubMed] [Google Scholar]
- 14.Lau SL, Samman N. Recurrence related to treatment modalities of unicystic ameloblastoma: A systematic review. Int J Oral Maxillofac Surg. 2006;35:681–90. doi: 10.1016/j.ijom.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 15.Gardner DG, Pecak AM. The treatment of ameloblastoma based on pathologic and anatomic principles. Cancer. 1980;46:2514–9. doi: 10.1002/1097-0142(19801201)46:11<2514::aid-cncr2820461133>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 16.Montoro JR, Tavares MG, Melo DH, Franco Rde L, Mello-Filho FV, Xavier SP, et al. Mandibular ameloblastoma treated by bone resection and immediate reconstruction. Braz J Otorhinolaryngol. 2008;74:155–7. doi: 10.1016/S1808-8694(15)30768-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anastassov GE, Rodriguez ED, Adamo AK, Friedman JM. Case report. Aggressive ameloblastoma treated with radiotherapy, surgical ablation and reconstruction. J Am Dent Assoc. 1998;129:84–7. doi: 10.14219/jada.archive.1998.0025. [DOI] [PubMed] [Google Scholar]
- 18.Grunwald V, Le Blanc S, Karstens JH, Weihkopf T, Kuske M, Ganser A, et al. Metastatic malignant ameloblastoma responding to chemotherapy with paclitaxel and carboplatin. Ann Oncol. 2001;12:1489–91. doi: 10.1023/a:1012522929861. [DOI] [PubMed] [Google Scholar]
- 19.Bachmann AM, Linfesty RL. Ameloblastoma, solid/multicystic type. Head Neck Pathol. 2009;3:307–9. doi: 10.1007/s12105-009-0144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


